Abstract
Introduction:
NRG/RTOG 1203 compared 3-D conformal radiotherapy (3D CRT) to intensity-modulated radiotherapy (IMRT) in patients with endometrial or cervical cancer requiring postoperative radiotherapy after hysterectomy. The purpose of this study was to report the first quality-adjusted survival analysis comparing the two treatments.
Methods:
NRG/RTOG 1203 randomized patients having undergone hysterectomy to either 3DCRT or IMRT. Stratification factors included RT dose, chemotherapy, and disease site. The EQ-5D, both index and visual analog scale (VAS), were obtained at baseline, 5 weeks after the start of RT, 4-6 weeks post RT and 1 and 3-years post RT. EQ-5D index and VAS scores along with quality-adjusted survival (QAS) were compared between treatment arms using the t-test at a two-sided significance level of 0.05.
Results:
NRG/RTOG 1203 enrolled 289 patients of which 236 consented to participate in the patient reported outcome (PRO) assessments. QAS was higher in women treated with IMRT, 1374 vs 1333 days (p=0.5) compared to patients treated with 3DCRT, but this difference was not statistically different. Patients treated with IMRT had less of a decline in VAS score 5 weeks post RT, −5.04, compared to patients treated with 3DCRT, −7.48, although not statistically significant (p=0.38).
Conclusion:
This is the first report of the use of the EQ-5D comparing two radiotherapy techniques in the treatment of gynecologic malignancies after surgery. While there were no significant differences in QAS and VAS scores between patients who received IMRT vs. 3DCRT, RTOG 1203 was not powered to show statistical differences in these secondary endpoints.
Keywords: Utilities, Intensity modulated radiotherapy (IMRT), patient reported outcomes, endometrial cancer, cervical cancer
Introduction
NRG Oncology-RTOG 1203 was a randomized phase III trial comparing standard four field pelvic radiotherapy (3DCRT) to intensity modulated radiotherapy (IMRT) in patients with cervix cancer or endometrial adenocarcinoma after hysterectomy. The primary endpoint of the trial was change in patient-reported acute GI toxicity from baseline to the end of radiation (RT) as measured by the bowel domain of the Expanded Prostate Cancer Index Composite instrument (EPIC). The mean EPIC bowel score declined more in patients treated with 3DCRT compared to patients treated with IMRT, 23.6 vs 18.6, respectively, (p=0.048).1 In addition, a statistical significant drop in the mean EPIC urinary score was found in women treated with 3DCRT as compared to women treated with IMRT, 10.4 vs 5.6 points respectively (p=0.03). Finally, at the end of radiotherapy, women treated with 3DCRT more commonly reported frequent or almost constant diarrhea as compared to women treated with IMRT, 51.9% vs 33.7% respectively, (p=0.01) and more frequent antidiarrheal medication use, 20.4% vs 7.8% respectively (p=0.04).
A secondary end point included a measure of quality adjusted survival (QAS) as measured by the EQ-5D instrument. QAS takes into account not only length of survival but also the quality of survival as perceived by the patient and is measured by multiplying survival measured in months or years by a factor measuring the quality of survival, usually ranging from 0 representing death to 1 for full health. So, for example, if a patient survived 1 year but felt the quality of survival was only .75 of full health their QAS would be 0.75 years. The premise of using IMRT is the advanced technology would be better able to spare normal tissues, such as bowel and bladder, and therefore improve quality of life by reducing toxicity such as diarrhea and urinary frequency. IMRT was found to result in clinically meaningful and statistically better QOL scores in some domains in a randomized controlled trial comparing to IMRT to 3DCRT in patients with head and neck cancer.2 The EQ-5D instrument has been used to measure health states in patients with gynecologic malignancies. Janda et al and Ferguson et al used the EQ-5D to evaluate patient reported outcomes (PRO) in comparing various surgical procedures in patients with Stage I endometrial cancer.3,4 Another study compared surgery and no vaginal brachytherapy to surgery and vaginal brachytherapy in patients with stage I endometrial cancer 1 year after surgery.5
The purpose of this analysis was to report the first QAS analysis comparing IMRT to 3D-CRT in the treatment of gynecologic malignancies after surgery. The results of this study could be used to inform a cost-effectiveness analysis comparing the two treatment techniques given the cost difference between the two radiotherapy treatment techniques.
Methods
Patients with endometrial or cervical cancer undergoing hysterectomy and requiring postoperative radiotherapy were randomized between 3D-CRT or IMRT. Stratification variables included radiotherapy dose (45 vs 50.4Gy), chemotherapy (none vs 5 cycles of weekly cisplatin at 40mg/m2) and disease site (endometrial vs cervix). The primary endpoint of the study was to determine if IMRT reduced acute gastrointestinal toxicity in the 5th week after pelvic radiotherapy as measured by the EPIC questionnaire and has already been reported.1 Measuring QAS was among the secondary objectives.
The EQ-5D is a validated, standardized instrument measuring generic health status. The instrument is completed by the patient having both an index score, ranging from 0 for death and 1 for perfect health, and a visual analog scale (VAS) measuring 10cm long ranging from 0-100 with 100 representing perfect health. There are 5 dimensions, measuring mobility, self-care, usual activities, pain/discomfort and anxiety/depression with each dimension having 3 response levels, no problems, some problems, and extreme problems. This results in the possibility of 243 unique health state combinations.
QAS was calculated by measuring patient reported utilities and then multiplying the utilities as determined by the index score by the time interval in days between measurements and was restricted to those patients completing the EQ-5D at baseline and at least 1 follow-up assessment. Utilities were obtained at baseline, 5 weeks after start of therapy, 4-6 weeks, 1 year and 3 years after completion of therapy. Patients were given the option of opting out of the QAS portion of the study. Pretreatment characteristics were compared between those patients completing the EQ-5D at baseline and at least 1 follow-up assessment to those who did not. Between group comparisons were performed using the t-test for continuous variables and chi-square test for categorical variables at a two-sided significance of 0.05. A linear mixed effects model was used to assess the effect of EQ-5D index score across time while adjusting for other factors including baseline score, treatment arm, time, and stratification factors. Change scores used only completed assessments within the time window while QAS and the mixed effects models used all completed assessments.
Results
A total of 289 patients enrolled of which 279 patients were deemed eligible. A separate consent form was required for participation in the patient reported outcome assessments with 236 eligible patients consenting. (Figure 1) Compliance rates for completion of the EQ-5D were >80% through 6 weeks post-RT and comparable between the two treatment arms. Compliance for IMRT and 3DCRT was 74% and 68% for 1 year and 44.5% and 52% for 3 years, respectively.
Figure 1:
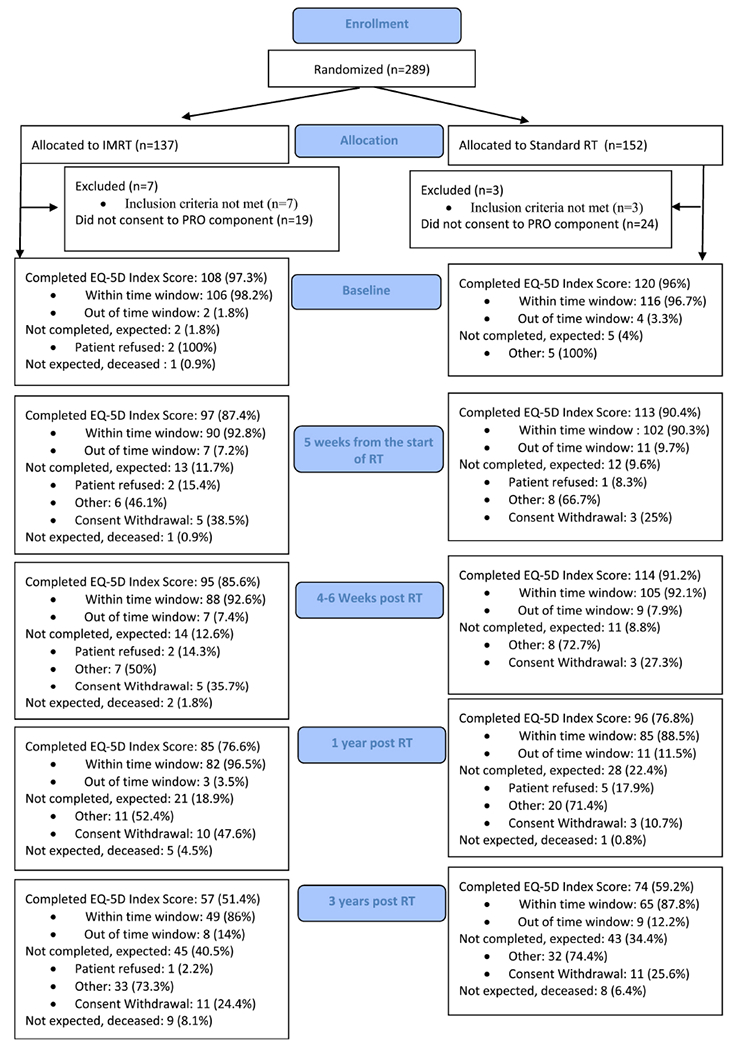
CONSORT Diagram
Figure 2 shows index and VAS scores at the different time points. No differences were noted between the treatment arms in either the index or VAS scores at baseline. There was no difference in change index or VAS scores from baseline to 5 weeks, 4-6 weeks, 1 year or 3 years post treatment between IMRT and 3DCRT. The linear mixed effects model for index score showed patients who did not report diarrhea had higher scores compared to those who did report diarrhea (estimate=−0.04, standard error [SE]=0.009, p<0.001) suggesting scores increase over time (estimate=0.008, SE=0.003, p=0.0126; Table 2A). The linear effects model for VAS score showed patients not receiving chemotherapy had higher VAS score compared to those receiving chemotherapy (estimate=5.15, SE=2.64, p=0.015; Table 2B), and patients who did not report diarrhea had higher VAS score compared to those reporting diarrhea (estimate=−0.64, SE1.05,p<00001). VAS score also increased over time (estimate=1.81, SE=0.33,p<0.001). Although not statistically significant, patients receiving IMRT had greater QAS compared to 3DCRT (mean=1374 days, standard deviation [SD]=478 vs. 1333 days, SD=409.6, p=0.5; Table 3).
Figure 2:
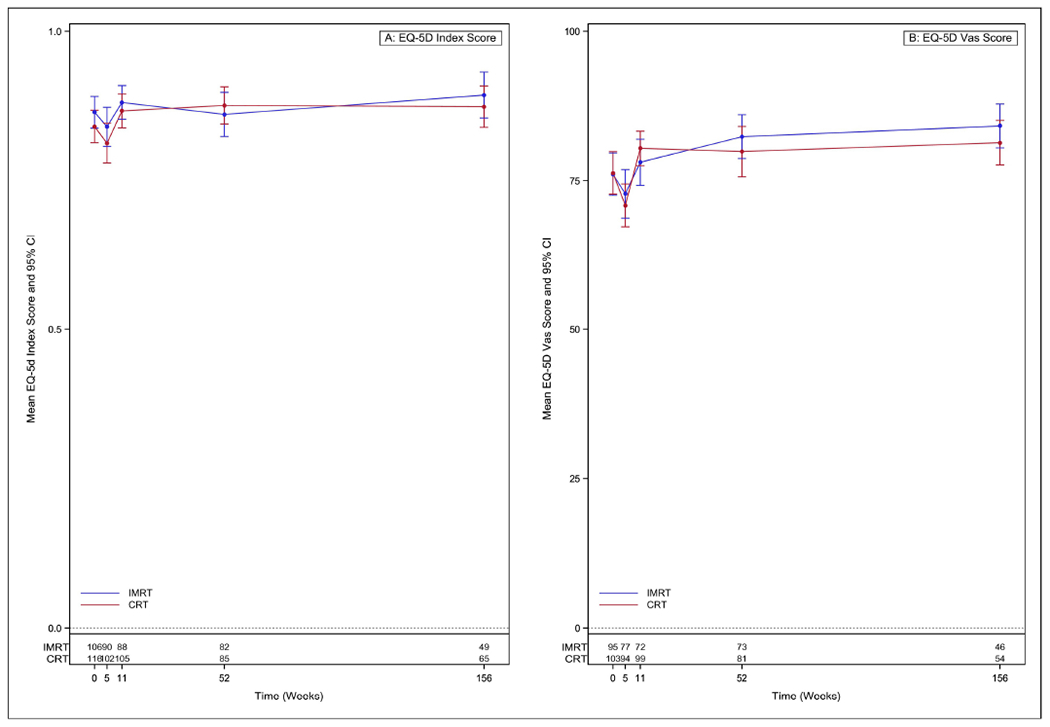
Mean index and Visual Analog Scale (VAS) scores across time.
Table 2.
Linear Mixed Effects Models for EQ-5D
| Variable | Estimate | Standard Error | p-value |
|---|---|---|---|
| A.EQ-5D Index Score | |||
| Diarrhea (Didn’t report) | −0.043 | 0.009 | <.0001 |
| Disease site (Cervix) | −0.002 | 0.023 | 0.92 |
| Chemotherapy (5 cycles of weekly cisplatin at 40 mg/m2) | 0.019 | 0.018 | 0.29 |
| Radiation dose (50.4 Gy) | −0.008 | 0.015 | 0.57 |
| Surgery (Laparoscopic Vaginal hysterectomy)* | −0.028 | 0.015 | 0.07 |
| Treatment Arm (IMRT) | −0.018 | 0.014 | 0.20 |
| Time | 0.008 | 0.003 | 0.0126 |
| B.EQ-5D VAS Score | |||
| Diarrhea (Didn’t report) | −6.431 | 1.054 | <.0001 |
| Disease site (Cervix) | −5.176 | 2.644 | 0.051 |
| Chemotherapy (5 cycles of weekly cisplatin at 40 mg/m2) | 5.150 | 2.105 | 0.015 |
| Radiation dose (50.4 Gy) | −1.070 | 1.670 | 0.52 |
| Surgery (Laparoscopic Vaginal hysterectomy)* | −2.965 | 1.741 | 0.09 |
| Treatment Arm (IMRT) | −2.034 | 1.635 | 0.21 |
| Time | 1.811 | 0.333 | <.0001 |
Outcome variable: EQ-5D index score at baseline, Week 3 of radiation, 5 weeks after start of radiation, 4-6 weeks post RT, 1-year and 3-year post-radiation. Reference levels are in parentheses for binary variables. IMRT=intensity-modulated radiation therapy.
Surgery was categorized into Laparoscopic assisted Vaginal hysterectomy vs. Other (TAH, Vaginal hysterectomy and Radical hysterectomy).
Table 3.
Quality-Adjusted Survival (QAS)
| IMRT (n=100) | CRT (n=116) | t-test p-value | |
|---|---|---|---|
| QAS | |||
| Mean (days) | 1374 | 1333 | 0.50 |
| Std. Dev. | 478.0 | 409.6 | |
| Median (days) | 1416 | 1340 | |
| Min - Max | 76.91 - 2422 | 369.0 - 2397 | |
| Q1 - Q3 | 1189 - 1708 | 1088 - 1523 |
Q1 = first quartile; Q3 = third quartile; IMRT=intensity-modulated radiation therapy; CRT=conventional radiation therapy.
Discussion
This is the first report of the use of the EQ-5D comparing two radiotherapy techniques in the treatment of gynecologic malignancies after surgery. The majority of reports have using the EQ-5D were in the comparison of different gynecologic surgical techniques. The EQ-5D was used to compare utility scores in patients with stage I endometrial cancer undergoing either total abdominal hysterectomy or total laparoscopic hysterectomy. Patients undergoing total laparoscopic hysterectomy had a 7.5% greater improvement in overall QOL compared to patients undergoing total abdominal hysterectomy.3 Similarly, Ferguson et al. used the EQ-5D comparing laparotomy, laparoscopic or robotic hysterectomy in patients with endometrial cancer. Patients undergoing minimally invasive surgery had less of a drop in index or VAS scores in the time intervals both immediately following surgery and long term after surgery compared to patients undergoing open surgeries.4 Damast et al. used the EQ-5D to evaluate QOL comparing surgery to vaginal brachytherapy in 205 survivors with stage I endometrial cancer. They found a significant correlation between Female Sexual Function Index (FSFI) and EQ5D-VAS score suggesting patients with improved sexual function had superior QOL.5
Two studies have reported the use of the EQ-5D instrument in patients with cervical cancer. Lang et al reported a mean EQ-5D index score of 0.87 in a cohort of patients in Taiwan with all stages of cervical cancer receiving various treatments.6 The survey was not longitudinal nor contemporaneous, occurring 3 months after treatment. In another study, EQ-5D index scores were obtained from a cohort of female nursing students in Japan. The investigators used hypothetical scenarios describing different stages of cervical cancer both at diagnosis and after treatment. Significant differences in scores were identified between stage IB1 and more advanced stages.7
This is the first study using the EQ-5D evaluating and comparing IMRT to 3DCRT in women with endometrial or cervical cancer. In addition, this is the first study to longitudinally collect utility scores three years post-treatment although compliance with PRO completion dropped to around 50%, a limitation of the study. An additional limitation is that the endpoint was secondary and not powered for significance. Thus, we interpret with caution the finding that this study did not find a significant between-arm difference in either utility or VAS scores at any time point or when analyzed longitudinally. The mixed linear effects model did find a significant difference across time in index scores between IMRT and 3DCRT irrespective of treatment arm, with the index scores increasing over time. A similar result was noted in the VAS score as well. Of interest is the 41-day difference in QAS (p=0.5) between patients treated with IMRT compared to 3DCRT. Patients treated with IMRT had more than a month greater quality adjusted survival compared to 3DCRT, although the large variance made this difference not statistically significant.
A potential criticism of this study is that the EQ-5D may not be sensitive enough to detect changes in health states. O Ceilleachair et al. make this point in a systematic review on the use of EQ-5D in patients with cervical disease.8 They posit the EQ-5D may not be sensitive to changes in health states given only 3 response options to the questions. Lang et al, however, concluded when compared to the EORTC QLQ-C30, the EQ-5D was reliable and valid for the assessment of health related quality of life in patients with cervical cancer.6 The introduction of the new EQ-5D-5L may help address this potential criticism by offering 5 instead of 3 response options. In addition, the group which designs the EQ-5D are developing disease and anatomic specific “bolt-ons” to improve the sensitivity of the EQ-5D. This may help to further improve the sensitivity of this instrument.9
This first of a kind study has reported longitudinal utility and VAS scores up to 3 years after treatment which can be used to inform the cost-effectiveness of the use of IMRT in the treatment of gynecologic malignancies. Though not statistically significant, a 41-day improvement in quality adjusted survival was seen in patients treated with IMRT. Future studies powered for quality-adjusted survival would further clarify improvements in quality-adjusted survival with IMRT’s use.
Table 1.
Pretreatment characteristics between patients who completed Baseline and at least 1 follow-up EQ-5D vs. those who did not
| Not Completed EQ-5D (n=61) |
Completed EQ-5D (n=218) |
p-value† | |
|---|---|---|---|
| Age (Years) | |||
| Median | 60 | 62 | 0.48§ |
| Min - Max | 29 - 81 | 28 - 83 | |
| Q1 - Q3 | 54 - 66 | 54 - 68 | |
| Gender | |||
| Female | 61 (100.0%) | 218 (100.0%) | |
| Race | White vs Other | 0.0087 | |
| American Indian or Alaskan Native | 0 ( 0.0%) | 4 ( 1.8%) | |
| Asian | 13 ( 21.3%) | 16 ( 7.3%) | |
| Black or African American | 7 ( 11.5%) | 19 ( 8.7%) | |
| Native Hawaiian or Other Pacific Islander | 1 ( 1.6%) | 1 ( 0.5%) | |
| White | 39 ( 63.9%) | 171 ( 78.4%) | |
| Unknown | 1 ( 1.6%) | 7 ( 3.2%) | |
| Ethnicity | |||
| Hispanic or Latino | 12 ( 19.7%) | 10 ( 4.6%) | 0.0005 ** |
| Not Hispanic or Latino | 49 ( 80.3%) | 204 ( 93.6%) | |
| Unknown | 0 ( 0.0%) | 4 ( 1.8%) | |
| Zubrod | 0 vs 1-2 | 0.24 | |
| 0 | 41 ( 67.2%) | 163 ( 74.8%) | |
| 1 | 20 ( 32.8%) | 50 ( 22.9%) | |
| 2 | 0 ( 0.0%) | 5 ( 2.3%) | |
| Surgical Resection | TAH,Vaginal,Radical vs Laparoscopic | 0.0174 | |
| TAH | 36 ( 59.0%) | 91 ( 41.7%) | |
| Vaginal hysterectomy | 3 ( 4.9%) | 4 ( 1.8%) | |
| Radical hysterectomy | 10 ( 16.4%) | 45 ( 20.6%) | |
| Laparoscopic assisted vaginal hysterectomy | 12 ( 19.7%) | 78 ( 35.8%) | |
| XRT dose* | |||
| 45 GY | 32 ( 52.5%) | 129 ( 59.2%) | 0.35 |
| 50.4 GY | 29 ( 47.5%) | 89 ( 40.8%) | |
| Disease Site* | |||
| Endometrium | 50 ( 82.0%) | 184 ( 84.4%) | 0.65 |
| Cervix | 11 ( 18.0%) | 34 ( 15.6%) | |
| Chemotherapy* | |||
| No Chemotherapy | 50 ( 82.0%) | 158 ( 72.5%) | 0.13 |
| 5 cycles of weekly cisplatin at 40 mg/m2 | 11 ( 18.0%) | 60 ( 27.5%) | |
| Treatment Arm | |||
| IMRT | 30 ( 49.2%) | 100 ( 45.9%) | 0.67 |
| CRT | 31 ( 50.8%) | 118 ( 54.1%) | |
Stratification factor.
p-value from Chi-Square test
p-value from two-sided t-test
fishers exact test
Q1 = first quartile; Q3 = third quartile.
NRG 1203 Highlights.
The first randomized clinical trial comparing two types of radiotherapy in gynecologic malignancies.
Utilities were measured a priori to calculate quality-adjusted survival between the two treatment arms.
Although not powered for these endpoints, non-statistically significant improvements were seen with the use of IMRT.
Acknowledgments
This study was supported by grants UG1CA189867 (NCORP) from the National Cancer Institute (NCI).
Disclosure Statement:
Drs Cantuaria, Chang, Doncals, Ferguson, Haas, Kim, Kachnic, Konski, Klopp, Pugh, Kundapur, Mohan, Thompson, Yeung and Ms Deshmukh have nothing to declare. Dr Bruner declares since the initial planning of the work, PI - NRG NCORP. Dr D’Souza declares in the past 36 months Consulting fees from AstraZeneca. Dr Westin declares in the past 36 months grants or contracts from AstraZeneca, Bayer, Novartis, OncXerna, Clovis Oncology, Roche/Genentech, Cotinga Pharma, Zentalis, GSK and Mereo.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Klopp AH, Yeung AR, Deshmukh S, et al. : Patient-Reported Toxicity During Pelvic Intensity-Modulated Radiation Therapy: NRG Oncology-RTOG 1203. J Clin Oncol 36:2538–2544, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rathod S, Gupta T, Ghosh-Laskar S, et al. : Quality-of-life (QOL) outcomes in patients with head and neck squamous cell carcinoma (HNSCC) treated with intensity-modulated radiation therapy (IMRT) compared to three-dimensional conformal radiotherapy (3D-CRT): evidence from a prospective randomized study. Oral Oncol 49:634–42, 2013 [DOI] [PubMed] [Google Scholar]
- 3.Janda M, Gebski V, Brand A, et al. : Quality of life after total laparoscopic hysterectomy versus total abdominal hysterectomy for stage I endometrial cancer (LACE): a randomised trial. Lancet Oncol 11:772–80, 2010 [DOI] [PubMed] [Google Scholar]
- 4.Ferguson SE, Panzarella T, Lau S, et al. : Prospective cohort study comparing quality of life and sexual health outcomes between women undergoing robotic, laparoscopic and open surgery for endometrial cancer. Gynecol Oncol 149:476–483, 2018 [DOI] [PubMed] [Google Scholar]
- 5.Damast S, Alektiar K, Eaton A, et al. : Comparative patient-centered outcomes (health state and adverse sexual symptoms) between adjuvant brachytherapy versus no adjuvant brachytherapy in early stage endometrial cancer. Ann Surg Oncol 21:2740–54, 2014 [DOI] [PubMed] [Google Scholar]
- 6.Lang HC, Chang K, Ying YH: Quality of life, treatments, and patients’ willingness to pay for a complete remission of cervical cancer in Taiwan. Health Econ 21:1217–33, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Murasawa H, Konno R, Okubo I, et al. : Evaluation of health-related quality of life for hypothesized medical states associated with cervical cancer. Asian Pac J Cancer Prev 15:9679–85, 2014 [DOI] [PubMed] [Google Scholar]
- 8.O Ceilleachair A, O’Mahony JF, O’Connor M, et al. : Health-related quality of life as measured by the EQ-5D in the prevention, screening and management of cervical disease: A systematic review. Qual Life Res 26:2885–2897, 2017 [DOI] [PubMed] [Google Scholar]
- 9.Finch AP, Brazier J, Mukuria C: Selecting Bolt-on Dimensions for the EQ-5D: Testing the Impact of Hearing, Sleep, Cognition, Energy, and Relationships on Preferences Using Pairwise Choices. Med Decis Making 41:89–99, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]


