Abstract
Background:
Pre-exposure prophylaxis (PrEP) is effective in preventing human immunodeficiency virus (HIV) infection among sexual and gender minorities (SGM). We evaluated characteristics associated with engagement in seven steps of the PrEP cascade among SGM in Nigeria.
Methods:
SGM without HIV from the Abuja site of TRUST/RV368 cohort who were surveyed on awareness of and willingness to use PrEP were approached for PrEP initiation upon availability of oral daily PrEP. To understand gaps in the uptake of oral daily PrEP, we categorized the HIV PrEP cascade as (i) education about PrEP, (ii) interest in PrEP, (iii) successful contact, (iv) appointment scheduled, (v) appointment attendance, (vi) PrEP initiation, and (vii) plasma protective levels of tenofovir (TDF). Multivariable logistic regression models were used to determine factors associated with each of the seven steps in the HIV PrEP cascade.
Results:
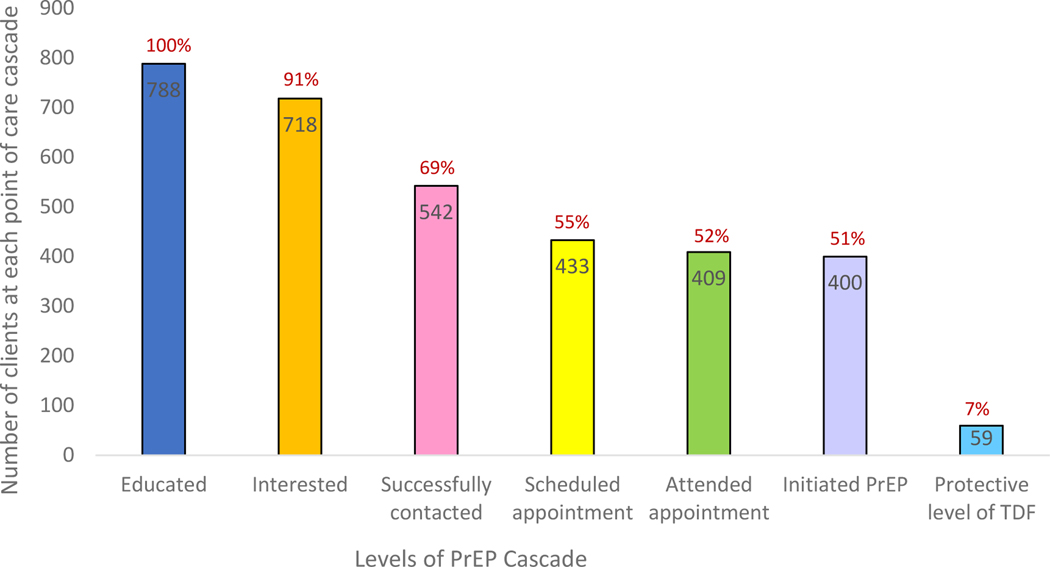
Of 788 participants, 718 (91.1%) showed interest in taking oral daily PrEP every day and/or after a sexual act, 542 (68.8%) were successfully contacted, 433 (54.9%) scheduled an appointment, 409 (51.9%) attended a scheduled appointment, 400 (50.8%) initiated oral daily PrEP, and 59 (7.4%) had protective levels of TDF. Of initiators of PrEP, 23 (5.8%) seroconverted at a rate of 13.9 cases/100 person-years. Better social support, larger network density, and higher education were associated with engagement in 4–5 components of the cascade.
Conclusions:
Our data highlight a gap between willingness and actual PrEP use. Despite PrEP’s effectiveness in preventing HIV, the optimal impact of PrEP for SGM in sub-Saharan Africa will require multifaceted approaches that combine social support, education, and de-stigmatization.
Keywords: Men who have sex with men, transgender women, PrEP cascade, HIV, sub-Saharan Africa
Short Summary
Our key population study in Nigeria found that better social support, larger network density, and higher education were associated with engagement in multiple steps of the PrEP cascade including uptake.
Introduction
With an estimated HIV incidence of 15.4/100 person years,1 men who have sex with men (MSM) account for one of the highest HIV incidences among members of key populations (KPs) in Nigeria. Interviews conducted by a human rights watch group showed that criminalizing same sex practices, and fear of isolation from society, compelled some KP members in Nigeria to marry or engage in heterosexual relationships, potentially as a means of concealing same-sex sexual practices.2 In our previous evaluation,3 we found that two-thirds of Nigerian MSM described themselves as bi-sexual, meaning that they have sex with both men and women. With a high prevalence and incidence of HIV and other sexually transmitted infections (STIs) among Nigerian MSM,4, 5 sexual interactions between MSM and women pose a risk of ongoing transmission throughout the population. Changing the course of HIV transmission requires appropriate use of pre-exposure prophylaxis (PrEP), post-exposure prophylaxis along with innovative methods to overcome structural, capacity-, and policy-related barriers.
Previous research has shown that oral daily PrEP is associated with a 96% reduction in the risk of contracting HIV among serodiscordant couples.6 Among MSM and transgender women (TGW) who adhere to PrEP more than 90% of the time, the risk of HIV transmission is reduced by 73%.7 Higher levels of PrEP adherence are associated with higher PrEP efficacy.8, 9 One systematic review showed that a higher proportion of HIV non-seroconverters have detectable plasma tenofovir disoproxil fumarate (TDF, a PrEP medication) than seroconverters, indicating a high level of adherence among non-seroconverters.10 Oral daily PrEP adherence among KP individuals in Africa has been low. For example, self-reported adherence in the Democratic Republic of Congo was 39%.11 A study done in Kenya showed that, among 76 MSM who reported use of oral daily PrEP, only 14.5% had protective levels of TDF in their plasma, and among five participants who seroconverted while on PrEP, only one had detectable, yet unprotective, levels of tenofovir.12
Despite the benefits of PrEP, several barriers to successful PrEP use have been documented, including stigma, the availability of HIV counseling and treatment services, possible drug-to-drug interactions, medication costs, lack of PrEP knowledge, and travel distance to the clinic.13, 14 Ability of KP individuals to network within their community, family or partner support, and less stress on condom use negotiations are potential enablers of oral daily PrEP uptake.15, 16 Most studies explored barriers and enablers associated with PrEP uptake—one of the components in the PrEP cascade. As new promising and innovative PrEP delivery options, such as injectables, vaginal films, microneedle patches, and subdermal implants emerge,17, 18 it is important to gain an understanding of the potential factors associated with engagement in the PrEP cascade prior to PrEP initiation. In this paper, we characterize engagement in and determinants of the stages of the PrEP cascade, ranging from interest in PrEP to receipt of oral daily PrEP medication among Nigerian MSM and TGW.
Materials and Methods:
Study design and population:
Since 2013, the TRUST/RV368 cohort has provided integrated prevention and treatment services for HIV and other STIs tailored to the needs of sexual and gender minorities in Abuja and Lagos, Nigeria, as previously described.19 In brief, participants were eligible if born male sex, aged ≥16 years, engaged in receptive or insertive anal intercourse in the past year and provided informed consent in English or Hausa. HIV testing and counseling was conducted at each three-month follow-up visit, and individuals found to be living with HIV underwent evaluation and initiated antiretroviral therapy (ART) per the test and treat strategy. At the Abuja site, a total of 788 MSM who tested HIV-negative completed a survey instrument on awareness and willingness to use oral daily PrEP. MSM who tested HIV-negative were approached and consented for oral daily PrEP initiation when oral daily PrEP medication became available in May 2018. The drugs used were a combination of tenofovir and emtricitabine (TDF/FTC). HIV testing and counseling was done prior to PrEP initiation and during study follow-up. PrEP medications were provided within the TRUST clinic on the same day of HIV testing. The study was approved by the University of Maryland, Baltimore Institutional Review Board (IRB)(HP-00052013), Baltimore, MD, USA; the Federal Capital Territory Health Research Ethics Committee, Abuja, Nigeria; and the Ministry of Defense Health Research Ethics Committee, Abuja, Nigeria.
Data collection
HIV-negative participants from the TRUST/RV368 cohort study were invited to discuss PrEP, and an interviewer-administered questionnaire was used to collect details on awareness and willingness to use oral daily PrEP. Because participants approached for PrEP discussions were part of TRUST/RV368 cohort, their other characteristics, such as demographics and network characteristics, were obtained from the parent cohort database. Blood samples were tested for HIV in real time using rapid HIV tests followed by the parallel testing algorithm for at-risk participants according to national guidelines with Determine first, Uni-gold second, and HIV1/2 Stat Pak as a tie-breaker for discrepant results.20 All participants who were diagnosed with HIV were offered treatment according to national guidelines.21 Because PrEP medications were not available at the time of assessment of PrEP awareness and willingness to use PrEP, those participants who showed interest in using PrEP were contacted by phone when medications became available. After PrEP initiation, follow-up visits were planned at months 1, 3, 6, and 9 during which blood samples were collected and archived. To determine the concentrations of TDF, stored plasma samples were used. Drug concentrations were determined via liquid chromatographic tandem mass spectrometry (LC151 MS/MS) analysis using previously validated assays.8, 22
Definition of Variables
To understand gaps at different levels of PrEP engagement, we categorized study participants as (i) those educated about PrEP, (ii) those who showed interest, (iii) those who were successfully contacted, (iv) those who scheduled appointments, (v) those who attended scheduled appointments, (vi) those who initiated oral daily PrEP, and (vii) those who had protective levels of TDF. Upon completion of the assessment of PrEP awareness, every study participant received basic education about PrEP from our study nurse. When asked if they were willing to use PrEP whenever PrEP medications became available, those who agreed were considered willing to use PrEP. When oral daily PrEP medications were available within the program, participants were contacted by phone to undergo evaluation and PrEP initiation. Those who spoke to our study team were considered successfully contacted. Of those successfully contacted, some made an appointment for further PrEP evaluation, and some of those individuals attended their scheduled appointments. Of those who were successfully evaluated after attending their appointments, some initiated oral daily PrEP. Of those who initiated oral daily PrEP, we assessed adherence using plasma protective levels of TDF. Drug concentrations of plasma TDF were determined via liquid chromatographic tandem mass spectrometry (LC-MS/MS) analysis, the assay lower limit of quantification was 0.31 ng/mls. Plasma levels of TDF were dichotomized at 4.2 ng/mL, based on the 90% sensitivity “inclusive” benchmark of plasma concentration for four tablets per week recommended for protective TDF concentration.22 We defined protective TDF concentration as plasma TDF concentration ≥4.2 ng/mL, irrespective of the visit at which sample was collected. We categorized participants by age and considered those ≤19 years to be in the younger age group, consistent with our previous work.23 All participants in the cohort were birth males and reported sex with men. We categorized participants as cisgender MSM, TGW, or other based on their self-reported gender identity of “man,” “woman,” or “other.”
Each study participant was asked to report up to five of their most recent MSM/TGW partners who they had interacted (i.e had sex with, social gathering e.t.c) with in the past six months. Potential connections were then computed based on the number of reported MSM/TGW partners. Network density was calculated as the total number of actual connections divided by the total number of potential connections, with higher proportions indicating larger network densities.24
Social support was defined as the extent of assistance an individual was likely to receive from friends in times of need, based on responses to five different social support questions, each measured using a Likert scale ranging from strongly disagree (0) to strongly agree (3). Scores were summed (score range: 0–15), and the Cronbach’s alpha was 0.83. For analyses, social support scores were dichotomized at the median with higher scores indicating stronger social support.
Latent class analysis was done to create a stigma index. The questions used to generate the stigma index included family-made discriminatory remarks, rejections from friends, refusal from police to protect them, verbal harassment, blackmail, physical violence, rape, fear of seeking health care, and fear of walking in public. Three categories of stigma (low, medium, high) were created from the stigma index as previously described.25
Depression was assessed using validated tool from self-reported information. Participants were asked if they ever felt sad or had depressed or low mood for more than two weeks at a time in the past three years. Depression was then categorized as ever depressed or never depressed.
Statistical analyses
Frequencies of categorical variables were calculated as the proportion of participants. Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for factors associated with PrEP interest, successfully contacted, scheduled appointment, attended scheduled appointment, oral daily PrEP initiation, and having plasma protective levels of TDF. Multivariable models included age, education, gender, concurrency partnership, participation in HIV prevention meetings, network density, social support, stigma, depression, and timing of assessment of PrEP willingness questionnaire. These variables were included in the multivariable model because of their plausible association with HIV risk that may influence an individual’s willingness to use oral daily PrEP. Each multivariable model included only individuals who were evaluated for the PrEP cascade characteristic being modeled. Dummy variables were created for missing data. Poison regression model was used to compute incidence rate of seroconversion. Two sensitivity analysis were performed (i) comparing characteristics of study participants who completed PrEP awareness questionnaire and those who didn’t complete (ii) comparing characteristics of study participants who had PrEP assessment before and those who had PrEP assessment after PrEP medication availability among those with detectable levels of TDF. Statistical analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC).
Results
Between May 2016 and November 2019, of 1,323 HIV-negative participants in the TRUST/RV368 cohort from the Abuja site, a total of 788 (59.6%) participants completed a survey for PrEP awareness and willingness to use oral daily PrEP. Of these, 718 (91.1%) indicated interest in taking PrEP every day and/or after a sexual act, 542 (68.8%) were successfully contacted for making appointments, 433 (54.9%) scheduled an appointment, 409 (51.9%) attended the scheduled appointment, 400 (50.8%) initiated oral daily PrEP, and 59 (7.5%) had protective levels of TDF (Figure 1). Of the 542 contacted, 133 participants did not attend an appointment because 43 (32.3%) lost interest, 24 (18.0%) promised to engage at a later date, and 30 (22.5%) perceived low HIV risk. The median age (interquartile range) of study participants was 23 (20–26) years. Among the study participants, 542 (68.8%) were 25 years or older and 419 (53.2%) had senior secondary school education (Table 1). Most study participants (620, 78.7%), were cis-gender MSM, 485 (61.5%) never participated in HIV prevention meetings, 345 (43.8%) reported high social support, and 463 (60.0%) felt a medium level of stigma. Of the 400 study participants who initiated PrEP, 23 (5.8%) seroconverted during follow up.
Figure 1:
PrEP Cascade among Nigerian MSM and TGW
Table 1:
Individual, structural and network characteristics at various stages of PrEP cascade among MSM at HIV prevention clinics, Abuja, Nigeria 2016 – 2019
| Characteristics | Total | Willing to initiate PrEP | Successfully contacted | Scheduled appointment | Attending scheduled appointment | Initiated PrEP | Protective levels of TDF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||
| N = 788 | n = 718 | n = 542 | n = 433 | n = 409 | n = 400 | n = 59 | ||||||||
|
|
||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
|
| ||||||||||||||
| Age | ||||||||||||||
| 16 – 19 | 177 | 22.5 | 159 | 89.8 | 104 | 58.8 | 90 | 50.9 | 87 | 49.2 | 85 | 48.0 | 7 | 19.4 |
| 20 – 24 | 69 | 8.8 | 65 | 94.2 | 54 | 78.3 | 44 | 63.8 | 38 | 55.1 | 36 | 52.2 | 5 | 41.7 |
| ≥ 25 | 542 | 68.8 | 494 | 91.2 | 384 | 70.9 | 299 | 55.2 | 284 | 52.4 | 279 | 51.2 | 49 | 33.1 |
| Education | ||||||||||||||
| < Senior sec school | 55 | 7.0 | 48 | 87.3 | 29 | 52.7 | 20 | 36.4 | 20 | 36.4 | 20 | 36.4 | 3 | 27.3 |
| Senior sec school | 419 | 53.2 | 389 | 92.8 | 278 | 66.4 | 234 | 55.9 | 221 | 52.7 | 215 | 51.3 | 26 | 28.3 |
| > Senior sec school | 267 | 33.9 | 240 | 89.9 | 217 | 81.3 | 163 | 61.1 | 153 | 57.3 | 150 | 56.2 | 29 | 37.2 |
| Missing | 47 | 6.0 | 41 | 87.2 | 18 | 38.3 | 16 | 34.0 | 15 | 31.9 | 15 | 31.9 | 1 | 11.1 |
| Cis gender | ||||||||||||||
| MSM | 620 | 78.7 | 564 | 91.0 | 445 | 71.8 | 349 | 56.9 | 334 | 53.9 | 326 | 52.6 | 49 | 32.7 |
| TGW | 58 | 7.4 | 53 | 91.4 | 43 | 74.1 | 37 | 63.8 | 35 | 60.3 | 34 | 58.6 | 4 | 20 |
| Others** | 76 | 9.6 | 71 | 93.4 | 49 | 64.5 | 43 | 56.6 | 36 | 47.4 | 36 | 47.4 | 5 | 26.3 |
| Missing | 34 | 4.3 | 30 | 88.2 | 5 | 14.7 | 4 | 11.8 | 4 | 11.8 | 4 | 11.8 | 1 | 100.0 |
| Concurrency last 12 months | ||||||||||||||
| No | 378 | 48.0 | 355 | 93.9 | 266 | 70.4 | 211 | 55.8 | 198 | 52.4 | 195 | 51.6 | 32 | 33.3 |
| Yes | 375 | 47.6 | 332 | 88.5 | 271 | 72.3 | 217 | 57.9 | 206 | 54.9 | 200 | 53.3 | 27 | 29.0 |
| Missing | 35 | 4.4 | 31 | 86.6 | 5 | 14.3 | 5 | 14.3 | 5 | 14.3 | 5 | 14.3 | 0 | 0.0 |
| Concurrency relationship now | ||||||||||||||
| No | 500 | 63.5 | 462 | 92.4 | 354 | 70.8 | 277 | 55.4 | 257 | 51.4 | 250 | 50.0 | 39 | 32.0 |
| Yes | 253 | 32.1 | 225 | 88.9 | 183 | 72.3 | 151 | 59.7 | 147 | 58.1 | 145 | 57.3 | 20 | 29.9 |
| Missing | 35 | 4.4 | 31 | 88.6 | 5 | 14.3 | 5 | 14.3 | 5 | 14.3 | 5 | 14.3 | 0 | 0.0 |
| Participation in HIV prevention meetings | ||||||||||||||
| No | 485 | 61.5 | 441 | 90.9 | 400 | 82.5 | 325 | 67.0 | 307 | 63.3 | 302 | 62.3 | 49 | 33.8 |
| Yes | 163 | 20.7 | 149 | 91.4 | 130 | 79.8 | 100 | 61.4 | 97 | 59.5 | 93 | 57.1 | 10 | 22.7 |
| Missing | 140 | 17.8 | 128 | 91.4 | 12 | 8.6 | 8 | 5.7 | 5 | 3.6 | 5 | 3.6 | 0 | 0.0 |
| Network density | ||||||||||||||
| < 50 % | 221 | 28.0 | 202 | 91.4 | 184 | 83.3 | 142 | 64.3 | 132 | 59.7 | 130 | 58.8 | 34 | 42.0 |
| ≥ 50 % | 267 | 33.9 | 242 | 90.6 | 217 | 81.3 | 170 | 63.7 | 161 | 60.3 | 156 | 58.4 | 21 | 24.7 |
| Missing | 300 | 38.1 | 274 | 91.3 | 141 | 40.3 | 121 | 40.3 | 116 | 38.7 | 114 | 38.0 | 4 | 16.7 |
| Social support score | ||||||||||||||
| < Median | 305 | 38.7 | 276 | 90.5 | 248 | 81.3 | 197 | 64.6 | 187 | 61.3 | 185 | 60.7 | 32 | 36.8 |
| ≥ Median | 345 | 43.8 | 316 | 91.6 | 284 | 82.3 | 230 | 66.7 | 219 | 63.5 | 212 | 61.5 | 27 | 26.6 |
| Missing | 138 | 17.5 | 126 | 91.3 | 10 | 7.2 | 6 | 4.3 | 3 | 4.3 | 3 | 4.3 | 0 | 0.0 |
| Stigma | ||||||||||||||
| Low | 48 | 6.1 | 45 | 93.8 | 29 | 60.4 | 22 | 45.8 | 18 | 37.5 | 18 | 37.5 | 6 | 60.0 |
| Medium | 463 | 58.8 | 428 | 92.4 | 332 | 71.7 | 270 | 58.3 | 255 | 55.1 | 247 | 53.5 | 36 | 28.3 |
| High | 228 | 28.9 | 203 | 89.0 | 162 | 71.0 | 124 | 54.4 | 119 | 52.2 | 118 | 51.8 | 15 | 34.9 |
| Missing | 49 | 6.2 | 42 | 85.7 | 19 | 38.8 | 17 | 34.7 | 17 | 34.7 | 17 | 34.7 | 2 | 20.0 |
| Ever had depression in the past 3 years | ||||||||||||||
| No | 755 | 95.8 | 687 | 91.0 | 524 | 68.1 | 414 | 54.8 | 394 | 52.2 | 386 | 51.1 | 51 | 28.7 |
| Yes | 33 | 4.2 | 31 | 93.9 | 28 | 84.9 | 19 | 57.6 | 15 | 45.5 | 14 | 42.4 | 8 | 66.7 |
| PrEP assessment after medication available | ||||||||||||||
| No | 305 | 38.7 | 272 | 89.1 | 211 | 69.2 | 134 | 43.9 | 112 | 36.7 | 108 | 35.4 | 36 | 43.4 |
| Yes | 483 | 61.3 | 446 | 92.3 | 231 | 68.5 | 299 | 61.9 | 297 | 61.5 | 292 | 60.5 | 23 | 21.5 |
Abbreviations: PrEP, Pre exposure prophylaxis; MSM, Men who have sex with men; TDF, Tenofovir
versatile or both man and woman
Timing of PrEP use questionnaire administration and the availability of oral daily PrEP medication
Of 788 study participants, 305 (38.7%) were assessed regarding their willingness to use oral daily PrEP before PrEP medications were available in the study (Table 1). For these participants, the median time (interquartile range) between the PrEP willingness assessment and PrEP medication availability was 10 (8–18) months. Among those who initiated PrEP, the median time (interquartile range) from PrEP initiation to plasma TDF assessment was 3 (3–6) months.
Engagement in PrEP cascade
A detailed description of the factors associated with each level of the PrEP cascade is presented in table 2. Participants aged 20–24 vs ≤ 19 years had higher odds of being successfully contacted and scheduling an appointment. Those with higher education, ≥ senior secondary school vs < senior secondary school were positively associated with willingness to initiate PrEP, being successfully contacted, scheduling an appointment, attending scheduled appointment and PrEP initiation. Individuals with higher network density and social support had higher odds of being successfully contacted, scheduling an appointment, attending scheduled appointment and initiating PrEP. Although participants whose PrEP willingness questionnaire was administered after oral daily PrEP medications were available had higher odds of scheduling an appointment, attending scheduled appointment and PrEP initiations, they were negatively associated with having protective levels of TDF. Participation in HIV prevention meetings was associated with lower odds of having protective levels of TDF. Those with medium levels of stigma were positively associated with being successfully contacted and attending scheduled appointment compared to those with low levels of stigma.
Table 2:
Multivariable logistic regression for factors Associated With being Successfully Contacted, Scheduled an Appointment, Attending an appointment, PrEP Initiation and having protective levels of Tenofovir Among HIV Negative MSM in Abuja, Nigeria, 2016– 2019:
| Willing to initiate PrEP | Successfully contacted | Scheduled appointment | Attending scheduled appointment | Initiated PrEP | Protective levels of TDF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Characteristic | aOR | 95%CI | aOR | 95%CI | aOR | 95%CI | aOR | 95%CI | aOR | 95%CI | aOR | 95%CI |
|
| ||||||||||||
| Age | ||||||||||||
| 16 – 19 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 20 – 24 | 1.70 | (0.54 – 5.31) | 2.67 | (1.30 – 5.50) | 2.00 | (1.06 – 3.75) | 1.44 | (0.78 – 2.65) | 1.32 | (0.72 – 2.42) | 2.00 | (0.46 – 8.84) |
| ≥ 25 | 1.30 | (0.68 – 2.47) | 1.24 | (0.80 – 1.92) | 1.15 | (0.76 – 1.72) | 1.10 | (0.74 – 1.64) | 1.12 | (0.75 – 1.66) | 1.41 | (0.50 – 3.96) |
| Education | ||||||||||||
| < Senior sec school | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Senior sec school | 2.03 | (1.10 – 4.12) | 1.93 | (1.18 – 3.15) | 1.84 | (1.13 – 1.98) | 1.72 | (1.06 – 2.78) | 1.64 | (1.01 – 1.65) | 1.90 | (0.46 – 7.87) |
| > Senior sec school | 1.23 | (0.54 – 2.79) | 4.22 | (2.38 – 7.50) | 2.25 | (1.32 – 3.84) | 2.03 | (1.19 – 3.46) | 1.97 | (1.16 – 3.34) | 2.24 | (0.55 – 9.12) |
| Cis gender | ||||||||||||
| MSM | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| TGW | 1.18 | (0.45 – 3.16) | 1.37 | (0.70 – 2.66) | 1.55 | (0.86 – 2.81) | 1.46 | (0.82 – 2.60) | 1.42 | (0.80 – 2.52) | 0.42 | (0.12 – 1.51) |
| Others** | 1.30 | (0.50 – 3.41) | 1.92 | (0.54 – 1.59) | 1.21 | (0.72 – 2.03) | 1.00 | (0.54 – 1.49) | 0.95 | (0.57 – 1.57) | 0.62 | (0.19 – 2.00) |
| Concurrency last 12 months | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 0.51 | (0.27 – 0.99) | 0.14 | (0.73 – 1.76) | 0.10 | (0.75 – 1.63) | 1.02 | (0.69 – 1.50) | 0.94 | (0.64 – 1.38) | 0.66 | (0.28 – 1.68) |
| Concurrency relationship now | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 0.98 | (0.52 – 1.85) | 1.05 | (0.66 – 1.68) | 1.16 | (0.77 – 1.76) | 1.34 | (0.89 – 2.02) | 0.94 | (0.64 – 1.38) | 1.48 | (0.56 – 3.96) |
| Participation in HIV prevention meetings | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.13 | (0.60 – 2.16) | 1.30 | (0.82 – 2.06) | 1.07 | (0.73 – 1.57) | 1.16 | (0.80 – 1.70) | 1.45 | (0.97 – 2.18) | 0.39 | (0.15 – 0.98) |
| Network density | ||||||||||||
| < 50 % | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| ≥ 50 % | 0.89 | (0.52 – 1.51) | 2.30 | (1.56 – 3.40) | 1.62 | (1.17 – 2.25) | 1.56 | (1.13 – 2.14) | 1.49 | (1.08 – 2.05) | 0.57 | (0.28 – 1.18) |
| Social support score | ||||||||||||
| < Median | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| ≥ Median | 1.17 | (0.69 – 1.96) | 02.87 | (2.00 – 4.13) | 2.23 | (1.63 – 3.06) | 2.18 | (1.60 – 2.96) | 2.04 | (1.50 – 2.77) | 0.87 | (0.43 – 1.76) |
| Stigma | ||||||||||||
| Low | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Medium | 1.20 | (0.52 – 2.81) | 1.80 | (1.03 – 3.13) | 1.61 | (0.95 – 2.73) | 1.74 | (1.03 – 2.95) | 1.62 | (0.96 – 2.73) | 0.32 | (0.09 – 1.14) |
| High | 0.86 | (0.36 – 2.07) | 1.57 | (0.87 – 2.83) | 1.27 | (0.72 – 2.21) | 1.48 | (0.84 – 2.57) | 1.48 | (0.84 – 2.57) | 0.62 | (0.16 – 2.42) |
| Depression in the past 3 years | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.73 | (0.39 – 7.65) | 1.98 | (0.68 – 5.74) | 1.08 | (1.49 – 2.37) | 0.67 | (1.31 – 1.41) | 0.61 | (0.29 – 1.28) | 2.06 | (0.51 – 8.36) |
| PrEP assessment after medication available | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Yes | 1.76 | (1.03 – 3.00) | 1.31 | (0.90 – 1.90) | 2.83 | (2.00 – 3.99) | 3.57 | (2.55 – 5.01) | 3.53 | (2.52 – 4.94) | 0.31 | (0.14 – 0.69) |
Abbreviations: aOR, adjusted odds ratio; CI, Confidence intervals; TDF, Tenofovir; Bolded, statistically significant results
, versatile or both man and woman
Sensitivity analysis: Comparison between participants who had baseline visit and completed survey questionnaire and those who had baseline visit but didn’t complete the survey questionnaire.
Enrollees in the cohort who had more than baseline visit and completed survey questionnaire (n=788) were significantly different from those who had baseline visit and didn’t complete survey questionnaire on certain characteristics. Those who did not complete the survey were more likely to be younger, had lower education level, currently being on concurrent partnerships, having larger network density, and social support score greater than the median. (Table 3)
Table 3.
Sensitivity analysis comparing characteristics of those who completed PrEP awareness questionnaire and those who didn’t complete.
| Characteristics | Completed survey questionnaire N = 788 | Did not complete survey questionnaire N = 535 | p value | ||
|---|---|---|---|---|---|
|
|
|||||
| n | % | n | % | ||
|
| |||||
| Age | |||||
| 16 – 19 | 177 | 22.5 | 182 | 34.0 | <0.001 |
| 20 – 24 | 69 | 8.8 | 78 | 14.5 | |
| ≥ 25 | 542 | 68.8 | 275 | 51.4 | |
| Education | |||||
| < Senior sec school | 55 | 7.4 | 176 | 33.0 | <0.001 |
| Senior sec school | 419 | 56.5 | 239 | 44.8 | |
| > Senior sec school | 267 | 36.0 | 118 | 22.1 | |
| Missing | 47 | 2 | |||
| Concurrency last 12 months | |||||
| No | 378 | 42.6 | 229 | 37.7 | 0.07 |
| Yes | 375 | 57.4 | 278 | 62.3 | |
| Missing | 35 | 28 | |||
| Concurrency relationship now | |||||
| No | 500 | 66.4 | 302 | 60.9 | <0.047 |
| Yes | 253 | 33.6 | 194 | 39.1 | |
| Missing | 35 | 28 | |||
| Participation in HIV prevention meetings | |||||
| No | 485 | 74.9 | 171 | 75.7 | 0.807 |
| Yes | 163 | 25.1 | 55 | 24.3 | |
| Missing | 140 | 309 | |||
| Network density | |||||
| < 50 % | 221 | 45.3 | 76 | 34.9 | <0.001 |
| ≥ 50 % | 267 | 54.7 | 142 | 65.1 | |
| Missing | 300 | 317 | |||
| Social support score | |||||
| < Median | 305 | 46.9 | 125 | 32.2 | <0.001 |
| ≥ Median | 345 | 53.1 | 263 | 67.8 | |
| Missing | 138 | 147 | |||
| Ever had depression in the past 3 years | |||||
| No | 755 | 95.8 | 500 | 93.5 | 0.057 |
| Yes | 33 | 4.2 | 35 | 6.5 | |
| HIV status of the recruiter | |||||
| Negative | 528 | 67.1 | 348 | 66.5 | 0.836 |
| Positive | 259 | 32.9 | 175 | 33.5 | |
| Missing | 1 | 12 | |||
Sensitivity analysis among study participants who had protective levels of TDF: Comparison between those who had PrEP assessment before and those who had PrEP assessment after PrEP medication availability
Although participants who completed survey assessment after the availability of PrEP medication were more likely to be younger, they had more social network density and social network support compared to those who completed survey assessment before the availability of PrEP medication (Table 4).
Table 4:
Sensitivity analysis among study participants who had protective levels of TDF: Comparison between those who had PrEP assessment before and those who had PrEP assessment after PrEP medication availability.
| Characteristics | Before PrEP medication availability N = 36 |
After PrEP medication availability N = 23 |
p-value | ||
|---|---|---|---|---|---|
|
|
|||||
| n | % | n | % | ||
|
| |||||
| Age | |||||
| 16 – 19 | 2 | 5.6 | 5 | 21.7 | < 0.001* |
| 20 – 24 | 3 | 8.3 | 2 | 8.7 | |
| ≥ 25 | 31 | 86.1 | 16 | 69.6 | |
| Education | |||||
| < Senior sec school | 3 | 8.3 | 0 | 0.0 | 0.048* |
| Senior sec school | 15 | 41.7 | 11 | 50.0 | |
| > Senior sec school | 18 | 50.0 | 11 | 50.0 | |
| Network density | |||||
| < 50 % | 24 | 66.7 | 10 | 52.6 | 0.308** |
| ≥ 50 % | 12 | 33.3 | 9 | 47.4 | |
| Social support score | |||||
| < Median | 23 | 63.9 | 9 | 39.1 | 0.062** |
| ≥ Median | 13 | 36.1 | 14 | 60.9 | |
Abbreviations: TDF, Tenofovir; PrEP, Pre exposure prophylaxis
Fishers exact p-value
Chi square p value
Discussion
Although there was a relatively low level of PrEP awareness among Nigerian MSM/TGW, 91% of participants were interested in using oral daily PrEP after learning of the medication. When oral daily PrEP medications became available, about 50% of study participants initiated, suggesting that willingness does not necessarily translate to actual oral daily PrEP uptake. We have identified factors influencing oral daily PrEP uptake–higher education, social support, and larger network density were associated with nearly all components of the PrEP cascade. Young individuals (16–19 years old) were less likely to be successfully contacted for PrEP discussions and to schedule appointments. The incidence of HIV among those initiated PrEP was 13.9 cases/100 person years compared to 20.0 cases/ 100 person years among TRUST cohort participants in Lagos site where PrEP was not implemented.1
Beyond individual characteristics, network characteristics play a role in the overall PrEP cascade. Participants reporting having better social support from their networks had increased odds of expressing interest of PrEP and initiating it. This finding is consistent with other research which has found that individuals who disclosed using oral daily PrEP to parents and other friend networks were more likely to continue using PrEP and had high levels of adherence.26
A notable barrier to PrEP uptake is stigma.26 Stigma related to using HIV medicines also affects PrEP use, as family members and friends might think individuals using oral daily PrEP are also among people living with HIV.27 PrEP use is also mistakenly associated with engagement in high-risk behaviors28, which creates another distinct form of stigma among individuals who would benefit from PrEP use.29 Those with better social support may be less concerned with stigma, leading to an increased likelihood of PrEP uptake. As evidenced in this analysis, compared to those with low levels of stigma, those with medium levels of stigma had higher odds of having been contacted and having attended a scheduled appointment. Although this association is contrary to the hypothesis, only 6% of the study participants experienced low levels of stigma. The proportion is small to serve as referent group. Despite having large number of study participants experiencing moderate to high levels of stigma, we were able to engage them within the TRUST cohort.
We also noted that participants with larger network density tended to have higher odds of all components of the PrEP cascade. This can be attributed to two factors. First, higher network density may explain higher social network support. Alternatively, higher network density may also mean having a higher number of sexual partners and a higher perceived risk of HIV acquisition. In addition to condom use, PrEP is considered an extra protective layer among MSM reporting multiple partners.30 Screening for PrEP eligibility may help providers identify people at increased risk of acquiring HIV who also have low PrEP uptake potential; this screening may help integrate PrEP discussions into every clinic encounter.
PrEP uptake in this cohort was consistently low and may need an alternative strategy to daily use to increase effectiveness of PrEP. One possibility to consider for the cohort is on demand PrEP 2–1-1 where users take two pills between 2 and 24 hours before having sex, then a pill a day, allowing an interval of 24 hours each, for the next two subsequent days. This type of regimen has shown to increase PrEP uptake,31 and may be worth exploring in Nigeria.
Although others showed high proportions of KP individuals willing to take PrEP 11, stigma, frequency of HIV testing, and adherence to oral daily PrEP are some of the challenges to PrEP in African setting.14 We showed low protective plasma levels of TDF similar to prior studies on PrEP.12, 32 Long acting injectables may shift the paradigm to address these challenges of PrEP uptake and continuation in sub-Saharan Africa. Evaluations of determinants of the PrEP cascade may be critical among persons receiving long acting injectables as these determinants may be different from those of oral daily PrEP. We observed low protective levels of TDF among TGW compared to MSM. Fears of negative effect of ART on feminizing hormones may have impacted low levels of TDF among TGW, and this would be important data to collect in further studies.
A limitation of this study was the time between administering the PrEP willingness questionnaire to the actual availability of oral daily PrEP medication; this period affected nearly 40% of the study participants. Due to this gap, some of the participants who completed questionnaires could not be traced and others lost interest in PrEP discussions. This time difference between administration of the PrEP willingness questionnaire and actual availability of PrEP medication may under-estimate daily PrEP uptake. Our analysis showed individuals whose willingness questionnaire was administered when oral daily PrEP medications were available were more likely to schedule an appointment, attend a scheduled appointment, and initiate PrEP. When assessing sexual network, each study participant was asked to report up to five of his most recent MSM/TGW partners. This limited our ability to explore potential female partners of MSM. The main strength of this study is its exploration of the factors associated with multiple components of the PrEP cascade, rather than only evaluating oral daily PrEP initiation. Depression was assessed using a few depressive components of the validated tool. Comprehensive assessment would be conducted using entire PHQ9 tool which was implemented at a later stage of the study cohort.
Conclusion
Successful PrEP use has the potential to reduce incidence of HIV among MSM and TGW in Nigeria; however, the optimal impact of PrEP as an appropriate prevention strategy, especially among KP individuals, has yet to be made clear. This study demonstrates that individual and network factors are associated with the overall processes of the PrEP cascade. Potential gaps exist between PrEP willingness and actual PrEP use. Improvement of oral daily PrEP uptake will require multifaceted approaches that combine social support, education, and de-stigmatization.
Supplementary Material
Acknowledgements
The TRUST/RV368 Study Group includes Principal Investigators: Manhattan Charurat (IHV, University of Maryland, Baltimore, MD, USA), Julie Ake (MHRP, Walter Reed Army Institute of Research, Silver Spring, MD, USA); Co-Investigators: Aka Abayomi, Sylvia Adebajo, Stefan Baral, Trevor Crowell, Charlotte Gaydos, Fengming Hu, Afoke Kokogho, Kara Lombardi, Jennifer Malia, Olumide Makanjuola, Nelson Michael, Nicaise Ndembi, , Rebecca Nowak, Oluwasolape Olawore, Zahra Parker, Sheila Peel, Habib Ramadhani, Merlin Robb, Cristina Rodriguez-Hart, Eric Sanders-Buell, Elizabeth Shoyemi, Abdulwasiu Tiamiyu, Sodsai Tovanabutra, Sandhya Vasan; Institutions: Institute of Human Virology at the University of Maryland School of Medicine (IHV-UMB), Johns Hopkins Bloomberg School of Public Health (JHSPH), Johns Hopkins University School of Medicine (JHUSOM), U.S. Military HIV Research Program (MHRP), Walter Reed Army Institute of Research (WRAIR), Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF), Henry M. Jackson Foundation Medical Research International (HJFMRI), Institute of Human Virology Nigeria (IHVN), International Centre for Advocacy for the Right to Health (ICARH), The Initiative for Equal Rights (TIERS), Population Council Nigeria
Sources of funding support: This work was supported by cooperative agreements between the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., and the U.S. Department of Defense [W81XWH-11-2-0174, W81XWH-18-2-0040]; the National Institutes of Health [R01 MH099001, R01 AI120913, R01 MH110358]; Fogarty Epidemiology Research Training for Public Health Impact in Nigeria program [D43TW010051]; and the President’s Emergency Plan for AIDS Relief through a cooperative agreement between the Department of Health and Human Services/Centers for Disease Control and Prevention, Global AIDS Program, and the Institute for Human Virology-Nigeria [NU2GGH002099]. and Gilead Sciences, Inc (ISR IN-EU-276-4468). The views expressed are those of the authors and should not be construed to represent the positions of the U.S. Army, the Department of Defense, the Department of Health and Human Services, or the Henry M. Jackson Foundation for the Advancement of Military Medicine. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70-25.
Footnotes
Conflict of interest: None declared.
Disclaimer
The views expressed are those of the authors and should not be construed to represent the positions of the U.S. Army, the Department of Defense, the Department of Health and Human Services, or the Henry M. Jackson Foundation for the Advancement of Military Medicine. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70–25
References
- 1.Nowak RG, Mitchell A, Crowell TA, et al. Individual and Sexual Network Predictors of HIV Incidence Among Men Who Have Sex With Men in Nigeria. J Acquir Immune Defic Syndr. Apr 1 2019;80(4):444–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. https://www.hrw.org/report/2016/10/20/tell-me-where-i-can-be-safe/impact-nigerias-same-sexmarriage-prohibition-act . [Google Scholar]
- 3.Ramadhani HO, Ndembi N, Nowak RG, et al. Individual and Network Factors Associated With HIV Care Continuum Outcomes Among Nigerian MSM Accessing Health Care Services. J Acquir Immune Defic Syndr. Sep 1 2018;79(1):e7–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keshinro B, Crowell TA, Nowak RG, et al. High prevalence of HIV, chlamydia and gonorrhoea among men who have sex with men and transgender women attending trusted community centres in Abuja and Lagos, Nigeria. J Int AIDS Soc. 2016;19(1):21270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramadhani HO, Liu H, Nowak RG, et al. Sexual partner characteristics and incident rectal Neisseria gonorrhoeae and Chlamydia trachomatis infections among gay men and other men who have sex with men (MSM): a prospective cohort in Abuja and Lagos, Nigeria. Sex Transm Infect. Aug 2017;93(5):348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyperendemic settings. Aids. Mar 13 2010;24(5):729–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. Dec 30 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donnell D, Baeten JM, Bumpus NN, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J Acquir Immune Defic Syndr. Jul 1 2014;66(3):340–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. Sep 12 2012;4(151):151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sidebottom D, Ekström AM, Strömdahl S. A systematic review of adherence to oral pre-exposure prophylaxis for HIV - how can we improve uptake and adherence? BMC Infect Dis. Nov 16 2018;18(1):581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franks J, Teasdale C, Olsen H, et al. PrEP for key populations: results from the first PrEP demonstration project in the Democratic Republic of the Congo. AIDS Care. Mar 2022;34(3):359–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wahome EW, Graham SM, Thiong’o AN, et al. PrEP uptake and adherence in relation to HIV-1 incidence among Kenyan men who have sex with men. EClinicalMedicine. Sep 2020;26:100541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mayer CM, Owaraganise A, Kabami J, et al. Distance to clinic is a barrier to PrEP uptake and visit attendance in a community in rural Uganda. J Int AIDS Soc. Apr 2019;22(4):e25276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emmanuel G, Folayan M, Undelikwe G, et al. Community perspectives on barriers and challenges to HIV pre-exposure prophylaxis access by men who have sex with men and female sex workers access in Nigeria. BMC Public Health. Jan 15 2020;20(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Durosinmi-Etti O, Nwala EK, Oki F, et al. Communication needs for improved uptake of PrEP and HIVST services among key populations in Nigeria: a mixed-method study. AIDS Res Ther. Nov 20 2021;18(1):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gombe MM, Cakouros BE, Ncube G, et al. Key barriers and enablers associated with uptake and continuation of oral pre-exposure prophylaxis (PrEP) in the public sector in Zimbabwe: Qualitative perspectives of general population clients at high risk for HIV. PLoS One. 2020;15(1):e0227632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patki M, Vartak R, Jablonski J, et al. Efavirenz nanomicelles loaded vaginal film (EZ film) for preexposure prophylaxis (PrEP) of HIV. Colloids Surf B Biointerfaces. Jun 6 2020;194:111174. [DOI] [PubMed] [Google Scholar]
- 18.Coelho LE, Torres TS, Veloso VG, et al. Pre-exposure prophylaxis 2.0: new drugs and technologies in the pipeline. Lancet HIV. Nov 2019;6(11):e788–e799. [DOI] [PubMed] [Google Scholar]
- 19.Charurat ME, Emmanuel B, Akolo C, et al. Uptake of treatment as prevention for HIV and continuum of care among HIV-positive men who have sex with men in Nigeria. J Acquir Immune Defic Syndr. Mar 1 2015;68 Suppl 2(Suppl 2):S114–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bassey O, Bond K, Adedeji A, et al. Evaluation of nine HIV rapid test kits to develop a national HIV testing algorithm in Nigeria. African Journal of Laboratory Medicine. 2015;4(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Guidelines For HIV and AIDS Treatment and Care in Adolescents and Adults. https://www.who.int/hiv/pub/guidelines/nigeria_art.pdf [Google Scholar]
- 22.Hendrix CW, Andrade A, Bumpus NN, et al. Dose Frequency Ranging Pharmacokinetic Study of Tenofovir-Emtricitabine After Directly Observed Dosing in Healthy Volunteers to Establish Adherence Benchmarks (HPTN 066). AIDS Res Hum Retroviruses. Jan 2016;32(1):32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramadhani HO, Ndembi N, Nowak RG, et al. Individual and Network Factors Associated with HIV Care Continuum Outcomes Among Nigerian MSM Accessing HealthCare Services. J Acquir Immune Defic Syndr. May 16 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guida J, Hu L, Liu H. The Impact of Occupational Stigma on the Social Networks of Older Female Sex Workers: Results from a Three-Site Egocentric Network Study in China. AIDS Patient Care STDS. Jan 2016;30(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez-Hart C, Nowak RG, Musci R, et al. Pathways from sexual stigma to incident HIV and sexually transmitted infections among Nigerian MSM. Aids. Nov 13 2017;31(17):2415–2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehrotra ML, Rivet Amico K, McMahan V, et al. The Role of Social Relationships in PrEP Uptake and Use Among Transgender Women and Men Who Have Sex with Men. AIDS Behav. Nov 2018;22(11):3673–3680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rael CT, Martinez M, Giguere R, et al. Barriers and Facilitators to Oral PrEP Use Among Transgender Women in New York City. AIDS Behav. Nov 2018;22(11):3627–3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luehring-Jones P, Palfai TP, Tahaney KD, et al. Pre-Exposure Prophylaxis (PrEP) Use is Associated With Health Risk Behaviors Among Moderate- and Heavy-Drinking MSM. AIDS Educ Prev. Oct 2019;31(5):452–462. [DOI] [PubMed] [Google Scholar]
- 29.Dubov A, Galbo P Jr., Altice FL, et al. Stigma and Shame Experiences by MSM Who Take PrEP for HIV Prevention: A Qualitative Study. Am J Mens Health. Nov 2018;12(6):1843–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pillay D, Stankevitz K, Lanham M, et al. Factors influencing uptake, continuation, and discontinuation of oral PrEP among clients at sex worker and MSM facilities in South Africa. PLoS One. 2020;15(4):e0228620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.