Abstract
Background:
Recreational cannabis laws (RCLs) may have spillover effects on binge drinking. Our aims were to investigate binge drinking time trends and the association between RCLs and changes in binge drinking in the United States (U.S.)
Methods:
We used restricted National Survey on Drug Use and Health data (2008–2019). We examined trends in the prevalence of past-month binge drinking by age groups (12–20, 21–30, 31–40, 41–50, 51+). Then, we compared model-based prevalences of past-month binge drinking before and after RCL by age group, using multi-level logistic regression with state random intercepts, an RCL by age group interaction term, and controlling for state alcohol policies.
Results:
Binge drinking declined overall from 2008 to 2019 among people aged 12–20 (17.54% to 11.08%), and those aged 21–30 (43.66% to 40.22%). However, binge drinking increased among people aged 31+ (ages 31–40: 28.11% to 33.34%, ages 41–50: 25.48% to 28.32%, ages 51+: 13.28% to 16.75%). When investigating model-based prevalences after versus before RCL, binge drinking decreased among people aged 12–20 (prevalence difference=−4.8%; adjusted odds ratio (aOR)=0.77, [95% confidence interval (CI) 0.70–0.85]), and increased among participants aged 31–40 (+1.7%; 1.09[1.01–1.26]), 41–50 (+2.5; 1.15[1.05–1.26]) and 51+ (+1.8%; 1.17[1.06–1.30]). No RCL-related changes were noted in respondents ages 21–30.
Conclusions:
Implementation of RCLs was associated with increased past-month binge drinking in adults aged 31+ and decreased past-month binge drinking in those aged < 21. As the cannabis legislative landscape continues to change in the U.S., efforts to minimize harms related to binge drinking are critical.
Keywords: Recreational cannabis laws (RCLs), binge drinking, state alcohol policies, adolescence
1. Introduction
Binge drinking is prevalent in the United States (U.S.) and is associated with adverse short- and long-term negative outcomes (Hingson and Zha, 2018; Jennings et al., 2015; Sacks et al., 2015). In 2019, approximately one in four people ages 12 or older in the U.S. reported past-month binge drinking (Lipari, 2019), defined as ≥ 5 drinks for men or ≥ 4 drinks for women per drinking session (National Institute on Alcohol Abuse and Alcoholism, NIAAA). Binge drinking is associated with acute adverse outcomes such as motor vehicle crashes and traffic fatalities, criminal legal system exposure (Hingson and Zha, 2018; Sacks et al., 2015), poor academic achievement (Jennings et al., 2015; Patte et al., 2017), and emergency department visits (White et al., 2018). Further, detrimental chronic effects of binge drinking include alcohol use disorders (AUD) (Dawson et al., 2008, 2005), alcohol-related liver disease, and death (Esser et al., 2020; White et al., 2020).
Trends in binge drinking prevalence vary by age (Lipari, 2019); thus, it is necessary to evaluate changes in the prevalence of binge drinking separately among adolescents (Clark Goings et al., 2019), young adults (Delker et al., 2016), middle-aged adults (Grucza et al., 2018) and older adults (Al-Rousan et al., 2022; Han et al., 2017). For example, past-month binge drinking declined from 11.1% to 4.7% in adolescents aged 12–17 years old from 2002 to 2016 (Clark Goings et al., 2019), while the prevalence of adult binge drinking increased by 0.7% annually on average over 10–15 years (Grucza et al., 2018). The average annual increases in binge drinking were higher among people ages 30–49 and over 50 years old (Grucza et al., 2018), an age group that has also experienced increases in alcohol-related deaths and emergency department visits (Esser et al., 2020; White et al., 2020, 2018). Past-month binge drinking has increased among middle-aged and older adults from 2005 to 2019 (Al-Rousan et al., 2022; Han et al., 2017) and can contribute to a unique set of alcohol-related problems such as insomnia, alcohol interaction with prescription medications, unintentional injuries (e.g., falls), and worsened chronic disease management in this age group (Breslow et al., 2017, 2015; Canham et al., 2015). Cannabis and alcohol policies are environmental factors that can influence binge drinking behavior by influencing the availability and risk perception of substance use (Guttmannova et al., 2016; Kim et al., 2021; Pacula et al., 2022; Smart and Pacula, 2019). However, these studies did not investigate the impact of changes in cannabis policies on binge drinking prevalence while considering modifications to alcohol policies (Al-Rousan et al., 2022; Clark Goings et al., 2019; Grucza et al., 2018; Han et al., 2017).
Prior research has shown the impact of legalizing cannabis on the perception and availability of cannabis use (Compton et al., 2019; Hasin et al., 2017; Levy et al., 2021; Martins et al., 2016) and in changes in alcohol use patterns, including binge drinking and alcohol and cannabis co-use (Gonçalves et al., 2022; Guttmannova et al., 2016; Kim et al., 2021; Pacula et al., 2022; Smart and Pacula, 2019). The current literature supports two possible hypotheses: the complementary and the substitution hypotheses. Under complementarity, both cannabis and alcohol use may increase after cannabis legalization as individuals use these substances together. Under substitution, alcohol use may decrease after cannabis legalization, as individuals may use cannabis instead of alcohol when both are readily available (Guttmannova et al., 2016; Kim et al., 2021; Pacula et al., 2022; Smart and Pacula, 2019). Evidence regarding these hypotheses remains inconclusive, especially regarding how cannabis legalization may impact binge drinking across different age groups (Guttmannova et al., 2016; Pacula et al., 2022; Smart and Pacula, 2019).
The impact of cannabis laws on binge drinking among different age groups remains inconclusive. Studies examining the relationship between medical cannabis laws (MCLs) and binge drinking among adolescents are inconsistent (Smart and Pacula, 2019). One study showed no change in binge alcohol use among individuals ages 12–20 years (Wen et al., 2015), while two studies showed decreases in past-month binge drinking among different adolescent subgroups (Cerdá et al., 2018; Johnson et al., 2018). More specifically, one study found a decreased prevalence of binge drinking among 8th graders following MCL enactment but no change in prevalence among 10th and 12th graders (Cerdá et al., 2018). These findings were consistent with another study finding MCLs were not associated with changes in binge drinking among 9th-12th graders (Chapman et al., 2016). However, less restrictive MCLs (i.e., difficulty in obtaining approval for medical cannabis, the quantity of cannabis permitted per individual, distribution, and monitoring of cannabis supply) were associated with lower odds of past-month binge drinking in adolescents (Johnson et al., 2018). Similarly, the literature regarding the associations between MCLs and adult binge drinking shows mixed results as reported in recent reviews (Guttmannova et al., 2016; Pacula et al., 2022; Smart and Pacula, 2019), for example, Wen and colleagues (2015) reported increases in the frequency of binge drinking after MML in the past 30 days among adults aged 21+ (Wen et al., 2015), while another study observed decrease in the probability of past-month binge drinking in adults (ages: 18–29 and 40–49 years) (Anderson et al., 2013). Some potential explanations for these inconsistencies in the literature are the different periods of MCL exposure (e.g., Wen et al. used data from 2004 to 2012, and Cerda et al. from 1991 to 2015). Differences in the exposure period are particularly significant when examining cannabis legislation, as it is an environment in constant change. Also, studies had different classifications of age groups among adolescents (e.g., 12–20 [Wen et al., 2015] vs. 9th-12th graders [Chapman et al., 2016]), which could have interfered with the results.
The current evidence regarding the association between recreational cannabis laws (RCLs) and binge drinking remains limited to data from a few states, small study samples (Smart and Pacula, 2019), and one prior U.S. national study using Behavioral Risk Factor Surveillance System (BRFSS) data (Macha et al., 2022). Three studies examined changes in alcohol use among undergraduate students in Colorado and Oregon after RCLs, finding increases in simultaneous alcohol and cannabis use but no change in heavy alcohol use (Jones et al., 2018; Kerr et al., 2018, 2017). Another study examining changes following RCLs in Washington and Oregon showed decreases in binge drinking (Dragone et al., 2019). Although these studies provide evidence regarding the association between RCLs and binge drinking, focusing on specific states may limit the generalizability of study findings. Finally, one study using national BRFSS data showed positive associations between RCLs and any alcohol use, but not binge drinking (Macha et al., 2022). However, the most recent BRFSS survey only included information on cannabis laws for 24 states with cannabis-related questions(Geissler et al., 2020) and focused on adults aged 18 and older. In addition, the authors combined participants aged 18–24 in the same group (Macha et al., 2022); grouping participants who are legally authorized to purchase these substances (age 21+) and those who are not (under 21 years old) complicates interpretation of these results participants had access to different cannabis supply channels (Macha et al., 2022). Furthermore, the authors adjusted for only one domain of alcohol policies (alcohol pricing) (Macha et al., 2022) out of the four main domains related to binge drinking patterns (Naimi et al., 2014; Silver et al., 2019; Xuan et al., 2013). Therefore, more research is needed to understand the incremental change in binge drinking associated with RCLs using nationally representative data across different age groups.
This study aimed to (a) examine trends in binge drinking and (b) investigate associations between the implementation of RCLs (defined as the presence of a legal supply mechanism in a state) and changes in binge drinking from 2008–2019 in the U.S. We hypothesized that following RCL implementation with a legal cannabis supply channel, prevalence of binge drinking use would decrease in youth aged 12–20 years old, as access to cannabis in this age group does not change after RCLs (legal age to purchase alcohol and cannabis is 21 and older), prior research suggests a decline in binge drinking among adolescents related to more flexible cannabis laws (Cerdá et al., 2018; Dragone et al., 2019; Johnson et al., 2018), and previously-observed declines in the prevalence of binge drinking among adolescents (Johnston et al., 2021; Keyes et al., 2020). We also hypothesized that the prevalence of binge drinking use would increase for adults ages 21+ after RCL implementation, particularly among those ages 51+, considering documented increases in binge drinking in the U.S. overall (Grucza et al., 2018) and increases in past month alcohol and cannabis use after medical and recreational cannabis policies in adults aged 50+ (Kim et al., 2021). Our study builds on existing literature by using nationally representative data to investigate the potential effects of the changing cannabis policy landscape in all age groups (adolescents, young adults, middle-aged and older adults) using a comprehensive measure of state alcohol policies to control for differences in state contexts.
2. Materials and Methods
We used restricted-access data from individuals aged 12+ who participated in the 2008–2019 National Survey on Drug Use and Health (NSDUH) (n=817,359). We included only participants who reported their state of residence, which enabled us to determine state RCL exposure status. The 2019 survey was the most recent survey available at the time of analysis (June 2021 to December 2022). The NSDUH used a multistage probability design for annual cross-sectional household surveys of the U.S. non-institutionalized population, excluding institutionalized individuals (e.g., active military, long-term hospital residents, prison populations, homeless not in shelters). Interviewers administered surveys with computer-assisted personal interviewing and audio computer-assisted self-interviewing for sensitive questions. The NSDUH provided survey weights to adjust for the probability of selection at each sampling stage, nonresponse, and coverage. Interview response rates over the study period varied from 64.9% to 75.6% (Substance Abuse and Mental Health Services Administration, 2020).
2.1. Measures
Outcome.
Past-month binge drinking (yes/no) was our primary outcome variable. The 2008–2014 surveys defined binge drinking as consuming ≥5 standard drinks per drinking session regardless of gender. The binge drinking question changed in 2015 to a gender-specific threshold (≥4 drinks for females and ≥5 drinks for males.) We allowed for this change in definition when creating a dichotomous measure of past-month binge drinking over the study period (Substance Abuse and Mental Health Services Administration, 2021).
Exposure.
Our primary exposure was living in a state that implemented RCL with a legal channel for obtaining cannabis for recreational purposes (i.e., legal cannabis supply) (Burris, 2014). This definition includes the adoption of laws allowing home cannabis cultivation or the presence of a legal retail outlet in the state, whichever came first. RCLs were distinguished from medical cannabis laws (MCL), with RCLs and MCLs dates obtained from multiple sources (Alcohol Policy Information System; Marijuana Policy Project, 2020; Procon, 2022; RAND Corporation). Where discrepancies between sources were noted, we referred to the specific text of the statute for clarification. These dates have been used in previous work (Cerdá et al., 2020; Gonçalves et al., 2022; Martins et al., 2021). Also, time-varying policies were lagged one year before participants were interviewed.
It is worth noting that cannabis legislation is complex, involving multiple policy decisions, including regulations of supply chain and operation: government monopoly, retail sales, legal home cultivation, advertisement, types of products distributed, prices, and taxes (Kilmer et al., 2019), and each state may have different policies when regulating recreational cannabis use. For example, among the states classified as RCL, eight allowed home cultivation and retail sales (i.e., Alaska, California, Colorado, Nevada, Massachusetts, Vermont [up to 6 plants], Oregon [up to 4 plants per residence], Washington [only with a permit]), and the District of Columbia permitted only home cultivation (up to 6 plants) (Alcohol Policy Information System; Marijuana Policy Project, 2020; Procon, 2022).
In descriptive analyses, state-level cannabis laws were categorized as a time-invariant three-level variable (No MCL nor RCL, MCL only, MCL and RCL) based on their legal status in 2019. In regression models, we utilized a time-varying indicator of state cannabis law status based on the date of the respondent interview relative to the legal cannabis supply date. As all states with RCLs previously implemented MCLs, we analyzed the predicted prevalence of binge drinking among five groups: (1) never MCL and RCL, (2) before MCL, (3) after MCL/never RCL, (4) after MCL/before RCL, (5) after MCL/after RCL (Gonçalves et al., 2022). Because our primary interest was to examine changes in binge drinking in response to RCL, our contrast of interest was, therefore, after MCL/after RCL versus after MCL/before RCL.
Individual covariates included age, categorized as 12–20, 21–30, 31–40, 41–50, and 51+ years old. The rationale for this categorization was to classify individuals in each life decade and to separate participants under age 21 (i.e., the legal age for purchasing alcohol/cannabis). Other individual-level covariates included: gender (male, female); racial and ethnic group (non-Hispanic white, non-Hispanic Black, Hispanic, Other [Native American, Pacific Islander, Asian and more than one race]); education (less than high school, high school graduate, some college, college graduate); family income (<$20,000; $20,000–49,999; $50,000–74,999; $75,000+); and urbanicity (small, large, non-metropolitan).
State-level covariates were based on 2010 U.S. Census data, including the proportion of each state’s population that was white, male, aged 10–24, aged 25+ with at least a high school education, state unemployment rates, and state median household income. Additional state-level covariates consisted of state alcohol policies. Prior research has suggested that alcohol use, especially binge drinking patterns, can be influenced by alcohol policies (Naimi et al., 2014; Silver et al., 2019; Xuan et al., 2013). For example, higher scores on alcohol scales (i.e., presence of more state alcohol policies) are associated with lower levels on binge drinking (Naimi et al., 2014; Silver et al., 2019). The State Alcohol Policy Score (SAPS) (Silver et al., 2022, 2019) is composed of 18 categories within four main domains: alcohol pricing (e.g., wholesale pricing practices, retail price restrictions, total beer tax), sales and retailer restrictions (e.g., Sunday sales ban, hours during which alcohol cannot be sold); driving-related laws (e.g., driving under the influence [DUI] penalties, open container laws); and underage alcohol furnishing and possession laws (e.g., underage purchasing, underage alcohol possession laws, false I.D. penalties, and laws prohibiting the furnishing of alcohol to minors). SAPS has shown that states vary considerably in the number of alcohol policies and that higher SAPS scores are negatively associated with binge drinking (Silver et al., 2022, 2019). Therefore, in our analyses we used SAPS from 2008–2019 to account for potential changes in the alcohol environment that might affect binge drinking. Finally, it is important to note that time-varying alcohol and cannabis policies were lagged one year before participants were interviewed.
2.2. Statistical Analysis
We initially described binge drinking prevalence and examined differences by sociodemographic characteristics, grouping respondents by state RCL exposure status at the end of the observation period, 2019 (No MCL nor RCL, MCL only, MCL and RCL). In order to investigate associations between RCLs and binge drinking, we then utilized a two-stage process to test associations between RCLs and binge drinking. First, we generated adjusted predicted prevalences of binge drinking by RCL exposure status group across different age groups. Next, to examine changes in the prevalence of binge drinking after versus before RCL implementation (i.e., after MCL/after RCL vs. after MCL/before RCL), we contrasted the model-based marginal predictions computed from adjusted odds ratios (aOR) and their 95% confidence intervals (95% CI). In the first step, we used the lme4 R package to fit a multilevel logistic regression, including an interaction between the RCL exposure group variable and age group. Models included state random intercepts to account for the clustering of individuals within states. We also included categorical year fixed effects to account for secular trends in binge drinking that would affect all states over the observation period. We further controlled for the individual-level and state-level covariates listed above. Similar to prior research (Cerdá et al., 2020; Martins et al., 2021; Segura et al., 2019), we did not apply survey weights; instead we included the individual-level indicators (listed above) that are related to the NSDUH sampling design (Little, 2004). In the second step of the process, we used the emmeans R package to compute the contrast of interest, after versus before RCL, as odds ratios and obtained model-based prevalence estimates.
In addition, we conducted a sensitivity analysis using e-values to evaluate the potential impact of unmeasured time-varying confounding (Haneuse et al., 2019; Segura et al., 2019; VanderWeele and Ding, 2017) on our results. Small e-values close to 1.0 suggest that little unmeasured confounding accounts for observed associations, whereas larger e-values indicate results that are increasingly robust to unmeasured confounding. We obtained e-values for the estimated aOR and lower level of the 95%CI (LL95%CI) using the EValue package in R software (Haneuse et al., 2019; Segura et al., 2019; VanderWeele and Ding, 2017).
All analyses were conducted at the New York Federal Statistical Research Data Center, a Census Bureau administered facility providing secure access to restricted-access NSDUH microdata. Statistical output was reviewed by Substance Abuse and Mental Health Services Administration (SAMSHA) staff and conformed to SAMSHA disclosure requirements to ensure confidentiality, including sample size rounding (to the nearest hundred) and suppression of values less than 100 or with large standard errors. This manuscript was prepared according to STROBE guidelines for cross-sectional studies (Elm et al., 2007) and approved by the Columbia University Institutional Review Board (approval number AAAS4624).
3. Results
Demographic characteristics were similar when comparing people in states by cannabis legalization status as of 2019 (Table 1). Overall, fifty-one percent of the participants were female, 14.0–15.0% were ages 12–20 years, 15.6–16.7% ages 21–30 years, 14.9–16.0% ages 31–40 years, 15.7–15.9% ages 41–50 years, and 36.8–39.9% ages 51+ years. In states where RCLs were implemented (i.e., Colorado, Washington, Alaska, Oregon, Nevada, California, Massachusetts, Vermont and District of Columbia), we observed higher family income and levels of urbanicity than in states that did not implement MCLs/RCLs or MCLs only.
Table 1.
Demographic characteristics, self-reported alcohol and cannabis use, and state-level covariates among states that differ by cannabis law status. National Survey on Drug use and Health (NSDUH), 2008–2019.
| No MCL nor RCL | MCL only | MCL and RCL | ||||
|---|---|---|---|---|---|---|
| weighted n’s | % Weighted | weighted n’s | % Weighted | weighted n’s | % Weighted | |
| Characteristics | ||||||
| Gender | ||||||
| Male | 42154400 | 48.40 | 54353500 | 48.29 | 31136700 | 48.98 |
| Female | 44947500 | 51.60 | 58197600 | 51.71 | 32428800 | 51.02 |
| Age | ||||||
| 12–20 | 13075500 | 15.01 | 15694800 | 13.95 | 9265600 | 14.58 |
| 21–30 | 14284500 | 16.40 | 17594900 | 15.63 | 10594200 | 16.67 |
| 31–40 | 13666400 | 15.69 | 16753300 | 14.89 | 10167700 | 15.99 |
| 41–50 | 13782100 | 15.82 | 17618400 | 15.65 | 10124000 | 15.93 |
| 51+ | 32293500 | 37.08 | 44889800 | 39.88 | 23414100 | 36.83 |
| Race/Ethnicity | ||||||
| Non-Hispanic white | 58044500 | 66.64 | 75550200 | 67.12 | 36538800 | 57.48 |
| Non-Hispanic Black | 13098600 | 15.04 | 14119800 | 12.55 | 4207800 | 6.62 |
| Hispanic | 11806700 | 13.55 | 14989900 | 13.32 | 14781500 | 23.25 |
| Non-Hispanic Other | 4152100 | 4.77 | 7891200 | 7.01 | 8037400 | 12.64 |
| Education | ||||||
| Less than HS | 12100900 | 15.42 | 13077200 | 12.78 | 7750200 | 13.45 |
| HS graduate | 22654300 | 28.87 | 29339200 | 28.68 | 14002200 | 24.31 |
| Some college | 22405200 | 28.56 | 28288500 | 27.65 | 16673400 | 28.94 |
| College graduate | 21298000 | 27.15 | 31609400 | 30.89 | 19182000 | 33.30 |
| Family Income | ||||||
| <$20,000 | 16244500 | 18.65 | 19159700 | 17.02 | 10233900 | 16.10 |
| $20,000-$49,999 | 28511900 | 32.73 | 34186800 | 30.37 | 18745100 | 29.49 |
| $50,000-$74,999 | 14935800 | 17.15 | 18576000 | 16.51 | 10114100 | 15.91 |
| $75,000+ | 27409700 | 31.47 | 40628600 | 36.10 | 24472400 | 38.50 |
| Urbanicity | ||||||
| Large Metro | 36841000 | 42.30 | 67020800 | 59.55 | 41904300 | 65.92 |
| Small Metro | 31497100 | 36.16 | 31250300 | 27.76 | 16836400 | 26.49 |
| Nonmetro | 18763900 | 21.54 | 14279900 | 12.69 | 4824800 | 7.59 |
| Binge drinking, past month | 19695200 | 22.61 | 27398800 | 24.34 | 15171000 | 23.87 |
Note: State-level cannabis laws were categorized as a time-invariant three-level variable (No MCL nor RCL, MCL only, MCL and RCL) in 2019.
All these results are weighted and rounded conforming to SAMSHA disclosure requirements to ensure confidentiality.
3.1. Trends in past-month binge drinking by age group and state cannabis policy
Figure 1 shows the prevalence of binge drinking by age group, according to state RCL status at the end of the observation period in 2019 (i.e., No MCL nor RCL, MCL only, MCL and RCL). Overall, states that never enacted cannabis laws (i.e., No MCL nor RCL) showed consistently lower rates of binge drinking over time among all age groups. Additionally, when examining binge drinking trends in all U.S. states, the most substantial declines in binge drinking were observed among people ages 12–20 (from 17.5% [95% CI, 16.9–18.2] in 2008 to 11.1% [10.4–11.8] in 2019), followed by respondents ages 21–30 (from 43.7% [95% CI, 42.4–44.9] to 40.2% [39.1–41.1] in 2019). However, we observed overall increases in binge drinking in all states regardless of cannabis laws among individuals ages 31+. The most extensive increases were noted among people ages 31– 40 (from 28.1% [95% CI, 26.6–29.6] to 33.3% [32.1–34.6]), followed by participants ages 51+ (from 13.3% [95% CI, 12.2–14.4] to 16.8% [15.8–17.7]), and those ages 41–50 (25.5% [95% CI, 24.1–26.9] to 28.3% [27.1–29.6]).
Figure 1.
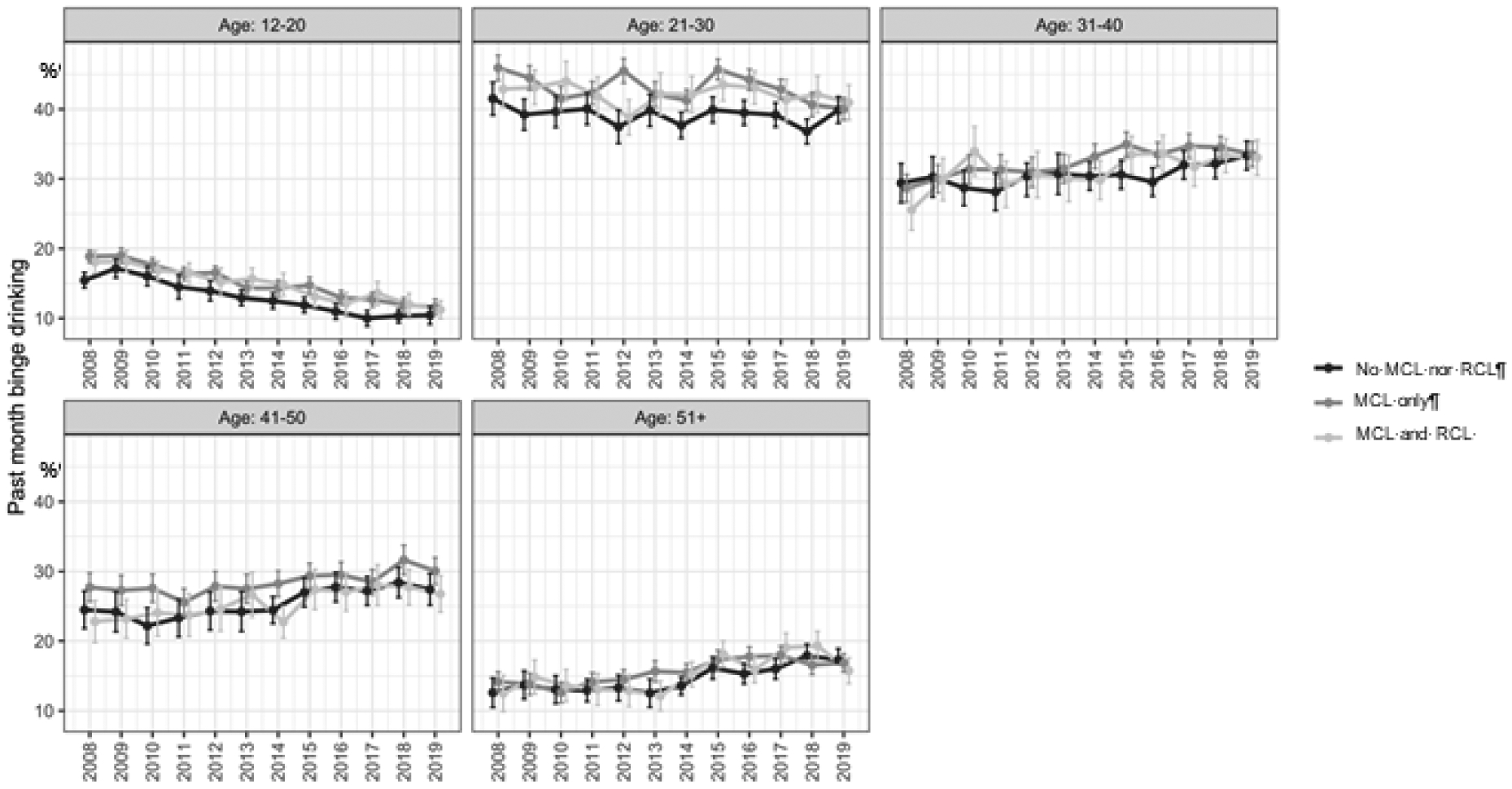
Trends in prevalences of past month binge drinking by status of cannabis law implementation during 2008–2019.
Note: State-level cannabis law status was classified by 2019 and categorized as a time-invariant the following three-level variable: (1) No MCL nor RCL – refers to states that have never implemented medical cannabis laws or recreational cannabis laws (e.g., Alabama, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Mississippi, Nebraska, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, Wyoming); (2) MCL only – refers to states that only implemented medical cannabis laws (e.g., Arizona [2011], Arkansas [2019], Connecticut [2015], Delaware [2015], Florida [2017], Hawaii [2000], Illinois [2016], Maine [1999], Maryland [2018], Michigan [2009], Minnesota [2016], Missouri [2019], Montana [2004], New Hampshire [2016], New Jersey [2013], New Mexico [2008], New York [2016], North Dakota [2019], Ohio [2019], Oklahoma [2019], Pennsylvania [2018], Rhode Island [2006], and West Virginia [2019]); and (3) MCL and RCL – refers to states implemented Recreational Cannabis Laws (e.g., Alaska [2015], California [2017], Colorado [2013], Massachusetts [2017], Nevada [2017], Oregon [2016], Vermont [2019], Washington [2013] and District of Columbia [2015]).
3.2. Changes in binge drinking by age after RCL implementation (Table 2)
Table 2.
Past month binge drinking after versus before RCL implementation among US individuals among different age groups between 2008–2019
| % who reported binge drinking | |||
|---|---|---|---|
| Age group | After MCL/Before RCL | After MCL/After RCL | AOR (95% CI) |
| 12–20 | 27.2 | 22.32 | 0.77 (0.70, 0.85) |
| 21–30 | 39.69 | 38.56 | 0.95 (0.90, 1.02) |
| 31–40 | 27.66 | 29.45 | 1.09 (1.01, 1.19) |
| 41–50 | 21.96 | 24.43 | 1.15 (1.05, 1.26) |
| 51+ | 12.43 | 14.27 | 1.17 (1.06, 1.30) |
Note: For point estimates with corresponding lower limit 95% confidence interval (LL95%CI) greater than 1, we estimated e-values to quantify the minimum strength of the relationship between an unmeasured/uncontrolled confounder and both our exposure (RCL) and outcome (binge drinking) needed to reduce the aOR and the lower limit of the 95% confidence interval (LL95%CI) to the null. For age group 12–20 years these were: ae-value for aOR = 1.92 & LL95%CI = 1.62, age group 31–40 years these were: ae-value for aOR = 1.41 & LL95%CI = 1.08, age group 41–50 years these were: ae-value for aOR = 1.56 & LL95%CI = 1.26, age group 51+ these were: ae-value for aOR = 1.62 & LL95%CI = 1.31
Individual and state-level predictors: state random effects, year fixed effects, gender, race/ethnicity, family income, and urbanicity, % white, % male, % ages 10–24, % of adults (<25) with at least a high school education, unemployment, and state’s median household income, State Alcohol Policy Score (SAPS).
Table 2 displays the model-based prevalences of binge drinking comparing after versus before RCL. Binge drinking decreased among people ages 12–20 (−4.8% [before RCL 27.2%. after RCL 22.32%]; adjusted odds ratio [aOR]= 0.77, 95%CI 0.70–0.85) and increased among adults ages 31–40 (+1.8% [before RCL 27.66%. after RCL 29.45%]; aOR=1.09 [95%CI = 1.01–1.26]), 41–50 (+2.5 [before RCL 21.96%. after RCL 24.43%]; 1.15[1.05–1.26]) and 51+ (+1.8% [before RCL 12.43%. after RCL 14.27%]; 1.17[1.06–1.30]). No policy-related changes were noted in young adults ages 21–30 following RCLs.
In sensitivity analyses, e-value results suggested that a moderate degree of unmeasured confounding would be required to explain the observed results if no relationship existed between RCLs and binge drinking. For example, the observed adjusted odds ratio for the 31–40-year-old group could be explained by an unmeasured confounder that was associated with both the RCL exposure and the binge drinking outcome by a risk ratio of 1.41 (e-value 95%CI lower limit=1.08) above the measured confounders, but weaker confounding could not do so. E-value results among those ages 12–20 were the most robust to potential unmeasured confounding (e-value 95%CI lower limit=1.62).
4. Discussion
Drawing on data from a nationally representative survey of the U.S. population, this study aimed to investigate changes in the prevalence of past-month binge drinking before and after RCL implementation permitting a legal supply channel across different age groups. Binge drinking declined in individuals younger than 21 years and increased in individuals aged 31+ years after RCL implementation. This is one of the first studies to report associations between binge drinking and RCLs in adolescents and adults at a national level, adjusting for state alcohol policies within four different domains.
Our findings of a 4.8% decline in binge drinking among individuals younger than 21 after RCLs are consistent with prior evidence on long-term trends (Clark Goings et al., 2019; Johnston et al., 2021; Keyes et al., 2020) and the association between more flexible cannabis laws (i.e., state cannabis laws allowing any medical and/or recreational cannabis use) and binge drinking in U.S. national surveys (Cerdá et al., 2018; Johnson et al., 2018; Pacula et al., 2022). Declines in adolescent binge drinking may be beneficial, as binge drinking in adolescence is associated with poor academic performance, sexual risk, and injury in the short-term (Delker et al., 2016; Hingson and Zha, 2018; Jennings et al., 2015; Jennison, 2004; Patte et al., 2017), and with development of AUD and academic disengagement in the long-term (Jennison, 2004; Patrick and Schulenberg, 2014). One possible explanation for our findings in adolescents could be that binge drinking declines co-occurred with increased cannabis use among adolescents living in RCL states (Guttmannova et al., 2016, Pacula et al., 2022), supporting the substitution hypothesis. However, most literature does not show increased cannabis use in adolescents related to flexible cannabis laws (Coley et al., 2021; Johnson and Guttmannova, 2019), including a meta-analysis (Sarvet et al., 2018a) suggesting that substituting cannabis for alcohol may not fully explain findings. Yet, prior studies have observed changes in cannabis use risk perception (Sarvet et al., 2018b) and frequency of cannabis use after more flexible cannabis laws (Ladegard and Bhatia, 2023), suggesting further research is needed to examine the relationship between the substitution hypothesis and RCLs among adolescents. Finally, we observed a moderate level of unmeasured confounding in our sensitivity analyses; therefore, future studies should examine the relationship of other environmental and individual factors (e.g., perceived risk, disapproval, availability, peer drinking, alcohol expectancy) among binge drinking and RCLs in this age group.
We observed increases (between +1.8% and 2.5%) in binge drinking associated with RCLs in adults ages 31–50 and middle-aged and older adults (51+ years), which aligns with prior research on MCLs (Wen et al., 2015). Our findings differ from Macha et al. (2022) who only found increases in binge drinking among men following RCL, but this discrepancy may be due to the number of states with cannabis use data in the BRFSS and lack of adjustment for multiple alcohol policies. Increases in binge drinking after RCLs in older adults are especially concerning because of the physiological effects of aging (i.e., declines in metabolism) and alcohol-medication interactions due to the presence of chronic health conditions (Al-Rousan et al., 2022; Breslow et al., 2017, 2015; Ferreira and Weems, 2008). Our findings support calls to reinforce healthcare providers’ discussions about alcohol use with older adults (Mauro et al., 2021), particularly in RCL states. Moreover, our results support the complementary hypothesis, which is further corroborated by prior research suggesting a rise in co-use of cannabis and alcohol among adults after the implementation of RCLs (Cerdá et al., 2020; Gonçalves et al., 2022; Kim et al., 2021). Our findings are also consistent with research highlighting a high prevalence of binge drinking among those with cannabis use, including older adults (Kepner et al., 2022; Vijapur et al., 2021). Future research should investigate relationships among the implementation of RCLs, changes in cannabis use, and its association with binge drinking.
We note several limitations in this study. First, alcohol-related measures, including binge drinking, were self-reported, which may introduce recall bias and underreporting due to social desirability. However, NSDUH collects sensitive information, such as alcohol and substance use, using computer-assisted self-interviewing, which should reduce differential measurement error. Further, NSDUH binge drinking measures did not adjust for sex differences from 2008 to 2014, which may result in underreporting of binge drinking in females before 2015. Additionally, our analyses investigated all RCL states as a single category without examining cannabis policy provisions (e.g., products permitted, cultivation restrictions, pricing control, the tax imposed, and consumption restrictions). We defined RCL states using cannabis supply dates (e.g., presence of a legal dispensary or home cultivation) instead of effective dates of recreational cannabis legislation, which limits comparisons with prior research (Gonçalves et al., 2022; Kilmer, 2019; Kilmer and Pacula, 2017). However, we believe that using supply dates better captures information on actual changes in cannabis availability, which provides a better measure of the construct of interest and helps account for the time variation between enactment and implementation of RCLs. Nonetheless, our study has significant strengths, such as using data from all U.S. states, including adolescents and adults, and adjusting for state alcohol policies using a multidomain scale (Silver et al., 2022, 2019).
5. Conclusion
Implementation of RCLs was associated with increased past-month binge drinking in individuals aged 31+ and decreased binge drinking in youth aged 12–20. Our study contributes to understanding age group differences in binge drinking after legalizing adult cannabis use in the U.S.. In addition, this study contributes to the ongoing debate on the effects of RCL implementation and alcohol-related outcomes, providing valuable information to policymakers, clinicians, and researchers. Intervention strategies, such as brief interventions and digital interventions (Kaner et al., 2018, 2017), may be needed to reduce harms related to binge drinking in adults aged 31+, especially in states with RCLs.
Highlights.
Decreases in binge drinking in youth <21 after Recreational Cannabis Laws (RCLs)
Increases in binge drinking in adults 31+ were noted after RCLs.
There was no association between binge drinking and RCLs in adults aged 21–30 years.
Findings support complementary hypotheses in adults after RCLs.
Acknowledgments
This study was funded by grants from the U.S. National Institutes of Health, National Institute on Drug Abuse R01DA037866 (Martins), T32DA031099 (MPI: Hasin and Martins), R01DA048860 (Hasin), K01DA045224 (Mauro). This research was supported in part by a Grant 1 R49 CE002096-01 from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention to the Center for Injury Epidemiology and Prevention at Columbia University (New York, NY).
Role of Funding Source
This study was funded by grants from U.S. National Institutes of Health and the Centers for Disease Control and Prevention, which had no role in the design, analysis, and interpretation of the data, writing of this manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
This study was approved by the Columbia University Institutional Review Board (approval number AAAS4624).
REFERENCES
- Alcohol Policy Information System, n.d. Cannabis Policy Topics. Recreational Use of Cannabis: Volume 1. National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Al-Rousan T, Moore AA, Han BH, Ko R, Palamar JJ, 2022. Trends in binge drinking prevalence among older U.S. men and women, 2015 to 2019. J. Am. Geriatr. Soc 70, 812–819. 10.1111/jgs.17573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson DM, Hansen B, Rees DI, 2013. Medical Marijuana Laws, Traffic Fatalities, and Alcohol Consumption. J. Law Econ 56, 333–369. 10.1086/668812 [DOI] [Google Scholar]
- Breslow RA, Castle I-JP, Chen CM, Graubard BI, 2017. Trends in Alcohol Consumption Among Older Americans: National Health Interview Surveys, 1997 to 2014. Alcohol. Clin. Exp. Res 41, 976–986. 10.1111/acer.13365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow RA, Dong C, White A, 2015. Prevalence of Alcohol-Interactive Prescription Medication Use Among Current Drinkers: United States, 1999 to 2010. Alcohol. Clin. Exp. Res 39, 371–379. 10.1111/acer.12633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris S, 2014. A Technical Guide for Policy Surveillance. SSRN Electron. J 10.2139/ssrn.2469895 [DOI] [Google Scholar]
- Canham SL, Kaufmann CN, Mauro PM, Mojtabai R, Spira AP, 2015. Binge drinking and insomnia in middle-aged and older adults: the Health and Retirement Study. Int. J. Geriatr. Psychiatry 30, 284–291. 10.1002/gps.4139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, Wall MM, Keyes KM, Martins SS, 2020. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry 77, 165. 10.1001/jamapsychiatry.2019.3254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Sarvet AL, Wall M, Feng T, Keyes KM, Galea S, Hasin DS, 2018. Medical marijuana laws and adolescent use of marijuana and other substances: Alcohol, cigarettes, prescription drugs, and other illicit drugs. Drug Alcohol Depend. 183, 62–68. 10.1016/j.drugalcdep.2017.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA, 2016. Capturing Heterogeneity in Medical Marijuana Policies: A Taxonomy of Regulatory Regimes Across the United States. Subst. Use Misuse 51, 1174–1184. 10.3109/10826084.2016.1160932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark Goings T, Salas-Wright CP, Belgrave FZ, Nelson EJ, Harezlak J, Vaughn MG, 2019. Trends in binge drinking and alcohol abstention among adolescents in the US, 2002–2016. Drug Alcohol Depend. 200, 115–123. 10.1016/j.drugalcdep.2019.02.034 [DOI] [PubMed] [Google Scholar]
- Coley RL, Kruzik C, Ghiani M, Carey N, Hawkins SS, Baum CF, 2021. Recreational Marijuana Legalization and Adolescent Use of Marijuana, Tobacco, and Alcohol. J. Adolesc. Health 69, 41–49. 10.1016/j.jadohealth.2020.10.019 [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, 2019. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 204, 107468. 10.1016/j.drugalcdep.2019.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Zhou Y, 2005. Effectiveness of the Derived Alcohol Use Disorders Identification Test (AUDIT-C) in Screening for Alcohol Use Disorders and Risk Drinking in the US General Population. Alcohol. Clin. Exp. Res 29, 844–854. 10.1097/01.ALC.0000164374.32229.A2 [DOI] [PubMed] [Google Scholar]
- Dawson DA, Li T-K, Grant BF, 2008. A Prospective Study of Risk Drinking: At Risk for What? Drug Alcohol Depend. 95, 62–72. 10.1016/j.drugalcdep.2007.12.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delker E, Brown Q, Hasin DS, 2016. Alcohol Consumption in Demographic Subpopulations. Alcohol Res. Curr. Rev 38, 7–15. [PMC free article] [PubMed] [Google Scholar]
- Dragone D, Prarolo G, Vanin P, Zanella G, 2019. Crime and the legalization of recreational marijuana. J. Econ. Behav. Organ 159, 488–501. 10.1016/j.jebo.2018.02.005 [DOI] [Google Scholar]
- Elm von E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, 2007. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335, 806–808. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser MB, Sherk A, Liu Y, Naimi TS, Stockwell T, Stahre M, Kanny D, Landen M, Saitz R, Brewer RD, 2020. Deaths and Years of Potential Life Lost From Excessive Alcohol Use - United States, 2011–2015. MMWR Morb. Mortal. Wkly. Rep 69, 981–987. 10.15585/mmwr.mm6930a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira MP, Weems MKS, 2008. Alcohol Consumption by Aging Adults in the United States: Health Benefits and Detriments. J. Am. Diet. Assoc 108, 1668–1676. 10.1016/j.jada.2008.07.011 [DOI] [PubMed] [Google Scholar]
- Geissler KH, Kaizer K, Johnson JK, Doonan SM, Whitehill JM, 2020. Evaluation of Availability of Survey Data About Cannabis Use. JAMA Netw. Open 3, e206039. 10.1001/jamanetworkopen.2020.6039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves PD, Levy NS, Segura LE, Bruzelius E, Boustead AE, Hasin DS, Mauro PM, Martins SS, 2022. Cannabis Recreational Legalization and Prevalence of Simultaneous Cannabis and Alcohol Use in the United States. J. Gen. Intern. Med 10.1007/s11606-022-07948-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, Hartz S, Virdi G, Bierut LJ, 2018. Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol. Clin. Exp. Res 42, 1939–1950. 10.1111/acer.13859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn R, 2022. Patterns of Cannabis and Alcohol Co-Use: Substitution Versus Complementary Effects. Alcohol Res. Curr. Rev 40, 04. 10.35946/arcr.v42.1.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmannova K, Lee CM, Kilmer JR, Fleming CB, Rhew IC, Kosterman R, Larimer ME, 2016. Impacts of Changing Marijuana Policies on Alcohol Use in the United States. Alcohol. Clin. Exp. Res 40, 33–46. 10.1111/acer.12942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ, 2017. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014. Drug Alcohol Depend. 170, 198–207. 10.1016/j.drugalcdep.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haneuse S, VanderWeele TJ, Arterburn D, 2019. Using the E-Value to Assess the Potential Effect of Unmeasured Confounding in Observational Studies. JAMA 321, 602. 10.1001/jama.2018.21554 [DOI] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, Wall MM, 2017. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry 74, 579. 10.1001/jamapsychiatry.2017.0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, 2018. Binge Drinking Above and Below Twice the Adolescent Thresholds and Health-Risk Behaviors. Alcohol. Clin. Exp. Res 42, 904–913. 10.1111/acer.13627 [DOI] [PubMed] [Google Scholar]
- Jennings WG, Piquero AR, Rocque M, Farrington DP, 2015. The effects of binge and problem drinking on problem behavior and adjustment over the life course: Findings from the Cambridge Study in Delinquent Development. J. Crim. Justice 43, 453–463. 10.1016/j.jcrimjus.2015.09.002 [DOI] [Google Scholar]
- Jennison KM, 2004. The Short-Term Effects and Unintended Long-Term Consequences of Binge Drinking in College: A 10-Year Follow-Up Study. Am. J. Drug Alcohol Abuse 30, 659–684. 10.1081/ADA-200032331 [DOI] [PubMed] [Google Scholar]
- Johnson JK, Johnson RM, Hodgkin D, Jones AA, Matteucci AM, Harris SK, 2018. Heterogeneity of state medical marijuana laws and adolescent recent use of alcohol and marijuana: Analysis of 45 states, 1991–2011. Subst. Abuse 39, 247–254. 10.1080/08897077.2017.1389801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RM, Guttmannova K, 2019. Marijuana Use among Adolescents and Emerging Adults in the Midst of Policy Change: Introduction to the Special Issue. Prev. Sci 20, 179–184. 10.1007/s11121-019-0989-7 [DOI] [PubMed] [Google Scholar]
- Johnston L, Miech R, O’Malley P, Bachman J, Schulenberg J, Patrick M, 2021. Monitoring the Future national survey results on drug use 1975–2020: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, University of Michigan. [Google Scholar]
- Jones J, Nicole Jones K, Peil J, 2018. The impact of the legalization of recreational marijuana on college students. Addict. Behav 77, 255–259. 10.1016/j.addbeh.2017.08.015 [DOI] [PubMed] [Google Scholar]
- Kaner EF, Beyer FR, Garnett C, Crane D, Brown J, Muirhead C, Redmore J, O’Donnell A, Newham JJ, de Vocht F, Hickman M, Brown H, Maniatopoulos G, Michie S, 2017. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst. Rev. 2017 10.1002/14651858.CD011479.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EF, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B, 2018. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst. Rev. 2018 10.1002/14651858.CD004148.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kepner WE, Han BH, Nguyen D, Han SS, Lopez FA, Palamar JJ, 2022. Past-month binge drinking and cannabis use among middle-aged and older adults in the United States, 2015–2019. Alcohol S0741832922000684. 10.1016/j.alcohol.2022.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr DCR, Bae H, Koval AL, 2018. Oregon recreational marijuana legalization: Changes in undergraduates’ marijuana use rates from 2008 to 2016. Psychol. Addict. Behav 32, 670–678. 10.1037/adb0000385 [DOI] [PubMed] [Google Scholar]
- Kerr DCR, Bae H, Phibbs S, Kern AC, 2017. Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon: Effects of marijuana legalization. Addiction 112, 1992–2001. 10.1111/add.13906 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hamilton A, Patrick ME, Schulenberg J, 2020. Diverging Trends in the Relationship Between Binge Drinking and Depressive Symptoms Among Adolescents in the U.S. From 1991 Through 2018. J. Adolesc. Health 66, 529–535. 10.1016/j.jadohealth.2019.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer B, 2019. How will cannabis legalization affect health, safety, and social equity outcomes? It largely depends on the 14 Ps. Am. J. Drug Alcohol Abuse 45, 664–672. 10.1080/00952990.2019.1611841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer B, Pacula RL, 2017. Understanding and learning from the diversification of cannabis supply laws. Addict. Abingdon Engl 112, 1128–1135. 10.1111/add.13623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Weinberger AH, Zhu J, Barrington-Trimis J, Wyka K, Goodwin RD, 2021. Impact of state-level cannabis legalization on poly use of alcohol and cannabis in the United States, 2004–2017. Drug Alcohol Depend 218, 108364. 10.1016/j.drugalcdep.2020.108364 [DOI] [PubMed] [Google Scholar]
- Ladegard K, Bhatia D, 2023. Impact of Cannabis Legalization on Adolescent Cannabis Use. Child Adolesc. Psychiatr. Clin. N. Am 32, 1–12. 10.1016/j.chc.2022.07.001 [DOI] [PubMed] [Google Scholar]
- Levy NS, Mauro PM, Mauro CM, Segura LE, Martins SS, 2021. Joint perceptions of the risk and availability of Cannabis in the United States, 2002–2018. Drug Alcohol Depend. 108873. 10.1016/j.drugalcdep.2021.108873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari RN, 2019. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health 114.
- Little RJ, 2004. To Model or Not To Model? Competing Modes of Inference for Finite Population Sampling. J. Am. Stat. Assoc 99, 546–556. 10.1198/016214504000000467 [DOI] [Google Scholar]
- Macha V, Abouk R, Drake C, 2022. Association of Recreational Cannabis Legalization With Alcohol Use Among Adults in the US, 2010 to 2019. JAMA Health Forum 3, e224069. 10.1001/jamahealthforum.2022.4069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marijuana Policy Project (Marijuana Policy Project; c1995–2022), 2020. . Washington. [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Hasin DS, Galea S, Wall M, 2016. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 169, 26–32. 10.1016/j.drugalcdep.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Segura LE, Levy NS, Mauro PM, Mauro CM, Philbin MM, Hasin DS, 2021. Racial and Ethnic Differences in Cannabis Use Following Legalization in US States With Medical Cannabis Laws. JAMA Netw. Open 4, e2127002. 10.1001/jamanetworkopen.2021.27002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauro PM, Askari MS, Han BH, 2021. Gender differences in any alcohol screening and discussions with providers among older adults in the United States, 2015 to 2019. Alcohol. Clin. Exp. Res 45, 1812–1820. 10.1111/acer.14668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Blanchette J, Nelson TF, Nguyen T, Oussayef N, Heeren TC, Gruenewald P, Mosher J, Xuan Z, 2014. A New Scale of the U.S. Alcohol Policy Environment and Its Relationship to Binge Drinking. Am. J. Prev. Med 46, 10–16. 10.1016/j.amepre.2013.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, n.d. Drinking Levels Defined | National Institute on Alcohol Abuse and Alcoholism (NIAAA) [WWW Document]. URL https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed 9.21.22).
- Pacula R, Smart R, Lira M, Pessar S, Blanchette J, Naimi TS, 2022. Relationships of Cannabis Policy Liberalization With Alcohol Use and Co-Use With Cannabis: A Narrative Review. Alcohol Res. Curr. Rev 41, 06. 10.35946/arcr.v42.1.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, 2014. Prevalence and Predictors of Adolescent Alcohol Use and Binge Drinking in the United States. Alcohol Res. Curr. Rev 35, 193–200. [PMC free article] [PubMed] [Google Scholar]
- Patte KA, Qian W, Leatherdale ST, 2017. Marijuana and Alcohol Use as Predictors of Academic Achievement: A Longitudinal Analysis Among Youth in the COMPASS Study. J. Sch. Health 87, 310–318. 10.1111/josh.12498 [DOI] [PubMed] [Google Scholar]
- Procon, 2022. Legal Medical & Recreational Marijuana States and DC.
- RAND Corporation, n.d. OPTIC-Vetted Policy Data Sets: Medical Marijuana Policy Data.
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD, 2015. 2010 National and State Costs of Excessive Alcohol Consumption. Am. J. Prev. Med 49, e73–e79. 10.1016/j.amepre.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, Pacula RL, Keyes KM, Cerdá M, Galea S, Hasin DS, 2018a. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction 113, 1003–1016. 10.1111/add.14136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Keyes KM, Cerdá M, Schulenberg JE, O’Malley PM, Johnston LD, Hasin DS, 2018b. Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 186, 68–74. 10.1016/j.drugalcdep.2017.12.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura LE, Mauro CM, Levy NS, Khauli N, Philbin MM, Mauro PM, Martins SS, 2019. Association of US Medical Marijuana Laws With Nonmedical Prescription Opioid Use and Prescription Opioid Use Disorder. JAMA Netw. Open 2, e197216. 10.1001/jamanetworkopen.2019.7216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver D, Bae JY, McNeill E, Macinko J, 2022. Do alcohol policies affect everyone equally? An assessment of the effects of state policies on education-related patterns of alcohol use, 2011–2019. Drug Alcohol Depend. 239, 109591. 10.1016/j.drugalcdep.2022.109591 [DOI] [PubMed] [Google Scholar]
- Silver D, Macinko J, Giorgio M, Bae JY, 2019. Evaluating the relationship between binge drinking rates and a replicable measure of U.S. state alcohol policy environments. PLOS ONE 14, e0218718. 10.1371/journal.pone.0218718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, Pacula RL, 2019. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: Findings from state policy evaluations. Am. J. Drug Alcohol Abuse 45, 644–663. 10.1080/00952990.2019.1669626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2021. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (No. PEP21-07-01-003), NSDUH Series H-56. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2020. 2019 National Survey on Drug Use and Health: Methodological summary and definitions. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- VanderWeele TJ, Ding P, 2017. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med 167, 268. 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- Vijapur SM, Levy NS, Martins SS, 2021. Cannabis use outcomes by past-month binge drinking status in the general United States population. Drug Alcohol Depend 228, 108997. 10.1016/j.drugalcdep.2021.108997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vital Signs: Binge Drinking Prevalence, Frequency, and Intensity Among Adults — United States, 2010. [WWW Document], n.d. URL https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6101a4.htm (accessed 9.21.22). [PubMed]
- Wen H, Hockenberry JM, Cummings JR, 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ 42, 64–80. 10.1016/j.jhealeco.2015.03.007 [DOI] [PubMed] [Google Scholar]
- White AM, Castle I-JP, Hingson RW, Powell PA, 2020. Using Death Certificates to Explore Changes in Alcohol-Related Mortality in the United States, 1999 to 2017. Alcohol. Clin. Exp. Res 44, 178–187. 10.1111/acer.14239 [DOI] [PubMed] [Google Scholar]
- White AM, Slater ME, Ng G, Hingson R, Breslow R, 2018. Trends in Alcohol-Related Emergency Department Visits in the United States: Results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol. Clin. Exp. Res 42, 352–359. 10.1111/acer.13559 [DOI] [PubMed] [Google Scholar]
- Xuan Z, Nelson TF, Heeren T, Blanchette J, Nelson DE, Gruenewald P, Naimi TS, 2013. Tax Policy, Adult Binge Drinking, and Youth Alcohol Consumption in the United States. Alcohol. Clin. Exp. Res. n/a-n/a 10.1111/acer.12152 [DOI] [PMC free article] [PubMed] [Google Scholar]


