Abstract
Aim:
To evaluate associations between characteristics of simulated point-of-care cardiopulmonary resuscitation (CPR) training with simulated and actual intensive care unit (ICU) CPR performance, and with outcomes of children after in-hospital cardiac arrest.
Methods:
This is a pre-specified secondary analysis of the ICU-RESUScitation Project; a prospective, multicentre cluster randomized interventional trial conducted in 18 ICUs from October 2016–March 2021. Point-of-care bedside simulations with real-time feedback to allow multidisciplinary ICU staff to practice CPR on a portable manikin were performed and quality metrics (rate, depth, release velocity, chest compression fraction) were recorded. Actual CPR performance was recorded for children 37 weeks post-conceptual age to 18 years who received chest compressions of any duration, and included intra-arrest haemodynamics and CPR mechanics. Outcomes included survival to hospital discharge with favourable neurologic status.
Results:
Overall, 18,912 point-of-care simulations were included. Simulation characteristics associated with both simulation and actual performance included site, participant discipline, and timing of simulation training. Simulation characteristics were not associated with survival with favourable neurologic outcome. However, participants in the top 3 sites for improvement in survival with favourable neurologic outcome were more likely to have participated in a simulation in the past month, on a weekday day, to be nurses, and to achieve targeted depth of compression and chest compression fraction goals during simulations than the bottom 3 sites.
Conclusions:
Point-of-care simulation characteristics were associated with both simulated and actual CPR performance. More recent simulation, increased nursing participation, and simulation training during daytime hours may improve CPR performance.
Keywords: cardiopulmonary resuscitation, cardiac arrest, simulation, neonate, infant, child
INTRODUCTION
Cardiac arrest affects thousands of children annually.1,2 Most paediatric in-hospital cardiac arrests (p-IHCA) occur in intensive care units (ICU).3 While many children who receive cardiopulmonary resuscitation (CPR) will survive the initial arrest, only about half of these children will survive to hospital discharge.3–5 Of the survivors, many will have significant morbidity, including neurologic sequelae.5 High-quality CPR is associated with improved outcome.6–9 Unfortunately, the quality of CPR is variable even in ICU settings.
Educational approaches to improve CPR quality have included standard courses with modest time-limited improvement in outcomes.10–12 Novel educational approaches include CPR real-time feedback devices and structured post-resuscitation debriefings. CPR real-time feedback devices provide quantitative CPR quality data (compression rate, depth, and release velocity) and have been associated with improved quality of CPR during actual cardiac arrest but have not translated to improved clinical outcomes.13–15 Single-centre data suggest that an educational bundle including point-of-care bedside CPR training on manikins, and structured post-arrest debriefings are associated with improved neurologic outcome in children.16 The multicentre Improving Outcomes from Paediatric Cardiac Arrest (ICU-RESUS) study assessed whether an educational bundle of structured debriefings that emphasized physiologic resuscitation targets, and point-of-care bedside education (simulated CPR with real-time feedback on a manikin) improved the rate of survival to hospital discharge with favourable neurologic outcome after p-IHCA.17 Compared with usual care, the bundled intervention did not significantly improve survival to hospital discharge with favourable neurologic outcome in that study.
The quality of both point-of-care simulated CPR and actual CPR during p-IHCA are likely associated with characteristics of the simulation training. Thus, the primary objective of the current study was to assess the extent to which characteristics of point-of-care bedside CPR simulation training are associated with simulated CPR performance (assessed by chest compression mechanics), actual CPR performance (assessed by intra-arrest haemodynamics and chest compression mechanics), and survival to hospital discharge with favourable neurologic outcome in children after p-IHCA.
METHODS
This study is a pre-specified secondary analysis of the ICU-RESUScitation Project.17 ICU-RESUS was a parallel, stepped-wedge, hybrid cluster randomized interventional trial conducted in 18 paediatric ICUs at 10 sites in the US between October 2016 and March 2021. The University of Utah Institutional Review Board (IRB) served as the central IRB and granted approval with waiver of consent.
Details of the ICU-RESUS intervention have been published.17,18 In brief, the two-part on-going training intervention for multidisciplinary ICU staff included at least monthly 1-hour CPR debriefings to review aspects of care with physiologic data from an actual CPR event. The second part of this intervention included point-of-care bedside simulation to allow ICU staff to practice CPR delivery on a portable manikin. The manikins were equipped with a monitor to provide real-time feedback on the quality of delivery (i.e., rate, depth, release velocity, chest compression fraction). Each ICU had a goal of at least 48 simulation trainings per month; each simulation was one minute in duration.
Details of each point-of-care simulation were recorded and included simulation characteristics and simulation performance. Simulation characteristics included site, time since participant’s last simulation, primary discipline of participant, time of simulation, and type of manikin (i.e., infant, large child). The number of days on which simulation training was done for the most recent month in which a minimum of 48 simulations were completed was recorded. Simulation performance indicators included average rate (target 90–130 compressions/minute), average depth (target ≥40 mm for infant and ≥50 mm for child manikin), full release, and chest compression fraction (target ≥80%).
Actual CPR performance was recorded for children 37 weeks post-conceptual age to 18 years who received chest compressions of any duration in an ICU. For this secondary analysis, only children who had an arterial catheter or defibrillator waveforms available were included. Children were excluded if, prior to arrest, they had (1) documented goals of care that limited aggressive ICU therapies; (2) brain death; or (3) an out-of-hospital cardiac arrest associated with the current hospitalization. For children with arterial waveforms, haemodynamic data used to assess actual CPR performance included average rate (target 90–130 compressions/minute), average diastolic blood pressure (target ≥25 mmHg for age <1 year or ≥30 mmHg for age ≥1 year), average systolic blood pressure (target ≥60 mmHg for age <1 year or ≥80 mmHg for age ≥1 year), and chest compression fraction (target ≥80%). For children with defibrillator data, mechanics used to assess actual CPR performance included average rate (target 90–130 compressions/minute), average compression depth (target ≥40 mm for age <1 year or ≥50 mm for age ≥1 year), average release velocity (target >300 mm/s) and chest compression fraction (target ≥80%). Averages for haemodynamic and mechanics data were calculated for each 30-second epoch of CPR; only data from the first 10 minutes of CPR were collected.
The primary child outcome was survival to hospital discharge with favourable neurologic outcome based on Paediatric Cerebral Performance Category (PCPC) score.19 Favourable neurologic outcome was defined as no more than moderate disability (PCPC of 1, 2 or 3) or no worse than baseline. Other child outcomes included sustained return of spontaneous circulation (ROSC ≥20 minutes), survival to hospital discharge, and functional status at hospital discharge. Functional status was based on the Functional Status Scale (FSS)20 and assessed in survivors as absolute change from baseline to hospital discharge. New morbidity was defined as worsening from baseline FSS by 3 or more points.20
Statistical Analysis
Characteristics of point-of-care simulations were summarized using frequencies and percentages or medians and quartiles (Table 1). Associations between simulation characteristics and simulation performance indicators were assessed using Fisher’s exact test for nominal variables, Cochran-Armitage test for trend for ordinal variables, and Wilcoxon rank-sum for continuous variables (Table 2).
Table 1.
Simulation Program Characteristics
| Overall | |
|---|---|
| Characteristics by simulation | 18,912 |
| Intensive care unit | |
| A | 2612 (13.8%) |
| B | 1284 (6.8%) |
| C | 1309 (6.9%) |
| D | 62 (0.3%) |
| E | 1422 (7.5%) |
| F | 1649 (8.7%) |
| G | 361 (1.9%) |
| H | 374 (2.0%) |
| I | 1708 (9.0%) |
| J | 1756 (9.3%) |
| K | 571 (3.0%) |
| L | 685 (3.6%) |
| M | 2369 (12.5%) |
| N | 2363 (12.5%) |
| O | 387 (2.0%) |
| Time since participant’s last simulation | |
| This is my first simulation | 4063 (21.5%) |
| Earlier this month | 2720 (14.4%) |
| Last month | 5439 (28.8%) |
| 2 months ago | 3095 (16.4%) |
| 3 or more months ago | 3595 (19.0%) |
| Primary discipline of participant | |
| Physician | 3717 (19.7%) |
| Nurse | 11986 (63.4%) |
| Respiratory therapist | 1852 (9.8%) |
| Other | 1357 (7.2%) |
| Time of training1 | |
| Weekday day | 14446 (76.4%) |
| Weekday night | 1620 (8.6%) |
| Weekend day | 1675 (8.9%) |
| Weekend night | 1171 (6.2%) |
| Type of manikin | |
| Infant | 12070 (63.8%) |
| Large child | 6842 (36.2%) |
| Characteristics by month | 378 |
| Number of days on which simulation training was done2 | 4.0 [3.0,5.0] |
Day is between 7:00 am to 11:00 pm. Weekday is Monday, starting from 7:00 am until Friday 11:00 pm. Weekend is after Friday 11 pm until Monday at 7:00 am.
For the most recent month prior to the current month in which a minimum of 48 simulations were conducted in the unit.
Table 2.
Association between Simulation Characteristics and Simulation Performance
| Average rate of 90–130 compressions/minute | Average depth of ≥ 40 mm for infant and ≥ 50 mm for child manikin | Chest compression fraction ≥ 80% | ||||
|---|---|---|---|---|---|---|
| Yes (N = 18697) | P-value | Yes (N = 17474) | P-value | Yes (N = 18812) | P-value | |
| Intensive care unit | <.0011 | <.0011 | <.0011 | |||
| A | 99.3% | 90.8% | 99.8% | |||
| B | 99.1% | 95.4% | 99.8% | |||
| C | 98.9% | 91.2% | 99.5% | |||
| D | 96.8% | 90.3% | 100.0% | |||
| E | 99.2% | 96.1% | 99.9% | |||
| F | 99.3% | 93.9% | 99.5% | |||
| G | 98.9% | 91.1% | 100.0% | |||
| H | 97.6% | 89.0% | 99.5% | |||
| I | 97.9% | 94.8% | 98.3% | |||
| J | 98.6% | 94.7% | 99.1% | |||
| K | 96.5% | 79.9% | 98.2% | |||
| L | 99.0% | 83.9% | 99.9% | |||
| M | 99.4% | 93.6% | 99.5% | |||
| N | 99.3% | 93.1% | 99.7% | |||
| P | 97.4% | 83.2% | 100.0% | |||
| Time since participants last simulation | <.0012 | <.0012 | 0.0372 | |||
| This is my first simulation | 98.2% | 86.9% | 99.6% | |||
| Earlier this month | 99.3% | 95.1% | 99.6% | |||
| Last month | 99.4% | 94.6% | 99.7% | |||
| 2 months ago | 99.3% | 94.5% | 99.7% | |||
| 3 or more months ago | 98.1% | 91.4% | 98.7% | |||
| Primary discipline of participant | 0.0021 | <.0011 | 0.0931 | |||
| Physician | 99.3% | 93.9% | 99.8% | |||
| Nurse | 98.9% | 92.5% | 99.4% | |||
| Respiratory therapist | 98.1% | 89.9% | 99.6% | |||
| Other | 98.5% | 90.6% | 99.0% | |||
| Time of simulation3 | 0.0921 | <.0011 | 0.0271 | |||
| Weekday day | 98.9% | 92.5% | 99.4% | |||
| Weekday night | 98.7% | 90.1% | 99.5% | |||
| Weekend day | 98.9% | 94.0% | 99.9% | |||
| Weekend night | 98.7% | 91.8% | 99.3% | |||
| Type of manikin | 0.3411 | <.0011 | 0.0041 | |||
| Infant | 98.8% | 95.6% | 99.4% | |||
| Large child | 99.0% | 86.7% | 99.5% | |||
| Number of days on which simulation training was done4 | 4.0 [30,5.0] | 0.9715 | 4.0 [3.0,5.0] | <.0015 | 4.0 [3.0,5.0] | 0.6095 |
Fisher’s exact test.
Cochran-Armitage test for trend.
Day is between 7:00 am to 11:00 pm. Weekday is Monday, starting from 7:00 am until Friday 11:00 pm. Weekend is after Friday 11 pm until Monday at 7:00 am.
For the most recent month prior to the current month in which a minimum of 48 simulations were conducted in the unit.
Wilcoxon rank-sum test.
Percentages are based on row totals.
Actual CPR performance measured by arterial catheter and defibrillator waveforms was summarized using frequencies and percentages or medians and first and third quartiles (Table 3). Associations between simulation characteristics and actual CPR performance indicators were assessed using logistic regression models of epoch-level targets (Supplemental Material 1 and 2). To account for correlation between 30-second epochs within the same resuscitation event, generalized estimating equations were used with an autoregressive, AR (1), correlation structure to account for a higher correlation between temporally close epochs within an event. For each CPR event, the characteristics of the most recent 48 simulations were used as predictors in the logistic regression. This reflects the characteristics of simulations over approximately one month immediately prior to the CPR event. Associations between the presence of an arterial catheter and achievement of mechanical targets from defibrillator data were similarly evaluated (Supplemental Material 3).
Table 3.
Resuscitation Performance in Actual CPR in Intensive Care Units
| Overall | |
|---|---|
| Haemodynamic (arterial data; 198 children) | 2309 epochs1 |
| Average rate of 90–130 compressions/minute | 74.6% |
| Average diastolic pressure ≥ 25 mmHg for age <1 year or ≥ 30 mmHg for age ≥ 1 year | 85.5% |
| Average systolic pressure ≥ 60 mmHg for age <1 year or ≥ 80 mmHg for age ≥ 1 year | 66.5% |
| Chest compression fraction ≥ 80% | 87.1% |
| Target rate, systolic pressure, and chest compression fraction indicated by the parameters above | 57.8% |
| Mechanics (defibrillator data; 115 children) | 3452 epochs1 |
| Average rate of 90–130 compressions/minute | 90.6% |
| Mean compression depth (mm) | |
| Age < 1 year | 26.5 [21.3,33.2] |
| Age ≥ 1 year | 49.2 [36.2,61.3] |
| Average depth of ≥ 40 mm for age < 1 year and ≥ 50 mm for age ≥1 year | 36.4% |
| Average release velocity > 300 mm/s | 35.3% |
| Chest compression fraction ≥ 80% | 70.4% |
| Target rate, depth, and chest compression fraction indicated by the parameters above | 28.1% |
The unit of observation for actual resuscitation in intensive care units is the individual 30-second epoch.
Simulation characteristics were also compared between the top two and bottom three sites with regard to improvement in achieving high quality CPR during actual events using Fisher’s exact and Wilcoxon rank-sum tests (Table 4). High quality CPR was based on arterial waveforms and defined as chest compression rate 90–130 compressions/minute, chest compression fraction ≥80%, and diastolic pressure ≥25 mmHg for age <1 year or ≥30 mmHg for age ≥1 year. For each site, improvement in achieving high quality CPR from the control period to the intervention period was assessed. Only sites with ≥10 CPR events in both the control and intervention periods were included in this analysis. Sites that transitioned to the intervention early or late in ICU-RESUS were therefore excluded. Six sites had ≥10 CPR events in each period but one site had only a single event in the intervention period with arterial waveform data, and was excluded. Five sites remained. The top 2 sites were compared to the bottom 3 sites.
Table 4.
Summary of Simulation Characteristics by Improvement in Achieving High Quality CPR Intensive Care Units
| Top 2 or Bottom 3 Units (Improvement in Achieving High Quality CPR)1 | ||||
|---|---|---|---|---|
| Overall | Top two | Bottom Three | P-value | |
| Characteristics by simulation | 6235 | 2593 | 3642 | |
| Time since participants last simulation | <.0012 | |||
| This is my first simulation | 19.4% | 20.8% | 18.4% | |
| Earlier this month | 18.6% | 25.7% | 13.5% | |
| Last month | 29.7% | 32.7% | 27.6% | |
| 2 months ago | 11.9% | 9.7% | 13.5% | |
| 3 or more months ago | 20.3% | 11.1% | 26.9% | |
| Primary discipline of participant | <.0012 | |||
| Physician | 13.5% | 13.1% | 13.8% | |
| Nurse | 70.1% | 76.4% | 65.6% | |
| Respiratory therapist | 9.0% | 3.2% | 13.1% | |
| Other | 7.4% | 7.3% | 7.5% | |
| Time of training3 | <.0012 | |||
| Weekday day | 77.0% | 93.8% | 65.0% | |
| Weekday night | 9.0% | 2.4% | 13.6% | |
| Weekend day | 9.1% | 3.2% | 13.2% | |
| Weekend night | 5.0% | 0.5% | 8.1% | |
| Type of manikin | <.0012 | |||
| Infant | 53.9% | 49.1% | 57.3% | |
| Large child | 46.1% | 50.9% | 42.7% | |
| Average rate of 90–130 compressions/minute | 98.9% | 99.0% | 98.8% | 0.5412 |
| Average depth of ≥ 40 mm for infant and ≥ 50 mm for child manikin | 92.9% | 93.3% | 92.6% | 0.2692 |
| Percentage of compressions with full release | 98.0 [91.0,100.0] | 97.0 [88.0,100.0] | 99.0 [93.0,100.0] | <.0014 |
| Chest compression fraction ≥ 80% | 99.5% | 99.7% | 99.4% | 0.1252 |
| Characteristics by month 5 | 127 | 50 | 77 | |
| Number of days on which simulation training was done | 4.0 [3.0,5.0] | 4.0 [3.0,5.0] | 4.0 [3.0,5.0] | 0.0804 |
Study units with less than 10 events in the control or intervention period were excluded.
High quality CPR was based on arterial waveform data and defined as chest compression rate 90–130 compressions/minute, chest compression fraction ≥80%, and diastolic pressure ≥25 mmHg for age <1 year or ≥30 mmHg for age ≥1 year.
Fisher’s exact test.
Day is between 7:00 am to 11:00 pm. Weekday is Monday, starting from 7:00 am until Friday 11:00 pm. Weekend is after Friday 11 pm until Monday at 7:00 am.
Wilcoxon rank-sum test.
Characteristics by month are the number of months per unit of rolling refreshers.
Associations between simulation characteristics and child outcomes were assessed using univariable Poisson regression with robust error estimates (Supplemental Material 4). As above, simulation characteristics were based on the site’s most recent 48 simulations prior to the CPR event. This shows the estimated increase (or decrease) in probability of each child outcome as a function of, for example, how many of the most recent 48 simulations were performed on a weekend night.
Simulation characteristics were also compared between the top three and bottom three sites with regard to improvement in survival to hospital discharge with favourable neurologic outcome (Table 5) using Fisher’s exact and Wilcoxon rank-sum tests. For each site, improvement in this outcome from the control period to the intervention period was assessed. Only the six sites with ≥10 CPR events in both periods were included in this analysis.
Table 5.
Summary of Simulation Characteristics and Improvement in Survival to Hospital Discharge with Favourable Neurologic Outcome
| Top 3 or Bottom 3 Units (Improvement in Survival with Favourable Neurologic Outcome)1 | ||||
|---|---|---|---|---|
| Overall | Top three | Bottom Three | P-value | |
| Characteristics by simulation | 6920 | 4015 | 2905 | |
| Time since participants last simulation | <.0012 | |||
| This is my first simulation | 20.9% | 17.7% | 25.3% | |
| Earlier this month | 17.2% | 21.3% | 11.4% | |
| Last month | 28.9% | 32.4% | 24.1% | |
| 2 months ago | 12.8% | 11.2% | 15.0% | |
| 3 or more months ago | 20.2% | 17.4% | 24.1% | |
| Primary discipline of participant | <.0012 | |||
| Physician | 12.4% | 9.9% | 16.0% | |
| Nurse | 69.3% | 74.6% | 62.0% | |
| Respiratory therapist | 10.9% | 6.9% | 16.5% | |
| Other | 7.3% | 8.6% | 5.5% | |
| Time of training3 | <.0012 | |||
| Weekday day | 78.3% | 83.4% | 71.1% | |
| Weekday night | 9.1% | 6.8% | 12.2% | |
| Weekend day | 8.2% | 7.4% | 9.2% | |
| Weekend night | 4.5% | 2.3% | 7.5% | |
| Type of manikin | <.0012 | |||
| Infant | 53.8% | 56.9% | 49.4% | |
| Large child | 46.2% | 43.1% | 50.6% | |
| Average rate of 90–130 compressions/minute | 98.9% | 99.0% | 98.7% | 0.1492 |
| Average depth of ≥ 40 mm for infant and ≥ 50 mm for child manikin | 92.0% | 94.3% | 88.8% | <.0012 |
| Percentage of compressions with full release | 98.0 [90.0,100.0] | 98.0 [90.0,100.0] | 98.0 [90.0,100.0] | 0.5514 |
| Chest compression fraction > 80% | 99.6% | 99.8% | 99.3% | 0.0062 |
| Characteristics by month 5 | 140 | 79 | 61 | |
| Number of days on which simulation training was done | 4.0 [3.0,5.0] | 4.0 [3.0,5.0] | 3.0 [2.0,4.0] | <.0014 |
Study units with less than 10 events in the control or intervention period were excluded.
Favourable neurologic outcome is Paediatric Cerebral Performance Category of 1, 2, or 3, or no change from baseline.
Fisher’s exact test.
Day is between 7:00 am to 11:00 pm. Weekday is Monday, starting from 7:00 am until Friday 11:00 pm. Weekend is after Friday 11 pm until Monday at 7:00 am.
Wilcoxon rank-sum test.
Characteristics by month are the number of months per unit of rolling refreshers.
Associations between child outcomes and achievement of compression depth targets during actual CPR were assessed using Fisher’s exact and Wilcoxon rank-sum tests (Supplemental Material 5). All p-values were reported based on a 2-sided alternative and considered statistically significant when <0.05. Analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Point-of-care simulation
Overall, 18,912 point-of-care simulations were included (Table 1). More simulations were performed by nurses (63.4%) than physicians (19.7%) and respiratory therapists (9.8%). Most simulations occurred during the day on weekdays (76.4%) using the infant manikin (63.8%). Simulation characteristics including site, time since participant’s last simulation, discipline of participant, time of simulation, type of manikin, and number of days per month in which simulation training was done were each associated with one or more simulation performance indicators (proportion achieving targeted rate, depth, and chest compression fraction) (Table 2).
Actual CPR Performance in ICU
Actual CPR performance data in the ICU is shown in Table 3 with haemodynamic data presented for children with arterial waveforms (n=198; 2309 epochs) and mechanics data for children with defibrillator waveforms (n=115; 3452 epochs). In children with haemodynamic data, targeted rate of compressions was achieved in 74.6% of epochs, targeted diastolic pressure in 85.5%, targeted systolic pressure in 66.5% and targeted chest compression fraction in 87.1%. In children with defibrillator data, targeted rate of compressions was achieved in 90.6% of epochs, targeted compression depth in 36.4%, targeted release velocity in 35.3% and targeted chest compression fraction in 70.4%.
Comparison of simulated CPR performance and actual CPR performance
CPR performance in point-of-care simulation was better than actual performance in terms of achieving targeted rate, depth and chest compression fraction (Figure 1).
Figure 1.
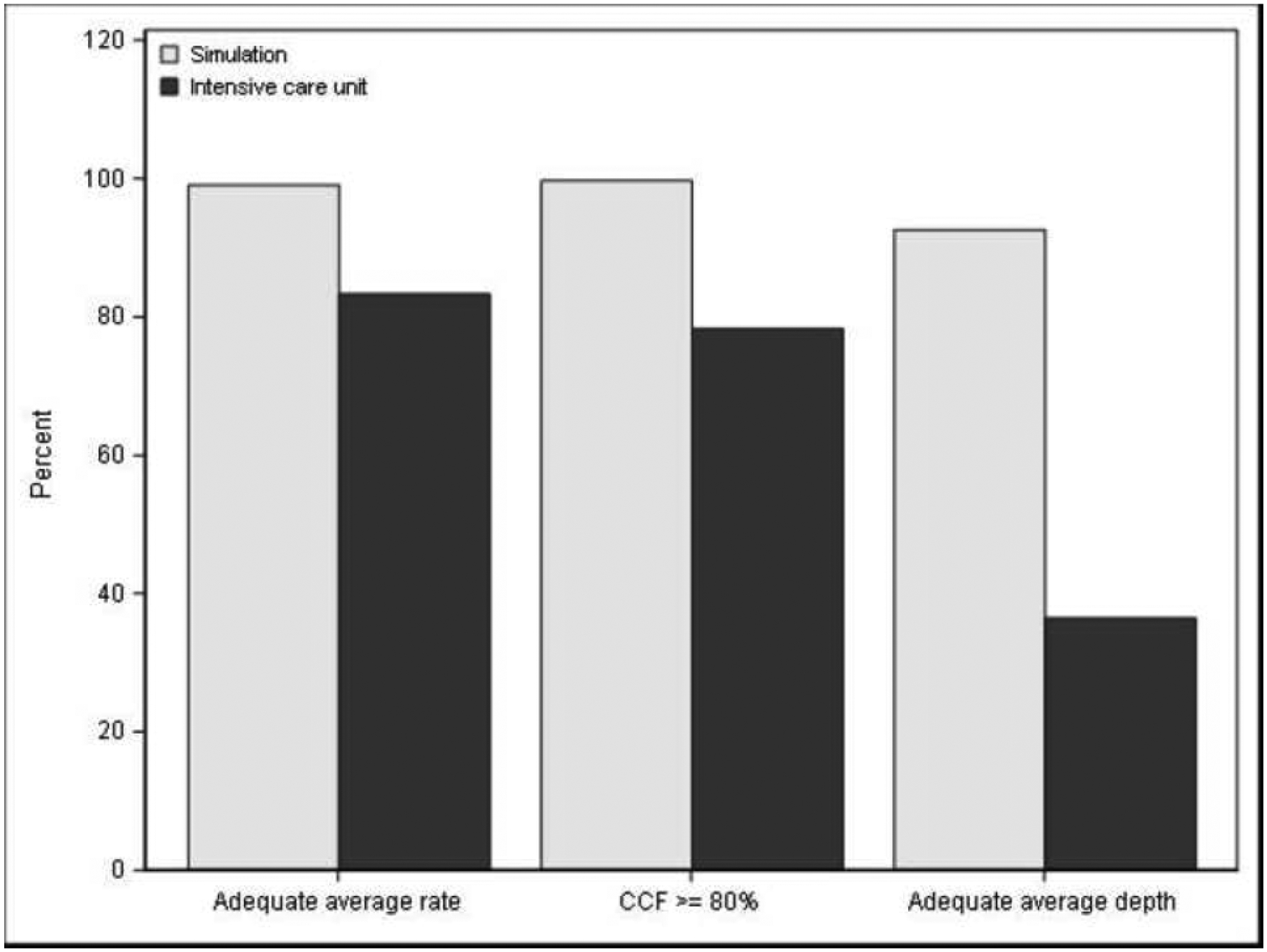
Simulated CPR Performance and Actual CPR Performance in Intensive Care Unit Figure 1 is a bar chart comparing resuscitation performance during simulated versus actual CPR in the intensive care unit (ICU). The unit of observation is the simulation (< 1 minute) or a 30-second epoch during an ICU resuscitation event. Bars show the percentage of simulations or epochs achieving the specified target. For ICU performance, average chest compression rate and chest compression fraction are obtained from arterial catheter waveforms, if available; otherwise, they are obtained from defibrillator waveforms if available. Only subjects whose index event had arterial catheter or defibrillator waveforms available are included. Average depth is only assessed for subjects whose index event had defibrillator waveforms available. All simulations are included.
Association between simulation characteristics and actual CPR performance
Associations between simulation characteristics and resuscitation haemodynamics during actual CPR events are presented in Supplemental Material 1. Site was associated with increased odds of achieving targeted chest compression fraction during actual CPR events. Physician participation was associated with increased odds of achieving average diastolic blood pressure targets, and simulation training during the day on weekends had increased odds of achieving average systolic blood pressure and chest compression fraction targets.
Associations between simulation characteristics and resuscitation mechanics during actual CPR events are presented in Supplemental Material 2. Nurse participants and simulation training during the day on weekdays had increased odds of achieving average rate of compressions in targeted range. The presence of an arterial catheter was not associated with increased odds of achieving mechanical targets during actual CPR (Supplemental Material 3).
Simulation characteristics summarized by top 2 and bottom 3 sites with respect to improvement in achieving high-quality CPR are presented in Table 4. Participants from the top 2 sites were more likely to have participated in a recent simulation (earlier the same month or the previous month) than the bottom 3 sites. Nursing participation was higher in the top 2 sites and simulations occurred more often during a weekday day with the child manikin.
Associations between simulation characteristics and child outcomes
Associations between simulation characteristics and child outcomes are presented in Supplemental Material 4. Site was associated with ROSC; however, no other simulation characteristics were associated with outcomes.
Simulation characteristics summarized by top 3 and bottom 3 sites with respect to improvement in survival to hospital discharge with favourable neurologic outcome are presented in Table 5. Participants at top 3 sites were more likely to have participated in a recent simulation and were more often nurses compared to the bottom 3 sites. Top 3 sites conducted simulations more often during weekday days and with the infant manikin. Simulation performance was better at top 3 sites with participants achieving targeted depth of compression and chest compression fraction goals more often than bottom 3 sites. Finally, simulations were performed on more days per month in top 3 than bottom 3 sites. No associations were found between achieving depth of compression targets during actual CPR and any child outcomes (Supplemental Material 5).
DISCUSSION
In this secondary analysis of the ICU-RESUS trial, we found that point-of-care simulation characteristics were associated with both simulated and actual performance in ICU CPR events. Simulation characteristics associated with simulation performance included site, time since last participation, participant discipline, time of simulation, manikin type and number of days per month in which simulation training was done. Simulation characteristics associated with actual CPR performance included site, participant discipline, and time of simulation training. Resuscitation performance in point-of-care simulation was better than actual performance in ICU CPR events in terms of achieving targeted rate, compression depth, and chest compression fraction. Simulation characteristics were not associated with survival to hospital discharge with favourable neurologic outcome. However, simulation characteristics that were associated with being among the top sites for improvement in achieving high-quality CPR and/or improvement in survival to discharge with favourable neurologic outcome included more recent participation in simulation, a higher proportion of nurse participation, and simulations conducted on weekday days. More days per month on which simulation training was done and better simulated compression depth and chest compression fraction were also more likely in the top sites for improvement in survival with favourable neurological outcome than the bottom sites.
Shorter time from last participation in a point-of-care simulation was associated with improved simulation performance and greater likelihood of being a top site for improvement in achieving high quality CPR and improvement in survival to discharge with favourable neurologic outcome. Previous studies suggest that substantial decay in resuscitation skills occurs within weeks to months after training.21,22 The American Heart Association (AHA) 2018 statement on resuscitation education science details education strategies;22 strategies focused on mastery learning and deliberate practice decrease the rate of decay of skills.23–25 However, mastery learning and deliberate practice are time- and resource-intensive. Our intervention was brief and targeted. More recent participation in simulation training likely resulted in less decay in skills. This finding is important especially in the current post-pandemic era of staffing shortages where time for educational opportunities is often limited.
We found that a higher proportion of nursing participation in point-of-care simulation was associated with improved actual CPR performance and greater likelihood of being a top site for improvement in achieving high quality CPR and improvement in survival to discharge with favourable neurologic outcome. Nurses are typically the first responders during p-IHCA. Their recognition and timely initiation of CPR during an actual resuscitation is key to improving outcomes. A single centre study reported substantial variability in time to initiate CPR in continuously monitored paediatric ICU patients.26 It is unclear whether higher nursing participation in our simulations resulted in better recognition of cardiac arrest, more timely initiation of CPR, or improved quality of CPR during an actual resuscitation. Another possibility is that this finding is unrelated to the educational intervention itself but that increased nursing participation reflects some unmeasured unit factor such as better staffing or more unit engagement in nursing education.
CPR simulations conducted during the daytime hours were associated with improved simulated and actual CPR performance compared to simulations conducted at night. It is possible that simulations conducted during the day results in better learning and retention of psychomotor skills. Additionally, since most simulation training was done during the day, it is possible that daytime staff became better trained to conduct high quality CPR. Better trained staff could account for the association observed between weekday day simulation training and being a top site for improvement in survival with favourable neurological outcome in our study. Other studies have reported increased survival when p-IHCA occurs on weekday days compared to nights and weekends despite no measureable difference in the quality of CPR between these time periods.27,28 These other studies suggest factors other than CPR quality may account for the difference in outcomes.
Resuscitation performance in point-of-care simulation was better than actual ICU performance, and actual performance assessed by haemodynamic data from arterial waveforms was better overall than actual performance assessed by mechanical defibrillator data. Clinicians conducting CPR on children with arterial catheters may have used the arterial waveforms displayed on bedside monitors to gauge the effectiveness of CPR and guide their actions. However, the presence of an arterial catheter did not improve the odds of achieving mechanical targets in our study. Perhaps adequate arterial blood pressures were achieved with less forceful compressions than needed to reach depth targets. It is also possible that clinicians focused more on physiologic targets than mechanical targets since the bundle of structured debriefings and point-of-care simulations emphasized that physiologic targets improve outcomes. Also consistent with the focus on physiologic rather than mechanical targets, we found no associations between achieving mechanical depth of compression targets during actual CPR and child outcomes. Prior reports from the ICU-RESUS dataset have shown association between achieving physiologic targets during actual CPR (average diastolic blood pressure ≥25 mmHg for age <1 year or ≥30 mmHg for age ≥1 year) and increased ROSC and survival to hospital discharge.29
Strengths of this study include the multicentre design, prospective data collection, and the large number of simulated point-of-care events recorded. Limitations include the fact that this study was performed in academic ICUs with existing educational programs; therefore, it may not be generalizable to all paediatric ICUs. Simulations trained participants to administer chest compressions to a compression depth target whereas our definition of high quality CPR was based on achieving a diastolic blood pressure target. Ideally, targets used for training and evaluating quality of actual CPR would be the same. Additionally, training performance for individual participants could not be paired with their performance in actual CPR. Importantly, this is an observational study and although associations were identified, the study design precludes our ability to determine causation.
CONCLUSIONS
Point-of-care simulation characteristics were associated with both simulated and actual performance in paediatric ICU CPR events. More recent simulation training, increased nursing participation, and simulation training during daytime hours may improve CPR performance.
Supplementary Material
Role of Funding Source
This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, or National Institutes of Health.
Declaration of Interest Statement
This study was funded by the following grants from the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development: R01HL131544, U01HD049934, UG1HD049981, UG1HD049983, UG1HD050096, UG1HD063108, UG1HD083166, UG1HD083170, UG1HD083171, and K23HL148541. Two of the co-authors, Dr. Robert Berg and Dr. Vinay Nadkarni, are members of the Resuscitation Editorial Board.
CRediT Author Statement
| Author | Contribution |
|---|---|
| Cashen | Conceptualization, writing- original draft |
| Sutton | Conceptualization, data curation, formal analysis, funding acquisition, methodology, supervision, writing – review and editing |
| Reeder | Formal analysis, methodology, validation |
| Ahmed | Investigation, writing – review and editing |
| Bell | Investigation, writing – review and editing |
| Berg | Conceptualization, funding acquisition, investigation, writing – review and editing |
| Bishop | Investigation, writing – review and editing |
| Bochkoris | Investigation, writing – review and editing |
| Burns | Investigation, writing – review and editing |
| Carcillo | Funding acquisition, investigation, writing – review and editing |
| Carpenter | Funding acquisition, investigation, writing – review and editing |
| Diddle | Investigation, writing – review and editing |
| Federman | Investigation, writing – review and editing |
| Fink | Investigation, writing – review and editing |
| Franzon | Investigation, writing – review and editing |
| Frazier | Investigation, writing – review and editing |
| Friess | Investigation, writing – review and editing |
| Hall | Funding acquisition, investigation, writing – review and editing |
| Graham | Investigation, writing – review and editing |
| Hehir | Investigation, writing – review and editing |
| Horvat | Investigation, writing – review and editing |
| Huard | Investigation, writing – review and editing |
| Maa | Investigation, writing – review and editing |
| Manga | Investigation, writing – review and editing |
| McQuillen | Funding acquisition, investigation, writing – review and editing |
| Morgan | Funding acquisition, investigation, writing – review and editing |
| Mourani | Funding acquisition, investigation, writing – review and editing |
| Nadkarni | Conceptualization, supervision, writing – review and editing |
| Naim | Investigation, writing – review and editing |
| Notterman | Supervision, writing – review and editing |
| Palmer | Formal analysis, writing – review and editing |
| Pollack | Funding acquisition, investigation, writing – review and editing |
| Sapru | Funding acquisition, investigation, writing – review and editing |
| Schneiter | Investigation, writing – review and editing |
| Sharron | Investigation, writing – review and editing |
| Srivastava | Investigation, writing – review and editing |
| Viteri | Investigation, writing – review and editing |
| Wolfe | Investigation, writing – review and editing |
| Yates | Investigation, writing – review and editing |
| Zuppa | Funding acquisition, investigation, writing – review and editing |
| Meert | Conceptualization, funding acquisition, investigation, writing – review and editing |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Holmberg MJ, Ross CE, Fitzmaurice GM, et al. Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes 2019; 12:e005580. [PMC free article] [PubMed] [Google Scholar]
- 2.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med 2011;39:2401–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berg RA, Sutton RM, Holubkov CE, et al. Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med 2013;41:2292–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmberg MJ, Wiberg S, Ross CE, et al. Trends in survival after pediatric in-hospital cardiac arrest in the United States. Circulation 2019;22:140:1398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Topjian AA, de Caen A, Wainwright MS, et al. Pediatric post-cardiac arrest care: A scientific statement from the American Heart Association. Circulation 2019;140:e194–e233. [DOI] [PubMed] [Google Scholar]
- 6.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA 2005;293:305–10. [DOI] [PubMed] [Google Scholar]
- 7.Cheskes S, Schmicker RH, Christenson J, et al. Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation 2011;124:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation 2009;120:1241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Idris AH, Guffey D, Aufderheide TP, et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation 2012;125:3004–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamilton R Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs 2005;51:288–97. [DOI] [PubMed] [Google Scholar]
- 11.Semeraro F, Signore L, Cerchiari EL. Retention of CPR performance in anaesthetists. Resuscitation 2006;68:101–8. [DOI] [PubMed] [Google Scholar]
- 12.Mancini ME, Kaye W. The effect of time since training on house officers’ retention of cardiopulmonary resuscitation skills. Am J Emerg Med 1985;3:31–2. [DOI] [PubMed] [Google Scholar]
- 13.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using real-time audiovisual feedback system. Resuscitation 2007;73:54–61. [DOI] [PubMed] [Google Scholar]
- 14.Hostler D, Everson-Stewart S, Rea TD, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ 2011;342:d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Niles D, Sutton RM, Donoghue A, et al. “Rolling refreshers”: a novel approach to maintain CPR psychomotor skill competence. Resuscitation 2009;80:909–12. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med 2014;42;1688–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutton RM, Wolfe HA, Reeder RW, et al. Effect of physiologic point of care cardiopulmonary resuscitation training on survival with favorable neurologic outcome in cardiac arrest in pediatric ICUs. JAMA 2022;327;934–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reeder RW, Girling A, Wolfe H, et al. Improving outcomes after pediatric cardiac arrest-the ICU-Resuscitation Project: study protocol for a randomized controlled trial. Trials 2018;19:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr 1992;121:68–74. [DOI] [PubMed] [Google Scholar]
- 20.Pollack MM, Holubkov R, Funai T, et al. Relationship between the functional status scale and the pediatric overall performance category and pediatric cerebral performance category scales. JAMA Pediatr 2014;168:671–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wayne DB, Siddall VJ, Butter J, et al. A longitudinal study of internal medicine residents’ retention of advanced cardiac life support skills. Acad Med 2006;81(suppl 10):9–12. [DOI] [PubMed] [Google Scholar]
- 22.Cheng A, Nadkarni VM, Mancini MB, et al. Resuscitation education science: educational strategies to improve outcomes from cardiac arrest: a scientific statement from the American Heart Association. Circulation 2018;138:e82–122. [DOI] [PubMed] [Google Scholar]
- 23.Moazed F, Cohen ER, Furiasse N, et al. Retention of critical care skills after simulation-based mastery learning. J Grad Med Educ 2013;5:458–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt EA, Jeffers J, McNamara L, et al. Improved cardiopulmonary resuscitation performance with CODE ACES: A resuscitation quality bundle. J Am Heart Assoc 2018;7:e009860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donoghue A, Heard D, Griffin R, et al. Longitudinal effect of high frequency training on CPR performance during simulated and actual pediatric cardiac arrest. Resuscitation Plus 2021;6:100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olson M, Helfenbein E, Su L, et al. Variability in the time to initiation of CPR in continuously monitored pediatric ICUs. Resuscitation 2018;127:95–9. [DOI] [PubMed] [Google Scholar]
- 27.Esangbedo I, Yu P, Raymond T, et al. Pediatric in-hospital CPR quality at night and on weekends. Resuscitation 2020;146:56–63. [DOI] [PubMed] [Google Scholar]
- 28.Yu P, Esangbedo I, Zhang X, et al. Paediatric in-hospital cardiopulmonary resuscitation quality and outcomes in children with CHD during nights and weekends. Cardiol Young 2022. Jan 21;1–10. doi: 10.1017/S1047951122000099. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 29.Berg RA, Morgan RW, Reeder RW, et al. Diastolic blood pressure threshold during pediatric cardiopulmonary resuscitation and survival outcomes: a multicenter validation study. Crit Care Med 2023;51:91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


