Abstract
COVID-19 vaccines effectively protect against COVID-19-related hospitalization or death, and 67.1% of the US population is fully vaccinated. However, the disparity in COVID-19 vaccination persists among minority and rural populations who often report greater hesitancy about COVID-19 vaccines. This exploratory study aimed to understand and document trusted sources of information about the COVID-19 vaccine among a diverse sample of hesitant adopters with in-depth interviews. Participants (n=21) described how information from trusted sources influenced their decision to get a COVID-19 vaccine despite being hesitant. Participants reported health care professionals, family members, friends, co-workers, community leaders, public health experts, government officials, and the mainstream media as trusted sources of information about the COVID-19 vaccines. Participants discussed obtaining trusted information from multiple modes, including direct conversations with trusted messengers and public health communications from public influencers who reinforced the information shared with trusted messengers. Notably, participants discussed having multiple conversations with trusted messengers during their decision-making process, and these trusted messengers often facilitated the participants’ vaccination process. Study findings highlight the continued need for clear, understandable information about vaccine side effects, safety, and efficacy to address concerns that contribute to vaccine hesitancy.
Keywords: COVID-19 vaccine, hesitant adopters, vaccine hesitancy, trusted sources, vaccine decision-making
Introduction
The United States (US) has reported over 100 million cases and over 1 million COVID-19 deaths since the pandemic began in March 2020 (Centers for Disease Control and Prevention, 2021a; Johns Hopkins University of Medicine, 2022). COVID-19 vaccines effectively protect against COVID-19-related hospitalization or death (Centers for Disease Control and Prevention, 2021b), and 69.5% of Americans are fully vaccinated (Centers for Disease Control and Prevention, 2021a). COVID-19 vaccination disparities continue for minority and rural populations who often report greater hesitancy about COVID-19 vaccines (Balasuriya et al., 2021; Khubchandani J et al., 2021; Kricorian et al., 2022; Malik et al., 2020; Nguyen et al., 2022; Shekhar et al., 2021; Szilagyi et al., 2021; Williams et al., 2022; Willis et al., 2021). In Arkansas, 41% of people live in rural areas, compared to only 14% of the US population who reside in rural counties, and racial and ethnic diversity has increased in Arkansas by 10% from 2010 to 2019 (Miller & Wheeler, 2021). Consistent with national data on decreased vaccination rates in rural and underrepresented communities, Arkansas lags behind other US states in COVID-19 vaccination coverage, with only 57.23% of its population fully vaccinated (Johns Hopkins University of Medicine, 2022).
The World Health Organization (WHO) has highlighted vaccine hesitancy as a top health concern impacting global health (World Health Organization, 2019). Some scholars have described vaccine hesitancy as a continuum of behaviors ranging from refusal to delay of vaccination (MacDonald & Hesitancy, 2015); however, other scholars describe vaccine hesitancy as an attitude related to vaccine behavior that may not represent vaccination status (Quinn et al., 2019). Research on vaccine hesitancy has frequently overlooked those who are hesitant but have been vaccinated, conflating vaccination behaviors with vaccine attitudes (Dubé et al., 2013). Recent research has emphasized a broader conception of vaccine hesitancy as an ongoing personal, community, social, economic, and political process, which has not been fully conceptualized (Larson et al., 2022). Conceptualizing health and health-seeking behaviors as an ongoing process illustrates how vaccination decisions are part of a dynamic and holistic understanding of individual health decision-making (Cowley, 1995; Heggdal, 2015; Larson, 2022; Turchi et al., 2022). Separating vaccination behaviors from vaccine hesitancy could inform approaches to vaccination as a series of processes of health-seeking affected by influences, nudges, and decision points (Larson, 2022).
Emerging research on hesitant adopters of COVID-19 vaccines documents that some individuals get vaccinated despite their continued hesitancy (Enkel et al., 2018; Kirzinger et al.; Moore, Purvis, Willis, et al., 2022; Purvis et al., 2022; Ward et al., 2022; D. E. Willis, J. P. Selig, et al., 2022). One recent study reported 60% of recently vaccinated individuals had some level of hesitancy about the COVID-19 vaccine despite being vaccinated (Don E. Willis et al., 2022), and a survey of French adults found that the number of vaccinated individuals reporting doubts about the vaccine rose from 44% to 61% (Ward et al., 2022). Hesitant adopters (i.e., individuals who received a COVID-19 vaccine despite hesitancy towards COVID-19 vaccines) are an understudied population who may provide insights that can inform future interventions to address vaccine hesitancy and reduce COVID-19 vaccination disparities.
Trusted sources of information about the COVID-19 vaccine can be an essential factor in the decision to become vaccinated (Langwerden et al., 2022; C. A. Latkin et al., 2021; Rusgis et al., 2022; Scherer et al., 2021). Studies show individuals who have high trust in healthcare professionals, the Centers for Disease Control and Prevention (CDC), and mainstream media (i.e., NBC, PBS, CBS) as sources of general COVID-19 and COVID-19 vaccine information are associated with being vaccinated and are more likely to encourage others to become vaccinated (Ali et al., 2020; Bogart et al., 2021; Brauer et al., 2021; Davis et al., 2022; Fridman et al., 2020; Malik et al., 2020; McFadden et al., 2020; Scherer et al., 2021; Wade et al., 2022). Among COVID-19 vaccine hesitant adopters, healthcare providers, medical research, and mainstream news have been documented as trusted sources of vaccine information (R. S. Purvis et al., 2021). Disparities in access to reliable COVID-19 vaccine information and the proliferation of misinformation have exacerbated vaccine hesitancy among minority and rural populations (Kricorian et al., 2022; Zhang et al., 2022). Furthermore, recent research shows that interpersonal communication with healthcare providers, family members, and friends is an important influence on COVID-19 vaccination intention (B. A. AlShurman et al., 2021; Cunningham-Erves et al., 2023; Francis et al., 2022; Zheng et al., 2022). A study examining the association of political ideology with COVID-19 vaccination found that discussion partners were a significant moderator of respondents’ perceived vaccine effectiveness (Jiang et al., 2022).
As the recommendations for vaccination have shifted to annual COVID-19 doses, it is clear that more targeted and specific tools must be developed to build, support, and take advantage of motivations to vaccinate (The White House, 2022). However, a gap remains with little documented about trusted sources of COVID-19 vaccine information and how it influenced the decision to vaccinate among hesitant adopters. To fill that gap, this exploratory study aimed to understand the types of trusted sources of information used related to the COVID-19 vaccine among a diverse sample of hesitant adopters.
Methods
Design and approach
A qualitative descriptive design (Colorafi & Evans, 2016) with individual interviews was used to explore how information from trusted sources influenced participants’ decisions to get a COVID-19 vaccine despite hesitancy. The University of Arkansas for Medical Sciences Institutional Review Board approved all study procedures and materials (IRB# 262907).
Study sample, participant recruitment, consent, and remuneration
From July 12-July 30, 2021, trained interviewers surveyed 1,500 adult Arkansans using computer-assisted telephone surveys, which examined primary influences on COVID-19 vaccine motivation and vaccine behavior. Participants were contacted through random digit dialing of cell phones and landlines. Minority residents were purposefully oversampled. Participants’ vaccine status, COVID-19 vaccine hesitancy level, demographic information (including age, sex, race, and ethnicity), and if they would like to participate in a follow-up interview were captured. To collect trust in the COVID-19 vaccines, we asked participants, “How much do you trust the COVID-19 vaccines?” Participants could respond ‘not at all,’ ‘very little,’ ‘somewhat,’ or ‘very much.’ We measured hesitancy about the COVID-19 vaccines by asking participants, “Thinking specifically about the COVID-19 vaccines, how hesitant were you about getting vaccinated?” Participants could respond ‘not at all hesitant,’ ‘a little hesitant,’ ‘somewhat hesitant,’ and ‘very hesitant.’ To operationalize ‘vaccine hesitancy,’ we have defined a ‘vaccine hesitant’ person as a person reporting any level of vaccine hesitancy. Data from the quantitative survey is published elsewhere (McElfish et al., 2022; D. E. Willis, J. A. Andersen, et al., 2022). Potential participants for the qualitative sample were drawn from respondents who completed the survey and agreed to be contacted for a follow-up interview. Inclusion criteria for interview participation were: 1) ≥18 years, 2) some level of vaccine hesitancy, and 3) vaccinated against COVID-19. Out of the 1,500 total survey respondents, 822 (54.80%) agreed to be contacted for an interview. Of those who agreed to a follow-up interview, 195 reported some level of vaccine hesitancy and had received the COVID-19 vaccine. Potential participants (n=195) were stratified by race, ethnicity, and sex, randomly ordered, and invited through email to participate in the interview. Twenty-eight potential participants responded and were scheduled for an interview; ultimately, 21 completed the interview and comprised the qualitative sample. At the beginning of the interview, the interviewer read the study information sheet, encouraged questions, allowed time for participants to ask questions, and confirmed consent to participate. All participants who completed an interview received a $50 gift card as remuneration.
Data collection
Qualitative data were collected from 21 participants using semi-structured individual interviews between January and March 2022. Participants were asked about their thoughts and feelings, social processes, practical issues, and motivation related to the decision to get the COVID-19 vaccination despite their hesitancy (see Figure 1). Four researchers with qualitative expertise conducted the interviews. Participants were assigned to an interviewer based on availability. Participants were emailed their unique meeting invitation with their scheduled interview date and time. All interviews were conducted using a secure video conferencing platform and telephone (Archibald et al., 2019). The interviews varied in length, ranging between 15 and 45 minutes.
Figure 1.
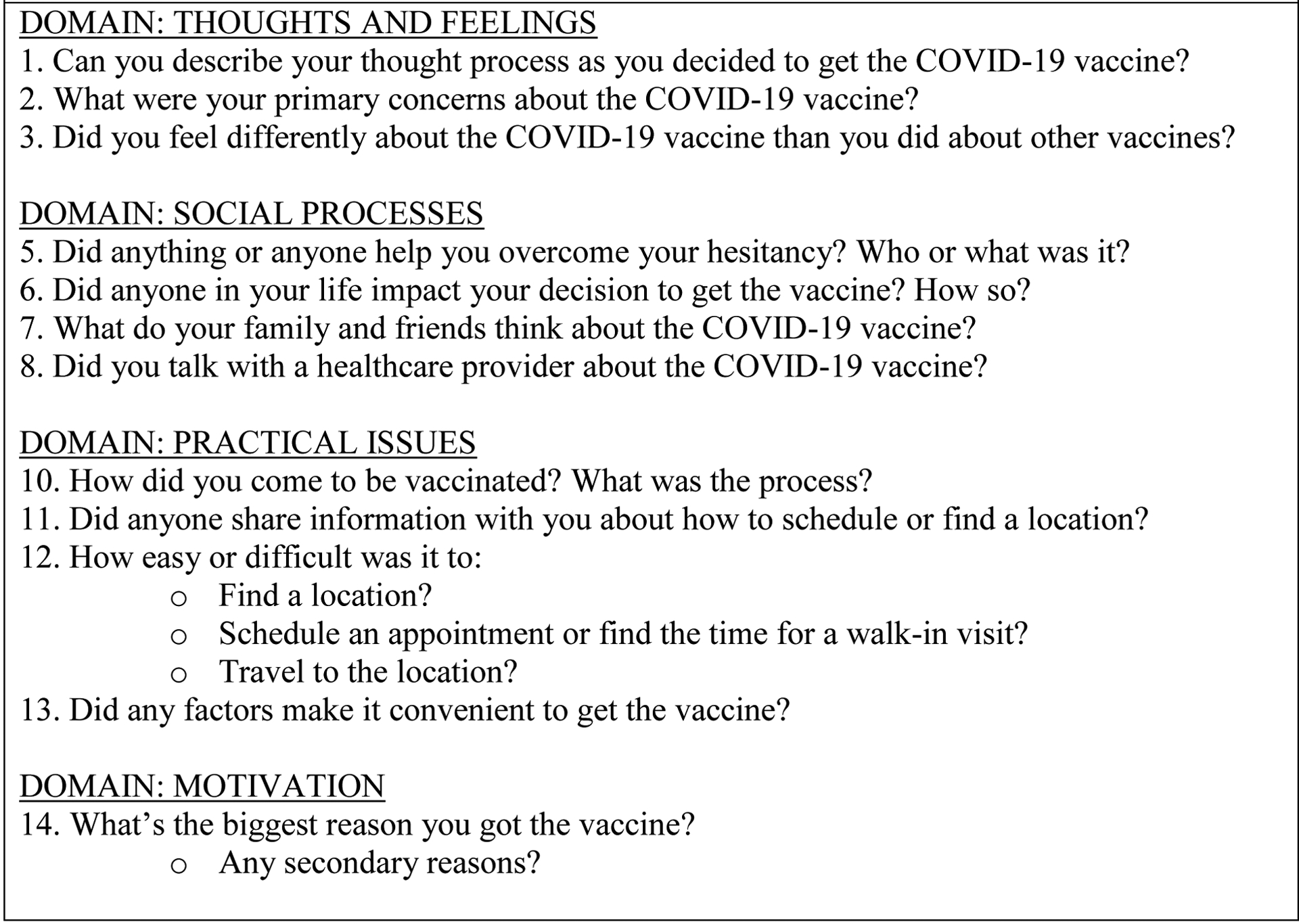
The Semi-Structured Interview Guide Was Used to Facilitate Individual Interviews
Qualitative data analysis
Researchers used a transcription service to transcribe recorded interviews verbatim. The qualitative analysis team imported the de-identified transcripts into a password-protected MAXQDA 2020 (MAXQDA, 1989–2015) project file for analysis (Webb, 1999). Three qualitative researchers conducted a content analysis of the data by carefully reviewing and coding transcripts after reading and rereading the interview data. The content analysis involved interpreting the meaning and labeling data segments with initial codes that emerged from the data (Burla et al., 2008; Hsieh & Shannon, 2005; Rubin & Rubin, 2005). The first author performed initial coding on ten transcripts, labeling data segments with summary emergent codes that were used to organize the data for further focused coding. A preliminary codebook was developed with these emergent codes, and two qualitative researchers conducted confirmation coding and reviewed five transcripts (each). Researchers discussed the coded transcripts, and any discrepancies in data interpretation were reviewed and resolved by consensus of the research team. The first author refined the preliminary codebook, updating codes and their definitions, which guided the coding of the remaining transcripts (Rolfe, 2006). The first author revised the codebook four times. As new codes were identified in the transcripts, the first author incorporated these new codes and their definitions into the codebook. Our team reviewed and re-coded all coded transcripts as necessary to ensure they reflected the final codebook. The research team critically reviewed the data, analysis summaries, codebook, and all coded segments to ensure analytic rigor and reliability (Hennink et al., 2011). The research team used the constant comparison technique to gain conceptual understanding, identify categories, and develop themes using an iterative process of comparing each datum with all other data (Hsieh & Shannon, 2005; Speziale & Carpenter, 2007). Thematic saturation was reached for the sample when no additional emergent themes were identified from the 21 interviews (Boddy, 2016; Morse, 2000). Using a consensus model, the research team identified exemplary quotes that represented the most salient codes and categorized them within the themes they best represented. Participants’ statements could be labeled with multiple codes within their responses; however, our team selected the most demonstrative quotes explaining thematic domains presented below, along with the descriptive sociodemographic characteristics of the sample.
Results
Participant characteristics
We present descriptive statistics of participants’ characteristics, including sociodemographic information, in Table 1. Participants’ mean age was approximately 40 years. Participants were diverse, with nine (42.86%) identifying as Black or African American, five (23.81%) identifying as Hispanic or Latinx, five (23.81%) identifying as White, one (4.76%) identifying as multiracial, and one (4.76%) identifying as non-Hispanic other. Most participants reported being employed for wages (61.90%), and over half reported having a bachelor’s or graduate degree (47.62%). Nine participants (42.9%) reported they were “a little hesitant,” nine participants (42.9%) reported they were “somewhat hesitant,” and three participants (14.3%) reported they were “very hesitant” about the COVID-19 vaccine.
Table 1.
Descriptive Statistics of Hesitant Adopters/Qualitative Sample (n=21)
| Freq. | Mean or % | |
|---|---|---|
| a Age | 20 | 40.4 |
| Gender | -- | -- |
| Men | 8 | 38.10 |
| Women | 13 | 61.90 |
| Race and Ethnicity | -- | -- |
| NH White | 5 | 23.81 |
| NH Black or African American | 9 | 42.86 |
| NH other | 1 | 4.76 |
| Hispanic or Latinx | 5 | 23.81 |
| NH multiracial | 1 | 4.76 |
| Marital Status | -- | -- |
| Married | 8 | 38.10 |
| Divorced | 1 | 4.76 |
| Separated | 1 | 4.76 |
| Never married | 9 | 42.86 |
| Unmarried couple | 2 | 9.52 |
| Parent Status | -- | -- |
| Parent or guardian | 12 | 57.14 |
| Not a parent or guardian | 9 | 42.86 |
| Employment Status | -- | -- |
| Employed for wages | 13 | 61.90 |
| Self-employed | 2 | 9.52 |
| Out of work for 1 year or more | 2 | 9.52 |
| Retired | 2 | 9.52 |
| Unable to work | 2 | 9.52 |
| Education | -- | -- |
| HS grad or equivalent | 4 | 19.05 |
| Some college, no degree | 4 | 19.05 |
| Associate degree | 1 | 4.76 |
| Bachelor’s degree | 10 | 47.62 |
| COVID-19 Vaccine Hesitancy | -- | -- |
| Not at all hesitant | 0 | 0.0 |
| A little hesitant | 9 | 42.9 |
| Somewhat hesitant | 9 | 42.9 |
| Very hesitant | 3 | 14.3 |
20 participants reported their age
NH=non-Hispanic; HS=High School
Percentages are column percentages
Qualitative findings
Participants reported encountering unreliable information and described trusted sources of information that influenced their decision to get a COVID-19 vaccine despite hesitancy. Researchers identified three emergent themes: 1) reasons for hesitancy, 2) multiple modes of getting trustworthy vaccine information, and 3) influential messages about the vaccine and vaccination outcomes.
Reasons for hesitancy
Participants discussed their perceptions and experiences regarding information about the COVID-19 vaccine that influenced their hesitancy. Researchers identified three emergent subthemes within this primary theme: misinformation, lack of trust in the COVID-19 vaccine, and lack of trust in government and/or medical research. These themes were often discussed as interrelated barriers to vaccination by participants.
Misinformation.
Participants discussed misinformation about the COVID-19 vaccine and its influence on their decision to vaccinate. A participant explained, “Well, the only doubts were very early in the process. You hear rumors, it is causing people to have enlarged hearts or whatever.” (58yr old White Male) Another participant discussed rumored side effects: “A lot of weird stories went along with COVID-19, a lot of them saying, ‘Well, it’s going to give it to you if you take it.’” (58yr old AA Female) Other participants described experiences of misinformation as a barrier to vaccination: “There’s so much disinformation going on about it, and everybody’s got their own agenda when they talk about it” (26yr old White Female) and “It was just hard to trust anything that was going on, cause, who is telling the truth? Who is lying? ‘Oh my Gosh, I don’t know what to do.’” (42yr old AA Female)
Lack of trust in the COVID-19 vaccine.
Participants described a lack of trust in the COVID-19 vaccine because it was new and quickly developed as a reason for their hesitancy. A participant summarized: “The reason why I hesitated was because how did they create a vaccine so quick?” (24yr old Hispanic Male) Another participant said, “When they came out with the vaccine, I was like, ‘Whoa, it was too quick.’ It was untrustworthy. I did not want to get it.” (32yr old AA Male) A participant explained, “I was very hesitant [to get vaccinated] because I felt like it was just done too quickly. The tests they did was done too quickly, so we were not sure how it was going to react with everybody.” (28yr old Hispanic Female) Other participants echoed concern about the new vaccine, stating, “I was afraid to take it like other people. I thought it was so fast. I feel they came up with a remedy too fast.” (58yr old AA Female) and “I was thinking that this vaccine was made overnight. I do not want it.” (40yr old Hispanic Female)
Lack of trust in government and/or medical research.
Participants also reported a lack of trust in the government and medical researchers who developed and managed the COVID-19 vaccine rollout as an interrelated reason for their hesitancy. One participant described a lack of trust in the government’s implementation of the vaccine because of past research efforts: “I forgot what they named it, but there was that incidence where they were saying they were giving a vaccine to the African American community. It ended up being syphilis. Forgive me then if I do not trust the government.” (32yr old AA Male) Another participant said, “There was a lot of people that had been shafted by this government and were very hesitant to go get the vaccination. I think of the Tuskegee Experiment. I think of my native brothers and sisters that accepted the boxes of wool blankets infested with smallpox.” (56yr old Hispanic Male) One participant explained a lack of trust in the government’s approach to COVID-19:
There was a little bit of untrust because the government would feel some people were expendable. I know that the government always factor in that some people will be lost with when things roll out. There is a threshold, even with things that are harmful, they factor in that, some people are going to be lost, but the majority of people will be helped.
(42yr old AA Female)
Multiple modes of getting trustworthy vaccine information
Participants identified multiple modes of getting trustworthy vaccine information, which helped them address their hesitancy. Researchers identified two emergent subthemes: key conversations with trusted messengers and public influence.
Key conversations with trusted messengers.
Participants in every interview discussed key conversations with trusted messengers such as healthcare professionals, family members, friends, co-workers, and recognized community leaders as a primary way they gathered information about the COVID-19 vaccine when deciding to get vaccinated.
Participants described key conversations with their primary care physician or pharmacist as important factors in getting vaccinated. A participant said, “I talked to my doctor, he told me how it was developed because I did have questions on how it was developed so quickly, I was pleased with his answers, so my husband and I both got vaccinated on the same day.” The participant said this conversation with her doctor led her to get her children vaccinated: “A couple of weeks after us, my 12-year-old and my 11-year-old did it.” (41yr old White Female)
Another participant described her conversation with her physician: “We talked for an extensive amount of time. She knows my medical history. We talked about the vaccine, the reactions of what I need to look forward to. We had a good conversation.” (53yr old AA Female) Some participants mentioned conversations with their pharmacist who facilitated their vaccination. One participant explained, “We use Sam’s Pharmacy for our other vaccinations, and I said, ‘How hard is it to get the vaccination?’ [her pharmacist responded] ‘I got two left, and we’re closing in five minutes, let’s get you done right now.’” (63yr old White Female) One participant spoke of how her church set up a conference call with a doctor from the congregation who “was able to answer all of our questions about the vaccine and about COVID-19 and she had a lot of good information that I think probably helped a lot of our church members.” (30yr old AA Female)
Participants also described key conversations with family members, friends, and co-workers, which helped them address their hesitancy to get the COVID-19 vaccine. One participant stated, “We decided as a family to get [the vaccine] because at first, we were not going to get it, then my mom’s husband [said] ‘I think we should go ahead and get it now.’ Once he made that decision, we all decided to go get the vaccine.” (30yr old AA Female) Another participant said, “I was on the fence when my mom and her husband got the vaccine, I was not in a rush to get it. We had a few discussions about it. She feels very strongly (about) everybody getting vaccinated.” (29yr old AA Female)
Participants described conversations with family members who were researchers or healthcare professionals. One participant said, “I talked to [my] niece. She is an epidemiologist, so she works with germs, and I talked to her a couple of times.” (43yr old Multiracial Male) Another participant described the value of input from co-workers who are healthcare professionals:
I work in a renal pathology lab, and the pathologists there all have PhDs in immunology, and the rest of them all study pathology. We had three company-wide meetings where they [were] breaking it down scientifically in laymen’s terms, in more detail for those who have a more scientific background. That helped a lot because I have a degree in kinesiology. They were breaking it down in that format for me was major helpful cause then, “Okay, cool. Now, I get it.”
(32yr old AA Male)
One participant described how a key conversation with a co-worker facilitated their vaccination: “We were talking about [the vaccine] at work one day and he told me, ‘Yeah, I got my vaccine a month ago, we’re essential workers’ [and] he pulled up the paperwork for me to get the vaccine.” (56yr old Hispanic Male)
Participants also discussed conversations with recognized community leaders that influenced them to become vaccinated. A participant said, “My pastor at my church helped us feel comfortable about getting [the vaccine].” (30yr old AA Female) Another participant explained, “Our pastor’s part of the CDC … He is very knowledgeable about everything going on with COVID and he’s made an impression on our church family to take the shot.” (58yr old AA Female) One participant discussed her conversation with a former government official: “It made me feel a little safer about it, having someone who I know is very smart—she worked in the Clinton Administration [and] she told me they did not just throw some stuff together, that it was probably in the works before some of us were even born, that piece of information is what persuaded me.” (40yr old Hispanic Female)
Public influence.
Participants described recognized public health experts, government officials, and the mainstream media as an additional mode for obtaining information about the COVID-19 vaccine. This public influence often supported or confirmed COVID-19 vaccine information participants heard in direct conversations within their social networks. One participant said, “Dr. [Anthony] Fauci influenced me because he has been around for a long time. I felt he would not lead me in the wrong direction on the vaccine.” (56yr old AA Female) Another participant explained, “Once the scientific community, the medical community said this is safe to take, I trusted that. I guess the tipping point is when it was encouraged by doctors and researchers.” (26yr old White Female)
Participants described the influence of the mainstream media and government-sponsored vaccine messages. One participant explained, “President Trump took it and said it was safe, and I felt comfortable with going ahead and taking the vaccine.” (43yr old Multiracial Male) Another participant said, “Watching President Biden and some of the people higher up on TV and watching my governor here influenced me [to become vaccinated].” (56yr AA Female) Another participant echoed this: “To some extent, it was comforting to see high-ranking political officials receive the vaccine on camera.” (Age not reported White Female) Other participants emphasized information obtained through the news, saying, “There was just so much on the news. There were so many doctors saying, take the vaccine,” (42yr old AA Female) and “I watched the news every day, and watched the doctors talk about it, and listened to them.” (56yr old AA Female)
Influential messages about the vaccine and vaccination outcomes
Participants provided descriptions of the information they found influential and persuasive in their decision to get the COVID-19 vaccine. Researchers identified three emergent subthemes: side effects (both short-term and long-term), the vaccine works and protects from known negative COVID-19 outcomes, and vaccine is safe.
Side effects (both short-term and long-term).
Participants discussed information about the more immediate side effects of the vaccine as important to their decision and described obtaining this information from direct conversations with a trusted messenger. This participant explained, “My dad had already been vaccinated, and he had no problems with the first or the second dose. I guess I felt more comfortable with hearing’ his experience.” (40yr old Hispanic Female) Another participant said, “My mom’s generation and older, the majority of them, have COVID shots, and in conversations with them, I’ve known you probably feel bad, or you feel tired.” (29yr old AA Male) The potential long-term effects of the vaccine were also mentioned when participants discussed the information they sought from trusted messengers. One participant summarized, “I was worried about long-term effects primarily, but it does not look like it’s going to have any long-term effects.” (26yr old White Female)
The vaccine works and protects from known negative COVID-19 outcomes.
Participants discussed conversations where they received information about the protection gained against negative COVID-19 outcomes from vaccination. A participant talked about her mother’s experiences:
She did not get the COVID vaccine. She got hit with COVID and was hospitalized; she was in the hospital for quite a bit. That also helped me, cause she could have got the vaccine. Then she became an advocate for it as well, and she got it and was like, “You need to get it”, so yeah. That also helped.
(28yr old AA Female)
Another participant discussed how a similar experience influenced her decision to get vaccinated: “I knew someone who got COVID before the vaccine, and I saw how that affected them. Once I learned your likelihood of dying decreases significantly once you get the vaccine I was like, I’ll go get it.” (30yr old AA Female) One participant explained:
My sister died. She caught COVID. She did not get the vaccine. She was not socially distancing. She did not take it seriously. She caught it and was hospitalized, and she was unconscious for weeks—basically, brain dead. If there was a way to minimize the possible effects of getting COVID, minimize the symptoms, or minimize possibly having to suffer through what I suffered through, and just get a vaccine.
(32yr old AA Male)
Vaccine is safe.
Participants reported information about the vaccine’s safety as influential in their decision. Participants discussed vaccine safety with trusted messengers, especially healthcare professionals. A participant stated, “I talked with my endocrinologist about it, because I didn’t know if there would be anything I should look out for with my diabetes, but there wasn’t any concern from him other than from not getting vaccinated.” (56yr old Hispanic Male) Another participant explained how knowing “that it was safe to take, there was nothing in it helped [me] know that I made the right decision [to get vaccinated].” (58yr old White Male) Another participant—a cancer patient with the potential for allergic reactions to the vaccine—said, “I needed to make sure [and] after I got the assurance that there wouldn’t be a problem, then I just went on and made the effort to have it done.” (53yr old AA Female)
Discussion
This exploratory study documented trusted sources of COVID-19 vaccine information and its influence on the decision to vaccinate among a diverse group of hesitant adopters in Arkansas. Participants discussed their hesitancy and how it related to experiencing misinformation that contributed to hesitancy about the COVID-19 vaccine. This is consistent with studies documenting the impact of misinformation on the lack of trust in the COVID-19 vaccines and related effects on vaccine uptake (Earnshaw et al., 2020; Kricorian et al., 2022; Langwerden et al., 2022; C. Latkin et al., 2021; Muric et al., 2021; Zhang et al., 2022). Participants described a lack of trust in the government response and medical professionals’ rollout of the COVID-19 vaccine that contributed to their hesitancy. This finding supports previous research demonstrating that a lack of trust in the federal government or medical research contributes to COVID-19 vaccine hesitancy (Ali et al., 2020; Bogart et al., 2021; Earnshaw et al., 2020; Zhang et al., 2022). Findings provide important insights into the persistent role of misinformation among hesitant adopters of the COVID-19 vaccine and suggest that interventions to encourage vaccine uptake must address misinformation.
Participants described trusted sources of COVID-19 vaccine information that influenced their decision to get vaccinated despite hesitancy, which included healthcare professionals, family members, friends, co-workers, community leaders, public health experts, government officials, and mainstream media. This is consistent with literature documenting high levels of trust for a wide variety of sources for COVID-19 vaccine information, which can be an important facilitator of vaccination (Kricorian et al., 2022; Langwerden et al., 2022; C. A. Latkin et al., 2021; Morales et al., 2022; Rhodes et al., 2020; Rusgis et al., 2022; Scherer et al., 2021). Findings are consistent with studies showing that a high level of trust in healthcare professionals, the CDC, and mainstream media as sources of general COVID-19 and COVID-19 vaccine information is associated with being vaccinated; in addition, these individuals are more likely to encourage others to become vaccinated (Ali et al., 2020; Bogart et al., 2021; Brauer et al., 2021; Davis et al., 2022; Fridman et al., 2020; Malik et al., 2020; McFadden et al., 2020; Scherer et al., 2021; Wade et al., 2022).
When describing how they addressed their vaccine hesitancy, participants discussed obtaining trusted information from multiple modes, such as key conversations with trusted messengers and public health communications from public influencers who supported or reinforced information shared by trusted messengers. These findings are consistent with studies documenting the influence of trusted sources of information, including healthcare providers, family members, and public officials, on the decision to get the COVID-19 vaccine (Bogart et al., 2021; Davis et al., 2022; Langwerden et al., 2022; C. A. Latkin et al., 2021; Malik et al., 2020; R. S. Purvis et al., 2021; Rhodes et al., 2020; Scherer et al., 2021). While some studies have shown a decline in trust in healthcare professionals, government public health officials, and mainstream media (Ali et al., 2020; Boyle et al., 2020a, 2020b, 2020c), our findings suggest these remain trusted sources of information and influence the decision-making process for COVID-19 vaccine hesitant adopters. This is consistent with research documenting the importance of interpersonal communication and the influence of conversation with others on the decision to get vaccinated against COVID-19 (B. AlShurman et al., 2021; Cunningham-Erves et al., 2023; Francis et al., 2022; Jiang et al., 2022; Zheng et al., 2022). An important new finding from this study is that participants discussed having multiple conversations with trusted messengers during the decision-making process. These same trusted messengers often facilitated the process of getting vaccinated for participants. This finding highlights the importance of understanding attitudes towards vaccination (e.g., hesitancy) as dynamic and vaccination behaviors as social processes involving many actors who might encourage or discourage vaccination. These findings suggest that interventions to increase COVID-19 vaccine uptake should utilize multiple communication strategies, including patient-provider discussions, peer-to-peer communication, and trusted messengers providing reliable information that is accessible to the target audience.
Participants described receiving information from trusted messengers specifically addressing vaccine side effects, safety, and efficacy as persuasive in their decision to become vaccinated. These findings are consistent with prior research documenting how concerns about vaccine side effects, safety, and factors influence the vaccine decision-making process (Berry et al., 2021; Boyle et al., 2022; Fridman et al., 2021; Kricorian et al., 2022; Morales et al., 2022). This study contributes nuanced insights by documenting the information that persuaded COVID-19 vaccine hesitant adopters to get vaccinated. It is important to understand the nuances of COVID-19 vaccine hesitancy and its implications for other recommended vaccinations, particularly routine childhood immunizations. Pediatric vaccine uptake has slowed with the COVID-19 pandemic, and vaccine hesitancy can further exacerbate vaccination disparities and result in a potential outbreak of diseases (Ellithorpe et al., 2022; Olusanya et al., 2021; Rhodes et al., 2020). Understanding what information was helpful in participants’ decisions to become vaccinated provides insights that can inform future efforts to increase vaccine uptake with multi-level vaccine education interventions.
While consistent with prior research, our findings document nuanced information about the role of trusted sources in the decision-making process among hesitant adopters. This study extends previous literature on COVID-19 vaccine hesitant adopters in several ways (Hallgren et al., 2021; Moore, Purvis, Hallgren, et al., 2022; Rachel S. Purvis et al., 2021; Don E. Willis et al., 2022). First, it provides insight into the role of misinformation and lack of trust in vaccines among hesitant adopters and expands knowledge about reasons for hesitancy. Second, study findings demonstrate that healthcare professionals, public health officials, and the mainstream media remain trusted sources of COVID-19 vaccine information. Third, our study documents that multiple modes of communication, especially conversations with trusted messengers, often facilitated vaccination. Fourth, findings emphasize the importance of providing understandable information about vaccine side effects, safety, and efficacy to persuade the hesitant to vaccinate. Finally, the study highlights the need to discuss the attitude of hesitancy and vaccination behavior as separate but related domains (Lloyd; Don E. Willis et al., 2022).
In separating vaccine hesitancy attitudes from vaccination behavior, this study also provides a potential approach to understanding vaccination as a dynamic and ongoing process. Our findings are consistent with recently published calls for new approaches to hesitancy, which engage with the complex aspects of this orientation towards vaccines (Larson, 2022; Larson et al., 2022). This study is among a handful of studies that provide a substantive analysis of vaccine hesitancy without conflating this attitude with vaccination behavior. Our results highlight pragmatic approaches for expanding our understanding of vaccination-as-process, developing targeted interventions related to the social processes of vaccination, and exploring the media ecology for individuals who became vaccinated despite hesitancy.
Strengths and limitations
The study is not without limitations. Findings may not be generalizable due to the focused and purposively recruited sample. However, our findings provide a nuanced insider perspective of trusted sources of COVID-19 vaccine information and its influence among hesitant adopters. This in-depth description is the main objective of qualitative exploration, not generalizability. The sample also reports a higher level of educational attainment than most with half of the participants reporting a bachelor’s or graduate degree. The diverse racial and ethnic sample strengthens the study, and findings can inform future research that seeks generalizability. Despite these limitations, this study documents reasons for hesitancy and the role of trusted sources of information in addressing or even overcoming hesitancy among hesitant adopters of the COVID-19 vaccine. Findings contribute important insights, which can inform future interventions to increase vaccine uptake among the hesitant.
Conclusion
The study findings document the type of information that may persuade patients to vaccinate despite their hesitancy and the multiple ways to deliver trusted information about vaccines and vaccination. Our findings make an important contribution by documenting influential conversations and information persuading hesitant individuals to vaccinate for COVID-19. Our findings expand our understanding of the role of misinformation and trust in vaccine hesitancy and show that healthcare professionals, public health officials, and mainstream media remain trusted sources of information. We also document that the role of multiple modes of communication, especially conversations with trusted messengers, often facilitated the vaccination process. Our findings also highlight the continued need for clear, understandable information about vaccine safety and efficacy to address major concerns that drive vaccine hesitancy. Finally, we demonstrate that attitudes towards vaccination are dynamic and contextual and that vaccine hesitancy often persists among those who become vaccinated, which points towards a more holistic approach to increasing vaccination as a social process.
Funding acknowledgment:
The community engagement related to this research is supported by the University of Arkansas for Medical Sciences Translational Research Institute funding awarded through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) (UL1 TR003107); Rapid Acceleration of Diagnostics (RADx) (NIH 3 R01MD013852-03S2); and Community Engagement Alliance (CEAL) Against COVID-19 Disparities (NIH 10T2HL156812-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of interest: Dr. Sheena CarlLee reports owning some Pfizer stock. All other authors declared no conflicts of interest.
References
- Ali SH, Foreman J, Tozan Y, Capasso A, Jones AM, & DiClemente RJ (2020). Trends and Predictors of COVID-19 Information Sources and Their Relationship With Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Health Surveill, 6(4), e21071. 10.2196/21071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlShurman BA, Khan AF, Mac C, Majeed M, & Butt ZA (2021). What Demographic, Social, and Contextual Factors Influence the Intention to Use COVID-19 Vaccines: A Scoping Review. Int J Environ Res Public Health, 18(17). 10.3390/ijerph18179342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archibald M, Ambagtsheer R, Casey M, & Lawless M (2019). Using Zoom Videoconferencing for Qualitative Data Collection: Perceptions and Experiences of Researchers and Participants. International Journal of Qualitative Methods, 18, 1–8. https://doi.org/doi: 10.1177/1609406919874596 [DOI] [Google Scholar]
- Balasuriya L, Santilli A, Morone J, Ainooson J, Roy B, Njoku A, … Venkatesh A (2021). COVID-19 Vaccine Acceptance and Access Among Black and Latinx Communities. JAMA Netw Open, 4(10), e2128575. 10.1001/jamanetworkopen.2021.28575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry SD, Johnson KS, Myles L, Herndon L, Montoya A, Fashaw S, & Gifford D (2021). Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J Am Geriatr Soc, 69(5), 1140–1146. 10.1111/jgs.17136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boddy C (2016). Sample size for qualitative research. Qualitative Market Research, 19(4), 426–432. https://doi.org/doi: 10.1108/QMR-06-2016-0053 [DOI] [Google Scholar]
- Bogart LM, Ojikutu BO, Tyagi K, Klein DJ, Mutchler MG, Dong L, … Kellman S (2021). COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. J Acquir Immune Defic Syndr, 86(2), 200–207. 10.1097/QAI.0000000000002570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle J, Brassell T, & Dayton J (2020a). American trust in COVID-19 information from federal and state/local government is trending downward. ICF International. https://www.icf.com/insights/health/covid-19-survey-trust-government-response-erodes [Google Scholar]
- Boyle J, Brassell T, & Dayton J (2020b). As cases increase, American trust in COVID-19 information from federal, state, and local governments continues to decline. ICF International. https://www.icf.com/insights/health/covid-19-survey-american-trust-government-june [Google Scholar]
- Boyle J, Brassell T, & Dayton J (2020c). Who do Americans trust for COVID-19 news and information? ICF International. https://www.icf.com/insights/health/covid-19-public-health-findings-mitigation [Google Scholar]
- Boyle J, Nowak G, Kinder R, Iachan R, & Dayton J (2022). Better Understanding Adult COVID-19 Vaccination Hesitancy and Refusal: The Influence of Broader Beliefs about Vaccines. Int J Environ Res Public Health, 19(11). 10.3390/ijerph19116838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauer E, Choi K, Chang J, Luo Y, Lewin B, Munoz-Plaza C, … Bruxvoort K (2021). Health Care Providers’ Trusted Sources for Information About COVID-19 Vaccines: Mixed Methods Study. JMIR Infodemiology, 1(1), e33330. 10.2196/33330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burla L, Knierim B, Barth J, Liewald K, Duetz M, & Abel T (2008). From text to codings: intercoder reliability assessment in qualitative content analysis. Nurs Res, 57(2), 113–117. 10.1097/01.NNR.0000313482.33917.7d [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021a). COVID Data Tracker. Retrieved May 31, 2021 from https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases [Google Scholar]
- Centers for Disease Control and Prevention. (2021b). Science Brief: COVID-19 Vaccines and Vaccination. Retrieved March 31, 2022 from https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html [PubMed]
- Colorafi KJ, & Evans B (2016). Qualitative Descriptive Methods in Health Science Research. HERD: Health Environments Research & Design Journal, 9(4), 16–25. 10.1177/1937586715614171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley S (1995). Health-as-process: a health visiting perspective. Journal of Advanced Nursing, 22(3), 433–441. 10.1046/j.1365-2648.1995.22030433.x [DOI] [PubMed] [Google Scholar]
- Cunningham-Erves J, George W, Stewart EC, Footman A, Davis J, Sanderson M, … Brandt HM (2023). COVID-19 Vaccination: Comparison of Attitudes, Decision-Making Processes, and Communication among Vaccinated and Unvaccinated Black Americans. Int J Environ Res Public Health, 20(4). 10.3390/ijerph20043481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TC, Beyl R, Bhuiyan MAN, Davis AB, Vanchiere JA, Wolf MS, & Arnold CL (2022). COVID-19 Concerns, Vaccine Acceptance and Trusted Sources of Information among Patients Cared for in a Safety-Net Health System. Vaccines (Basel), 10(6). 10.3390/vaccines10060928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, & Bettinger JA (2013). Vaccine Hesitancy: An Overview. Hum Vaccin & Immunother, 9(8), 1763–1773. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V, Eaton L, Kalichman S, Brousseau N, Hill E, & Fox A (2020). COVID-19 conspiracy beliefs, health behaviors, and policy support. Translational behavioral medicine, 10(4). 10.1093/tbm/ibaa090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellithorpe ME, Aladé F, Adams RB, & Nowak GJ (2022). Looking ahead: Caregivers’ COVID-19 vaccination intention for children 5 years old and younger using the health belief model. Vaccine, 40(10), 1404–1412. 10.1016/j.vaccine.2022.01.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enkel S, Attwell K, Snelling T, & Christian H (2018). ‘Hesitant compliers’: Qualitative analysis of concerned fully-vaccinating parents. Vaccine, 36(44). 10.1016/j.vaccine.2017.09.088 [DOI] [PubMed] [Google Scholar]
- Francis DB, Mason N, & Occa A (2022). Young African Americans’ Communication with Family Members About COVID-19: Impact on Vaccination Intention and Implications for Health Communication Interventions. J Racial Ethn Health Disparities, 9(4), 1550–1556. 10.1007/s40615-021-01094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman A, Gershon R, & Gneezy A (2021). COVID-19 and vaccine hesitancy: A longitudinal study. PloS one, 16(4), e0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman I, Lucas N, Henke D, & Zigler CK (2020). Association Between Public Knowledge About COVID-19, Trust in Information Sources, and Adherence to Social Distancing: Cross-Sectional Survey. JMIR Public Health Surveill, 6(3), e22060. 10.2196/22060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren E, Moore R, Purvis RS, & et al. (2021). Facilitators to Vaccination among Hesitant Adopters. Hum Vaccin & Immunother, 17(12), 5168–5175. 10.1080/21645515.2021.201042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heggdal K (2015). Patient’s experience of the outcomes of engaging in a broadly applicable health promotion intervention for individuals facing chronic illness. Health, 7(6), 765–775. 10.4236/health.2015.76091 [DOI] [Google Scholar]
- Hennink M, Hutter I, & Bailey A (2011). Qualitative Research Methods. London: Sage Publications. [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qual Health Res, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jiang X, Hwang J, Su MH, Wagner MW, & Shah D (2022). Ideology and COVID-19 Vaccination Intention: Perceptual Mediators and Communication Moderators. J Health Commun, 27(6), 416–426. 10.1080/10810730.2022.2117438 [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University of Medicine. (2022). Coronavirus Resource Center. Accessed June 6, 2023 from https://coronavirus.jhu.edu/
- Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, & Webb FJ. (2021). COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. Journal of community health, 46(2), 270–277. 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirzinger A, Sparks G, & Brodie M KFF COVID-19 Vaccine Monitor: In Their Own Words, Six Months Later. Kaiser Family Foundation. Retrieved March 31, 2022 from https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/ [Google Scholar]
- Kricorian K, Civen R, & Equils O (2022). COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother, 18(1), 1950504. 10.1080/21645515.2021.1950504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langwerden RJ, Wagner EF, Hospital MM, Morris SL, Cueto V, Carrasquillo O, … Campa AL (2022). A Latent Profile Analysis of COVID-19 Trusted Sources of Information among Racial and Ethnic Minorities in South Florida. Vaccines (Basel), 10(4). 10.3390/vaccines10040545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson HJ (2022). Defining and measuring vaccine hesitancy. Nature Human Behaviour, 6(12), 1609–1610. 10.1038/s41562-022-01484-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson HJ, Gakidou E, & Murray CJL (2022). The Vaccine-Hesitant Moment. New England Journal of Medicine, 387(1), 58–65. 10.1056/NEJMra2106441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Dayton LA, Yi G, Konstantopoulos A, Park J, Maulsby C, & Kong X (2021). COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine, 39(16), 2288–2294. 10.1016/j.vaccine.2021.02.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Dayton L, Miller JR, Yi G, Jaleel A, Nwosu CC, … Falade-Nwulia O (2021). Behavioral and Attitudinal Correlates of Trusted Sources of COVID-19 Vaccine Information in the US. Behav Sci (Basel), 11(4). 10.3390/bs11040056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd R People are getting COVID shots despite hesitation. Scientific American. Retrieved June 6, 2023 from https://www.scientificamerican.com/article/people-are-getting-covid-shots-despite-hesitation/ [Google Scholar]
- MacDonald NE, & SAGE Working Group on Vaccine Hesitancy (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. doi: 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- Malik AA, McFadden SM, Elharake J, & Omer SB (2020). Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine, 26, 100495. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAXQDA. (1989–2015). MAXQDA, software for qualitative data analysis. In VERBI Software. http://www.maxqda.com/ [Google Scholar]
- McElfish PA, Willis DE, Shah SK, Reece S, Andersen JA, Schootman M, … Warmack TS (2022). Parents’ and Guardians’ Intentions to Vaccinate Children against COVID-19. Vaccines (Basel), 10(3). 10.3390/vaccines10030361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadden SM, Malik AA, Aguolu OG, Willebrand KS, & Omer SB (2020). Perceptions of the adult US population regarding the novel coronavirus outbreak. PLoS One, 15(4), e0231808. 10.1371/journal.pone.0231808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W, & Wheeler E (2021). 2021 Rural Profile of Arkansas: Social & Economic Trends Affecting Rural Arkansas. University of Arkansas, Division of Agriculture, Research & Extension. Retrieved June 6, 2023 from https://www.uaex.edu/publications/pdf/MP564.pdf [Google Scholar]
- Moore R, Purvis RS, Hallgren E, Willis DE, Hall S, Reece S, … McElfish PA (2022a). Motivations to Vaccinate Among Hesitant Adopters of the COVID-19 Vaccine. Journal of community health, 47(2), 237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore R, Purvis RS, Willis DE, Worley KC, Hervey D, Reece S, … McElfish PA (2022b). The vaccine hesitancy continuum among hesitant adopters of the COVID-19 vaccine. Clinical and Translational Science, 15(12), 2844–2857. 10.1111/cts.13385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales GI, Lee S, Bradford A, De Camp A, & Tandoc EC (2022). Exploring vaccine hesitancy determinants during the COVID-19 pandemic: An in-depth interview study. SSM Qual Res Health, 2, 100045. 10.1016/j.ssmqr.2022.100045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse J (2000). Determining Sample Size. Qualitative Health Research, 10(1), 3. https://doi.org/doi: 10.1177/104973200129118183 [DOI] [Google Scholar]
- Muric G, Wu Y, & Ferrara E (2021). COVID-19 Vaccine Hesitancy on Social Media: Building a Public Twitter Data Set of Antivaccine Content, Vaccine Misinformation, and Conspiracies. JMIR Public Health Surveill, 7(11), e30642. 10.2196/30642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen KH, Anneser E, Toppo A, Allen JD, Scott Parott J, & Corlin L (2022). Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults ≥ 18 years, United States. Vaccine, 40(1), 107–113. 10.1016/j.vaccine.2021.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olusanya OA, Bednarczyk RA, Davis RL, & Shaban-Nejad A (2021). Addressing Parental Vaccine Hesitancy and Other Barriers to Childhood/Adolescent Vaccination Uptake During the Coronavirus (COVID-19) Pandemic. Front Immunol, 12, 663074. 10.3389/fimmu.2021.663074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purvis RS, Hallgren E, Moore RA, Willis DE, Hall S, Gurel-Headley M, & McElfish PA (2021). Trusted Sources of COVID-19 Vaccine Information among Hesitant Adopters in the United States. Vaccines, 9(12), 1418. 10.3390/vaccines9121418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purvis RS, Moore R, Willis DE, Hallgren E, & McElfish PA (2022). Factors influencing COVID-19 vaccine decision-making among hesitant adopters in the United States. Human Vaccines & Immunotherapeutics, 18(6), 2114701. 10.1080/21645515.2022.2114701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn SC, Jamison AM, An J, Hancock GR, & Freimuth VS (2019). Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine, 37(9), 1168–1173. 10.1016/j.vaccine.2019.01.033 [DOI] [PubMed] [Google Scholar]
- Rhodes ME, Sundstrom B, Ritter E, McKeever BW, & McKeever R (2020). Preparing for A COVID-19 Vaccine: A Mixed Methods Study of Vaccine Hesitant Parents. J Health Commun, 25(10), 831–837. 10.1080/10810730.2021.1871986 [DOI] [PubMed] [Google Scholar]
- Rolfe G (2006). Validity, trustworthiness and rigour: quality and the idea of qualitative research. J Adv Nurs, 53(3), 304–310. 10.1111/j.1365-2648.2006.03727.x [DOI] [PubMed] [Google Scholar]
- Rubin HJ, & Rubin IS (2005). Qualitative Interviewing: The Art of Hearing Data (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Rusgis MM, Bays JE, Abt RM, & Sperry ML (2022). Impact of COVID-19 health information sources on student vaccine hesitancy. Curr Pharm Teach Learn, 14(4), 468–475. 10.1016/j.cptl.2022.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer AM, Gedlinske AM, Parker AM, Gidengil CA, Askelson NM, Petersen CA, … Lindley MC (2021). Acceptability of Adolescent COVID-19 Vaccination Among Adolescents and Parents of Adolescents - United States, April 15–23, 2021. MMWR Morb Mortal Wkly Rep, 70(28), 997–1003. 10.15585/mmwr.mm7028e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekhar R, Sheikh A, Upadhyay S, Singh M, Kottewar S, Mir H, … Pal S (2021). COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines, 9(2). https://doi.org/ttps://doi.org/ 10.3390/vaccines9020119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speziale HJ, & Carpenter DR (2007). Qualitative Research In Nursing (4th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Szilagyi PG, Thomas K, Shah MD, Vizueta N, Cui Y, Vangala S, & Kapteyn A (2021). National Trends in the US Public’s Likelihood of Getting a COVID-19 Vaccine—April 1 to December 8, 2020. JAMA, 325(4), 396–398. 10.1001/jama.2020.26419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The White House. (2022). Statement by President Biden on FDA and CDC Authorizing Updated COVID-19 Vaccines. The White House. Retrieved June 6 ,2023 from https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/06/statement-by-president-biden-on-fda-and-cdc-authorizing-updated-covid-19-vaccines/
- Turchi GP, Orrù L, Iudici A, & Pinto E (2022). A contribution towards health. Journal of Evaluation in Clinical Practice, 28(5), 717–720. 10.1111/jep.13732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade J, Poit ST, Lee A, Ryman S, McCain D, Doss C, … Morgan AA (2022). Navigating a Pandemic: A Qualitative Study of Knowledge, Sources of Information, and COVID-19-Related Precautions Taken by HBCU Students. J Racial Ethn Health Disparities. 10.1007/s40615-021-01210-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward JK, Gauna F, Gagneux-Brunon A, Botelho-Nevers E, Cracowski J-L, Khouri C, … Peretti-Watel P (2022). The French health pass holds lessons for mandatory COVID-19 vaccination. Nature Medicine, 28(2), 232–235. 10.1038/s41591-021-01661-7 [DOI] [PubMed] [Google Scholar]
- Webb C (1999). Analysing qualitative data: computerized and other approaches. J Adv Nurs, 29(2), 323–330. [DOI] [PubMed] [Google Scholar]
- Williams AM, Clayton HB, & Singleton JA (2022). Racial and Ethnic Disparities in COVID-19 Vaccination Coverage: The Contribution of Socioeconomic and Demographic Factors. Am J Prev Med, 62(4), 473–482. 10.1016/j.amepre.2021.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, … McElfish PA (2021). COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin Transl Sci. 10.1111/cts.13077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis DE, Andersen JA, Montgomery BEE, Selig JP, Shah SK, Zaller N, … McElfish PA (2022). COVID-19 Vaccine Hesitancy and Experiences of Discrimination Among Black Adults. J Racial Ethn Health Disparities. 10.1007/s40615-022-01290-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis DE, Selig JP, Andersen JA, Hall S, Hallgren E, Williams M, … McElfish PA (2022). Hesitant but vaccinated: assessing COVID-19 vaccine hesitancy among the recently vaccinated. J Behav Med, 46(1–2), 15–24. 10.1007/s10865-021-00270-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2019). Ten threats to global health in 2019. World Health Organization. Retrieved September 23, 2020 from https://www.who.int/vietnam/news/feature-stories/detail/ten-threats-to-global-health-in-2019 [Google Scholar]
- Zhang R, Qiao S, McKeever BW, Olatosi B, & Li X (2022). Listening to Voices from African American Communities in the Southern States about COVID-19 Vaccine Information and Communication: A Qualitative Study. Vaccines (Basel), 10(7). 10.3390/vaccines10071046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Jiang S, & Wu Q (2022). Factors influencing COVID-19 vaccination intention: The roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ Couns, 105(2), 277–283. 10.1016/j.pec.2021.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]


