Abstract
Background
The efficacy of empiric calcium for patients with undifferentiated cardiac arrest has come under increased scrutiny, including a randomized controlled trial that was stopped early due to a trend towards harm with calcium administration. However, small sample sizes and non-significant findings have hindered precise effect estimates. In this analysis we evaluate the association of calcium administration with survival in a large retrospective cohort of patients with cardiac arrest treated in the emergency department (ED).
Methods
We conducted a retrospective review of medical records from two academic hospitals (one quaternary care center, one county trauma center) in San Francisco between 2011–2019. Inclusion criteria were patients aged greater than or equal to 18 years old who received treatment for cardiac arrest during their ED course. Our primary exposure was the administration of calcium while in the ED and the main outcome was survival to hospital admission. The association between calcium and survival to admission was estimated using a multivariable log-binomial regression, and also with two propensity score models.
Results
We examined 781 patients with cardiac arrest treated in San Francisco EDs between 2011–2019 and found that calcium administration was associated with decreased survival to hospital admission (RR 0.74; 95% CI 0.66 – 0.82). These findings remained significant after adjustment for patient age, sex, whether the cardiac arrest was witnessed, and including an interaction term for shockable cardiac rhythms (RR 0.60; 95% CI 0.50 – 0.72) and non-shockable cardiac rhythms (RR 0.87; 95% CI 0.76 – 0.99). Risk ratios for the association between calcium and survival to hospital admission were also similar between two propensity score-based models: nearest neighbor propensity matching model (RR 0.79; 95% CI 0.68 – 0.89) and inverse propensity weighted regression adjustment model (RR 0.75; 95% CI 0.67 – 0.84).
Conclusions
Calcium administration as part of ED-directed treatment for cardiac arrest was associated with lower survival to hospital admission. Given the lack of statistically significant outcomes from smaller, more methodologically robust evaluations on this topic, we believe these findings have an important role to serve in confirming previous results and allowing for more precise effect estimates. Our data adds to the growing body evidence against the empiric use of calcium in cardiac arrest.
Keywords: Cardiac arrest, calcium, out-of-hospital cardiac arrest, pharmacotherapy, emergency medicine
Introduction
The use of empiric calcium in undifferentiated cardiac arrest has long been a topic of scientific inquiry, with a plausible pathophysiologic argument for benefit in cardiac arrest due to calcium’s role as an inotrope, vasopressor, and important mediator of cardiac muscle contractility.1 Several early studies from the 1980s had point estimates that favored calcium administration, although the effects on return of spontaneous circulation (ROSC) did not reach statistical significance.2,3 Since then, smaller observational studies have found mixed results when assessing the effect of calcium during cardiac arrest.4–7 National resuscitation guidelines for the treatment of cardiac arrest stopped recommending the empiric use of calcium during cardiac arrest in the 1980s and 1990s, and the most recent American Heart Association guidelines from 2020 do not recommend routine calcium administration.8,9
In spite of these recommendations, calcium use during cardiac arrest has continued; in one study, the odds of patients with in-hospital cardiac arrest receiving calcium doubled from 2001 to 2016, with almost 30% of patients receiving the medication.10 A recent randomized controlled trial of calcium in out-of-hospital cardiac arrest (OHCA) that was stopped early due to a trend towards harm with calcium administration has renewed scrutiny of this practice.11 Yet, the majority of the reported findings, including this recent trial, have examined a relatively small numbers of patients.12,13 Given relatively small sample sizes and non-statistically-significant findings regarding the use of calcium in undifferentiated cardiac arrest, additional results from larger datasets may add complementary information to this discussion and inform more precise effect estimates. This is especially important given recent recommendations to avoid further interventional studies of calcium in cardiac arrest.13 In this study we sought to evaluate the association of calcium administration with survival to hospital admission in a large retrospective cohort of patients with cardiac arrest treated in the emergency department (ED).
Methods
Study Participants, Setting, and Data Collection
We conducted a nine-year retrospective database review of patients with cardiac arrest who were treated in the EDs of two Emergency Medicine residency-affiliated hospitals in San Francisco between 2011–2019. Their combined ED census was approximately 114,000 patient visits per year. We observed patients who received standard care in these two EDs, which typically consists of ED doctors and nurses; when available, respiratory therapists and/or pharmacists joined the resuscitation team. EDs are typically notified by paramedics en route with critically-ill patients, including those in cardiac, so they can prepare to provide immediate care on patient arrival to the ED. We abstracted patient medical charts from the electronic health record for all patients that were treated for cardiac arrest during their ED stay, as identified through the presence of a standardized “code narrator” in the patient chart. Additional medical records were identified using free text searches for cardiac arrest synonyms followed by manual chart review. Patient inclusion criteria were patient age greater than or equal to 18 years and receipt of treatment for active cardiac arrest during some portion of their ED course. Exclusion criteria were traumatic cause of the cardiac arrest. Patients with no instance of active cardiac arrest while in the ED were excluded (e.g., patients who obtained ROSC prior to ED arrival and did not rearrest during their ED course).
The primary exposure was the administration of calcium during the patient’s ED course, identified using the medication administration record (MAR). The exposed group received calcium and the control group did not. The primary outcome of interest was patient survival to hospital admission, as recorded in the electronic health record. Potential confounding variables were selected based on review of current literature: age, sex, initial cardiac rhythm, and whether the cardiac arrest was witnessed.13 Age, sex, and initial cardiac rhythm were abstracted directly from the electronic hearth record. Whether the cardiac arrest was witnessed or not was identified using free text searches for witnessed synonyms followed by manual chart review. This research was approved by the institutional review board at the University of California San Francisco (IRB# 21–34353).
Quantitative Analysis
We present binary data as counts and percentages, continuous data as means and standard deviations or median and interquartile range (IQR), and between-group differences as absolute risk differences (ARDs) and risk ratios (RRs) with 95% confidence intervals (CIs). Data were analyzed using log-binomial regression. While no data were available to assess for direct clinical indications for calcium administration (e.g., hypocalcemia, hyperkalemia), an interaction term was included in our log-binomial model for calcium administration and initial cardiac rhythm based on our review of current literature.10 The interaction term was included to estimate the presence of effect modification between calcium and cardiac rhythm. Planned sensitivity analyses included evaluating outcomes for patients who arrested in the ED compared to those who were transported to the ED after an OHCA.
To reduce the risk of selection bias, we generated two propensity score models: inverse probability weighted regression adjustment, and nearest neighbor propensity score matching. For the inverse probability weighted regression adjustment model, we performed a propensity score regression using the same variables as the log-binomial regression. Estimated parameters of the exposure model were used to compute inverse-probability weights, which were then used to fit weighted regression models of the exposure-specific predicted outcome for each patient. Exposure-specific predicted outcomes were compared to estimate the average exposure effect. For the nearest neighbor propensity score matching model, we generated propensity scores from a regression model using the same variables as the log-binomial regression. We then matched patients in a 1:1 fashion using a caliper matching method without replacement and a caliper width of 0.1 SD of the logit of the propensity score. The exposed and not exposed groups were comparable for included variables for both propensity score models (−0.1 < standardized mean difference < 0.1). Figure 1 shows adequate propensity score overlap. Data were analyzed using Stata software (StataCorp, version 17, 2021. College Station, TX).
Figure 1.
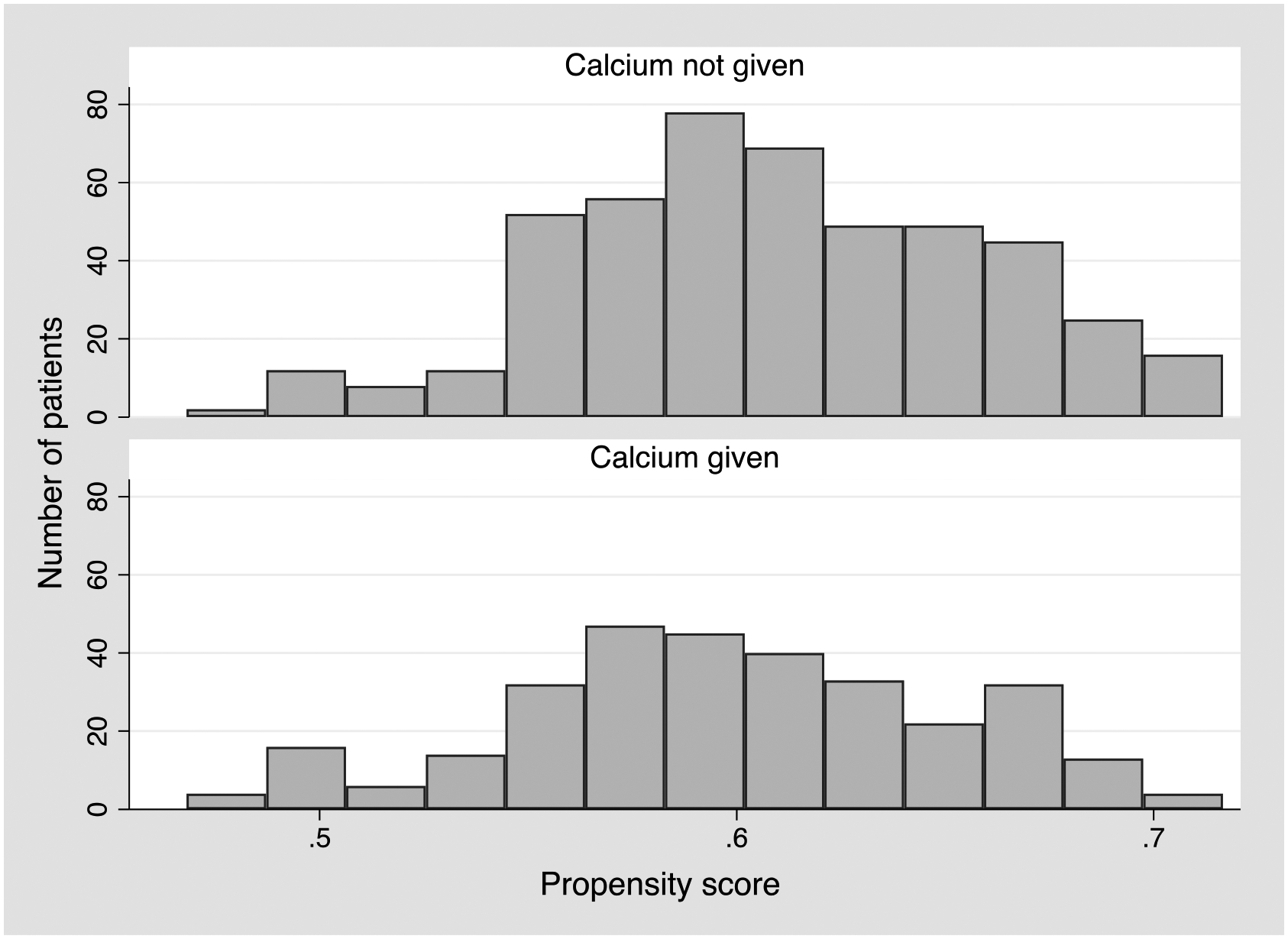
Overlap of propensity scores by exposure to calcium
Propensity scores calculated using a regression model with the following variables: age, sex, initial cardiac rhythm, and whether the cardiac arrest was witnessed.
Results
Study Participants
We identified 1,040 charts of patients potentially treated for cardiac arrest between 2011–2019 that met our inclusion criteria. After manual chart review, 232 charts were excluded for not being true cardiac arrests and 27 charts were excluded for meeting our predefined exclusion criteria (i.e. traumatic cardiac arrest). Of the 781 cardiac arrest patients treated between 2011–2019, most were male (529; 67.7%), and their median age was 65 years (IQR 52–76) (Table 1). Most cases were witnessed arrests (67.3%) and had an initial non-shockable rhythm (54.3%), and arrested prior to hospital arrival (78.8%). Of the 333 (42.6%) patients who had race and ethnicity data, 98 were White (28.2%), 84 were Asian (25.2%), 62 were Black (18.9%), and 54 were Hispanic (16.2%). Calcium was administered in 308 (39.4%) cases, with a survival rate to hospital admission of 75.5% when calcium was not given (357 patients out of 473 total) and 56.2% when calcium was given (173 patients out of 308 total; risk ratio for calcium administration 0.74, 95% confidence interval 0.66 – 0.83). We found an overall survival rate to hospital admission of 67.9% (530 patients).
Table 1.
Baseline patient and cardiac arrest characteristics
| Calcium not given N = 473 | Calcium given N = 308 | All arrests N = 781 | |
|---|---|---|---|
| Patient characteristics | |||
| Age, mean (SD), years | 62 (18) | 64 (17) | 63 (18) |
| Sex, No. (%) | |||
| Female | 144 (30.4) | 108 (35.1) | 252 (32.3) |
| Male | 329 (69.6) | 200 (64.9) | 529 (67.7) |
| Race/ethnicity, No. (%) | |||
| Asian | 58 (12.3) | 26 (8.4) | 84 (10.8) |
| Black | 39 (8.2) | 24 (7.8) | 63 (8.1) |
| Hispanic | 35 (7.4) | 19 (6.2) | 54 (6.9) |
| White | 77 (16.3) | 17 (5.5) | 94 (12.0) |
| Other | 30 (6.3) | 8 (2.6) | 38 (4.9) |
| Unknown | 234 (49.5) | 214 (69.5) | 448 (57.4) |
| Cardiac arrest characteristics, No. (%) | |||
| Witnessed status | |||
| Unwitnessed arrest | 154 (32.6) | 101 (32.8) | 255 (32.7) |
| Witnessed arrest | 319 (67.4) | 207 (67.2) | 526 (67.3) |
| Initial cardiac rhythm | |||
| Shockable rhythm | 205 (43.3) | 152 (49.4) | 357 (45.7) |
| Non-shockable rhythm | 268 (56.7) | 156 (50.7) | 424 (54.3) |
| Location of arrest | |||
| In hospital arrest | 87 (18.4) | 79 (25.7) | 166 (21.2) |
| Out of hospital arrest | 386 (81.6) | 229 (74.3) | 615 (78.8) |
SD = standard deviation, No. = number.
Regression Models
The estimated risk ratio of calcium on survival to hospital admission was 0.74 (95% CI 0.66 – 0.83) in an unadjusted regression model (Table 2). In the fully-adjusted model, the risk ratio for calcium on survival to admission was 0.60 (95% CI 0.50 – 0.72) for patients with a shockable cardiac rhythm and 0.87 (95% CI 0.76 – 0.99) for those with non-shockable rhythms. Having a witnessed cardiac arrest was associated with an increased rate of survival to hospital admission compared to unwitnessed arrests (RR 1.24; 95% CI 1.11 – 1.38), while patient age and sex were not found to be significantly associated with survival.
Table 2.
Survival to hospital admission by patient and cardiac arrest characteristics by progressively more adjusted regression model
| Unadjusted model | Adjusted for patient and arrest characteristics | Adjusted for patient and arrest characteristics with rhythm interaction | |
|---|---|---|---|
| Risk ratio (95% CI) | Risk ratio (95% CI) | Risk ratio (95% CI) | |
| Exposure | |||
| Calcium given | 0.74 (0.66 – 0.83) | 0.74 (0.66 – 0.82) | |
| Calcium given in shockable rhythm | 0.60 (0.50 – 0.72) | ||
| Calcium given in non-shockable rhythm | 0.87 (0.76 – 0.99)* | ||
| Age | 1.00 (0.99 – 1.00)** | 1.00 (0.99 – 1.00) | |
| Sex | |||
| Female | -- | -- | |
| Male | 1.04 (0.94 – 1.14) | 1.04 (0.95 – 1.15) | |
| Witnessed status | |||
| Unwitnessed arrest | -- | -- | |
| Witnessed arrest | 1.24 (1.11 – 1.38) | 1.24 (1.11 – 1.38) | |
| Initial cardiac rhythm | |||
| Shockable rhythm | -- | ||
| Not shockable rhythm | 0.99 (0.91 – 1.09) |
Risk ratios are presented as risk of survival to hospital admission for patients receiving calcium compared to those that do not receive calcium. Risk ratios greater than 1 represent a protective association for calcium and risk ratio less than 1 represent a harmful association.
upper limit of 95% CI is 0.999.
lower limit of 95% CI is 0.998. 95% CI = 95% confidence interval.
Propensity Score-Based Models
Risk ratios for the association of calcium on survival to hospital admission were similar in the adjusted regression model and the propensity score-based models (Table 3). Absolute risk differences (ARD) for the nearest neighbor propensity matching model (ARD 16.0%; 95% CI 8.2 – 23.8) and the inverse propensity weighted regression adjustment model (ARD 18.9%; 95% CI 12.2 – 25.7) were also similar to the fully adjusted regression model (ARD 19.5%; 95% CI 12.7 – 26.2). The number needed to harm when giving calcium to a cardiac arrest treated in the ED was 5.1 according to the adjusted regression model and between 5.29 – 6.25 based on the propensity score-based models. The association between calcium and survival to hospital admission was similar for patients who arrested prior to arrival in the ED and those who arrested while in the ED (Appendix 1).
Table 3.
Propensity score adjusted models of survival to hospital admission for patients given Calcium during cardiac arrest in the emergency department
| Risk ratio (95% CI) | Abs risk diff (95% CI) | |
|---|---|---|
| Fully adjusted regression model | 0.74 (0.66 – 0.82) | 19.5% (12.7 – 26.2) |
| Nearest neighbor propensity matching | 0.79 (0.68 – 0.89) | 16.0% (8.2 – 23.8) |
| Inverse propensity weighted regression adjustment | 0.75 (0.67 – 0.84) | 18.9% (12.2 – 25.7) |
Risk ratios are presented for patients receiving calcium compared to those that do not receive calcium. Risk ratios greater than 1 represent a protective association for calcium and risk ratio less than 1 represent a harmful association. Abs risk diff = absolute risk difference, 95% CI = 95% confidence interval.
Discussion
In this nine-year retrospective study of ED-treated cardiac arrest patients, the administration of calcium was associated with a significant decrease in patient survival to hospital admission. These findings remained robust after adjustment for potential confounders, and we found similar estimates using propensity score-based approaches.
Our study of 781 patients represents the largest single study of the association between calcium administration and cardiac arrest outcomes. The Messias Hirano Padrao et al. systematic review on the subject identified data from 1,846 patients from 6 non-randomized studies.13 The selection criteria for our patient population were similar to the criteria used in prior evaluations of this topic. Main differences in study populations include the geographic location of our participants, who represent an inclusive sample of patients treated in two academic hospitals in the Western United States, as well as the length of time covered in our dataset.
Our findings add to the growing body of evidence that empiric calcium administration in cardiac arrest is ineffective and may be harmful. In their systematic review of three randomized clinical trials (554 total patients), Messias Hirano Padrao et al. reported that none of these studies showed a statistically significant effect of calcium on cardiac arrest outcomes, although there was marked heterogeneity in the resulting point estimates.2,3,11,13 Our study likewise found no evidence of benefit, and did so consistently: our results were consistent in unadjusted and adjusted models, as well as in subgroups of patients presenting in both shockable and non-shockable cardiac rhythms. The largest and most recent clinical trial of calcium in cardiac arrest by Vallentin et al. found a risk ratio of 0.72 (95% CI 0.49 – 1.03) for sustained ROSC after administration of calcium,11 similar to our point estimate for survival to hospital admission after calcium administration. Notably, the Vallentin et al. study was halted early by the data and safety monitoring board given the anticipated trend towards harm with calcium administration. Our data from real-world clinical practice supports this notion of potential harm from empiric calcium administration.
There are several pathophysiologic hypotheses for why calcium may be harmful during cardiac arrest. Iatrogenically increasing calcium levels during cardiac arrest may cause cellular calcium overload and cardiac hypercontraction, often referred to as stone heart.14,15 This is thought to be secondary to a reduced transmembrane sodium gradient during ischemia causing the sodium-calcium exchange protein to operate in reverse.16 Additionally, because calcium is involved in multiple cellular signaling pathways, excessive calcium may result in increased oxidative stress and apoptosis.17,18 Interestingly, we observed a larger negative association among patients with shockable rhythms. It is unclear what drove this association; two possibilities are that people with non-shockable rhythms were more likely to have an indication for calcium or because clinicians treated people with refractory shockable rhythms with more interventions.19
These findings are important given the pervasive clinical use of calcium in treating cardiac arrest. In spite of national guidelines not including the empiric use of calcium during cardiac arrest, prior investigators have estimated that calcium is given in 20–30% of adult in-hospital cardiac arrests in the United States, or approximately 75,000 patients receiving calcium during a cardiac arrest each year.10,20 We found a similar rate of 39.4% of cardiac arrest patients who received calcium in our study population.
Limitations
Our analyses have several limitations. Our primary outcome of survival to hospital admission is an imperfect proxy compared to 30-day mortality, modified Rankin score, or other longer-term patient-centered outcome measure. However, our primary outcome is upstream from these outcomes and is easily ascertained retrospectively without risk of measurement bias.
Our data had very limited information on patient comorbidities, and there was no ability to determine what, if any, of this information was available during the course of ED care. However, the inability to control for comorbidities describes the pragmatic usage of calcium in cardiac arrest in emergency departments. The reality of caring clinically for an emergent cardiac arrest patient often means data on comorbidities is not immediately available. Our current results are directly relevant to clinicians making decisions in real time for undifferentiated patients with limited or no data available, as the data included in our models represent the data that are routinely available to a front-line provider during a patient’s initial resuscitation.
The observational nature of our study introduces the potential for biases. Our data was limited in that it did not allow us to observe the formulation or total dose of calcium administered; we do know that each patient who received calcium received at least 1 gram (either as calcium gluconate or chloride), which suggests that this medication was not under-dosed.13 Selection bias, in which calcium was given in a targeted manner for a specific clinical indication (e.g., hypocalcemia, hyperkalemia, calcium channel blocker intoxication) would likely bias the results towards finding a benefit; however a similar selection bias may occur in which patients with more comorbidities may be more likely to receive calcium. To the extent that selection bias is present in our analysis it did not outweigh the negative association between calcium and survival. Further, sicker patients might receive more treatments in general, including calcium. In addition, there could be a selection bias referred to as a “resuscitation time bias,” which postulates that an exposure is more likely to occur during a longer cardiac arrest.21 Since long resuscitation times are strongly associated with worse outcomes, this would bias our results towards harm. We were unable to directly address this bias retrospectively, however we attempted to mitigate this limitation through regression adjustment and propensity score modeling. We were unable to measure the effect of each of these biases alone or in combination, and the degree to which they influence our results is unclear.
Conclusion
Calcium administration as part of ED-directed treatment for cardiac arrest was associated with lower survival to hospital admission in our retrospective cohort. Our data adds to the growing body evidence against the empiric use of calcium in cardiac arrest.
Funding statement:
DGD was supported by National Heart Lung and Blood Institute grant R38HL143581.
Role of the Sponsors:
The sponsors had no role in the design and conduct of the study, in the collection, analysis, and interpretation of data, or in the preparation of the manuscript, review, or approval of the manuscript.
Appendix 1. Survival to hospital admission by patient and cardiac arrest characteristics by progressively more adjusted regression model, according to location of arrest
| Unadjusted model | Adjusted for patient and arrest characteristics | |
|---|---|---|
| Risk ratio (95% CI) | Risk ratio (95% CI) | |
| Out of Hospital Cardiac Arrest | ||
| Calcium given | 0.73 (0.64 – 0.83) | 0.73 (0.59 – 0.91) |
| Age | 1.00 (0.99 – 1.01) | |
| Sex | ||
| Female | -- | |
| Male | 1.01 (0.81 – 1.26) | |
| Witnessed status | ||
| Unwitnessed arrest | -- | |
| Witnessed arrest | 1.25 (1.00 – 1.56) | |
| Initial cardiac rhythm | ||
| Shockable rhythm | -- | |
| Not shockable rhythm | 1.05 (0.86 – 1.28) | |
| In Hospital Cardiac Arrest | ||
| Calcium given | 0.75 (0.63 – 0.91) | 0.75 (0.53 – 1.08) |
| Age | 1.00 (0.99 – 1.01) | |
| Sex | ||
| Female | -- | |
| Male | 0.98 (0.67 – 1.43) | |
| Witnessed status | ||
| Unwitnessed arrest | -- | |
| Witnessed arrest | 1.16 (0.80 – 1.70) | |
| Initial cardiac rhythm | ||
| Shockable rhythm | -- | |
| Not shockable rhythm | 1.04 (0.73 – 1.49) |
Risk ratios are presented as risk of survival to hospital admission for patients receiving calcium compared to those that do not receive calcium. Risk ratios greater than 1 represent a protective association for calcium and risk ratio less than 1 represent a harmful association.
Footnotes
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: The authors have no relevant financial interest in this article.
Declarations of interest: None
Bibliography
- 1.Lindqwister AL, Lampe JW, Gould JR, Kaufman CL, Moodie KL, Paradis NA. Intravenous calcium as a pressor in a swine model of hypoxic pseudo-pulseless electrical mechanical activity-a preliminary report. Intensive Care Med Exp. Sep 4 2020;8(1):50. doi: 10.1186/s40635-020-00340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stueven HA, Thompson B, Aprahamian C, Tonsfeldt DJ, Kastenson EH. The effectiveness of calcium chloride in refractory electromechanical dissociation. Ann Emerg Med. Jul 1985;14(7):626–9. doi: 10.1016/s0196-0644(85)80874-x [DOI] [PubMed] [Google Scholar]
- 3.Stueven HA, Thompson B, Aprahamian C, Tonsfeldt DJ, Kastenson EH. Lack of effectiveness of calcium chloride in refractory asystole. Ann Emerg Med. Jul 1985;14(7):630–2. doi: 10.1016/s0196-0644(85)80875-1 [DOI] [PubMed] [Google Scholar]
- 4.Gando S, Tedo I, Tujinaga H, Kubota M. Variation in serum ionized calcium on cardiopulmonary resuscitation. J Anesth. Sep 1 1988;2(2):154–60. doi: 10.1007/s0054080020154 [DOI] [PubMed] [Google Scholar]
- 5.Stiell IG, Wells GA, Hebert PC, Laupacis A, Weitzman BN. Association of drug therapy with survival in cardiac arrest: limited role of advanced cardiac life support drugs. Acad Emerg Med. Apr 1995;2(4):264–73. doi: 10.1111/j.1553-2712.1995.tb03220.x [DOI] [PubMed] [Google Scholar]
- 6.Urban P, Scheidegger D, Buchmann B, Barth D. Cardiac arrest and blood ionized calcium levels. Ann Intern Med. Jul 15 1988;109(2):110–3. doi: 10.7326/0003-4819-109-2-110 [DOI] [PubMed] [Google Scholar]
- 7.van Walraven C, Stiell IG, Wells GA, Hebert PC, Vandemheen K. Do advanced cardiac life support drugs increase resuscitation rates from in-hospital cardiac arrest? The OTAC Study Group. Ann Emerg Med. Nov 1998;32(5):544–53. doi: 10.1016/s0196-0644(98)70031-9 [DOI] [PubMed] [Google Scholar]
- 8.Levy RD, Rhoden WE, Shearer K, Varley E, Brooks NH. An audit of drug usage for in-hospital cardiopulmonary resuscitation. Eur Heart J. Dec 1992;13(12):1665–8. doi: 10.1093/oxfordjournals.eurheartj.a060122 [DOI] [PubMed] [Google Scholar]
- 9.Panchal AR, Bartos JA, Cabanas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. Oct 20 2020;142(16_suppl_2):S366–S468. doi: 10.1161/CIR.0000000000000916 [DOI] [PubMed] [Google Scholar]
- 10.Moskowitz A, Ross CE, Andersen LW, et al. Trends Over Time in Drug Administration During Adult In-Hospital Cardiac Arrest. Crit Care Med. Feb 2019;47(2):194–200. doi: 10.1097/CCM.0000000000003506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vallentin MF, Granfeldt A, Meilandt C, et al. Effect of Intravenous or Intraosseous Calcium vs Saline on Return of Spontaneous Circulation in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. Dec 14 2021;326(22):2268–2276. doi: 10.1001/jama.2021.20929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kette F, Ghuman J, Parr M. Calcium administration during cardiac arrest: a systematic review. Eur J Emerg Med. Apr 2013;20(2):72–8. doi: 10.1097/MEJ.0b013e328358e336 [DOI] [PubMed] [Google Scholar]
- 13.Messias Hirano Padrao E, Bustos B, Mahesh A, et al. Calcium use during cardiac arrest: A systematic review. Resusc Plus. Dec 2022;12:100315. doi: 10.1016/j.resplu.2022.100315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piper HM, Meuter K, Schafer C. Cellular mechanisms of ischemia-reperfusion injury. Ann Thorac Surg. Feb 2003;75(2):S644–8. doi: 10.1016/s0003-4975(02)04686-6 [DOI] [PubMed] [Google Scholar]
- 15.Lomivorotov VV, Leonova EA, Belletti A, Shmyrev VA, Landoni G. Calcium Administration During Weaning From Cardiopulmonary Bypass: A Narrative Literature Review. J Cardiothorac Vasc Anesth. Jan 2020;34(1):235–244. doi: 10.1053/j.jvca.2019.06.016 [DOI] [PubMed] [Google Scholar]
- 16.Allen DG, Cairns SP, Turvey SE, Lee JA. Intracellular calcium and myocardial function during ischemia. Adv Exp Med Biol. 1993;346:19–29. doi: 10.1007/978-1-4615-2946-0_3 [DOI] [PubMed] [Google Scholar]
- 17.Clapham DE. Calcium signaling. Cell. Dec 14 2007;131(6):1047–58. doi: 10.1016/j.cell.2007.11.028 [DOI] [PubMed] [Google Scholar]
- 18.Cerella C, Diederich M, Ghibelli L. The dual role of calcium as messenger and stressor in cell damage, death, and survival. Int J Cell Biol. 2010;2010:546163. doi: 10.1155/2010/546163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim YM, Park JE, Hwang SY, et al. Association between wide QRS pulseless electrical activity and hyperkalemia in cardiac arrest patients. Am J Emerg Med. Jul 2021;45:86–91. doi: 10.1016/j.ajem.2021.02.024 [DOI] [PubMed] [Google Scholar]
- 20.Holmberg MJ, Ross CE, Fitzmaurice GM, et al. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ Cardiovasc Qual Outcomes. Jul 9 2019;12(7):e005580. [PMC free article] [PubMed] [Google Scholar]
- 21.Andersen LW, Grossestreuer AV, Donnino MW. “Resuscitation time bias”-A unique challenge for observational cardiac arrest research. Resuscitation. Apr 2018;125:79–82. doi: 10.1016/j.resuscitation.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]


