Abstract
This article aims to present the results of a national, cross-sectional, voluntary, online survey on the presence and roles of associations of breast cancer patients and volunteers in Italian specialist breast centres. The survey was developed according to standard methods. The questionnaire was pre-tested by a random sample of three breast centres, loaded onto the SurveyMonkey platform, and piloted by one volunteer breast centre. The breast centre clinical leads were invited to participate via email. A link to the online instrument was provided. No financial incentives were offered. The results were reported using standard descriptive statistics. The response rate was 82/128 (65%). Members of associations were routinely present in 70% Italian breast centres. Breast centres most often reporting their presence were those certified by the European Society of Breast Cancer Specialists. Patient support (reception and information, listening, identification of needs, and psychological support) was the primary area where associations were reported to offer services. The magnitude of this phenomenon warrants a study to investigate the impact of the activities of associations on the quality of life of patients and on the cost–benefit ratio of the service, and the modes of their interactions with the nursing staff and the medical staff.
Keywords: breast cancer, breast centre, associations, patients, volunteers, survey
1. Introduction
The most important study conducted so far on the role of associations of cancer patients and volunteers (hereafter briefly referred to as “associations”) in health systems, particularly in patient care and support, showed a great deal of diversity of national models [1]. This derives from differences in organisation and governance of national and local health systems coupled with an even more pronounced heterogeneity of health legislation, which encompasses a variety of laws, regulations, directives and other legislative instruments.
As a consequence, the activities undertaken by associations have evolved along many different directions. First, more and more emphasis is currently being placed on the shared decision-making process, in which clinicians and cancer patients collaborate to make shared medical decisions based both on clinical evidence and patient values and preferences [2]. As a parallel phenomenon, associations have increasingly exerted an influence in important areas like health and research ethics, guideline development and implementation [3], research agenda-setting processes, health policy processes, cancer education and awareness programmes [4], and general cancer care strategies. This trend is expected to be boosted by scientific advances, especially by the introduction of new and diversified options to diagnose, characterise, and treat the disease [5].
Second, many associations—especially in Europe—promote group activities for patients, including, for example, physical activities and provision of information to newly diagnosed patients. For these patients, receiving cancer-related information and support may positively affect treatment adherence, psychological well-being, and quality of life [5,6,7], because involvement in an association represents a valuable means to fulfil many disease-related needs.
Third, associations have gained increasing consideration by health and medical research stakeholders, because they can have a function in several research activities, including, for example, conducting clinical trials [8] and quality-of-life studies, especially of long-term survivors. Some of the most common cancers are poorly—or not at all—represented in this type of literature, and long-term survivors are particularly underrepresented [9]. Associations can provide crucial assistance in identifying and contacting the potential target populations of patients [10,11].
In spite of these multifaceted and important functions, a recent systematic review of the medical literature showed that only 18 studies worldwide—for all cancer sites—have formally addressed the type of initiatives undertaken by associations and other similar organisations, the type of care they offer, and the type of evaluation of the related outcomes [12]. There were major differences between associations with respect to the selection of persons. Interestingly, a personal history of cancer was an inclusion criterion in certain instances and an exclusion criterion in others. Differences also existed as to the training programmes (presence/absence, duration, type, and inclusion/exclusion of medical and emotional aspects) and the type of care and support being offered. The evaluation of outcomes was generally poor. Although patients had positive experiences according to all studies, the experiences of volunteers and of health staff members were evaluated much less frequently and with less favourable results. Very importantly, one-third of volunteer cancer patients interviewed in one study reported that the service brought up distressing thoughts about their own cancer experience.
In Italy, an in-depth analysis of the outcomes of associations’ activities is particularly warranted in one specific setting—that of specialist breast centres. A breast centre (also referred to as a breast unit) is defined as the place that provides all breast care services on a multidisciplinary basis, including genetics and prevention, primary treatment, care of advanced disease, supportive and palliative care, and survivorship care [13,14]. In the last 20 years and longer, strong evidence has been collected that patients treated by specialist teams in these centres have a survival advantage [15]. In 2014, the Italian Ministry of Health issued a directive [16] to the Departments of Health of the regional administrations (responsible for healthcare delivery) requiring the creation of a regional network of breast centres in line with the technical criteria established by the European Society of Breast Cancer Specialists (EUSOMA) [13,14]. The directive gave associations an official role and recommended that they provide well-defined types of support, including patient information on access modalities, identification and advocacy of patient needs, assessment of patient satisfaction, provision of support to manage the illness and to engage in rehabilitation programmes, collaboration with the staff in order to ensure equity of access to services, and participation in healthcare quality assessment initiatives. It must be considered that, in Italy, the members of associations include both persons with a personal history of cancer and unaffected volunteers, with the former being the majority.
Subsequently, the presence of one or more associations was included as a recommendation in the EUSOMA requirements and in the certification of Italian breast centres through BCCert [17], that is, the certification scheme of the EUSOMA.
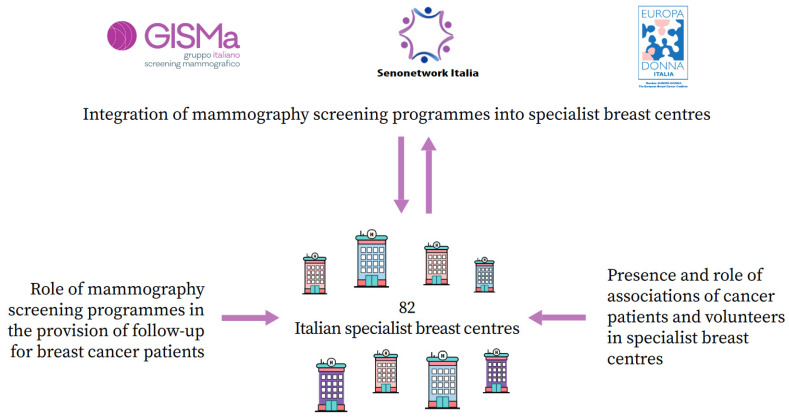
The Italian Group for Mammography Screening (GISMa), Senonetwork, and Europa Donna Italia carried out a national, cross-sectional, voluntary, online survey of Italian specialist breast centres [18,19]. Figure 1 depicts the three-section design of the protocol. The primary objective was to assess the degree of integration of mammography screening programmes into breast centres. One of the secondary objectives was to quantify the presence and assess the role(s) of associations in breast centres. In this article, the survey findings about this topic are briefly presented and discussed.
Figure 1.
Scheme depicting the three-section design of the national, cross-sectional, voluntary, online survey of Italian specialist breast centres associated with Senonetwork, 2020. The primary objective of the survey was to investigate the integration of mammography screening programmes into breast centres [18]. The secondary objectives were (1) to assess the role of mammography screening programmes in the provision of follow-up for breast cancer patients [19] and (2) to quantify the presence and assess the role of associations of cancer patients and volunteers in breast centres (present study). Of the 128 breast centres associated with Senonetwork in 2020, 82 responded to the survey.
2. Materials and Methods
2.1. Survey Development
The survey was developed and implemented according to standard guidelines [20]. The questionnaire addressed appropriate themes proposed by the main national stakeholders. Consideration was given to the relevant national legislation and to the EUSOMA requirements for breast centres [13,14]. The final version of the questionnaire consisted of 73 questions grouped under five domains: (i) breast centre identification and main characteristics, including, among others, the certification according to the EUSOMA standards [17] (questions 1–16); (ii) the breast centre clinical lead’s perception of utility, effort required, acceptability, and facilitating conditions of the integration of the screening programme into the breast centre (17–34); (iii) breast centre’s screening mammogram volume and relationship with the screening programme (35–48); (iv) dimension of integration: organizational (49–51), functional (52–58), service-related (59–64), and clinical (65); and (v) structural and functional details of the integration (65–73).
Four questions concerned the presence and role of associations in breast centres. They were developed by taking into account the 2014 directive from the Ministry of Health. In the directive, the types of support expected from associations were grouped into six major areas: (1) patient reception and information, (2) patient listening and identification of patient needs, (3) psychological support, (4) participation in assessment of the quality of services, (5) participation in fundraising initiatives, and (6) other, including support to engage in rehabilitation programmes, diet sessions, and health groups.
2.2. Survey Pre-Testing and Piloting
The questionnaire was pre-tested by a random sample of three breast centres. After collecting their feedback, unclearly worded, ambiguous, and misleading questions were modified. The survey was then loaded onto the SurveyMonkey platform (https://it.surveymonkey.com/, accessed on 31 August 2023) and piloted by one volunteer breast centre. A PDF version of the questionnaire (in Italian) is available on the website of the GISMa [21]. Further details can be found in two previously published articles [18,19].
2.3. Survey Process
At the time the survey was conducted, an official national list of breast centres was not available because their creation was still incomplete in some administrative regions. As a consequence, the survey was presented to breast centres associated with Senonetwork, the Italian network of breast cancer services, which is nationally recognised as a representative professional body for breast specialists. The clinical leads of these centres, or the main contact persons, were invited to participate via email. A link to the online instrument was provided. No financial incentives were offered. The survey was conducted between July and October 2020. The emergency caused by the COVID-19 pandemic, particularly severe in breast care services, led to a delay both in the roll-out of the initiative and in the analysis of questionnaire responses.
2.4. Data Analysis
In the present article, the results are reported using standard descriptive statistics, that is, frequencies, proportions, medians, ranges, and interquartile ranges (IR).
3. Results
3.1. Characteristics of Participating Breast Centres
Of the 128 breast centres associated with Senonetwork on 1 July 2020, 82 (65%) responded to the survey. The response rate was higher in northern Italy (53/74 or 72%) than in central–southern Italy (29/54 or 54%). The responding centres had a median of 345 (IR, 250–484) new breast cancer cases per year, and all but one (99%) reported > 150 cases per year. The median number of staff in the multidisciplinary team was 21 (IR, 14–30). The reported median number of mammograms per year was 15,000 (IR, 9000–24,750). Twenty-four (29%) breast centres were EUSOMA-certified through the BCCert scheme. Sixty-one (74%) were formally appointed as breast centres by the regional administrations’ bodies. All of the centres surveyed responded to all questions concerning the presence and role of associations.
3.2. Presence and Roles of Associations in Breast Centres
According to the 82 questionnaires filled out, members of one or more associations were routinely present and active in 57 (70%) Italian breast centres. No difference whatsoever in this regard was observed in relation to the size of the centre, as defined on the basis of the number of new breast cancer cases seen per year or the number of health professionals on the multidisciplinary team. The proportion was greater in the north of the country (41/53 or 77%) than in central (10/19 or 53%) and southern Italy (6/10 or 60%).
The subgroups of breast centres most often reporting the presence of associations were those certified through the BCCert scheme (20/24 or 83% versus 37/58 or 64%) and particularly those appointed by a regional administration (54/61 or 88% versus 3/21 or 14%). An official administrative designation as a part of the regional network of breast centres predicted the presence of an association with a considerable degree of sensitivity and specificity.
Table 1 shows the proportion of breast centres where associations had a permanent and active role, by breast centre characteristic and type of support offered. Patient support, that is, reception and information, listening, identification of needs, and psychological support, was the primary area where associations were reported to offer services. In approximately 50% of breast centres, associations were involved in the provision of all of these services. Less often did they participate in healthcare quality assessment initiatives or in providing support to engage in rehabilitation programmes. Interestingly, the participation in fundraising initiatives was as common as patient support initiatives.
Table 1.
Number and (in parentheses) percentage proportion of Italian specialist breast centres where associations of breast cancer patients and volunteers have a permanent and active role, by breast centre characteristic and type of support offered.
| Breast Centre Characteristic | Type of Support | Total | |||||
|---|---|---|---|---|---|---|---|
| Patient Reception and Information |
Patient Listening, Identification of Needs |
Psychological Support |
Assessment of Quality of Services | Participation in Fundraising Initiatives |
Other * | ||
| Total | 42 (51) | 35 (43) | 43 (52) | 15 (18) | 39 (48) | 4 (5) | 82 |
| Geographic area | |||||||
| North | 30 (57) | 24 (45) | 32 (60) | 12 (23) | 27 (51) | 3 (6) | 53 |
| Centre | 7 (37) | 7 (37) | 6 (32) | 1 (5) | 9 (47) | 1 (5) | 19 |
| South | 5 (50) | 4 (40) | 5 (50) | 2 (20) | 3 (30) | 0 (0) | 10 |
| No. of new breast cancer cases per year | |||||||
| <345 | 19 (46) | 16 (39) | 20 (49) | 6 (15) | 21 (51) | 2 (5) | 41 |
| ≥345 | 23 (56) | 19 (46) | 23 (56) | 9 (22) | 18 (44) | 2 (5) | 41 |
| No. of staff on the multidisciplinary team | |||||||
| <21 | 18 (44) | 18 (44) | 21 (51) | 6 (15) | 22 (54) | 3 (7) | 41 |
| ≥21 | 24 (59) | 17 (41) | 22 (54) | 9 (22) | 17 (41) | 1 (2) | 41 |
| BCCert certification | |||||||
| No | 27 (47) | 20 (34) | 29 (50) | 11 (19) | 25 (43) | 3 (5) | 58 |
| Yes | 15 (63) | 15 (63) | 14 (58) | 4 (17) | 14 (58) | 1 (4) | 24 |
| Regional appointment † | |||||||
| No | 2 (10) | 0 (0) | 2 (10) | 0 (0) | 2 (10) | 0 (0) | 21 |
| Yes | 40 (66) | 35 (57) | 41 (67) | 15 (25) | 37 (61) | 4 (7) | 61 |
| Hospital classification | |||||||
| Public hospital | 24 (46) | 22 (42) | 24 (46) | 8 (15) | 29 (56) | 4 (8) | 52 |
| Private accredited hospital | 2 (40) | 2 (40) | 4 (80) | 1 (20) | 3 (60) | 0 (0) | 5 |
| IRCCS and AOU | 8 (57) | 4 (29) | 8 (57) | 4 (29) | 3 (21) | 0 (0) | 14 |
| Private accredited IRCCS | 8 (73) | 7 (64) | 7 (64) | 2 (18) | 4 (36) | 0 (0) | 11 |
BCCert, European Society of Breast Cancer Specialists Breast Centre Certification; IRCCS, Istituto di Ricovero e Cura a Carattere Scientifico (non-university research hospital); AOU, Azienda Ospedaliero-Universitaria (university hospital). * Mainly including patient support to engage in rehabilitation programmes, diet sessions, and health groups. † In Italy, only breast centres receiving an official appointment by the Departments of Health of the regional administrations, which are largely responsible for healthcare provision in the country, become part of the regional network of breast centres.
4. Discussion
4.1. Main Findings
With a response rate of about two-thirds, this survey provided sound evidence that members of the associations are routinely active in 70% of Italian breast centres and that breast centres most often reporting their presence are those that are EUSOMA-certified through the BCCert scheme and particularly those officially appointed by a regional administration. Patient reception and information, listening, identification of needs, and psychological support are the main areas of commitment of associations.
4.2. Main Comments
The magnitude of engagement of cancer patients and volunteers in favour of women attending the Italian breast centres has probably become much larger than perceived by healthcare professionals and providers. In our opinion, this can be explained by the absence of previous comparable statistics and, possibly, by a general tendency to underestimate the level of commitment of the associations.
We believe that the large presence of officially appointed associations in breast centres and their very frequent engagement in key patient support services indicate the need to conduct a study to determine the qualitative impact of this work. There are two types of endpoints that would be important to measure. First, and most important, it is necessary to formally assess whether and to what extent the efforts made by the associations are capable of improving the quality of life of patients and optimising the cost–benefit ratio of the service. According to Europa Donna Italia, these should be the main objectives of the associations [22]. Ethical and acceptability issues can be overcome using a propensity score model in an observational comparative effectiveness study, with the objective of reducing confounding by covariates that are associated both with the outcome and with the exposure. Propensity score models are increasingly used for observational comparative studies in the area of health services research [23].
Second, other important issues that would need to be better understood are the types and modes of the interactions between the associations and the medical and nursing staff. This is a vital necessity, considering that patient information and support remain the primary areas where associations offer services.
Third, it has also been suggested that the personal experiences of cancer patients and their contact with members of associations should be thoroughly explored [24].
A different but equally interesting aspect to explore is why Italian breast cancer patients and volunteers engage less frequently, on average, in activities that are not directly related to patient support services, such as, for example, interaction with the breast centre staff, in order to ensure equity of access, and participation in healthcare quality evaluation initiatives (both recommended by the 2014 directive of the Italian Ministry of Health) [16]. There is, however, a notable exception: the participation in fundraising initiatives, which was reported almost as frequently as patient support activities. Considering the budget constraints affecting the health system, this interesting finding merits further investigation.
4.3. Methodological Considerations
The conduct of the survey was satisfactory both from a technical and a theoretical point of view. Firstly, the SurveyMonkey platform fit well for the purpose and enabled the questionnaire to be created, the responses to be edited and collected, and the results to be analysed in a practical way. Secondly, the highly multidisciplinary composition of the working group allowed us to approach and solve the different issues concerning the development and the management of the survey.
The results of this study must be seen in light of the fact that the representativeness of participating centres is difficult to establish with certainty. When the survey was developed, an official national list of Italian breast centres was not available. We targeted the pool of centres associated with Senonetwork, 128 on 1 July 2020, which represents an acceptable approximation. In this way, we were able to make a reasonable estimate of the response rate. The figure we obtained, 65%, allowed us to rule out a substantial nonresponse bias. Although it is true that participation was lower in central–southern Italy, this simply reflects the fact that the prevalence of active local screening programmes is lower in the south of the country, with approximately 27% of 50–69-year-old women being regularly screened versus 52% in central Italy and 62% in northern Italy [25]. This inevitably caused a lower interest in a survey that addressed primarily the integration between the breast centres and the screening programmes [18]. In any case, the geographic difference in the survey participation rate was not substantial. As a final remark, it should be noted that the number of new breast cancer cases per year was above 150 (minimum acceptable standard according to the EUSOMA criteria) in all of the participating centres except one, which does not reflect a self-selection bias but, rather, an increasing and favourable trend that is ongoing [26].
5. Conclusions
This study showed, first, that members of one or more associations of cancer patients and volunteers are routinely present and active in as many as 70% of Italian breast centres and, second, that patient information and support are the main areas where associations offer services. The magnitude of engagement of cancer patients and volunteers in favour of Italian breast centres is probably much larger than perceived by healthcare professionals and providers. Our conclusion is that the impact of this effort on the quality of life of patients and the interactions with the nursing staff and the medical staff need to be formally investigated with an observational comparative effectiveness study.
Acknowledgments
The authors thank Tiziana Tarasco (A.P.S. Senonetwork Italia, Firenze, Italy) for the secretariat support, Maurizio Bersani (ATS della Città Metropolitana di Milano, Milano, Italy) for his valuable input on the design of the project, and the following Senonetwork associates (in parentheses, the name of the institution or breast centre of affiliation) for responding to the survey: Francesco Abbonante (Azienda Ospedaliera Pugliese Ciaccio, Catanzaro), Luciana Ambrosiani (Ospedale Valduce, Como), Catia Angiolini (Breast Unit, Azienda Ospedaliero-Universitaria Careggi, Firenze), Giovanni Angiolucci (Ospedale San Donato, Arezzo), Bettina Ballardini (Multimedica S.p.A, Milano), Maggiorino Barbero (Ospedale Cardinal Massaia, Asti), Anna Bassini (Ospedale di Pordenone, Pordenone), Claudio Battaglia (Ospedale Civile, Sanremo), Rossana Berardi (Azienda Ospedaliera Ospedali Riuniti, Ancona), Laura Biganzoli (Ospedale Santo Stefano, Prato), Nicoletta Biglia (Ospedale Mauriziano Umberto I, Torino), Giancarlo Bisagni (IRCCS Azienda Ospedaliera Santa Maria Nuova, Reggio Emilia), Andrea Bonetti (AULSS 9 Scaligera, Legnago), Marina Bortul (Ospedale di Cattinara, Trieste), Massimo Busani (Azienda Ospedaliera Carlo Poma, Mantova), Carlo Cabula (Ospedale Oncologico Regionale Armando Businco, Cagliari), Claudio Caponi (Ospedale San Giuseppe, Empoli), Luciano Carli (Ospedale Città di Castello, Città di Castello), Francesco Caruso (Humanitas Istituto Clinico Catanese, Catania), Donato Casella (UOC Chirurgia Oncologica della Mammella, Policlinico Santa Maria alle Scotte, Siena), Francesca Catalano (Azienda Ospedaliera Cannizzaro, Catania), Luigi Ciuffreda (IRRCS Casa Sollievo della Sofferenza, San Giovanni Rotondo), Fabio Corsi (Fondazione Salvatore Maugeri, Pavia), Corrado De Sanctis (Breast Unit, Città della Salute e della Scienza, Torino), Franca Delle Fratte (Ospedale Sandro Pertini e Ospedale Sant’Eugenio, Roma), Biancamaria Di Marco (ASST Ovest Milanese, Milano), Fabio Falcini (Centro di Senologia Multidisciplinare, AUSL Romagna, Forlì), Antonella Ferro (Ospedale Santa Chiara, Trento), Secondo Folli (Istituto Nazionale Tumori, Milano), Francesca Fornasa (Ospedale di Marzana, Verona), Antonio Frassoldati (Arcispedale Sant’Anna, Cona, Ferrara), Vittorio Fregoni (ASST Valtellina, Sondrio), Nicoletta Gandolfo (Dipartimento delle Immagini, Ospedale Villa Scassi, Genova), Ornella Garrone (Azienda Ospedaliera Santa Croce a Carle, Cuneo), Daniele Generali (ASST Cremona, Cremona), Giuliana Gentile (Presidio Ospedaliero di San Daniele e Tolmezzo, Tolmezzo), Monica Giordano (ASST Lariana, Como), Riccardo Giovanazzi (Ospedale San Gerardo, Monza), Massimo Maria Grassi (Humanitas Gavazzeni, Bergamo), Simona Grossi (Ospedale Gaetano Bernabeo, Ortona), Alessandra Huscher (Fondazione Poliambulanza, Brescia), Gianfranco Lolli (Ospedale San Giovanni Battista, Foligno), Carla Magni (ASST Lecco, Lecco), Francesca Martella (Ospedale Santa Maria Annunziata, Bagno a Ripoli), Samuele Massarut (Centro di Riferimento Oncologico, Aviano), Alberto Massocco (IRCCS Sacro Cuore Don Calabria, Negrar), Tiziana Mastropietro (Azienda Ospedaliera San Giovanni-Addolorata, Roma), Graziano Meneghini (UOC Breast Unit Berica, AULSS 8, Montecchio Maggiore), Lorenzo Menghini (Breast Unit di Rimini, Rimini), Francesco Millo (SOS Senologia, Presidio Ospedaliero di Tortona, Tortona), Maria Alessandra Mirri (Centro di Senologia Integrato San Filippo Neri-Santo Spirito, Roma), Guido Mondini (Breast Unit Ovidio Paino, ASL TO4, Torino), Stefania Montemezzi (Azienda Ospedaliero-Universitaria Integrata, Verona), Marco Moschetta (Azienda Ospedaliero-Universitaria Consorziale Policlinico, Bari), Antonio Musolino (Azienda Ospedaliero-Universitaria, Parma), Dante Palli (Ospedale Guglielmo Da Saliceto, Piacenza), Guido Papaccio (AULSS 3 Serenissima, Chioggia), Matteo Passamonti (Azienda Ospedaliera della Provincia di Lodi, Lodi), Mariagrazia Pieraccini (Ospedale della Misericordia, Grosseto), Francesca Pietribiasi (Ospedale Santa Croce, Moncalieri), Laura Pizzorno (Ospedale San Salvatore, L’Aquila), Romano Polato (Ospedale di Bolzano, Bolzano), Riccardo Ponzone (FPO IRCCS Istituto di Candiolo, Torino), Paolo Pramaggiore (Nuovo Ospedale degli Infermi, Biella), Maurizio Ressa (IRCCS Istituto Tumori Giovanni Paolo II, Bari), Fabio Ricci (Ospedale Santa Maria Goretti, Latina), Manuela Roncella (Ospedale Santa Chiara, Pisa), Francesca Rovera (Ospedale di Circolo, Varese), Antonio Rulli (Azienda Ospedaliera, Perugia), Gianni Saguatti (Ospedale Bellaria, Bologna), Alessandro Sanguinetti (Azienda Ospedaliera Santa Maria, Terni), Maria Sciamannini (Ospedale San Jacopo, Pistoia), Maria Silvia Sfondrini (Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milano), Adele Sgarella (Breast Unit Fondazione IRCCs Policlinico San Matteo, Pavia), Edda Simoncini (Azienda Spedali Civili Brescia/SSVD, Brescia), Pietra Stancampiano (Breast Unit Interaziendale, ASL VCO-ASL NO, Novara), Francesca Svegliati (AO San Camillo-Forlanini, Roma), Mario Taffurelli (Policlinico Sant’Orsola-Malpighi, Bologna), Giovanni Tazzioli (Breast Unit Policlinico, Modena), Corrado Tinterri (Humanitas Cancer Center, Rozzano), Paolo Veronesi (Istituto Europeo di Oncologia, Milano) and Eugenio Zanon (Ospedale Cottolengo, Torino).
Author Contributions
Conceptualization, R.D., S.D., F.F., L.B., I.M., C.N., E.P., M.V. and L.C.; investigation, R.D., E.S., L.P., C.A., M.B., F.C., L.F., L.G., M.G., P.M., G.M., G.S. and C.T.; data analysis, F.F. and L.B.; writing—original draft, L.B.; supervision, S.D. and L.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee at the Romagna Cancer Institute, IRCCS Istituto Romagnolo per lo Studio dei Tumori (IRST) Dino Amadori, Meldola, Forlì, Italy (ID: IRST100.37).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this article are available from the authors on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Souliotis K., Peppou L.E., Tzavara C., Agapidaki E., Varvaras D., Buonomo O., Debiais D., Hasurdjiev S., Sarkozy F. Cancer patients’ organisation participation in heath policy decision-making: A snapshot/cluster analysis of the EU-28 countries. BMJ Open. 2018;8:e018896. doi: 10.1136/bmjopen-2017-018896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong K.A., Metlay J.P. Annals clinical decision making: Communicating risk and engaging patients in shared decision making. Ann. Intern. Med. 2020;172:688–692. doi: 10.7326/M19-3495. [DOI] [PubMed] [Google Scholar]
- 3.Björkqvist J., Giles R.H., Cornford P., Makaroff L.E., Van Hemelrijck M., Darraugh J., Cowl J., MacLennan S., MacLennan S.J. Providing a framework for meaningful patient involvement in clinical practice guideline development and implementation. Eur. Urol. Focus. 2021;7:947–950. doi: 10.1016/j.euf.2021.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Gonzalez P., Schwartz E.L. Maximize Life Global Cancer Awareness Campaign: Improving the lives of cancer patients while increasing global awareness of their needs. Stud. Health Technol. Inform. 2012;172:27–32. [PubMed] [Google Scholar]
- 5.Carlsson C., Bendahl P.O., Nilsson K., Nilbert M. Benefits from membership in cancer patient associations: Relations to gender and involvement. Acta Oncol. 2006;45:559–563. doi: 10.1080/02841860600724419. [DOI] [PubMed] [Google Scholar]
- 6.Bunston T., Mings D. Identifying the psychosocial needs of individuals with cancer. Can. J. Nurs. Res. 1995;27:59–79. [PubMed] [Google Scholar]
- 7.Tamburini M., Gangeri L., Brunelli C., Beltrami E., Boeri P., Borreani C., Fusco Karmann C., Greco M., Miccinesi G., Murru L., et al. Assessment of hospitalised cancer patients’ needs by the Needs Evaluation Questionnaire. Ann. Oncol. 2000;11:31–37. doi: 10.1023/A:1008396930832. [DOI] [PubMed] [Google Scholar]
- 8.Franchina V., Cagnazzo C., Di Costanzo A., Arizio F., Frazzetto A.M.E., Gori S., Cenna R., Nicolis F., Procopio G., Adamo V., et al. Patient associations and clinical oncology research: How much does a patient’s voice really matter? Expert Rev. Pharmacoecon. Outcomes Res. 2021;21:433–440. doi: 10.1080/14737167.2021.1850274. [DOI] [PubMed] [Google Scholar]
- 9.Gotay C.C., Muraoka M.Y. Quality of life in long-term survivors of adult-onset cancers. J. Natl. Cancer Inst. 1998;90:656–667. doi: 10.1093/jnci/90.9.656. [DOI] [PubMed] [Google Scholar]
- 10.Fransson P. Quality of life for members of Swedish prostate cancer patient associations. Cancer Nurs. 2008;31:23–31. doi: 10.1097/01.NCC.0000305671.60469.c9. [DOI] [PubMed] [Google Scholar]
- 11.Fosså S.D., Dahl A.A. Global quality of life after curative treatment for prostate cancer: What matters? A study among members of the Norwegian Prostate Cancer Patient Association. Clin. Genitourin. Cancer. 2015;13:518–524. doi: 10.1016/j.clgc.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Driessen H.P.A., Kranenburg L.W., van der Rijt K.C.D., Bakker E.M., van Busschbach J.J., Jabbarian L.J., Bramer W.M., Elfrink E.J. Evaluation of centers for information and support combining formal and informal care for patients with cancer: A systematic review of the literature. Support. Care Cancer. 2022;30:7079–7098. doi: 10.1007/s00520-022-07047-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson A.R., Marotti L., Bianchi S., Biganzoli L., Claassen S., Decker T., Frigerio A., Goldhirsch A., Gustafsson E.G., Mansel R.E., et al. The requirements of a specialist Breast Centre. Eur. J. Cancer. 2013;49:3579–3587. doi: 10.1016/j.ejca.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Biganzoli L., Cardoso F., Beishon M., Cameron D., Cataliotti L., Coles C.E., Delgado Bolton R.C., Trill M.D., Erdem S., Fjell M., et al. The requirements of a specialist breast centre. Breast. 2020;51:65–84. doi: 10.1016/j.breast.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gillis C.R., Hole D.J. Survival outcome of care by specialist surgeons in breast cancer: A study of 3786 patients in the west of Scotland. BMJ. 1996;312:145–148. doi: 10.1136/bmj.312.7024.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conferenza Stato-Regioni Linee di Indirizzo Sulle Modalità Organizzative ed Assistenziali della Rete dei Centri di Senologia. 2014. [(accessed on 7 July 2023)]. Available online: https://www.osservatorionazionalescreening.it/sites/default/files/allegati/DOC_045999_185%20%20CSR%20PUNTO%204.pdf.
- 17.Breast Centres Certification. 2023. [(accessed on 7 July 2023)]. Available online: https://www.breastcentrescertification.com/
- 18.Deandrea S., Ferrè F., D’Antona R., Angiolini C., Bortul M., Bucchi L., Caumo F., Fortunato L., Giordano L., Giordano M., et al. Integrating mammography screening programmes into specialist breast centres in Italy: Insights from a national survey of Senonetwork breast centres. BMC Health Serv. Res. 2022;22:723. doi: 10.1186/s12913-022-08111-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deandrea S., Sardanelli F., Calabrese M., Ferré F., Vainieri M., Sestini E., Caumo F., Saguatti G., Bucchi L., Cataliotti L. Provision of follow-up care for women with a history of breast cancer following the 2016 position paper by the Italian Group for Mammographic Screening and the Italian College of Breast Radiologists by SIRM: A survey of Senonetwork Italian breast centres. Radiol. Med. 2022;127:484–489. doi: 10.1007/s11547-022-01485-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burns K.E., Duffett M., Kho M.E., Meade M.O., Adhikari N.K., Sinuff T., Cook D.J. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Associazione Senonetwork Italia Onlus Indagine Sull’integrazione e Collaborazione tra i Programmi di Screening Mammografico e i Centri Aderenti a Senonetwork. 2020. [(accessed on 7 July 2023)]. Available online: https://www.gisma.it/wp-content/uploads/2022/04/QUESTIONARIO_SCREENING-BU_test-finale.pdf.
- 22.Europa Donna Italia Libro Bianco delle Associazioni di Volontariato nei Centri di Senologia in Italia. 2018. [(accessed on 7 July 2023)]. Available online: https://europadonna.it/wp-content/uploads/2018/04/LIBRO-BIANCO-17.pdf.
- 23.Robinson J.W. Propensity score models in observational comparative effectiveness studies: Cornerstone of design or statistical afterthought? J. Comp. Eff. Res. 2012;1:129–135. doi: 10.2217/cer.12.4. [DOI] [PubMed] [Google Scholar]
- 24.Carlsson C., Nilbert M., Nilsson K. Supporter or obstructer; experiences from contact person activities among Swedish women with breast cancer. BMC Health Serv. Res. 2005;5:9. doi: 10.1186/1472-6963-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Battisti F., Mantellini P., Falini P., Ventura L., Giordano L., Saguatti G., Zappa M., Deandrea S., Gorini G. Key performance indicators of breast cancer screening programmes in Italy, 2011-2019. Ann. Ist. Super. Sanita. 2022;58:244–253. doi: 10.4415/ANN_22_04_04. [DOI] [PubMed] [Google Scholar]
- 26.Ferrara L., Tozzi V.D., Zazzera A. Centro di Ricerche sulla Gestione dell’Assistenza Sanitaria e Sociale. Università Bocconi; Milan, Italy: 2020. Le unità specialistiche di patologia: Modelli e sistemi di gestione delle Breast Unit in Italia. Rapporto OASI 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this article are available from the authors on reasonable request.