B-type natriuretic peptide (BNP) is a cardiac-derived hormone used for diagnosing, prognosticating, and risk stratification of heart failure.1 Though BNP levels differ by sex, obesity, and race/ethnicity, the prognostic value of BNP for heart failure remains intact in these subgroups.2,3 However, data characterizing BNP levels in end-stage heart failure patients with cardiogenic shock is limited. This nationwide Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) study characterized BNP levels and tested the association of BNP levels with clinical outcomes in stage D heart failure patients with cardiogenic shock.
Patients receiving a continuous-flow LVAD between 2005 and 2017 with cardiogenic shock (INTERMACS profiles 1-3) and BNP data were included. BNP levels were assessed at the time of LVAD implantation. The cohort was divided into quartiles based on BNP values. The primary outcome was long-term mortality post-LVAD implantation. Long-term mortality was assessed in LVAD recipients alive at 1-month post-implantation. Secondary outcomes of the study included post-LVAD implantation peri-operative mortality (within 30 days of LVAD implantation), cardiovascular mortality, arrhythmias, and right heart failure.
All analyses were conducted on SAS 9.4 (Cary, NC). Continuous and categorical variables were compared using the Wilcoxon rank sum and Chi-square tests, respectively. Cox regression models were used to assess the association of BNP levels with the study outcomes after accounting for age, sex, race/ethnicity, BMI, INTERMACS profile, estimated glomerular filtration rate, implantation year, device strategy, employment status, education level, and implantation center volume.4,5 The model assessing peri-operative mortality was additionally adjusted for temporary circulatory support in the past 48 hours (extra-corporeal membrane oxygenation or intra-aortic balloon pump), intravenous inotrope use, right atrial pressure, and pulmonary capillary wedge pressure. For the primary outcome, a Fine and Gray sub-distribution model was used to account for the competing risk of heart transplantation. A two-sided p<0.05 was considered statistically significant.
Among 7,290 LVAD recipients with cardiogenic shock, the median value of BNP was 859 (427, 1,614) pg/mL. Upon stratification by factors known to influence BNP, the pre-implantation BNP levels were lower in males, non-Hispanic Blacks, and obese patients compared with their respective counterparts. (Table 1) Compared with the first quartile of BNP, the risk for long-term mortality in the second quartile was 1.06 (95%CI: 0.94-1.20), the third quartile was 0.97 (95%CI: 0.85-1.10), and the fourth quartile was 1.04 (95%CI: 0.91-1.18). The risk of peri-operative mortality was 1.06 (95%CI: 0.67-1.70) in the second quartile of BNP, 1.30 (95%CI: 0.83-2.02) in the third quartile of BNP, and 1.27 (95%CI: 0.81-1.98) in the fourth quartile of BNP compared with the first quartile of BNP. Taking the lowest quartile of BNP as the reference group, the risk for cardiovascular mortality for the second quartile was 0.76 (95%CI: 0.55-1.05), the third quartile was 0.98 (95%CI: 0.73-1.32), and the fourth quartile was 0.89 (95%CI: 0.65-1.23). With the lowest quartile of BNP as the reference group, the risk for arrhythmias in the second quartile was 0.98 (95%CI: 0.87-1.11), the third quartile was 0.94 (95%CI: 0.83-1.06), and the fourth quartile was 1.04 (95%CI: 0.92-1.17). With the lowest quartile of BNP as the reference group, the risk for right heart failure was similar in the second [HRadj: 1.01 (95%CI: 0.88-1.15)], third [HRadj: 0.97 (95%CI: 0.84-1.11)], and fourth [HRadj: 1.04 (95%CI: 0.91-1.20)] quartiles of BNP. The risk of long-term mortality [HRadj: 1.01 (95%CI: 0.97-1.06)], peri-operative mortality [HRadj: 1.11 (95%CI: 0.94-1.30)], cardiovascular mortality [HRadj: 1.00 (95%CI: 0.90-1.11)], arrhythmias [HRadj: 1.03 (95%CI: 0.98-1.07)], right heart failure [HRadj: 1.01 (95%CI: 0.97-1.06)] was not associated with a log-unit increase in BNP levels. Figure 1 summarizes the association of BNP levels with study outcomes.
Table 1:
Median Absolute and Log-Transformed Values of B-Type Natriuretic Peptide Stratified by Race/Ethnicity, Gender, and Body Mass Index
| Absolute value | Log Transformed Value |
p-values | ||
|---|---|---|---|---|
| Unadjusted | Adjusted* | |||
| Race/Ethnicity | ||||
| Non-Hispanic White (n=4,532) | 870 (438, 1,639) | 6.77 (6.08, 7.40) | <0.001 | 0.002 |
| Non-Hispanic Black (n=1,836) | 777 (362, 1,514) | 6.66 (5.89, 7.32) | ||
| Sex | ||||
| Male (n=5,670) | 851 (429, 1,577) | 6.75 (6.06, 7.36) | 0.07 | 0.27 |
| Female (n=1,620) | 893 (404, 1,765) | 6.79 (6.00, 7.48) | ||
| Body Mass Index | ||||
| <25 kg/m2 (n=2,389) | 1,186 (630,2,170) | 7.09 (6.45, 7.68) | <0.001 | <0.001 |
| 25-30 kg/m2 (n=2,289) | 873 (438, 1,632) | 6.77 (6.08, 7.40) | ||
| ≥30 kg/m2 (n=2,612) | 642 (311, 1,170) | 6.46 (5.74, 7.06) | ||
Median (interquartile range) of BNP values depicted in pg/mL.
Adjusted for age, sex, body mass index, and race/ethnicity
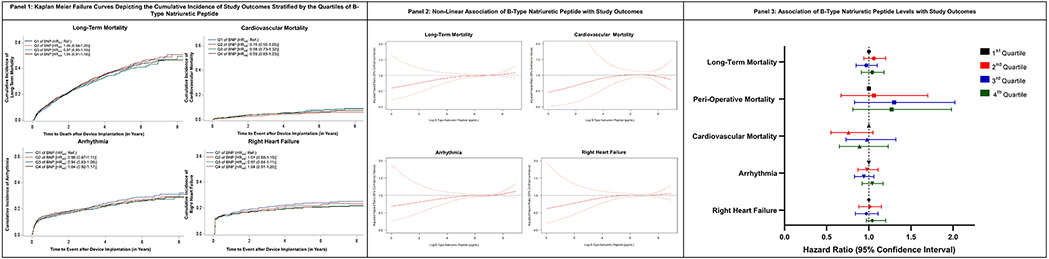
Figure 1: Association of B-Type Natriuretic Peptide with Study Outcomes in Continuous Flow Left Ventricular Assist Device Recipients.
Panel 1: Kaplan Meier Failure Curves Depicting the Cumulative Incidence of Study Outcomes Stratified by the Quartiles of B-Type Natriuretic Peptide
The cumulative incidence curves for long-term mortality, cardiovascular mortality, right heart failure, and arrhythmia stratified by the quartiles of B-type natriuretic peptide (BNP) have been depicted. Quartiles 1, 2, 3, and 4 of BNP have been presented in blue, red, green, and brown, respectively.
Panel 2: Non-Linear Association of B-Type Natriuretic Peptide with Study Outcomes
The figure represents the non-linear association of B-type natriuretic peptide (BNP) with long-term mortality, cardiovascular mortality, arrhythmia, and right heart failure. Restricted cubic spline modeling adjusted for age, sex, race/ethnicity, body mass index, INTERMACS profile, estimated glomerular filtration rate (2021 CKD-EPI creatinine equation), implantation year, device strategy, employment status, education level, and volume of the center at which the device was implanted was used to demonstrate the non-linear association of BNP and study outcomes.
Panel 3: Association of B-Type Natriuretic Peptide Levels with Study Outcomes
Multivariable-adjusted Cox proportional hazard regression models were used to assess the risk of the study outcomes which accounted for age, sex, race/ethnicity, body mass index, INTERMACS profile, estimated glomerular filtration rate (2021 CKD-EPI creatinine equation), implantation year, device strategy, employment status, education level, and volume of the center at which the device was implanted. The Cox model for peri-operative mortality was additionally adjusted for extra-corporeal membrane oxygenation use in the past 48 hours, intra-aortic balloon pump use in the past 48 hours, intravenous inotrope use, right atrial pressure, and pulmonary capillary wedge pressure. The first, second, third, and fourth quartiles of BNP are presented in black, red, blue, and green, respectively.
A sensitivity analysis of 3,390 LVAD recipients assessing the prognostic value of NT-proBNP for mortality was performed. Compared with the first quartile of NT-proBNP, the risk of long-term mortality was similar in the second [0.88 (95%CI: 0.71-1.09)], third [0.88 (95%CI: 0.71-1.09)], and fourth [1.14 (95%CI: 0.92-1.42)] quartiles of NT-proBNP. Similarly, the risk of peri-operative mortality in the second [0.85 (95%CI: 0.46-1.57)], third [1.01 (95%CI: 0.55-1.84)], and fourth [0.69 (95%CI: 0.36-1.34)] quartiles of NT-proBNP was comparable to the first quartile of NT-proBNP. There was no association of per unit increase in log NT-proBNP with the risk of long-term mortality [HRadj: 1.07 (95%CI: 0.99-1.15)] or peri-operative mortality [HRadj: 0.96 (95%CI: 0.79-1.17)].
This nationwide study of >7,000 LVAD recipients characterized and assessed the prognostic value of BNP in stage D heart failure patients with cardiogenic shock. BNP levels were lower in males, non-Hispanic Blacks, and obese individuals compared with their respective counterparts suggesting that factors affecting BNP levels in healthy individuals2,3,6,7 persist throughout the clinical spectrum of heart failure. Additionally, BNP levels were not associated with mortality or any adverse events such as right heart failure and arrhythmias.
BNP levels in end-stage heart failure are not used to guide therapeutic decisions. The current study informs the broader cardiology audience about the futility of measuring BNP in a protocolized manner in patients with end-stage heart failure due to the lack of prognostic value for mortality or other adverse outcomes. Considering the shift of device strategy to destination therapy in the contemporary era8, biomarkers with intact prognostic ability may improve patient selection and promote judicious utilization of limited healthcare resources.
Given the lack of prognostic value of a single biomarker in LVAD recipients, a multi-biomarker approach representing different pathophysiological pathways may have prognostic value in this patient population.9 Considering that the offloading of the left ventricle by an LVAD increases the circulatory burden of the right ventricle, about 35% of LVAD recipients develop right ventricular failure.10 Therefore, a marker that can help predict right heart failure in LVAD recipients can be of great clinical significance. These markers may be combined with other variables to develop a prognostic score for end-stage heart failure patients. Machine-learning models may be employed to develop a comprehensive score incorporating a large number of variables that accurately estimate the risk of post-LVAD adverse events. These scores may guide clinical decision-making by allowing weighing the risk of adverse outcomes after LVAD implantation against the potential years of life gained.
Limitations of this study include the use of self-reported race/ethnicity, exclusion of patients without BNP measurements, and the timing of the BNP measurements before LVAD implantation was not standardized.
In summary, BNP levels in patients with Stage D heart failure varied by sex, race/ethnicity, and BMI, with lower levels noted in males, non-Hispanic Blacks, and obese patients. BNP values did not predict mortality or other adverse events post-LVAD implantation. The role of routine measurement of pre-implantation BNP in LVAD recipients for prognostication requires further investigation.
Sources of Funding:
Dr. Pankaj Arora is supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health (NIH) awards R01HL160982, R01HL163852, R01HL163081, and K23HL146887.
Footnotes
Disclosures: Dr . Pankaj Arora reports grant support from Merck Sharp & Dohme LLC and Bristol-Myers Squibb and consulting income from Bristol-Myers Squibb, which are all unrelated to this work.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Patel N, Gutierrez OM, Arora G, Howard G, Howard VJ, Judd SE, Prabhu SD, Levitan EB, Cushman M, Arora P. Race-based demographic, anthropometric and clinical correlates of N-terminal-pro B-type natriuretic peptide. Int J Cardiol 2019;286:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parcha V, Patel N, Kalra R, Arora G, Januzzi JL Jr., Felker GM, Wang TJ, Arora P. Racial Differences in Serial NT-proBNP Levels in Heart Failure Management: Insights From the GUIDE-IT Trial. Circulation 2020;142:1018–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parcha V, Patel N, Kalra R, Suri SS, Arora G, Wang TJ, Arora P. Obesity and Serial NT-proBNP Levels in Guided Medical Therapy for Heart Failure With Reduced Ejection Fraction: Insights From the GUIDE-IT Trial. J Am Heart Assoc 2021;10:e018689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shetty NS, Parcha V, Abdelmessih P, Patel N, Hasnie AA, Kalra R, Pandey A, Breathett K, Morris AA, Arora G, Arora P. Sex-Associated Differences in the Clinical Outcomes of Left Ventricular Assist Device Recipients: Insights From Interagency Registry for Mechanically Assisted Circulatory Support. Circ Heart Fail 2023;16:e010189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shetty NS, Parcha V, Hasnie A, Pandey A, Arora G, Arora P. Mechanical Circulatory Support Devices Among Patients With Familial Dilated Cardiomyopathy: Insights From the INTERMACS. Circulation 2022;146:1486–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parcha V, Patel N, Musunuru K, Margulies KB, Cappola TP, Halade G, Wang TJ, Arora G, Arora P. Natriuretic Peptide Deficiency in Obese Individuals: Mechanistic Insights From Healthy Organ Donor Cohort. J Am Coll Cardiol 2021;77:3138–3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parcha V, Patel N, Gutierrez OM, Li P, Gamble KL, Musunuru K, Margulies KB, Cappola TP, Wang TJ, Arora G, Arora P. Chronobiology of Natriuretic Peptides and Blood Pressure in Lean and Obese Individuals. J Am Coll Cardiol 2021;77:2291–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varshney AS, DeFilippis EM, Cowger JA, Netuka I, Pinney SP, Givertz MM. Trends and Outcomes of Left Ventricular Assist Device Therapy: JACC Focus Seminar. J Am Coll Cardiol 2022;79:1092–1107. [DOI] [PubMed] [Google Scholar]
- 9.Ibrahim NE, Januzzi JL Jr. Established and Emerging Roles of Biomarkers in Heart Failure. Circ Res 2018;123:614–629. [DOI] [PubMed] [Google Scholar]
- 10.Bellavia D, Iacovoni A, Scardulla C, Moja L, Pilato M, Kushwaha SS, Senni M, Clemenza F, Agnese V, Falletta C, Romano G, Maalouf J, Dandel M. Prediction of right ventricular failure after ventricular assist device implant: systematic review and meta-analysis of observational studies. Eur J Heart Fail 2017;19:926–946. [DOI] [PubMed] [Google Scholar]