Abstract
Introduction:
American Indian and Alaska Native (AI/AN) populations are disproportionately affected by substance use disorders (SUDs) and related health disparities in contrast to other ethnoracial groups in the United States. Over the past 20 years, substantial resources have been allocated to the National Institute on Drug Abuse Clinical Trials Network (CTN) to disseminate and implement effective SUD treatments in communities. However, we know little about how these resources have benefitted AI/AN peoples with SUD who arguably experience the greatest burden of SUDs. This review aims to determine lessons learned about AI/AN substance use and treatment outcomes in the CTN and the role of racism and Tribal identity.
Method:
We conducted a scoping review informed by the Joanna Briggs framework and PRISMA Extension for Scoping Reviews checklist and explanation. The study team conducted the search strategy within the CTN Dissemination Library and nine additional databases for articles published between 2000 and 2021. The review included studies if they reported results for AI/AN participants. Two reviewers determined study eligibility.
Results:
A systematic search yielded 13 empirical articles and six conceptual articles. Themes from the 13 empirical articles included: (1) Tribal Identity: Race, Culture, and Discrimination; (2) Treatment Engagement: Access and Retention; (3) Comorbid Conditions; (4) HIV/Risky Sexual Behaviors; and (5) Dissemination. The most salient theme was Tribal Identity: Race, Culture, and Discrimination, which was present in all articles that included a primary AI/AN sample (k=8). Themes assessed but not identified for AI/AN peoples were Harm Reduction, Measurement Equivalence, Pharmacotherapy, and Substance Use Outcomes. The conceptual contributions used AI/AN CTN studies as exemplars of community-based and Tribal participatory research (CBPR/TPR).
Conclusion:
CTN studies conducted with AI/AN communities demonstrate culturally congruent methods, including CBPR/TPR strategies; consideration/assessment of cultural identity, racism, and discrimination; and CBPR/TPR informed dissemination plans. Although important efforts are underway to increase AI/AN participation in the CTN, future research would benefit from strategies to increase participation of this population. Such strategies include reporting AI/AN subgroup data; addressing issues of cultural identity and experiences of racism; and adopting an overall effort for research aimed at understanding barriers to treatment access, engagement, utilization, retention, and outcomes for both treatment and research disparities for AI/AN populations.
Keywords: American Indian, Alaska Native, Clinical Trials Network, Substance use, Treatment, Scoping review
1. Introduction
American Indian and Alaska Native (AI/AN) populations are disproportionately affected by substance use disorders (SUDs) and related health disparities in contrast to other ethnic/racial groups in the United States (U.S.; Gone, 2022; Substance Abuse and Mental Health Service Administration [SAMHSA], 2019; Whitesell et al., 2012). Data from the National Survey on Drug Use and Health (NSDUH; SAMHSA, 2019) indicate that AI/AN peoples have the highest prevalence of past-year alcohol, marijuana, methamphetamine, opioid, inhalant, hallucinogen, and tobacco use disorders compared to the general US population. Further, AI/AN people are more likely to report problematic drug use in the past month (17.4%) and year (28.5%) than any other ethnic/racial group. However, these substance issues are complicated by traumas (historical, racial, mental/physical) and related health disparities (e.g., cancer, chronic lower respiratory diseases), with little attention given to cultural strengths and inherent protective factors (Blume, 2020; Gone et al., 2019). While disparities exist, narratives are important tools for effecting systemic change and addressing stigma. For example, AI/AN peoples have higher rates of alcohol abstinence compared to White, Black, and Hispanic groups in the United States (Cunningham et al., 2016).
AI/AN peoples have been historically under- and misrepresented in substance use research as a function of systemic racism; mistrust of researchers has also contributed to less willingness of Tribes to partner in research endeavors (Skewes & Blume, 2019; Wendt et al., 2019). A deeply painful history of colonization, racist practices, and culturally unresponsive research has perpetuated negative stereotypes about AI/AN peoples with SUDs and has contributed to internalized negative beliefs, underutilization of health care, increased substance use and related risk behaviors, exacerbated health disparities, and enlarged the gap in treatment seeking and engagement (Blume, 2020; Cunningham et al., 2016; Gone et al., 2019; Gonzalez & Skewes, 2021). Culturally protective factors and cross-tribal variability in substance use highlight the crucial role of research in addressing multilevel risk and resilience factors among AI/AN peoples to understand SUDs, adapt interventions, and improve holistic health outcomes (Skewes & Blume, 2019; Wendt et al., 2019; Whitesell et al., 2012).
Persistent issues related to SUD inequities among AI/AN peoples include limited access to treatment; underutilization of services; lack of culturally sensitive and adapted interventions; and compounding burdens of historical trauma, discrimination, and systemic racism (Greenfield & Venner, 2012; Skewes & Blume, 2019; Wendt et al., 2019). The need for culturally inclusive research among the AI/AN population is imperative. Importantly, in one study (Brave Heart et al., 2016) AI/AN peoples’ prevalence of SUDs and related disparities were reduced when controlling for socioeconomic factors. AI/AN peoples experience higher rates of barriers to care (e.g., health insurance, formal education) and upward mobility (e.g., low socioeconomic status, rurality) in contrast to other ethnic/racial groups, especially non-Hispanic White people. Further, when socioeconomic factors and barriers are considered, the disparate rates of mental health and SUDs are mitigated across ethnic/racial US groups. Thus, sociopolitical, environmental, and systemic issues that are key drivers in oppression and discriminatory views toward AI/AN communities contribute to their high health disparities and substance misuse.
Research and clinically effective services are vital to addressing these disproportionate health disparities. In fact, epidemiological data demonstrate that in addition to health-related outcomes, AI/AN peoples have lower uptake, engagement, and retention in alcohol and drug-related health service in contrast to other US ethnic/racial groups (Novins et al., 2016; Soto et al., 2022; Whitesell et al., 2012). Clinical trials are a standardized way to test and establish culturally developed/adapted, evidence-based interventions that can mitigate barriers to care and increase inclusion and use. Engaging and partnering with well-funded and far-reaching research entities is a critical entry point for AI/AN research. It offers much promise toward equitable and ethical SUD clinical research for AI/AN peoples that is culturally congruent, evidence-based, and destigmatizing. Important clinical trials research has been done within the National Institutes of Health (NIH) system. For example, the Intervention Research to Improve Native American Health (IRINAH) consortium, established in 2011, has produced 27 projects to address AI/AN community priority needs (e.g., health equity, disease prevention, SUD treatment) (Crump et al., 2020; Rasmus et al., 2020). However, more research and increased efforts designed to meet the unique needs of the AI/AN population are still needed.
One such large research enterprise is the National Institute on Drug Abuse Clinical Trials Network (CTN), a collaborative of behavioral, integrated, and pharmacological research trials that are rigorous, diverse, and often multi-site. The CTN represents an optimal infrastructure for research of interventions delivered to physicians, clinicians, providers, and patients. Further, it is critical that the CTN resources benefit all people with SUDs, especially groups that have been minoritized. To investigate this, two prior scoping reviews were conducted to identify how the CTN has informed and improved SUD treatment among Black (Montgomery et al., 2020) and Hispanic populations (Eghaneyan et al., 2020). The scoping review focused on Black CTN participants yielded 50 articles, primarily reporting baseline characteristics (Montgomery et al., 2020). Themes also included treatment outcomes, HIV/risky sex behaviors, retention, comorbidity, and measurement. The scoping review focused on Hispanic CTN participants yielded 24 articles, and themes included study characteristics; engagement and assessment; baseline sample characteristics; treatment outcomes; and HIV/risky sex behaviors. Both reviews inform unique substance use issues, barriers to treatment, culturally salient strategies for engagement, and recommendations for the CTN to establish more deliberate efforts for inclusion of and research with these populations.
However, no review of published CTN data have been conducted to understand how the CTN has informed and improved SUD treatment for AI/AN communities. The CTN’s previous estimates of AI/AN inclusion report approximately 2% of CTN research participants were AI/AN (Burlew et al., 2011). Of the 49 active or in-development CTN protocols, four are specific to AI/AN participants. The purpose of the current research is to conduct a scoping review of more than two decades of CTN studies to understand the unique contributions of the AI/AN participants. Specifically, we aim to characterize this body of research, such as the research questions addressed, and designs employed to make recommendations for future research endeavors.
2. Method
We conducted a scoping review following the Joanna Briggs Institute (JBI; Peters et al., 2020) framework and the PRISMA Extension for Scoping Reviews Checklist and Explanation (Page et al., 2021; Tricco et al., 2018). The JBI framework is developed from Arksey and O’Malley’s (2005) framework for scoping reviews. Scoping reviews are an evidenced-based methodology for synthesis and summary of research results that are topic-based versus question-based (Peters et al., 2020). Scoping reviews are broader than systematic reviews, which answer a specific question about the effectiveness of treatment(s). We conducted all scoping review procedures (i.e., abstract review, full text review, extraction) using Covidence, a web-based screening and extraction software platform.
The study team developed the protocol a priori in March 2021 and preregistered it through the Open Science Framework registration: https://osf.io/3xsbc/. Our method was based on two prior CTN scoping reviews (Eghaneyan et al., 2020; Montgomery et al., 2020) conducted among research populations that are minoritized (i.e., Black, Hispanic). Thus, given that prior CTN research has been conducted to synthesize studies that provide outcomes for AI/AN people, we developed the research question to be broad and reflect the range of data that could be identified: What has been learned about AI/AN participants in CTN research?
2.1. Selection of studies
The team conducted a medical subject heading (MeSH) analysis to identify CTN articles published between 2000 and 2021. To maximize sensitivity, the formal search used minimal controlled vocabulary terms and synonymous free-text words to capture the concepts of (1) “American Indian,” “Alaska Native,” and “Native Hawaiian” and (2) “the National Institute on Drug Abuse Clinical Trials Network”. The search strategy was peer reviewed by a second librarian, not associated with the project, using the Peer Review of Electronic Search Strategies (PRESS) standard (McGowan et al., 2016). On January 5, 2021, the librarian searched the following databases: MEDLINE, Embase, PsycInfo, PubMed Central, Google Scholar, ProQuest Dissertations & Theses, and the CTN Dissemination Library. Both English and foreign language articles were included in the search; however, we identified only English language articles. No date limit was applied. Appendix A describes all search strategies. The final search retrieved a total of 360 references, 90 of which were duplicates. Two hundred and seventy references were screened for eligibility.
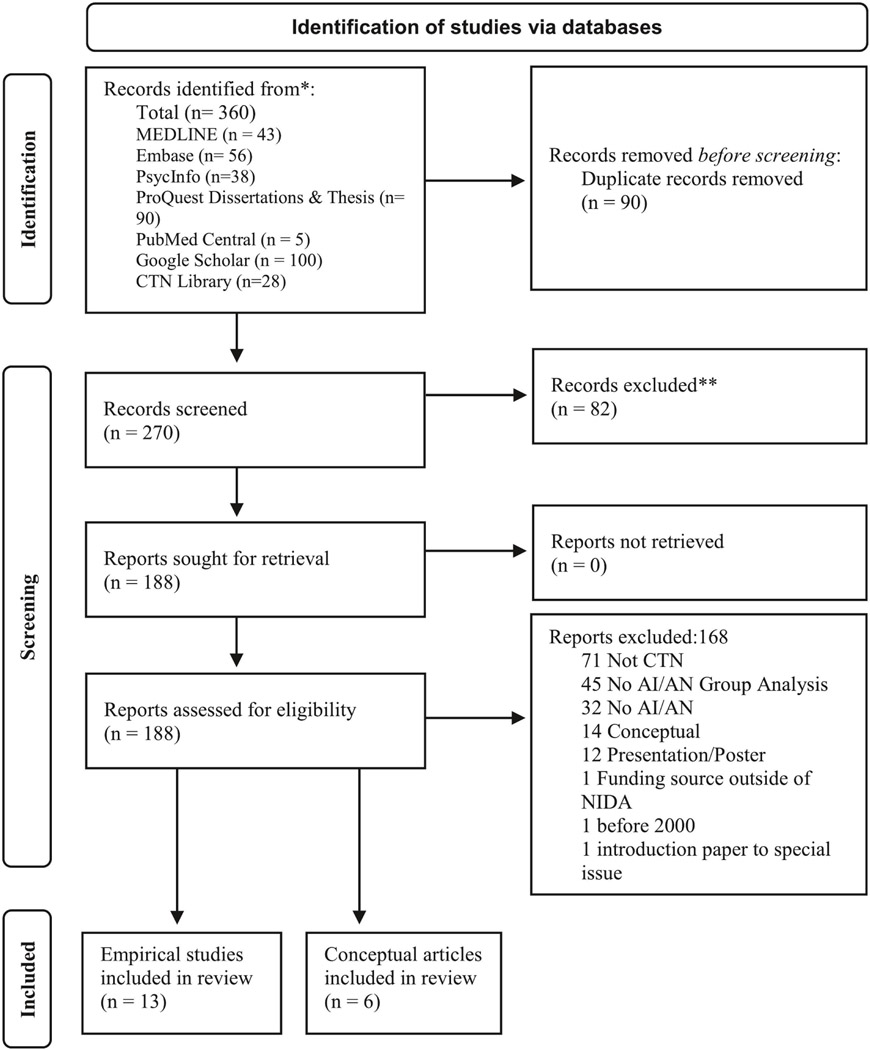
The review included studies if they (1) reported findings pertaining to AI/AN peoples (inclusive of Indigenous, Native Hawaiian, First Nations, Inuit, and/or Métis participants); and (2) mentioned CTN in text or in the acknowledgements. We excluded studies if they (1) did not include AI/AN participants or report findings for AI/AN; (2) were not CTN studies; (3) were published prior to 2000, the year the CTN was established; and (4) were not empirical (i.e., research study) manuscripts. We used the same inclusion criteria for the conceptual articles as we did for the empirical studies, with the exception that they were not empirical studies, rather, summarized data reported for AI/AN populations. The review included conceptual articles based on their assessed contribution to CTN research and to this scoping review. Two screeners independently reviewed the titles, abstracts, and full text of the eligible articles. Conflicts were resolved through consensus. The PRISMA flowchart is presented in Figure 1. Three reviewers were used for each phase, so that two independent reviewers made decisions on the abstracts, full-text, and thematic charting and a third reviewer settled discrepancies for final decision making.
Figure 1.
PRISMA flow diagram of search strategy (McKenzie et al., 2020).
Note. CTN = Clinical Trails Network; AI/AN = American Indian/Alaska Native.
2.2. Data charting
The study team collated data and analyzed them thematically, which included group consensus of conceptual and contextual factors pertinent to AI/AN populations and SUD research (Peters et al., 2020). Themes were determined as being key indicators of each study’s origin, aims, population, sampling, methods, interventions, outcomes, and key findings. Prior CTN scoping reviews (Eghaneyan et al., 2020; Montgomery et al., 2020) and the literature (Blume, 2020; Greenfield & Venner, 2012; Novins et al., 2016; Soto et al., 2022) relevant to AI/AN people and SUD treatment informed the final themes. For example, AI/AN literature includes issues of how tribal identity is determined, use of community-based participatory research (CBPR) approaches, and tribal approvals in addition to university-based Institutional Review Board (IRBs).
3. Results
3.1. Empirical papers
This scoping review yielded 13 studies that reported data specific to AI/AN participants. We identified five themes describing these studies: (1) Tribal Identity: Race, Culture, and Discrimination; (2) Treatment Engagement: Access and Retention; (3) Comorbid Conditions (e.g., medical, psychiatric); (4) HIV/Risky Sexual Behaviors; and (5) Dissemination (e.g., sharing the results; sharing the intervention). Some studies (k=4) reflected one theme, with the majority (k=9) reflecting two or more themes. Although we anticipated reporting on themes related to harm reduction, measurement equivalence, pharmacotherapy, and substance use outcomes, none of these 13 studies reported data within these themes specifically for AI/AN peoples. We provide a comprehensive list of authors and key observations in Table 1.
Table 1.
Key observations for AI/AN participants in each study
| Author(s) and date | CTN protocol # | Secondary Analysis | N (% AI/AN) | Theme(s) | Key observations for AI/AN peoples |
|---|---|---|---|---|---|
| 1. Brown et al., 2009 | NR | No | NR (19.4) | Tribal Identity; Treatment Engagement; HIV/Risky Sexual Behaviors |
Treatment programs with addiction services tailored for AI/AN people were substantially more likely to provide 5 of the 21 different infection-related health services (24.0%) than programs without tailored-addiction services. |
| 2. Calsyn et al., 2013 | 0018, 0019 | Yes | 76 (7.3) | HIV/Risky Sexual Behaviors | AI/AN participants represented 7.0% of men and 8.1% of women engaged in heterosexual anal sex; and represented 8.7% of men and 3.3% of women not engaged. |
| 3. Campbell et al., 2015 | NR | No | 40 (100) | Tribal Identity; Treatment Engagement; HIV/Risky Sexual Behaviors; Dissemination |
A web-based version of the Therapeutic Education System was acceptable in an urban sample of AI/AN people; and qualitative interviews suggest adapting the intervention to include cultural factors could improve adoption of the Therapeutic Education System. |
| 4. Foley et al., 2010 | 00020 | No | 102 (100) | Tribal Identity; Treatment Engagement |
There was no statistically significant difference at a three-month follow-up between two job skills trainings delivered either in person (Job Seekers Workshop) versus watching a video (Job Interviewing Video); or between substance use frequency by group among unemployed AI/AN participants in residential treatment. |
| 5. Forcehimes et al., 2011 | 0033-Ot-2 | No | 300 (100) | Tribal Identity; Treatment Engagement; Dissemination |
Data suggested concerning rates of methamphetamine use among AI/AN peoples, with women more adversely affected by substance use in general, however, alcohol was identified as the biggest substance use problem for AI/AN populations in the Southwest. |
| 6. Kropp et al., 2013 | NR | No | 77 (100) | Tribal Identity; Treatment Engagement; Comorbid Conditions |
A sample of AI/AN clients seeking treatment at an urban, non-tribal treatment program indicated that alcohol is the leading substance of abuse, followed by marijuana; alcohol and marijuana by far are used earlier, longer, and by more treatment-seeking clients; substance use onset and patterns are correlated with victimization, cognitive impairment, and suicidal behavior; and most participants reported receiving support for recovery from both interpersonal and cultural sources. |
| 7. Kropp et al., 2014 | 0033-Ot-4 | No | 143 (100) | Tribal Identity; Treatment Engagement |
Providing linkage services, such as case management, to AI/AN clients on the waiting list would assist in stabilization and encourage ongoing motivation for treatment during the interim between the initial intake and treatment entry. |
| 8. Loree et al., 2019 | 0072-0T | Yes | 1218 (1.4) | Comorbid Conditions | AI/AN people with comorbid psychiatric disorders were more likely to initiate but no more likely to engage in alcohol or other drug treatment compared with those without a comorbid psychiatric disorder, which was consistent with the findings for the overall sample. |
| 9. Radin et al., 2012 | NR | Yes | 4,851 (100) | Tribal Identity; Treatment Engagement; Dissemination |
Community health is tied to access to resources, services, and culturally appropriate and effective interventions. Treatment data results were consistent with interviewee reported substance use/abuse trends, with alcohol as the primary drug for 56.0% of AI/AN adults compared to 46.0% of non-AI/AN. |
| 10. Radin et al., 2015 | NR | No | 153 (NR) | Tribal Identity; Treatment Engagement; Dissemination |
Qualitative data analysis among a sample of primarily AI/AN participants observed robust themes: prescription medications and alcohol were perceived as most prevalent and concerning; family and peer influences and emotional distress were prominent perceived risk factors; and substance use disorder/alcohol use disorder intervention resources varied across communities. |
| 11. Rieckmann et al., 2012 | NR | Yes | 195 (100) | Tribal Identity; Treatment Engagement; Comorbid Conditions |
Urban AI/AN clients were more likely to report employment problems, polysubstance use, and a history of abuse. Reservation-based clients reported having more severe medical problems and a greater prevalence of psychiatric problems. |
| 12. Stephens et al., 2020 | NR | Yes | 118 (1.2) | Comorbid Conditions | Of the AI/AN participants, 17.8% had diabetes (19% of those had any substance use disorder), 77.1% hypertension (9.9% of those had any substance use disorder), and 36.4% obesity (9.3% of those had any substance use disorder). |
| 13. Wu et al., 2015 | NR | Yes | 587 (0.3) | Comorbid Conditions | AI/AN patients had greater odds of having type 2 diabetes mellitus than White patients. |
Note. AI/AN = Alaska Native/American Indian; CTN = Clinical Trials Network; NR = Not Reported.
The results of the 13 yielded studies include primary (k=6) and secondary (k=6) outcomes, and one study included both primary and secondary outcomes. Notably, more than half of the studies in this review included secondary analyses (k=7). Of the 13 studies, AI/AN representation ranged from 1.4% to 100% of participants, with eight studies exclusively sampling AI/AN communities and one additional primary data collection study that expanded recruitment beyond AI/AN participants. Eight studies reported reservation and village involvement in research processes and tribal approval(s). Substances targeted for treatment were tobacco (n=1), methamphetamines (n=1), opioids (n=2), alcohol and other drugs (n=2), and any substance (n=7). Overall, alcohol was identified as the substance of most concern to the AI/AN population (k=8).
3.1.1. Tribal identity: Race, culture, and discrimination.
Nine studies (Brown et al., 2009; Campbell et al., 2015; Foley et al., 2010; Forcehimes et al., 2011; Kropp et al., 2013; Kropp et al., 2014; Radin et al., 2012; Radin et al., 2015; Rieckmann et al., 2012) reported on tribal identity, race, culture, and discrimination. These studies demonstrated that internalized stigma, experiences of discrimination, lack of available culturally congruent care, and lower racial and tribal identity are related to increased substance use among AI/AN peoples. The studies operationalized race and tribal identity differently. Most studies reported that race was self-identified without specifying how this was collected (e.g., multiple choice, open response). Kropp et al. (2013) reported tribal affiliation in general (e.g., Northern Plains) rather than identifying specific tribes to maintain anonymity.
Stigma and discrimination were based on external (e.g., social attitudes) and internal (e.g., shame) factors. These included lack of support from family based on stigmatizing views of treatment and substance use (Kropp et al., 2013; Kropp et al., 2014). Providers’ stigmatizing beliefs and discriminatory practices were identified as barriers to treatment and recovery (Campbell et al., 2015; Forcehimes et al., 2011). The studies also correlated discriminatory practices to poverty, health disparities, and lack of contextualized and culturally congruent care (Foley et al., 2010; Radin et al., 2012). All of these were viewed as contributing to continued systemic oppression, intergenerational traumas, and substance misuse.
Campbell et al. (2015) assessed for cultural/ethnic identity, which was the only study in this review to do so. They observed that higher perceived discrimination (i.e., perceived treatment of one’s ethnic group in society) was associated with lower acceptability of a treatment module focused on skills to receive constructive criticism. In turn, this might improve the relationships with providers and engagement with treatment.
Stigma was also a significant factor in acceptability of infectious disease–related services. Brown et al. (2009) observed that stigmatizing views of infection-related diseases (e.g., HIV/AIDS) compounded by negative views of substance use are a large barrier to patient’s acceptance of integrated services. The study suggested that “patient acceptance may in part be a consequence of the stigma often associated with these infections and the background of discrimination often experienced by members of these special populations” (Brown et al., 2009, p. 100).
In addition to issues of stigma and discrimination, the eight AI/AN focused studies assessed cultural factors to varying degrees. These included tribal affiliation, ever lived on a reservation or tribal land, cultural identity, cultural practices, spiritual beliefs, and spiritual or ceremonial practices. Importantly, cultural factors and experiences of discrimination were highly correlated. All studies were specific to the AI/AN community, except for Brown et al. (2009), which noted that culturally tailored substance use treatment programs were more likely to support infection-related services (e.g., treatment for HIV/AIDS) within AI/AN substance use treatment programs.
One study (Foley et al., 2010) conducted a cultural adaptation of the Job Seekers Workshop (JSW) for an AI/AN tribal program, Na’Nizhoozhi Center, that included multiple resources (e.g., employment, custody) embedded in a residential treatment program for SUDs. This study compared the culturally adapted JSW and a 40-minute job interview video. Study staff were AI/AN peoples who could translate Dine’ (Navajo) and referred to participants as “relatives” and Dine’ speaking fidelity monitoring was used for appropriate translations. Reservation-based participants indicated that maintaining family relationships and connections were most important to well-being and even more than maintaining employment. Barriers included “transportation, feelings of cultural conflict, cultural-bound tests and assessments, and the use of English as a second language” (Foley et al., 2010, p. 2). The study found no treatment differences between the culturally adapted JSW and a 40-minute job interview video.
Two studies (Campbell et al., 2015; Rieckmann et al., 2012) used cultural/culturally adapted measures. First, Campbell et al. (2015) used the Addiction Severity Index-Native American Version (ASI-NAV) as well as a cultural identity measure (i.e., Scale of Ethnic Experiences; Malcarne et al., 2006), which includes assessment across four dimensions: (1) ethnic identity; (2) perceived discrimination; (3) mainstream comfort; and (4) social affiliation. The study observed significant associations between higher perceived discrimination and lower acceptability of the module for criticism and between higher mainstream comfort and higher acceptability of the self-management planning module. Campbell et al. also reported on client interview results, suggesting that the digital therapeutic intervention was acceptable but should be culturally tailored, such as including AI/AN actors in the videos, use of storytelling to teach the skills, and incorporating Native spirituality. Participant interviews also indicated using AI/AN slang words, including cultural values (e.g., humor, nature), and incorporating cultural practices (e.g., sweat lodge, drumming) for culturally tailored treatment and treatment videos. Second, Rieckmann et al. (2012) described AI/AN populations in two specialty addiction treatment programs (one in an urban center and one on a reservation) in which one used the ASI-NAV and the other used an adapted Addiction Severity Index (ASI) with no psychometric validation. However, no ASI-NAV data were reported. The study recommended culturally tailored treatment given the prevalence of mental health and medical comorbidities; variations in substance use by setting (i.e., urban, rural, reservation); differences in tribal affiliation; and given the importance of culture and ceremony among AI/AN peoples. However, the study provided no explicit recommendations.
The remaining five studies used primarily focus group and interview methods to understand cultural factors of treatment apart from one study. Kropp et al. (2013) used deidentified intake data to provide descriptions of substance use and cultural variables for an urban specialty addiction program in the Great Plains area. The study assessed cultural heritage as important, not important, or not sure/maybe. Of the 129 participant responses, 91 (71.1%) reported that their culture was important, while 22 (17.2%) reported it was not. Cultural heritage was rated as most important to those who were raised in a setting other than the one in which they were born (78.8%). Male participants placed more importance on cultural aspects of treatment and expressed more frustration with the lack of cultural resources.
Kropp et al. (2014) shared client and provider focus group results on barriers to treatment. Male clients indicated a strong desire for culture to be included in treatment, whereas female clients said it was important but did not experience the lack of it as a barrier to treatment. Providers emphasized the need to individualize the incorporation of culture rather than assume all AI/AN clients are the same. They offered recommendations to programs interested in including culture, such as inviting Elders to speak; finding AI/AN people to serve as sponsors in 12-Step programs; increasing access to AI/AN traditional healing practice; and increasing the number of AI/AN staff and providers.
Forcehimes et al. (2011) observed that participants (including community members and the provider group) mostly endorsed Western treatment methods, except for one community group that endorsed traditional spiritual practices for treatment. Conversely, Radin et al.’s (2012) interviews with tribal health directors “described an ongoing revitalization of Native/tribal culture through reconnection with cultural history, traditional Native practices, and cultural ways as an important part of substance use/abuse recovery and overall community health and wellness” (p. 514).
Last, Radin et al. (2015) sought input from tribal members, leaders, and providers to understand culturally salient SUD treatment among tribal communities in Washington State. The study observed that effective prevention and treatment were viewed as inseparable from cultural practices that were tribal community centric. Participants indicated that treatment and recovery services need to be integrated into, offered within, and derived from the strengths and resources embedded in the local community. Culturally congruent, tailored, and/or adapted treatment were perceived to mitigate health disparities (i.e., treating comorbid conditions) and cultural trauma (i.e., historical trauma, historical grief).
3.1.2. Treatment engagement: Access and retention.
Nine studies (Brown et al., 2009; Campbell et al., 2015; Forcehimes et al., 2011; Foley et al., 2010; Kropp et al., 2013; Kropp et al., 2014; Radin et al., 2012; Radin et al., 2015; Rieckmann et al., 2012) reported information related to treatment engagement, access, and recruitment.
Eight studies (Campbell et al., 2015; Forcehimes et al., 2011; Foley et al., 2010; Kropp et al., 2013; Kropp et al., 2014; Radin et al., 2012; Radin et al., 2015; Rieckmann et al., 2012) were specific to AI/AN communities and reported using a CBPR and/or tribal participatory research (TPR) approach. Across all nine studies, culturally tailoring services increased integrative care and access to said care (i.e., infection services embedded in substance use treatment; Brown et al., 2009); culturally tailoring interventions increased adoption of web- and evidence-based practices (Campbell et al., 2015); culturally congruent methods and ethnic- and gender-matching of study staff are integral for enhancing treatment engagement (Foley et al., 2010; Forcehimes et al., 2011; Kropp et al., 2013; Kropp et al., 2014); and CBPR/TPR is the cornerstone of effectively designed AI/AN research that optimizes access, treatment engagement, and retention (Radin et al., 2012; Radin et al., 2015; Rieckmann et al., 2012).
An example of using a CBPR/TPR approach to recruit, Radin et al. (2015) regularly attended community events and recruited participants through nominations by community advisory boards, fliers, word of mouth, and other types of community advertising. Foley et al. (2010) reported using staff fluent in Dine’ (Navajo); escalating compensation for each assessment (and a bonus for full participation); and being flexible with the format of interviews (e.g., over the phone), all as CBPR/TPR strategies that increased treatment engagement.
3.1.3. Comorbid conditions.
Five studies (Kropp et al., 2013; Loree et al., 2019; Rieckmann et al., 2012; Stephens et al., 2020; Wu et al., 2015) in this review reported on comorbid conditions (e.g., medical, mental illness). Specifically, AI/AN peoples disproportionately experience psychiatric disorders, HIV, and other infection-related illnesses (e.g., hepatitis C virus) that co-occur with SUDs (SAMHSA, 2019; Whitesell et al., 2012).
Loree et al. (2019) observed that of the AI/AN participants (N=893) with a prior psychiatric disorder and alcohol and other drug (AOD) issue, 33.8% initiated treatment, and of those, 0.08% engaged in treatment. Stephens et al. (2020) found that among AI/AN participants (n=118), 17.8% had diabetes, 19% of which had co-occurring SUD; 77.1% had hypertension, 9.9% of which had co-occurring SUD; and 36.4% had obesity, 9.3% of which had co-occurring SUD. Last, Wu et al. (2015) reported that AI/AN participants (N=587) had higher odds of developing type 2 diabetes mellitus (T2DM) than White participants.
Kropp et al. (2013) found that “substance use onset and patterns are [positively] correlated with victimization, cognitive impairment, and suicidal behavior” (p. 719). In a sample of AI/AN participants, Rieckmann et al. (2012) observed that reservation-based participants have more frequent urgent medical issues, such as past 30-day prevalence of medical problems and hospitalizations; whereas urban-based participants (57%) experience more chronic medical issues in contrast to reservation-based participants (40%). Most of the sample (74%) reported a lifetime history of depression and/or anxiety; 39% had a lifetime history of suicidal ideation, and 19% reported one or more suicide attempt(s); and opioid use was significantly associated with a chronic medical issue, polysubstance use, more severe depression and anxiety, and increased suicidality/attempt(s).
3.1.4. HIV/Risky sexual behaviors.
The CTN approach to investigating HIV and risky sexual behaviors among AI/AN peoples was limited to three studies (Brown et al., 2009; Calsyn et al., 2013; Campbell et al., 2015). Moreover, the work varied from simply reporting the number of AI/AN peoples in the study to one intervention study (Campbell et al., 2015) focused on AI/AN people.
Findings from Brown et al. (2009) suggest that racial discrimination and stigmatization of HIV, sexually transmitted infections (STI), and SUD diagnoses might explain the lack of infection-related health services tailored to AI/AN peoples and other communities beyond the availability of federal funding or health care insurance. Additionally, treatment programs with addiction services tailored for AI/AN people were 24% more likely to provide 5 of the 21 different infection-related health services than programs without tailored-addiction services. Low patient acceptance of services was the second most important barrier to HIV-related treatment after lack of government funding for serving AI/AN peoples, despite the use of tailored services in approximately one fifth of treatment sites.
Calsyn et al. (2013) investigated gender differences in heterosexual anal intercourse practices among substance using men and women participating in two CTN HIV risk reduction interventions (Real Men Are Safe and Safer Sex Building). However, the only information reported on AI/AN participants (n=76) was that 26 men (34.2%) and 29 women (38.2%) engaged in heterosexual anal intercourse, whereas 17 men (22.4%) and four women (5.3%) did not engage in such.
The only study (Campbell et al., 2015) focused on AI/AN participants and infectious diseases, aimed to evaluate the acceptability of a web-based version of a therapeutic education system (TES) intervention among an AI/AN sample. The TES comprises 32 modules, five of which were specific to HIV, STIs, and risky sex behaviors: (1) Managing triggers for risky sex; (2) Sexual transmission of HIV and STIs; (3) Drug use, HIV, and hepatitis; (4) Sexually transmitted infections; and (5) HIV and AIDS. The first three modules were among the highest rated for acceptability by participants.
3.1.5. Dissemination.
Four studies (Campbell et al., 2015; Forcehimes et al., 2011; Radin et al., 2012; Radin et al., 2015) reported findings related to dissemination. All studies were conducted among the AI/AN community. First, Campbell et al. (2015) highlighted the need for dissemination efforts (i.e., sharing the intervention) to be novel and innovative in their design of a web-based intervention that could address unique barriers (e.g., rurality, transportation). Forcehimes et al. (2011) recruited partners from local communities and collaborated with partners in the Tribal center (i.e., NCI). Both partners assisted in all phases of the study including dissemination of results. They made a dissemination plan collaboratively with the Tribal partners, which was required from the Tribal IRB: Navajo Nation Human Research Review Board (NNHRRB). Radin et al. (2012) highlighted community partnerships in the dissemination and adoption of results. Last, Radin et al. (2015) used a CBPR/TPR approach with the intent of improving the study, facilitating community relationships, and increasing dissemination and useability. They reported that “each community’s data were analyzed and disseminated separately for their own use” (p. 38). Overall, dissemination was addressed as a function of the CBPR/TPR approach and as a culturally relevant practice of tribal ownership of data, sharing of information, and ensuring ethical reporting. However, none of the four studies explicity reported implementation of these plans.
3.2. Conceptual articles
We also identified and summarized suggestions for AI/AN people from six conceptual articles (Burlew et al., 2020; Burlew et al., 2011a; Burlew et al., 2011b; Carroll et al., 2007; Perl, 2011; Thomas et al., 2011; see Table 2).
Table 2.
Key observations for AI/AN participants in each conceptual contribution
| Author(s) and date | CTN Protocol # | Type of source | Key contributions for AI/AN peoples |
|---|---|---|---|
| 1. Burlew et al., 2020 | 0018; 0019; 0021; 0033 | Perspective, opinion, or commentary | Limited information is available for community engaged, collaborative, cultural adaptation of effective interventions. A study of substance use among AI/AN communities was one of the earliest efforts within the CTN to consider the role of culture in treatment and the need for community participation. |
| 2. Burlew et al., 2011a | NR | Perspective, opinion, or commentary | A CTN partnership with the Na’nizhoozhi Center, an AI/AN substance use treatment program, exemplified how cultural adaptations and community based participatory research strategies increase efficacy, acceptability, and inclusion of substance use treatment for underrepresented ethnoracial groups within the CTN. |
| 3. Burlew et al., 2011b | 0004; 0006; 0007; 0013; 0014; 0015; 0018; 0020; 0020-A-1; 0029; 0042-S | Perspective, opinion, or commentary | AI/AN studies are used to demonstrate community based participatory research strategies for recruitment, treatment access, retention, measurement, and appropriate analyses related to CTN research among underrepresented ethnoracial groups. |
| 4. Carroll et al., 2007 | NR | Conference proceedings | The CTN is an ideal avenue for research addressing unmet substance use needs among underrepresented ethnoracial groups. For AI/AN groups, this is supported by the Native American Workgroup who advocates for more Indigenous inclusion at all levels; by challenging stigma and addressing historical trauma; and by the CTN partnering with AI/AN Tribes. |
| 5. Perl, 2011 | 0033 | Perspective, opinion, or commentary | To support more resources for implementation science for addiction treatment, three strategies are identified: (1) developing scientific tools to better understand implementation; (2) building an implementation workforce; and (3) including clinicians at the start to have more relevant research. Successful examples include three collaborations between academic partners and AI/AN Tribal entities. |
| 6. Thomas et al., 2011 | 0033 | Perspective, opinion, or commentary | Five partnerships between academic institutions and AI/AN Tribes/organizations that represented community based participatory research observed common themes for addressing barriers and establishing successful partnerships included community driven research; contextualized community knowledge and protocols; destigmatizing and trust building methods; researcher personal responsibility; proper use of Institutional Review Boards; and inclusion of Indigenous researchers and cultural values |
Note. AI/AN = Alaska Native/American Indian; CTN = Clinical Trials Network; NR = Not Reported.
Three articles (Burlew et al., 2020; Perl, 2011; Thomas et al., 2011) detailed collaborations between academic partners and AI/AN tribal entities. These articles posit that research among AI/AN communities represents the earliest efforts within the CTN to consider the role of culture in treatment and the need for community participation (Burlew et al., 2020). The Methamphetamine and Other Drugs in American Indian and Alaska Native Communities project is discussed in two articles (Perl, 2011; Thomas et al., 2011). This project reflects CBPR/TPR and common themes for addressing barriers and establishing successful partnerships, including community driven research; contextualized community knowledge and protocols; destigmatizing and trust building methods; researcher personal responsibility; proper use of institutional review boards; and inclusion of Indigenous researchers and cultural values (Thomas et al., 2011). Further, to support more resources for implementation science for addiction treatment, which can be applied to research in AI/AN communities, a study identified three strategies: (1) developing scientific tools to better understand implementation; (2) building an implementation workforce; and (3) including clinicians at the start to have more relevant research (Perl, 2011).
Three articles (Burlew et al., 2011a; Burlew et al., 2011b; Carroll et al., 2007) included collaborations with NCI, a Tribal SUD treatment center. These articles exemplify how cultural adaptations and CBPR/TPR strategies increase recruitment, treatment access, and retention; influence appropriate methods, measurement, and analyses; and increases substance use treatment efficacy, acceptability, and inclusion for underrepresented ethnic/racial groups within the CTN. Moreover, one article (Carroll et al., 2007) reiterates that the CTN is an optimal avenue to address unmet SUD needs among AI/AN communities—namely, by the AI/AN Special Interest Group of the CTN, who advocates for more Indigenous inclusion at all levels; by challenging stigma and addressing historical trauma; and by the CTN partnering with AI/AN tribes.
4. Discussion
We conducted this scoping review to answer the question: What has been learned about AI/AN participants in CTN research? This scoping review yielded 13 studies on substance use in any AI/AN population, and eight of these were specifically sampling the AI/AN community. For the studies not sampling the AI/AN community, the lack of research could be the result of geographic limitations, ambiguities about identity, and antiquated research practices. This review focused on important factors not included in other CTN scoping reviews (Eghaneyan et al., 2020; Montgomery et al., 2020), such as tribal identity, race, culture, discrimination, and dissemination efforts. Unfortunately, the persistence of SUDs and associated negative sequalae in the AI/AN population follows years of research and implementation of new programs and strategies within and outside the CTN (Blume, 2020; Wendt et al., 2019; Whitesell et al., 2012).
4.1. Tribal identity: Race, culture, and discrimination
The eight AI/AN-specific studies (Campbell et al., 2015; Foley et al., 2010; Forcehimes et al., 2011; Kropp et al., 2013; Kropp et al., 2014; Radin et al., 2012; Radin et al., 2015; Rieckmann et al., 2012) highlight the role of tribal identity, cultural stressors, and discrimination. In fact, unique discriminatory experiences, and stigmatization of AI/AN peoples with substance misuse are embedded in context (e.g., reservations, rurality), socioeconomic factors (e.g., transportation, poverty), and sociopolitical attitudes (e.g., racialization, stigmatizing clinical practices). Further, these factors serve as large barriers to substance use treatment; to implementing culturally derived and adapted methods and treatment; and to adopting evidence-based practices within tribal communities. Moreover, implementing treatment strategies based on limited treatment outcome research with AI/AN people may not only be ecologically invalid, but also could ignore important cultural factors that may contribute to lack of access, acceptability, engagement, and retention.
Issues of identity and tribal enrollment are intricate and longstanding. Since the majority of AI/AN peoples live in urban areas, most are outside the realm of their affiliated Tribes (National Congress of American Indians [NCAI], 2020). Due to the recent recognition that research with AI/AN communities necessitate formal tribal approvals to conduct or participate in research, an unintended consequence could be reduced efforts to conduct AI/AN research (Griffiths et al., 2021; Thomas et al., 2011). Future studies need to be mindful of the role of tribal approvals as well as the distance between the tribes and urban centers where substance use treatment services are largely embedded. In addition, research would benefit from an emphasis on connections (e.g., between researcher and tribe; between tribes and culture). Recognition of these limitations presents an opportunity to reconsider the research approach (e.g., CBPR. TPR) on matters of substance use in the AI/AN population.
Given that the focus of this review is on AI/AN peoples and race is a social construct with myriad assessment approaches, a critical review of how race and tribal identity was determined across studies is imperative. These findings highlight the variability in approaches for assessing and reporting how race and tribal identity are determined in research studies. Given the heterogeneity of the AI/AN population, researchers must assess and report AI/AN cultural identity. Often AI/AN participants are categorized as “other” due to small sample sizes, which is problematic because it erases unique experiences of AI/AN peoples that may impact the research question and limits our understanding of the effect of evidence-based SUD treatments among AI/AN communities (Crouch & Andrew, 2022; Friedman et al., 2023; Haozous et al., 2021). To ensure equitable access and benefit of research for all communities, researchers need to specify how race/ethnicity was assessed during recruitment and operationalized in analyses to increase our ability to compare findings across studies (Haeny & Polimanti, 2022). Namely, researchers should defer to the tribal leadership/community on how to ask questions of tribal enrollment and inquire about blood quantum only if necessary (e.g., biological study).
4.2. Measurement and methodology
Our review revealed that the CTN did inform two important methodological issues for studying AI/AN populations: design and measurement. Several design issues are salient for improving the knowledge base on AI/AN substance use as well. First, when either asking about race/ethnicity or analyzing data, we encourage the CTN to avoid grouping AI/AN peoples into a catch-all category with other groups frequently called “other”. Second, we discourage combining different ethnic/racial groups together in analyses. Third, current methods frequently treat AI/AN peoples as a monolithic group without adequately considering consequential within-group differences due to tribal heritage, geographic location, and a host of other culturally related dynamics. For example, as mentioned earlier, Campbell et al. (2019) found that ethnic (i.e., AI/AN) identity was related to acceptance of a web-based TES intervention. We encourage more within-group analyses that consider rather than ignore the impact of such differences. In areas with a low population of AI/AN people, we recommend partnering with researchers from areas with higher populations of AI/AN people. Finally, we encourage CTN researchers to utilize randomization methods (e.g., blocked randomization) that allow for assessing effect size for specific ethnic/racial groups. Effect size findings may both be suggestive of whether a specific intervention is effective for an AI/AN group and/or may provide pilot data for a larger study specifically among AI/AN peoples.
Of the 13 studies in the review, less than half addressed cultural factors and assessment and three studies (Campbell et al., 2015; Foley et al., 2010; Rieckmann et al., 2012) were specific to cultural/culturally adapted measures. Walls et al. (2019) argue that a certain tension exists between the use of tailored and nontailored measures for AI/AN peoples. However, they recommend including both types when appropriate. Tailored measures may better capture important cultural constructs that nontailored measures fail to include. Tailored measures benefit from psychometric testing to guide future research efforts (e.g., Greenfield et al., 2015; Serier et al., 2019). Although, none of the CTN articles in this scoping review tested measures for nonequivalence, all measures should be evaluated for measurement nonequivalence to ensure they are assessing the same construct similarly across groups of interest (e.g., sex, tribal identity, age, SES). For example, while commonly used measures may adequately assess patterns of use, they may ignore cultural differences such as the amount of drinking that is socially acceptable within a specific AI/AN subgroup or unique dynamics in the etiology of drug use (e.g., historical trauma).
The need for assessing measurement equivalence extends beyond assessing substance use to also include risk and protective factors for AI/AN substance use. For example, findings from Stevens et al. (1999) demonstrated that negatively worded scale items yielded poor psychometric properties within certain AI/AN communities when assessing depression, a known risk factor for substance misuse. However, positively worded items yielded better psychometric properties. Future research on measurement equivalence and other psychometric testing of culturally tailored instruments among AI/AN samples is warranted.
4.3. Limitations and future directions
These findings must be interpreted in the context of the study limitations. The objective of this study was to identify the types of studies conducted within the CTN to garner what knowledge has been gained on substance use and treatment for AI/AN peoples. The aim was to indicate whether the substantial resources delegated to the CTN also benefit AI/AN communities. Given the scope of this review, the findings herein do not include studies outside of the CTN that inform substance use and treatment among the AI/AN population.
We are aware that much research with AI/AN communities has been conducted outside the CTN to address social determinants of health (Blue Bird Jernigan et al., 2020; Dickerson et al., 2020), health equity (Whitesell et al., 2020), health promotion (Walters et al., 2020), harm reduction (Blue Bird Jernigan et al., 2020; Nelson et al., 2022), and utilize randomized control trials (RCT; D’Amico et al., 2020; Dickerson et al., 2021; McDonell et al., 2021; Venner et al, 2021). Notably, practice-based evidence (i.e., traditional practices used for time immemorial) and evidenced-based practices have been integrated in RCTs for motivational interviewing (MI) and cultural treatment of alcohol and other drug problems among urban AI/AN youth (D’Amico et al., 2020); drum-assisted recovery therapy for AI/AN adults with alcohol and other drug problems (Dickerson et al., 2021); culturally congruent CM for alcohol problems among AI/AN adults (McDonell et al., 2021); and culturally tailored MI and the Community Reinforcement Approach for treating SUDs among AI/AN adults (Venner et al, 2021) to highlight some.
Given the body of AI/AN research outside the CTN, we anticipated that we would review multiple themes (i.e., harm reduction, pharmacotherapy, measurement equivalence, substance use outcomes); however, no CTN study informed these themes using an AI/AN sample. Including more harm reduction strategies dispels racist beliefs (e.g., myth of AI/AN biological vulnerability); may reduce substance use and risky behaviors; and improve treatment outcomes (e.g., pharmacotherapy is important in the treatment of SUDs like opioid use disorder). Thus, lack of CTN studies reporting on harm reduction techniques and pharmacotherapy among AI/AN communities could be improved. Importantly, most of the studies included in this review were secondary analyses without the primary aim of studying outcomes among AI/AN people. This is a limitation, because the review did not take into consideration important cultural factors (e.g., tribal identity) in the design of these studies and related analyses and interpretations.
Many of the measures used in treatment studies, including those in the CTN, have not been developed or validated for AI/AN samples. This methodological factor may bias these findings. Multiple studies included AI/AN peoples, but they did not conduct subgroup analyses due to small sample sizes, which results in missed opportunities to provide even descriptive preliminary information on AI/AN people that could be used to inform larger studies.
Leveraging and utilizing research (Dickerson et al., 2020; Whitesell et al., 2020) conducted outside the auspices of the CTN could be beneficial. Future research directions in the CTN could include AI/AN studies on harm reduction and measurement equivalence, and they could aim to develop culturally relevant treatments for AI/AN communities that are tested within rural and urban settings. Additionally, CTN research would benefit from recruiting more AI/AN participants and engaging with more tribes and urban tribal communities. Further, CBPR/TPR approaches include cultural factors and adaptations that greatly influence methods and measurement; access, engagement, and retention; and tribally appropriate dissemination practices. Moreover, culturally congruent strategies also build a research infrastructure within the CTN that has considerable reach, applicable usage, and sustainability (Burlew et al., 2020).
5. Conclusion
Although the inclusion of more AI/AN participants in CTN research is essential, inclusion alone is insufficient. The CTN has a unique opportunity, due to large multisite studies, to address myriad issues that are critical for contributing to the knowledge base on AI/AN substance use and treatment. AI/AN peoples represent thriving communities and have cultural strengths (e.g., traditional practices, language) and unique protective factors (e.g., community connection, tribal identity) that serve as both prevention and traditional medicine (Gone et al., 2019; Rasmus et al., 2019). However, the AI/AN population also has a long and complex history of forced migration, boarding schools, historical trauma, and marginalization (Skewes & Blume, 2019; Wendt et al., 2019). Racist attitudes and discriminatory practices not only affect AI/AN people overtly and contribute to internalized racial stigma, but they also are insidious amalgamations permeating all levels of systems including those related to SUD treatment. However, antiracist research is on the horizon as is a new paradigm that demands an uprooting of racism and lays charge to antiracist science that is actionable (Buchanan et al., 2021). For the CTN, this movement ought to include concerted efforts to allocate funds toward AI/AN research that is led by AI/AN investigators, staff, and community partners; a commitment to culturally appropriate methodology and measures as standard practice; contextual and cultural reporting of ethnicity/race; conducting subgroup analyses and avoiding comparisons with the dominant group for norming (i.e., White); and actively reducing barriers related to design (e.g., sampling the majority society), methods (e.g., one-dimensional data, default comparisons to White outcomes), publication (e.g., lack of diverse authors and reviewers), and dissemination (e.g., inaccessible language, lack of reporting findings to tribal communities) for researchers studying AI/AN populations. Such efforts by the CTN may significantly contribute to the mitigation of AI/AN substance use–related health disparities. We commend the efforts of AI/AN specific research that has been conducted within the CTN, as it embodies robust themes and aspects of research that are lacking within the current paradigm of substance use research. We look forward to continued progress.
Supplementary Material
Highlights:
The Clinical Trials Network is well funded; however, few studies recruit enough AI/AN participants to conduct analyses that would add to treatment outcome knowledge, thus, limiting ability to improve treatment outcomes.
This review identified key constructs not previously examined in Clinical Trials Network scoping reviews of specific participant groups (i.e., Black, Hispanic): Tribal identity, race, culture, and discrimination.
Eight Clinical Trials Network studies specifically sampled American Indian and Alaska Native participants and included critical aspects of Tribal/community based participatory research.
Acknowledgments
The authors would like to thank the CTN Publication Committee for review and approval of this manuscript. Additionally, the authors would like to share their gratitude to the American Indian and Alaska Native participants who gave of their time, culture, and emotional labor to CTN research, which made this review possible. Dogidinh (thank you). Lastly, the authors wish to acknowledge the Native Hawaiian, First Nations, Metis, Inuit, and other Indigenous relatives who also have inhabited Turtle Island (i.e., North America) for time immemorial and who share similar histories, stories, and worldviews to American Indian and Alaska Native peoples. You, too, deserve increased inclusion and representation. Nginh itltthonh (we see you).
Funding Source
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number F32AA029627. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CRediT Authorship Contribution Statement
The authorship team worked collaboratively to develop the protocol, design, and conduct this scoping review. Maria C. Crouch led the scoping review. Melissa C. Funaro conducted and validated the initial and subsequent article searchers. Maria C. Crouch, Kamilla Venner, Dennis C. Wendt, Ann Kathleen Burlew, Paulette Baukol, Tanya Sorrell, and Angela M. Haeny participated in all levels of review (abstract, full text, extraction). In addition, Maria C. Crouch, Kamilla Venner, Dennis C. Wendt, Ann Kathleen Burlew, Paulette Baukol, Melissa C. Funaro, and Angela M. Haeny developed, revised, and approved the final manuscript.
Disclosure Statement
Drs. Crouch, Venner, Wendt, Burlew, Sorrell, Haeny, Ms. Baukol, and Ms. Funaro, declare that they have no actual or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arksey H, & O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Blue Bird Jernigan V, D’Amico EJ, Duran B, & Buchwald D. (2020). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prevention Science, 21(Suppl 1), 65–73. 10.1007/s11121-018-0916-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blume AW (2020). An Indigenous American conceptualization of substance abuse and its treatment. Alcoholism Treatment Quarterly, 39(2). 135–153. 10.1080/07347324.2020.1741330 [DOI] [Google Scholar]
- Brave Heart MYH, Lewis-Fernández R, Beals J, Hasin DS, Sugaya L, Wang S, Grant BF, & Blanco C. (2016). Psychiatric disorders and mental health treatment in American Indians and Alaska Natives: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. Social Psychiatry and Psychiatric Epidemiology, 51(7), 1033–1046. 10.1007/s00127-016-1225-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LS, Kritz S, Muhammad A, Bini EJ, Goldsmith RJ, Robinson J, Alderson D, Hasin DS, & Rotrosen J. (2009). Disparities in health services for HIV/AIDS, hepatitis C virus, and sexually transmitted infections: Role of substance abuse treatment programs. Journal of Addiction Medicine, 3(2), 95–102. 10.1097/ADM.0b013e318190f0e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan NT, Perez M, Prinstein MJ & Thurston IB (2021). Upending racism in psychological science. American Psychologist, 76(7), 1097–1112. 10.1037/amp0000905. [DOI] [PubMed] [Google Scholar]
- Burlew K, Larios S, Suarez-Morales L, Holmes B, Venner K, & Chavez R. (2011). Increasing ethnic minority participation in substance abuse clinical trials: Lessons learned in the National Institute on Drug Abuse’s Clinical Trials Network. Cultural Diversity & Ethnic Minority Psychology, 17(4), 345–356. 10.1037/a0025668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burlew AK, McCuistian C, Lanaway D, Hatch-Maillette M, & Shambley-Ebron D. (2020). One size does not fit all: A NIDA CTN inspired model for community engaged cultural adaptation. Journal of Substance Abuse Treatment, 112S, 28–33. 10.1016/j.jsat.2020.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burlew AK, Weekes JC, Montgomery L, Feaster DJ, Robbins MS, Rosa CL, Ruglass LM, Venner KL, & Wu LT (2011). Conducting research with racial/ethnic minorities: methodological lessons from the NIDA Clinical Trials Network. The American Journal of Drug and Alcohol Abuse, 37(5), 324–332. 10.3109/00952990.2011.596973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calsyn DA, Hatch-Maillette MA, Meade CS, Tross S, Campbell ANC, & Beadnell B. (2013). Gender differences in heterosexual anal sex practices among women and men in substance abuse treatment. AIDS and Behavior, 17(7), 2450–2458. 10.1007/S10461-012-0387-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell ANC, Turrigiano E, Moore M, Miele GM, Rieckmann T, Hu M, Kropp F, Ringor-Carty R, & Nunes EV (2015). Acceptability of a web-based community reinforcement approach for substance use disorders with treatment-seeking American Indians/Alaska Natives. Community Mental Health Journal, 51(4), 393–403. 10.1007/s10597-014-9764-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rosa C, Brown LS Jr., Daw R, Magruder KM, & Beatty L. (2007). Addressing ethnic disparities in drug abuse treatment in the Clinical Trial Networks. Drug and Alcohol Dependence, 90(1), 101–106. 10.1016/j.drugalcdep.2006.12.033 [DOI] [Google Scholar]
- Crouch MC, & Andrew NT (2022). Strategies for inclusivity of American Indian and Alaska Native peoples in behavior therapy research: Within-group diversity, data, and ethical recommendations. the Behavior Therapist, 45(5), 168–174. https://www.abct.org/journals/the-behavior-therapist-journal/ [PMC free article] [PubMed] [Google Scholar]
- Crump AD, Etz K, Arroyo JA, Hemberger N, & Srinivasan S. (2020). Accelerating and strengthening Native American health research through a collaborative NIH initiative. Prevention Science, 21(Suppl 1), 1–4. 10.1007/s11121-017-0854-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JK, Solomon TA, & Muramoto ML (2016). Alcohol use among Native Americans compared to Whites: Examining the veracity of the ‘Native American elevated alcohol consumption’ belief. Drug and Alcohol Dependence, 160, 65–75 10.1016/j.drugalcdep.2015.12.015 [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Dickerson DL, Brown RA, Johnson CL, Klein DJ, & Agniel D. (2020). Motivational interviewing and culture for urban Native American youth (MICUNAY): A randomized controlled trial. Journal of Substance Abuse Treatment, 111, 86–99. 10.1016/j.jsat.2019.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson D, Baldwin JA, Belcourt A, Belone L, Gittelsohn J, Keawe’aimoku Kaholokula J, Lowe J, Patten CA, & Wallerstein N. (2020). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science, 21(Suppl 1), 33–42. 10.1007/s11121-018-0926-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, D’Amico EJ, Klein DJ, Johnson CL, Hale B, Ye F, & Dominguez BX (2021). Drum-assisted recovery therapy for Native Americans (DARTNA): Results from a feasibility randomized controlled trial. Journal of Substance Abuse Treatment, 126, 108439–108439. 10.1016/j.jsat.2021.108439 [DOI] [PubMed] [Google Scholar]
- Eghaneyan BH, Sanchez K, Haeny AM, Montgomery L, Lopez-Castro T, Burlew AK, Rezaeizadeh A, & Killian MO (2020). Hispanic participants in the National Institute on Drug Abuse’s Clinical Trials Network: A scoping review of two decades of research. Addictive Behaviors Reports, 12, 1–9. 10.1016/j.abrep.2020.100287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley K, Pallas D, Forcehimes AA, Houck JM, Bogenschutz MP, Keyser-Marcus L, & Svikis D. (2010). Effect of job skills training on employment and job seeking behaviors in an American Indian substance abuse treatment sample. Journal of Vocational Rehabilitation, 33(3), 181–192. 10.3233/JVR-2010-0526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forcehimes AA, Venner KL, Bogenschutz MP, Foley K, Davis MP, Houck JM, Willie EL, & Begaye P. (2011). American Indian methamphetamine and other drug use in the Southwestern United States. Cultural Diversity & Ethnic Minority Psychology, 17(4), 366–376. 10.1037/a0025431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Hansen H, & Gone JP (2023). Deaths of despair and Indigenous data genocide. Lancet. Advance online publication. 10.1016/S0140-6736(22)02404-7 [DOI] [PubMed] [Google Scholar]
- Gone JP (2022). Community mental health services for American Indians and Alaska Natives: Reconciling evidence-based practice and alter-native psy-ence. Annual Review of Clinical Psychology. Advance online publication. 10.1146/annurev-clinpsy-080921-072950 [DOI] [PubMed] [Google Scholar]
- Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, & Burrage RL (2019). The impact of historical trauma on health outcomes for Indigenous populations in the USA and Canada: A systematic review. The American Psychologist, 74(1), 20–35. 10.1037/amp0000338 [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, & Skewes MC (2021). Belief in the myth of an American Indian/Alaska Native biological vulnerability to alcohol problems among reservation-dwelling participants with a substance use problem. Alcoholism: Clinical and Experimental Research, 45(11), 2309–2321. https://doi-org.libproxy.unm.edu/10.1111/acer.14703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield BL, Hallgren KA, Venner KL, Hagler KJ, Simmons JD, Sheche JN, Homer E, & Lupee D. (2015). Cultural adaptation, psychometric properties, and outcomes of the Native American Spirituality Scale. Psychological Services, 12(2), 123–133. 10.1037/ser0000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield BL, & Venner KL (2012). Review of substance use disorder treatment research in Indian Country: Future directions to strive toward health equity. American Journal of Drug and Alcohol Abuse, 38, 483–492. 10.3109/00952990.2012.702170 [DOI] [PubMed] [Google Scholar]
- Griffiths KE, Blain J, Vajdic CM, & Jorm L. (2021). Indigenous and tribal peoples data governance in health research: A systematic review. International Journal of Environmental Research and Public Health, 18(19), 10318. 10.3390/ijerph181910318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haozous EA, Faan JL, & Soto C. (2021). Urban American Indian and Alaska Native data sovereignty: Ethical issues. American Indian and Alaska Native Mental Health Research, 28(2), 77–99. 10.5820/AIAN.2802.2021.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeny AM, & Polimanti R. (2022). From evolutionary history to the concepts of race and ancestry: Shifting our perspective in clinical research. Biological Psychiatry, e1-e2. Advance online publication. 10.1016/j.biopsych.2022.02.953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Hirchak KA, Herron J, Lyons AJ, Alcover KC, Shaw J, Kordas G, Dirks LG, Jansen K, Avey J, Lillie K, Donovan D, McPherson SM, Dillard D, Ries R, Roll J, Buchwald D, & HONOR Study Team. (2021). Effect of incentives for alcohol abstinence in partnership with 3 American Indian and Alaska Native communities: A randomized clinical trial. JAMA Psychiatry, 78(6), 599–606. 10.1001/jamapsychiatry.2020.4768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp F, Lilleskov M, Richards J, Somoza E, & Ctn0033-Ot-4 Team. (2014). Client and provider views on access to care for substance-using American Indians: Perspectives from a Northern Plains urban clinic. American Indian and Alaska Native Mental Health Research, 21(2), 43–65. 10.5820/aian.2102.2014.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp F, Somoza E, Lilleskov M, Moccasin MG, Moore M, Lewis D, Boetel B, Smith C, & Winhusen T. (2013). Characteristics of Northern Plains American Indians seeking substance abuse treatment in an urban, non-tribal clinic: A descriptive study. Community Mental Health Journal, 49(6), 714–721. 10.1007/s10597-012-9537-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loree AM, Yeh HH, Satre DD, Kline-Simon AH, Yarborough B, Haller IV, Campbell CI, Lapham GT, Hechter RC, Binswanger IA, Weisner C, & Ahmedani BK (2019). Psychiatric comorbidity and Healthcare Effectiveness Data and Information Set (HEDIS) measures of alcohol and other drug treatment initiation and engagement across seven health care systems. Substance Abuse, 40(3), 311–317. 10.1080/08897077.2018.1545727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malcarne VL, Chavira DA, Fernandez S, & Liu P. (2006). The scale of ethnic experience: Development and psychometric author section properties. Journal of Personality Assessment, 86(2), 150–161. 10.1207/s15327752jpa8602_04 [DOI] [PubMed] [Google Scholar]
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, & Lefebvre C. (2016). PRESS peer review of electronic search strategies: 2015 Guideline Statement. Journal of Clinical Epidemiology, 75, 40–46. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- Montgomery L, Burlew AK, Haeny AM, & Jones CA (2020). A systematic scoping review of research on Black participants in the National Drug Abuse Treatment Clinical Trials Network. Psychology of Addictive Behavior, 34(1), 117–127. 10.1037/adb0000483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Congress of American Indians. (2020). Tribal nations and the United States: An introduction. https://www.ncai.org/about-tribes [Google Scholar]
- Nelson L, Squetemkin-Anquoe A, Ubay T, King V, Taylor E, Masciel K, Black Bear L, Buffalomeat S, Duffing-Romero X, Mahinalani-Garza C, Clifasefi S, & Collins S. (2022). Content analysis informing the development of adapted harm reduction talking circles (HaRTC) with urban American Indians and Alaska Natives experiencing alcohol use disorder. International Journal of Indigenous Health, 17(2), 33–50. 10.32799/ijih.v17i2.36677 [DOI] [Google Scholar]
- Novins DK, Croy CD, Moore LA, & Rieckmann T. (2016). Use of evidence-based treatments in substance abuse treatment programs serving American Indian and Alaska Native communities. Drug and Alcohol Dependence, 161, 214–221. 10.1016/j.drugalcdep.2016.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, . . . Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372, 1–9. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perl HI (2011). Addicted to discovery: Does the quest for new knowledge hinder practice improvement? Addictive Behaviors, 36(6), 590–596. 10.1016/j.addbeh.2011.01.027 [DOI] [PubMed] [Google Scholar]
- Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, & Khalil H. (2020). Chapter 11: Scoping reviews. In Aromataris E. & Munn Z. (Eds.), Joanna Briggs Institute manual for evidence synthesis. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- Radin SM, Banta-Green CJ, Thomas LR, Kutz SH, & Donovan DM (2012). Substance use, treatment admissions, and recovery trends in diverse Washington state tribal communities. The American Journal of Drug and Alcohol Abuse, 38(5), 511–517. 10.3109/00952990.2012.694533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radin SM, Kutz SH, La Marr J, Vendiola D, Vendiola M, Wilbur B, Thomas LR, & Donovan DM (2015). Community perspectives on drug/alcohol use, concerns, needs, and resources in four Washington state tribal communities. Journal of Ethnicity in Substance Abuse, 14(1), 29–58. 10.1080/15332640.2014.947459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmus SM, Whitesell NR, Mousseau A, & Allen J. (2020). An intervention science to advance underrepresented perspectives and Indigenous self-determination in health. Prevention Science, 21(Suppl 1), 83–92. 10.1007/s11121-019-01025-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmus SM, Trickett E, Charles B, John S, & Allen J. (2019). The Qasgiq Model as an Indigenous intervention: Using the cultural logic of contexts to build protective factors for Alaska Native suicide and alcohol misuse prevention. Cultural Diversity & Ethnic Minority Psychology, 25(1), 44–54. 10.1037/cdp0000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieckmann T, McCarty D, Kovas A, Spicer P, Bray J, Gilbert S, & Mercer J. (2012). American Indians with substance use disorders: Treatment needs and comorbid conditions. The American Journal of Drug and Alcohol Abuse, 38(5), 498–504. 10.3109/00952990.2012.694530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serier KN, Venner KL, & Sarafin RE (2019). Evaluating the validity of the DSM-5 alcohol use disorder diagnostic criteria in a sample of treatment-seeking Native Americans. Journal of Addiction Medicine, 13(1), 35–40. 10.1097/ADM.0000000000000452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skewes MC, & Blume AW (2019). Understanding the link between racial trauma and substance use among American Indians. American Psychologist, 74(1), 88–100. 10.1037/amp0000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto C, West AE, Ramos GG, & Unger JB (2022). Substance and behavioral addictions among American Indian and Alaska Native populations. International Journal of Environmental Research and Public Health, 19(5), 2974. 10.3390/ijerph19052974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens KA, West II, Hallgren KA, Mollis B, Ma K, Donovan DM, Stuvek B, & Baldwin L. (2020). Service utilization and chronic condition outcomes among primary care patients with substance use disorders and co-occurring chronic conditions. Journal of Substance Abuse Treatment, 112, 49–55. 10.1016/j.jsat.2020.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J, Cornell C, Story M, French S, Levin S, Becenti A, Reid R. (1999). Development of a questionnaire to assess knowledge, attitudes, and behaviors in American Indian children. The American Journal of Clinical Nutrition, 69(4), 773s–781s. 10.1093/ajcn/69.4.773S [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2019). National Survey on Drug Use and Health: Annual national report. U.S. Department of Health and Human Services. https://www.samhsa.gov/data/report/2019-nsduh-annual-national-report [Google Scholar]
- Thomas LR, Rosa C, Forcehimes A, & Donovan DM (2011). Research partnerships between academic institutions and American Indian and Alaska Native Tribes and organizations: Effective strategies and lessons learned in a multisite CTN study. The American Journal of Drug and Alcohol Abuse, 37(5), 333–338. 10.3109/00952990.2011.596976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, . . . Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Venner KL, Serier K, Sarafin R, Greenfield BL, Hirchak K, Smith JE, & Witkiewitz K. (2021). Culturally tailored evidence-based substance use disorder treatments are efficacious with An American Indian Southwest Tribe: An open-label pilot-feasibility randomized controlled trial. Addiction, 116(4), 949–960. 10.1111/add.15191 [DOI] [PubMed] [Google Scholar]
- Walls ML, Whitesell NR, Barlow A, & Sarche M. (2019). Research with American Indian and Alaska Native populations: Measurement matters. Journal of Ethnicity in Substance Abuse, 18(1), 129–149. 10.1080/15332640.2017.1310640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Johnson-Jennings M, Stroud S, Rasmus S, Charles B, John S, Allen J, Kaholokula JK, Look MA, de Silva M, Lowe J, Baldwin JA, Lawrence G, Brooks J, Noonan CW, Belcourt A, Quintana E, Semmens EO, & Boulafentis J. (2020). Growing from our roots: Strategies for developing culturally grounded health promotion interventions in American Indian, Alaska Native, and Native Hawaiian communities. Prevention Science, 21(Suppl 1), 54–64. 10.1007/s11121-018-0952-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendt DC, Hartmann WE, Allen JA, Burack JA, Charles B, D’Amico E, Dell CA, Dickerson DL, Donovan DM, Gone JP, O’Connor RM, Radin SM, Rasmus SR, Venner KL, & Walls ML (2019). Substance use research with Indigenous communities: Exploring and extending foundational principles of community psychology. American Journal of Community Psychology, 64(1–2), 146–158. 10.1002/ajcp.12363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Crow CB, Mitchell CM, & Novins DK (2012). Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38(5), 376–382. 10.3109/00952990.2012.694527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Mousseau A, Parker M, Rasmus S, & Allen J. (2020). Promising practices for promoting health equity through rigorous intervention science with Indigenous communities. Prevention Science, 21(Suppl 1), 5–12. 10.1007/s11121-018-0954-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Ghitza UE, Batch BC, Pencina MJ, Rojas LF, Goldstein BA, Schibler T, Dunham AA, Rusincovitch S, & Brady KT (2015). Substance use and mental diagnoses among adults with and without type 2 diabetes: Results from electronic health records data. Drug and Alcohol Dependence, 156, 162–169. 10.1016/j.drugalcdep.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.