Abstract
Background:
The combination of opioid misuse and cigarette smoking contributes to increased morbidity and mortality compared to each substance use alone. We estimated the incidence of opioid misuse for persons who currently or formerly smoked versus never smoked.
Methods:
Data came from the 2015-2020 National Surveys on Drug Use and Health cross-sectional surveys of US civilians aged 12+ (n=315,661). Weighted opioid misuse incidence and average time between cigarette use initiation and opioid misuse initiation were calculated annually by smoking status. Logistic regression models tested time trends in incidence by smoking status.
Results:
Overall, 0.75% of persons initiated opioid misuse per year; opioid misuse incidence was 1.35% for those who currently smoked cigarettes, 0.54% for those who formerly smoked, and 0.67% for those who never smoked. For persons who currently smoked and misused opioids (1.50%), 95.08% smoked prior to opioid use. The average time between smoking followed by opioid misuse was 12.93 years and for opioid misuse followed by smoking was 4.36 years. Persons who currently smoked were more likely to initiate opioid misuse than those who had never smoked (AOR=1.81, 95% 1.60, 2.06). There was a decrease in the opioid misuse incidence over time (AOR=0.90; 95% CI: 0.85, 0.92), which did not differ by smoking status.
Conclusions:
Persons who currently smoked cigarettes, relative to those who never smoked, were more likely to initiate opioid misuse. As most individuals smoked before opioid misuse, it may be useful for primary prevention efforts to decrease opioid misuse initiation by focusing on smoking status.
Keywords: Tobacco Use, Smoking, Opioid misuse, Opioid misuse, Epidemiology
1. Introduction
With the ongoing opioid epidemic now in its fourth wave (Ciccarone, 2021) and high morbidity and mortality due to cigarette smoking (U.S. Department of Health and Human Services et al., 2020), it is critical to understand how population-level interactions between opioid misuse and cigarette smoking might best inform public health programs. People who smoke cigarettes experience disparities in opioid misuse and related consequences (Parker et al., 2018). Individuals with versus without cigarette use have been estimated to be at least twice as likely to misuse opioids (Parker and Villanti, 2019; Zale et al., 2015) and smoking prevalence is much higher for persons with versus without opioid misuse (65% versus 26%; Parker et al., 2020). The combination of nicotine and opioid misuse leads to an increased risk of premature mortality compared to use of either substance alone (Kertesz et al., 2012).
The strong relationship between opioids and nicotine may be due to the overlapping and long-lasting effects of nicotine and opioids in the brain (Hadjiconstantinou and Neff, 2011; Kishioka et al., 2014). Treatment of nicotine to the brain may sensitize and augment the reinforcing effects of opioids (Vihavainen et al., 2008) and tolerance and/or withdrawal can happen from chronic exposure to nicotine or opioids (Kohut, 2017). Nicotine depresses the central nervous system and may also decrease the effects of opioids (e.g., reduced pain relief) (National Institute on Drug Abuse, 2018).
Efforts to understand factors related to opioid misuse initiation are critical to reduce opioid misuse and the harms of opioid misuse across the lifespan as the peak risk of first opioid misuse and transition from initiation to opioid use disorder are seen in mid-adolescence (Parker and Anthony, 2015). The number of overall past year initiates of opioid misuse has declined from 2.1 million people in 2015 to 1.6 million people in 2019 in the United States (US) (United States, 2020) but it is not clear that this decline has been the same for those who are particularly vulnerable to opioid misuse such as people using cigarettes. As described above, there is a connection between cigarette use and opioid use, and cigarette use has been linked to the initiation of use or misuse of other substance (e.g., Weinberger et al., 2017); however, research has not yet examined the association of cigarette use with opioid misuse incidence.
The aim of this study was to determine the incidence of opioid misuse for US individuals who currently or formerly smoked cigarette versus never smoked. We hypothesized that opioid misuse incidence would be most likely for persons who currently smoked followed by those who formerly smoked and both would be higher than the incidence of those who never smoked. Due to the increasing prevalence of electronic cigarette (e-cigarettes/vaping) use among youth and young adults (United States Department of Health and Human Services, 2016) and the documented association between e-cigarettes and opioid misuse (e.g., Conway et al., 2017; Parker and Villanti, 2019), an exploratory aim investigated differences in opioid misuse for persons who ever vaped nicotine and those who vaped nicotine recently.
2. Methods
2.1. Data Source & Sample
Data were harnessed from annual, cross-sectional, nationally representative samples of the US National Survey on Drug Use and Health (NSDUH) from 2015-2020 (individuals aged 12+; total sample combined n=315,661; 2020 exploratory sample n=32,893). The NSDUH employs multistage probability sampling and audio computer-assisted self-interviewing (Center for Behavioral Health Statistics and Quality, 2018).
2.2. Measures
2.2.1. Outcome: Incidence of opioid misuse
Opioid misuse was defined as any misuse of opioid prescription drugs or heroin. Respondents in a specific survey year were considered to have initiated opioid misuse if they started to use opioid prescription drugs to get high and for related feelings and experiences, or otherwise outside the boundaries of a prescriber’s intent (Parker and Anthony, 2015) and/or started heroin use in the past two years as reported at the interview for that year. Based on the NSDUH detailed tables and annual reports, “past year initiation” was calculated as the difference between the year of first opioid misuse and the survey year which was verified with any opioid misuse in the past 30 days (Substance Abuse and Mental Health Services Administration, 2017).
2.2.2. Exposure: Cigarette Smoking
Three mutually exclusive cigarette smoking status groups were determined: current smoking, former smoking, and never smoking. Among those with lifetime smoking (≥100 lifetime cigarettes), current smoking was classified as smoking ≥1 cigarette in the past month and former smoking was classified as not smoking any cigarettes in the past 12 months. Respondents who smoked within the past 12 months, but <1 cigarette in the past month were included in the never smoking group along with persons who smoked <100 lifetime cigarettes. Definitions of lifetime smoking (smoked ≥100 lifetime cigarettes) and never smoking (smoked <100 lifetime cigarettes) were consistent with the Centers of Disease Control and Prevention’s definitions (Creamer, 2019).
2.2.3. Vaping
Beginning in 2020, the NSDUH began asking questions about vaping. In the codebook, lifetime vaping was defined as ever vaping nicotine or tobacco with an e-cigarette or a vaping device. Vaping was categorized into three mutually exclusive groups by recency of use (within the past month, within the past 12 months but not the past month, and more than 12 months ago) (United States, 2021).
2.2.4. Background characteristics
Sociodemographic factors included: sex (male, female), age (18-25 years, 26-34 years, 35-49, 50+ years), race/ethnicity (Non-Hispanic (NH) White, NH Black, Hispanic, NH Other [NH Native American/Alaskan Native, NH Hawaiian/Pacific Islander, NH Asian, NH more than one race]), and annual household income (<$20,000, $20,000-$49,999, $50,000-$74,999, ≥$75,000).
Past-month alcohol and cannabis use were additional covariates due to strong associations of these variables with opioid misuse and lower cigarette quit ratios (e.g., Weinberger et al., 2019). Past-month alcohol and cannabis use were defined like opioid misuse (i.e., any use in the past 30 days).
2.2.5. Statistical Analyses
First, the weighted incidence of opioid misuse and average time between cigarette smoking initiation and opioid misuse initiation were calculated annually by smoking status (i.e., current, former, never). Next, logistic regression models were conducted for the outcome, opioid misuse incidence, given the exposure, smoking status, for all survey years. Then, we tested time trends in opioid misuse incidence by smoking status from 2015-2020. Additional logistic regression models examined linear time trends of opioid misuse with 1) continuous year as the predictor stratified by smoking status, and 2) a two-way interaction between year and smoking status. Models with year-by-cigarette smoking status assessed differential time trends among smoking statuses. Finally, in postestimation exploratory analyses, (1) adjusted odds ratios (AOR) for 2015-2019 and 2020 were estimated separately to determine whether there were differences in this year due to COVID-19 and/or differences in survey procedures, and (2) logistic regression models were conducted for vaping as the exposure in 2020. These analyses began with unadjusted models followed by models that adjusted for covariates found in Table 1; they were conducted in Stata version 17 to account for complex sampling (Stata Corp, 2020).
Table 1.
Opioid misuse incidence by cigarette smoking status (weighted %, standard error).a Data from the 2015-2020 National Survey on Drug Use and Health (individuals age 12+, n=315,661).
| Never cigarette smoking (n=229,381) weighted %, standard error | Former cigarette smoking (n=38,203) weighted %, standard error | Current cigarette smoking (n=48,077) weighted %, standard error | ||||
|---|---|---|---|---|---|---|
| Background characteristic | ||||||
|
| ||||||
| Total sample | ||||||
| Sex/Gender | ||||||
| Female | 54.93 | 0.171 | 44.83 | 0.389 | 45.62 | 0.391 |
| Male | 44.07 | 0.171 | 55.17 | 0.389 | 54.38 | 0.391 |
| Age, years | ||||||
| 12-17 | 13.90 | 0.100 | 0.16 | 0.014 | 0.71 | 0.023 |
| 18-25 | 15.38 | 0.112 | 3.26 | 0.086 | 12.18 | 0.162 |
| 26-34 | 14.26 | 0.110 | 10.14 | 0.175 | 20.87 | 0.292 |
| 35-49 | 20.87 | 0.143 | 21.79 | 0.281 | 29.27 | 0.299 |
| 50+ | 35.59 | 0.233 | 64.65 | 0.365 | 36.97 | 0.426 |
| Race/ethnicity | ||||||
| White, non-Hispanic | 56.59 | 0.295 | 77.27 | 0.387 | 69.49 | 0.442 |
| Black, non-Hispanic | 13.49 | 0.211 | 6.82 | 0.212 | 12.49 | 0.328 |
| Other, non-Hispanic | 9.91 | 0.116 | 5.07 | 0.145 | 6.50 | 0.218 |
| Hispanic | 20.01 | 0.223 | 10.85 | 0.276 | 11.52 | 0.271 |
| Annual Income | ||||||
| <$20,000 | 15.26 | 0.173 | 11.22 | 0.198 | 25.61 | 0.367 |
| $20,000-$49,999 | 27.40 | 0.166 | 29.52 | 0.313 | 34.72 | 0.347 |
| $50,000-$74,999 | 15.34 | 0.119 | 17.48 | 0.297 | 14.97 | 0.258 |
| $75,000+ | 41.99 | 0.267 | 41.78 | 0.361 | 24.70 | 0.409 |
| Past-month alcohol use | 45.59 | 0.196 | 60.20 | 0.414 | 60.98 | 0.393 |
| Past-month cannabis use | 6.54 | 0.073 | 9.64 | 0.179 | 24.17 | 0.286 |
Percentages may not sum to 100% due to rounding.
3. Results
Of the entire sample, 61.36% reported never smoking, 21.11% reported former smoking, and 17.53% reported current smoking. Persons with never smoking were a majority female (55.86%) while persons with a smoking history were a majority male (between 54%-55%)(Table 1).
Overall, 0.75% of persons initiated opioid misuse per year. From 2015-2020, the overall incidence of opioid misuse was 0.67% for those with never smoking, 1.35% for those who currently smoked, and 0.54% for those who formerly smoked (Figure 1). For persons who both currently smoked and initiated opioid misuse (1.50%), 95.08% smoked prior to opioid misuse. The average time between smoking followed by incident opioid misuse was 12.93 years and for those who first misused opioids followed by smoking was 4.36 years.
Figure 1.
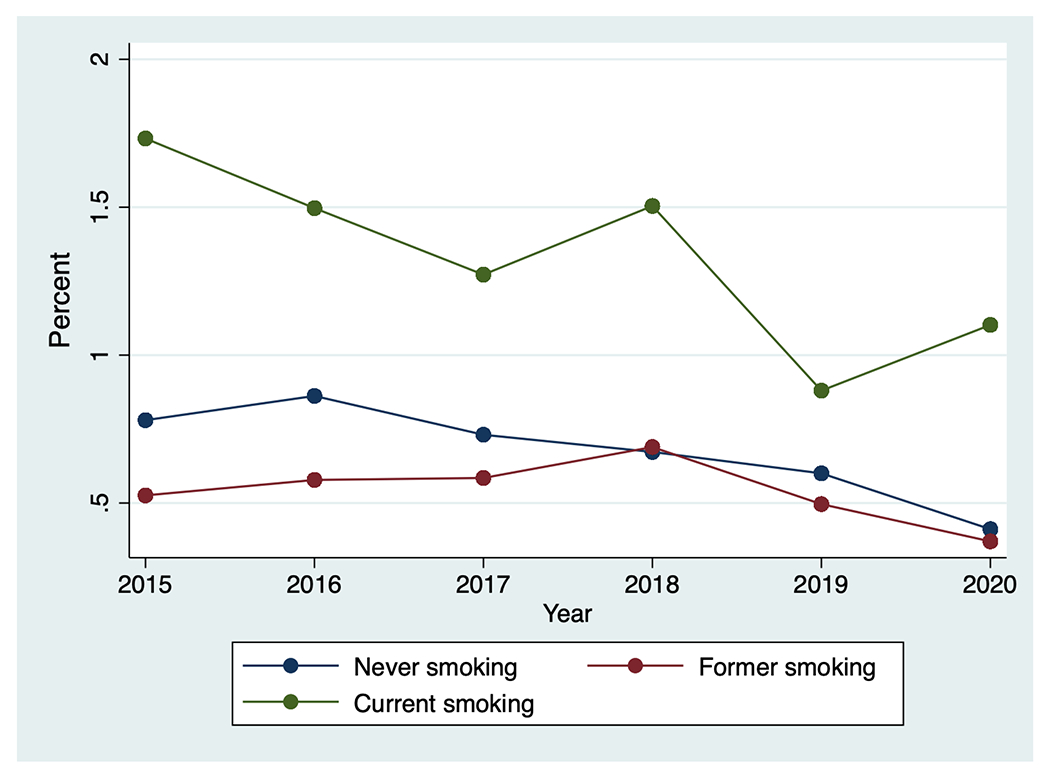
Opioid misuse incidence by cigarette smoking status. Data from the 2015-2020 National Survey on Drug Use and Health (individuals age 12+, n=315,661).
Compared to those who never smoked cigarettes, those who currently smoked were more likely to misuse opioids (AOR=1.81, 95% 1.60, 2.06) and those who formerly smoked were as likely to misuse opioids (AOR=1.15, 95% CI: 0.94, 1.40; see Supplemental Table). There was a statistical difference between those who formerly versus currently smoked (p<0.001) such that adults who currently smoked were more likely to initiate opioid misuse compared to adults who formerly smoked. Additionally, there was a decrease in the incidence of opioid misuse over time (AOR=0.90; 95% CI: 0.85, 0.92), which did not differ by smoking status.
In the first postestimation exploratory analyses, current and former smoking estimates for 2015-2019 and 2020 separately were similar to models including all survey years as evidenced by overlapping 95% CI (AOR=1.73, 95% CI: 1.50, 1.99; AOR=1.15, 95% CI: 0.92, 1.44 vs. AOR=2.19, 95% CI: 1.14, 4.23; AOR=1.14, 95% CI: 0.56, 2.35; respectively).
In the second postestimation exploratory analyses, there were no significant differences for opioid misuse incidence in logistic regression models for vaping as the exposure in 2020. Compared with persons who vaped more than 12 months ago, those who vaped within the past month or within the past 12 months but not the past month were just as likely to initiate opioid misuse (AOR=2.40, 95% CI: 0.91, 6.35; AOR=1.49, 95% CI: 0.53, 4.16, respectively; p>0.05).
4. Discussion
Among US individuals, the incidence of opioid misuse decreased from 2015-2020 with no differences in the decrease by cigarette smoking status. However, persons who currently smoked cigarettes were more likely to initiate opioid misuse than those who never smoked. Importantly, most individuals smoked before misusing opioids with a longer duration of misuse when smoking preceded opioid misuse. Persons who vaped were just as likely to initiate opioid misuse than those who had not vaped.
We know the prevalence of opioid misuse is at least two times higher for persons with versus without cigarette smoking (Parker et al., 2019; Zale et al., 2015), the findings herein extend this literature to show that not only are persons with cigarette smoking more likely to have opioid misuse, but they are more likely to start misusing opioids than persons who do not smoke. This highlights an additional and novel disparity around opioid misuse based on smoking status not previously examined in the literature.
An exploratory analysis of young adults (18-25 years old) found that those who currently smoked had the highest odds of misuse and those who never smoked had lower odds of misuse (Romberg et al., 2019). Our findings in a sample of individuals 12 and older showed a difference in the incidence of opioid misuse between current and former smoking, but no difference between former and never smoking. A study of adults age 50 and above found significantly higher tobacco use for those with opioid misuse compared to those with prescribed use of opioids (Han et al., 2019). While tobacco use was not significant in their adjusted models, we found a significant association between cigarette smoking and incident opioid misuse, even after adjusting for other characteristics.
This study has several strengths and limitations. Study findings are generalizable to the US population 18 years or older and we were able to examine opioid misuse incidence by smoking status over time (2015-2020). Yet, the self-reported nature of opioid misuse could reflect recall or social acceptability bias. The opioid incidence variable was calculated without the month of first use, so estimates are likely not precise. Estimates for past year initiation of cigarette smoking with this method were compared to the NSDUH detailed tables, which show consistent results (United States, 2020). Further, we were unable to include consistent measures of health across the entire sample due to the limitations of the data. Future studies should consider additional covariates and subgroup analyses (e.g., depression, race/ethnicity, sex/gender, age, other tobacco product use).
There was a clear association between opioid misuse incidence and current cigarette smoking with opioid misuse more likely to occur among those who currently smoked (vs. never smoked), regardless of vaping status. Further, cigarette smoking most often occurred before opioid misuse and opioids were misused for an average of 10 years when initiation happened after cigarette smoking initiation. While the incidence of opioid misuse has decreased across all smoking statuses, we offer evidence for a need to focus on persons who smoke to help continue the trajectory of decreased opioid misuse incidence. Cessation of smoking for individuals with opioid misuse or opioid use disorder has been less than half the rate seen among those without opioid misuse or OUD (Parker et al., 2020). Smoking cessation has been associated with higher opioid misuse abstinence for persons in addiction treatment and in recovery (Prochaska et al., 2004). Although causal analyses are needed to make recommendations for interventions, smoking cessation or preventing smoking initiation may help decrease the number of persons who misuse opioids over time. Targeting individuals who smoke cigarettes in primary prevention efforts could be effective in reducing the incidence of opioid misuse.
Supplementary Material
HIGHLIGHTS.
We examined opioid misuse incidence by cigarette smoking status.
Opioid misuse incidence was higher for persons who currently smoked vs did not smoke.
Persons who smoked were more likely to start opioid misuse vs those who never smoked.
There was a decrease in opioid misuse incidence over time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Center for Behavioral Health Statistics and Quality, 2018. 2017. National Survey on Drug Use and Health: Methodological summary and definitions. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Ciccarone D, 2021. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Current Opinion in Psychiatry 34, 344–350. 10.1097/YCO.0000000000000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Green VR, Kasza KA, Silveira ML, Borek N, Kimmel HL, Sargent JD, Stanton C, Lambert E, Hilmi N, Reissig CJ, Jackson KJ, Tanski SE, Maklan D, Hyland AJ, Compton WM, 2017. Co-occurrence of tobacco product use, substance use, and mental health problems among adults: Findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study. Drug and Alcohol Dependence 177, 104–111. 10.1016/j.drugalcdep.2017.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer MR, 2019. Tobacco Product Use and Cessation Indicators Among Adults — United States, 2018. MMWR Morb Mortal Wkly Rep 68. 10.15585/mmwr.mm6845a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjiconstantinou M, Neff NH, 2011. Nicotine and endogenous opioids: Neurochemical and pharmacological evidence. Neuropharmacology, Trends in Neuropharmacology: In Memory of Erminio Costa 60, 1209–1220. 10.1016/j.neuropharm.2010.11.010 [DOI] [PubMed] [Google Scholar]
- Han BH, Sherman SE, Palamar JJ, 2019. Prescription opioid misuse among middle-aged and older adults in the United States, 2015–2016. Preventive Medicine 121, 94–98. 10.1016/j.ypmed.2019.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Khodneva Y, Richman J, Tucker JA, Safford MM, Jones B, Schumacher J, Pletcher MJ, 2012. Trajectories of Drug Use and Mortality Outcomes Among Adults Followed Over 18 Years. J Gen Intern Med 27, 808–816. 10.1007/s11606-011-1975-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishioka S, Kiguchi N, Kobayashi Y, Saika F, 2014. Nicotine Effects and the Endogenous Opioid System. Journal of Pharmacological Sciences 125, 117–124. 10.1254/jphs.14R03CP [DOI] [PubMed] [Google Scholar]
- Kohut SJ, 2017. Interactions between nicotine and drugs of abuse: A review of preclinical findings. Am J Drug Alcohol Abuse 43, 155–170. 10.1080/00952990.2016.1209513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse, 2018. Prescription CNS Depressants DrugFacts [WWW Document]. National Institute on Drug Abuse. URL https://www.drugabuse.gov/publications/drugfacts/prescription-cns-depressants (accessed 3.24.21). [Google Scholar]
- Parker MA, Anthony JC, 2015. Epidemiological evidence on extra-medical use of prescription pain relievers: transitions from newly incident use to dependence among 12–21 year olds in the United States using meta-analysis, 2002–13. PeerJ 3. 10.7717/peerj.1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Sigmon SC, Villanti AC, 2019. Higher smoking prevalence among United States adults with co-occurring affective and drug use diagnoses. Addict Behav 99, 106112. 10.1016/j.addbeh.2019.106112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Streck JM, Sigmon SC, 2018. Associations between opioid and nicotine dependence in nationally representative samples of United States adult daily smokers. Drug Alcohol Depend 186, 167–170. 10.1016/j.drugalcdep.2018.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Villanti AC, 2019. Patterns and frequency of current e-cigarette use in United States adults. Subst Use Misuse 54, 2075–2081. 10.1080/10826084.2019.1626433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Weinberger AH, Villanti AC, 2020. Quit ratios for cigarette smoking among individuals with opioid misuse and opioid use disorder in the United States. Drug and Alcohol Dependence 108164. 10.1016/j.drugalcdep.2020.108164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Delucchi K, Hall SM, 2004. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of Consulting and Clinical Psychology 72, 1144–1156. 10.1037/0022-006X.72.6.1144 [DOI] [PubMed] [Google Scholar]
- Romberg AR, Miller Lo EJ, Barton AA, Xiao H, Vallone DM, Hair EC, 2019. Cigarette smoking, prescription opioid use and misuse among young adults: An exploratory analysis. Preventive Medicine 129, 105845. 10.1016/j.ypmed.2019.105845 [DOI] [PubMed] [Google Scholar]
- Stata Corp, 2020. Stata Statistical Software: Release 17. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2017. Population Data / NSDUH Reports, Special Issue: Behavior change, health, and health disparities 2016. [Google Scholar]
- United States, 2021. 2020 National Survey on Drug Use and Health Public Use File Codebook. Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- United States, 2020. Results from the 2019 National Survey on Drug Use and Health: Detailed Tables. Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- United States Department of Health and Human Services, 2016. E-cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Rockville, MD. [Google Scholar]
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, Office on Smoking and Health, 2020. Smoking Cessation: A Report of the Surgeon General - Executive Summary. Atlanta, GA. [Google Scholar]
- Vihavainen T, Piltonen M, Tuominen RK, Korpi ER, Ahtee L, 2008. Morphine-nicotine interaction in conditioned place preference in mice after chronic nicotine exposure. Eur J Pharmacol 587, 169–174. 10.1016/j.ejphar.2008.03.028 [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Pacek LR, Wall MM, Gbedemah M, Lee J, Goodwin RD, 2019. .Cigarette smoking quit ratios among adults in the USA with cannabis use and cannabis use disorders, 2002–2016. Tobacco Control. 10.1136/tobaccocontrol-2018-054590 [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, Esan H, Galea S, Erlich D, Goodwin RD, 2017. Cigarette Smoking Is Associated With Increased Risk of Substance Use Disorder Relapse: A Nationally Representative, Prospective Longitudinal Investigation. J Clin Psychiatry 78, 152–160. 10.4088/JCP.15m10062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zale EL, Dorfman ML, Hooten WM, Warner DO, Zvolensky MJ, Ditre JW, 2015. Tobacco smoking, nicotine dependence, and patterns of prescription opioid misuse: Results from a nationally representative sample. Nicotine Tob Res 17, 1096–1103. 10.1093/ntr/ntu227 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


