Abstract
Due to structural racism and pathways between racism and health, Black and Native American people die at younger ages than white people. This means that those groups are likely to experience deaths of family members at younger ages. Evidence is mixed about whether family deaths affect educational attainment. We aim to 1) estimate the prevalence of family deaths by age and race 2) estimate the effect of a family death on later educational attainment and 3) analyze whether the effect of a family death varies by age, socioeconomic status, gender, and race. The National Longitudinal Study of Adolescent to Adult Health (Add Health) is a nationally representative sample of U.S. adolescents in grades 7–12 at baseline in 1994–1995. Add Health has a large and racially diverse sample and records family deaths across the entire life course starting from birth. Participants were included in this analysis if they reported their educational attainment in Wave IV (N=14,796). The racial group with the lowest proportion experiencing a sibling or parent death in the first 23 years of their lives was white participants (11.7%), followed by Asian (12.5%), Hispanic (15.0%), Black (24.3%) and Native American participants (30.3%). In adjusted models, those who experienced a family death had 0.60 times the odds (95% CI 0.51 – 0.71) of achieving a bachelor’s degree compared to those without a family death. Mother deaths, father deaths, and sibling deaths were each harmful for obtaining a college degree and their effects were similar in magnitude. The age range when the effect of a family death was strongest was 10 to 13 years old (OR=0.52 95% CI 0.40 – 0.67). The effect of a family death on college degree attainment did not vary by baseline parent education, participant sex, or race/ethnicity.
Keywords: bereavement, mortality, Social determinants of health, Health Disparities, Life Course, family death, population health, structural racism
Background
Mortality is an important measure of population health (Murray et al., 2000), with stark racial differences in the United States. Black and Native American people have a higher risk of dying than white people from birth until age 54 (Centers for Disease Control and Prevention, 2017), ages when death is more preventable. Because of this, they are also likely to be younger when family members die. From birth through midlife, Black people are more likely than white people to live through the death of a sibling, mother, or father (Umberson et al., 2017). Family deaths among Native Americans have been found to be a similarly elevated but with large confidence intervals due to small sample sizes (Thyden et al., 2020).
Premature mortality represents a form of structural racism that reverberates across the social system to adversely affect health across the life course. Structural racism “refers to the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice.” (p. 1453) (Bailey et al., 2017). Early death is one outcome caused by racial discrimination and racial inequity. Mortality is usually conceptualized as a finite outcome at the end of a lifetime of exposures. However, we argue that mortality should also be conceptualized as an exposure. This means that exposure to the death of a child’s family member then in turn influences social determinants of later health (such as education) (Braveman and Gottlieb, 2014), as well as population health and health inequity in the longer run (World Health Organization, 2008).
If Black and Native American people experience deaths of family members more often early in life, and if family deaths negatively affect educational attainment, then that link is a structural problem within the system of education. Perhaps right now there are “color-blind” policies in place that are not intended to create unequal harm for minoritized groups but have that effect nevertheless (Bailey et al., 2017). For instance, perhaps primary education systems perceive a grieving student as an underperforming student and place them in a lower academic track which affects their long-term educational trajectory. Or perhaps higher education admissions systems are overly punitive in how they perceive short-term lapses in academic performance which could be due to a family death.
It is important to pay attention to the racial distribution of an exposure in order to understand causes of racial disparities at the population level (Ward et al., 2018). For example, the unequal distribution of wealth by race in conjunction with the effect of wealth on health, together contribute to racial health inequities (Bond Huie et al., 2003). The fact that early death of a family member is strongly racially patterned (Thyden et al., 2020, Umberson et al., 2017) is a key aspect of how it reverberates as a form of structural racism to impact outcomes.
Early deaths among minoritized groups are caused by a longstanding system of white supremacy and structural racism, which leads to increased rates of disease and injuries (Bailey et al., 2017). Some deaths may be attributable to discriminatory events such as police murders of Black and Native American people (Edwards et al., 2019) while others are a more cumulative effect of discrimination. For example, minoritized groups experience weathering processes of constant exposure to racial residential segregation (Williams and Collins, 2001), daily discrimination, racism, and/or hardship (Geronimus, 1992).
The legacy of past racial inequity continues to play a role in current racial inequity. Powerful institutions – including those of higher education – were often created during eras of explicit racial discrimination. This codification of white supremacy caused intergenerational trauma (Williams and Mohammed, 2009) - which is trauma whose effects can be passed down through generations - as well as historical trauma such as the lasting effects of the Native American genocide (Heart and DeBruyn, 1998). Today these legacies mutually reinforce each other and intertwine with new forms of discrimination to perpetuate structural racism and inequity (Bailey et al., 2017).
Education is one intervention to improve health and reduce racial health disparities (Hahn and Truman, 2015). Higher education, including obtaining a college degree, is associated with better health (Egerter et al., 2011) and longer life expectancy (Rogot et al., 1992). In addition, college degrees confer more health benefits for certain minoritized students, with Black women gaining more mental health benefits from each year of education compared to socially advantaged groups (Vable et al., 2018). However, there are racial inequities in college completion rates by race with Black and Native American college students half as likely to graduate in four years compared to white and Asian students (DeAngelo et al., 2011). Factors that might account for the beneficial connection between education and health include social networks, income, health insurance (Cutler and Lleras-Muney, 2010), work, knowledge, social standing (Braveman et al., 2011), among others (Egerter et al., 2011).
We hypothesize that experiencing the death of family members negatively affects college graduation rates. A systematic review about bereavement and educational outcomes in children and young people found mixed evidence (Elsner et al., 2021), partly because much of the research is from countries with high quality population data and less income inequality. For instance, in Denmark a family death was associated with increasing disparities in educational attainment for higher levels (Høeg et al., 2018). In Finland, a family death was associated with higher likelihood of dropping out of secondary school (Prix and Erola, 2017), and in Finland (Prix and Erola, 2017) and Norway (Steele et al., 2009) a lower likelihood of entering higher education.
The literature among college-aged adults in the U.S. has focused on grief symptoms, mostly in cross-sectional surveys. Seventeen percent of undergraduates reported that the death of a friend or family member was difficult to handle, and 7% reported that it affected their academic performance (American College Health Association 2018). A cross-sectional survey of college students found that among students who lost a loved one on the past two years, predictors of grief symptoms included a closer relationship with the deceased, a shorter time since the death, younger age of the deceased, and a violent death compared to a nonviolent death (Hardison et al., 2005). The same survey found a higher prevalence of insomnia in bereaved (22%) compared to non-bereaved (17%) students. Again, there is a racial dimension to this evidence. When reporting their top 5 stressors, “death of family” made the list for Black college students but not for white students (Negga et al., 2007).
In addition to using a structural racism framework, the effects of family deaths can also be examined through intersectionality theory (Crenshaw, 1989) and life course models (Kuh et al., 2003). An intersectional approach acknowledges that people within one social category - such as race - differ along other social categories such as gender, and those combinations produce qualitatively and quantitatively unique experiences in ways that are not simply additive. For example, it is plausible that a young woman who experiences the death of a parent will be affected in a different way than a young man, and those experiences may also be unique depending on the person’s race, SES, etc. A life course perspective acknowledges that an exposure can have different effects depending on someone’s life stage (Halfon and Hochstein, 2002). For example, the time when young adults transition away from their childhood household may be particularly sensitive to shocks (Kuh et al., 2003).
One objective of our paper is to examine whether one’s social position affects how a family death influences education, including race, gender, age, SES, and social relationships. Evidence suggests that rates of family deaths differ by race, but whether race modifies the effect of family deaths on educational attainment is less clear. In one study, the only significant interaction between a family death and race (Black or white) on the effect of getting a college degree was for grandparent deaths, with white respondents more likely to graduate from college after a grandparent death and Black respondents less likely to graduate, a possible effect of financial inheritance among white respondents (Patterson et al., 2020). Another study, which combined parent and sibling deaths, did not find a race interaction (Thyden et al., 2020).
Gender may also modify the effect of a family death on education, but there is little prior research. Education trajectories are patterned by gender, as are caregiving roles within families (Marks et al., 2002), and either or both of those could play into differential effects of a family member’s death by gender. One study documented a difference in the likelihood of getting a college degree by the gender of the grandparent who died, with grandfather deaths associated positively with attaining a college degree and grandmother deaths associated negatively with attaining a college degree. That finding – perhaps hinting at an effect of inheritance – points toward another possible mechanism, which is economic. When the death of family member is accompanied by a drop in economic resources, the risk of adverse health outcomes increases (Stroebe et al., 2007). Family members are a source of financial support for students, and therefore the effect of a family death might vary by socioeconomic status.
Age is also important to consider as a modifier. The effect of a family death on college degree varies by the age of the child when the family death occurs, but the nature of that relationship has not been explored from a developmental or life course perspective. A National Longitudinal Study of Youth 1997 (NLSY97) analysis found that the effect of a sibling or parent death on obtaining a college degree was more harmful during college-aged years than during high-school aged years, but deaths prior to age 13 were not assessed (Thyden et al., 2020). An analysis with the Panel Study of Income Dynamics (PSID) found a negative effect of family deaths on educational outcomes, but it collapsed ages (0–5, 6–10, 11–15, 16–20, 21–25) across life transitions (Patterson et al., 2020), mixing potentially heterogeneous effects between high school ages, college ages, and post-college ages, which are important distinctions when using educational outcomes.
This study is a contribution to the literature because it reconceptualizes death as an exposure, and as a form of structural racism, using a large, nationally-representative, longitudinal study across 15 years, begun in childhood, which includes the largest racial/ethnic groups, and measures multiple forms of social vulnerability early in life. We posit that a child’s experience of the premature mortality of a close family member represents a form of structural racism, which subsequently impacts that child’s educational chances. We hypothesize that this death reverberates across the family social system to adversely affect educational outcomes, during a particularly influential time of life, in childhood, and among those who are already socially vulnerable. Specifically, we test the following research questions:
-
1
What is the racial distribution of experiencing a parent or sibling death?
Hypothesis 1: Native Americans experience the highest rates of parent and sibling deaths in early life. This is our hypothesis because of prior (underpowered) estimates (Thyden et al., 2020) and because of high mortality rates in the early life course.
-
2
When in early life is the experience a sibling or parent death most strongly associated with educational attainment?
Hypothesis 2: Deaths experienced during high school years and college years will be most harmful for obtaining a college degree. Our hypothesis assumes that a family death is a large shock in the short-term, and that high school and college performance are strong predictors of college degree attainment.
-
3
What social disadvantages modify the relationship between a family death and college degree attainment?
Hypothesis 2: Deaths experienced during high school years and college years will be most harmful for obtaining a college degree. Our hypothesis assumes that a family death is a large shock in the short-term, and that high school and college performance are strong predictors of college degree attainment.
-
3
What social disadvantages modify the relationship between a family death and college degree attainment?
Hypothesis 3: The effect of a family death will be especially detrimental for educational outcomes for children in families of lower socioeconomic status. We hypothesize that families that are already disadvantaged in their likelihood of attending college would be most vulnerable to an additional barrier such as a family death.
Methods
Dataset and sample
We used the National Longitudinal Study of Adolescent to Adult Health (Add Health) cohort study which is particularly well-suited for these research questions because it has a large and racially diverse sample and its prospective design records family deaths across the entire life course from birth until age 23. Add Health is a nationally representative sample of adolescents in the United States who were in grades 7–12 in 1994–1995 at baseline (Harris, 2013). High schools were sampled with a probability proportional to school size, and all students at sampled schools took an in-school survey (N=90,118). From those students, stratified samples were selected to continue with in-home surveys and longitudinal follow-up (N=20,745). Participants have been surveyed in 5 waves, with the most recent wave in 2016–2018 when participants were 32–42 years old. Participants were included in this analysis if they reported their educational attainment in Wave IV and they had a Wave IV weight (N=14,796). Wave IV weight is the survey weight Add Health recommends using in order to correct for sampling and attrition when analyzing data from several different waves including an outcome at Wave IV. In Wave IV there was an 80.3% response rate, and bias analyses showed that the small magnitude of attrition bias was corrected for by sampling weights (Harris et al., 2019). We obtained and analyzed the restricted-use Add Health data which is available to researchers by contractual agreement, and has more detailed data than the public-use data.
Exposures – Family Deaths
Biological parent deaths
At each wave, participants were asked if their biological mother and biological father were alive. If they said no, they were then asked to report how old they were when their parent died (in Waves I and II), or the month and year their parent died (in Waves III and IV). Deaths for this analysis were measured up until participants were 23 years old.
Sibling Deaths
In Wave IV (2008, ages 24–32), participants reported the number of siblings they had, living and deceased, including biological, adoptive, and step siblings. Participants then reported if any of those siblings had died, and the year of each death. Some sibling deaths occurred before the participant was born, which was not considered to be a family death for this analysis. We used data for sibling deaths up until the participant was 23 years old.
Outcome – Bachelor’s Degree
At Wave IV (2008, ages 24–32), participants reported their highest level of education from a list of 16 possible categories from “8th grade or less” up to professional and doctoral degrees. We collapsed these categories into a binary category of whether the participant had a bachelor’s degree or less than a bachelor’s degree. We chose to focus on bachelor’s degree because it is consistently related to earnings (Autor, 2014), and because we can more reliably approximate an age range for pursuing a Bachelor’s degrees compared to other degrees, which allows us to draw inferences about the effect of family deaths during typical pre-college years compared to typical college years.
Effect Modifiers
Respondent’s Age at family death
Participants’ birth date.
In the restricted dataset, Add Health provides the participant’s birth year and month, but removes the day. Similarly, they provide the year and month of the Add Health interview, but not always the day. In cases where a birth date was needed to calculate participant’s age at a family member’s death, we set the day of the birth month to “15” in accordance with common practice in demography.
Age categories.
We created respondent age categories that loosely correspond to typical stages of education in the U.S., and modeled age categorically. (Pre-Kindergarten: 0 to 4, elementary school: 5 to 9, middle school: 10 to 13, high school: 14 to 18, college: 19–23). If a participant reported more than one death in their family up until age 23, they are coded as the age at death for the first death they experienced. One hundred participants reported the deaths of both biological parents, and 63 participants reported more than one sibling death. If a participant reported a death but did not report a year or age associated with the death, that participant was excluded from age analyses.
Race/ethnicity
We estimated the prevalence of family deaths by race/ethnicity, and modeled race/ethnicity as an effect modifier of the relationship between family deaths and college education. Participants reported their race at Wave I (grades 7–12). Participants could first indicate multiple race categories (including ‘other’). Those who checked multiple categories were then asked to choose one. Participants also reported their ethnicity (Hispanic, not Hispanic). Much of the sample who chose the ‘other’ race category identified as Hispanic. We created a six-category mutually-exclusive race/ethnicity variable: Non-Hispanic (NH) white, NH Black, NH Native American, NH Asian American, Hispanic, NH other, where all race categories are non-Hispanic and multi-racial participants were categorized as the race they selected when asked which one category best describes their racial background.
Parent-reported variables
The most complete variable available for baseline socioeconomic status (SES) in Add Health is parents’ education level, measured at baseline (Pampel et al., 2014). Parents reported their education level, and because the parent report was missing for a lot of parents, we supplemented that data with the participant’s report on their parents’ education level collected in the first two waves. From there we created a 3-level ordinal measure of parent education using the parent with the highest education (less than high school, high school or equivalent, college degree), as done previously in Add Health (Goodman, 1999). In the same baseline parent survey, parents reported their household income and health.
Covariates
We selected covariates for regression analyses based on a previously published Directed Acyclic Graph (DAG) (Thyden et al., 2020), a method used in causal inference to reduce confounding (Glymour, 2006). All models were accordingly adjusted for baseline sex, age, self-reported health (excellent, very good or good vs fair or poor) (Idler and Benyamini, 1997), household income, parent education (less than high school degree, high school degree, college degree), parent health (excellent, very good or good vs fair or poor) , race, region (West, Midwest, South, Northeast), and urbanicity (urban, suburban, rural).
Analysis
We ran univariate descriptive statistics for all analytic variables, as well as bivariable descriptives by the binary outcome of experiencing a family death or not. We ran logistic regression models with bachelor’s degree (vs. lower) as the outcome, comparing participants with family deaths to participants without family deaths, adjusted for baseline demographic, SES and health covariates. To test whether the type of social relationship mattered, we next ran separate models for each type of family member (biological mother, biological father, sibling) modeled both as a binary exposure and as a categorical exposure of 5 age groups with ‘no death’ as the reference. For models of sibling deaths we ran models adjusted for baseline covariates as well as additional models that adjusted for the number of siblings (alive and deceased) the participant had. We converted the odds ratios into predicted probabilities – measures of absolute risk – using Stata’s post-estimation margins command based on the regression model coefficients. We used interaction models to assess whether family deaths interacted with gender, parental education, or race to affect educational attainment (interaction test p<0.05). All analyses adjusted for the Add Health design by applying weights, modeling region as a strata variable, and modeling school as a cluster (primary sampling unit) variable. (Chen and Harris, 2020) We used the Wave IV cross-sectional survey weights and multiply imputed missing baseline covariates using the “ice” command in Stata 15.1 with 5 imputations.
Results
The analytic sample was 14,796 participants. Four participants were excluded because they did not report their educational attainment. Weighted descriptive statistics for all analytic variables – overall and stratified by whether participants experienced a sibling or parent death by the age of 23 – are in Table 1. Overall, 51% of the Add Health analytic baseline sample was male, 67% of the sample was white, and 30% of participants had attained a Bachelor’s degree by Wave IV (ages 24–32).
Table 1:
Add Health Sample: Descriptives of baseline covariates and educational attainment by Wave IV, overall and stratified by whether the participant experienced a family death during ages 0 to 23 (N=14,796)
| Overall | No family death (N=12,635) | Family death (N=2,161) | ||||
|---|---|---|---|---|---|---|
| raw N | imputed, weighted % | raw N | imputed, weighted % | raw N | imputed, weighted % | |
| Family deaths age 0–23 | ||||||
| Biological parent, or sibling | 2,184 | 14.2% | ||||
| Biological mother | 520 | 3.4% | ||||
| Biological father | 1,183 | 7.7% | ||||
| Sibling | 670 | 4.2% | ||||
| Bachelor’s degree | ||||||
| No Bachelor’s degree | 10,059 | 70.1% | 8,346 | 68.2% | 1,713 | 81.2% |
| Bachelor’s degree | 4,737 | 29.9% | 4,268 | 31.8% | 469 | 18.6% |
| missing | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Baseline characteristics (1994–1995, grades 7–12) | ||||||
| Race | ||||||
| White (NH) | 8,123 | 67.3% | 7,146 | 69.3% | 977 | 55.4% |
| Black (non-Hispanic) | 3,177 | 15.8% | 2,491 | 14.0% | 686 | 27.0% |
| Native American (NH) | 112 | 0.7% | 84 | 0.6% | 28 | 1.5% |
| Asian American (NH) | 903 | 3.2% | 771 | 3.3% | 132 | 2.8% |
| Hispanic | 2,356 | 12.0% | 2,012 | 11.9% | 344 | 12.7% |
| Other | 125 | 0.9% | 110 | 1.0% | 15 | 0.5% |
| missing | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Age (mean in years) | 15.4 | 15.4 | 15.5 | |||
| missing | 10 | 0.0% | 8 | 0.0% | 2 | 0.0% |
| Male | 6,930 | 50.7% | 5,993 | 51.4% | 937 | 46.8% |
| missing | 2 | 0.0% | 2 | 0.0% | 0 | 0.0% |
| Good Health | 13,718 | 93.0% | 11,738 | 93.4% | 1,980 | 90.6% |
| missing | 12 | 0.0% | 10 | 0.0% | 2 | 0.0% |
| Parent Education | ||||||
| Less than high school | 1,475 | 11.6% | 1,156 | 10.6% | 319 | 17.6% |
| High school diploma | 7,102 | 57.4% | 6,049 | 57.0% | 1,053 | 60.3% |
| College degree | 4,169 | 31.0% | 3,725 | 32.5% | 444 | 22.1% |
| missing | 2,050 | 0.0% | 1,684 | 0.0% | 366 | 0.0% |
| Annual household income (mean) | $45,288 | $46,556 | $37,641 | |||
| missing | 3,581 | 2,961 | 620 | |||
| Region | ||||||
| West | 3,452 | 16.7% | 2,939 | 16.9% | 513 | 15.3% |
| Midwest | 3,772 | 31.2% | 3,289 | 31.7% | 483 | 28.7% |
| South | 5,646 | 38.6% | 4,715 | 37.6% | 931 | 44.3% |
| Northeast | 1,926 | 13.5% | 1,671 | 13.8% | 255 | 11.7% |
| missing | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Metro | ||||||
| Urban | 4,267 | 26.2% | 3,642 | 26.0% | 625 | 27.3% |
| Suburban | 7,939 | 58.4% | 6,748 | 58.6% | 1,191 | 57.2% |
| Rural | 2,587 | 15.4% | 2,221 | 15.4% | 366 | 15.5% |
| missing | 3 | 0.0% | 3 | 0.0% | 0 | 0.0% |
% missing by variable was modeled in Table 1 here to inform magnitude of missing, although missing data was imputed for the regression model results through multiple imputation.
Overall, 14% of the Add Health sample experienced a parent or sibling death before age 23, with variation by race/ethnicity. The racial group with the lowest proportion of experiencing a sibling or parent death in the first 23 years of their lives was white participants (12%, 95% CI 11% - 13%), followed by Asian participants (13%, 95% CI 9% - 17%), Hispanic participants (15%, 95% CI 12% - 19%), Black participants (24%, 95% CI 21% - 27%) and Native American participants (30%, 95% CI 20% - 43%) (See Figure 1). Black participants and Native American participants experienced a higher rate of family deaths at each of the five age categories compared to white participants, apart from the 10–13 category for Native Americans for which no deaths were reported. While 14% of the Add Health population experienced any death of a parent or sibling, exposure to a biological father’s death before age 23 was the largest category of family relationship deaths in Add Health (prevalence 7.7% (N=1,183) (Table 1). The prevalence of experiencing a biological mother’s death before age 23 in this sample is 3.4% (N=520) and the prevalence of a sibling’s death was 4.2% (N=647).
Figure 1:
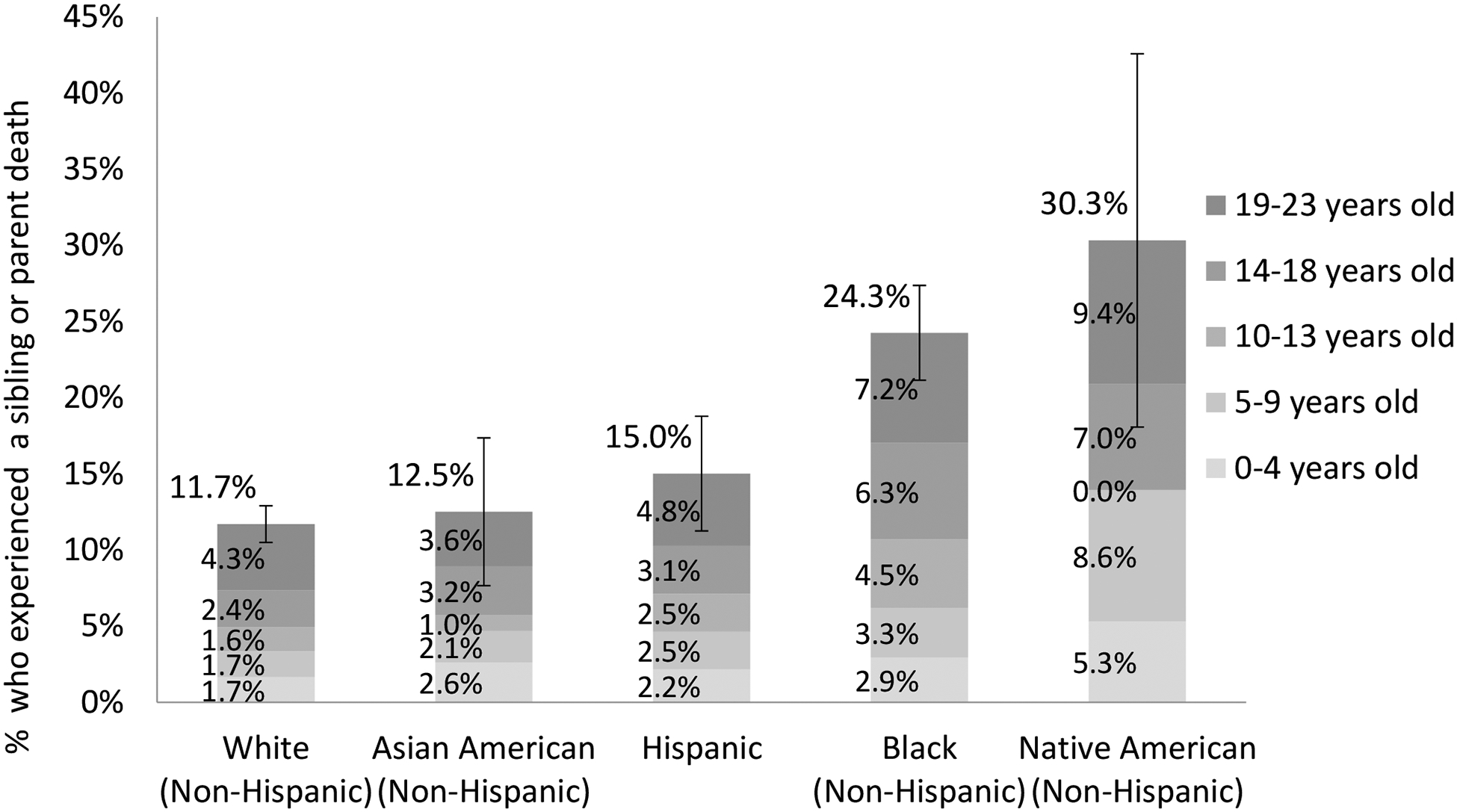
Frequency of experiencing a sibling or parent death by age 23, by race and age (N=14,675)
Percentages are survey-weighted, and unadjusted for covariates (descriptives). “Other” race category not included because of small numbers (N=125)
Participants who experienced a sibling or parent death by Wave IV had significantly lower chances of obtaining a college degree by Wave IV (ages 24 to 32) compared to those who did not experience a family death. In bivariate analysis, 19% of respondents who experienced the death of a family member graduated with at least a Bachelor’s degree, while that number was much higher at 32% among those who never experienced a family death. In models adjusted for covariates, those who experienced a family death had 0.60 times the odds (95% CI 0.51 – 0.71) (Supplemental Table 1) of achieving a bachelor’s degree, compared to those who did not have a family death.
The relationship of a family death with obtaining higher education was statistically significant for every age group of the child when the death occurred (Figure 2), compared with no death. The largest difference in effect by child’s age was between no family death (predicted probability of a bachelor’s degree was = 0.31, 95% CI 0.29 – 0.33) compared to a family death between the ages of 10 to 13 (predicted probability of a bachelor’s degree= 0.20, 95% CI 0.13– 0.26). Mother deaths, father deaths, and sibling deaths were each significantly associated with lowered likelihood of obtaining a college degree and were similar in magnitude, although a sibling death was most harmful (Figure 3; range of ORs from 0.52 to 0.69). The effect of a sibling death on college degree attainment (OR = 0.52, 95% CI 0.40 – 0.67) was attenuated but still statistically significant after adjusting for number of siblings (OR = 0.66, 95% CI 0.51 – 0.85) (Supplemental Table 1). The ages at which a family member’s death were most strongly associated with college degree attainment varied slightly across whether the death was a sibling, mother, or father, with stronger effects at age 10–13 for mothers and fathers, versus stronger effects at ages 0–4 for siblings.
Figure 2:
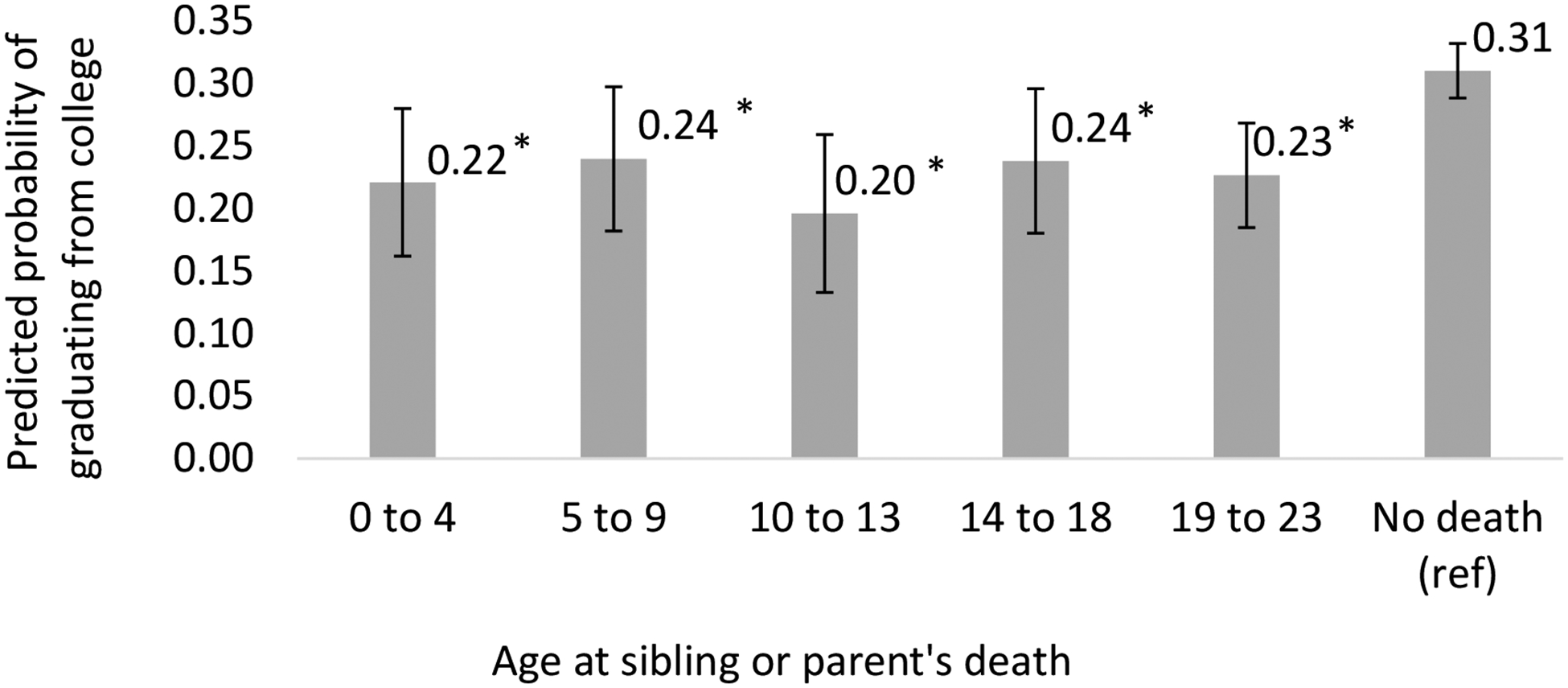
Adjusted Likelihood of graduating from college by wave 4 (ages 24–32), by age at family member’s death (N=14,796)
* significantly different from “no death” at p<.05
Predicted probabilities of college graduate were derived using post estimation commands from covariate-adjusted, multiply imputed, survey-weighted logistic regression models.
Covariates: baseline sex, age, self-reported health, household income, parent education, parent health, race, region, and urbanicity
Corresponding odds ratios presented in Supplemental Table 1 as Model 4
Figure 3:
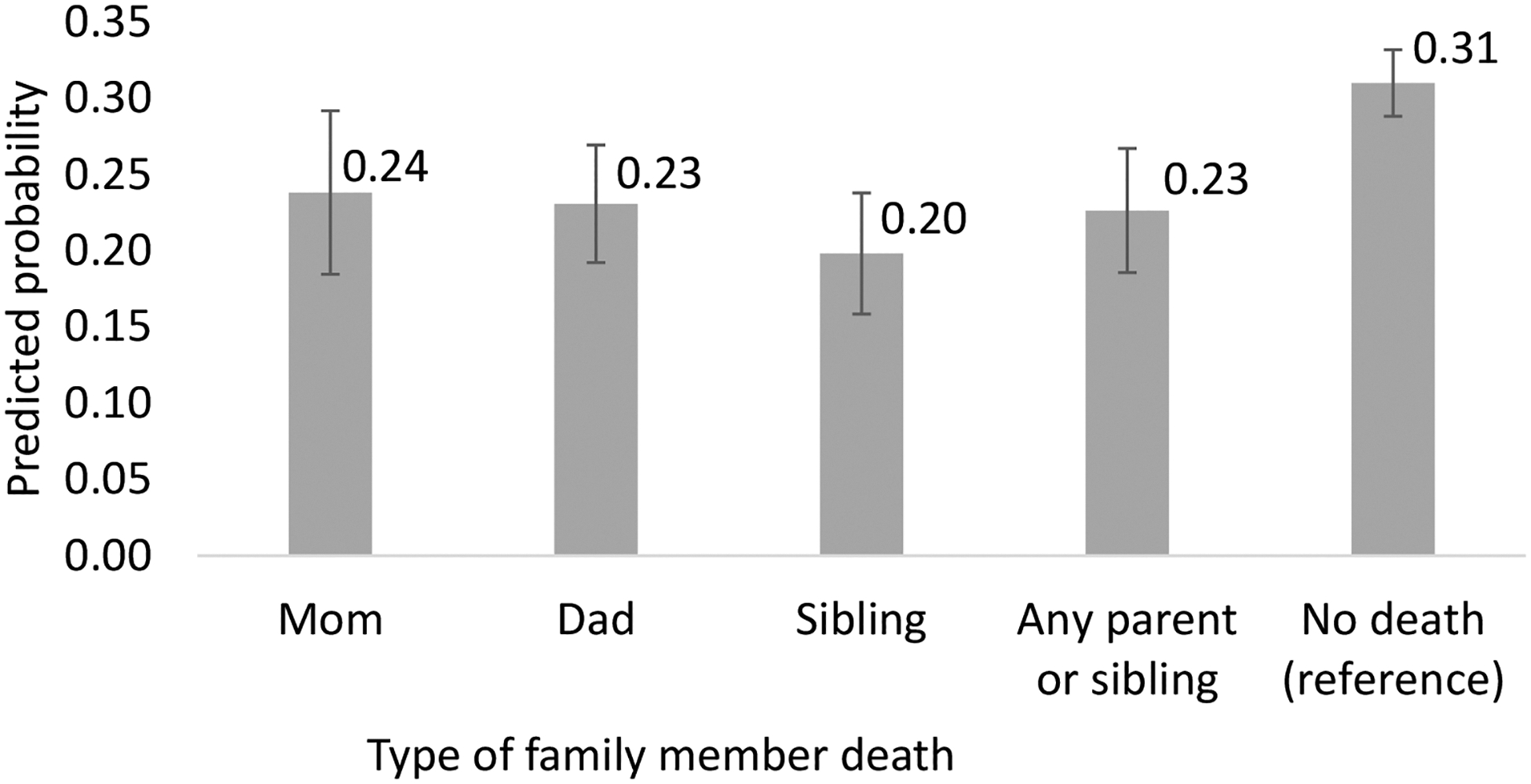
Adjusted Predicted probabilities of attaining a college degree by Wave IV (ages 24–32), by type of family member’s death that occurred during ages 0–23, in Add Health (N=14,796)
* significantly different from “no death” at p<.05
Predicted probabilities of attaining a college degree are based on post estimation commands using covariate-adjusted, multiply imputed, survey-weighted logistic regression models.
Covariates: baseline sex, age, self-reported health, household income, parent education, parent health, race, region, and urbanicity
Corresponding odds ratios presented in Supplemental Table 1 as Model 5, Model 6, Model 7, and Model 8
There were no statistically significant interactions between the participant’s gender and the effect of a sibling’s (p=0.7), mother’s (p=0.8) or father’s (p=0.2) death on college degree attainment. The effect of a family death on college degree attainment also did not vary by baseline parent education (p= 0.17) or race/ethnicity (p=0.38) (results not shown).
Discussion
Native American and Black children were much more likely to experience the death of a parent or sibling from birth to age 23 compared to all other racial/ethnic groups. We found that a child who experiences a parent or sibling death in early life has lower odds of graduating from college compared to no sibling or parent death (OR=0.60, 95% CI 0.51 – 0.71). There were minor differences by age and by type of family member’s death, but the death of a parent or sibling was consistently harmful.
This analysis is the first to measure racial disparities in sibling and parent deaths from birth to emerging adulthood among Asian Americans, Hispanics, and Native Americans. Previous work has measured Black-white disparities only (Umberson, 2017, Patterson et al., 2020) or family deaths at age 13 and older (Thyden et al., 2020). Although small samples of Native American participants in our analyses led to imprecise estimates (i.e. large confidence intervals), the finding that young Native Americans experience an enormous disparity in parent and sibling deaths – on the order of 2.5 times higher – compared to other racialized groups has now been replicated in two large longitudinal cohort studies, including in Add Health (this study) and NLSY97 (Thyden et al., 2020). However, the previous finding in NLSY97 that Asian Americans experience relatively high rates of family deaths (Thyden et al., 2020) was not replicated in this study, as we found a reduced rate of family deaths among Asian Americans compared to other racial/ethnic groups. Perhaps it is due to imprecise estimates from small samples, or perhaps Add Health and NLSY97 have different representation of Asian ancestry subgroups. The racial disparity in higher risk of family deaths likely reflects effects of ongoing structural discrimination against Black and Native American populations, occurring across sectors and domains, in both acute and chronic exposures (Bailey et al., 2017).
Whether a family death affects Black and Native American young people differently or not, the fact that Black and Native American people experience more family deaths is enough to create disparities in the outcome of education. Disproportionate exposures by themselves – in this case, family deaths by race – influence population health (Ward et al., 2018). Unpacking these “risks of risks” is a core task to identify fundamental causes of population health and structural inequity (Berkman et al., 2014, Link and Phelan, 1995).
Age of exposure modified the impact of a family death on obtaining a bachelor’s degree, with strongest effects when the family death occurred from ages 10 to 13 – the tween years. Previous studies on educational outcomes at this age have found bereaved children negatively affected by worse study habits and concentration, while other studies found no negative effects, or that children used school as an escape (Elsner et al., 2021). The combination of ‘type of family death’ and ‘age at family death’ with the most harmful effect on educational attainment was a sibling death while the participant was 19 to 22 (OR=0.43, 95% CI 0.23 – 0.80), the typical years of college enrollment.
A sibling’s death, a mother’s death, and a father’s death were each independently associated with a decreased likelihood of graduating from college, compared to no death of that type. Adjusting for the participant’s number of siblings attenuated the effect, but sibling death still mattered. At the same time, adjusting for number of siblings introduces the methodological issue of positivity violation (Westreich and Cole, 2010) where those without siblings cannot have been exposed to a sibling death. When modeled ordinally, as is most appropriate, the statistical software omits the variable of number of siblings altogether. Our findings were robust regardless of sibling adjustment.
Those who experienced a sibling or parent death were 7 percentage points less likely to graduate from college. Previous studies in the U.S. have found mixed results about the association between a family death and attaining a college degree (Elsner et al., 2021). However, those samples were school-based, and may only be generalizable to certain types of schools (Cox et al., 2016) or to students identified as bereaved by their university (Servaty-Seib and Hamilton, 2006), rather than being population based. Another study used age categories that mixed high schoolers with college-age participants, and college-aged participants with older participants, so it is difficult to compare with our study (Patterson et al., 2020). We chose to separate and test ages of the child which correspond to grades and different levels of schooling, as a test for socially-relevant periods and transitions in our life course informed model (Kuh et al., 2003).
The COVID-19 pandemic has exacerbated existing racial health inequities, including the rates of who experienced the deaths of friends and family (Verdery et al., 2020). Black, Hispanic, Native American/Alaska Native, and Native Hawaiian/Pacific Islander children were all twice as likely to have a parent die from COVID-19 compared to white children (Treglia et al., 2022). Children 0 to 17 experienced 20% higher rates of parental bereavement compared to before COVID-19 (Kidman et al., 2021), and in the first 15 months of the pandemic about 140,000 children in the U.S. experienced the death of a parent or grandparent caregiver (Hillis et al., 2021). The implications of parent deaths have become more and more salient as today’s youth lose caregivers at an unprecedented rate.
Limitations and future research
Add Health accurately represents and generalizes to the cohort of people who were in grades 7–12 in 1995 in the U.S. With the fourth wave of data, the sample continues to produce representative and generalizable estimates thanks to relatively low rates of attrition, little bias induced by attrition, and weights re-calculated for each wave of data (Harris et al., 2019). However, Add Health and this analysis also have limitations.
Family deaths may have been measured imprecisely. We operationalized family deaths as: biological parents and any type of sibling. This is a limitation because a biological parent is not necessarily someone’s main parental figure. Because grandparent caregivers are more common in communities of color, our operationalization has the potential to underestimate racial disparities. (Kropf and Kolomer, 2004) Focusing on biological parents also underestimates the impact of a parent’s death for children with same-sex parents. Future research should be inclusive when defining caregivers.
While we were able to estimate overall proportions of family deaths by race, small numbers made it difficult to delve deeper into the unique experiences of different minoritized groups. For instance, Black and white Americans differ significantly in how many full siblings, half siblings, grandchildren, and cousins they have (Daw et al., 2016). In addition, different communities have different practices around “fictive kin”, people who have close emotional ties but are not legally or biologically related (Taylor et al., 2013, Ebaugh and Curry, 2000). Qualitative research about family deaths would be one way to better understand the nuances of that experience within and between groups. There is a lot of diversity within each of the large minoritized racial categories of Native American, Hispanic, Black, and Asian.
Our analysis included participants who enrolled in college as well as those who did not enroll in college in order to capture both those who enrolled in college and a family death affected their likelihood of graduating, and those whose family death affected their likelihood of enrolling in college in the first place. However, we could not measure those two effects separately because years of college enrollment was not measured as precisely as age at a family member’s death.
Measurement of family deaths could be improved. Respondents reported family member deaths from several decades ago, which makes recall bias a concern. For instance, when participants reported their own age at the same death more than once (i.e. reported in several waves when their biological mother died), there were some discrepancies. However, sensitivity analysis (not shown here) were robust, whereby the age of the participant reported multiple times across waves was usually not off by more than a couple years. We mitigated this reporting error by assuming less recall bias sooner after the event and used the age reported soonest after the death. Future research should collect detailed and validated information about deaths, including date of death as well as cause of death to determine which causes of death may have an outsized impact on surviving relatives.
Future research should investigate mechanisms and policy solutions that buffer effects of family deaths on educational attainment. For example, students may encounter barriers to college enrollment such as recruitment and financial aid policies that are designed for ‘traditional’ students coming straight from high school and may not serve students as well if they matriculate later or take a break from college due to a life event such as a family death. Moreover, some policies are overly punitive regarding short-term lapses in academic performance, instead of offering supports like placing coursework on hold, modifying assignments, or offering financial refunds if students cannot balance their schoolwork after experiencing a disruptive life event like the death of a family member. It is important for educational institutions to be aware of this vulnerable population which is disproportionately from racially marginalized groups and adjust their policies to support students experiencing family deaths.
In conclusion, this study found that family deaths in early life disproportionately occur to Native American, Black, and Hispanic youth, and at particularly large magnitudes for Native American and Black youth (2–3 times the family mortality rates as whites’ rate of 10%). Because racial disparities in premature deaths occur as a result of structural forces of discrimination and disparity across sectors and life domains (Bailey et al., 2017), we conceptualize the exposure of family deaths as a form of structural racism. And although death is usually considered the ultimate event in population health research, we argue that death as an exposure is a particularly relevant mechanism by which one generation’s mortality experiences may continue to affect the inequity of the next generation in the longer view of what causes population health. Although here we examined college degree attainment in relation to family deaths, education may be just one of many outcomes affected by family deaths and other exposures that are disproportionately experienced by people of color in the U.S.
Supplementary Material
Table 2:
Adjusted likelihood of graduating from college by wave 4 (ages 24–32), by type of family member death and age at family member’s death (N=14,796)
| predicted probability of college graduation | standard error | lower 95% confidence interval | upper 95% confidence interval | |
|---|---|---|---|---|
| Model 1: participant’s age at mom’s death | ||||
| 0 to 4 | 0.27 | 0.08 | 0.10 | 0.43 |
| 5 to 9 | 0.22 | 0.06 | 0.11 | 0.34 |
| 10 to 13 | 0.18 | 0.05 | 0.08 | 0.29 |
| 14 to 18 | 0.24 | 0.06 | 0.12 | 0.36 |
| 19 to 22 | 0.25 | 0.04 | 0.18 | 0.33 |
| no death | 0.30 | 0.01 | 0.28 | 0.32 |
| Model 2: participant’s age at dad’s death | ||||
| 0 to 4 | 0.25 | 0.04 | 0.16 | 0.34 |
| 5 to 9 | 0.25 | 0.05 | 0.16 | 0.34 |
| 10 to 13 | 0.18 | 0.04 | 0.10 | 0.27 |
| 14 to 18 | 0.25 | 0.04 | 0.17 | 0.33 |
| 19 to 22 | 0.23 | 0.03 | 0.17 | 0.29 |
| no death | 0.30 | 0.01 | 0.28 | 0.33 |
| Model 3: participant’s age at sibling’s death | ||||
| 0 to 4 | 0.18 | 0.04 | 0.10 | 0.26 |
| 5 to 9 | 0.27 | 0.05 | 0.16 | 0.37 |
| 10 to 13 | 0.24 | 0.06 | 0.12 | 0.35 |
| 14 to 18 | 0.18 | 0.04 | 0.10 | 0.26 |
| 19 to 22 | 0.17 | 0.04 | 0.09 | 0.25 |
| no death | 0.30 | 0.01 | 0.28 | 0.32 |
“Predicted probabilities of obtaining a bachelor’s degree were derived from post estimation commands of covariate-adjusted, multiply imputed, survey-weighted logistic regression models.
Covariates: baseline sex, age, self-reported health, household income, parent education, parent health, race, region, and urbanicity.
The corresponding odds ratios for these models are presented in Supplemental Table 1 with the same model numbering (Model 1, Model 2, Model 3)
Acknowledgments
We appreciate support provided by the Eunice Kennedy Shriver National Institute for Child Health and Human Development of the U.S. National Institutes for Health, for supporting Dr. Thyden’s training [T32HD095134 (MPIs: Warren & Osypuk], for supporting the University of Minnesota’s Minnesota Population Center [grant number P2CHD041023] and the National Institute on Aging of the U.S. National Institutes of Health to the University of Minnesota’s Life Course Center [grant number P30AG066613].
This publication was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $2,736,250 with 0 percentage financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.”
Add Health is directed by Robert A. Hummer and funded by the National Institute on Aging cooperative agreements U01 AG071448 (Hummer) and U01AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Waves I-V data are from the Add Health Program Project, grant P01 HD31921 (Harris) from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Young Native Americans experience 2.5 times more family deaths than other groups A family death during ages 10 to 13 most strongly reduced college degree attainment Sibling deaths were particularly harmful for completing a bachelor’s degree
References
- AMERICAN COLLEGE HEALTH ASSOCIATION 2018. American College Health Association-National College Health Assessment II: Undergraduate Student Reference Group Executive Summary Spring 2018. Silver Spring, MD: American College Health Association. [Google Scholar]
- AUTOR DH 2014. Skills, education, and the rise of earnings inequality among the “other 99 percent”. Science , 344, 843–851. [DOI] [PubMed] [Google Scholar]
- BAILEY ZD, KRIEGER N, AGENOR M, GRAVES J, LINOS N & BASSETT MT 2017. Structural racism and health inequities in the USA: evidence and interventions. Lancet , 389, 1453–1463. [DOI] [PubMed] [Google Scholar]
- BERKMAN LF, KAWACHI I & GLYMOUR MM 2014. Social epidemiology, Oxford University Press. [Google Scholar]
- BOND HUIE SA, KRUEGER PM, ROGERS RG & HUMMER RA 2003. Wealth, race, and mortality. Social Science Quarterly , 84, 667–684. [Google Scholar]
- BRAVEMAN P, EGERTER S & WILLIAMS DR 2011. The social determinants of health: coming of age. Annual review of public health , 32, 381–398. [DOI] [PubMed] [Google Scholar]
- BRAVEMAN P & GOTTLIEB L 2014. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep , 129, 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BRENT D, MELHEM N, DONOHOE MB & WALKER M 2009. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. American Journal of Psychiatry , 166, 786–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CENTERS FOR DISEASE CONTROL AND PREVENTION 2017. Underlying Cause of Death 1999–2016 on CDC WONDER Online Database. Data are from the Multiple Cause of Death Files, 1999–2016, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. [Google Scholar]
- COX BE, REASON RD, NIX S & GILLMAN M 2016. Life happens (outside of college): Non-college life-events and students’ likelihood of graduation. Research in Higher Education , 57, 823–844. [Google Scholar]
- CRENSHAW K 1989. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 139. [Google Scholar]
- CUTLER DM & LLERAS-MUNEY A 2010. Understanding differences in health behaviors by education. Journal of health economics , 29, 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAW J, VERDERY AM & MARGOLIS R 2016. Kin count (s): Educational and racial differences in extended kinship in the United States. Population and Development Review , 42, 491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEANGELO L, FRANKE R, HURTADO S, PRYOR JH & TRAN S 2011. Completing college: Assessing graduation rates at four-year institutions , Los Angelos, Higher Education Research Institute. [Google Scholar]
- EBAUGH HR & CURRY M 2000. Fictive kin as social capital in new immigrant communities. Sociological Perspectives , 43, 189–209. [Google Scholar]
- EDWARDS F, LEE H & ESPOSITO M 2019. Risk of being killed by police use of force in the United States by age, race–ethnicity, and sex. Proceedings of the national academy of sciences , 116, 16793–16798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EGERTER S, BRAVEMAN P, SADEGH-NOBARI T, GROSSMAN-KAHN R & DEKKER M 2011. Exploring the social determinants of health: Education and Health. Robert Wood Johnson Foundation. [Google Scholar]
- ELSNER TL, KRYSINSKA K & ANDRIESSEN K 2021. Bereavement and educational outcomes in children and young people: A systematic review. School Psychology International, 01430343211057228. [Google Scholar]
- GERONIMUS AT 1992. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethnicity & disease, 207–221. [PubMed] [Google Scholar]
- GLYMOUR MM 2006. Using causal diagrams to understand common problems in social epidemiology. In: OAKES JM & KAUFMAN JS (eds.) Methods in Social Epidemiology . San Francisco: Jossey-Bass. [Google Scholar]
- GOODMAN E 1999. The role of socioeconomic status gradients in explaining differences in US adolescents’ health. American journal of public health , 89, 1522–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAHN RA & TRUMAN BI 2015. Education improves public health and promotes health equity. International journal of health services , 45, 657–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HALFON N & HOCHSTEIN M 2002. Life course health development: an integrated framework for developing health, policy, and research. The Milbank Quarterly , 80, 433–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARDISON HG, NEIMEYER RA & LICHSTEIN KL 2005. Insomnia and complicated grief symptoms in bereaved college students. Behavioral sleep medicine , 3, 99–111. [DOI] [PubMed] [Google Scholar]
- HARRIS KM 2013. The add health study: Design and accomplishments. Chapel Hill: Carolina Population Center, University of North Carolina at Chapel Hill. [Google Scholar]
- HARRIS KM, HALPERN CT, WHITSEL EA, HUSSEY JM, KILLEYA-JONES LA, TABOR J & DEAN SC 2019. Cohort profile: The national longitudinal study of adolescent to adult health (add health). International Journal of Epidemiology , 48, 1415–1415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HEART B & DEBRUYN LM 1998. The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska native mental health research , 8, 56–78. [PubMed] [Google Scholar]
- HILLIS SD, BLENKINSOP A, VILLAVECES A, ANNOR FB, LIBURD L, MASSETTI GM, DEMISSIE Z, MERCY JA, NELSON CA III & CLUVER L 2021. COVID-19–associated orphanhood and caregiver death in the United States. Pediatrics , 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HØEG B, JOHANSEN C, CHRISTENSEN J, FREDERIKSEN K, DALTON SO, BØGE P, DENCKER A, DYREGROV A & BIDSTRUP P 2018. Does losing a parent early influence the education you obtain? A nationwide cohort study in Denmark. Journal of Public Health. [DOI] [PubMed] [Google Scholar]
- IDLER EL & BENYAMINI Y 1997. Self-rated health and mortality: a review of twenty-seven community studies. Journal of health and social behavior, 21–37. [PubMed] [Google Scholar]
- KIDMAN R, MARGOLIS R, SMITH-GREENAWAY E & VERDERY AM 2021. Estimates and projections of COVID-19 and parental death in the US. JAMA pediatrics , 175, 745–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KROPF NP & KOLOMER S 2004. Grandparents raising grandchildren: A diverse population. Journal of Human Behavior in the Social Environment , 9, 65–83. [Google Scholar]
- KUH D, BEN-SHLOMO Y, LYNCH J, HALLQVIST J & POWER C 2003. Life course epidemiology. Journal of epidemiology and community health , 57, 778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LINK BG & PHELAN J 1995. Social conditions as fundamental causes of disease. Journal of health and social behavior, 80–94. [PubMed] [Google Scholar]
- MARKS NF, LAMBERT JD & CHOI H 2002. Transitions to caregiving, gender, and psychological well-being: A prospective US national study. Journal of Marriage and Family , 64, 657–667. [Google Scholar]
- MURRAY CJ, SALOMON JA & MATHERS C 2000. A critical examination of summary measures of population health. Bulletin of the World Health Organization , 78, 981–994. [PMC free article] [PubMed] [Google Scholar]
- NEGGA F, APPLEWHITE S & LIVINGSTON I 2007. African American college students and stress: school racial composition, self-esteem and social support. College Student Journal , 41. [Google Scholar]
- PAMPEL FC, MOLLBORN S & LAWRENCE EM 2014. Life course transitions in early adulthood and SES disparities in tobacco use. Social Science Research , 43, 45–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PATTERSON SE, VERDERY AM & DAW J 2020. Linked Lives and Childhood Experience of Family Death on Educational Attainment. Socius , 6, 2378023120975594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRIX I & EROLA J 2017. Does death really make us equal? Educational attainment and resource compensation after paternal death in Finland. Social Science Research , 64, 171–183. [DOI] [PubMed] [Google Scholar]
- ROGOT E, SORLIE PD & JOHNSON NJ 1992. Life expectancy by employment status, income, and education in the National Longitudinal Mortality Study. Public health reports , 107, 457. [PMC free article] [PubMed] [Google Scholar]
- ROSE G 2001. Sick individuals and sick populations. International journal of epidemiology , 30, 427–432. [DOI] [PubMed] [Google Scholar]
- SERVATY-SEIB HL & HAMILTON LA 2006. Educational performance and persistence of bereaved college students. Journal of College Student Development , 47, 225–234. [Google Scholar]
- STEELE F, SIGLE-RUSHTON W & KRAVDAL Ø 2009. Consequences of family disruption on children’s educational outcomes in Norway. Demography , 46, 553–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STROEBE M, SCHUT H & STROEBE W 2007. Health outcomes of bereavement. The Lancet , 370, 1960–1973. [DOI] [PubMed] [Google Scholar]
- TAYLOR RJ, CHATTERS LM, WOODWARD AT & BROWN E 2013. Racial and ethnic differences in extended family, friendship, fictive kin, and congregational informal support networks. Family relations , 62, 609–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- THYDEN NH, SCHMIDT NM & OSYPUK TL 2020. The unequal distribution of sibling and parent deaths by race and its effect on attaining a college degree. Annals of epidemiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TREGLIA D, CUTULI J, ARASTEH K, BRIDGELAND J, EDSON G, PHILLIPS S & BALAKRISHNA A 2022. Hidden pain: children who lost a parent or caregiver to COVID-19 and what the nation can do to help them. [Google Scholar]
- UMBERSON D 2017. Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors. Journal of health and social behavior , 58, 405–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UMBERSON D, OLSON JS, CROSNOE R, LIU H, PUDROVSKA T & DONNELLY R 2017. Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences , 114, 915–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VABLE AM, COHEN AK, LEONARD SA, GLYMOUR MM, DP DUARTE C & YEN IH 2018. Do the health benefits of education vary by sociodemographic subgroup? Differential returns to education and implications for health inequities. Annals of epidemiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VERDERY AM, SMITH-GREENAWAY E, MARGOLIS R & DAW J 2020. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences , 117, 17695–17701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WARD JB, GARTNER DR, KEYES KM, FLISS MD, MCCLURE ES & ROBINSON WR 2018. How do we assess a racial disparity in health? Distribution, interaction, and interpretation in epidemiological studies. Annals of Epidemiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WESTREICH D & COLE SR 2010. Invited commentary: positivity in practice. American journal of epidemiology , 171, 674–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILLIAMS DR & COLLINS C 2001. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports , 116, 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILLIAMS DR & MOHAMMED SA 2009. Discrimination and racial disparities in health: evidence and needed research. Journal of behavioral medicine , 32, 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WORLD HEALTH ORGANIZATION 2008. Social determinants of health. WHO Regional Office for South-East Asia. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


