Summary
Background
Household wealth is positively related to cognitive health outcomes in later life. However, the association between negative wealth shocks and cognitive function in later life, and whether this association might differ across countries at different levels of economic development, is unclear. We aimed to investigate whether negative wealth shocks in later life are associated with cognitive function in older adults in China, England, Mexico, and the USA, and whether this association is modified by country income level.
Methods
For this population-based, cross-nationally harmonised, longitudinal study, data were analysed from core interviews of the population-based US Health and Retirement Study (2012 and 2016) and its partner studies in China (the China Health and Retirement Longitudinal Study; 2015 and 2018), England (the English Longitudinal Study of Ageing; 2012 and 2016), and Mexico (Mexican Health and Aging Study; 2012 and 2015–16), and their respective Harmonized Cognitive Assessment Protocols (HCAPs). Negative wealth shocks over the follow-up periods of the respective cohorts were defined in two ways: an extreme loss of 75% or greater from the baseline amount of wealth, and a decline in within-population wealth quintile rank. The primary outcome was the harmonised general cognitive function (GCF) factor score, which was constructed with factor analysis on the HCAP neuropsychological assessments of memory, orientation, attention, executive function, and verbal fluency performance (mean 0; SD 1). We used sampling-weighted, multivariable-adjusted linear models to examine associations.
Findings
Data from 9465 participants were included in this analysis: 3796 from China, 1184 from England, 1193 from Mexico, and 3292 from the USA. The mean baseline age of participants was 68·5 (SD 5·4) years in China (49·8% women), 72·0 (7·0) years in England (54·6% women), 70·6 (6·8) years in Mexico (55·1% women), and 72·7 (7·5) years in the USA (60·4% women). A wealth loss of 75% or greater was negatively associated with subsequent cognitive function in the USA (β −0·16 SD units; 95% CI −0·29 to −0·04) and China (−0·14; −0·21 to −0·07), but not in England (−0·01; −0·24 to 0·22) or Mexico (−0·11; −0·24 to 0·03). Similarly, within-population wealth quintile rank declines were negatively associated with subsequent cognitive function in the USA (β −0·07 per quintile rank decline; 95% CI −0·11 to −0·03) and China (β −0·07; −0·09 to −0·04), but not in England (−0·05; −0·11 to 0·01) or Mexico (−0·03; −0·07 to 0·01).
Interpretation
The impact of wealth shocks in later life on subsequent lower level of cognitive function of older adults in China, England, Mexico, and the USA differed across macro-level socioeconomic structures. These findings suggest that government policies and social safety nets in countries with different levels of economic development might have a role in protecting older adults from adverse health effects of wealth losses in later life.
Funding
US National Institute on Aging, US National Institutes of Health.
Introduction
Dementia is a major public health and clinical concern for the growing ageing population worldwide.1 Cognitive decline is a hallmark early symptom of dementia, and poor cognitive function in later life can affect daily function, quality of life, and wellbeing. Evidence from countries with diverse social and economic structures consistently indicates that markers of socioeconomic position across the life course—such as education, employment, income, and wealth—affect cognitive function, decline, and dementia risk in later life.1-6 Wealth reflects aggregate economic capital that can be drawn upon to protect health, especially for older adults who are at or above retirement age and might have insufficient or no employment income. Wealth losses in later life can increase stress, worsen mental health, reduce spending on health care and basic needs such as food, and change time allocation (eg, from social engagement to fulfilling financial obligations resulting from wealth losses), all of which might be harmful for cognitive function.7,8 Negative wealth shocks—defined as a sudden major loss in total net worth—could occur due to personal stressful life events, such as a divorce or major illness in the family, or an economic crisis, such as the 2008 Great Recession.9 Negative wealth shocks have been associated with mid-life elevated depressive symptoms,9,10 mid-life psychiatric disorders,11 and increased risk of all-cause mortality in later life,12 supporting the plausibility of their association with cognitive health outcomes in later life.
The fact that the potential cognitive health effects of negative wealth shocks could be modified by the macrosocial context of a country warrants attention, as many countries around the world are experiencing slowdowns in economic growth and rising inflation, and many households are experiencing economic volatility.13,14 Middle-income (eg, China and Mexico) and high-income countries (eg, England and the USA) face dissimilar levels of economic inequality and provide disparate levels of social support. Inequalities in disposable income among people aged 65 years and older are highest in China, followed by Mexico, the USA, and England, although income inequality has decreased in Mexico and increased in the USA in the past decade.15 Additionally, England has a public health-care system, and although the USA provides public health care for adults aged 65 years and older through Medicare, a federal health insurance programme, there are certain eligibility requirements to receive Medicare benefits. In China and Mexico, all citizens are entitled to receive public health care, although disparities exist in the coverage, quality, and accessibility of medical resources. Moreover, all four countries provide public pensions. However, compared with China and Mexico, England and the USA contribute a larger share of spending on public pensions.15 Contextual differences in the social safety nets provided by these countries could affect older adults’ experiences of negative wealth shocks, although whether and how these effects vary across countries is unknown.
Using harmonised data from four nationally representative longitudinal studies of ageing in China, England, Mexico, and the USA, we aimed to assess the association between negative wealth shocks in later life and subsequent lower level of cognitive function in older adults, and to evaluate whether this association varied across these four middle-income and high-income countries. We hypothesised that negative wealth shocks are negatively associated with cognitive function in later life across all four countries; and that the magnitude of the association is stronger in the two middle-income countries (China and Mexico) than in the two high-income countries (England and the USA), potentially due to fewer available social safety nets for older adults, lower levels of economic development, and greater economic inequality in these countries.
Methods
Study population
For this population-based, cross-nationally harmonised, longitudinal study, data were analysed from core interviews of the population-based US Health and Retirement Study (HRS; 2012 and 2016) and its harmonised, population-based, international partner studies: the China Health and Retirement Longitudinal Study (CHARLS; 2015 and 2018), the English Longitudinal Study of Ageing (ELSA; 2012 and 2016), and the Mexican Health and Aging Study (MHAS; 2012 and 2015–16). We linked these cohorts to their respective Harmonized Cognitive Assessment Protocol (HCAP) substudies: the US Health and Retirement Study Harmonized Cognitive Assessment Protocol (HRS-HCAP; 2016), the CHARLS Harmonized Cognitive and Dementia Assessment in China (CHARLS-HCAP; 2018), the ELSA Healthy Cognitive Ageing Project (ELSA-HCAP; 2018), and the MHAS Cognitive Aging Ancillary Study (Mex-Cog; 2016). All parent cohort studies collected nationally representative random samples. The minimum inclusion age is 51 years in the HRS, 50 years in ELSA and MHAS, and 45 years in CHARLS. HRS-HCAP and ELSA-HCAP comprise random samples of participants aged 65 years and older in each parent cohort in 2016, Mex-Cog is a random sample of participants aged 55 years and older in the 2015–16 parent cohort, and CHARLS-HCAP includes all CHARLS participants aged 60 years and older in the 2018 parent cohort. An overview of datasets, timepoints, and references to additional documentation on the study design and methods for each cohort and its embedded HCAP study is provided in the appendix (p 2). We included HCAP participants from each parent cohort who were aged 65 years or older when the HCAP was administered, to ensure that samples were of consistent ages across countries. The study population comprised 9465 individuals in total: 3796 in China, 1184 in England, 1193 in Mexico, and 3292 in the USA. The study flow diagrams are provided in the appendix (pp 3-6).
Local institutional review boards gave ethical approval for all parent cohorts and their HCAP substudies used here. All recruited people provided written consent to participate in the study. HRS was approved by the Health Sciences/Behavioral Sciences Institutional Review Board at the University of Michigan (Ann Arbor, MI, USA; HUM00061128). CHARLS was approved by the Biomedical Ethics Review Committee of Peking University (Beijing, China; IRB00001052–11015). ELSA was approved by the National Health Service Research Ethics Committees under the National Research and Ethics Service (NRES Committee South Central – Berkshire approval on ELSA Wave 6: 11/SC/0374, and Wave 8: 15/SC/0526). MHAS was approved by the Institutional Review Board or Ethics Committee of the University of Texas Medical Branch (Galveston, TX, USA), the Instituto Nacional de Estadística y Geografía (Aguascalientes, Mexico), and the Instituto Nacional de Salud Pública (Mexico City, Mexico). This analysis was deemed exempt from human subjects’ regulation by the Health Sciences and Behavioral Sciences Institutional Review Board at the University of Michigan (HUM00178420).
Measurement of general cognitive function
The primary outcome was the harmonised general cognitive function (GCF) factor score, capturing HCAP data on memory, orientation, attention, executive function, and verbal fluency performance.16 The HCAP is a neuropsychological battery that was designed to facilitate cross-national comparisons of later-life cognitive function, impairment, and dementia, through a suite of validated test items capturing domains of memory, orientation, attention, and verbal fluency. In-depth details of the selection and content of individual neuropsychological test items included in HCAP are available elsewhere.16 All HCAP materials were translated into local languages and adapted for cultural and educational appropriateness across countries, and all HCAP interviews were conducted in person by trained interviewers. We conducted a rigorous pre-statistical and statistical harmonisation procedure to generate a cross-nationally harmonised GCF factor score.17-19 In brief, we first convened an expert panel of cultural neuropsychologists and epidemiologists to identify HCAP test items that were comparable and non-comparable, based on necessary translations and adaptations across countries, in consultation with primary fieldwork study teams. We then used an item-banking approach whereby a confirmatory factor analysis model was estimated to generate a GCF factor score for the first study (HRS-HCAP), and item parameters from this model were saved to our item bank. We then estimated a second confirmatory factor analysis model for the second study (ELSA-HCAP), holding item parameters constant for items deemed comparable to those in HRS-HCAP, and freely estimating parameters for items that were non-comparable to those in HRS-HCAP. We then repeated this process to generate GCF factor scores for the third and fourth studies (Mex-Cog and CHARLS-HCAP). The confirmatory factor analysis models were of good fit to the data across countries according to standard model fit statistics (ie, root mean square error of approximation, comparative fit index, and standardised root mean residual), and robust to the order in which countries were added to the item bank. The final harmonised GCF factor score was standardised to the distribution of the HRS-HCAP sample, which had a mean of 0 and an SD of 1. Model estimates in this analysis are thus expressed in SD units of the HRS-HCAP study population distribution.
Measurement of negative wealth shocks
The exposure was negative household wealth shocks from 2012 to 2016 for the USA, from 2012 to 2016 for England, from 2012 to 2015 for Mexico, and from 2015 to 2018 for China. For each country, wealth was measured with couple-level wealth variables (total net worth of assets owned by one and one’s spouse or partner) derived from the 2018 US RAND HRS Longitudinal File for the HRS, and from the harmonised ELSA, MHAS, and CHARLS datasets provided on the Gateway to Global Aging Data website. The components of wealth considered in each country are documented in the appendix (p 7). Wealth per capita at each timepoint was constructed by dividing wealth by 1·5 for coupled households and by 1 for single households.20 Imputed wealth data were provided by survey study teams, except for the 2015 wealth data in CHARLS, which were the raw records reported by study participants. Approximately 38% of participants from the CHARLS sample and 2% of participants from the ELSA sample were excluded due to missing data on wealth. However, the characteristics of excluded participants were largely similar to those who were included (appendix pp 8-9).
Using the per-capita wealth measures, we created two exposure variables to measure negative wealth shocks. First, consistent with previous research, we defined an extreme wealth loss as a 75% or greater loss in wealth from the baseline value over the 3–4-year follow-up period.9,12 Second, we created a continuous variable representing a change in within-population wealth quintile ranking over the follow-up period (range: −4 to 4), to capture more subtle volatilities over time in an individual’s relative wealth ranking within their country. For example, moving from the top 20% of the population wealth distribution to the bottom 20% of the population wealth distribution would result in a value of 4 (ie, a decline of four quintiles) for this variable.
Covariates
We selected as model covariates sociodemographic, lifestyle-related, and health-related factors that might be common causes (confounders) of the association between negative wealth shocks and subsequent lower level of cognitive function; data were collected at baseline in each cohort, guided by a directed acyclic graph shown in the appendix (p 10). Sociodemographic factors were age (linear and quadratic terms), sex (male or female), marital status (married or partnered, separated or divorced, widowed, and never married), minority status indicator (minority racial or ethnic group for England and the USA, and rural or urban residential status for China and Mexico), household size, highest educational attainment harmonised according to the International Standard Classification of Education (ISCED) 2011 (lower secondary education or below, upper secondary education, and more than upper secondary education),21 father’s and mother’s education according to the ISCED 2011 (less than primary education, primary education, and secondary education or higher), and baseline household wealth quintile. The lifestyle attributes were smoking status (current smoker, former smoker, or never smoker) and BMI (underweight or normal [<25·0 kg/m2], overweight [25·0–29·9 kg/m2], and obese [≥30·0 kg/m2]). Health conditions were a categorical composite of self-reported physician-diagnosed conditions (0, 1, 2, and ≥3 for each of hypertension, diabetes, stroke, cancer, and chronic lung disease), self-reported health status (excellent, very good, good, fair, and poor), screening for positive depressive symptoms (yes vs no) according to the Center for Epidemiologic Studies Depression Scale (scores ≥3/8 for England and the USA,22 ≥5/9 for Mexico,23 and ≥10/30 for China24), and within-country episodic memory scores in quartiles. Episodic memory was measured as immediate and delayed oral recall of a brief word list read out loud by the interviewer in the main parent cohort interviews in all four countries under study. Because episodic memory is highly sensitive to ageing-related change and episodic memory loss is a hallmark early symptom of dementia,1 we controlled for episodic memory before negative wealth shock as assessed in each main parent cohort at our analytical baseline to help rule out the possibility of reverse causation. Although the neuropsychological construct assessed by tests of immediate and delayed recall is the same across countries, the number of words presented in the recall tests varied across countries, resulting in different scale ranges, so we created within-country quartiles of memory scores to harmonise this variable. Up to 14·3% of data were missing in the covariates (appendix p 11). To account for missing data, we did multiple imputation by chained equations considering all the covariates used in the main analysis.
Statistical analysis
We estimated the associations of extreme wealth loss and decline in within-population wealth quintile rank with subsequent cognitive function using multivariable-adjusted linear regression models. First, we ran models stratified by country to estimate the country-specific associations between each negative wealth shock exposure measure and subsequent lower level of cognitive function. Then, we ran models with data from all countries pooled together. The pooled models estimated the marginal differences in estimates for China, England, and Mexico, relative to the USA as the reference. All models were adjusted for the covariates listed above, and all models incorporated survey sampling weights to make inferences for the older populations (ie, those aged ≥61 years) of each country. The survey sampling weights accounted for differential selection probabilities and response rates for each parent cohort. In pooled analyses, within-country sampling weights were further rescaled so that each country had a sampling weight proportional to its HCAP sample size. All model standard errors were adjusted for household clusters and accounted for country strata.
We did a series of sensitivity analyses to assess the robustness of our findings. First, we re-ran the models using stabilised inverse probability of treatment weights (mean 1·00 [SD 0·06], range 0·04–2·06) to address time-varying confounders: marital status, physician-diagnosed health conditions, self-reported health status, and screening positive for depressive symptoms. The final weights were the product of the inverse probability of treatment weights and sampling weights.25 This analysis aimed to account for the potential impacts of stressful, time-varying personal events during the exposure period (eg, marriage loss through widowhood, divorce, or separation, and comorbid health conditions) on cognitive function. Second, we re-ran the models with primary residential assets and liquid assets instead of total wealth to construct the wealth shock exposure variables, since market-based changes in housing value might cause large fluctuations in total wealth. Third, to examine more fine-grained fluctuations in wealth, we used declines in wealth deciles rather than declines in wealth quintiles as the within-population wealth rank change exposure variable. Although this fine categorisation allows investigation of subtle changes in rank across the population wealth distribution, it is more sensitive to non-differential misclassification due to self-reporting or random errors due to regional market dynamics (eg, inflation rates). Fourth, to focus on older adults at similar stages of financial worries related to retirement, we re-ran our analyses to only include individuals who were at each country’s official retirement age at baseline: 66 years or older for the USA (n=2569), 65 years or older for England (n=985), 65 years or older for Mexico (n=930), and 60 years or older for China (n=3796).15 Additionally, we re-ran our analyses on two subsamples by HCAP participants’ age at follow-up (65–74 years vs ≥75 years). Finally, we re-ran our analyses on covariates before imputation to assess the impact of imputation on our findings. All analyses were done with Stata SE 17.0.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
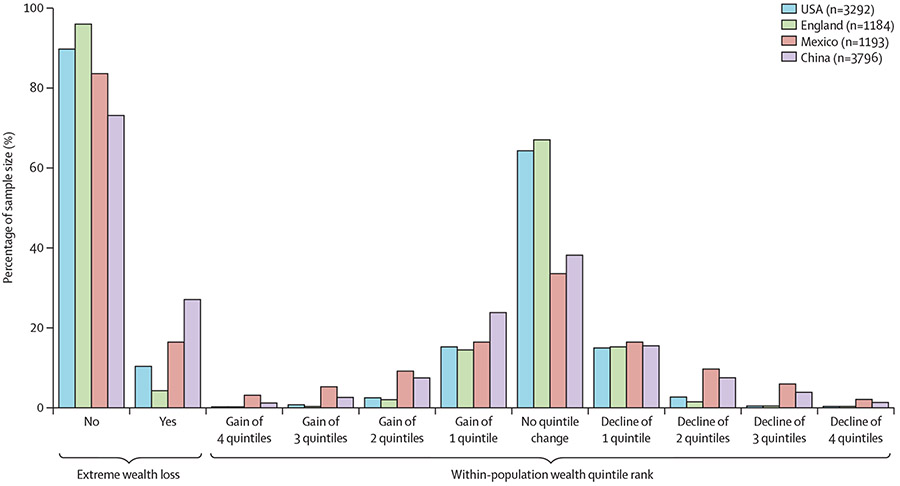
Data from 9465 participants were included in this analysis (table). Extreme wealth loss was less common among older adults in the USA (10·2%) and England (4·1%) than among those in Mexico (16·3%) and China (26·9%). Similarly, within-population declines in wealth quintile rank were more common in China and Mexico than in the USA and England (figure 1). The mean GCF scores in China and Mexico were lower than those in England and the USA.
Table:
Participant characteristics by country
| HRS (USA; n=3292) |
ELSA (England; n=1184) |
MHAS (Mexico; n=1193) |
CHARLS (China; n=3796) |
|
|---|---|---|---|---|
| Mean age (years) | 72·7 (7·5) | 72·0 (7·0) | 70·6 (6·8) | 68·5 (5·4) |
| Sex | ||||
| Female | 1990 (60·4%) | 646 (54·6%) | 657 (55·1%) | 1890 (49·8%) |
| Male | 1302 (39·6%) | 538 (45·4%) | 536 (44·9%) | 1906 (50·2%) |
| Marital status | ||||
| Married or living with partner | 2073 (63·0%) | 808 (68·2%) | 776 (65·1%) | 3001 (79·1%) |
| Separated or divorced | 426 (12·9%) | 102 (8·6%) | 76 (6·4%) | 24 (0·6%) |
| Widowed | 684 (20·8%) | 220 (18·6%) | 291 (24·4%) | 747 (19·7%) |
| Never married | 109 (3·3%) | 54 (4·6%) | 50 (4·2%) | 24 (0·6%) |
| Minority group | 940 (28·6%) | 38 (3·2%) | 343 (28·8%) | 2427 (63·9%) |
| Median household size (people) | 2 (0 to 2) | 2 (1 to 2) | 2 (2 to 4) | 2 (2 to 3) |
| Educational attainment | ||||
| Lower secondary education or below | 598 (18·2%) | 461 (38·9%) | 1088 (91·2%) | 3555 (93·7%) |
| Upper secondary | 1749 (53·1%) | 219 (18·5%) | 26 (2·2%) | 195 (5·1%) |
| Higher than upper secondary | 945 (28·7%) | 504 (42·6%) | 79 (6·6%) | 46 (1·2%) |
| Father’s educational attainment | ||||
| Less than primary | 319 (9·7%) | 39 (3·3%) | 915 (76·7%) | 2809 (74·0%) |
| Primary | 653 (19·8%) | 901 (76·1%) | 155 (13·0%) | 797 (21·0%) |
| Secondary or higher | 2320 (70·5%) | 244 (20·6%) | 123 (10·3%) | 190 (5·0%) |
| Mother’s educational attainment | ||||
| Less than primary | 137 (4·2%) | 29 (2·4%) | 1012 (84·8%) | 3656 (96·3%) |
| Primary | 515 (15·6%) | 921 (77·8%) | 137 (11·5%) | 106 (2·8%) |
| Secondary or higher | 2640 (80·2%) | 234 (19·8%) | 44 (3·7%) | 34 (0·9%) |
| Baseline wealth quintiles | ||||
| ≤20% | 812 (24·7%) | 219 (18·5%) | 240 (20·1%) | 786 (20·7%) |
| 21–40% | 699 (21·2%) | 258 (21·8%) | 232 (19·4%) | 888 (23·4%) |
| 41–60% | 634 (19·3%) | 259 (21·9%) | 219 (18·4%) | 818 (21·5%) |
| 61–80% | 581 (17·6%) | 229 (19·3%) | 261 (21·9%) | 734 (19·3%) |
| >80% | 566 (17·2%) | 219 (18·5%) | 241 (20·2%) | 570 (15·0%) |
| Smoking status | ||||
| Current smoker | 308 (9·4%) | 108 (9·1%) | 124 (10·4%) | 1058 (27·9%) |
| Former smoker | 1505 (45·7%) | 646 (54·6%) | 334 (28·0%) | 733 (19·3%) |
| Never smoker | 1479 (44·9%) | 430 (36·3%) | 735 (61·6%) | 2005 (52·8%) |
| BMI category | ||||
| Underweight or normal (<25·0 kg/m2) | 913 (27·7%) | 295 (24·9%) | 441 (37·0%) | 2598 (68·4%) |
| Overweight (25·0–29·9 kg/m2) | 1240 (37·7%) | 501 (42·3%) | 472 (39·6%) | 1007 (26·5%) |
| Obese (≥30·0 kg/m2) | 1139 (34·6%) | 388 (32·8%) | 280 (23·5%) | 191 (5·0%) |
| Number of self-reported diagnosed health conditions | ||||
| 0 | 340 (10·3%) | 290 (24·5%) | 279 (23·4%) | 916 (24·1%) |
| 1 | 851 (25·9%) | 430 (36·3%) | 405 (33·9%) | 1466 (38·6%) |
| 2 | 1123 (34·1%) | 333 (28·1%) | 335 (28·1%) | 987 (26·0%) |
| ≥3 | 978 (29·7%) | 131 (11·1%) | 174 (14·6%) | 427 (11·2%) |
| Self-reported general health | ||||
| Excellent | 299 (9·1%) | 118 (10·0%) | 24 (2·0%) | 47 (1·2%) |
| Very good | 1056 (32·1%) | 333 (28·1%) | 44 (3·7%) | 373 (9·8%) |
| Good | 1113 (33·8%) | 405 (34·2%) | 330 (27·7%) | 431 (11·4%) |
| Fair | 648 (19·7%) | 248 (20·9%) | 652 (54·7%) | 2043 (53·8%) |
| Poor | 176 (5·3%) | 80 (6·8%) | 143 (12·0%) | 902 (23·8%) |
| Positive for depressive symptoms | 605 (18·4%) | 239 (20·2%) | 408 (34·2%) | 1377 (36·3%) |
| Baseline memory score quartiles | ||||
| ≤25% | 1205 (36·6%) | 514 (43·4%) | 407 (34·1%) | 1054 (27·8%) |
| 26–50% | 815 (24·8%) | 262 (22·1%) | 301 (25·2%) | 1175 (31·0%) |
| 51–75% | 654 (19·9%) | 223 (18·8%) | 281 (23·6%) | 1049 (27·6%) |
| >75% | 618 (18·8%) | 185 (15·6%) | 204 (17·1%) | 518 (13·6%) |
| Extreme wealth loss | 336 (10·2%) | 48 (4·1%) | 194 (16·3%) | 1022 (26·9%) |
| Median wealth quintile rank decline (−4 to 4) | 0 (0 to 0) | 0 (0 to 0) | 0 (−1 to 1) | 0 (−1 to 1) |
| Mean GCF factor scores | −0·1 (1·0) | 0·0 (1·1) | −1·2 (0·9) | −1·4 (0·9) |
Data are mean (SD), n (%), or median (IQR). Participant characteristics are obtained from the core interviews of the US Health and Retirement Study (HRS) in 2012; the English Longitudinal Study of Ageing (ELSA) in 2012; the Mexican Health and Aging Study (MHAS) in 2012; and the China Health and Retirement Longitudinal Study (CHARLS) in 2015.
Values are not sampling weighted. GCF=general cognitive function.
Figure 1: Distribution of negative wealth shocks by country.
An extreme wealth loss is defined as a 75% or greater decline from the baseline amount of household wealth.
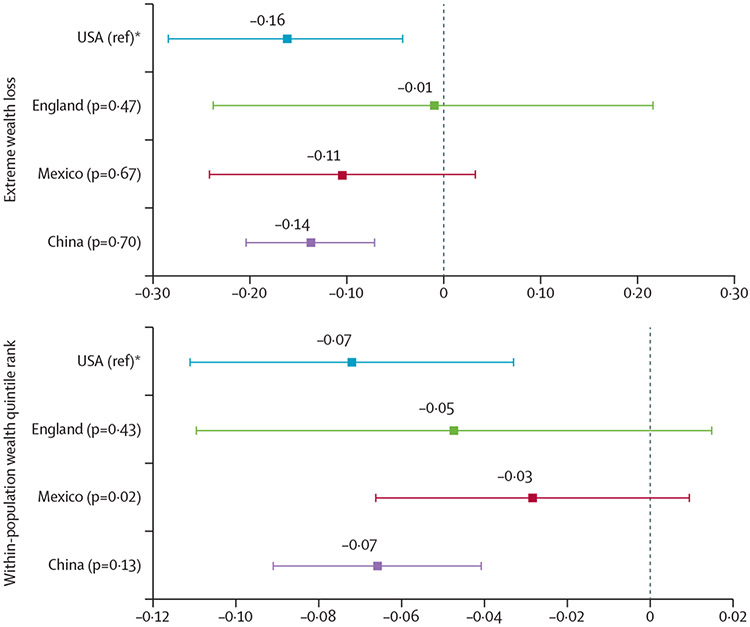
A wealth loss of 75% of total wealth or greater was negatively associated with subsequent cognitive function in the USA (β −0·16 SD units; 95% CI −0·29 to −0·04) and China (−0·14; −0·21 to −0·07), but not in England (−0·01; −0·24 to 0·22) or Mexico (−0·11; −0·24 to 0·03; figure 2). The point estimate for England was close to the null, and was also imprecisely estimated since negative wealth shocks were least common in this population. The estimates for England, Mexico, and China did not differ significantly from that for the USA in the pooled model (figure 2). Declines in within-population wealth quintile ranking were also negatively associated with subsequent cognitive function in the USA (β −0·07 per quintile rank decline; 95% CI −0·11 to −0·03) and China (−0·07; −0·09 to −0·04), but not in England (−0·05; −0·11 to 0·01) or Mexico (−0·03; −0·07 to 0·01; figure 2). The pooled model to test for cross-country differences indicated that the estimate for Mexico was weaker than that for the USA (figure 2).
Figure 2: Adjusted, weighted regression coefficients for the association between negative wealth shocks and subsequent lower level of cognitive function by country.
Estimates are from pooled models stratified by country, adjusted for age, age squared, sex or gender, marital status, minority status, household size, participant’s and parents’ education level, baseline wealth quintile, smoking status, BMI, self-reported diagnosed health conditions, self-reported general health, positive for depressive symptoms, and baseline memory score quartile, and accounted for survey sampling weights and household clusters. An extreme wealth loss is defined as a 75% or greater decline from the baseline amount of household wealth. The error bars show the 95% CIs of the point estimates, which use standard errors adjusted for household clusters, country strata, and sampling weights. *In the parentheses are p values of cross-country interaction effects, with the USA as the reference.
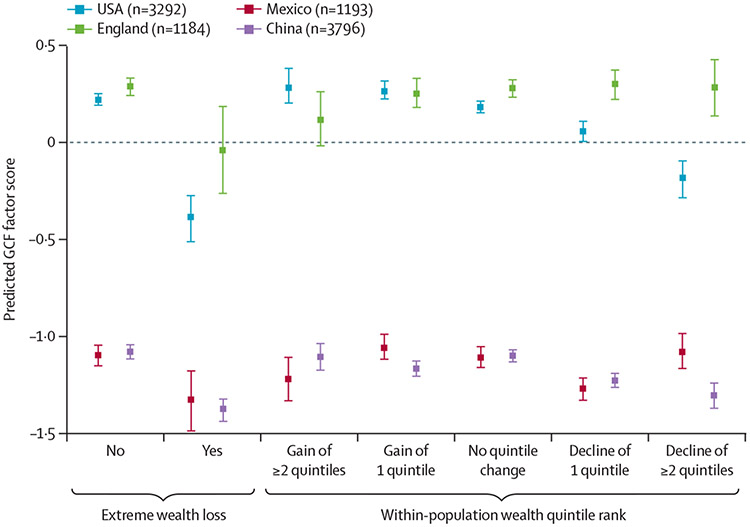
Although some estimates were imprecise, the point estimates mostly showed lower-level cognitive function of older adults who experienced a loss of 75% or greater of total wealth, compared with those who did not, within each country (figure 3). Furthermore, a nearly linear pattern of lower cognitive function across declines in wealth quintile was observed in the USA and China, but not in England and Mexico (figure 3).
Figure 3: Predicted general cognitive function factor scores following negative wealth shock by country.
The predicted GCF scores were based on the pooled models adjusted for age, age squared, sex or gender, marital status, minority status, household size, participant’s and parents’ education level, baseline wealth quintile, smoking status, BMI, self-reported diagnosed health conditions, self-reported general health, positive for depressive symptoms, and baseline memory score quartile, and accounted for survey sampling weights and household clusters. The predicted GCF scores were calculated by holding the covariates at the mean value within each category of negative wealth shock in each study. Individuals who experienced an increase or decrease in two or more quintile ranks were categorised into one group for prediction due to small sample size. An extreme wealth loss is a 75% or greater decline from the baseline amount of household wealth. The error bars show the 95% CIs of the point estimates, which use standard errors adjusted for household clusters, country strata, and sampling weights. GCF=general cognitive function.
The results from the sensitivity analyses were mostly consistent with those from the main analyses, although results were somewhat sensitive to the choice of measure of wealth shock and the stratified analyses often lacked precision due to a reduced sample size (appendix pp 12-17). After controlling for the time-varying confounding effects of marital status and health conditions, the association between negative wealth shocks and cognitive function was similar in all countries (appendix p 12). The association was similar in all countries when restricting to housing value, but was null in most countries when restricting to liquid asset values (appendix pp 13-14). The coefficients of determination of the analysis on housing values and the main analysis were similar, possibly indicating that loss in housing value was primarily contributing to this association (data not shown).
Discussion
In this large, population-based, cross-nationally harmonised, longitudinal study, we found that experiencing a negative wealth shock in later life was associated with a lower level of subsequent cognitive function in China and the USA, but not in England or Mexico. Losses in housing value appeared to largely explain these associations. Although further longitudinal studies are needed, these findings might shed light on the roles of government policies and social safety nets in tempering the adverse health effects of wealth losses in later life in older adults living in middle-income and high-income countries.
To the best of our knowledge, this is the first cross-nationally comparative study to link extreme losses in household wealth in later life to subsequent lower level of cognitive function. Previous research has shown that negative wealth shocks are related to an increased risk of subsequent all-cause mortality,12 elevated depressive symptoms,9 and psychiatric disorders11 among older adults. Among older adults approaching retirement age, economic downturns are also associated with poorer cognitive function in later life.26 This study expands on the available literature by connecting extreme wealth losses and loss in one’s relative rank within their population wealth distribution to a subsequent lower level of cognitive function in later life in a cross-national framework. We also identified new cross-national disparities in the potential impacts of wealth loss in later life on subsequent cognitive health, and these results might largely be driven by losses in housing value.
Our findings are largely consistent with existing studies on absolute values of wealth and cognitive health outcomes in later life in each of the four countries included here.3 Positive associations between household wealth and depressive symptoms, a psychosocial factor that might link wealth shocks and cognition, have also been observed in China,27 England,28 Mexico,29 and the USA.30 Importantly, we observed an association between negative wealth shocks and cognitive function in later life in the USA and China, but not in England or Mexico. The null association in England is noteworthy considering its established public health-care and welfare system (known as benefits).15 Negative wealth shocks were also rarely experienced in England. The less evident association between negative wealth shocks in later life and cognitive function in Mexico might be explained by the non-contributory pension programme introduced in Mexico in 2007 for citizens aged 70 years and older, and subsequent reductions in income inequality among older adults.15 This expanded pension programme has since been shown to promote memory function of adults aged 70 years and older in Mexico,6 consistent with our findings.
This study has several limitations. First, the observed wealth changes could be subject to measurement error, especially as only two waves of longitudinal data on wealth changes were available across all studies. Second, the estimates might be biased by residual confounding, given that we had to coarsen certain model covariates to achieve harmonised covariates for use in the pooled models. For instance, minority status indicates White versus non-White individuals in the USA, regardless of ethnicity, and smoking status identifies former, current, and never smokers, regardless of lifetime smoking frequency and intensity. Our estimates might also be biased by unmeasured confounding, especially if the confounding structures vary across the countries under study. Third, if the pattern of missing data in CHARLS is related to unmeasured variables that are also related to cognitive function, then the results for CHARLS-HCAP might be biased in a direction that is difficult to predict and beyond the scope of this study. Fourth, our results could be subject to reverse causation, whereby declines in cognitive function might lead to wealth losses. We adjusted for baseline episodic memory as a marker of pre-wealth shock dementia risk, but this might not have provided complete control for pre-baseline cognitive trajectories. Future studies should further investigate the potential for reverse causality or bidirectionality of the association between wealth loss and cognitive function in later life.
Strengths of this study include its large sample, which is representative of four diverse middle-income and high-income countries. We used harmonised assessments of general cognitive function as assessed by the HCAP, capturing domains of orientation, language, memory, and executive function. This study is one of the first large, population-representative, harmonised, cross-national comparisons of the potential role of later-life negative wealth shocks on subsequent cognitive function. Our results were robust to control for a comprehensive set of potential confounders as well as to sensitivity analyses that addressed the potential for time-varying confounding by marriage loss and health conditions. Our results could lead to the generation of new hypotheses about potential causal mechanisms. Relevant differences in the macro-level contextual aspects of the USA and China relative to England or Mexico should be investigated, in addition to individual-level mediating factors such as psychosocial and material conditions. Our findings require further investigation and replication in other settings.
In conclusion, this study showed cross-national variation in the association between later-life negative wealth shocks and subsequent lower level of cognitive function. We found that negative wealth shocks were negatively associated with cognitive function in older adults in the USA and China, but not in England or Mexico, which might be due to differences between countries in factors such as government policies and social safety nets for older adults. Future investigation is warranted to confirm our findings, as well as to explore potential mechanisms and reasons for cross-national differences in this association.
Supplementary Material
Research in context.
Evidence before this study
We searched PubMed for cross-national population-based prospective studies published from Nov 10, 2021, to March 6, 2023, examining the association between negative wealth shocks and cognitive function in older adults at or approaching retirement age—about 60 years or older, varying across countries. We used different combinations of the following search terms and synonyms: “cross-country”, “cross-national”, “middle-income”, Mexico”, “China”, “England”, “UK”, “older adult”, “later adulthood”, “later-life”, AND “late-life” for population; “wealth loss”, “wealth shock”, AND “wealth drop” for exposure; and “cognition”, AND “cognitive” for outcome. We found no studies examining the association between negative wealth shocks and cognitive function or whether this association was modified by country. We found previous studies of negative wealth shocks in relation to other health outcomes, and studies of macroeconomic shocks in relation to cognitive function in early life and mid-life. We also found that the correlation of wealth with cognitive outcomes in later life is more often studied in high-income countries than in middle-income countries.
Added value of this study
This population-based, cross-nationally harmonised, longitudinal study explores the association between negative wealth shocks and cognitive function in later life in older adults in China, England, Mexico, and the USA, and compares the magnitude of associations across these four economically distinct middle-income and high-income countries.
Implications of all the available evidence
Our findings suggest that government policies and social support might buffer the potential detrimental effects of later-life wealth losses on cognitive function in middle-income and high-income countries.
Acknowledgments
The Health and Retirement Study is funded by the US National Institute on Aging (U01AG009740) and done at the Institute for Social Research, University of Michigan. LCK was supported by US National Institute on Aging at the US National Institutes of Health (grants P30AG012846, R01AG069128, and R01AG070953). JL was supported by US National Institute on Aging at the US National Institutes of Health (grant R01AG030153). YSZ was supported by US National Institute on Aging at the US National Institutes of Health (grant K99AG070274).
Footnotes
Declaration of interests
We declare no competing interests.
Contributor Information
Tsai-Chin Cho, Center for Social Epidemiology and Population Health, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, MI, USA.
Xuexin Yu, Center for Social Epidemiology and Population Health, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, MI, USA.
Alden L Gross, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health and Johns Hopkins University Center on Aging and Health, Baltimore, MD, USA.
Yuan S Zhang, Robert N. Butler Columbia Aging Center, Department of Sociomedical Sciences, Columbia University Mailman School of Public Health, New York, NY, USA.
Jinkook Lee, Center for Economic and Social Research and Department of Economics, University of Southern California, Los Angeles, CA, USA.
Kenneth M Langa, Department of Internal Medicine, School of Medicine, University of Michigan Institute for Social Research, University of Michigan, Ann Arbor, MI, USA; Veterans Affairs Ann Arbor Center for Clinical Management Research, Ann Arbor, MI, USA; Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, MI, USA.
Lindsay C Kobayashi, Center for Social Epidemiology and Population Health, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, MI, USA.
Data sharing
We downloaded data on the website of the Gateway to Global Aging (https://g2aging.org/). Some datasets are available for public use; others might require additional data access approval. Please contact respective study teams for data use. The contact information of each study team is available on the respective study websites, which can be accessed through the website of the Gateway to Global Aging.
References
- 1.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020; 396: 413–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford KJ, Kobayashi LC, Leist AK. Childhood socioeconomic disadvantage and pathways to memory performance in mid to late adulthood: what matters most? J Gerontol B Psychol Sci Soc Sci 2022; 77: 1478–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cadar D, Lassale C, Davies H, Llewellyn DJ, Batty GD, Steptoe A. Individual and area-based socioeconomic factors associated with dementia incidence in England: evidence from a 12-year follow-up in the English Longitudinal Study of Ageing. JAMA Psychiatry 2018; 75: 723–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu X, Zhang W, Kobayashi LC. Duration of poverty and subsequent cognitive function and decline among older adults in China, 2005–2018. Neurology 2021; 97: e739–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Díaz-Venegas C, Samper-Ternent R, Michaels-Obregón A, Wong R. The effect of educational attainment on cognition of older adults: results from the Mexican Health and Aging Study 2001 and 2012. Aging Ment Health 2019; 23: 1586–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aguila E, Casanova M. Short-term impact of income on cognitive function: evidence from a sample of Mexican older adults. J Aging Health 2020; 32: 591–603. [DOI] [PubMed] [Google Scholar]
- 7.Boen C, Yang YC. The physiological impacts of wealth shocks in late life: evidence from the Great Recession. Soc Sci Med 2016; 150: 221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Desmond M, Kimbro RT. Eviction’s fallout: housing, hardship, and health. Soc Forces 2015; 94: 295–324. [Google Scholar]
- 9.Pool LR, Needham BL, Burgard SA, Elliott MR, de Leon CFM. Negative wealth shock and short-term changes in depressive symptoms and medication adherence among late middle-aged adults. J Epidemiol Community Health 2017; 71: 758–63. [DOI] [PubMed] [Google Scholar]
- 10.Addo FR. Seeking relief: bankruptcy and health outcomes of adult women. SSM Popul Health 2017; 3: 326–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolfe JD, Baker EH, Uddin J, Kirkland S. Varieties of financial stressors and midlife health problems, 1996–2016. J Gerontol B Psychol Sci Soc Sci 2022; 77: 149–59. [DOI] [PubMed] [Google Scholar]
- 12.Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a negative wealth shock with all-cause mortality in middle-aged and older adults in the United States. JAMA 2018; 319: 1341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.OECD. Paying the price of war. OECD economic outlook, interim report. September, 2022. https://www.oecd.org/economic-outlook/september-2022/ (accessed July 21, 2023).
- 14.Chancel L, Piketty T, Saez E, Zucman G, eds. World inequality report 2022. Cambridge, MA: Belknap Press, 2022. [Google Scholar]
- 15.OECD. Pensions at a glance 2021: OECD and G20 indicators. Dec 8, 2021. https://www.oecd.org/els/public-pensions/oecd-pensions-at-a-glance-19991363.htm (accessed June 28, 2023).
- 16.Langa KM, Ryan LH, McCammon RJ, et al. The health and retirement study harmonized cognitive assessment protocol project: study design and methods. Neuroepidemiology 2020; 54: 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briceño EM, Arce Rentería M, Gross AL, et al. A cultural neuropsychological approach to harmonization of cognitive data across culturally and linguistically diverse older adult populations. Neuropsychology 2023; 37: 247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vonk JMJ, Gross AL, Zammit AR, et al. Cross-national harmonization of cognitive measures across HRS HCAP (USA) and LASI-DAD (India). PLoS One 2022; 17: e0264166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gross AL, Li C, Briceño EM, et al. Harmonization of later-life cognitive function across national contexts: results from the harmonized cognitive assessment protocols (HCAPs). medRxiv 2023; published online June 12. 10.1101/2023.06.09.23291217 (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Vos K, Zaidi MA. Equivalence scale sensitivity of poverty statistics for the member states of the European Community. Rev Income Wealth 1997; 43: 319–33. [Google Scholar]
- 21.OECD. ISCED 2011 operational manual: guidelines for classifying national education programmes and related qualifications. Paris: Organisation for Economic Co-operation and Development, 2015. https://www.oecd-ilibrary.org/education/isced-2011-operational-manual_9789264228368-en (accessed June 28, 2023). [Google Scholar]
- 22.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr 1999; 11: 139–48. [DOI] [PubMed] [Google Scholar]
- 23.Alvarez-Cisneros T, Roa-Rojas P, Garcia-Peña C. Longitudinal relationship of diabetes and depressive symptoms in older adults from Mexico: a secondary data analysis. BMJ Open Diabetes Res Care 2020; 8: e001789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fu H, Si L, Guo R. What is the optimal cut-off point of the 10-item Center for Epidemiologic Studies Depression Scale for screening depression among Chinese individuals aged 45 and over? An exploration using latent profile analysis. Front Psychiatry 2022; 13: 820777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference 2015; 3: 237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hessel P, Riumallo-Herl CJ, Leist AK, Berkman LF, Avendano M. Economic downturns, retirement and long-term cognitive function among older Americans. J Gerontol B Psychol Sci Soc Sci 2018; 73: 744–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang R, Zhang C, Xia J, Feng D, Wu S. Household wealth and individuals’ mental health: evidence from the 2012–2018 China Family Panel Survey. Int J Environ Res Public Health 2022; 19: 11569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qin M, Evandrou M, Falkingham J, Vlachantoni A. Did the socio-economic gradient in depression in later-life deteriorate or weaken during the COVID-19 pandemic? New evidence from England using path analysis. Int J Environ Res Public Health 2022; 19: 6700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Torres JM, Rizzo S, Wong R. Lifetime socioeconomic status and late-life health trajectories: longitudinal results from the Mexican Health and Aging Study. J Gerontol B Psychol Sci Soc Sci 2018; 73: 349–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallo WT, Bradley EH, Dubin JA, et al. The persistence of depressive symptoms in older workers who experience involuntary job loss: results from the health and retirement survey. J Gerontol B Psychol Sci Soc Sci 2006; 61: S221–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We downloaded data on the website of the Gateway to Global Aging (https://g2aging.org/). Some datasets are available for public use; others might require additional data access approval. Please contact respective study teams for data use. The contact information of each study team is available on the respective study websites, which can be accessed through the website of the Gateway to Global Aging.