Abstract
Objective
The Transitions of Stroke Care Disparities Study (TCSD-S) is an observational study designed to determine race-ethnic and sex disparities in post-hospital discharge transitions of stroke care and stroke outcomes and to develop hospital-level initiatives to reduce these disparities to improve stroke outcomes.
Materials and Methods
Here, we present the study rationale, describe the methodology, report preliminary outcomes, and discuss a critical need for the development, implementation, and dissemination of interventions for successful post-hospital transition of stroke care. The preliminary outcomes describe the demographic, stroke risk factor, socioeconomic, and acute care characteristics of eligible participants by race-ethnicity and sex. We also report on all-cause and vascular-related death, readmissions, and hospital/emergency room representations at 30- and 90-days after hospital discharge.
Results
The preliminary sample included data from 1048 ischemic stroke and intracerebral hemorrhage discharged from 10 comprehensive stroke centers across the state of Florida. The overall sample was 45% female, 22% Non-Hispanic Black and 21% Hispanic participants, with an average_age of 64±14 years. All cause death, readmissions, or hospital/emergency room representations are 10% and 19% at 30 and 90 days, respectively. One in 5 outcomes was vascular-related.
Conclusions
This study highlights the transition from stroke hospitalization as an area in need for considerable improvement in systems of care for stroke patients discharged from hospital. Results from our preliminary analysis highlight the importance of investigating race-ethnic and sex differences in post-stroke outcomes.
Keywords: stroke, transitions of stroke care, outcomes, mortality, hospital readmissions, methods
Introduction
Despite successful stroke therapies, women, minority, and other disadvantaged populations continue to experience a disproportionate burden of stroke and poor outcomes after stroke (1,2). Hospital based quality improvement stroke programs have demonstrated greater adherence to evidence-based stroke care recommendations. However, it is less evident if the implementation of these programs minimizes race-ethnic, sex and geographic disparities in stroke care post hospitalization. About 25% of discharged stroke patients are readmitted to the hospital within 30 days of initial event (3). Hospital readmission is now an important outcome measure as readmission after discharge has an enormous health care impact and economic burden (4).
In Florida, we have a unique state-wide stroke registry, the Florida Stroke Registry (FSR), funded by the Florida Department of Health. The FSR collects stroke data from 168 Florida hospitals that participate in the Get With the Guidelines Stroke (GWTG-S) program with the main objective to improve stroke care and hospital outcomes (5–7). In 2019, FSR non-Hispanic Black Medicare beneficiaries had higher 1-year post-stroke mortality and 30-day readmission when compared to non-Hispanic White and Hispanic Medicare beneficiaries (8). Similarly, other studies have shown racial/ethnic differences in stroke treatment received, treatment effects, and post stroke outcomes (9, 10). This data underscores the need to prioritize addressing race-ethnic disparities in hospital and post-hospital stroke care.
The Transitions of Care Stroke Disparities-Study (TCSD-S) is a prospective, multi-center observational study funded by the NIH/NIMHD to investigate the drivers of and disparities in factors that lead to successful transition of stroke care (TOSC) after hospital discharge as well as their effects on stroke recurrence and hospital readmission (NCT03452813). The TCSD-S aims to close disparity gaps in transitions of stroke care post hospitalization by determining key factors in transitions of stroke care, including social determinants of health (SDH) and the utilization of stroke prevention care services, rehabilitation, adherence to medication and lifestyle modification interventions, and evaluate disparities in hospital readmissions and long-term stroke outcomes. The results of the TCSD-S will help develop system-level initiatives that can improve TOSC performance and reduce disparities. Following the conceptual framework (Figure 1) where demographic disparities and SDH affect stroke hospitalization, hospital to home transition of stroke care and stroke outcomes, recurrence, and hospital readmissions, we examine disparities in successful transition of stroke care, and identify determinants of hospital readmissions.
Figure 1:
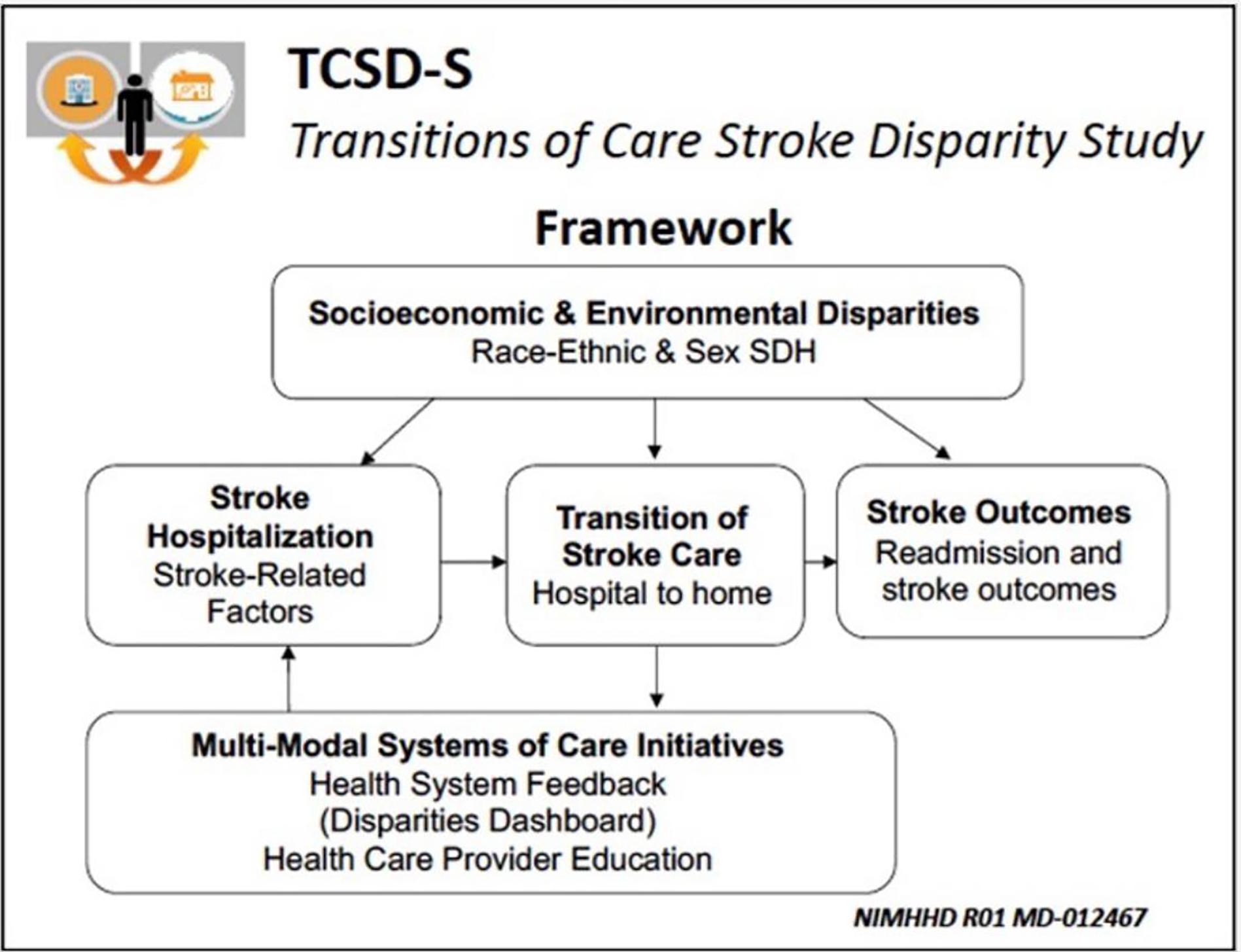
The Framework Diagram of Transitions of Care Stroke Disparities Study (TCSD-S)
Materials and Methods
TCSD-S Design
Participating institutions include 10 nationally certified comprehensive stroke centers participating in FSR, selected as they are representative of the state geographic regions, include a mix of county-operated, privately-owned, and academic institutions, have large stroke volumes, are referral centers that care for minorities with more prevalent stroke disparities, have developed infrastructure and resources to contact patients after discharge, and have more complete GWTG-S data capture. The study was reviewed and approved by the University of Miami Institutional Review Board; participating sites signed a reliance agreement with the central IRB (Institutional Review Board).
Study population:
A total of 1250 stroke patients were enrolled in TSCD-S. For intermediate analyses in this report, 1048 participants had data linked with the GWTG-S and available data on 30 and/or 90-day outcomes.
Inclusion and Exclusion Criteria:
The study includes participants ≥18 years of age with a final diagnosis of stroke or intracerebral hemorrhage, included in the GWTG-S database, and discharged to home or acute inpatient rehabilitation. Those with subarachnoid hemorrhage, TIA, stroke not otherwise specified, no stroke related diagnosis and admission for elective carotid intervention are excluded. We also exclude those discharged to nursing homes, hospice care, or subacute rehabilitation facilities, as these facilities support medication adherence, provide prescribed diets, often provide in-house medical follow-up, and therefore disparities in TOSC are less likely to be detected and not amenable to the proposed study. All participants or their legally appointed representative provided informed consent.
Primary and Secondary Outcomes:
The primary outcome of interest is 90-day readmission. Secondary outcomes include 90-day modified Rankin Score (mRS), 30- and 90-day stroke recurrence, 30-day readmission, death, and other cardiovascular events.
Data Collection:
Data is obtained using three sources: 1) The Transitions of Stroke Care Disparities Study (TCSD-S) data collection, 2) Get with the Guidelines Stroke (GWTG-S), and 3) Sciera™ data. Post-stroke outcomes are obtained through telephone-based structured interviews with the patient or caregiver at 30+/− 7 and 90+/−14 days, and review of patient charts. GWTG-S data provides data about medication use prior to the stroke and at discharge, clinically relevant comorbidities, in-hospital treatment, sociodemographic data, medical history, and clinical characteristics of the index stroke. Each patient is assigned a unique GWTG-S identification number, an identification number of the hospital where they received treatment, and a record/patient identification number. These numbers link the data from GWTG-S with patient data from the TCSD-S dataset. Using zip+4 data from TCSD-S members, Sciera™ data provides environmental-level social determinants of health (SDH) variables, including neighborhood-level socioeconomic status, variables, demographics, and access to various resources and businesses. To quantify successful post-hospital transitions of stroke care we assessed medication adherence, diet modification, toxic habit/substance use cessation, exercise), therapy/rehabilitation use, and medical follow-up appointment at 30-days post-discharge (see Supplemental Table 2 for variable definitions).
Analyses and Statistical Methodologies
Data collected during hospitalization for index stroke are ascertained from GWTG-S data collection tools abstracted by trained hospital personnel, and from baseline TCSD-S specific variables, including TOAST (Trial or Org 10172 in Acute Stroke Treatment) ischemic stroke classification, modified Rankin Score (mRS), education, employment status, ability to pay for basic and medical needs, social support network size, language spoken at home, country of birth, living arrangement, and who is the main source of social support in the household. Case ascertainment for the diagnosis of stroke is performed by prospective clinical identification and retrospective chart review using International Classification of Diseases and discharge codes followed by chart review to confirm the final diagnosis. Data for GWTG-S is collected using an interactive internet-based Patient Management Tool (PMT), including baseline demographic, clinical and medical history and medication use factors, final diagnosis, and stroke mechanism. Pre-specified stroke hospital performance measures are collected (5, 6), including tPA utilization, antithrombotic at discharge, anticoagulation at discharge for atrial fibrillation/flutter, statin medication at discharge for patients with LDL>100, counseling/medication for smoking cessation and other in-hospital lifestyle interventions. We will also use the composite variable of “defect-free care” (DFC) to identify the proportion of patients who received all applicable stroke measures that they are eligible to receive (5).
For each outcome, the time to event is defined as the time from discharge to the onset of the specific outcome event (i.e., readmission). The data are censored at the date of last planned observation, death, or lost to follow-up. We will employ Kaplan-Meier curves to estimate the event-free survivor function grouped by race-ethnicity and sex and perform log rank test to examine whether the survivor functions across the subgroups are the same in a nonparametric way. To investigate whether the effect of race-ethnicity and sex are independent of, or interactive with SDH, we will fit Cox proportional hazards model and estimate the adjusted hazard ratio.
Community Social Determinants of Health (SDH) include health-related features of neighborhoods (walkability) and socioeconomic factors (income, wealth, education) that relate to health outcomes (13) and stroke (14). Community SDH data is acquired from publicly available data sources through an agreement with a third party (Sciera, Inc.™). SDH are identified based on the participant’s zip code+4-digit area of residence, calculated from their address (and obtained through informed consent); if these are unavailable for some participants, we will use the zip code for the recruiting institution in secondary sensitivity analyses. From this data, we calculate distance, density, and count of a variety of businesses (health care facilities, alcohol-selling, tobacco-selling, fast food, restaurants, grocery, gym, and pharmacy). Within the TCSD-S questionnaire, individual SDH questions asked prior to hospital discharge include years in US for foreign-born patients, language spoken at home, years at current address, level of education, employment status, difficulty paying for essentials, and social support network (i.e., number of friends, living arrangement). Future publications will investigate the complex relationships between SDH and post-stroke transitions of care outcomes.
Discharge education and guidance provided to patients are recorded by GWTG-S. Receipt of discharge education and guidance are patient-reported via telephone survey at 30 days post-discharge, with structured interview questions indicating receipt of three forms of health education and guidance at discharge: tobacco/alcohol/drug cessation (only applicable to patients with a history of substance use), dietary management, and medical follow-up appointment. Participant-reported sufficient discharge education and guidance is a composite measure consisting of patient responses to questions evaluating receipt or sufficient education and guidance provided at hospital discharge. These binary (yes/no) questions provided to participants at 30 day post-discharge address patient receipt of sufficient dietary education (Were you provided sufficient information about how to modify your diet once you returned home?), receipt of scheduled follow-up medical appointment (Did you receive appointments for medical follow-up in clinic or doctor’s office at hospital discharge?), and receipt of sufficient substance use education for participants with a history of substance use (At the time of discharge, were you given sufficient information about how to stop these habits?).
To define successful transition of stroke care, we will construct and validate a transitions of stroke care performance index (TOSC PI), which will serve as an evaluation tool to detect disparities and measure relationships with outcomes including readmission. We will examine this performance index as a potential predictor of stroke outcomes. We will also examine social determinants of health as predictors of this performance index, as a measure to quantify adequate transitions of care. TOSC PI incorporates: 1) Medication adherence (high, medium, and low, based on the MMA-4 scoring classification (11); 2) Diet, characterized as modified diet with lower salt and greater fruit and vegetable intake; 3) Substance (tobacco, drug, or excessive alcohol) use for those that used or abused these agents prior to stroke; 4) Exercise, any aerobic, strengthening, or stretching exercise per week (12); 5) Participation in prescribed outpatient therapy; and 6) Medical follow-up by outpatient health provider. We hypothesize that a high TOSC PI is a protective factor against poor post-stroke outcomes (stroke recurrence, hospital readmission, presentation to the emergency room, and death).
We will examine the TOSC PI score as a continuous variable. In addition to the composite score, we will also examine the six individual TOSC measures as categorical variables separately and will determine adequate transitions of care through a binary (yes/no) variable. Patients that have completed all applicable components of the TOSC PI within 30 days (TOSC PI = 100%) are defined as having achieved adequate transitions of care. Univariate analyses will be performed to evaluate the relation to individual sociodemographic and clinical characteristics and community sociodemographic factors using t-test or F-test for the composite score and c2 test for individual categorical TOSC measures. Using a generalized estimating equations (GEE) approach to account for the clustering by stroke center, we will employ generalized linear models (GLM) to examine the independent and interactive effects of select covariates on the TOSC PI. Specifically, we will model composite TOSC PI score via linear regression as a function of demographics, medical history, and social determinants of health by assuming normal distribution and using an identity link function. For the individual TOSC performance measures, we will model each categorical component using logistic regression as a function of demographics, medical history, and social determinants of health by assuming binomial distribution and using a logit link function.
Statistical analyses are planned to compare the race-ethnic and sex differences in TOSC performance (as measured by the PI) and poor stroke outcomes and identify the individual and community-level sociodemographic determinants. For the analyses of TOSC performance and stroke outcomes, we will create a series of multivariable-adjusted regression models to examine whether any observed race/ethnic and sex disparities persist after controlling for potential explanatory factors. Variables that may be potential determinants and are of interest include stroke-related factors at discharge (e.g., independent ambulation status), insurance status (Medicaid and self-pay vs. Medicare and private), vascular risk factors (e.g., hypertension, dyslipidemia, smoking, medical history of atrial fibrillation, coronary heart disease or myocardial infarction, diabetes mellitus, and peripheral vascular disease), discharge counseling and education (including sufficient discharge education and guidance), and SDH factors. These variables will be included in a sequence of multivariable-adjusted models.
As an exploratory analysis, we will perform classification and regression tree (CART) analysis to explore the high order interactions. We will examine the frequency of missing data for race/ethnicity, TOSC performance indicators, and the covariates of interest. We will also evaluate the patterns of missingness to determine whether missingness of race/ethnicity and covariates are related to the TOSC performance indicators, and whether missingness of the covariates and TOSC performance indicators differs across race/ethnic and sex groups.
Sample size and power were calculated based on the quantitative 30-day TOSC PI, the main metric of race-ethnic and sex disparities in TOSC. After calculating effect sizes of predictors required for 80% power, we derived sample sizes at two-sided type I error= 0.05. To determine the effect of hospital-to-home transitions of stroke care (achievement of 100% TOSC PI) on poor 0–90-day stroke outcomes (all-cause death, readmission, or hospital/emergency room (ER) representation), a sample size of 1048 should provide at least 80% power to detect an effect size of protective OR = 0.58 (15). For the same analysis examined within a 0–30-day timeframe, a sample size of 1048 should provide at least 80% power to detect an effect size of protective OR=0.47 (15).
We calculated sample size required for estimated detectable effect sizes (hazards ratio: HR) for 80% power for Cox regression analysis of 100% TOSC PI on 90-day outcomes at two-sided type I error=0.05 [16, 17] by assuming a range of readmission rates during the 90 days follow-up. To detect an estimated protective HR= 0.75, we require a sample size of 1058 for 80% power. In our Center for Medicaid Services-matched Florida Stroke Registry data, 30-day readmission rates were at 12% between the years 2017–2019. Previous literature has demonstrated all-cause hospital readmission rates of 12% at 30 days [18] and 25.5% at 90 days [19].
Statistical Analysis for Preliminary Results
In our preliminary analysis, we utilized GWTG-S and TCSD-S specific data that includes individual-level SDH but did not include external Sciera™ data for community-level SDH. We report on both all-cause and vascular-related death, readmissions, or hospital/emergency room (ER) representations within 30-and 90-days post-discharge. Hospital/ER representation is a patient-reported return to the hospital or emergency room after their initial stroke discharge. We include this measure in our outcome of interest for power purposes. Patients that re-presented to the hospital or ER were either released or readmitted to the hospital. All-cause readmission within 30 days and 90 days includes all causes of readmission (including unknown cause or other causes). Death is defined as a hospital-or-family/representative-reported death within 30 days or 90 days. For some patients in the cohort, these three outcomes may overlap. All-cause Hospital/ER representation at 30 days and 90 days includes all causes/reasons for representation (including unknown cause or other causes). Vascular-specific readmission or hospital/ER representation requires the hospital coordinator to use patient records to specify the final diagnosis for 30- and 90-day readmission or hospital/ER visit. A readmission is determined as vascular-related if the patient was diagnosed with the following: new ischemic stroke, reactivation of old deficit, transient ischemic attack, intracerebral hemorrhage, acute coronary syndrome, or congestive heart failure. Vascular-specific death is classified from hospital coordinators that find patient records with a final cause of death as ischemic stroke, intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage, myocardial infarction, congestive heart failure, or arrhythmia.
All preliminary analyses use chi-square test to observe frequencies of categorical variables and t-test or F-test for continuous variables. For all statistical tests, we used two-sided hypothesis testing with a significance level of 0.05. All analyses were conducted using SAS Version 9.4. Variables with denominators smaller than the overall sample size (n=1048) include race/ethnicity, statin medication prescribed at discharge, anticoagulation medication prescribed at discharge, TOAST for ischemic stroke mechanism classification, intracerebral hemorrhage score, substance use/toxic habit cessation, and smoking cessation counseling referral. Those with missing race-ethnic data (4%) but other data available are excluded from race/ethnicity specific analyses.
Results
TCSD-S Patient Population Characteristics
In this preliminary analysis, we report on 1048 eligible participants with linked GWTG-S data enrolled from June 2018 through October 2022. Table 1 provides the descriptive characteristics. The overall cohort has an average age of 64±14 years; 45% female, 22% non-Hispanic Black, and 21% Hispanic participants. Non-Hispanic Black participants were younger (58±13 years). Prevalent stroke risk factors in the overall cohort included hypertension (76%), dyslipidemia (44%), diabetes mellitus (30%), and smoking (22%). The prevalence of hypertension was 71% in Non-Hispanic White, 82% in Non-Hispanic Black, and 84% in Hispanic participants.
Table 1.
Characteristics of the TCSD-S population: ischemic stroke and intracerebral hemorrhage discharged directly to home from 10 CSC in Florida in 2018–2022
| All N= 1048 |
White n= 551 |
Black n= 232 |
Hispanic n= 223 |
Male n=575 |
Female n=473 |
|
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, yrs±SD | 63.8 (13.9) | 66.1 (13.2) | 57.7 (12.6) | 65.2 (14.8) | 63.2 (13.1) | 64.6 (14.8) |
| Women, % | 45.1 | 45.0 | 50.4 | 40.3 | . | . |
| Black, % | 22.1 | . | . | . | 20.9 | 25.7 |
| Hispanic, % | 21.3 | . | . | . | 24.1 | 19.8 |
| Stroke Risk Factors % | ||||||
| Smoker | 22.2 | 24.5 | 23.7 | 17.0 | 24.0 | 20.1 |
| Hypertension | 75.6 | 71.1 | 82.3 | 83.9 | 76.9 | 74.0 |
| Diabetes Mellitus | 30.2 | 23.6 | 38.4 | 39.5 | 30.6 | 29.6 |
| Dyslipidemia | 44.4 | 50.3 | 35.3 | 42.6 | 55.1 | 54.7 |
| Atrial Fibrillation/Flutter | 13.5 | 14.9 | 9.9 | 13.5 | 13.6 | 13.3 |
| Discharge medication % | ||||||
| Antithrombotic | 95.8 | 94.4 | 96.4 | 95.6 | 95.3 | 96.5 |
| Antihypertensive | 49.9 | 57.0 | 45.7 | 36.8 | 49.2 | 50.7 |
| Statin* | 99.7 | 99.4 | 100 | 100 | 99.8 | 99.5 |
| Anticoagulation** | 98.7 | 98.0 | 100 | 100 | 97.8 | 100 |
| SDH % | ||||||
| Education | ||||||
| Less than High School | 11.8 | 6.2 | 16.8 | 19.7 | 12.7 | 10.8 |
| Completed High School | 33.9 | 30.1 | 44.4 | 34.5 | 32.0 | 36.2 |
| Some College or More | 54.3 | 63.7 | 38.8 | 45.7 | 55.3 | 53.1 |
| Insurance Status | ||||||
| Private Insurance | 28.6 | 34.6 | 25.9 | 16.6 | 30.3 | 26.6 |
| Medicare | 43.1 | 50.8 | 27.2 | 43.1 | 40.7 | 46.1 |
| Medicaid | 6.1 | 4.2 | 12.1 | 4.5 | 5.2 | 7.2 |
| Self-Pay/No Insurance | 22.1 | 10.3 | 34.9 | 35.9 | 23.8 | 20.1 |
| Foreign Born | 30.4 | 9.4 | 22.8 | 84.8 | 33.4 | 26.9 |
| English Spoken at Home | 79.7 | 95.3 | 89.2 | 30.9 | 77.7 | 82.0 |
| Social Support Network of 3 or More | 78.7 | 76.2 | 79.7 | 83.4 | 77.0 | 80.8 |
| Difficulty Paying for Medical Care | ||||||
| Hard or Very Hard | 25.5 | 19.4 | 36.6 | 42.1 | 26.4 | 24.3 |
| Somewhat Hard | 14.2 | 14.3 | 15.5 | 12.6 | 13.2 | 15.4 |
| Not Very Hard | 57.6 | 68.2 | 46.6 | 44.4 | 57.9 | 57.3 |
| Discharge disposition % | ||||||
| Home | 80.4 | 83.1 | 75.0 | 79.8 | 81.9 | 78.7 |
| Rehabilitation | 19.6 | 16.9 | 25.0 | 20.2 | 18.1 | 21.4 |
| Stroke Type % | ||||||
| Ischemic | 93.0 | 94.0 | 93.1 | 91.0 | 93.0 | 93.0 |
| Intracerebral Hemorrhage | 7.0 | 6.0 | 6.9 | 9.0 | 7.0 | 7.0 |
| TOAST Ischemic Stroke Classification % *** | ||||||
| Large-Artery Atherosclerosis | 18.5 | 16.4 | 18.6 | 23.9 | 19.6 | 17.2 |
| Cardio embolism | 23.2 | 25.4 | 20.1 | 22.6 | 25.5 | 20.5 |
| Small-Vessel Disease | 21.0 | 20.2 | 25.3 | 18.1 | 21.3 | 20.8 |
| Stroke of Undetermined Etiology | 4.3 | 4.6 | 3.1 | 5.2 | 3.4 | 5.4 |
| Cryptogenic Stroke | 33.0 | 33.5 | 33.0 | 30.3 | 30.3 | 36.2 |
| IV tPA (for Ischemic Stroke Patients) % | 21.2 | 20.5 | 20.9 | 23.7 | 20.7 | 21.9 |
| Intracerebral Hemorrhage (ICH) Score % **** | ||||||
| 0–1 | 90.6 | 83.8 | 100 | 80.0 | 94.6 | 85.2 |
| 2–3 | 9.4 | 16.2 | 0.0 | 20.0 | 5.4 | 14.8 |
| Discharge Modified Rankin Scale Score % | ||||||
| 0–1 (No to No significant Disability) | 55.6 | 58.3 | 51.7 | 55.6 | 59.3 | 51.2 |
| 2–5 (Slight to Moderate Disability) | 32.3 | 30.1 | 39.7 | 31.4 | 31.0 | 35.1 |
| 4–5 (Moderately Severe to Severe Disability) | 11.5 | 11.6 | 8.6 | 13.0 | 9.7 | 13.7 |
| NIHSS Mean (SD) | 4.4 (5.4) | 3.7 (4.7) | 5.0 (5.5) | 5.2 (6.5) | 4.1 (5.1) | 4.7 (5.7) |
| 30-Day Post Discharge Healthy Behaviors % | ||||||
| Physical activity, walking or treadmill | 58.3 | 58.8 | 58.1 | 56.5 | 64.3 | 51.0 |
| Diet Modification | 59.9 | 51.2 | 69.8 | 72.2 | 66.0 | 52.4 |
| Substance Use/Toxic Habit Cessation***** | 37.1 | 38.1 | 29.0 | 45.2 | 31.7 | 47.4 |
| Discharge Counseling % | ||||||
| TLC diet recommendation | 54.2 | 58.3 | 50.4 | 47.1 | 53.5 | 46.5 |
| Diabetes teaching | 15.7 | 15.4 | 15.1 | 16.6 | 17.2 | 14.0 |
| Low sodium diet recommendation | 46.2 | 54.1 | 39.7 | 39.9 | 46.4 | 49.0 |
| Smoking cessation counseling referral***** | 16.7 | 14.3 | 23.7 | 19.4 | 18.6 | 13.2 |
| Sufficient Discharge Education and Guidance (Yes) % | 29.0 | 20.7 | 41.4 | 37.7 | 32.7 | 24.5 |
| Adequate Transitions of Care at 30 days (100% TOSC PI) % | 28.6 | 25.8 | 31.5 | 32.7 | 31.3 | 25.4 |
| Adequate Transitions of Care at 30 days (≥75% TOSC PI) % | 62.1 | 59.7 | 62.9 | 66.8 | 65.2 | 58.4 |
[Denominator is only ischemic stroke patients eligible for statin (n = 901)]
[Denominator is only for ischemic stroke patients with atrial fibrillation/flutter (n = 138)]
[Denominator is only for ischemic stroke patients measured for TOAST criteria (n = 865)]
[Denominator is only for intracerebral hemorrhage patients (n=61)]
[Denominator is only for patients that reported a history of substance use prior to stroke (n=221)]
Most participants had an ischemic stroke (93%). Among ischemic stroke participants with recorded TOAST criteria (n=865), most had cryptogenic stroke (33%), followed by cardio embolism (24%) and small-vessel disease (21%). Among hemorrhagic stroke participants (n=61), 91% had a low intracerebral hemorrhage score (0–1) and all participants had scores below 4. Hispanic participants with ischemic strokes had a higher NIHSS (average 5.2), greater use of intravenous tissue plasminogen activator (IV tPA) (24%), and higher prevalence of intracerebral hemorrhage (9%).
Most participants with ischemic stroke received antithrombotic medications, anticoagulation for atrial fibrillation/flutter, and statins, without race/ethnic differences noted in the provision of these medications. For discharge counseling, 54% received recommendations for Therapeutic Lifestyle Changes (TLC) diet and 29% reported having sufficient discharge education and guidance [highest for non-Hispanic Blacks at 41%]. Women were less likely to report having sufficient discharge education (24% female vs 33% male, P = 0.004). Most participants were discharged directly to home (80%).
At 30 days, 62% of participants achieved at least 75% adequate transitions of care (i.e., ≥75% TOSC PI), but only 29% achieved 100% adequate transitions of care (i.e., 100% TOSC PI). Women were less likely to attain 100% adequate transitions of care when compared to men (25% vs 31%, P=0.03).
Table 2 describes total deaths, readmissions, or hospital/emergency room (ER) representations at 30 days and 90 days post-discharge. Overall, 108 (10%) and 200 (19%) participants experienced all-cause death, readmission, or hospital/ER representation at 0–30-days and 0–90-days, respectively. At 30 days, 10 (1%) died and 100 (10%) re-presented to the hospital/ER within 30-days, of whom 62 were readmitted to the hospital. At 90 days, 15 (1%) died and 189 (18%) re-presented to hospital/ER, of whom 127 (67%) were readmitted. Most were readmitted for non-vascular reasons (62% 0–30 days and 72% 0–90 days). Although most patients had an unspecified cause for readmission (51% all within 0–30 days), notable self-reported causes for non-vascular ED representation or readmission included fever (6%), passed out (3%), cough (2%), urination problems (5%), fall and/or trauma and/or fracture (2%) (not shown in table).
Table 2.
30- and 90-Day All-Cause Death, Readmission, or Hospital/ER Representation in the Transitions of Stroke Care Disparities Study (2018–2022)
| Event | 0–30-Day (n=1048) | 0–90-Day (n=1048) | ||
|---|---|---|---|---|
| n | % | n | % | |
| All-Cause Death Readmission or Hospital/ER Representation | 108 | 10.3 | 200 | 19.1 |
| All-Cause Death* | 10 | 1.0 | 15 | 1.4 |
| All-Cause Hospital/ER Representation* | 100 | 9.5 | 189 | 18.0 |
| All-Cause Readmission* | 62 | 5.9 | 127 | 12.1 |
Please note that death, readmission, and hospital/ER representation may overlap for some patients
Table 3 provides descriptive characteristics at 0–30-days and 0–90-days for patients with all-cause and vascular-related death, readmission, or hospital/ER representation. Race-ethnic and sex differences in all-cause and vascular-related 0–30-day and 0–90-day outcomes were not significant. Fewer participants with 100% adequate transitions of care (n=300) experienced 0–30-day all-cause death, readmission, or hospital/ER representation when compared to those with less than 100% group (7.3% vs. 11.5%, p=0.0451). With a more liberal definition of >75% adequate transitions of care (n=651 participants), the 0–30-day all-cause death, readmission, or hospital/ER representation was 7.4% vs. 15% in the less than 75% group (p<0.0001). Amongst those participants reporting sufficient discharge education and guidance, 10% had experienced death, readmission, or hospital/ER representation at 30 days. Only 19% of the 0–30-day deaths, readmissions, or hospital/ER representations were vascular-related, with an average age of 60 years.
Table 3.
Characteristics of 30- and 90-Day All-Cause and Vascular-Related Death, Readmission, or Hospital/ER Representation among the Transitions of Care Disparities Study (2018–2022)
| All Participants (n=1048) | All-Cause Death, Readmission, or Hospital/ER Representation (n=1048) | Vascular-Related Death, Readmission, or Hospital/ER Representation (n=1048) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–30-Day | 0–30-Day | p-value | 0–90-Day | p-value | 0–30-Day | p-value | 0–90-Day | p-value | |
| Age in years, Mean (SD) | 63.8 (13.9) | 63.8 (14.4) | <0.0001 | 63.6 (14.4) | <0.0001 | 59.9 (14.1) | <0.0001 | 59.6 (14.1) | <0.0001 |
| Sex, n (%) | |||||||||
| Male | 575 (54.9) | 53 (9.2) | 0.2015 | 100 (17.4) | 0.1242 | 9 (1.6) | 0.2639 | 17 (3.0) | 0.5621 |
| Female | 473 (45.1) | 55 (11.6) | 100 (21.1) | 12 (2.5) | 17 (3.6) | ||||
| Race/Ethnicity, n (%) * | |||||||||
| Non-Hispanic White | 551 (52.3) | 62 (11.3) | 0.1462 | 107 (19.4) | 0.3540 | 11 (2.0) | 0.9624 | 16 (2.9) | 0.7160 |
| Non-Hispanic Black | 232 (22.1) | 26 (11.2) | 48 (20.7) | 5 (2.2) | 8 (3.5) | ||||
| Hispanic | 223 (21.3) | 15 (6.7) | 35 (15.7) | 4 (1.8) | 9 (4.0) | ||||
| Patient Disposition, n (%) | |||||||||
| Home | 843 (80.4) | 90 (10.7) | 0.4233 | 161 (19.1) | 0.9807 | 19 (2.3) | 0.2415 | 30 (3.6) | 0.2440 |
| Rehabilitation | 205 (19.6) | 18 (8.8) | 39 (19.0) | 2 (1.0) | 4 (2.0) | ||||
| NIHSS, Mean (SD) | 4.4 (5.4) | 5.1 (5.5) | <0.0001 | 4.9 (5.7) | <0.0001 | 3.6 (4.1) | 0.0006 | 3.5 (3.8) | <0.0001 |
| Intracerebral Hemorrhage (ICH) Score, n (%) ** | |||||||||
| 0–1 | 58 (90.6) | 6 (10.3) | 0.0116 | 12 (20.7) | 0.0767 | 0 (0.0) | -- | 1 (1.7) | 0.6628 |
| 2–3 | 6 (9.4) | 3 (50.0) | 4 (66.7) | 0 (0.0) | 0 (0.0) | ||||
| Discharge Modified Rankin Scale Score, n (%) | |||||||||
| 0–1 | 583 (55.6) | 62 (11.6) | 0.7035 | 110 (18.9) | 0.3715 | 14 (2.4) | 0.5174 | 22 (3.8) | 0.6203 |
| 2–3 | 344 (32.8) | 31 (9.0) | 61 (17.7) | 6 (1.7) | 10 (2.9) | ||||
| 4–5 | 121 (11.5) | 15 (12.4) | 29 (24.0) | 1 (0.8) | 2 (1.7) | ||||
| Stroke-Type, n (%) | |||||||||
| Ischemic | 975 (93.0) | 99 (10.2) | 0.5555 | 183 (18.8) | 0.3433 | 21 (2.2) | 0.2053 | 33 (3.4) | 0.3487 |
| Intracerebral Hemorrhage | 73 (7.0) | 9 (12.3) | 17 (23.3) | 0 (0.0) | 1 (1.4) | ||||
| Sufficient Discharge Education and Guidance (Yes) n (%) | 304 (29.0) | 29 (9.5) | 0.6022 | 56 (18.4) | 0.7270 | 6 (2.0) | 0.9645 | 10 (3.3) | 0.9579 |
| Adequate Transitions of Care (100% TOSC PI) % | 300 (28.6) | 22 (7.3) | 0.0451 | 46 (15.3) | 0.0504 | 6 (2.0) | 0.9955 | 9 (3.0) | 0.7774 |
| Adequate Transitions of Care (≥75% TOSC PI) % | 651 (62.1) | 48 (7.4) | <0.0001 | 114 (17.5) | 0.0972 | 11 (1.7) | 0.3528 | 20 (3.1) | 0.6872 |
[Statistics for race/ethnicity other than Non-Hispanic Black, Non-Hispanic White, and Hispanic not shown in race/ethnicity variable not shown but are included in overall sample (n = 42)]
[Denominator is only for patients with intracerebral hemorrhage (n = 64)]
Figure 2 describes all-cause 30-and 90-day death, readmission, or hospital/ER representation by race/ethnicity in the cohort using chi-square analyses. The numerically greater prevalence of combined 0–30-day and 0–90-day outcomes in Non-Hispanic Black participants was not statistically significant. Although women had higher prevalence of readmission or hospital/ER representation than males, differences in post-stroke outcomes were not significant (Figure 3).
Figure 2:
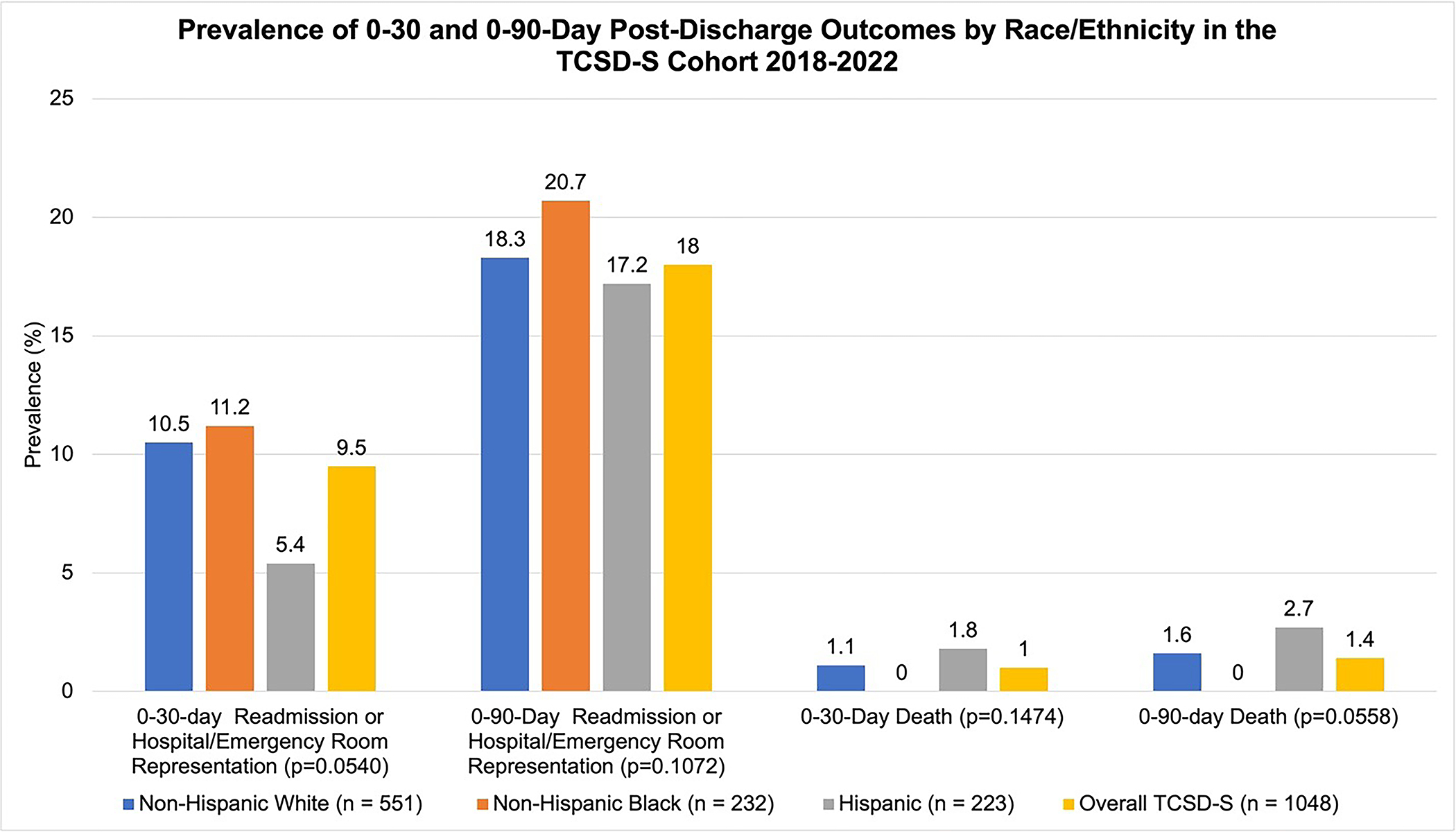
Post-stroke discharge outcomes by race-ethnicity in the TCSD-S cohort for the years 2018–2022 (n=1048).
Figure 3:
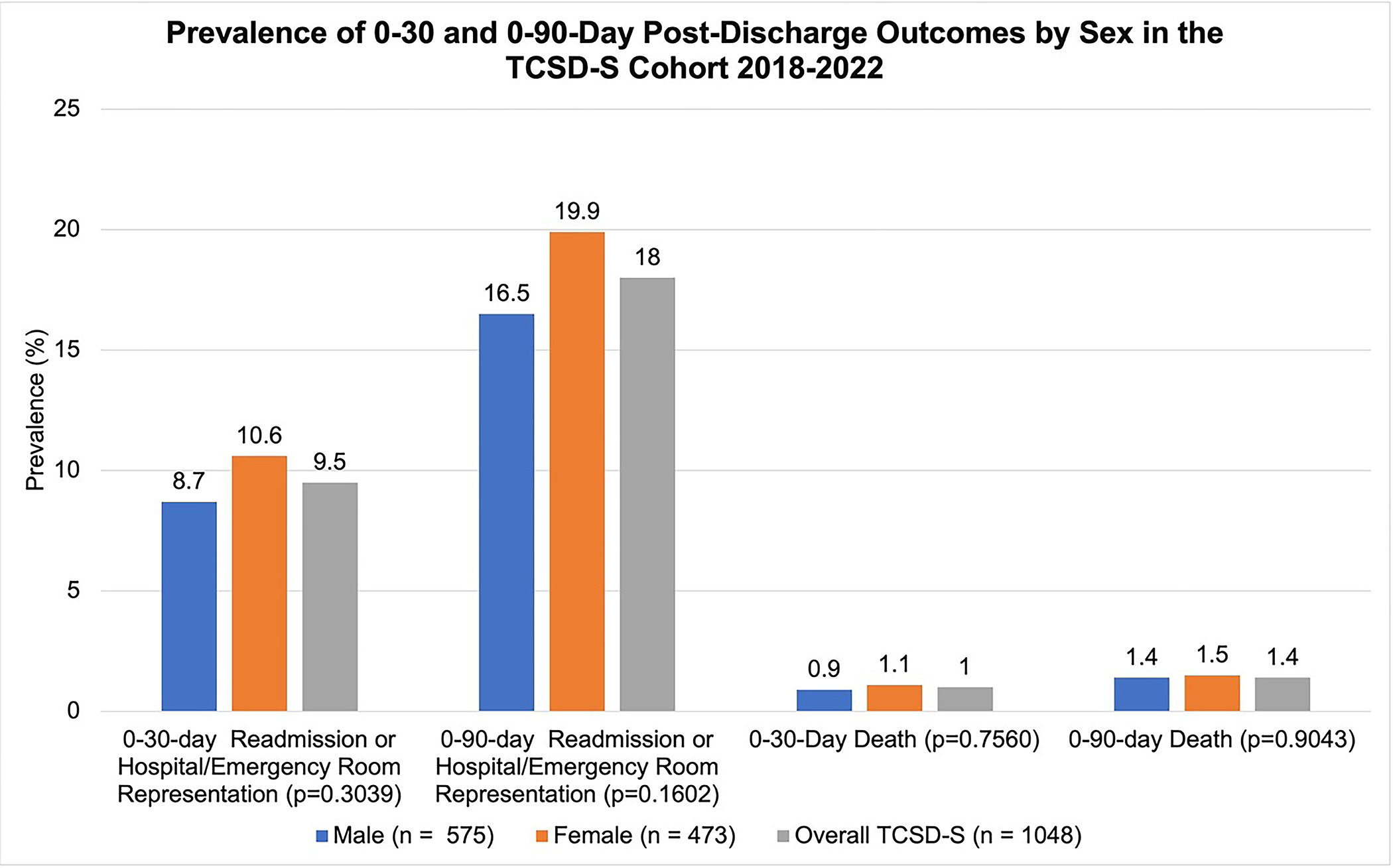
Post-stroke discharge outcomes by sex in the TCSD-S cohort for the years 2018–2022 (n=1048).
Discussion
The TCSD-S is designed to identify race and sex disparities in post-hospital discharge transition of stroke care and evaluate stroke- and social health-related determinants of successful transition of stroke care. The goal of this line of research is to reduce these disparities and improve outcomes.
In our preliminary analyses, we identified younger non-Hispanic Black stroke patients and sex disparities in reporting sufficient discharge stroke education/guidance and accomplishment of adequate transitions of care. Also, we found a noticeable prevalence of both all-cause and vascular related poor stroke outcomes in our cohort and evidence supporting 100% adequate transitions of care as a potential protective factor against these outcomes. Additional analyses will need to further evaluate the trends of race-ethnic and sex differences in systems of care, antihypertensive medication prescription, and discharge counseling, and discharge education found in this analysis.
By design, most stroke participants were discharged directly to home. This finding was reflected by the lower stroke severity. Some race-ethnic differences observed in systems of care during hospitalization (e.g., greater use of intravenous tissue plasminogen activator (IV tPA) in Hispanic patients) have been previously reported (5–7), but some are novel (e.g., higher prevalence of intracerebral hemorrhage in Hispanic patients). Although biased by our study inclusion/exclusion criteria, these observations deserve further explorations.
The observed lower prescription of antihypertensive medication among Black and Hispanic patients when compared to non-Hispanic White patients also warrants further examination on post-stroke outcomes. In the 2002–2012 National Health and Nutrition Examination Survey, Black and Hispanic patients had lower blood pressure control and lower use of antihypertensives when compared to non-Hispanic White patients (20). Blood pressure control is critical to reducing the increased burden of stroke among Black adults, with hypertension as a more potent risk factor among Black adults and several studies linking racial/ethnic disparities in stroke burden to high prevalence of hypertension in Black populations (21–25). Management of blood pressure continues to be the major challenge in transitions of stroke care interventions (26–28). Future TCSD-S analyses will examine the association of antihypertensive medication prescribed at discharge on post-stroke outcomes by race-ethnicity and sex.
A unique focus of the TCSD-S was assessment of patient perception of education received at discharge. Discharge education provided by care providers to stroke patients, can be crucial to reducing hospital readmissions (29–31) and improving patient knowledge and adherence to healthy lifestyle changes (31–33). Patient perception of discharge education can also affect patient discharge readiness, which is a driver of post discharge ability to handle medical and non-medical demands at home, and readmissions (34–35). Our study indicated that less than half of stroke patients reported having received sufficient information regarding post-discharge dietary intake, medical follow-up, or substance use cessation. Sufficient education relied on patient recollection of their discharge experience 30-days later, and therefore may be a subject of recall bias. Nevertheless, the patient’s perception of receiving sufficient education at discharge is an important factor that can significantly affect post-stroke care and outcomes (34–36).
Poor post-stroke outcomes were still prevalent among participants who achieved adequate transitions of care as measured by the TOSC PI. These findings demonstrate the importance of factors beyond post-stroke health behavior management, including medication use and delivery of discharge education/guidance, in potentially reducing poor post-stroke outcomes. Less than half of our cohort reported receiving low sodium diet recommendation, which can be crucial to improving control of hypertension (37). Also, less than a quarter of reported smokers in our sample reported receiving smoking cessation counseling, an education strategy shown by previous interventions to reduce smoking among stroke and TIA patients (38). Future analyses in our study will investigate the effect of patient-perceived appropriate discharge education and healthy lifestyle guidance on post-stroke outcomes of 30-day lifestyle and behavioral changes (adequate transitions of care), death, readmission, and hospital/emergency room representation, and the contribution of social determinants of health (marital status, employment status, social support size), as SDH together with clinical factors predicted achievement of all applicable activities at 30-days in our prior report (39). We found that 29% were not able to achieve all applicable activities within 30 days (39) and only 62% achieved a more liberal composite index of ≥75% TOSC PI.
Our preliminary analysis showed that 30-day and 90-day deaths, rehospitalizations, and readmissions were prevalent, particularly in women. This is consistent with literature showing women having an increased risk of mortality and unplanned readmission after stroke (40, 41). This can be in part explained by our finding that women had a lower prevalence of reported engagement in healthy behaviors such as walking or treadmill exercise or smoking cessation counseling and had lower report of having received sufficient discharge education when compared to men. Although slightly more women in our study reported a social support network size of three or greater than men, women had more death, readmissions, or hospital/ER representations in our study. Previous research has shown that low social support has a greater detrimental impact on the health of women when compared to men (42–44) and therefore sex disparity in the size and quality of social support needs to be further examined.
Many transitions of stroke care studies and initiatives include hospital-initiated discharge support, patient and family education, community-based support through health navigators, and chronic disease management. Some care models have implemented follow-up calls addressing adverse effects and barriers to taking medication and other health issues (45, 46). However, a systematic review of these studies found no effect on readmission rates. Recently, the Comprehensive Post-Acute Stroke Services (COMPASS) study did not show a significant effect of a comprehensive post-acute stroke transitional care management program on functional status at 90 days post-discharge (47), a strong predictor of hospital readmissions (48–50).
Previous studies such as the COMPASS, SUCCEED, and DESERVE studies provide useful insight into both effective and ineffective strategies to monitor stroke outcomes and disparities. The Secondary Stroke Prevention by Uniting Community and Chronic Care Model Teams Early to End Disparities (SUCCEED) clinical trial utilized an optimal care model to reduce blood pressure in stroke and TIA patients 1-year post-discharge. However, this study did not show a significant difference in systolic blood pressure improvement between usual care and the intervention groups (27). While the Discharge Educational Strategies for Reduction of Vascular Events (DESERVE) study focused on culturally tailored discharge education to reduce systolic blood pressure among Hispanic patients at 1-year post discharge, overall differences between intervention and control groups were not statistically significant (28). These studies highlight the challenges that the transitions of care studies face in their efforts to improve risk factor management, improve stroke outcomes, and reduce hospital readmissions.
Our study has some limitations. We were unable to see many significant associations between our select explanatory variables and outcomes which may be related to our sample size. Due to sample size limitations, we observed death, readmissions, or hospital/emergency room representations as a single outcome. Separate analyses of each type of outcome can potentially provide more detailed insight into predictors of poor post-stroke outcomes. We were not able to analyze race-ethnic differences in American Indian, Alaska Native, and Asian and Pacific Islander populations due to their limited representation in Florida. Attrition bias is also another potential challenge to the overall study.
Conclusion
The preliminary findings show that poor post-stroke outcomes are prevalent, correlate with the adequate transitions of stroke care Index (TOSC PI), and appear to vary by race-ethnicity and sex. The goal of the TCSD-S is to identify and reduce disparities in transition of care and outcomes for stroke survivors. Our study will inform large interventions to reduce disparities in transition of stroke care and improve stroke outcomes through a strong partnership between health care providers, patients, communities, government, and other stakeholders to optimize transition of stroke care for the diverse population of stroke patients in Florida.
Supplementary Material
Highlights.
Death and readmission are prevalent outcomes after index stroke.
Transitions of stroke care strategies aim to improve post-stroke outcomes.
Race-ethnic disparities exist in patient characteristics of the TCSD-S.
Acknowledgements
In memoriam of Ralph Sacco MD, MS, FAHA, FAAN, co-author of this manuscript
Sources of Funding
National Institutes of Health/National Institute on Minority Health and Health Disparities 1R01MD012467
Footnotes
Disclosures:
Dr. Romano and Dr. Gutierrez receive research support from National Institutes of Health (NIH) grants. Dr. Romano, Dr. Gardener, Dr. Gordon Perue, and Dr. Gutierrez receive research support from Florida Department of Health (FDOH) Grants. Dr. Rundek is funded by grants from National Institutes of Health (R01 MD012467, R01 NS029993, R01 NS040807, U24 NS107267), the National Center for Advancing Translational Sciences (UL1 TR002736, KL2 TR002737), and the Florida Department of Health. Dr. Sacco received research support from NIH grants and the Florida Department of Health, and personal compensation from the American Heart Association for serving as Editor-In-Chief of Stroke. All other authors have no relevant conflicting interests or disclosures.
Declaration of Interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Tatjana Rundek, MD reports a relationship with National Institutes of Health that includes: funding grants. Jose Romano, MD reports a relationship with National Institutes of Health that includes: funding grants. Ralph Sacco, MD reports a relationship with National Institutes of Health that includes: funding grants. Carolina Gutierrez, PhD reports a relationship with National Institutes of Health that includes: funding grants. Tatjana Rundek, MD reports a relationship with Florida Department of Health that includes: funding grants. Jose Romano, MD reports a relationship with Florida Department of Health that includes: funding grants. Ralph Sacco, MD reports a relationship with Florida Department of Health that includes: funding grants. Carolina Gutierrez, PhD reports a relationship with Florida Department of Health that includes: funding grants. Hannah Gardener, ScD reports a relationship with Florida Department of Health that includes: funding grants. Gillian Gordon Perue, MD reports a relationship with Florida Department of Health that includes: funding grants. Erika Marulanda, MD reports a relationship with Florida Department of Health that includes: funding grants. Tatjana Rundek, MD reports a relationship with National Center for Advancing Translational Sciences that includes: funding grants. Ralph Sacco, MD reports a relationship with American Heart Association that includes: funding grants.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Writing Group M, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP et al. : Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2016, 133(4):e38–360. [DOI] [PubMed] [Google Scholar]
- 2.Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, Howard VJ, Lichtman JH, Lisabeth LD, Pina IL et al. : Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45(5):1545–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J: Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the medicare population. Stroke 2007, 38(6):1899–1904. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM: Medicine in the era of outcomes measurement. Circ Cardiovasc Qual Outcomes 2009, 2(3):141–143. [DOI] [PubMed] [Google Scholar]
- 5.Sacco RL, Gardener H, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, Asdaghi N, Burgin WS, Carrasquillo O, Garcia-Rivera EJ et al. : Racial-Ethnic Disparities in Acute Stroke Care in the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities Study. J Am Heart Assoc 2017, 6(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asdaghi N, Romano JG, Wang K, Ciliberti-Vargas MA, Koch S, Gardener H, Dong C, Rose DZ, Waddy SP, Robichaux M et al. : Sex Disparities in Ischemic Stroke Care: FL-PR CReSD Study (Florida-Puerto Rico Collaboration to Reduce Stroke Disparities). Stroke 2016, 47(10):2618–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polineni SP, Perez EJ, Wang K, Gutierrez CM, Walker J, Foster D, Dong C, Asdaghi N, Romano JG, Sacco RL et al. : Sex and Race-Ethnic Disparities in Door-to-CT Time in Acute Ischemic Stroke: The Florida Stroke Registry. J Am Heart Assoc 2021, 10(7):e017543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gardener H, Leifheit EC, Lichtman JH, Wang Y, Wang K, Gutierrez CM, Ciliberti-Vargas MA, Dong C, Oluwole S, Robichaux M et al. : Racial/Ethnic Disparities in Mortality Among Medicare Beneficiaries in the FL - PR CR eSD Study. J Am Heart Assoc 2019, 8(1):e009649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gardener H, Rundek T, Lichtman J, Leifheit E, Wang K, Asdaghi N, Romano JG, Sacco RL: Adherence to Acute Care Measures Affects Mortality in Patients with Ischemic Stroke: The Florida Stroke Registry. J Stroke Cerebrovasc Dis 2021, 30(3):105586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gardener H, Leifheit EC, Lichtman JH, Wang K, Wang Y, Gutierrez CM, Ciliberti-Vargas MA, Dong C, Robichaux M, Romano JG et al. : Race-Ethnic Disparities in 30-Day Readmission After Stroke Among Medicare Beneficiaries in the Florida Stroke Registry. J Stroke Cerebrovasc Dis 2019, 28(12):104399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morisky DE, Green LW, Levine DM: Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986, 24(1):67–74. [DOI] [PubMed] [Google Scholar]
- 12.Billinger SA, Arena R, Bernhardt J, Eng JJ, Franklin BA, Johnson CM, MacKay-Lyons M, Macko RF, Mead GE, Roth EJ et al. : Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45(8):2532–2553. [DOI] [PubMed] [Google Scholar]
- 13.Braveman P, Gottlieb L: The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014, 129 Suppl 2:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howard VJ, McClure LA, Kleindorfer DO, Cunningham SA, Thrift AG, Diez Roux AV, Howard G: Neighborhood socioeconomic index and stroke incidence in a national cohort of blacks and whites. Neurology 2016, 87(22):2340–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleiss JL, Tytun A, Ury HK: A simple approximation for calculating sample sizes for comparing independent proportions. Biometrics 1980, 36(2):343–346. [PubMed] [Google Scholar]
- 16.Hsieh FY and Lavori PW, Sample-size calculations for the Cox proportional hazards regression model with nonbinary covariates. Control Clin Trials 2000. 21(6): p. 552–60. [DOI] [PubMed] [Google Scholar]
- 17.Schoenfeld DA, Sample-size formula for the proportional-hazards regression model. Biometrics 1983. 39(2): p. 499–503. [PubMed] [Google Scholar]
- 18.Vahidy FS, Donnelly JP, McCullough LD, Tyson JE, Miller CC, Boehme AK, Savitz SI, Albright KC. Nationwide Estimates of 30-Day Readmission in Patients With Ischemic Stroke. Stroke 2017. 48(5): 1386–1388. [DOI] [PubMed] [Google Scholar]
- 19.Andrews AW, Li D, and Freburger JK, Association of Rehabilitation Intensity for Stroke and Risk of Hospital Readmission. Phys Ther 2015. 95(12): p. 1660–7. [DOI] [PubMed] [Google Scholar]
- 20.Gu A, Yue Y, Desai RP, Argulian E: Racial and Ethnic Differences in Antihypertensive Medication Use and Blood Pressure Control Among US Adults With Hypertension: The National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes 2017, 10(1). [DOI] [PubMed] [Google Scholar]
- 21.Gerber Y, Rana JS, Jacobs DR Jr., Yano Y, Levine DA, Nguyen-Huynh MN, Lima JAC, Reis JP, Zhao L, Liu K et al. : Blood Pressure Levels in Young Adulthood and Midlife Stroke Incidence in a Diverse Cohort. Hypertension 2021, 77(5):1683–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hussain A, Virani SS, Zheng L, Gluckman TJ, Borden WB, Masoudi FA, Maddox TM: Potential Impact of 2017 American College of Cardiology/American Heart Association Hypertension Guideline on Contemporary Practice: A Cross-Sectional Analysis From NCDR PINNACLE Registry. J Am Heart Assoc 2022, 11(11):e024107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cao C, Jain N, Lu E, Sajatovic M, Still CH: Secondary Stroke Risk Reduction in Black Adults: a Systematic Review. J Racial Ethn Health Disparities 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hathidara MY, Saini V, Malik AM: Stroke in the Young: a Global Update. Curr Neurol Neurosci Rep 2019, 19(11):91. [DOI] [PubMed] [Google Scholar]
- 25.Chong JY, Sacco RL: Epidemiology of stroke in young adults: race/ethnic differences. J Thromb Thrombolysis 2005, 20(2):77–83. [DOI] [PubMed] [Google Scholar]
- 26.Bushnell CD, Kucharska-Newton AM, Jones SB, Psioda MA, Johnson AM, Daras LC, Halladay JR, Prvu Bettger J, Freburger JK, Gesell SB et al. : Hospital Readmissions and Mortality Among Fee-for-Service Medicare Patients With Minor Stroke or Transient Ischemic Attack: Findings From the COMPASS Cluster-Randomized Pragmatic Trial. J Am Heart Assoc 2021, 10(23):e023394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Towfighi A, Cheng EM, Ayala-Rivera M, Barry F, McCreath H, Ganz DA, Lee ML, Sanossian N, Mehta B, Dutta T et al. : Effect of a Coordinated Community and Chronic Care Model Team Intervention vs Usual Care on Systolic Blood Pressure in Patients With Stroke or Transient Ischemic Attack: The SUCCEED Randomized Clinical Trial. JAMA Netw Open 2021, 4(2):e2036227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boden-Albala B, Goldmann E, Parikh NS, Carman H, Roberts ET, Lord AS, Torrico V, Appleton N, Birkemeier J, Parides M et al. : Efficacy of a Discharge Educational Strategy vs Standard Discharge Care on Reduction of Vascular Risk in Patients With Stroke and Transient Ischemic Attack: The DESERVE Randomized Clinical Trial. JAMA Neurol 2019, 76(1):20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albano MG, Gagnayre R, de Andrade V, d’Ivernois JF: [Discharge education, a new type of therapeutic patient education. Quality criteria and perspective of application to our context]. Rech Soins Infirm 2020(141):70–77. [DOI] [PubMed] [Google Scholar]
- 30.Koelling TM, Johnson ML, Cody RJ, Aaronson KD: Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation 2005, 111(2):179–185. [DOI] [PubMed] [Google Scholar]
- 31.Braet A, Weltens C, Sermeus W: Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI Database System Rev Implement Rep 2016, 14(2):106–173. [DOI] [PubMed] [Google Scholar]
- 32.Benoit C, Lopez D, Loiseau M, Labreuche J, Kyheng M, Bourdain F, Lapergue B: Impact of a Pre-Discharge Education Session on Stroke Knowledge: a Randomized Trial. J Stroke Cerebrovasc Dis 2020, 29(12):105272. [DOI] [PubMed] [Google Scholar]
- 33.Nurhayati N, Songwathana P, Vachprasit R. Surgical patients’ experiences of readiness for hospital discharge and perceived quality of discharge teaching in acute care hospitals. J Clin Nurs. 2019; 28(9–10): 1728–1736. [DOI] [PubMed] [Google Scholar]
- 34.Knier S, Stichler JF, Ferber L, Catterall K: Patients’ perceptions of the quality of discharge teaching and readiness for discharge. Rehabil Nurs 2015, 40(1):30–39. [DOI] [PubMed] [Google Scholar]
- 35.Weiss ME, Piacentine LB, Lokken L, Ancona J, Archer J, Gresser S, Holmes SB, Toman S, Toy A, Vega-Stromberg T: Perceived readiness for hospital discharge in adult medical-surgical patients. Clin Nurse Spec 2007, 21(1):31–42. [DOI] [PubMed] [Google Scholar]
- 36.Weiss ME, Yakusheva O, Bobay KL: Quality and cost analysis of nurse staffing, discharge preparation, and postdischarge utilization. Health Serv Res 2011, 46(5):1473–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khalesi S, Williams E, Irwin C, Johnson DW, Webster J, McCartney D, Jamshidi A, Vandelanotte C: Reducing salt intake: a systematic review and meta-analysis of behavior change interventions in adults. Nutr Rev 2022, 80(4):723–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parikh NS, Salehi Omran S, Kamel H, Elkind MSV, Willey JZ: Smoking-cessation pharmacotherapy for patients with stroke and TIA: Systematic review. J Clin Neurosci 2020, 78:236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Romano JGD C; Gardener H; Rundek T; Marulanda-Londoño E; Gutierrez C; Campo-Bustillo I; Gordon Perue G; Johnson K; Sacco RL: Factors and behaviors related to successful transition of care after hospitalization for ischemic stroke Stroke (in press) 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kilkenny MF, Dalli LL, Kim J, Sundararajan V, Andrew NE, Dewey HM, Johnston T, Alif SM, Lindley RI, Jude M et al. : Factors Associated With 90-Day Readmission After Stroke or Transient Ischemic Attack: Linked Data From the Australian Stroke Clinical Registry. Stroke 2020, 51(2):571–578. [DOI] [PubMed] [Google Scholar]
- 41.Rexrode KM, Madsen TE, Yu AYX, Carcel C, Lichtman JH, Miller EC: The Impact of Sex and Gender on Stroke. Circ Res 2022, 130(4):512–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Donato KM, León-Pérez G, Wallston KA, Kripalani: Something Old, Something New: When Gender Matters in the Relationship between Social Support and Health. J Health Soc Behav. 2018;59(3):352–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shumaker SA, Hill DR: Gender differences in social support and physical health. Health Psychol. 1991;10(2):102–111. [DOI] [PubMed] [Google Scholar]
- 44.Lyyra TM, Heikkinen RL: Perceived social support and mortality in older people. J Gerontol B Psychol Sci Soc Sci. 2006. May 61(3):S147–52. [DOI] [PubMed] [Google Scholar]
- 45.Ho PM, Tsai TT, Maddox TM, Powers JD, Carroll NM, Jackevicius C, Go AS, Margolis KL, DeFor TA, Rumsfeld JS et al. : Delays in filling clopidogrel prescription after hospital discharge and adverse outcomes after drug-eluting stent implantation: implications for transitions of care. Circ Cardiovasc Qual Outcomes 2010, 3(3):261–266. [DOI] [PubMed] [Google Scholar]
- 46.Mansukhani RP, Bridgeman MB, Candelario D, Eckert LJ: Exploring Transitional Care: Evidence-Based Strategies for Improving Provider Communication and Reducing Readmissions. P T 2015, 40(10):690–694. [PMC free article] [PubMed] [Google Scholar]
- 47.Duncan PW, Bushnell CD, Jones SB, Psioda MA, Gesell SB, D’Agostino RB Jr., Sissine ME, Coleman SW, Johnson AM, Barton-Percival BF et al. : Randomized Pragmatic Trial of Stroke Transitional Care: The COMPASS Study. Circ Cardiovasc Qual Outcomes 2020, 13(6):e006285. [DOI] [PubMed] [Google Scholar]
- 48.Shih SL, Gerrard P, Goldstein R, Mix J, Ryan CM, Niewczyk P, Kazis L, Hefner J, Ackerly DC, Zafonte R et al. : Functional Status Outperforms Comorbidities in Predicting Acute Care Readmissions in Medically Complex Patients. J Gen Intern Med 2015, 30(11):1688–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Slocum C, Gerrard P, Black-Schaffer R, Goldstein R, Singhal A, DiVita MA, Ryan CM, Mix J, Purohit M, Niewczyk P et al. : Functional Status Predicts Acute Care Readmissions from Inpatient Rehabilitation in the Stroke Population. PLoS One 2015, 10(11):e0142180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gesell SB, Bushnell CD, Jones SB, Coleman SW, Levy SM, Xenakis JG, Lutz BJ, Bettger JP, Freburger J, Halladay JR et al. : Implementation of a billable transitional care model for stroke patients: the COMPASS study. BMC Health Serv Res 2019, 19(1):978. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


