Abstract
Background:
Cardiovascular and critical care professional societies recommend incorporating family engagement practices into routine clinical care. However, little is known about current family engagement practices in contemporary cardiac intensive care units (CICUs).
Methods:
We implemented a validated 12-item family engagement practice survey among site investigators participating in the Critical Care Cardiology Trials Network, a collaborative network of CICUs in North America. The survey includes 9 items assessing specific engagement practices, 1 item about other family-centered care practices, and 2 open-ended questions on strategies and barriers concerning family engagement practice. We developed an engagement practice score by assigning 1 point for each family engagement practice partially or fully adopted at each site (max score 9). We assessed for relationships between the engagement practice score and CICU demographics.
Results:
All sites (N=39;100%) completed the survey. The most common family engagement practices were open visitation (95%), information and support to families (85%), structured care conferences (n=82%), and family participation in rounds (77%). The median engagement practice score was 5 (interquartile range 4,6). There were no differences in engagement practice scores by geographical region or CICU type. The most commonly used strategies to promote family engagement were family presence during rounds (41%), communication (28%), and family meetings (28%). The most common barriers to family engagement were COVID-related visitation policies (38%) and resource limitations (13%).
Conclusion:
Family engagement practices are routinely performed in many CICUs; however, considerable variability exists. There is a need for strategies to address the variability of family engagement practices in CICUs.
Keywords: Family engagement, cardiac intensive care unit, survey
Introduction
Family-centered care is an approach to health care that is respectful of and responsive to families’ needs and values.1, 2 The key components of family-centered care are family presence in the ICU, family support, communication, use of specific consultations and ICU team members (i.e., ethics, palliative, social worker, spiritual care), and operational and environmental issues (i.e., hospital policies, noise reduction).
There is a growing body of evidence supporting the role of family engagement in the care of critically ill patients. Family engagement in the ICU is associated with improved medical goal achievement, patient and family experience, satisfaction with care, delirium prevention, and patient and family psychological outcomes.3, 4 Critical care professional societies currently recommend incorporating family engagement policies and practices into routine care standards, as incorporated in the ABCDEF bundle (in which “F” represents “Family Engagement/Empowerment”).5, 6
Cardiac critical care shares many aspects of care delivery with the general critical care environment.7 An American Heart Association statement on engaging families in cardiovascular care emphasized the importance of family engagement in these settings, including cardiac critical care.8 Yet the current landscape of practice of family engagement in the cardiac ICU (CICU) setting has not been well-described. An international survey of family engagement practices in ICUs included few CICUs.9
To drive quality improvement, there is a need to understand which family engagement polices and practices are currently implemented in CICUs. Thus, the objective of this survey-based study was to quantify current family engagement practices in CICUs, and to identify existing barriers to family engagement in CICUs.
Methods
Study design
We performed a cross-sectional survey of CICUs within the Critical Care Cardiology Trials Network (CCCTN). The reporting of this survey follows the Checklist for Reporting Of Survey Studies (CROSS) guideline for studies reporting surveys.10 The data that support the findings of this study are available from the corresponding author upon reasonable request.
Family engagement survey
The 12-item family engagement survey used in this study was originally developed for an international study of ICU engagement practices by a taskforce of the World Federation of Societies of Intensive and Critical Care Medicine (WFSICCM).9 The WFSICCM survey was developed to assess the degree that specific types of patient- and family-centered care practices are implemented in ICUs and to explore barriers to and strategies for implementing patient- and family-centered care practices. The survey was developed through an iterative process and was found to have face, content, and construct validity. Written permission to use the survey for the current study was received from the WFSICCM.
The WFSICCM survey includes 9 items that assess specific family engagement practices or polices and 1 general item about other family-centered care practices (Supplemental Table S1). The survey items on specific family engagement practices or polices include structured patient and family care conferences, family participation in rounds (family-centered rounds that enable the family member to listen to rounds and participate by offering information and/or asking questions), patient and/or family ICU diaries, integrative therapies, a patient and family advisory group that meets regularly, disseminating information and providing support to families about assisting with care, open visitation (flexible family presence or non-restricted ICU hours), family presence during resuscitation, and family presence during invasive procedures. Response choices for each survey item utilizes a 3-point Likert scale with options to select if practices have been fully adopted, somewhat adopted, or not at all. There are also 2 open-ended questions to assess strategies and barriers concerning patient and family-centered care or engagement in the ICU. Thematic analysis was performed for the open-ended questions. For strategies, responses were categorized using Oldring’s framework for family engagement in care.11 For barriers, responses were categorized into health system, healthcare provider, and family related. CICU demographic questions were available within the CCCTN database.
Study population
All sites participating in the CCCTN (n=39) at the time of survey distribution were eligible for participation. The CCCTN is a collaborative network of CICUs in North America. The sites included in the CCCTN are primarily academic and tertiary American Heart Association Level 1 CICUs, which means that the unit delivers comprehensive critical care to people with acute cardiovascular conditions requiring critical care.12, 13 All sites participating in the CCCTN registry have received local institutional ethics approval.
Survey administration
The survey was distributed on July 18, 2022 to CCCTN site investigators by an email containing an individualized link to access the survey. A follow-up message was sent if a response was not received within 10 days of the initial email. The majority of responses (37/39) were within the first month of the initial email. The final response was 51 days after the initial email. The survey was available via Research Electronic Data Capture (REDCap), a secure, web-based application. (https://www.project-redcap.org/).14 Multiple participation of sites in the survey was not possible since the provided link was personalized.
Data analysis
Data were reported as counts with frequencies. Continuous variables were reported as median with interquartile range. To quantify the degree of engagement practice, we calculated an “engagement practice score” by giving 1 point for each family engagement practice that a respondent listed as “somewhat adopted” or “fully adopted”. The maximum total engagement practice score was 9. We categorized engagement practice score by percentile: Low (<25th percentile), medium (25th – 75th percentile), and high (>75th percentile). We assessed the relationship between the engagement practice score and CICU demographic variables (geographical location, CICU type, and CICU setting) using the Wilcoxon Rank Sum test or Kruskal-Wallis test, as appropriate. We performed a sensitivity analysis by calculating the engagement practice score (method 2) by assigning a score of 1 for “somewhat adopted” and a score of 2 for “fully adopted”. Statistical analyses were performed using SAS (SAS Software, Cary, NC, Version 9.4).
Results
Respondent and site demographics
All sites in CCCTN (n=39; 100%) completed the survey. There were no missing data points. Sites were mostly urban (n=31; 79%) and academic (n=39; 100%) with a closed organizational model (n=33; 85%; Table 1). Survey respondents were either the CICU director (n=23; 59%) or a CICU intensivist (n=16; 41%).
Table 1.
Characteristics of cardiac intensive care units in the Critical Care Cardiology Trials Network
| Cardiac ICU characteristics | Survey respondents (N=39) |
|---|---|
| Setting | |
| Urban | 31 (79%) |
| Suburban | 7 (18%) |
| Rural | 1 (3%) |
| Geographical region | |
| Midwest US | 7 (18%) |
| Northeast US | 8 (21%) |
| South US | 11 (28%) |
| Western US | 5 (13%) |
| Canada | 8 (21%) |
| ICU Type | |
| Closed | 33 (85%) |
| Mixed | 6 (15%) |
| Length of stay (days; median, IQR) | 4.0 (3; 5) |
| Mortality (median, IQR) | 9.0% (5%; 13.7%) |
Abbreviations: ICU, intensive care unit; IQR, interquartile range; US, United States
Engagement practices
The median engagement practice score was 5 (range 1–9; interquartile range 4, 6; Figure 1). The most common family engagement practices were open visitation (n=37; 95%), information and support to families (n=33; 85%), structured care conferences (n=32; 82%), and family participation in rounds (n=30; 77%; Figure 2). The least common engagement practice was patient and/or family ICU diaries (n=6; 15%). Nearly two-thirds of sites (n=25; 64%) had at least one other patient- or family-centered care practice. There were no differences in engagement practice scores by geographical region, CICU type, or CICU setting (all P>0.05). In the sensitivity analysis using method 2, the median engagement practice score was 8 (range 1–13; interquartile range 6, 9; Supplemental Figure 1). There were no differences in engagement practice scores using method 2 by geographical region, CICU type, or CICU setting (all P>0.05).
Figure 1.
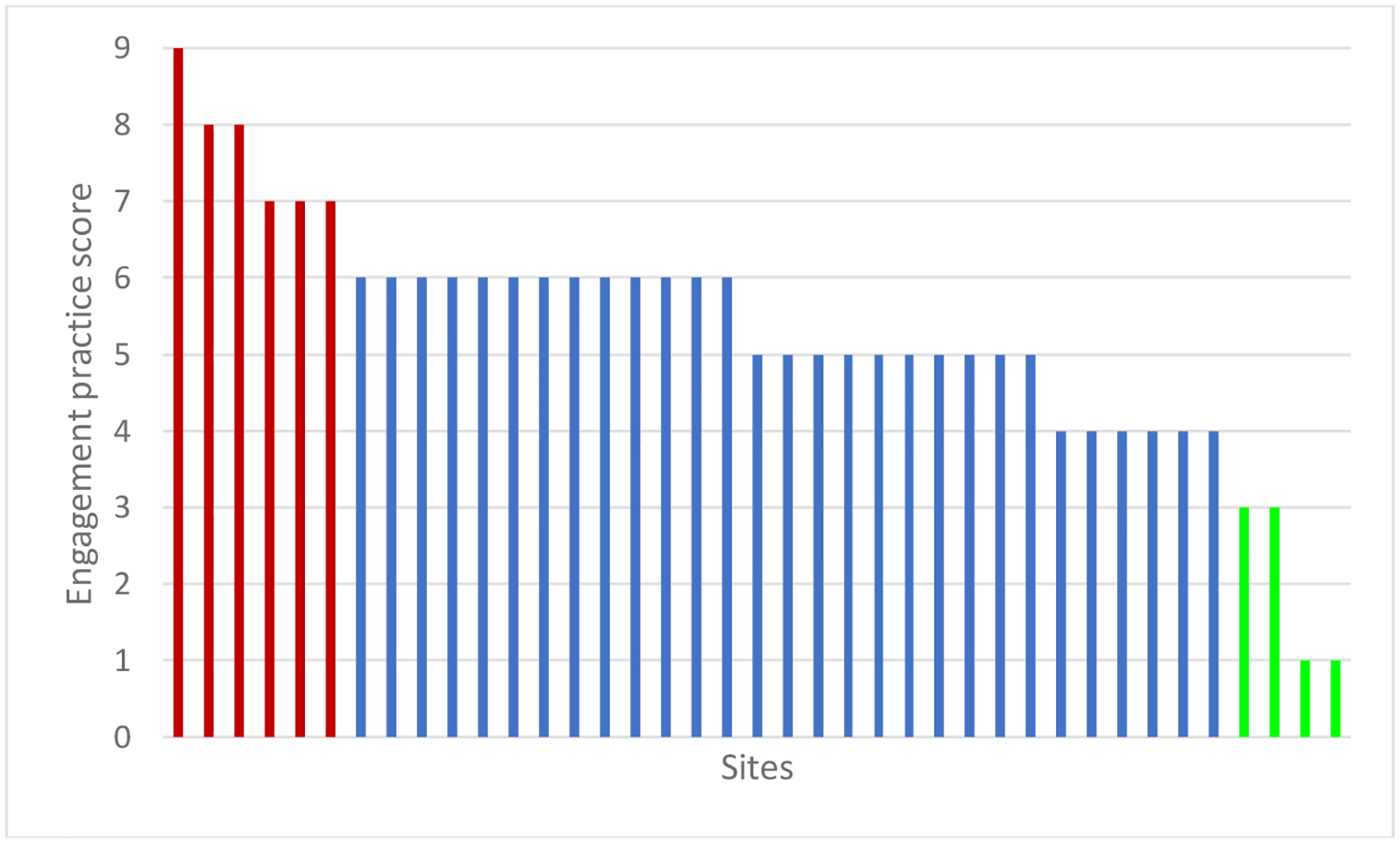
Engagement practice score by site
Each bar represents one site in the Cardiac Critical Care Trials Network. The sites are arranged with the highest engagement practice score on the left to the lowest score on the right.
Figure 2.
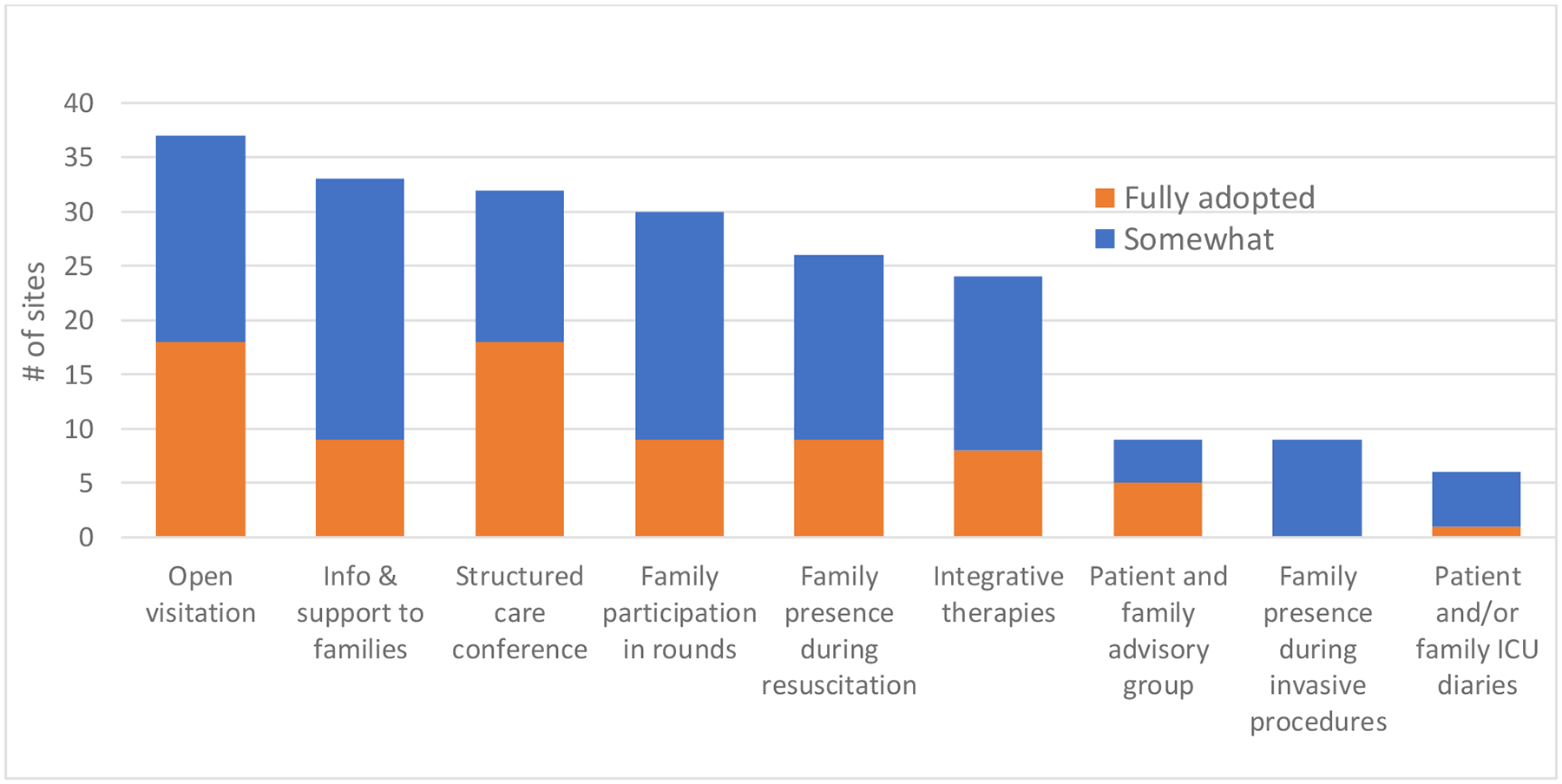
Frequency of engagement strategies in cardiac intensive care units
Abbreviations. ICU, Intensive care unit
The site-reported most effective strategies used to promote patient and family engagement in the CICU included family presence during rounds (n=16; 41%), ad hoc communication between provider and family (n=11; 28%), regularly scheduled structured, multidisciplinary family meetings (n=11; 28%), and proactive palliative care involvement (n=5; 13%; Table 2).
Table 2.
Strategies to improve family engagement in the cardiac intensive care unit
| Family presence |
| Encourage family visitation |
| Proactively invite family member to be present and participate in daily rounds |
| Communication |
| Regular contact (phone, in person, or virtual) between clinician and family |
| Weekly contact between clinician and family for patients with a prolonged ICU course |
| Ad hoc meetings with family members |
| Teach back method to ensure understanding of daily plan of care |
| Providing education to family members about patient’s condition |
| Post-cardiac arrest debrief with family |
| Open discussions regarding complications |
| Proactive involvement of ethics and palliative care when appropriate |
| Ensure consistency of message when communicating with family |
| Family needs |
| Spiritual care / chaplain support available 24/7 |
| Spiritual care / chaplain attend all code blues |
| Early identification of patients and families that need social support |
| Surrogate decision making |
| Early goals of care discussion |
| Participation of family in shared decision making |
| Direct care |
| Family engagement in delirium management |
| Organizational |
| Standardized protocol to involve families, rather than being physician dependent |
| Patient/family feedback is assessed and taken into consideration |
Abbreviations: ICU, intensive care unit
Barriers to family engagement
The most common barriers to family engagement were COVID-related visitation policies (n=15; 38%), resource limitations (n=5; 13%), family availability (n=4; 10%), time limitations (n=4; 10%), variability in care provider interest in family engagement (n=3; 8%), family distance to study center (n=3; 8%), and problematic family dynamics (n=3; 8%; Table 3) All sites reported at least one barrier to family engagement practice.
Table 3.
Barriers to implementing and practicing family engagement in the cardiac intensive care unit
| Healthcare system-related |
|---|
| Policies and Leadership |
| COVID-related visitor restrictive policies (n=15) |
| Lack of leadership; leadership content with status quo (n=2) |
| Lack of support by hospital administration (n=1) |
| Culture |
| Unit culture does not favor engagement in acute care situations (i.e., resuscitation, invasive procedures; n=1) |
| Resources |
| Resource limitations (i.e., staff shortages, lack of available of integrative therapies, 24/7 chaplain; n=5) |
| Financial constraints (n=2) |
| Other challenges |
| Lack of formalized protocols (n=2) |
| Infection control (n=1) |
| Security issues (n=1) |
| Healthcare provider related |
| Time limitations (n=4) |
| Physician/nurse interest is variable; lack of buy-in from the group (n=3) |
| Lack of knowledge of physician about the importance and practice of family engagement (n=2) |
| Coordination of multidisciplinary team availability (n=1) |
| Family-related |
| Family availability (i.e., unable to reach, family not available at convenient time; n=4) |
| Family distance to the unit (n=3) |
| Problematic family dynamics and unclear roles among family members (i.e., intrafamily conflict; n=3) |
| Family health literacy (n=1) |
| Insufficient trust in physicians-in-training during rounds (n=1) |
The number of survey respondents reporting the barrier to engagement is listed next to each item. The total number of responses may add up to more than 39 as some respondents listed more than 1 barrier.
Discussion
We found considerable between-site variability in family engagement practices among North American level 1 CICUs. Open visitation was the most common family engagement practice. Restrictions on visitation during the COVID-19 pandemic was the greatest barrier to engaging families. Allowing family members to be present during CICU rounds was the most reported strategy to improve family engagement. These findings shed light on the current landscape of family engagement practices in high-level CICUs.
Comparison to general ICUs
An international survey of family engagement practices in the ICU received 345 responses from 40 countries.9 Most responding sites (96%) were medical, surgical, or mixed medical-surgical ICUs; the remaining sites (4%) were a combination of cardiac, pediatric, trauma, neuroscience, and burn ICUs. Our findings in the CICU show a similar pattern to data from general ICUs. For example, this international survey reported that open visitation (77%) and structured family care conferences (74%) were the most commonly performed family engagement practices, although these frequencies were lower than in our study population. The prevalence of family presence on ICU rounds was also much higher in our population compared to a broad international general ICU population (77% vs 44%). Possible explanations for the higher prevalence of family engagement practices in our cohort include the evolution of family engagement awareness and practice since the previous study was conducted 5 years prior, the primarily urban, academic, and tertiary/quaternary care nature of the cohort, the inclusion of North American sites and CICUs only, and survey administration during the post-pandemic period.
Family presence during CICU rounds
Family presence during CICU rounds was the most frequently cited effective strategy to increase family engagement in our cohort. Including family members in daily multidisciplinary rounds care allows information sharing and decision-making with the healthcare team, as well as provides families an opportunity to resolve questions. Family presence during rounds is associated with improved family satisfaction, family psychological outcomes, and physician-family relationship.15 Family presence during rounds, when desired by the family, is recommended as a standard care practice by critical care professional societies.1, 2 However, our survey found that family presence on rounds has only been fully adopted by one-quarter of CICUs. The lack of implementation of this practice may be due to a lack of local initiative and support, insufficient clinician knowledge about the potential benefits of family presence on rounds, and a lack of education on how to perform it. In addition, clinicians have reported concerns about perceived efficacy of rounds and impact on teaching trainees when including family members on rounds.16 The available evidence suggests that including family on rounds has a neutral or positive impact on rounding quality and does not impact teaching quantity or quality.17, 18 Additional research is needed to explore how to best implement family presence on ICU rounds in the CICU context.
Healthcare provider barriers to family engagement
We observed considerable variation in family engagement but there were no differences in engagement practice scores by geographical region, CICU type, or CICU setting. Another factor that may influence variability is the existence of provider level barriers to engaging families. Previously reported healthcare provider level barriers to engaging family in care include clinician education and training, time requirement, resource availability, financial remuneration, support for clinicians, privacy concerns, and insufficient evidence for the effectiveness of patient and family engagement strategies.19 There is individual level variation in the perspective of clinicians toward family engagement. This was aptly expressed by one respondent in our survey: “There is a lot of variability in the attending interest in family-centered care, which has hampered a standardized approach for this type of care. Some of our attending staff are very much interested in family-centered care, while others do not feel it is necessary.” A potential solution to address variable engagement practice is to educate physicians on the role of family participation in care and the existing evidence supporting it. Educational initiatives have been shown to increase understanding and performance of family engagement practices in medical trainees and advanced care providers.20 To minimize physician dependent variability, there may be utility to implementing unit wide standardized family engagement protocols.
Healthcare system barriers to family engagement
Competing organization priorities and leadership commitment to family engagement may limit family engagement uptake.19 The COVID-19 pandemic also created many disruptions to engaging families in care.21 In particular, strict visitor restriction policies during the early waves of the pandemic, which still persist in many centers, albeit to a lesser extent, have greatly impacted family presence and participation in care. One study of 117 ICUs across the United Kingdom found that 79% of the ICUs did not allow any in-person visitation during the pandemic, with only two-thirds of these ICUs allowing end-of-life visitation.22 Yet nearly all of these centers (97%) incorporated virtual visitation as an alternative option to in-person presence centers. Virtual ICU visitation was shown to be beneficial for patients (reduced psychological distress), families (improved ‘sense making’, happiness, gratitude), and the health care team (improved morale).22–24 The use of virtual communication strategies with the healthcare team during the pandemic was also shown to be a positive experience for family members and healthcare providers alike.25 Increasing virtual visitation and other virtual family engagement strategies, such as virtual participation in ICU rounds, can also be useful for family members who live far away from the hospital or who have work or social reasons that they cannot attend in-person, as well as for infection control reasons.
Knowledge gaps and areas for future research
There is a need to generate high-quality evidence for the impact of family engagement on patients, family, clinicians, and healthcare system to inform professional society recommendations and increase in family engagement policy and practice uptake. There is also a need to measure the engagement process itself to evaluate the impact of engagement interventions on key person-centered and clinical outcomes. A novel tool to measure engagement in critical care practice, the FAMily Engagement (FAME) instrument, was developed and awaiting validation within the CICU setting.26 An engagement measure could potentially be used to benchmark engagement performance internally and between CICUs. There is a need to explore the longitudinal family involvement in multidisciplinary teams in the CICU, such as the heart team or shock team. New strategies are needed to address existing barriers to engagement. Virtual family participation in care, such as for patient visitation, multidisciplinary team rounds, and structured care conferences, should be explored further. Finally, there is also need for a health economics perspective on family engagement, such as considering the value (quality/cost of care) and return on investment. Studies could evaluate whether family engagement policies and practices improve care experience and reduce costs.
Strengths and limitations
The major strengths of our study are the use of a validated survey and a 100% response rate with no missing data. Multiple participation in the survey was not possible. Respondents were largely CICU directors. There was also a robust response to open-ended questions, which could mean that respondents answered questions more thoughtfully. This is the first study focused on family engagement practice in CICUs and it highlights the opportunity for further research specifically in CICUs.
There are also several limitations to our study. First, study sites were all tertiary level 1 CICUs in North America and were mainly urban and academic centers. Thus, results may not be generalizable to other CICU types or settings where critical care cardiology and general critical care may be practiced in different ways. It is possible that the prevalence of family engagement in our cohort is higher than for other CICU settings. Second, we created an engagement practice score to quantify the number of engagement practices performed in study sites, but this is not a validated measure. The engagement practice score also does not account for the degree to which each item was adopted in the study sites. In addition, some engagement practices may be more important than others and should be weighted more strongly. Further studies are needed to develop a method to objectify and compare engagement practice that can be used for both internal and external performance assessment. Third, the survey only included 9 specific family engagement practices. There are other aspects of engagement practice that were not part of the survey, such as shared decision making and direct care practices (i.e., mobility assistance, delirium detection). It is possible that these were not included in the original design as they are challenging to quantify. Fourth, survey terms such as “somewhat adopted” and “fully adopted” were used as in the WFSICCM survey survey and may be subject to interpretation by the respondent. There may have been differences in actual policy and practice between two centers who each respond with somewhat or fully adopted. Fifth, this was a point prevalence survey that was reflective of the time period that it was administered (the post-pandemic period) and this likely impacted the survey findings. Sixth, nursing leadership did not directly receive the survey. However, the survey was directed at the engagement practices in the CICU as a whole and thus we believe reflect the interprofessional collaborative effort essential to implement family-centered care protocols.
Conclusions
Family engagement practices are routinely performed in many CICUs, although considerable variability exists. There is a need for effective strategies to address barriers to increase family engagement policies and practices in the CICU.
Supplementary Material
What is Known
There is a growing body of evidence supporting the role of family engagement in the care of critically ill patients.
Cardiovascular and critical care professional societies recommend incorporating family engagement into routine care policies and practices
What the Study Adds
The current landscape of practice of family engagement in the cardiac intensive care unit (CICU) setting has not been previously described.
In a network of North American level 1 CICUs, we found considerable between-site variability in family engagement practices.
The study identified the most common family engagement practices, as well as barriers and facilitators to engaging families in the CICU.
Funding source:
Dr. Michael Goldfarb is supported by a Clinical Research Award from the Fonds de recherche du québec sante; Dr. Andrea Thompson is supported by NIH-NHLBI [K08HL163328] and Michigan Biology of cardiovascular Aging (M-BoCA) at the University of Michigan.
Role of funding source:
The funding organization had no role in the survey’s design, implementation, or analysis.
Non-standard Abbreviations and Acronyms
- CICU
Cardiac Intensive Care Unit
- CCCTN
Critical Care Cardiology Trials Network
- CROSS
Checklist for Reporting Of Survey Studies
- WFSICCM
World Federation of Societies of Intensive and Critical Care Medicine
- REDCap
Research Electronic Data Capture
- FAME
FAMily Engagement
Footnotes
Conflict of interest: None to declare
Data availability statement:
Data available on request.
References
- 1.Davidson JE. Family presence on rounds in neonatal, pediatric, and adult intensive care units. Ann Am Thorac Soc. 2013;10:152–6. [DOI] [PubMed] [Google Scholar]
- 2.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, Cox CE, Wunsch H, Wickline MA, Nunnally ME, Netzer G, Kentish-Barnes N, Sprung CL, Hartog CS, Coombs M, Gerritsen RT, Hopkins RO, Franck LS, Skrobik Y, Kon AA, Scruth EA, Harvey MA, Lewis-Newby M, White DB, Swoboda SM, Cooke CR, Levy MM, Azoulay E and Curtis JR. Guidelines for Family-Centered Care in the Neonatal, Pediatric, and Adult ICU. Crit Care Med. 2017;45:103–128. [DOI] [PubMed] [Google Scholar]
- 3.Netzer G Families in the Intensive Care Unit: A Guide to Understanding, Engaging, and Supporting at the Bedside. 1 ed: Springer; 2018. [Google Scholar]
- 4.Wang G, Antel R and Goldfarb M. The Impact of Randomized Family-Centered Interventions on Family-Centered Outcomes in the Adult Intensive Care Unit: A Systematic Review. J Intensive Care Med. 2023: 1–12; doi: 10.1177/08850666231173868 [DOI] [PubMed] [Google Scholar]
- 5.Marra A, Ely EW, Pandharipande PP and Patel MB. The ABCDEF Bundle in Critical Care. Critical care clinics. 2017;33:225–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Thoracic Society. Managing The Intensive Care Unit (ICU) Experience: A Proactive Guide for Patients and Families. 2022. https://www.thoracic.org/patients/patient-resources/managing-the-icu-experience. Accessed March 1, 2023.
- 7.Katz JN, Minder M, Olenchock B, Price S, Goldfarb M, Washam JB, Barnett CF, Newby LK and van Diepen S. The Genesis, Maturation, and Future of Critical Care Cardiology. J Am College Cardiol 2016;68:67–79. [DOI] [PubMed] [Google Scholar]
- 8.Goldfarb MJ, Bechtel C, Capers Qt, de Velasco A, Dodson JA, Jackson JL, Kitko L, Piña IL, Rayner-Hartley E, Wenger NK and Gulati M. Engaging Families in Adult Cardiovascular Care: A Scientific Statement From the American Heart Association. J Am Heart Assoc. 2022:e025859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kleinpell R, Heyland DK, Lipman J, Sprung CL, Levy M, Mer M, Koh Y, Davidson J, Taha A and Curtis JR. Patient and family engagement in the ICU: Report from the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2018;48:251–256. [DOI] [PubMed] [Google Scholar]
- 10.Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, Huy NT, Marušić A, Paul CL, Kwok J, Karbwang J, de Waure C, Drummond FJ, Kizawa Y, Taal E, Vermeulen J, Lee GHM, Gyedu A, To KG, Verra ML, Jacqz-Aigrain ÉM, Leclercq WKG, Salminen ST, Sherbourne CD, Mintzes B, Lozano S, Tran US, Matsui M and Karamouzian M. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Int Med. 2021;36:3179–3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olding M, McMillan SE, Reeves S, Schmitt MH, Puntillo K and Kitto S. Patient and family involvement in adult critical and intensive care settings: a scoping review. Health Expect. 2016;19:1183–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metkus TS, Baird-Zars VM, Alfonso CE, Alviar CL, Barnett CF, Barsness GW, Berg DD, Bertic M, Bohula EA, Burke J, Burstein B, Chaudhry SP, Cooper HA, Daniels LB, Fordyce CB, Ghafghazi S, Goldfarb M, Katz JN, Keeley EC, Keller NM, Kenigsberg B, Kontos MC, Kwon Y, Lawler PR, Leibner E, Liu S, Menon V, Miller PE, Newby LK, O’Brien CG, Papolos AI, Pierce MJ, Prasad R, Pisani B, Potter BJ, Roswell RO, Sinha SS, Shah KS, Smith TD, Snell RJ, So D, Solomon MA, Ternus BW, Teuteberg JJ, van Diepen S, Zakaria S and Morrow DA. Critical Care Cardiology Trials Network (CCCTN): a cohort profile. Eur Heart J Qual Care Clin Outcomes. 2022;8:703–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, Kuvin JT, Lopez-Sendon J, McAreavey D, Nallamothu B, Page RL, Parrillo JE, Peterson PN and Winkelman C. Evolution of Critical Care Cardiology: Transformation of the Cardiovascular Intensive Care Unit and the Emerging Need for New Medical Staffing and Training Models. Circulation. 2012;126:1408–1428. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J and Duda SN. The REDCap consortium: Building an international community of software platform partners. J Biomedical Informatics. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calderone A, Debay V and Goldfarb MJ. Family Presence on Rounds in Adult Critical Care: A Scoping Review. Crit Care Explor. 2022;4:e0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ludmir J, Liu X, Gupta A, Ramani GV, Liu SS, Zakaria S, Verceles AC, Shah NG, McCurdy MT, Dammeyer JA and Netzer G. Cardiologist perceptions of family-centred rounds in cardiovascular clinical care. Open Heart. 2018;5:e000834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Au SS, Roze des Ordons AL, Parsons Leigh J, Soo A, Guienguere S, Bagshaw SM and Stelfox HT. A Multicenter Observational Study of Family Participation in ICU Rounds. Crit Care Med. 46:1255–1262. [DOI] [PubMed] [Google Scholar]
- 18.Jaberi AA, Zamani F, Nadimi AE and Bonabi TN. Effect of family presence during teaching rounds on patient’s anxiety and satisfaction in cardiac intensive care unit: A double-blind randomized controlled trial. J Educ Health Promot. 2020;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herrin J, Harris KG, Kenward K, Hines S, Joshi MS and Frosch DL. Patient and family engagement: a survey of US hospital practices. BMJ Qual Saf. 2016;25:182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewis KD, Destino L, Everhart J, Subramony A, Dreyer B, Allair B, Anderson M, Baird J, Bismilla Z, Good B, Hepps J, Khan A, Kuzma N, Landrigan CP, Litterer K, Sectish TC, Spector ND, Yin HS, Yu CE, Calaman S and O’Toole JK. Patient and Family-Centered I-PASS SCORE Program: Resident and Advanced Care Provider Training Materials. MedEdPORTAL. 2022;18:11267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldfarb M, Bibas L and Burns K. Family Engagement in the Cardiovascular Intensive Care Unit in the COVID-19 Era. Can J Cardiol. 2020;36:1327.e1–1327.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose L, Yu L, Casey J, Cook A, Metaxa V, Pattison N, Rafferty AM, Ramsay P, Saha S, Xyrichis A and Meyer J. Communication and Virtual Visiting for Families of Patients in Intensive Care during the COVID-19 Pandemic: A UK National Survey. Ann Am Thorac Soc. 2021;18:1685–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xyrichis A, Pattison N, Ramsay P, Saha S, Cook A, Metaxa V, Meyer J and Rose L. Virtual visiting in intensive care during the COVID-19 pandemic: a qualitative descriptive study with ICU clinicians and non-ICU family team liaison members. BMJ open. 2022;12:e055679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sasangohar F, Dhala A, Zheng F, Ahmadi N, Kash B and Masud F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: an interview study and sentiment analysis. BMJ Qual Saf. 2021;30:715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levido A, Clement P, Gregory B, Morrey H, Kirrane M, Stott A, Sullivan C, Jackman K, Brown J, Doubrovsky A and Coyer F. Virtual Engagement of Families in the Intensive Care Unit During COVID-19: A Descriptive Survey of Family Members of Patients and Health Care Workers. Telemed J E Health. 2023; 3:466–472. [DOI] [PubMed] [Google Scholar]
- 26.Goldfarb M, Debigaré S, Foster N, Soboleva N, Desrochers F, Craigie L and Burns KEA. Development of a Family Engagement Measure for the Intensive Care Unit. CJC Open. 2022;4:1006–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request.


