Abstract
Time from first DSM4 major depressive episode (MDE) until treatment in the community was compared across racial/ethnic groups. This secondary analysis used structured baseline data from a depression research clinic (N=260). Chi-square and survival analyses compared rates and delays to antidepressant medication and psychotherapy. Non-Hispanic Black and Hispanic (any race) participants had lower rates of both antidepressant medication and psychotherapy and longer delays to antidepressant medication compared with non-Hispanic White participants. The results underscore the need to reduce these disparities.
Keywords: Depression, Antidepressant, Psychotherapy
1. Introduction
Depression is the most common mood disorder among US adults, with reported lifetime prevalence of 20.6% (Hasin et al., 2018). As the leading cause of disability worldwide, depression ranks high in importance when examining health care disparities. Factors contributing to appropriate depression care include recognition and willingness to address symptoms, diagnosis, delay to, adequacy of, and adherence to treatment. Despite evidence of higher risk (Dunlop et al., 2003), depression is underdiagnosed among Hispanic and Black versus White populations (Hasin et al., 2018; McGuire & Miranda, 2008; Shao et al., 2016). Compared to White individuals these groups experience disparities in depression care (Alegría et al., 2008; Bailey et al., 2019; Gonzalez et al., 2008; McGregor et al., 2020; Shao et al., 2016; Simpson et al., 2007). In a nationally representative sample of Medicaid beneficiaries with depression, Black participants were half as likely as White participants to receive any depression treatment, and Hispanic participants were a third as likely (McGregor et al., 2020). Another study found Black participants with Major Depressive Disorder (MDD) in the past year were less likely than White participants to receive antidepressant treatment (Gonzalez et al., 2008). Disparities in MDD treatment for Black and Hispanic persons lead to greater impairment and disease burden (Bailey et al., 2019; Simpson et al., 2007). There is limited empirical data on disparities in delay to initial treatment. The first National Comorbidity Survey (NCS)(1990-92; N=8,098), contrary to what was hypothesized, did not find an association between delay and race/ethnicity (Wang et al., 2004). The NCS-Replication (NCS-R) (2001-3; N=9,282) found shorter delays to initial mental health treatment for non-Hispanic Whites, but the outcome was defined broadly to include physicians, herbalists, or other healers and not specified for depression (Wang et al., 2005). We used structured baseline data from a depression research clinic to analyze rates and delays from a first Major Depressive Episode (MDE) to initial treatment with antidepressant medication or psychotherapy across non-Hispanic Black, non-Hispanic White, and Hispanic (any race) subgroups.
2. Methods
Subjects 18-72 years of age (N=260) participated in a long-term depression study over two decades at Columbia University Medical Center-NY State Psychiatric Institute. Participants were recruited by one research group using uniform criteria and measures. Baseline diagnosis used the Structured Clinical Interview for DSM4 (First et al., 1997). A structured baseline survey developed by our clinic obtained cross-sectional sociodemographic and clinical history data. This analysis used data collected July 1995 – May 2012. The survey included items asking participants to recall their “age of first treatment” with antidepressant medication and “age at first outpatient psychotherapy” (age in years). Exclusions included unstable medical illness, current substance use disorder, and significant cognitive impairment. All subjects gave written informed consent as approved by the Institutional Review Board. Recruitment used ads offering participation in depression research posted in local media, online, and at our medical center. Typically about five times the number of subjects who enroll and provide data are initially screened.
Race and ethnicity were self-identified by participants following non-overlapping NIH categories: Black or African American, Hispanic, and White. We analyzed the following groups: non-Hispanic Black, non-Hispanic White, and Hispanic (any race). We excluded other racial groups due to small numbers (pooled N=19). The primary outcome was years elapsed between the age of a subject’s first DSM4 MDE and their age at first antidepressant medication or psychotherapy received elsewhere i.e. not including in our research clinic after study participation.
In the analysis of delays to antidepressant medication, we excluded those prescribed one before their first MDE (N=16). In the analysis of delays to psychotherapy, participants prescribed an antidepressant before their first MDE (N=16) were included, but those who received psychotherapy before their first MDE were excluded (N=89). Differences in presence/absence of antidepressant medication treatment or psychotherapy were examined across racial groups without any exclusions.
We defined subjects who came to us depressed without having received prior treatment (N=57), as “censored” because it is unknown how long their delay to treatment in the community (elsewhere) would have been had they not received treatment in our research clinic. We used the log-rank test to compare time from first MDE to a first antidepressant medication or psychotherapy between racial-ethnic groups. Individuals who received a first antidepressant after MDE onset but within the same year were assumed to have 0.1 years delay to treatment. A power calculation was not performed for this secondary analysis.
3. Results
At baseline, racial-ethnic groups did not differ in age, sex, income, or total lifetime number of MDEs (Kruskal-Wallis p=0.911). Non-Hispanic Black and Hispanic (any race) participants were more likely to have not received a course of antidepressant medication since their first MDE (51.7% and 39.3%, respectively) compared to non-Hispanic White participants (16.7%) (X2=21.59; df=2; p<0.001). Furthermore, non-Hispanic Black and Hispanic (any race) participants were more likely to have not received antidepressant medication in their lifetime (51.7% and 37.9%, respectively) as compared with non-Hispanic White subjects (15.8%)(X2= 23.4; p<0.001).
Non-Hispanic Black (N=29; 12%) and Hispanic (any race) (N=28; 11.5%) participants experienced extraordinarily longer delays from a first MDE to a first antidepressant medication (median=15.0 years, 95% CI 6.8-23.2 and median=13 years, 95% CI 6.5-19.5, respectively) as compared with non-Hispanic White subjects (N=186; 77%; median=8.0 years, 95% CI 5.5-10.5) (Log rank X2=7.33; df=2; p=0.026)(Figure 1).
Figure. 1.
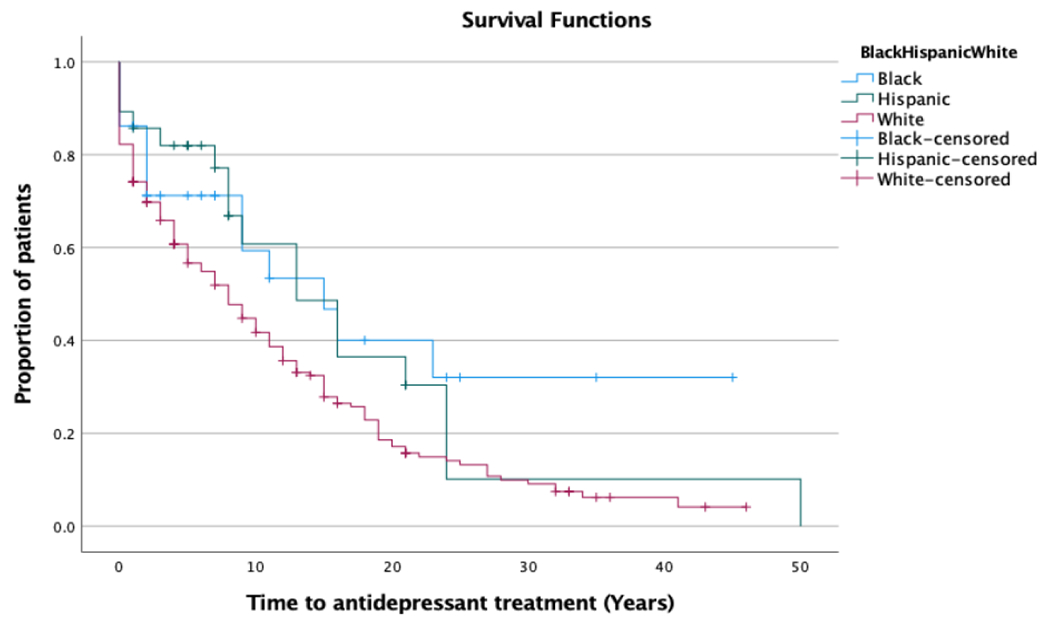
Kaplan-Meier survival curves for proportion of participants receiving a first course of antidepressant medication by years after first DSM4 major depressive episode.
Time from first DSM4 major depressive episode to first antidepressant medication was longer for non-Hispanic Black and Hispanic (any race) participants of any race compared with non-Hispanic White participants (Log rank X2=7.33; df=2; p=0.026).
The percentage of subjects who had not received psychotherapy since their first MDE was larger for non-Hispanic Black (28.6%) compared with Hispanic (any race) (5.3%) and non-Hispanic White participants (8.5%) (X2= 8.4; p=0.023). Non-Hispanic Black and Hispanic (any race) participants were also more likely to have not received psychotherapy in their lifetime (41.4% and 17.2%, respectively) as compared with non-Hispanic White participants (12.9%)(X2= 14.9; p=0.001).
Comparison of delays from first MDE to psychotherapy across racial-ethnicity groups was not statistically significant (non-Hispanic Black: median=7.0 years, 95% CI .04-14.0; Hispanic (any race): median=3.0 years, 95% CI 0.0-7.3; non-Hispanic White: median=5.0 years, 95% CI 2.7-7.3) (Log rank X2=1.16; df=2; p=0.56).
4. Discussion
Non-Hispanic Black and Hispanic (any race) participants experienced longer delays from a first DSM4 MDE to first antidepressant medication treatment in the community compared to non-Hispanic White participants. The lack of difference in lifetime number of MDEs between groups suggests illness severity did not cause this disparity. The groups also did not differ in age, sex, or income level.
Non-Hispanic Black and Hispanic (any race) individuals were less likely to receive antidepressant medication or psychotherapy at all in their lifetime compared with non-Hispanic White participants. Delay from first MDE to psychotherapy was longest for non-Hispanic Black participants, but between group differences were not statistically significant.
Our results are consistent with epidemiological findings that groups other than non-Hispanic Whites are less likely to receive depression care (Simpson et al., 2007). We found long delays from DSM4 depression to antidepressant medication of about 8 years in non-Hispanic White participants. But this delay was markedly longer in non-Hispanic Black and Hispanic (any race) groups at 15 and 13 years, respectively. These delays are consistent with the NCS-R analysis which was irrespective of the specific type of depression treatment and pre-dated most of the expansion in antidepressant prescribing in recent decades (Wang et al., 2005). Thus, our analysis finds persisting disparities even after the marked growth in antidepressant prescribing and adds specificity for antidepressant medication versus psychotherapy.
To make matters worse, racial and ethnic minorities have less access to mental health services, depression treatment received is reported to be lower quality, and mental illness stigma is reported to be higher (Alegría et al., 2008; Eylem et al., 2020; McGuire & Miranda, 2008). In one study, fewer than half of Black participants sought treatment for depression, despite rating it as severe or disabling (Williams et al., 2007). Hispanic adults reported fears about perceived addictive and harmful potential of antidepressant drugs and stigma attached to mental health treatment (Sanchez et al., 2019). Finally, we found that more non-Hispanic Black and Hispanic (any race) participants did not receive antidepressant medication or psychotherapy in their lifetime, despite suffering a DSM4 episode of major depression.
Our study has limitations including a relatively small sample and data on a first MDE and first antidepressant medication or psychotherapy were based on participant recall. The fact that participants were recruited by one research group using uniform criteria and measures throughout the study period reduces the chance that recall bias would be the source of our results. Our clinic is in a diverse neighborhood and proportions of non-Hispanic Black and Hispanic (any race) individuals in the sample, 12% and 11.5%, respectively, were comparable to the U.S. population in this time period - 13% and 16%, respectively (Census Bureau). Lack of greater diversity in our sample may be partly due to lack of trust in research and medical providers resulting from historical persecution, abuse, and perceived mistreatment in health care (Sanchez et al., 2016).
Another limitation is lack of data after 2012 because shortening of our baseline survey that year removed a key variable. However, racial disparities in MDE treatment are unlikely to have diminished substantially as Black and Hispanic individuals continue to receive less mental health treatment than White persons (Lu, 2020; Terlizzi & Zablotsky, 2020). Subjects were not asked further details about intensity of or adherence to first antidepressant or psychotherapy, thus we cannot draw conclusions about adequacy of treatment.
We found lower rates of receiving antidepressant medication or psychotherapy and a much longer average delay from a first MDE to a first antidepressant medication for Hispanic (any race) and non-Hispanic Black participants compared with non-Hispanic White individuals. Evidence-based interventions to reduce such healthcare inequities for major depression, the leading cause of disability worldwide - such as improving provider diversity and cultural competence, enhancing mental health in primary care, increasing community engagement, and psycho-education - are urgently needed (Bailey et al., 2019; Flores et al., 2021; Simpson et al., 2007).
Highlights.
Race-ethnicity groups did not differ in age, sex, income, or depressive episode number
Longer delays from first major depressive episode to antidepressant medication for non-Hispanic Black and Hispanic (any race) participants
Non-Hispanic Black and Hispanic (any race) participants have lower rates of lifetime depression treatment
Acknowledgements
This work was supported by federal grant P50 MH062185 (Conte Center for the Neuroscience of Mental Disorders: The Neurobiology of Suicidal Behavior).
Declaration of Interest:
This work was supported by federal grant P50 MH062185 (Conte Center for the Neuroscience of Mental Disorders: The Neurobiology of Suicidal Behavior (PI: Mann). Dr. Mann receives royalties from the Research Foundation for Mental Hygiene for commercial use of the C-SSRS, which was not part of this work. The other authors report no conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Dr. Mann receives royalties from the Research Foundation for Mental Hygiene for commercial use of the C-SSRS, which was not part of this work. The other authors report no conflicts of interest.
References
- Alegría M, Chatterji P, Wells K, Cao Z, Chen C.-n., Takeuchi D, Jackson J, & Meng X-L (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric services (Washington, D.C.), 59(11), 1264–1272. 10.1176/appi.ps.59.11.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey RK, Mokonogho J, & Kumar A (2019). Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat, 15, 603–609. 10.2147/NDT.S128584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau, U. S. (March/24/2011). 2010 Census Shows America’s Diversity https://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn125.html
- Dunlop DD, Song J, Lyons JS, Manheim LM, & Chang RW (2003). Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health, 93, 1945–1952. (In File) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eylem O, de Wit L, van Straten A, Steubl L, Melissourgaki Z, Danışman GT, de Vries R, Kerkhof A, Bhui K, & Cuijpers P (2020). Stigma for common mental disorders in racial minorities and majorities a systematic review and meta-analysis. BMC Public Health, 20(1), 879. 10.1186/s12889-020-08964-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1997). Structured Clinical Interview for DSM-IV Axis I Disorders. American Psychiatric Press. [Google Scholar]
- Flores MW, Moyer M, Rodgers CRR, & Cook BL (2021). Major Depressive Episode Severity Among Adults from Marginalized Racial and Ethnic Backgrounds in the US. JAMA Psychiatry, 78(11), 1279–1280. 10.1001/jamapsychiatry.2021.2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez HM, Croghan T, West B, Williams D, Nesse R, Tarraf W, Taylor R, Hinton L, Neighbors H, & Jackson J (2008). Antidepressant use in black and white populations in the United States. Psychiatr Serv, 59(10), 1131–1138. 10.1176/ps.2008.59.10.1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, & Grant BF (2018). Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry, 75(4), 336–346. 10.1001/jamapsychiatry.2017.4602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W (2020). Treatment for Adolescent Depression: National Patterns, Temporal Trends, and Factors Related to Service Use Across Settings. J Adolesc Health, 67(3), 401–408. 10.1016/j.jadohealth.2020.02.019 [DOI] [PubMed] [Google Scholar]
- McGregor B, Li C, Baltrus P, Douglas M, Hopkins J, Wrenn G, Holden K, Respress E, & Gaglioti A (2020). Racial and Ethnic Disparities in Treatment and Treatment Type for Depression in a National Sample of Medicaid Recipients. Psychiatr Serv, 71(7), 663–669. 10.1176/appi.ps.201900407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire TG, & Miranda J (2008). New evidence regarding racial and ethnic disparities in mental health: policy implications. Health affairs (Project Hope), 27(2), 393–403. 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez K, Killian MO, Eghaneyan BH, Cabassa LJ, & Trivedi MH (2019). Culturally adapted depression education and engagement in treatment among Hispanics in primary care: outcomes from a pilot feasibility study. BMC Fam Pract, 20(1), 140. 10.1186/s12875-019-1031-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez K, Ybarra R, Chapa T, & Martinez ON (2016). Eliminating Behavioral Health Disparities and Improving Outcomes for Racial and Ethnic Minority Populations. Psychiatr Serv, 67(1), 13–15. 10.1176/appi.ps.201400581 [DOI] [PubMed] [Google Scholar]
- Shao Z, Richie WD, & Bailey RK (2016). Racial and Ethnic Disparity in Major Depressive Disorder. J Racial Ethn Health Disparities, 3(4), 692–705. 10.1007/s40615-015-0188-6 [DOI] [PubMed] [Google Scholar]
- Simpson SM, Krishnan LL, Kunik ME, & Ruiz P (2007). Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatr Q, 78(1), 3–14. 10.1007/s11126-006-9022-y [DOI] [PubMed] [Google Scholar]
- Terlizzi EP, & Zablotsky B (2020). Mental Health Treatment Among Adults: United States, 2019. NCHS Data Brief(380), 1–8. [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, & Kessler RC (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry, 62(6), 603–613. 10.1001/archpsyc.62.6.603 [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund PA, Olfson M, & Kessler RC (2004). Delays in initial treatment contact after first onset of a mental disorder. Health Serv Res, 39(2), 393–415. 10.1111/j.1475-6773.2004.00234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, & Jackson JS (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry, 64(3), 305–315. 10.1001/archpsyc.64.3.305 [DOI] [PubMed] [Google Scholar]


