Abstract
PURPOSE:
The uninsured rate began rising after 2016, which some have attributed to health policies undermining aspects of the Affordable Care Act. Our primary objectives were to assess the changes in insurance coverage and forgoing medical care because of cost in cancer survivors from pre-enactment (2016) through postenactment of those policies (2019) and determine whether there were subgroups that were disproportionately affected.
METHODS:
The 2016-2019 Behavioral Risk Factor Surveillance System surveys were queried for 18- to 64-year-old cancer survivors. Survey-weighted logistic regression was used to assess temporal changes in (1) insurance coverage and (2) forgoing medical appointments because of cost in the preceding 12 months.
RESULTS:
A total of 62,669 cancer survivors were identified. The percentage of insured cancer survivors decreased from 92.4% in 2016 to 90.4% in 2019 (odds ratio for change in insurance coverage or affordability per one-year increase [ORyear], 0.92; 95% CI, 0.86 to 0.98; P = .01), translating to 161,000 fewer cancer survivors in the United States with insurance coverage. There were decreases in employer-sponsored insurance coverage (ORyear, 0.89) but increases in Medicaid coverage (ORyear, 1.17) from 2016 to 2019. Forgoing medical appointments because of cost increased from 17.9% in 2016 to 20.0% in 2019 (ORyear, 1.05; 95% CI, 1.01 to 1.1; P = .025), affecting an estimated 169,000 cancer survivors. The greatest changes were observed among individuals with low income, particularly those residing in nonexpansion states.
CONCLUSION:
Between 2016 and 2019, there were 161,000 fewer cancer survivors in the United States with insurance coverage, and 169,000 forwent medical care because of cost.
INTRODUCTION
There will likely be over 22 million individuals with a history of cancer (hereafter referred to as cancer survivors) living in the United States by 2030.1 Cancer survivors, particularly those who are younger than 65 years or uninsured, are at increased risk of financial hardship.2 Insurance coverage increases the likelihood of receiving guideline-recommended therapy and survival among patients with cancer.3-6 Furthermore, insurance coverage may be a protective factor against some effects of financial toxicity, which has implications on access to cancer care as well as cancer outcomes.7,8 The Affordable Care Act (ACA) improved insurance coverage in nonelderly (age < 65 years) cancer survivors.9-12 Likely as a result of improved access to care, the ACA is associated with decreased care unaffordability, more localized stage cancer diagnoses, and improved survival in patients with cancer.9,11,13-20 However, although the uninsured rate reached its lowest point in 2016, it has steadily increased since that time.21 Some hypothesize that these changes may be secondary to policies attempting to undermine the ACA, such as eliminating the tax penalty associated with the individual mandate, eliminating cost-sharing reductions to insurers, and permitting non–ACA-compliant health insurance plans with limited coverage.21,22
Early data through 2017 showed nonsignificant increases in the uninsured rate and care unaffordability for cancer survivors, and updated data for cancer survivors as a whole confirmed further increases in the uninsured rate.13,21 Similarly, in another study focusing on changes in insurance coverage and care unaffordability from pre-ACA to post-ACA, trend figures suggest worsening increases in care unaffordability from 2017 to 2018.11 However, it is unknown whether this pattern represents random fluctuations or if there have been persistent increases in cancer survivors forgoing medical care because of costs. Furthermore, it is unclear which subgroups of cancer survivors were most at risk of losing health insurance or experiencing care unaffordability after 2016. Our primary objectives were to assess changes in insurance coverage and forgoing medical care from pre-enactment (2016) through postenactment of the potentially detrimental health insurance policies (2019) among cancer survivors as well as determine if there were subgroups of cancer survivors that were disproportionately affected.
METHODS
Study Population
The Behavioral Risk Factors Surveillance System (BRFSS), weighted surveys performed nationwide assessing behavioral risk factors in the noninstitutionalized population,23 was used to identify 18- to 64-year-old individuals in the 50 states who had a history of cancer. We focus on data from 2016, the year before potentially detrimental policies were enacted, through 2019.21 We excluded data from 2020 to 2021 from our primary analyses because of the COVID-19 pandemic and associated response, which may have had impacts on both insurance coverage and cost-related measures irrespective of policy changes in 2017-2019. However, 2020-2021 were included in secondary analyses. Patients whose only cancer diagnosis was a history of nonmelanoma skin cancer were excluded.14 Health insurance status was based on the question, “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?” Health insurance type was based on the question, “What is the primary source of your health care coverage?” Responses were recoded into employer-sponsored, individually purchased, Medicaid, and other (includes TRICARE, VA, military, Alaska Native, Indian Health Service, Tribal Health Services, Medicare [for which patients should not typically be eligible until age 65 years, outside the scope of this study], and others). Only individuals who stated they had some form of insurance coverage were asked the insurance type question. Forgoing medical appointments because of cost was defined using the question, “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?”24 Income measured as percent federal poverty level (FPL) for each respondent was estimated using household income and household size on the basis of poverty guidelines.25 Cases with missing information were excluded (Data Supplement, online only). Institutional review board oversight was not required for this study of deidentified publicly available data.
Data Analysis
To analyze changes in the percentage insured and percentage reporting forgoing medical appointments because of cost, we used logistic regression models with robust standard errors, accounting for the complex survey design of the BRFSS. The survey weights were adjusted to account for the multiple survey years. The coefficient of interest in these models was the effect for survey year. We compared a number of approaches for modeling trends in insurance coverage and forgoing medical appointments because of cost over time and ultimately selected two different approaches: using a continuous year term, and, because of mixed evidence of nonlinear trends over time, a model testing for changes from 2016 (pre-enactment) to 2019 (postenactment), which model was limited to participants in the 2016 and 2019 surveys (see the Data Supplement for details). To mitigate confounding with the enactment of health insurance policies that could affect access to care, models were adjusted for the following covariates selected a priori on the basis of expected associations with access to care: age, sex, race/ethnicity, state Medicaid expansion status, household income, educational attainment, marital status, and employment status (Table 1).13,26 Subgroup analyses were conducted on the basis of socioeconomic factors, including income (the primary basis of eligibility for ACA initiatives: individuals with income ≤ 138% FPL could become Medicaid-eligible under Medicaid expansions, and individuals with income < 250% FPL are eligible for insurance plans with decreased cost-sharing),14 state Medicaid expansion status (limited to potentially Medicaid-eligible individuals, those with income ≤ 138% FPL), race/ethnicity, metropolitan residence status, and employment status. To explore the degree to which temporal changes in forgoing medical appointments because of cost might be affected by changes in insurance coverage, we expanded our forgoing medical appointments because of cost regression models to include insurance status as a covariate in addition to analyses without including insurance status. Secondary analyses evaluating changes in the outcomes from 2019 through 2021 were also conducted, but with separate models because of the differing nature and consequences of the policies (Data Supplement). All analyses were conducted using R v3.6.2. P values were two-sided, not adjusted for multiplicity, and P < .05 was considered statistically significant.
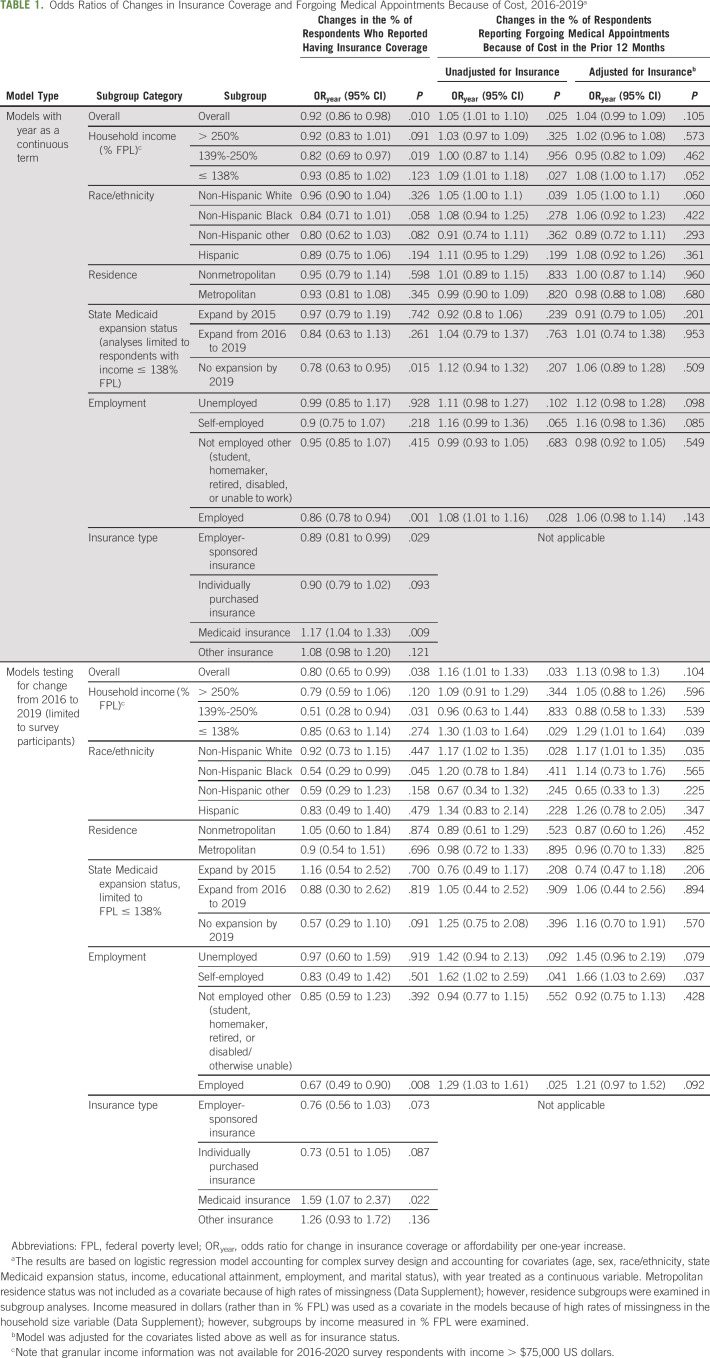
TABLE 1.
Odds Ratios of Changes in Insurance Coverage and Forgoing Medical Appointments Because of Cost, 2016-2019a
RESULTS
Study Sample
A total of 1,792,023 BRFSS participants were identified. Among these, 62,669 participants age 18-64 years reported being cancer survivors, representing over 8.1 million cancer survivors in the United States on the basis of the survey weights. Most of the cancer survivors were age 40-64 years (82.9%), female (67.1%), non-Hispanic White (71.5%), and metropolitan residents (79.6%; Data Supplement). There were very low rates of missingness in the outcomes of interest, insurance coverage (0.3%) and forgoing medical appointments because of cost (0.3%; Data Supplement).
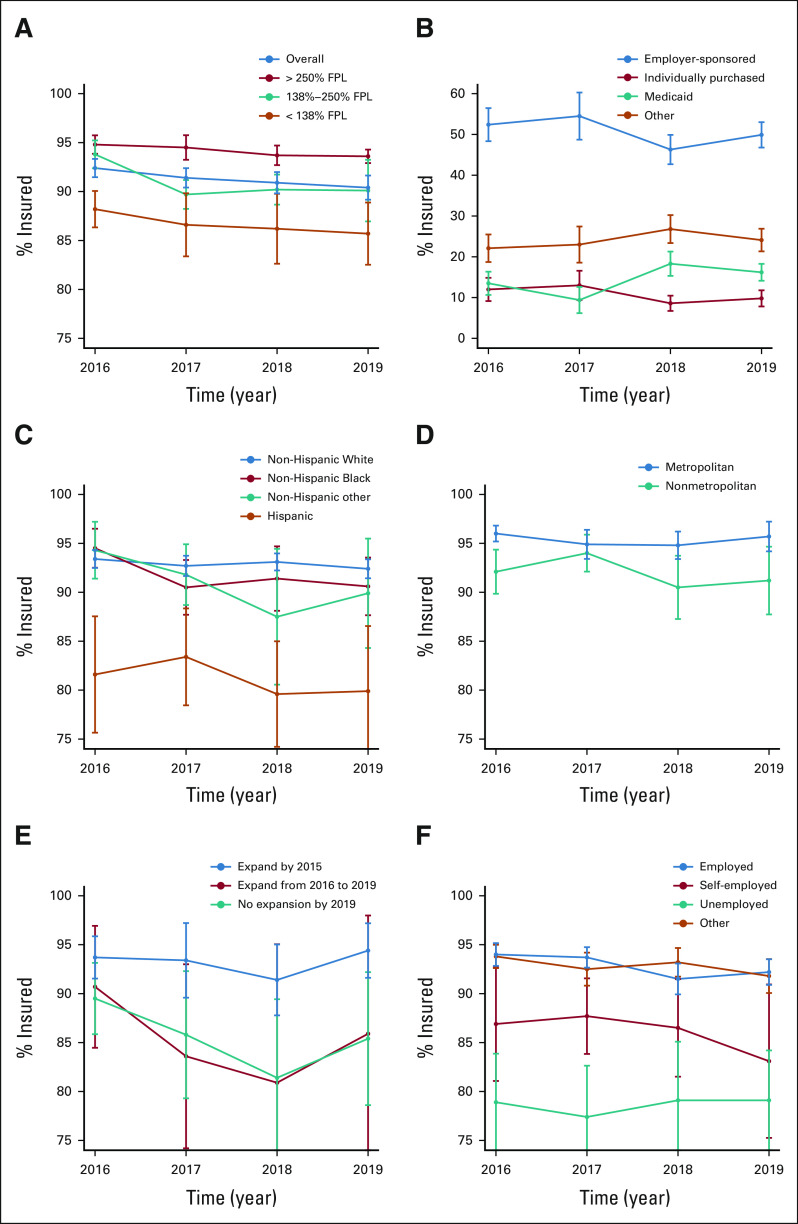
Insurance Coverage
Among our study population, the percentage of insured cancer survivors decreased from 92.4% in 2016 to 90.4% in 2019 (odds ratio for change in insurance coverage or affordability per one-year increase [ORyear], 0.92; 95% CI, 0.86 to 0.98; P = .01), which translates to over 161,000 fewer cancer survivors in the United States who reported insurance coverage in 2019 (Table 1, Fig 1). Over the study period, there was a decrease in employer-sponsored insurance coverage (ORyear, 0.89; 95% CI, 0.81 to 0.99; P = .029), nonsignificant changes in individually purchased plans (ORyear, 0.90; 95% CI, 0.79 to 1.02; P = .093), and other coverage (ORyear, 1.08; 95% CI, 0.98 to 1.2; P = .12), and increases in Medicaid coverage (ORyear, 1.17; 95% CI, 1.04 to 1.33; P = .009).
FIG 1.
Temporal trends in (A) insurance coverage overall and by income, (B) insurance coverage type, (C) race/ethnicity, (D) residence, (E) state Medicaid expansion status, and (F) employment. Subgroups by state Medicaid expansion status are limited to individuals with income ≤ 138% FPL. FPL, federal poverty level.
The decreases in insurance coverage were greatest among employed individuals (ORyear, 0.86; 95% CI,= 0.78 to 0.94; P = .001), those with income 139%-250% FPL (ORyear, 0.82; 95% CI, 0.69 to 0.97; P = .019), and low-income (FPL ≤ 138%) residents of nonexpansion states (ORyear, 0.78; 95% CI, 0.63 to 0.95; P = .015). By contrast, there was very little change in insurance coverage among low-income residents of states that expanded Medicaid by 2015 (ORyear, 0.97).
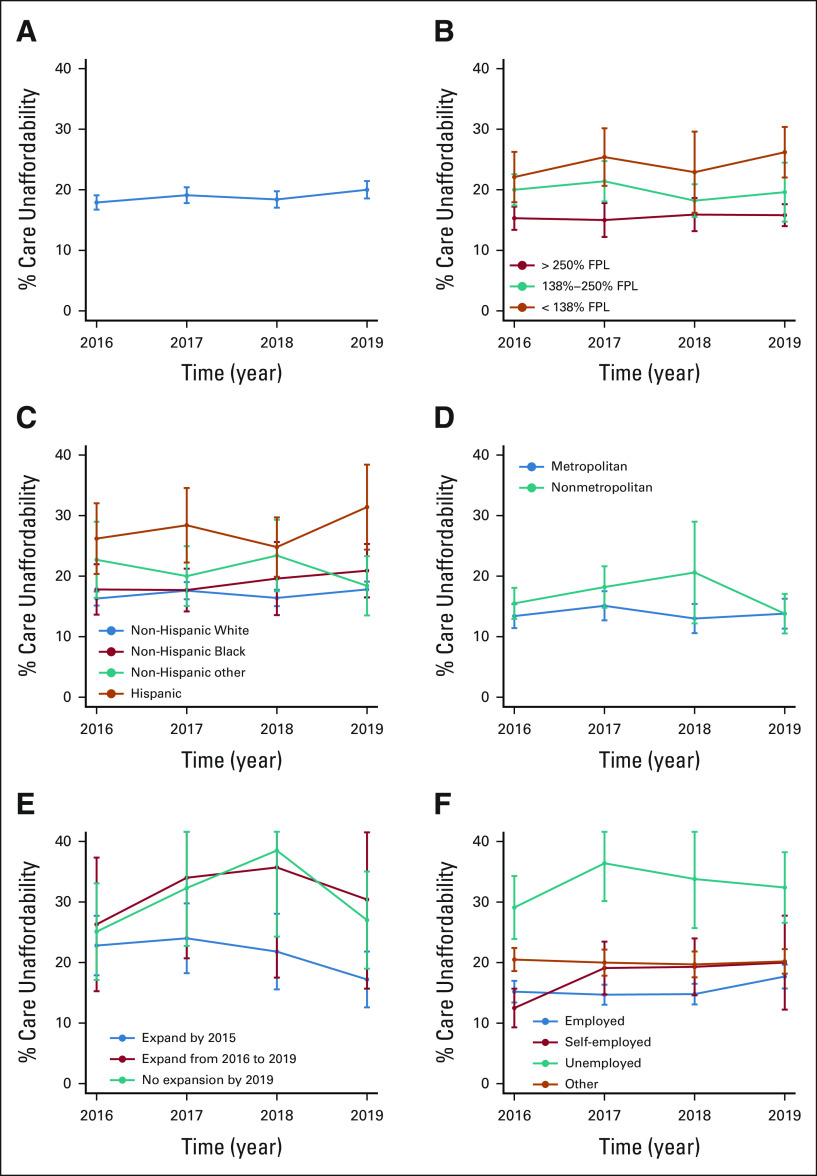
Forgoing Medical Appointments Because of Cost
The percentage of cancer survivors who could not afford to see a doctor because of cost increased from 17.9% in 2016 to 20.0% in 2019 (ORyear, 1.05; 95% CI, 1.01 to 1.1; P = .025), which translates to over 169,000 additional cancer survivors in the United States who forwent medical appointments because of cost in 2019 (Table 1, Fig 2). Subgroup analyses demonstrated that increases in the odds of forgoing care were largest among low-income (≤ 138% FPL) individuals (ORyear, 1.09; 95% CI, 1.01 to 1.18; P = .027), and which changes were numerically greatest in nonexpansion states (ORyear, 1.12; 95% CI, 0.94 to 1.32; P = .21). Notably, the groups without statistically significant changes in the odds of forgoing care included those with income > 138% FPL (> 250% FPL: ORyear, 1.03; 139%-250% FPL: ORyear, 1.00), non-Hispanic others (ORyear, 0.91), low-income individuals in states that expanded Medicaid by 2015 (ORyear, 0.92), and those who were other not employed (ie, student, homemaker, retired, and disabled or otherwise unable to work; ORyear, 0.99). After adjusting for insurance status, since changes in insurance status over time could be driving some of the changes in forgoing medical appointments because of cost, the estimates were slightly attenuated overall (ORyear, 1.04; 95% CI, 0.99 to 1.09; P = .11) and across most subgroup analyses (Table 1).
FIG 2.
Temporal trends in forgoing at least one doctor visit in the prior 12 months because of (A) cost overall and by (B) income, (C) race/ethnicity, (D) residence, (E) state Medicaid expansion status, and (F) employment. Care unaffordability refers to forgoing medical appointments because of cost. Subgroups by state Medicaid expansion status are limited to individuals with income ≤ 138% FPL. FPL, federal poverty level.
Changes From 2016 to 2019
The results were largely similar in analyses with our alternative model specification comparing changes from 2016 to 2019 (Table 1).
Changes From 2019 Through 2021
In our secondary analyses, insurance coverage increased in 2021 relative to 2019 overall, with the most prominent increases in Medicaid expansion states (Data Supplement). Forgoing medical appointments because of cost decreased after 2019 overall, with the most prominent decreases in Medicaid expansion states and among non-Hispanic White individuals.
DISCUSSION
Our primary objectives were to assess changes in insurance coverage and forgoing medical appointments because of cost from pre-enactment (2016) through postenactment (2019) of policies affecting the ACA in cancer survivors and identify which subgroups were at greatest risk of reduced coverage and increased forgoing medical appointments because of cost. We found decreases in insurance coverage and increases in individuals reporting forgoing medical appointments because of cost within 12 months, translating to approximately 161,000 fewer cancer survivors who had coverage and 169,000 more survivors reporting forgoing medical appointments because of cost in 2019. Previous studies have shown the trends in insurance coverage for cancer survivors as a whole,21 and early data showed a nonsignificant uptick in noninsurance and care unaffordability from 2016 to 2017-2018 in several vulnerable cancer survivor subgroups, particularly those in nonexpansion states.11,13 Our work adds to present knowledge by (1) demonstrating statistically significant worsening in insurance coverage and care affordability with additional follow-up, (2) examining changes by insurance type revealing increases in Medicaid coverage and decreases in employer-sponsored coverage, (3) exploring the subgroups of cancer survivors most affected by the changes, which included individuals with low income and low-income residents of states that did not expand Medicaid, and (4) additionally evaluating changes in the outcomes during the COVID-19 pandemic, which results demonstrated improved access to care relative to 2019, especially among low-income cancer survivors in states that had previously expanded Medicaid.
Although the causes for the changes in health insurance coverage and forgoing medical appointments because of cost cannot be definitively identified because of the nature of our data, the changes may be related to changes in health insurance policies. Before the trends observed in this study after 2016, ACA provisions were associated with increased insurance coverage and decreased care unaffordability after 2014.9,10,12-14 Although multiple attempts to repeal the ACA since 2017 have been unsuccessful, several other policy changes did occur and may have influenced the present findings.21,27 These policies include cutting resources allocated to enrollment outreach, eliminating the tax penalty associated with the individual mandate, eliminating cost-sharing reductions to insurers, and permitting non–ACA-compliant health insurance plans with limited coverage.21,22,28-30
Although accounting for insurance status in our analyses of forgoing medical appointments because of cost attenuated the estimated odds ratios and resulted in nonsignificant P values, the degree of attenuation was relatively small, suggesting that factors beyond insurance status may have driven changes in forgoing medical appointments because of cost. There are at least three relevant health and public policy changes that may be contributing. First, initially under the ACA, insurers were compensated for the ACA's requirement that they provide reduced cost-sharing to low-income marketplace enrollees, with payments totaling $7 billion US dollars in 2017; however, these payments were later terminated.22 Second, the individual mandate, requiring individuals to purchase health insurance or pay a tax penalty, was removed.22 At least in part because of decreased compensation and loss of healthier enrollees on ACA-compliant health plans (with resultant concentration of sicker enrollees), health insurance providers increased premiums.22 Third, these patterns may have been further exacerbated by the introduction of loosely regulated health plans and short-term insurance policies,22,30 which provide fewer covered benefits. As a result of insurance market destabilization and subsequent out-of-pocket increases, some individuals' financial stability may have jeopardized, leading to the increased forgoing medical appointments because of cost observed in this study. However, other factors may also contribute, such as the rising cost of cancer care.31 However, most of our cohort was not undergoing active anticancer treatments (only 1,974 respondents, or 1.1% of those with a cancer history, reported active treatment).
A subgroup of cancer survivors with among the largest decreases in insurance coverage and especially increases in forgoing medical appointments because of cost were individuals with lower income. Among cancer survivors with income ≤ 138% FPL, the changes in insurance coverage and forgoing medical appointments because of cost were most obvious among those residing in states that did not expand Medicaid. By contrast, there were minimal changes among low-income survivors in states that expanded Medicaid before the study period, which is unsurprising, since Medicaid expansion enabled coverage of this population and has previously been associated with improved health insurance coverage rates and care affordability.13 Hence, Medicaid expansion seems to have been a protective factor against policy changes that otherwise disparately affected individuals with lower income. Combined with the findings that the insurance coverage decreases were primarily in employer-sponsored coverage and that there were increases in Medicaid coverage, disparate changes in insurance coverage and forgoing medical appointments because of cost among low-income cancer survivors suggest that it was working individuals in the coverage gap (ie, individuals residing in nonexpansion states whose income is too high to be eligible for Medicaid coverage but not enough to qualify for subsidized marketplace plans, which require income > 100% FPL) who were disproportionately affected, likely because of increasing costs of coverage as described above. However, it is interesting to note that there were greater absolute and relative decreases in insurance coverage from 2016 to 2019 among individuals eligible for subsidized marketplace plans (income 138%-250% FPL) relative to those with income ≤ 138% FPL. These findings may indicate that marketplace plans were either inadequately used because of inadequate enrollment outreach or inaccessible to these individuals because of still-prohibitive costs as a result of price increases as described above.
We found that insurance coverage and forgoing medical appointments because of cost were stable or improved from 2019 to 2021. These encouraging findings may imply that policies such as expanded premium tax credits and the continuous Medicaid enrollment provision and/or policies addressing the economic impacts of the COVID-19 pandemic were successful in supporting health care access for cancer survivors.32-34
Strengths of this study include the use of a population-based national survey. However, the study has many limitations, largely related to the observational cross-sectional study design and possibility for confounding because of additional policies or other factors for which we could not control. Survey responses may be subject to recall bias, and many participants were not asked or did not answer some of the survey questions (Data Supplement). Furthermore, the outcome of not seeing a doctor because of cost is a limited measure of cancer-related financial burden hardship that fails to capture potentially other relevant domains (eg, forgoing medications, withdrawing savings, forgoing spending on food or housing, etc). Finally, the reliance on the prior 12 months for the forgoing medical appointments because of cost measure leads to a temporal disconnect with the measure of insurance status (on the basis of time of the interview) and timing of federal and state policy enactment, which could affect our results.
From 2016 to 2019, possibly related to policy actions affecting the ACA, fewer cancer survivors had health insurance coverage and more forwent medical care because of cost. Given the association of the ACA adoption with improved cancer prognosis, reversal of the insurance coverage gains may negatively affect cancer outcomes.9,16,17,19,20 Additionally, given the impacts of financial insecurity on access to care and mortality among patients with cancer,7,8 the increase in missing medical appointments because of cost is also concerning. Although early data suggest that insurance coverage and care affordability among cancer survivors during the first 2 years of the COVID-19 pandemic were stable or improving, underscoring the importance of policies directed toward access to care, it is unclear how access to care will be affected after health insurance policies issued under the public health emergency are no longer in effect.32-34 Hence, additional efforts to improve insurance coverage and health care affordability in cancer survivors will likely be needed. The executive order in January 2021 to strengthen the ACA and the recent extension of ACA subsidies may help improve insurance coverage and affordability in cancer survivors.35,36 Recent legislation limiting out-of-pocket medication expenses for Medicare recipients may improve health care affordability for elderly cancer survivors, although its implications on care affordability for the nonelderly population with other insurance types is unclear at this time.36 Other efforts, such as promoting Medicaid expansion in additional states, particularly those actively considering expansion policies,37 or exploring other health and social policies, may also be warranted.
In conclusion, after the enactment of several policies undermining the ACA, the percentage of insured cancer survivors has decreased and the percentage who have forgone medical appointments because of cost has increased. Low-income cancer survivors were particularly affected, which may have been counteracted by Medicaid expansion in the states that chose to expand. Future efforts should focus on improving health care access and reducing cost as a barrier to medical care in patients with cancer.
Evan M. Graboyes
Honoraria: Castle Biosciences
Research Funding: Castle Biosciences (Inst)
Other Relationship: National Cancer Institute
Yvonne M. Mowery
Employment: Duke Health Private Diagnostic Clinic
Honoraria: Oakstone, UpToDate
Research Funding: Merck (Inst)
Nosayaba Osazuwa-Peters
Consulting or Advisory Role: Navigating Cancer
Travel, Accommodations, Expenses: Navigating Cancer
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented in part at the (virtual) 2021 American Society for Clinical Oncology (ASCO) annual meeting.
SUPPORT
N.O.-P. receives funding from the National Institute of Dental and Craniofacial Research (Grant No. K01 DE030916) for research outside the present work. E.M.G. reports receiving funding from the National Cancer Institute and Triologic Society/American College of Surgeons for research outside the presented work.
AUTHOR CONTRIBUTIONS
Conception and design: Justin M. Barnes, Eric Adjei Boakye, Mario Schootman, Haley A. Moss, Nosayaba Osazuwa-Peters
Collection and assembly of data: Justin M. Barnes, Nosayaba Osazuwa-Peters
Data analysis and interpretation: Justin M. Barnes, Evan M. Graboyes, Eric Adjei Boakye, Mario Schootman, Junzo P. Chino, Yvonne M. Mowery, Nosayaba Osazuwa-Peters
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Insurance Coverage and Forgoing Medical Appointments Because of Cost Among Cancer Survivors After 2016
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Evan M. Graboyes
Honoraria: Castle Biosciences
Research Funding: Castle Biosciences (Inst)
Other Relationship: National Cancer Institute
Yvonne M. Mowery
Employment: Duke Health Private Diagnostic Clinic
Honoraria: Oakstone, UpToDate
Research Funding: Merck (Inst)
Nosayaba Osazuwa-Peters
Consulting or Advisory Role: Navigating Cancer
Travel, Accommodations, Expenses: Navigating Cancer
No other potential conflicts of interest were reported.
REFERENCES
- 1.Miller KD, Nogueira L, Mariotto AB, et al. : Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 69:363-385, 2019 [DOI] [PubMed] [Google Scholar]
- 2.Zheng Z, Jemal A, Han X, et al. : Medical financial hardship among cancer survivors in the United States. Cancer 125:1737-1747, 2019 [DOI] [PubMed] [Google Scholar]
- 3.Ellis L, Canchola AJ, Spiegel D, et al. : Trends in cancer survival by health insurance status in California from 1997 to 2014. JAMA Oncol 4:317-323, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harlan LC, Greene AL, Clegg LX, et al. : Insurance status and the use of guideline therapy in the treatment of selected cancers. J Clin Oncol 23:9079-9088, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Parikh-Patel A, Morris CR, Kizer KW: Disparities in quality of cancer care: The role of health insurance and population demographics. Medicine (Baltimore) 96:e9125, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halpern MT, Ward EM, Pavluck AL, et al. : Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol 9:222-231, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Ramsey SD, Bansal A, Fedorenko CR, et al. : Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 34:980-986, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knight TG, Deal AM, Dusetzina SB, et al. : Financial toxicity in adults with cancer: Adverse outcomes and noncompliance. J Oncol Pract 14:e665-e673, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Han X, Yabroff KR, Ward E, et al. : Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the patient protection and Affordable Care Act. JAMA Oncol 4:1713-1720, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soni A, Sabik LM, Simon K, et al. : Changes in insurance coverage among cancer patients under the Affordable Care Act. JAMA Oncol 4:122-124, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Su CT, Okullo D, Hingtgen S, et al. : Affordable Care Act and cancer survivors' financial barriers to care: Analysis of the National Health Interview Survey, 2009-2018. JCO Oncol Pract 17:e1603-e1613, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jemal A, Lin CC, Davidoff AJ, et al. : Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the Affordable Care Act. J Clin Oncol 35:3906-3915, 2017 [DOI] [PubMed] [Google Scholar]
- 13.Han X, Jemal A, Zheng Z, et al. : Changes in noninsurance and care unaffordability among cancer survivors following the Affordable Care Act. J Natl Cancer Inst 112:688-697, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barnes JM, Johnson KJ, Adjei Boakye E, et al. : Impact of the Patient Protection and Affordable Care Act on cost-related medication underuse in nonelderly adult cancer survivors. Cancer 126:2892-2899, 2020 [DOI] [PubMed] [Google Scholar]
- 15.Soni A, Simon K, Cawley J, et al. : Effect of Medicaid expansions of 2014 on overall and early-stage cancer diagnoses. Am J Public Health 108:216-218, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lam MB, Phelan J, Orav EJ, et al. : Medicaid expansion and mortality among patients with breast, lung, and colorectal cancer. JAMA Netw Open 3:e2024366, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Colditz GA, Kozower BD, et al. : Association of Medicaid expansion under the patient protection and Affordable Care Act with non–small cell lung cancer survival. JAMA Oncol 6:1289-1290, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark CR, Ommerborn MJ, Coull BA, et al. : State Medicaid eligibility and care delayed because of cost. N Engl J Med 368:1263-1265, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnes JM, Johnson KJ, Adjei Boakye E, et al. : Early Medicaid expansion and cancer mortality. J Natl Cancer Inst 113:1714-1722, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han X, Zhao J, Yabroff KR, et al. : Association between Medicaid expansion under the Affordable Care Act and survival among newly diagnosed cancer patients. J Natl Cancer Inst 114:1176-1185, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moss HA, Han X, Yabroff KR, et al. : Declines in health insurance among cancer survivors since the 2016 US elections. Lancet Oncol 21:e517, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levitt L: The health care law that continues to escape death. JAMA Health Forum A6, 2017 [Google Scholar]
- 23.CDC—2019 BRFSS survey data and documentation. https://www.cdc.gov/brfss/annual_data/annual_2019.html
- 24.Schootman M, Walker MS, Jeffe DB, et al. : Breast cancer screening and incidence in communities with a high proportion of uninsured. Am J Prev Med 33:379-386, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.2018 Poverty Guidelines. ASPE. https://aspe.hhs.gov/2018-poverty-guidelines [Google Scholar]
- 26.Tarazi WW, Bradley CJ, Harless DW, et al. : Medicaid expansion and access to care among cancer survivors: A baseline overview. J Cancer Surviv 10:583-592, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suit Challenging ACA Legally Suspect but Threatens Loss of Coverage for Tens of Millions. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/suit-challenging-aca-legally-suspect-but-threatens-loss-of-coverage-for-tens-of [Google Scholar]
- 28.McIntyre A, Song Z: The US Affordable Care Act: Reflections and directions at the close of a decade. PLoS Med 16:e1002752, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sommers BD, Clark KL, Epstein AM: Early changes in health insurance coverage under the trump administration. N Engl J Med 378:1061-1063, 2018 [DOI] [PubMed] [Google Scholar]
- 30.Barnes JM, Chino F: Short-term health insurance plans come up short for patients with cancer. JAMA Oncol 8:1101-1103, 2022 [DOI] [PubMed] [Google Scholar]
- 31.Laviana AA, Luckenbaugh AN, Resnick MJ: Trends in the cost of cancer care: Beyond drugs. J Clin Oncol 38:316-322, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilensky GR: Health insurance coverage after the COVID-19 public health emergency ends. JAMA Heal Forum 3:e224207, 2022 [DOI] [PubMed] [Google Scholar]
- 33.Sommers BD, Haffajee RL: Federal policies to expand health insurance coverage during the COVID-19 pandemic and beyond. JAMA Health Forum 2:e214608, 2021 [DOI] [PubMed] [Google Scholar]
- 34.Han X, Shi SK, Zhao J, et al. : The first year of the COVID-19 pandemic and health among cancer survivors in the United States. Cancer 128:3727-3733, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biden JR: Executive Order on Strengthening Medicaid and the Affordable Care Act. The White House. https://www.whitehouse.gov/briefing-room/presidential-actions/2021/01/28/executive-order-on-strengthening-medicaid-and-the-affordable-care-act/ [Google Scholar]
- 36.Biden J: Statement by President Biden on Senate Passage of the Inflation Reduction Act. https://www.whitehouse.gov/briefing-room/statements-releases/2022/08/07/statement-by-president-biden-on-senate-passage-of-the-inflation-reduction-act/ [Google Scholar]
- 37.Status of State Action on the Medicaid Expansion Decision. The Henry J. Kaiser Family Foundation. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Google Scholar]