Abstract
Background:
Home blood pressure (BP) monitoring (HBPM) over a 7-day period is recommended to confirm the diagnosis of hypertension.
Methods:
We determined upper and lower home BP thresholds with >90% positive predictive value (PPV) and >90% negative predictive value (NPV) using 1 to 6 days of monitoring to identify high home BP (systolic BP [SBP] ≥130 mm Hg or diastolic BP [DBP] ≥ 80 mm Hg) based on 7 days of HBPM. The sample included 361 adults from the Improving the Detection of Hypertension Study who were not taking antihypertensive medication. We used two 7-day periods, at least 3 days apart, the first being a sampling period and the second a reference period. For each number of days in the sampling period, we determined the percentage of participants who had a high likelihood of having (>90% PPV) or not having (>90% NPV) high BP and would not need to continue HBPM. Only the participants in an uncertain category (i.e. PPV ≤90% and NPV ≤90%) after each day were carried forward to the next day of HBPM.
Results:
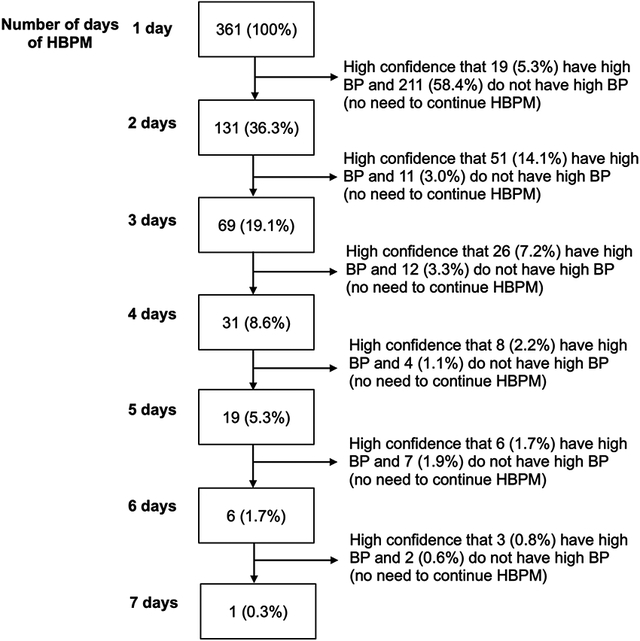
Of the 361 participants (mean [SD] age of 41.3 [13.2] years, 60.4% women), 38.0% had high home BP during the reference period. There were 63.7%, 17.1%, 10.5%, 3.3%, 3.6%, and 1.4% participants who would not need to continue after 1, 2, 3, 4, 5, and 6 days of monitoring.
Conclusions:
In most people, high home BP can be identified or excluded with a high degree of confidence with 3 days or less of monitoring.
Keywords: out-of-office blood pressure monitoring, home blood pressure monitoring, diagnosis, screening, blood pressure thresholds
Graphical Abstract
The diagnosis of hypertension typically relies on blood pressure (BP) measurements taken in the office setting1. To improve the diagnosis of hypertension, out-of-office BP monitoring is recommended in clinical practice guidelines, scientific statements, and policy statements2,3. One method for measuring out-of-office BP is home BP monitoring (HBPM), which involves a person measuring BP at home during the morning and evening over a period of days to weeks.
There are limited data on the number of days that HBPM should be performed to obtain an accurate estimate of someone’s mean home BP4-6. Guidelines recommend that 2 readings be obtained in the morning and in the evening for 7 days7,8. The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guideline recommends that decisions to initiate or intensify antihypertensive medication be based on the average of readings taken over a 7-day monitoring period2. However, conducting HBPM over 7 days may be challenging for patients due to the feasibility of measuring BP twice a day for 7 days in daily life, which is a barrier to the widespread use of HBPM9,10. If fewer days of HBPM are sufficient for confirming or excluding high home BP with a sufficient degree of confidence for most individuals, HBPM would be easier for patients to implement in clinical practice.
The goals of the current study were to determine thresholds for combinations of systolic BP (SBP) and diastolic BP (DBP) on HBPM over 1- to 6-day periods of monitoring that could be used to identify those with high home BP (≥130/80 mm Hg) on 7 days of HBPM with a high positive predictive value (PPV) and high negative predictive value (NPV). The study also determined whether only morning readings or only evening readings based on 1 to 6 days were sufficient to confirm or exclude high home BP.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Sample population.
The study sample consisted of participants from the Improving the Detection of Hypertension (IDH) study, a community-based study in New York City. Enrollment occurred between March 2011 and October 2013. The IDH study included 408 adults aged ≥18 years who were free from known cardiovascular disease (CVD). Study exclusion criteria included office SBP ≥160 mm Hg or DBP ≥105 mm Hg assessed during a screening visit; history of secondary hypertension; taking antihypertensive medication; taking other medications that affect BP (e.g., steroids, tricyclic antidepressants); a self-reported history of kidney, liver, adrenal, thyroid, rheumatologic, or hematologic disease; organ transplantation; recent cancer; dementia; or current pregnancy. The protocol of the IDH study was approved by the Institutional Review Board at Columbia University and all participants provided written informed consent.
As described below, IDH study participants were asked to perform 21 days of HBPM. As BP guidelines, scientific statements, and policy statements recommend a preferred period of 7 days with a minimum of 3 days of HBPM for determining mean home BP1,2,11, we identified the first consecutive 7-day period that included at least 3 days of home BP data with two morning and two evening readings as a sampling period (Figure S1). To obtain an accurate estimate of HBPM over 7 days, a second consecutive 7-day period starting at least 3 days after the end of the sampling period that included at least 24 of the targeted 28 readings (two morning and two evening) was used as a reference period. In this study, we intentionally separated the sampling period from the reference period to allow for the inherent short-term variability in repeat HBPM over time. The current study included 361 participants who met the criteria for the sampling and reference periods.
Study procedures.
Eligible participants attended 5 study visits over a 4-week period (see Figure S2). The IDH study involved three separate assessments of office BP; two 24-hour ambulatory BP monitoring (ABPM) recordings; and 21 days of HBPM. Demographic information was ascertained at the time of study enrollment (Visit 1) using a self-administered questionnaire, and information about CVD risk factors was ascertained by a structured interview. Office BP was measured at Visits 1, 3, and 4 (see Supplemental Methods). HBPM was conducted during the 3 weeks (i.e., 21 days) between Visits 2 and 4.
HBPM.
During Visit 2, participants were provided a HBPM device, Omron HEM-790IT (HEM-7080-ITZ2)12 or HEM-791IT (HEM-7222-ITZ)13 and trained on how to perform HBPM. Participants were instructed to take measurements from their non-dominant arm, after resting for 5 minutes in the seated position, with their arm at heart level. For the 21 days between Visits 2 and 4, participants were asked to measure home BP with 1 minute between readings, twice in the morning after waking and twice before going to bed. For the sampling period, we computed the average of the first day’s readings, the average of the first two days’ readings, the average of the first three days’ readings, and so forth. We also computed the average of all readings obtained during the 7-day reference period. High home BP was defined as mean home SBP/DBP ≥130/80 mm Hg (i.e., mean home SBP ≥130 mm Hg or home DBP ≥80 mm Hg) during the reference period. In a sensitivity analysis, high home BP was defined as mean home SBP/DBP ≥135/85 mm Hg during the reference period.
Statistical Analyses.
Participant characteristics were summarized as mean and SD for continuous variables and frequency and percentage for categorical variables. The sensitivity, specificity, PPV, and NPV for diagnosing high home BP during the reference period (mean home SBP/DBP ≥130/80 mm Hg based on all morning and evening readings) were calculated using high home BP (mean home SBP/DBP ≥130/80 mm Hg) based on 1, 2, 3, 4, 5, 6, and 7 days of morning and evening readings from the sampling period.
Using a previously described method,14,15 among the 361 participants, we determined combinations of mean home SBP and DBP, calculated from the first 1, 2, 3, 4, 5, or 6 days of morning and evening readings from the sampling period that would provide >90% PPV or >90% NPV for having high home BP based on all morning and evening readings from the 7-day reference period. Briefly, logistic regression was used to predict high home BP in the reference period from mean home SBP and DBP for each number of days in the sampling period (see Supplemental Methods for further details). Predicted probabilities for having high home BP during the reference period were then generated for each participant based on their mean home SBP and DBP for 1, 2, 3, 4, 5, and 6 days of morning and evening readings during the sampling period. For each number of days of monitoring, we determined the sensitivity, specificity, PPV, and NPV for high home BP associated with different predicted probability thresholds. We determined the predicted probability that yielded a 90% and secondarily a 95% PPV, and a 90% and secondarily a 95% NPV for having high home BP. BP boundary lines, representing the probability cutoff that yielded these PPV and NPV for high home BP was estimated using the logistic regression equation: . Using this equation, the upper boundary lines for 90% and 95% PPV and lower boundary lines for 90% and 95% NPV in a graph can be generated by calculating home SBP values (on the ordinate axis) from home DBP values (on the abscissa axis), because the predicted probability cutoff, , and the intercept are known:
This formula allows for the determination of the SBP value which, in conjunction with the DBP value, provides 90% (or 95%) PPV, and alternatively, 90% (or 95%) NPV for having high home BP. Three regions on the graph were defined: region A, which included participants above the PPV threshold for whom one could be 90% confident that they would have high home BP during the reference period; region B, which included participants below the NPV threshold for whom one could be 90% confident that they would not have high home BP during the reference period; and region C, an “uncertain category”, which included the remaining participants for whom a determination could not be made with more than 90% confidence. For each number of days of HBPM in the sampling period, we determined the number and percentage of participants who were in each region with only the participants in the uncertain category (region C) being carried forward to the next day of HBPM. Although not the primary focus of the current study, we also conducted these analyses for 7 days of readings from the sampling period to determine the number of participants in regions A, B, and C after a 7-day period of HBPM.
The number and percentage of individuals with a misdiagnosis were determined using the two approaches: when all participants monitored their BP up to a given day of HBPM and using the same BP threshold to define high home BP, and alternatively, when participants moved to the next day of HBPM if they were in the uncertain category using >90% and >95% PPV and NPV thresholds. For the former approach, misdiagnosis was defined as participants who had high home BP based on the sampling period but did not have high home BP on the reference period, and participants who did not have high home BP based on the sampling period but had high home BP on the reference period. For the latter approach, misdiagnosis was defined as participants in region A who did not have high home BP on the reference period, and individuals in region B who had high home BP on the reference period.
The analyses were repeated and the BP boundary lines for 90% PPV and 90% NPV for having high home BP in the reference period (mean home SBP/DBP ≥130/80 mm Hg based on morning and evening readings) were estimated using mean home BP based on only morning readings during the sampling period and, separately, using only evening readings during the sampling period. Finally, a sensitivity analysis was performed by defining high home BP as mean home SBP/DBP ≥135/85 mm Hg.
RESULTS
Participant characteristics
The mean (SD) age of the 361 participants was 41.3 (13.2) years, 60.4% were women, 63.2% and 24.7% self-identified as Hispanic ethnicity and Black race, respectively.
Of the 361 participants, 141 (39.1%) had high office BP, and 138 (38.2%) had high home BP during the 7-day sampling period (Table 1). During the reference period, 137 (38.0%) had high home BP. During the 7-day sampling period, the median (25% percentile - 75% percentile) number of morning and evening readings was 26 (23 - 28), with a median (25% percentile - 75% percentile) of 14 (12 - 14) morning readings, and a median (IQR) of 13 (12 - 14) evening readings.
Table 1.
Participant characteristics (N=361)
| Age, y | 41.3 ± 13.2 |
| Female, % | 218 (60.4%) |
| Race | |
| Black race, % | 89 (24.7%) |
| Hispanic ethnicity, % | 228 (63.2%) |
| Smoking status | |
| Never, % | 296 (82.0%) |
| Past smoker, % | 34 (9.4%) |
| Current smoker, % | 31 (8.6%) |
| Body mass index, kg/m2 | 27.6 ± 5.2 |
| Diabetes, % | 8 (2.2%) |
| SBP, mmHg | |
| Mean office SBP, mercury, Visit 1* | 116.3 ± 15.8 |
| Mean of home morning and evening SBP† | 115.5 ± 13.3 |
| Mean of home morning SBP‡ | 114.8 ± 13.5 |
| Mean of home evening SBP‡ | 116.0 ± 14.0 |
| Mean of home morning and evening SBP (reference period) | 115.9 ± 13.7 |
| DBP, mmHg | |
| Mean office DBP, mercury, Visit 1* | 76.1 ± 10.1 |
| Mean of home morning and evening DBP† | 76.7 ± 9.1 |
| Mean of home morning DBP‡ | 76.8 ± 9.3 |
| Mean of home evening DBP‡ | 76.2 ± 9.4 |
| Mean of home morning and evening DBP (reference period) | 77.0 ± 9.1 |
| Hypertension status based on SBP and DBP§ | |
| Office, mercury, Visit 1* | 141 (39.1%) |
| Home (sampling period)† | 138 (38.2%) |
| Home (reference period) | 137 (38.0%) |
Values are mean ± SD or N (%).
SBP: systolic blood pressure, DBP: diastolic blood pressure
Based on mean of 3 readings
Mean of all readings during the sampling period (for 7 days).
Mean of morning or evening readings during sampling period (for 7 days).
As defined by the 2017 ACC/AHA BP Guideline (mean SBP ≥130 mm Hg or mean DBP ≥80 mm Hg)
Diagnostic accuracy for high home BP
The sensitivity and specificity increased from 78.8% (95% CI: 72% - 86.7%) and 86.6% (95% CI 82.3%-91.1%), respectively, with 1 day of monitoring to 86.9% (95% CI 81.2%-92.5%) and 91.5% (87.8%-95.2%) respectively, with 7 days of monitoring (Table 2). The PPV and NPV increased from 78.3% (95% CI 71.4%-85.1%) and 87.0% (95% CI 82.6%-91.4%), respectively, with 1 day of monitoring to 86.2% (95% CI 80.5%-92.0%) and 91.9% (95% CI 88.4%-95.5%) respectively, with 7 days of monitoring.
Table 2.
Sensitivity, specificity, PPV, and NPV for detecting high home blood pressure in the reference period according to having high home blood pressure (≥130/80 mmHg) based on 1, 2, 3, 4, 5, 6 and 7 days of morning and evening readings during the sampling period
| High home blood pressure (≥130/80 mmHg) based on the number of days in the sampling period | |||||||
|---|---|---|---|---|---|---|---|
| 1 day | 2 days | 3 days | 4 days | 5 days | 6 days | 7 days | |
|
Sensitivity
(95% CI) |
78.8% (72.0% - 86.7%) |
81.0% (74.5% - 87.6%) |
81.8% (75.3% - 88.2%) |
81.8% (75.3% - 88.2%) |
83.9% (77.8% - 90.1%) |
86.1% (80.3% - 91.9%) |
86.9 % (81.2% - 92.5%) |
|
Specificity
(95% CI) |
86.6% (82.3% - 91.1%) |
85.3% (80.6% - 89.9%) |
89.7% (85.8% - 93.7%) |
92.0% (88.4% - 95.5%) |
93.8% (90.1% - 96.9%) |
91.1% (87.3% - 94.8%) |
91.5% (87.8% – 95.2%) |
|
PPV
(95% CI) |
78.3% (71.4% - 85.1%) |
77.1% 70.2% - 84.0%) |
83.0% (76.6% - 89.3%) |
86.2% (80.2% - 92.1%) |
89.2% (83.8% - 94.5%) |
85.5% (79.6% - 91.4%) |
86.2% (80.5% - 92.0%) |
|
NPV
(95% CI) |
87.0% (82.6% - 91.4%) |
88.0% (83.7% - 92.3%) |
88.9% (84.9% - 93.0%) |
89.2% (85.2% - 93.2%) |
90.5% (86.8% - 94.3%) |
91.5% (87.8% - 95.1%) |
91.9% (88.4% - 95.5%) |
NPV: negative predictive value, PPV: positive predictive value
BP thresholds to detect high home BP with high PPV and NPV based on an increasing number of days of monitoring using morning and evening readings
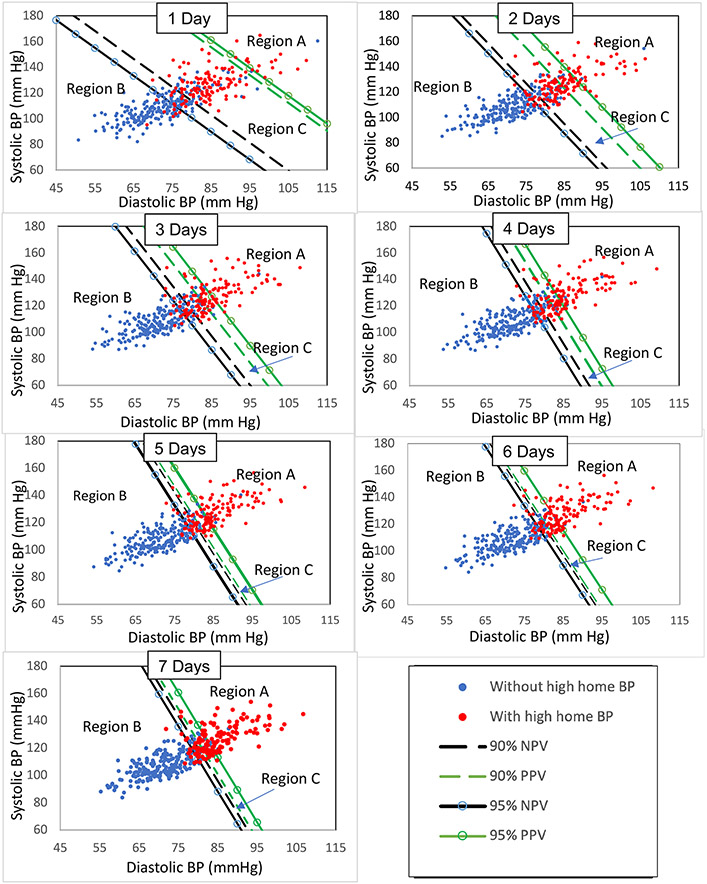
Figure 1 shows the scatter plots of the mean home SBP and DBP measurements for 1, 2, 3, 4, 5, 6, and 7 days of monitoring, and the 90% PPV, 95% PPV, 90% NPV, and 95% NPV boundary lines for detecting high home BP based on the reference period. Values for predictive probability corresponding to the 90% PPV and 90% NPV, and 95% PPV and 95% NPV boundary lines are provided in Table S1. Table 3 shows the formulae for determining the boundary lines, which were used to identify if an individual’s BP is in region A (i.e. high likelihood for having high home BP), B (i.e. high likelihood for not having high home BP), or C (i.e. uncertain category). The boundary lines for 90% PPV and 90% NPV, and boundary lines for 95% PPV and 95% NPV became closer to one another as the number of days used to calculate mean home BP increased from 1 to 7 days, which resulted in fewer participants in the uncertain category.
Figure 1. Scatter plots of home systolic and diastolic BP levels for 361 participants based on 1, 2, 3, 4, 5, 6, and 7 days of morning and evening readings from the sampling period.
Participants with high home BP based on the reference period appear as red circles while participants without high home BP are shown in blue. Region A contains combinations of systolic and diastolic BP levels with a high degree of confidence for having high home BP (greater than 90% PPV and greater than 95% PPV). Region B contains combinations systolic and diastolic BP levels with a high degree of confidence for not having high home BP (greater than 90% NPV and greater than 95% NPV). Region C represents the region of uncertainty.
BP: blood pressure; NPV: negative predictive value; PPV: positive predictive value
Table 3.
Formulae to calculate the systolic blood pressure threshold from diastolic blood pressure using morning and evening readings during the sampling period
| 1 day | 2 days | 3 days | 4 days | 5 days | 6 days | 7 days | |
|---|---|---|---|---|---|---|---|
| 90% PPV | 340.0 – 2.2 x DBP | 391.1 – 3.2 x DBP | 430.3 – 3.7 x DBP | 505.9 – 4.7 x DBP | 483.9 – 4.5 x DBP | 476.7 – 4.4 x DBP | 504.9 – 4.8 x DBP |
| 90% NPV | 287.4 – 2.2 x DBP | 363.2 – 3.2 x DBP | 413.4 – 3.7 x DBP | 491.0 – 4.7 x DBP | 479.4 – 4.5 x DBP | 473.0 – 4.4 x DBP | 499.9 – 4.8 x DBP |
| 95% PPV | 345.5 – 2.2 x DBP | 407.9 – 3.2 x DBP | 443.5 – 3.7 x DBP | 519.1 – 4.7 x DBP | 497.7 – 4.5 x DBP | 492.0 – 4.4 x DBP | 517.1 – 4.8 x DBP |
| 95% NPV | 274.2 – 2.2 x DBP | 355.5 – 3.2 x DBP | 402.9 – 3.7 x DBP | 480.0 – 4.7 x DBP | 470.0 – 4.5 x DBP | 465.7 – 4.4 x DBP | 492.2 – 4.8 x DBP |
These formulae can be used to determine if an individual’s BP is in region A, B, or C. For example, a person with SBP/DBP of 170/85 mm Hg after one day of HBPM (Day 1), would be in region A (using a 90% PPV threshold) since the person’s SBP (170 mm Hg) is greater than the calculated SBP of 153.0 mm Hg based on the individual’s DBP of 85 mm Hg. Another person with SBP/DBP of 122/70 mm Hg after one day of HBPM (Day 1), would be in region B (using a 90% NPV threshold) since the person’s SBP (122 mm Hg) is less than the calculated SBP of 133.4 mm Hg based on the individual’s DBP of 70 mm Hg. By definition, a person not in region A or region B is in region C.
NPV: negative predictive value, PPV: positive predictive value, SBP: systolic blood pressure, DBP: diastolic blood pressure
For the 90% PPV and 90% NPV boundary lines, of the 361 participants, there were 230 (63.7%), 62 (17.1%), 38 (10.5%), 12 (3.3%), 13 (3.6%), 5 (1.4%), and 1 (0.3%) not in the uncertain category after 1, 2, 3, 4, 5, 6, and 7 days of monitoring (Table 4). For the 95% PPV and 95% NPV boundary lines, of the 361 participants, there were 178 (49.3%), 55 (15.3%), 27 (7.5%), 24 (6.7%), 18 (5.0%), 9 (2.5%), and 3 (0.8%) not in the uncertain category after 1, 2, 3, 4, 5, 6, and 7 days of monitoring.
Table 4.
Number and percentage of participants in each category for 1 day, 2 days, 3 days, 4 days, 5 days, 6 days, and 7 days of readings with participants moving to the next day of HBPM only if in the uncertain category using 90% and 95% positive and negative predictive value thresholds for high home BP (≥130/80 mmHg)
| 1 day | 2 days | 3 days | 4 days | 5 days | 6 days | 7 days | |
|---|---|---|---|---|---|---|---|
| Using 90% PPV and 90% NPV thresholds | |||||||
| Region A | 19 (5.3%) | 51 (14.1%) | 26 (7.2%) | 8 (2.2%) | 6 (1.7%) | 3 (0.8%) | 0 (0%) |
| Region B | 211 (58.4%) | 11 (3.0%) | 12 (3.3%) | 4 (1.1%) | 7 (1.9%) | 2 (0.6%) | 1 (0.3%) |
| Region C | 131 (36.3%) | 69 (19.1%) | 31 (8.6%) | 19 (5.3%) | 6 (1.7%) | 1 (0.3%) | 0 (0%) |
| Total | 361 | 131 | 69 | 31 | 19 | 6 | 1 |
| Using 95% PPV and 95% NPV thresholds | |||||||
| Region A | 17 (4.7%) | 23 (6.4%) | 19 (5.3%) | 18 (5.0%) | 5 (1.4%) | 4 (1.1%) | 3 (0.8%) |
| Region B | 161 (44.6%) | 32 (8.9%) | 8 (2.2%) | 6 (1.7%) | 13 (3.6%) | 5 (1.4%) | 0 (0%) |
| Region C | 183 (50.7%) | 128 (35.5%) | 101 (28.0%) | 77 (21.3%) | 59 (16.3%) | 50 (13.9%) | 47 (13.1%) |
| Total | 361 | 183 | 128 | 101 | 77 | 59 | 50 |
Region A represents systolic and diastolic BP levels with greater than the PPV thresholds for high home BP (≥130/80 mmHg). Region B represents systolic and diastolic BP levels with greater than the NPV thresholds for high home BP. Region C represents the region of uncertainty. The table shows the number of participants in regions A and B when only the participants in the uncertain category (region C) were carried forward to the subsequent day of monitoring. The percentages shown are out of the total 361 participants.
HBPM: home blood pressure monitoring, NPV: negative predictive value, PPV: positive predictive value
When all 361 participants monitored their BP up to a given day of HBPM, the percentage of participants with a misdiagnosis decreased from 1 to 7 days of monitoring (Table S2). In contrast, using either >90% or >95% PPV and NPV BP thresholds, the percentage of participants required to do HBPM for the specified monitoring period decreased as the cumulative percentage of participants with a misdiagnosis increased. Compared to having participants monitor their BP up to a given day, the percentage of participants with a misdiagnosis was lower for days 1-3, and higher for days 4-7 using 90% PPV and 90% NPV thresholds. The percentage of participants with a misdiagnosis was consistently lower for days 1-7 using 95% PPV and 95% NPV thresholds. When all 361 participants monitored their BP for 3 days, 48 (13.3%) had a misdiagnosis. Using >90% PPV and >90% NPV thresholds, of the 361 participants, 69 (19.1%) were required to perform HBPM for 3 days, and 40 (11.1%) participants had a misdiagnosis. Using >95% PPV and >95% NPV thresholds, of the 361 participants, 128 (35.5%) participants were required to perform HBPM for 3 days, and 19 (5.3%) participants had a misdiagnosis.
BP thresholds to diagnose high home BP with high PPV and NPV based on an increasing number of days of monitoring using only morning or evening readings
The scatter plots of home SBP and DBP for 1 to 7 days of monitoring along with the corresponding 90% PPV, 95% PPV, 90% NPV, and 95% NPV boundary lines, using only morning readings and only evening readings are shown in Figure S3 and Figure S4, respectively. Values for predictive probability corresponding to the 90% PPV and 90% NPV, and 95% PPV and 95% NPV boundary lines using only morning readings and only evening readings, are provided in Table S3 and Table S4, respectively. Tables S5 and S6 show the formulae for determining boundary lines for only morning readings and only evening readings, respectively. The boundary lines for 90% PPV and 90% NPV became closer to one another as the number of days used to calculate mean home BP increased. Participants in the uncertain category (region C) contained fewer participants with more days of HBPM.
Sensitivity analysis defining high home BP as ≥135/85 mm Hg
The prevalence of high home BP (≥135/85 mm Hg) was 18.8% and 20.5% in the sampling and reference periods, respectively. Sensitivity, specificity, PPV, and NPV after defining high home BP as ≥135/85 mm Hg are provided in Table S7. Table S8 shows the number and percentage of participants who were in regions A and B with only the participants in the uncertain category (region C) being carried forward to the next day of HBPM. Compared to having participants monitor their BP up to a given day, the percentage of participants with a misdiagnosis was lower for days 1 and 2, and higher for days 3, 4, 5, 6, and 7 using 90% PPV and 90% NPV thresholds for having high home BP defined as ≥135/85 mm Hg (Table S9).
DISCUSSION
Among participants not currently taking antihypertensive medication, the use of higher or lower BP thresholds that provide a high confidence of having (i.e. greater than 90% PPV) or not having (i.e. greater than 90% NPV) high BP would allow many individuals to monitor home BP for far less than the currently recommended 7 days. Higher or lower BP thresholds for only morning or only evening home BP readings would similarly allow for shorter duration of HBPM. When evaluating individuals for the presence or absence of high home BP, clinicians could use the formulae presented in Table 3 (using morning and evening readings), Table S5 (using only morning readings), and Table S6 (using only evening readings) to determine if an individual’s BP is in regions A or B (i.e. high degree of confidence for identifying or excluding high home BP, respectively), or alternatively, in region C (uncertain category) after each number of days of HBPM. If the BP is in region C, the person would need to perform an additional day of HBPM.
Several guidelines and scientific statements recommend that HBPM with 2 morning and 2 evening readings each day for 7 days is the preferred approach for HBPM2,3. However, this approach may not be practical for conducting HBPM. Chen et al reported in a study of 2272 participants, only 4.4% in clinical practice were obtaining 2 morning and 2 evening readings for 7 days22. The current study demonstrated that higher and lower BP thresholds could be identified that would permit many individuals to be classified as having or not having high BP with a fewer number of days of monitoring.
BP guidelines indicate that 3 days of HBPM may be sufficient23,24. A systematic review by Verberk et al. concluded that a minimum of 3 days of monitoring has sufficient diagnostic accuracy for high BP7. Bello et al. found that for diagnosing high BP, there was good reproducibility for 3 days of HBPM4. Kyriakoulisa et al. also showed that 3 days of HBPM may be sufficient for determining mean home BP25. In a systematic review conducted by Hodgkinson et al., there was only a small theoretical increase in prognostic value of home BP for cardiovascular events from 3 to 7 days of monitoring26. In the current study, using a BP threshold of 130/80 mm Hg to define high home BP, 3 days of HBPM had 81.8% sensitivity, 89.7% specificity, 83.0% PPV, and 88.9% NPV for diagnosing high home BP defined as ≥130/80 mm Hg using 7 days of monitoring. While the PPV and NPV are high, neither was greater than 90%. Using BP thresholds that have a high degree of confidence for identifying or excluding high home BP (>90% PPV or 90% NPV, respectively), 230 (63.7%), 62 (17.1%), and 38 (10.5%) were not in the uncertain category after completing 1, 2, and 3 days of HBPM, and therefore could stop HBPM. These results indicate that a large majority of participants can already be identified or excluded for having high home BP within the first 3 days of HBPM.
After 3 days, misdiagnosis was more common with the approach of having all participants conducting HBPM each day compared with having participants move to the next monitoring day only if they are in the uncertain category. Although misdiagnosis was more common with the latter approach after 4, 5 and 6 days of monitoring, it only affected a small percentage of participants who performed this duration of monitoring and were deemed to have or not have high home BP. Therefore, it may be reasonable for this small group of individuals to complete 7 days of HBPM. Finally, for all number of days of monitoring, compared with using a BP threshold of 130/80 mm Hg, misdiagnosis was consistently less common using BP thresholds with an even higher degree of confidence for identifying or excluding high home BP (>95% PPV and >95% NPV, respectively). The trade-off is that more individuals would be in the uncertain category after each day of monitoring, using >95% PPV and >95% NPV BP thresholds than using >90% PPV and >90% NPV BP thresholds.
Implementing the use of these higher and lower home BP thresholds with fewer days of HBPM would be advantageous to use with emerging home telemonitoring technologies that allow for home BP data to be sent to the clinician. If the HBPM data software was able to automatically average BP readings, and apply these thresholds to patient data on a daily basis, it could alert clinicians and their patients that it was no longer necessary to continue if the mean home BP measurements were above the 90% PPV or below the 90% NPV BP threshold after a particular number of days of monitoring. This would allow patients to undergo fewer days of HBPM, which may encourage greater use of HBPM by clinicians as HBPM would be less burdensome to patients.
Finally, the results of the current study also suggest that a large percentage of individuals could perform fewer days of HBPM if a high home BP is defined as ≥135/85 mm Hg. Of the 361 participants, 310 (85.9%) and 19 (5.3%) were not in the uncertain category after completing 1 and 2 days of HBPM. Further, after 1 or 2 days, misdiagnosis was less common having participants move to the next day only if they are in the uncertain category, compared with having all participants conduct HBPM each day. Misdiagnosis was more common with the former approach after 3, 4, 5, and 6 days of monitoring, but this issue only affected a small percentage of participants.
There are several strengths to this study. First, the participants reflect a diverse, community-based population. The study had good representation of women and men, and persons who self-reported being Black or Hispanic. Second, the study design was rigorous, and the participants were trained on proper HBPM data collection. The current study may also have several limitations. The population was relatively young, comprised of mostly never smokers, and had a low prevalence of diabetes, suggesting that our results may not apply to older adults with comorbid conditions and who have higher baseline risk for CVD. Future studies should conduct analyses stratified by categories defined by age, gender, race/ethnicity, and comorbid conditions to determine whether our findings are generalizable to those who are more likely or less likely to have hypertension. Individuals taking antihypertensive medication were excluded, therefore our results may not be applicable for determining BP control among those taking antihypertensive medication. The mean office BP and home BP were relatively low. However, the prevalence of hypertension was 39.1% based on office BP, and 38.0% based on home BP, indicating that the sample had sufficient BP distribution for the analyses. The study required for the sampling period that there be at least 3 days of home BP data with two morning and two evening readings. This may be challenging for some individuals to perform. Finally, the analysis relied on a reference period that may not reflect the “true” reference standard for having high home BP or not. However, this issue reflects the practical nature of classifying and managing high BP in the real world, where a true reference standard for high home BP is not available due to imperfect reproducibility. We chose a 7-day period for a reference period as multiple BP guidelines, scientific statements, and policy statements recommend 7 days as a preferred period of HBPM1,2,11. Our data confirms that HBPM does not have perfect reproducibility since after 7 days of HBPM, the sensitivity, specificity, PPV, and NPV were not 100%.
Perspectives
Patients may have difficulty conducting HBPM over a 7-day period to confirm the diagnosis of hypertension. The current study demonstrates that using higher or lower BP thresholds with a high degree of confidence for identifying (greater than 90% PPV) or excluding (greater than 90% NPV) high home BP, respectively, would allow for fewer than 7 days of HBPM for almost everyone. Using this approach, many individuals with and without high home BP could be detected with 3 days or less of monitoring being collected. These findings suggest that this approach may be practical for high BP screening in the general population.
Supplementary Material
Novelty and Relevance.
What Is New?
Using 90% PPV and 90% NPV thresholds with 7 days of monitoring as a reference period, of the 361 participants, there were 230 (63.7%), 62 (17.1%), 38 (10.5%), 12 (3.3%), 13 (3.6%), 5 (1.4%), and 1 (0.3%) not in the uncertain category after 1, 2, 3, 4, 5, 6, and 7 days of monitoring, and would not need to do an additional day of monitoring.
What Is Relevant?
This study determined thresholds for combinations of SBP/DBP on HBPM over fewer days of monitoring that could be used to identify those with a high PPV and high NPV for having high home BP (≥130/80 mm Hg) on 7 days of HBPM.
Clinical/Pathophysiological Implications.
Most people’s high home BP can be detected with >90% PPV, or ruled out with >90% NPV with 3 days or less of monitoring, which may improve adherence to home monitoring and improve clinical utilization.
Funding
Dr. Bradley received support through T32 HL007854-25. This work was supported by P01-HL047540 (D. Shimbo, J.E. Schwartz) from the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health (NIH).
Abbreviations:
- BP
Blood pressure
- HBPM
home blood pressure monitoring
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- IDH
Improving the Detection of Hypertension
- ABPM
ambulatory blood pressure monitoring
Footnotes
Disclosures
None
REFERENCES
- 1.Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend R, et al. Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension. 2019;73(5):e35–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. [DOI] [PubMed] [Google Scholar]
- 3.Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021–3104. [DOI] [PubMed] [Google Scholar]
- 4.Bello NA, Schwartz JE, Kronish IM, Oparil S, Anstey DA, Wei Y, Cheung YK, Muntner P, Shimbo D. Number of Measurements Needed to Obtain a Reliable Estimate of Home Blood Pressure: Results From the Improving the Detection of Hypertension Study. Journal of the American Heart Association. 2018;7(20):e008658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niiranen TJ, Asayama K, Thijs L, Johansson JK, Hara A, Hozawa A, Tsuji I, Ohkubo T, Jula AM, Imai Y, et al. Optimal number of days for home blood pressure measurement. American Journal of Hypertension. 2015;28(5):595–603. [DOI] [PubMed] [Google Scholar]
- 6.Verberk WJ, Kroon AA, Kessels AG, de Leeuw PW. Home blood pressure measurement: a systematic review. Journal of the American College of Cardiology. 2005;46(5):743–751. [DOI] [PubMed] [Google Scholar]
- 7.Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, Cloutier L, Gelfer M, Lamarre-Cliché M, Milot A, Bolli P, et al. Hypertension Canada's 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. The Canadian Journal of Cardiology. 2016;32(5):569–588. [DOI] [PubMed] [Google Scholar]
- 8.Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. Journal of Human Hypertension. 2010;24(12):779–785. [DOI] [PubMed] [Google Scholar]
- 9.Kronish IM, Kent S, Moise N, Shimbo D, Safford MM, Kynerd RE, O'Beirne R, Sullivan A, Muntner P. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. Journal of the American Society of Hypertension. 2017;11(9):573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niessen MA, van der Hoeven NV, van den Born BJ, van Kalken CK, Kraaijenhagen RA. Home blood pressure measurement as a screening tool for hypertension in a web-based worksite health promotion programme. European Journal of Public Health. 2014;24(5):776–781. [DOI] [PubMed] [Google Scholar]
- 11.Shimbo D, Artinian NT, Basile JN, Krakoff LR, Margolis KL, Rakotz MK, Wozniak G. Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement From the American Heart Association and American Medical Association. Circulation. 2020;142(4):e42–e63. [DOI] [PubMed] [Google Scholar]
- 12.Coleman A, Steel S, Freeman P, de Greeff A, Shennan A. Validation of the Omron M7 (HEM-780-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Pressure Monitoring. 2008;13(1):49–54. [DOI] [PubMed] [Google Scholar]
- 13.Topouchian J, Agnoletti D, Blacher J, Youseff A, Chahine MN, Ibanez I, Assemani N, Asmar R. Validation of four devices: Omron M6 Comfort, Omron HEM-7420, Withings BP-800, and Polygreen KP-7670 for home blood pressure measurement according to the European Society of Hypertension International Protocol. Vascular Health and Risk Management. 2014;10:33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shimbo D, Kuruvilla S, Haas D, Pickering TG, Schwartz JE, Gerin W. Preventing misdiagnosis of ambulatory hypertension: algorithm using office and home blood pressures. Journal of Hypertension. 2009;27(9):1775–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Booth JN 3rd, Muntner P, Diaz KM, Viera AJ, Bello NA, Schwartz JE, Shimbo D. Evaluation of Criteria to Detect Masked Hypertension. Journal of Clinical Hypertension. 2016;18(11):1086–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Studies comparing ambulatory blood pressure and home blood pressure on cardiovascular disease and mortality outcomes: a systematic review. Journal of the American Society of Hypertension. 2016;10(3):224–234.e217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Annals of Internal Medicine. 2015;163(9):691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nwankwo T, Coleman King SM, Ostchega Y, Zhang G, Loustalot F, Gillespie C, Chang TE, Begley EB, George MG, Shimbo D, et al. Comparison of 3 Devices for 24-Hour Ambulatory Blood Pressure Monitoring in a Nonclinical Environment Through a Randomized Trial. American Journal of Hypertension. 2020;33(11):1021–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Viera AJ, Lingley K, Hinderliter AL. Tolerability of the Oscar 2 ambulatory blood pressure monitor among research participants: a cross-sectional repeated measures study. BMC Medical Research Methodology. 2011;11:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwartz JE, Muntner P, Kronish IM, Burg MM, Pickering TG, Bigger JT, Shimbo D. Reliability of Office, Home, and Ambulatory Blood Pressure Measurements and Correlation With Left Ventricular Mass. Journal of the American College of Cardiology. 2020;76(25):2911–2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinderliter AL, Lin FC, Viera LA, Olsson E, Klein JL, Viera AJ. Hypertension-mediated organ damage in masked hypertension. Journal of Hypertension. 2022;40(4):811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zuo HJ, Ma JX, Wang JW, Chen XR. Assessing the routine-practice gap for home blood pressure monitoring among Chinese adults with hypertension. BMC Public Health. 2020;20(1):1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stergiou GS, Skeva II, Zourbaki AS, Mountokalakis TD. Self-monitoring of blood pressure at home: how many measurements are needed? Journal of Hypertension. 1998;16(6):725–731. [DOI] [PubMed] [Google Scholar]
- 24.Stergiou GS, Nasothimiou EG, Kalogeropoulos PG, Pantazis N, Baibas NM. The optimal home blood pressure monitoring schedule based on the Didima outcome study. Journal of Human Hypertension. 2010;24(3):158–164. [DOI] [PubMed] [Google Scholar]
- 25.Kyriakoulis KG, Ntineri A, Niiranen TJ, Lindroos A, Jula A, Schwartz C, Kollias A, Andreadis EA, McManus RJ, Stergiou GS. Home blood pressure monitoring schedule: optimal and minimum based on 2122 individual participants' data. J Hypertens. 2022;40(7):1380–1387. [DOI] [PubMed] [Google Scholar]
- 26.Hodgkinson JA, Stevens R, Grant S, Mant J, Bray EP, Hobbs FDR, Martin U, Schwartz C, McCartney D, O'Mahony R, et al. Schedules for Self-monitoring Blood Pressure: A Systematic Review. Am J Hypertens. 2019. Mar 16;32(4):350–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.