Abstract
Written instructions improve patient comprehension of discharge instructions but are often provided only in English even for patients with a non-English language preference (NELP). We implemented standardized written discharge instructions in English, Spanish, and Chinese for hospital medicine patients at an urban academic medical center. Using an interrupted time series analysis, we assessed impact on medication-related post-discharge questions for patients with English, Spanish, or Chinese language preference. Of 4013 patients, ~15% had NELP. Pre-intervention, Chinese-preferring patients had a 5.6 percentage point higher probability of questions (aOR=1.55, 95% CI: 1.08, 2.21) compared to English-preferring patients; Spanish-preferring and English-preferring patients had similar rates of questions. Post-intervention, English-preferring and Spanish-preferring patients had no significant change; Chinese-preferring patients had a significant 10.9 percentage point decrease in probability of questions (aOR=0.38, 95% CI 0.21, 0.69) thereby closing the disparity. Language-concordant written discharge instructions may reduce disparities in medication-related post-discharge questions for patients with NELP.
Keywords: Language Barriers, Limited English Proficiency, Patient Discharge, Discharge Instructions
INTRODUCTION
Transitions from hospital to home are high-risk times for adverse events. Adverse drug events (ADEs) are particularly common with studies estimating ADEs in ~20% of hospital discharges, resulting in worse patient outcomes and increased costs.1 Poor patient recall and comprehension of discharge instructions is a major contributor, particularly in patients with language barriers.2,3
High-quality written instructions reinforce important information and improve recall.4 The Society of Hospital Medicine and an Institute of Medicine publication have recommendations for optimal discharge instructions.5,6 However, there is significant variation in implementation of comprehensive instructions,7 which is exacerbated for patients with a non-English language preference (NELP) who often do not receive instructions in their preferred language in the United States.
Although American policy requires hospitals receiving funding from the Centers for Medicare and Medicaid Services to provide language access for patients with NELP, including translation of “vital documents,” one study found that only ~60% of hospitals provide discharge instructions in their most common non-English language, and ~25% of hospitals provide instructions in more than one non-English language.8 In many clinical settings where only English written instructions are available and clinicians use interpreters to assist with communicating discharge instructions, studies have shown that patients with NELP have lower understanding of follow-up and medication instruction and are less likely to receive counseling on all the elements of discharge instructions.3,9
To address the limited provision of language-concordant written instructions to patients with NELP and its impact on patient comprehension, we implemented a quality improvement intervention where we provided standardized written instructions in English and the most common non-English languages in our patient population. By leveraging already collected data from our automated post-discharge phone call program, we studied the impact of these standardized instructions on patient reported questions about their medications after discharge.
METHODS
Study Setting and Intervention
We implemented standardized written instructions on the Medicine Service at the University of California San Francisco Medical Center at Parnassus, a 600-bed quaternary care academic medical center. Our instructions were created by initially consulting published recommendations5,6 and then modified based on feedback from patient advisory boards and multidisciplinary clinical unit leadership teams. Instructions included: the admission diagnosis and hospital course; medication changes (new medications, dose changes, and discontinuations); follow-up plans; and return precautions (Appendix 1). In March 2018, we implemented the instructions in English. After ensuring acceptance and assessing for unanticipated consequences through conversations with unit leadership, clinicians, and bedside nurses, we implemented Spanish and Chinese instructions in August 2018. This evaluation included only patients discharged from the Hospital Medicine Service with an English, Spanish, or Chinese language preference who received a post discharge phone call from 7/1/2017 – 4/30/2019. We included any Chinese language preference because written Chinese is the same for all dialects, and our intervention was focused on written communication. Patients with an English language preference who answered the post-discharge phone call in Spanish or Chinese were also included in the Spanish or Chinese language preference group respectively. This study was approved by our institutional review board.
Primary Outcome and Data Collection
Our primary outcome was whether patients had questions about their medications (yes/no) collected from 7/1/2017–4/30/2019 via an automated 72-hour post-discharge phone call conducted in English, Spanish, or Chinese (Cantonese). This program has been previously described in detail.10,11 In brief, our institution implemented a hospital wide care transitions outreach program in March 2017 with a goal of contacting all patients discharged from the hospital to identify and address care transition problems. All patients received an automated phone call through a third-party system (CipherHealth Voice, New York City) that delivered a scripted call and recorded patient’s entered responses (e.g., 1 = yes, 2 = no). If patients identified issues, a care transition nurse called the patient manually to follow-up in the patient’s preferred language, using an interpreter if the nurse was not fluent in the patient’s preferred language. The nurse recorded details about the interaction in the electronic health record.
Analytic Approach
All analyses were conducted in R Statistical Software (v4.2.1; R Core Team 2022).12 We conducted a logistic regression using generalized estimating equations with robust standard errors clustered on person (to account for patients with multiple admissions) using the geepack package. We assessed the intervention’s effect on outcomes with an interrupted time series analysis, using the corresponding intervention month for patients based on language preference. The final model adjusted for age and length of stay (LOS) and included an interaction term for intervention and language preference. We generated estimated marginal probabilities using the ggeffects package and plotted them using ggplot2. We also report descriptive statistics on the uptake of the standardized instructions.
RESULTS
Among 5154 discharges, we included 4013 patients who spoke English, Spanish, or Chinese (Table 1). Approximately 9% (366) preferred Chinese and 5% (197) preferred Spanish. The mean LOS was 4.22 days in the 5154 encounters, and there were medication questions after 597 (11.6%) of the discharges. Patients reported more post-discharge medication questions pre-intervention than post-intervention (13.0% vs 10.6%, p=0.010). Within the first three months of the intervention implementation, physicians used the standardized instructions in 75% (464/618) of patients discharged with an English preference and 84% (87/104) of patients discharged with a NELP. Rates were similar in the last three months of our studied period: 86% (458/532) of English-preferring patients and 81% (86/106) of patients with a NELP.
Table 1.
Characteristics of hospital medicine patients from 07/2017–04/2019.
| Pre1
N = 1731 |
Post1 N = 2510 |
Total N = 40132 |
|
|---|---|---|---|
| Mean number of hospital encounters per person (sd) | 1.19 (0.64) | 1.23 (0.69) | 1.28 (0.82) |
| Median number of hospital encounters per person (1st quartile, 3rd quartile) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| Language preference | |||
| English | 1372 (79.3%) | 2267 (90.3%) | 3450 (86.0%) |
| Chinese | 232 (13.4%) | 159 (6.3%) | 366 (9.1%) |
| Spanish | 127 (7.3%) | 84 (3.3%) | 197 (4.9%) |
| Sex | |||
| Male | 848 (49.0%) | 1248 (49.7%) | 2008 (50.0%) |
| Female | 883 (51.0%) | 1262 (50.3%) | 2005 (50.0%) |
| Mean Age (sd) | 60.1 (19.3) | 59.0 (18.9) | 59.4 (18.9%) |
| Race/Ethnicity | |||
| White or Caucasian | 764 (44.1%) | 1261 (50.2%) | 1925 (48.0%) |
| Asian | 412 (23.8%) | 468 (18.6%) | 830 (20.7%) |
| Hispanic or Latino | 255 (14.7%) | 332 (13.2%) | 548 (13.7%) |
| Black or African American | 173 (10.0%) | 267 (10.6%) | 411 (10.2%) |
| Native Hawaiian or Other Pacific Islander | 26 (1.5%) | 34 (1.4%) | 58 (1.5%) |
| American Indian or Alaska Native | 10 (0.6%) | 16 (0.6%) | 25 (0.6%) |
| Unknown or Declined | 17 (1.0%) | 16 (0.6%) | 33 (0.8%) |
| Other | 74 (4.3%) | 116 (4.6%) | 183 (4.6%) |
For those with an English language preference, the Pre-Intervention period was 07/2017–02/2018 (8 months) and the Post-Intervention period was 03/2018–04/2019 (14 months). For those with a non-English language preference, the Pre-Intervention period was 07/2017–07/2018 (13 months) and the Post-Intervention period was 08/2018–04/2019 (9 months).
Total number of individuals is 4013. Some individuals are represented in both the pre and post groups, thus the pre and post sample sizes add up to more than the total.
In adjusted analyses, pre-intervention the probability of having post-discharge medication questions was 4.2 percentage points higher among patients with NELP versus English-preferring patients (aOR=1.38, 95% CI: 1.01, 1.88; see Appendix 2 and 3). This was driven by Chinese-preferring patients who had a 5.6 percentage point higher probability of post-discharge medication questions (aOR=1.55, 95% CI: 1.08, 2.21; see Appendix 4) compared to English-speakers. There was no significant difference between Spanish and English-speakers (aOR for Spanish-speakers = 1.12, 95% CI: 0.69, 1.80; see Appendix 4).
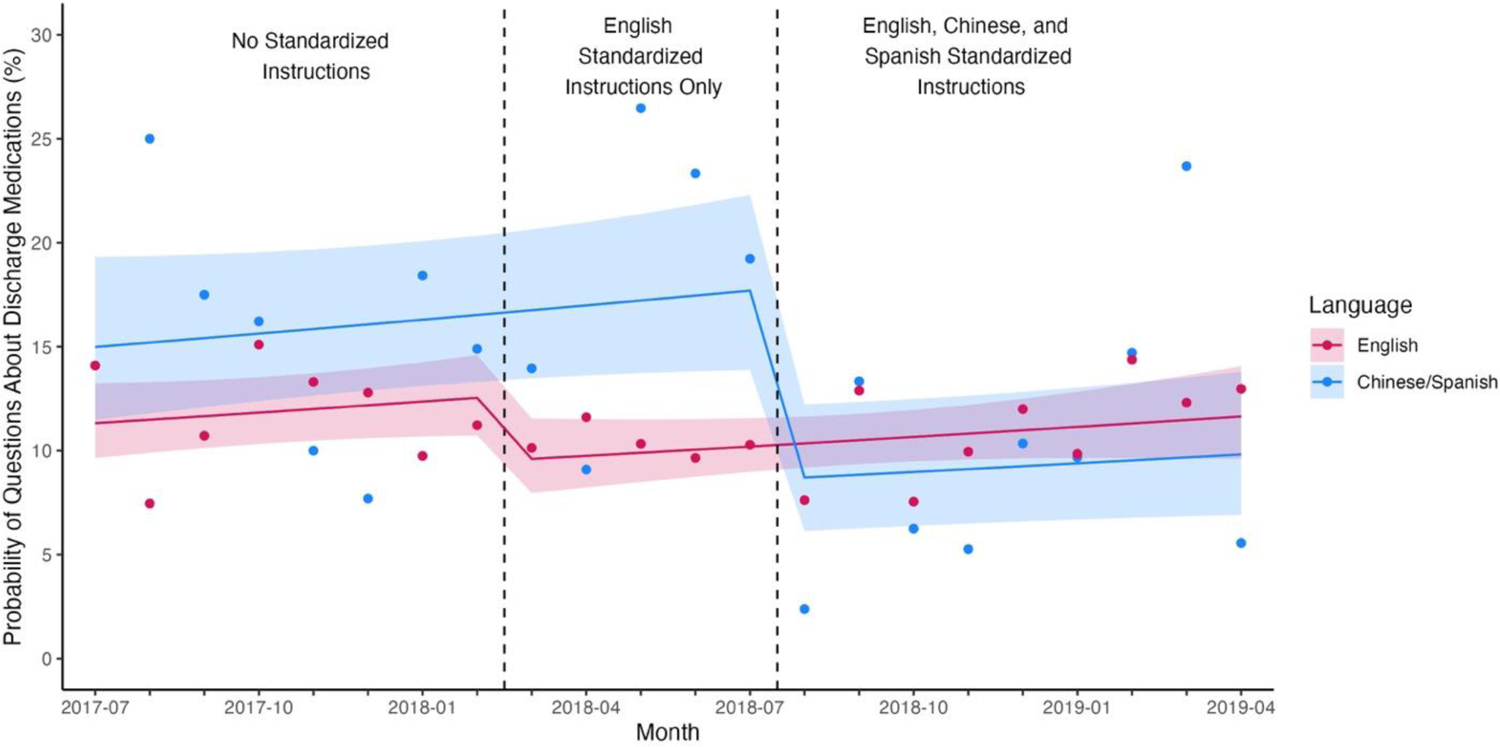
After the intervention, the probability of having medication questions after discharge decreased 2.9 percentage points for English-preferring patients (aOR=0.73, 95% CI 0.52, 1.02) and 8.9 percentage points for patients with NELP (aOR=0.44, 95% CI 0.26, 0.72). Again, this decrease was primarily driven by a 10.9 percentage points for Chinese-preferring patients (aOR=0.38, 95% CI 0.21, 0.69) though there was a non-significant 5.6 percentage point decrease for Spanish-preferring patients (aOR=0.58, 95% CI 0.26, 1.29). This closed the disparity in rates of post-discharge medication between patients with Chinese versus English preference (Figure 1).
Figure 1.
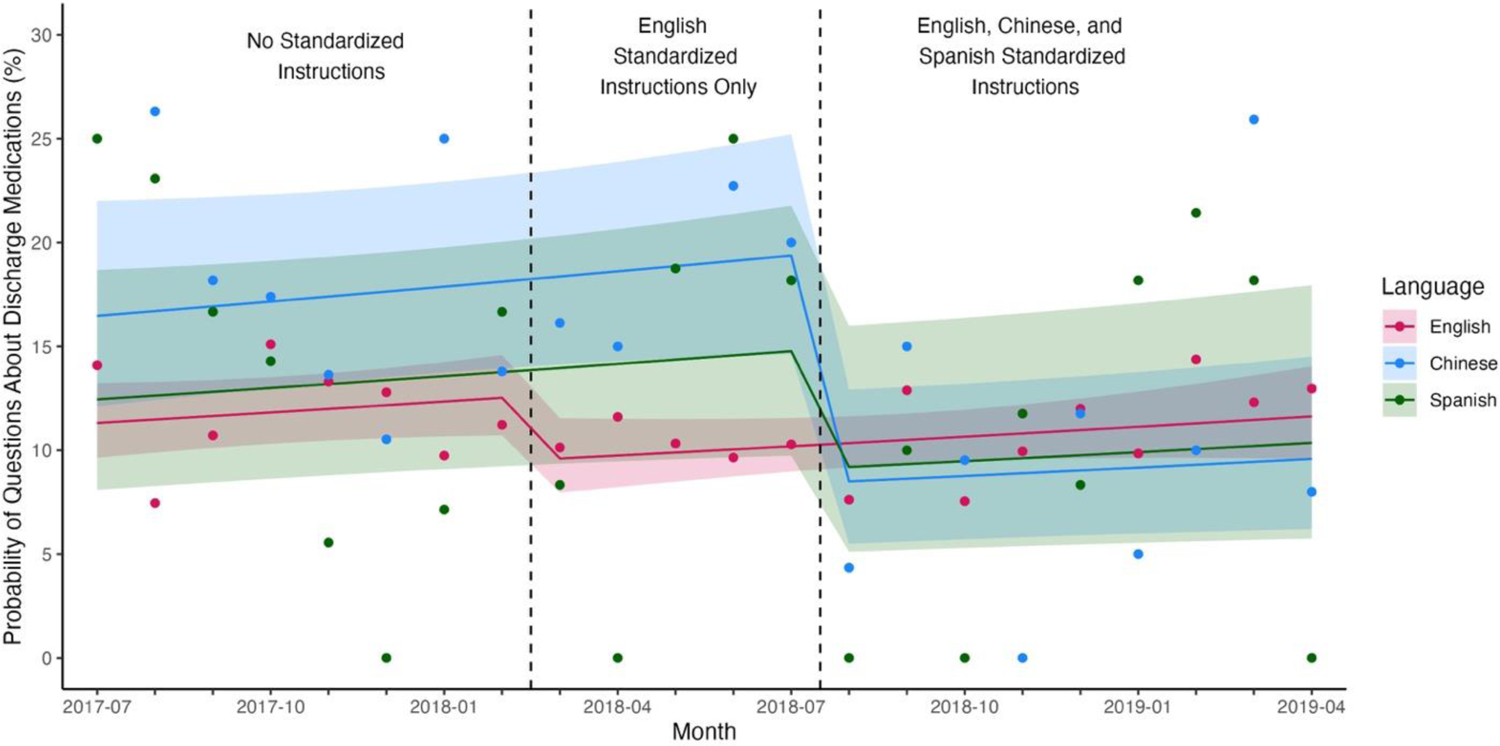
Probability of questions about discharge medications before and after implementation of standardized instructions.
Since race/ethnicity and sex were not associated with our intervention, we did not include them in our model; sensitivity analysis including race/ethnicity and sex did not change our results.
DISCUSSION
Consistent with our prior study,11 at baseline, patients with NELP had more post-discharge medication-related questions, though these differences were only significant between Chinese and English-speakers. After implementing our standardized written discharge instructions in English, Spanish, and Chinese, which were used in ~75–80% discharges, the probability of post-discharge medication questions for patients with a Chinese language preference decreased, thereby closing the disparity in rates of questions between patients with a Chinese versus English preference.
While it is not inherently better to have fewer medication-related questions post-discharge, we believe that closing the disparity in rates of these question for patients with NELP is desirable. In our prior work, we found that patients with NELP had higher rates of post-discharge questions but similar rates of high severity/urgency post-discharge issues that required escalation to staff beyond the care transition nurse.11 This suggests that some of these additional questions could be resolved with better counseling or communication from a nurse or member of the clinical team with similar training. Better counseling may be facilitated by both written instructions and increased use of language access services, such as interpreters, which are often underutilized.13
Our prior study of all patients admitted to the hospital did not find differences between Spanish and Chinese-preferring patients; specifically, both populations had higher rates of questions than English-preferring patients. However, in this study, limited to our hospital medicine patients, we found only baseline disparities between Chinese-preferring and English-preferring patients. We are uncertain of the reason for this discrepancy but hypothesize that our hospital medicine patients are different from the overall hospital population. Our population is older, and the language distribution is different; whereas the sample included in this study had two times as many Chinese-speakers as Spanish-speakers, Spanish was the most common non-English language in the entire hospital population.
Our study is limited as a single site study in an urban medical center only within the medicine service. We do not have information about what types of medication-related questions decreased after the intervention, which would provide insights on questions mitigated by the language concordant written instructions.
Further studies are needed to understand if closing disparities in rates of questions about post-discharge medications impacts disparities in other patient-reported or clinical outcomes for patients with NELP. Language concordant, standardized written discharge instructions may address communication barriers for patients with NELP and thereby mitigate disparities in post-discharge medication questions between patients who prefer English and patients with NELP.
ACKNOWLEDGEMENTS
Funders:
Dr. Khoong was supported for this work by National Institute for Health’s National Research Service Award (grant number T32HP19025), National Center for Advancing Translational Sciences of the NIH under Award Number KL2TR001870, and National Heart Lung and Blood Institute of the NIH under Award Number K23HL157750. The content is solely the responsibility of the authors and do not necessarily represent the official views of the NIH
Dr. Harrison is supported by the National Institute Of Aging of the National Institutes of Health under Award Number K01AG073533 and the National Center for Advancing Translational Sciences of the NIH under Award Number KL2TR001870. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix 1: Standardized discharge instructions (intervention)
Dear .NAME,
You were admitted for .PRIMARYDIAGNOSIS. In the hospital, we *** (tests and interventions provided)
Key information for you to know:
MEDICATION CHANGES (for dosing see complete medication list below):
- Please STOP taking ***
- Please START taking ***
- The following medications have CHANGES IN DOSE ***
FOLLOW-UP INSTRUCTIONS:
- After you leave the hospital, you need to get the labs and imaging studies listed in the summary because ***:
- Follow-up appointments with your outpatient providers are listed below.
RETURN INSTRUCTIONS:
- Please contact a healthcare provider or return to the emergency room for: ***
- If you have questions, please contact your primary care provider or hospital team (phone numbers above).
It was a pleasure taking care of you.
Sincerely,
Dr. *** - Intern
Dr. *** - Resident
Dr. .ATTENDINGPROVIDER - Attending
Dear .NAME, / Estimado(a) .NAME,
You were admitted for .PRIMARYDIAGNOSIS. / Fue ingresado(a) por .PRIMARYDIAGNOSIS.
In the hospital, we … / En el hospital, realizamos *** (tests and interventions provided / pruebas e intervenciones realizadas)
Key information for you to know: / Información clave para usted:
MEDICATION CHANGES (for dosing see complete medication list below) /
CAMBIOS A SU MEDICACIÓN (para la dosificación vea la lista completa de medicamentos a continuación):
- Please STOP taking / Por favor DEJE de tomar ***
- Please START taking / Por favor COMIENCE a tomar ***
- The following medications have CHANGES IN DOSE / Los siguientes medicamentos tienen CAMBIOS EN LA DOSIS ***
FOLLOW-UP INSTRUCTIONS / INSTRUCCIONES DE SEGUIMIENTO:
- After you leave the hospital, you need to get the labs and imaging studies listed in the summary because / Después de salir del hospital, debe hacerse las pruebas y los estudios de radiología enumerados en el resumen porque ***
- Follow-up appointments with your outpatient providers are listed below. / Sus citas de seguimiento con los proveedores ambulatorios se enumeran a continuación.
RETURN INSTRUCTIONS / INSTRUCCIONES PARA REGRESAR:
- Please contact a healthcare provider or return to the emergency room for / Por favor comuníquese con un proveedor médico o regrese a la sala de emergencias si experimente: ***
- If you have questions, please contact your primary care provider or hospital team (phone numbers above). / Si tuviera alguna pregunta, comuníquese con su proveedor primario o su equipo del hospital (a los números telefónicos enumerados arriba)
It was a pleasure taking care of you. / Fue un placer cuidarle.
Sincerely / Sinceramente,
Dr(a). *** - Intern / Interno
Dr(a). *** - Resident / Médico residente
Dr(a). .ATTENDINGPROVIDER – Attending physician / Médico supervisor
Dear .NAME, / 亲爱的 .NAME:
You were admitted for .PRIMARYDIAGNOSIS. / 您被送入医院治疗 .PRIMARYDIAGNOSIS。
In the hospital, we … / 在医院里, 我们 ***(tests and interventions provided / 提供的测试和干预措施)。
Key information for you to know: / 重要信息供您了解:
MEDICATION CHANGES (for dosing see complete medication list below): / 药物变更(关于剂量见下面的完整药物清单):
- Please STOP taking / 停止服用 ***
- Please START taking / 开始服用 ***
- The following medications have CHANGES IN DOSE / 以下药物有剂量变化: ***
FOLLOW-UP INSTRUCTIONS: / 跟进说明:
- After you leave the hospital, you need to get the labs and imaging studies listed in the summary because / 在您离开医院后, 您需要获得摘要中列出的实验室和影像学研究, 因为***
- Follow-up appointments with your outpatient providers are listed below. / 以下是您的门诊医生跟进预约。
RETURN INSTRUCTIONS: / 返回指示:
- Please contact a healthcare provider or return to the emergency room for… / 如果您有***, 请联系医务人员或返回急诊室。
- If you have questions, please contact your primary care provider or hospital team (phone numbers above). / 如果您有任何疑问, 请联系您的家庭医生或医院医生(电话号码在上文)。
It was a pleasure taking care of you. / 很高兴照顾您。
Sincerely, / 此致,
Dr. *** 医生 – Intern / 实习医生
Dr. *** 医生 – Resident / 住院医生
.ATTENDINGPROVIDER 医生 - Attending physician / 主治医生
Appendix 2: Figure A1. Probability of questions about discharge medications before and after implementation of standardized instructions (NELP patients aggregated)
Appendix 3: Table A1 - Odds Ratio from Multivariable Model (NELP patients aggregated)
| Odds Ratio | 95% CI | |
|---|---|---|
| Intercept | 0.0706 | 0.0499, 0.100 |
| Month | 1.017 | 0.991, 1.04 |
| Before Standardized Instructions | Ref | Ref |
| After Standardized Instructions | 0.729 | 0.521, 1.02 |
| English Language | Ref | Ref |
| Chinese or Spanish Language | 1.380 | 1.01, 1.88 |
| After Standardized Instructions*Chinese or Spanish Language | 0.598 | 0.372, 0.970 |
| Age | 1.01 | 1.00, 1.01 |
| Length of Stay | 1.03 | 1.01, 1.04 |
Appendix 4: Table A2 - Odds Ratio from Final Multivariable Model (Chinese-preferring and Spanish-preferring patients disaggregated)
| Odds Ratio | 95% CI | |
|---|---|---|
| Intercept | 0.0722 | 0.0507, 0.1 |
| Month | 1.017 | 0.991, 1.04 |
| Before Standardized Instructions | Ref | Ref |
| After Standardized Instructions | 0.730 | 0.521, 1.02 |
| English Language | Ref | Ref |
| Chinese Language | 1.55 | 1.08, 2.21 |
| Spanish Language | 1.115 | 0.689, 1.80 |
| After Standardized Instructions*Chinese Language | 0.380 | 0.211, 0.69 |
| After Standardized Instructions*Spanish Language | 0.575 | 0.256, 1.29 |
| Age | 1.01 | 1.00, 1.01 |
| Length of Stay | 1.03 | 1.01, 1.04 |
Footnotes
Disclosures
Dr. Khanna receives licensing income from Voalte, Inc. (now owned by Baxter) for the development of CareWeb, a communication tool unrelated to the current study.
Prior presentation:
Preliminary results were presented at the national Society of General Internal Medicine Annual Meeting in 2020.
REFERENCES
- 1.Alqenae FA, Steinke D, Keers RN. Prevalence and Nature of Medication Errors and Medication-Related Harm Following Discharge from Hospital to Community Settings: A Systematic Review. Drug Saf. 2020;43(6):517–537. doi: 10.1007/s40264-020-00918-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albrecht JS, Gruber-Baldini AL, Hirshon JM, et al. Hospital Discharge Instructions: Comprehension and Compliance Among Older Adults. J Gen Intern Med. 2014;29(11):1491–1498. doi: 10.1007/s11606-014-2956-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karliner LS, Auerbach A, Nápoles A, Schillinger D, Nickleach D, Pérez-Stable EJ. Language Barriers and Understanding of Hospital Discharge Instructions. Med Care. 2012;50(4):283–289. doi: 10.1097/MLR.0b013e318249c949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson A, Sandford J, Tyndall J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Johnson A, ed. Cochrane Database Syst Rev. 2003;(4)(4):CD003716. doi: 10.1002/14651858.CD003716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Society of Hospital Medicine: Project BOOST (Better Outcomes by Optimizing Safe Transitions). Advancing Successful Care Transitions to Improve Outcomes. https://www.hospitalmedicine.org/clinical-topics/care-transitions/. Published 2023.
- 6.Roundtable on Health Literacy; Institute of Medicine. Approaches to Developing Improved Discharge Instructions. In: Alper Joe and Hernandez Lyla M., ed. Facilitating Patient Understanding of Discharge Instructions: Workshop Summary. Washington (DC): National Academies Press (US); 2014. https://www.ncbi.nlm.nih.gov/books/NBK268650/. [PubMed] [Google Scholar]
- 7.Rodriguez VA, Boggs EF, Verre MC, et al. Hospital Discharge Instructions: Characteristics, Accessibility, and National Guideline Adherence. Hosp Pediatr. 2022;12(11):959–970. doi: 10.1542/hpeds.2021-006493 [DOI] [PubMed] [Google Scholar]
- 8.Diamond L, Wilson-Stronks A, Jacobs E. Do Hospitals Measure up to the National Culturally and Linguistically Appropriate Services Standards? Med Care. 2010. doi: 10.1097/MLR.0b013e3181f380bc [DOI] [PubMed] [Google Scholar]
- 9.Choe AY, Thomson JE, Unaka NI, et al. Disparity in Nurse Discharge Communication for Hospitalized Families Based on English Proficiency. Hosp Pediatr. 2021;11(3):245–253. doi: 10.1542/hpeds.2020-000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison JD, Sudore RL, Auerbach AD, et al. Automated telephone follow-up programs after hospital discharge: Do older adults engage with these programs? J Am Geriatr Soc. 2022;70(10):2980–2987. doi: 10.1111/jgs.17939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malevanchik L, Wheeler M, Gagliardi K, Karliner L, Shah SJ. Disparities After Discharge: The Association of Limited English Proficiency and Postdischarge Patient-Reported Issues. Jt Comm J Qual Patient Saf. 2021;47(12):775–782. doi: 10.1016/j.jcjq.2021.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The R Foundation. The R Project for Statistical Computing. https://www.r-project.org/. Published 2022. Accessed February 13, 2023.
- 13.Schenker Y, Pérez-Stable EJ, Nickleach D, Karliner LS. Patterns of Interpreter Use for Hospitalized Patients with Limited English Proficiency. J Gen Intern Med. 2011;26(7):712–717. doi: 10.1007/s11606-010-1619-z [DOI] [PMC free article] [PubMed] [Google Scholar]


