Despite decades of research and programmatic focus, anaemia is a persistent global health problem and can have negative health implications across the lifecycle, including impaired child development and work productivity and increased risk of adverse birth outcomes, morbidity and mortality.1,2
In The Lancet Haematology, the GBD 2021 Anaemia Collaborators use 2021 data from the Global Burden of Disease, Injuries and Risk Factors Study (GBD 2021) to report that nearly one in four individuals worldwide have anaemia, with notable differences by age, sex, and geography.3 The most common estimated causes of anaemia were dietary iron deficiency, haemo-globinopathies and haemolytic anaemias, and other neglected tropical diseases; iron deficiency alone contributed up to 66% of the total anaemia burden. These findings highlight the crucial role of nutrition in reducing anaemia. Although iron deficiency has long been considered a leading cause of anaemia, estimates vary widely across reports and settings. GBD 2021 presents the most comprehensive and current analysis of anaemia burden and causes globally; however, some researchers have questioned how micronutrient deficiencies, including iron deficiency, are estimated in the GBD analyses.4 Rather than estimating iron deficiency using valid inflammation-adjusted micronutrient biomarker data from representative surveys, GBD 2021 used complex statistical modelling.3 In brief, spatiotemporal Gaussian process regression models were used to estimate the prevalence of anaemia and predictive covariates were modelled using separate mixed-effects linear regression to create an ensemble model. Iron deficiency was modelled as a residual cause, which assumes that the causal attribution not explained by other causes of anaemia was due to iron deficiency. The comparability of the GBD modelling approach to a biomarker approach for estimating iron deficiency is unclear.
To examine this research gap, we compared nutrition surveys from 28 countries from the Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project, including 29 surveys for preschool-age children (6 months–5 years; n=37 688) and 23 surveys for women of reproductive age (15–49 years; n=52 555), with the estimates for the same 28 countries in GBD 2021 (data from population surveys that measured haemoglobin concentrations).3 The BRINDA research group has previously reported on the causes of anaemia in preschool-age children and women of reproductive age.5,6 An updated analysis was conducted using a subset of data from BRINDA to match datasets included in GBD 2021. The prevalence of iron-deficiency anaemia (defined as the presence of both anaemia and iron deficiency) and the percentage of anaemia associated with iron deficiency (defined as [iron-deficiency anaemia]/[anaemia]) were estimated for each country using inflammation-adjusted ferritin concentrations and applying WHO ferritin cutoffs,7 and overall median values across approaches were compared. The proportions of anaemia associated with iron deficiency were higher in GBD models (median 71% for preschool-age children and 69% for women of reproductive age) than in nutrition surveys (median 42% for preschool-age children and 45% for women of reproductive age). GBD 2021 estimates were consistently higher than nutrition surveys for the prevalence of anaemia (8 percentage points higher for preschool-age children and 12 percentage points higher for women of reproductive age), iron-deficiency anaemia (15 and 16 percentage points higher), and anaemia associated with iron deficiency (29 and 25 percentage points higher; figure).
Figure: Prevalence of anaemia and iron-deficiency anaemia and percentage of anaemia associated with iron deficiency using nutrition surveys and GBD 2021 estimates.
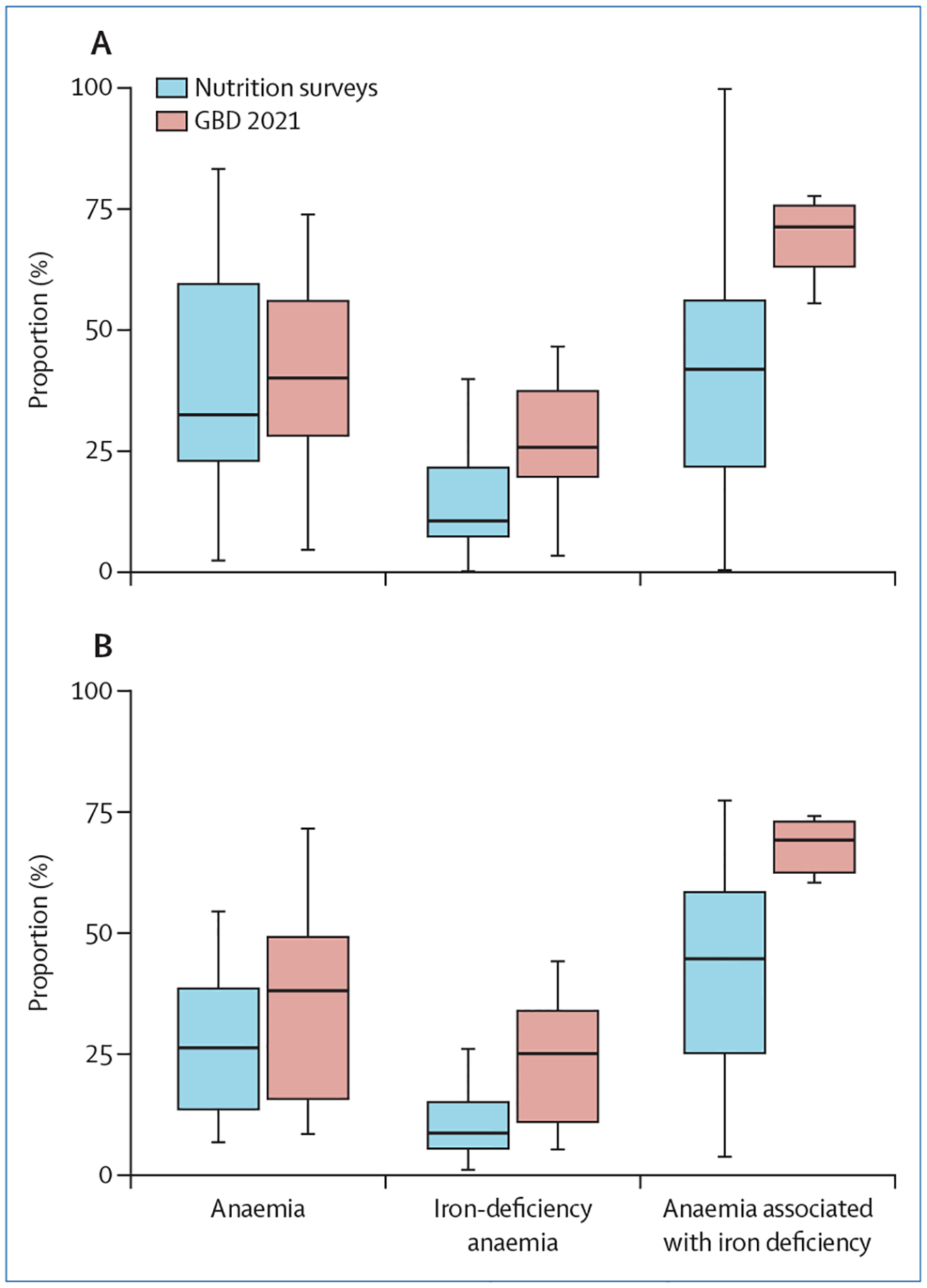
Data for preschool-age children (A) and women of reproductive age (B). Anaemia (adjusted for altitude and smoking) is defined as haemoglobin concentrations less than 120 g/L for non-pregnant women in nutrition surveys and GBD 2021 and less than 110 g/L for pregnant women in GBD 2021 estimates. Iron-deficiency anaemia is defined as anaemia with inflammation-adjusted serum ferritin concentrations of less than 12 μg/L for preschool-age children and less than 15 μg/L for non-pregnant women of reproductive age for nutrition surveys and as a modelled residual cause for GBD 2021 estimates. GBD=Global Burden of Disease, Injuries and Risk Factors Study.
Iron deficiency was an important cause of anaemia using both approaches; however, closer examination of the key challenges for accurately characterising iron-deficiency anaemia—including physiological state, biomarker cutoffs, and data availability and interpretation of the causes of anaemia—are merited. The GBD 2021 estimates for women of reproductive age include both pregnant and non-pregnant women, whereas the nutrition surveys included only non-pregnant women. The high iron demands during pregnancy, to support plasma volume expansion and placental and fetal growth and development, could contribute to a higher proportion of iron-deficiency anaemia in pregnant than in non-pregnant women. In future GBD analyses, separate reports for pregnant women would help to guide population-specific and context-specific anaemia reduction strategies. Another consideration is the use of cutoffs for defining anaemia and iron deficiency that are physiologically validated and are not just statistical thresholds.8,9 Using binary cutoffs for anaemia or iron deficiency could hinder understanding of the physiological effects of these conditions on cognitive development, immunity, and other health outcomes. Finally, anaemia aetiology is complex and multifactorial, and there are data gaps on leading causes of anaemia as well as inherent challenges in accurately quantifying the contribution of causes of anaemia in populations.10 In the GBD study, iron deficiency was calculated as a proxy residual estimate, the accuracy of which depends on several model assumptions, including that each anaemia case is caused by one factor and that all other anaemia determinants are accurately estimated. However, multiple causes of anaemia can coexist and are driven by underlying and interconnected pathophysiological, social, economic, political, and geographic factors.1 Assuming only one cause of anaemia with either approach could lead to inaccurate estimation of other contributing factors and limit the clinical utility and actionability of the findings. The effort of GBD 2021 to quantify the global burden and causes of anaemia is an important step forward; however, the lack of population-level micronutrient and pregnancy-specific data is concerning and such data are urgently needed to improve the global characterisation of iron deficiency and iron-deficiency anaemia. This report of the GBD 2021 data is a call to action to improve the collection and use of data to enable a systematic approach to assess the causes of anaemia in populations (including all relevant nutritional and non-nutritional causes) to inform evidenced-based strategies that address the persistent global anaemia burden.
Acknowledgments
We declare no competing interests. This work was supported by the Bill & Melinda Gates Foundation (INV-010744), Centers for Disease Control and Prevention, Eunice Kennedy Shriver National Institute of Child Health and Human Development, HarvestPlus, and the United States Agency for International Development. The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann NY Acad Sci 2019; 1450: 15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young MF, Oaks BM, Rogers HP, et al. Maternal low and high hemoglobin concentrations and associations with adverse maternal and infant health outcomes: an updated global systematic review and meta-analysis. BMC Pregnancy Childbirth 2023; 23: 264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2021 Anaemia Collaborators. Prevalence, years lived with disability, and trends in anaemia burden by severity and cause, 1990–2021: findings from the Global Burden of Disease Study 2021. Lancet Haematol 2023; published online July 31. 10.1016/S2352-3026(23)00160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hess SY, McLain AC, Frongillo EA, et al. Challenges for estimating the global prevalence of micronutrient deficiencies and related disease burden: a case study of the Global Burden of Disease Study. Curr Dev Nutr 2021; 5: nzab141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wirth JP, Woodruff BA, Engle-Stone R, et al. Predictors of anemia in women of reproductive age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr 2017; 106 (suppl 1): 416S–27S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engle-Stone R, Aaron GJ, Huang J, et al. Predictors of anemia in preschool children: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr 2017; 106 (suppl 1): 402S–15S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Geneva: World Health Organization, 2020. [PubMed] [Google Scholar]
- 8.Mei Z, Addo OY, Jefferds ME, Sharma AJ, Flores-Ayala RC, Brittenham GM. Physiologically based serum ferritin thresholds for iron deficiency in children and non-pregnant women: a US National Health and Nutrition Examination Surveys (NHANES) serial cross-sectional study. Lancet Haematol 2021; 8: e572–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Addo OY, Yu EX, Williams AM, et al. Evaluation of hemoglobin cutoff levels to define anemia among healthy individuals. JAMA Netw Open 2021; 4: e2119123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ko YA, Williams AM, Peerson JM, et al. Approaches to quantify the contribution of multiple anemia risk factors in children and women from cross-sectional national surveys. PLoS Glob Public Health 2022; 2: e0001071. [DOI] [PMC free article] [PubMed] [Google Scholar]


