Abstract
Transdiagnostic treatments have been designed to target common processes for clusters of disorders. One such treatment, transdiagnostic behavior therapy (TBT), targets avoidance across emotional disorders, including posttraumatic stress disorder (PTSD), depressive disorders, and anxiety disorders, and has demonstrated efficacy in randomized controlled trials. The current study was designed to examine whether distinct treatment trajectories would emerge in a sample of 112 veterans receiving TBT and whether diagnostic comorbidity, baseline levels of several transdiagnostic risk factors, or treatment engagement influence trajectory membership. Growth mixture modeling revealed three distinct trajectories across depression, ds = 0.55–1.09; PTSD ds = −0.07–1.43; and panic disorder symptoms, ds = −0.13–1.09. Notably, for PTSD and panic disorder symptoms, separate classes for responders and nonresponders emerged among participants with high baseline symptom levels. Findings for the risk factors suggested that PTSD and panic nonresponders evidenced significantly higher behavioral avoidance at baseline and reduced engagement in treatment procedures and homework completion compared to responders. Together, the findings provide additional support for the use of TBT in the treatment of emotional disorders, including PTSD. Potential adaptations are discussed for patients with significantly elevated behavioral avoidance to improve treatment engagement and related outcomes.
Emotional disorders, including depressive, traumatic stress–related, and anxiety disorders, are among the most common psychiatric diagnoses (Kessler et al., 2012). Major depressive disorder (MDD) and posttraumatic stress disorder (PTSD) are elevated in U.S. military veterans compared to civilians (Blore et al., 2015; Schein et al., 2021), and comorbidity amongst these disorders is the rule rather than the exception (Ginzburg et al., 2010; Kessler et al., 2005). These disorders are associated with severe occupational, educational, and social impairment as well as an elevated risk for cardiovascular disease, suicide, and substance use (Adler et al., 2011; Hoge et al., 2007; Hoglund & Schwartz, 2014).
Despite their prevalence, access to evidence-based psychotherapies (EBPs) remains scant (Maguen et al., 2020; Mott et al., 2014). Several limitations of EBPs have been hypothesized as contributors to these challenges. Namely, with the focus on disorder-specific EBPs, providers must learn myriad protocols to provide services for various emotional disorders, resulting in significant training and financial burdens to providers (Gros et al., 2016). For example, per the Department of Veterans Affairs’ (VA) well-established training model, training for a single disorder-specific protocol involves a multiday intensive workshop and 6 months of postworkshop consultation (Ruzek et al., 2012). Learning sufficient treatments to address all emotional disorders could take many years to complete and discourage continued participation in training (Gros et al., 2016). In addition, disorder-specific EBPs largely rely on secondary effects for comorbid diagnoses and necessitate the administration of a second disorder-specific EBP if secondary symptoms persist, increasing the resources necessary for the adequate treatment of comorbid presentations (Gros et al., 2023; Kline et al., 2021).
In response to concerns for disorder-specific EBPs, transdiagnostic psychotherapies have been developed for emotional disorders (Barlow et al., 2004; Gros et al., 2016). These treatments target underlying symptoms via common treatment components found across EBPs to address a cluster of diagnoses. If effective, transdiagnostic treatments may provide improved coverage of presenting comorbid conditions (Coyne & Gros, 2022), improved perceptions of fit by patients (Shapiro & Gros, 2021), and improved perceptions of fit by providers (Gros et al., 2017). Although the transdiagnostic treatment findings are still in the early phases, there is much promise for their treatment of emotional disorders (Norton & Paulus, 2016).
Given these hypothesized strengths of transdiagnostic treatments, more research is needed to identify for whom treatment is working and what factors contribute to its success. To investigate these questions, growth mixture modeling (GMM) can be used to place individuals into classes based on their treatment response trajectories over time and provide an opportunity to examine the heterogeneity of treatment response (Jung & Wickrama, 2008). Similar investigations have been completed in disorder-specific therapies for PTSD (Allan et al., 2017), MDD (Cuijpers et al., 2005), and panic disorder (Santa-cana et al., 2016) separately but not for a transdiagnostic psychotherapy nor within a diagnostically diverse sample.
GMM also allows for the investigation of predictors of treatment response trajectory classes (Allan et al., 2017). Given the limited study of predictors to date (Sauer-Zavala et al., 2012), for this study, initial predictors were selected from the transdiagnostic treatment literature and related literatures for emotional disorders. Diagnostic comorbidity and treatment participation were selected given their significance in the rationale for transdiagnostic treatments and the initial findings on their relevance (Coyne & Gros, 2022; Shapiro & Gros, 2022). Additional predictors were selected to represent three subsystems commonly identified in componential emotion theories: physical sensations, cognitive appraisals, and behaviors (Moors et al., 2013; Zeelenberg et al., 2008). More specifically, anxiety sensitivity was selected due to its relation to physical sensations as well as its consistent importance in the development and treatment of emotional disorders (Naragon-Gainey, 2010; Taylor et al., 2007). Perseverative thinking was selected to represent cognitive appraisals; similar significance has been demonstrated for perseverative thinking across emotional disorders (Ehring et al., 2011; Sorg et al., 2012). Finally, behavioral avoidance was selected given its significance across emotional disorders (Gros, 2014) and because it serves as a primary target for the transdiagnostic psychotherapy investigated in the present study, transdiagnostic behavior therapy (TBT; Gros, 2014; Gros et al., 2020). Although there are numerous candidates to serve as additional predictors (Dewar et al., 2020), we sought to focus the scope of the present study on these predictors as an initial evaluation of transdiagnostic treatment trajectories and their associated predictors and to inform future study.
The present study investigated risk factors in veterans receiving TBT as part of an ongoing clinical trial comparing TBT to disorder-specific psychotherapies (NCT04293341). More specifically, GMM was used to investigate treatment trajectories in veterans receiving TBT, with diagnostic comorbidity, treatment participation, anxiety sensitivity, perseverative thinking, and behavioral avoidance examined across the derived latent classes as potential predictors of outcomes. Based on prior studies (Allan et al., 2017; Owen et al., 2015), we expected at least two trajectories to emerge: treatment responders, reflecting moderate-to-large reductions in symptoms of depression, PTSD, and panic disorder, and treatment nonresponders, reflecting trivial reductions in symptoms. We further expected that participants would demonstrate consistent patterns of response across symptoms. Finally, based on the design of TBT (Gros, 2014) and initial findings related to the treatment (Coyne & Gros, 2022; Gros et al., 2020; Shapiro & Gros, 2022), behavioral avoidance, treatment participation, and diagnostic comorbidity were hypothesized as the strongest predictors of latent class membership.
METHOD
Participants
The present data were collected as part of a randomized clinical trial investigating TBT (NCT04293341). Participants (N = 112) had primary diagnoses of MDD (n = 43, 38.4%), panic disorder (n = 30, 26.8%), or PTSD (n = 39, 34.8%) and were recruited at a VA Health Care System (VAHCS). Study inclusion criteria were competence to complete study consent and procedures; meeting the diagnostic criteria for a principal diagnosis of panic disorder, PTSD, or MDD, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) and assessed using the Anxiety Disorders Interview Schedule (ADIS-5; Brown, 2014); and being between 18 and 80 years of age. Study exclusion criteria were a recent history (i.e., within 2 months or less) of a psychiatric hospitalization or suicide attempt; severe illness or medical condition that would interfere with study procedures; the recent start of new psychiatric medication (i.e., within 4 weeks or less); or the diagnosis of a psychotic disorder, personality disorder, or bipolar disorder based on medical chart review. The mean participant age at baseline was 47.3 years (SD = 15.0), 68.8% of participants were male, 57.1% were White, and 37.5% were Black. Comorbidity was common in the sample, with 82.1% of the sample meeting the diagnostic criteria for more than one mental health condition (range: 0–4 comorbid conditions). Military service branch was predominately Army (n = 43, 38.4%), and participants most commonly reported serving in support of operations in Iraq and Afghanistan following the September 11, 2002, terrorist attacks (n = 27, 24.1%).
Procedure
Study design and ethical approval
Participants were recruited from November 2020 to December 2022. All procedures were approved by the affiliated university institutional review board and VA Research and Development Committee. Interested patients were scheduled for an intake appointment to complete consent documents, evaluate the study criteria, and complete diagnostic and self-report measures. As part of the larger study, eligible participants were randomly assigned (i.e., 1:1) to receive either TBT or disorder-specific psychotherapy. Randomization was stratified by three principal diagnostic groups (i.e., panic disorder, PTSD, or MDD). Only participants randomized into the TBT treatment condition were included in the present study. Upon randomization, participants were assigned to a project therapist to complete 12 weekly sessions of psychotherapy, delivered either in person or via telehealth. Participants completed symptom measures biweekly throughout the course of TBT, with larger assessment batteries at midtreatment and posttreatment.
TBT
TBT was designed to address overall psychiatric well-being and rehabilitation in patients via reengagement in significant activities, relationships, and community involvement, which are typically avoided due to psychiatric symptoms (Gros, 2014; Gros & Allan, 2019). The unifying symptom targeted by TBT is avoidance (Gros, 2014; Gros et al., 2023). The primary focus of TBT is to educate on, prepare for, and challenge four different types of avoidance associated with negative and positive emotions (i.e., situational, physical, thought, and positive emotional avoidance). Specialized exposure practices are used to reduce avoidance across types and lead to decreases in negative emotions and increases in positive emotions as well as improve overall well-being and social functioning (Gros, 2014). Optional modules can be incorporated into TBT to further improve the efficiency of the exposure practices.
Measures
Clinician-administered and therapist-report measures
Psychiatric diagnoses.
The ADIS-5 (Brown, 2014) is a semi-structured interview assessing a range of Axis I disorders (Brown, 2014). The ADIS-5 is used to assess current and past diagnoses per DSM-5 diagnostic criteria and severity scores. The measure has demonstrated excellent interrater reliability and validity of emotional disorder diagnoses, including in similar studies by this research group (Gros & Allan, 2019). The ADIS-5 was administered at baseline to determine primary diagnostic status and assess for comorbid diagnoses. The presence of any diagnostic comorbidity above the primary diagnosis was used as a binary predictor in the analyses.
Posttreatment review.
At posttreatment, the treating therapist completed the Post-Treatment Therapist Review (PTTR; Shapiro & Gros, 2011). The PTTR inquires about a variety of posttreatment outcomes, such as session completion, homework adherence, and engagement. The present study utilized Item 1 (i.e., “total sessions attended”), Item 8 (“participation in session procedures (e.g., providing examples, problem-solving, completing forms, in-session exposures – if applicable”), and Item 10 (“weekly average homework engagement”). Therapists were asked to rate Items 8 and 10 on a scale of 0 (none) to 6 (maximum).
Mental health disorder outcomes
Panic disorder.
The seven-item Panic Disorder Severity Scale (PDSS; Shear et al., 2001) was used to assess the frequency of and distress stemming from panic attacks and related symptoms. Items are scored on a 0–4 scale, with scores of 8 and higher indicating diagnosis-consistent panic symptoms. The scale has demonstrated good internal consistency, test–retest reliability, and sensitivity to change during the course of treatment (Shear et al., 2001). In the current sample, Cronbach’s alpha was .91 at baseline.
Depressive symptoms.
The nine-item Patient Health Questionnaire9 (PHQ-9; Kroenke et al., 2001) was used to assess depressive symptoms. Items are scored on a 0–3 scale, with scores of 10 or higher suggesting moderate-to-severe depressive symptoms. The PHQ-9 has been shown to have good reliability as well as validity in clinical samples (Kroenke et al., 2001). In the present sample, Cronbach’s alpha was .85 at baseline.
PTSD symptoms.
The PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) is a 20-item self-report measure assessing DSM-5 PTSD symptoms. Items are scored on a 0–4 scale, with scores of 31 and higher indicating diagnosis-consistent PTSD symptoms. The PCL has demonstrated excellent internal consistency and test–retest reliability (Bovin et al., 2016). In the present sample, Cronbach’s alpha was .93 at baseline.
Baseline transdiagnostic risk factors
Behaviors.
The Albany Panic and Phobia Questionnaire (APPQ; Rapee et al., 1994/1995) is a 27-item self-report measure composed of subscales measuring agoraphobia, social anxiety, and interoceptive avoidance. Items are scored on a scale of 0 to 8, with higher scores indicating more severe symptoms. Each subscale has evidenced good internal consistency and temporal stability (Rapee et al., 1994/1995). The Agoraphobia subscale was used to assess behavioral avoidance in the current study (Gros et al., 2020). In the present sample, Cronbach’s alpha was .85 at baseline.
Physical sensations.
The Anxiety Sensitivity Index 3 (ASI-3; Taylor et al., 2007) is an 18-item self-report measure of anxiety sensitivity (Taylor et al., 2007). Items are scored on a 1–5 scale, with higher scores indicating higher levels of severity. The measure has shown good psychometric properties (Taylor et al., 2007). The ASI-3 was utilized to assess participants’ level of overall anxiety sensitivity. In the present sample, Cronbach’s alpha was .92 at baseline.
Cognitive appraisals.
The Perseverative Thinking Questionnaire (PTQ; Ehring et al., 2011) is a 15-item measure of repetitive negative thinking. Items are scored on a 0–4 scale, with higher scores indicating higher levels of severity. The PTQ has demonstrated acceptable convergent validity, predictive validity, internal consistency, and test–retest reliability (Ehring et al. 2011). In the present sample, Cronbach’s alpha was .95 at baseline.
Data analysis
GMM was performed using Mplus (Version 8.3; Muthén & Muthén, 1998–2022) separately for PHQ-9, PCL-5, and PDSS scores from Session 1 to posttreatment. Data were centered at Session 1. Baseline data were used in cases where Session 1 data were missing. Model estimation began with 500 starting values optimized to avoid local maxima (Jung & Wickrama, 2008). Models were compared for increasing classes using latent class growth analysis (LCGA) and restricted GMM. LCGA restricts variance across intercept and slope parameters to zero, whereas restricted GMM allows for variance to be estimated, similarly across classes, for intercept, slope, or intercept and slope parameters. The Bayesian information criterion (BIC) was used as the primary statistical criterion for model selection given the robust support for this parameter (Nylund et al., 2007). BIC values that decreased by 10 or more were considered meaningful (Raftery, 1995). Additional statistical indices used for model selection were the Akaike information criterion (AIC), Lo–Mendell–Rubin likelihood ratio test (LMR-LRT), and the bootstrapped likelihood ratio test (BLRT). Lower AIC scores indicate better fit, and significant LMR-LRT or BLRT values support n over n – 1 classes. Entropy also was presented; values range from 0 to 1, with values closer to 1 suggesting better class separation. Effect sizes from baseline to postintervention were calculated for each class. Classes were named to capture initial effect size levels and treatment response. Predictors of class status were examined using a three-step procedure to account for unequal variance in variables across classes (Asparouhov & Muthén, 2014). Lanza’s method (Lanza et al., 2013) was used to evaluate class differences for binary variables.
RESULTS
Descriptive statistics and correlations
Table 1 contains baseline descriptive statistics and bivariate correlations. Problematic skew or kurtosis was not detected based on values from structural equation modeling (SEM) simulation studies (Curran et al., 1996). Treatment completion was defined as completing at least six sessions of TBT, based on the structure of the treatment (Gros, 2014). Of the 108 participants with recorded sessions, 79 (70.5%) completed treatment, and participants completed an average of 8.8 sessions (SD = 4.1). There were no significant differences between participants who dropped out and those who completed treatment for any variable.
TABLE 1.
Bivariate correlations and descriptive statistics for baseline symptoms and predictors
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. PHQ-9 | – | .69* | .17 | .35* | .42* | .43* | −.17 | −.21 | .27* |
| 2. PCL-5 | – | .38* | .51* | .53* | .58* | −.04 | −.01 | .28* | |
| 3. PDSS | – | .57* | .11 | .49* | −.20 | .02 | .28* | ||
| 4. ASI-3 | – | .39* | .54* | −.02 | −.01 | .25* | |||
| 5. PTQ | – | .31* | −.27* | .10 | .14 | ||||
| 6. APPQ-A | – | .01 | −.21 | .20 | |||||
| 7. Age | – | .12 | −.16 | ||||||
| 8. Sexa | – | −.06 | |||||||
| 9. Comorbidityb | – | ||||||||
| M | 17.99 | 49.27 | 13.09 | 56.74 | 38.96 | 25.83 | 47.32 | ||
| SD | 5.55 | 15.95 | 6.11 | 15.25 | 11.60 | 17.67 | 14.98 | ||
| % | 68.8 | 82.1 |
Note N: = 66–112 for means and correlations.
Dummy-coded as 1 = male.
Dummy-coded as 1 = the presence of any comorbid mental health condition.
p < .05.
GMM
Depression
PHQ-9 restricted GMM model fit information is presented in the top panel of Table 2; LCGA and restricted GMM model fit are presented in Supplementary Table S1. The five-class LCGA linear growth solution had the lowest AIC and BIC values; the maximum threshold in the GMMs was set as five classes. The three-class restricted GMM with slope variance freed had the lowest BIC value and significant LMR-LRT and BLRT values and was thus considered the best-fitting solution.
TABLE 2.
Fit indices for growth mixture models of depressive symptoms from Session 1 to postintervention
| Model | −2LL | Parameters | AIC | BIC | Entropy | LMR-LRT | BLRT |
|---|---|---|---|---|---|---|---|
| Restricted GMM (intercept variance estimated) | |||||||
| 1 class | −1,435.04 | 10 | 2,890.09 | 2,917.00 | |||
| 2 class | −1,404.35 | 13 | 2,834.70 | 2,869.69 | .53 | 57.31 | 61.38 |
| 3 class | −1,396.70 | 16 | 2,825.40 | 2,868.47 | .52 | 14.28 | 15.30 |
| 4 class | −1,394.04 | 19 | 2,824.17 | 2,875.31 | .55 | 6.75 | 7.23 |
| 5 class | −1,390.08 | 22 | 2,824.15 | 2,883.36 | .71 | 5.62 | 6.02 |
| Restricted GMM (slope variance estimated) | |||||||
| 1 class | −1,494.71 | 10 | 3,009.42 | 3,036.33 | |||
| 2 class | −1,426.43 | 13 | 2,878.85 | 2,913.84 | .87 | 127.50** | 136.56** |
| 3 class | −1,393.15 | 16 | 2,818.30 | 2,861.36 | .87 | 62.14 * | 66.56 * |
| 4 class | −1,389.52 | 19 | 2,817.03 | 2,868.17 | .75 | 6.79 | 7.27 |
| 5 class | −1,386.25 | 22 | 2,816.50 | 2,875.71 | .78 | 6.10 | 6.53 |
| Restricted GMM (intercept and slope variance estimated) | |||||||
| 1 class | −1,405.38 | 12 | 2,834.75 | 2,867.05 | |||
| 2 class | −1,398.59 | 15 | 2,827.18 | 2,867.55 | .53 | 12.67 | 13.57 |
| 3 class | −1,392.15 | 18 | 2,820.30 | 2,868.75 | .68 | 12.03 | 12.88 |
| 4 class | −1,386.45 | 21 | 2,814.90 | 2,871.42 | .76 | 10.64 | 11.40 |
| 5 class | |||||||
Note: Bolding indicates the best-fitting model. GMM = growth mixture modeling; LL = log-likelihood; AIC = Akaike information criterion; BIC = Bayesian information criterion; LMR-LRT = Lo–Mendell–Rubin likelihood ratio test; BLRT = bootstrapped likelihood ratio test.
p < .05.
p < .01.
Figure 1 contains mean estimated PHQ-9 trajectories for the three classes. Class 1, labeled high responders, contained 22 participants with a posterior probability (pp) of .94 and captured a medium effect size symptom reduction, d = 0.55. Class 2, labeled moderate responders, contained 64 participants, pp = .97, and captured a large effect size reduction, d = 1.09. Class 3, categorized as low responders, contained 23 participants, pp = .89, and captured a large effect size reduction, d = 0.78. An entropy value of .87 indicated an acceptable degree of class separation.
FIGURE 1.
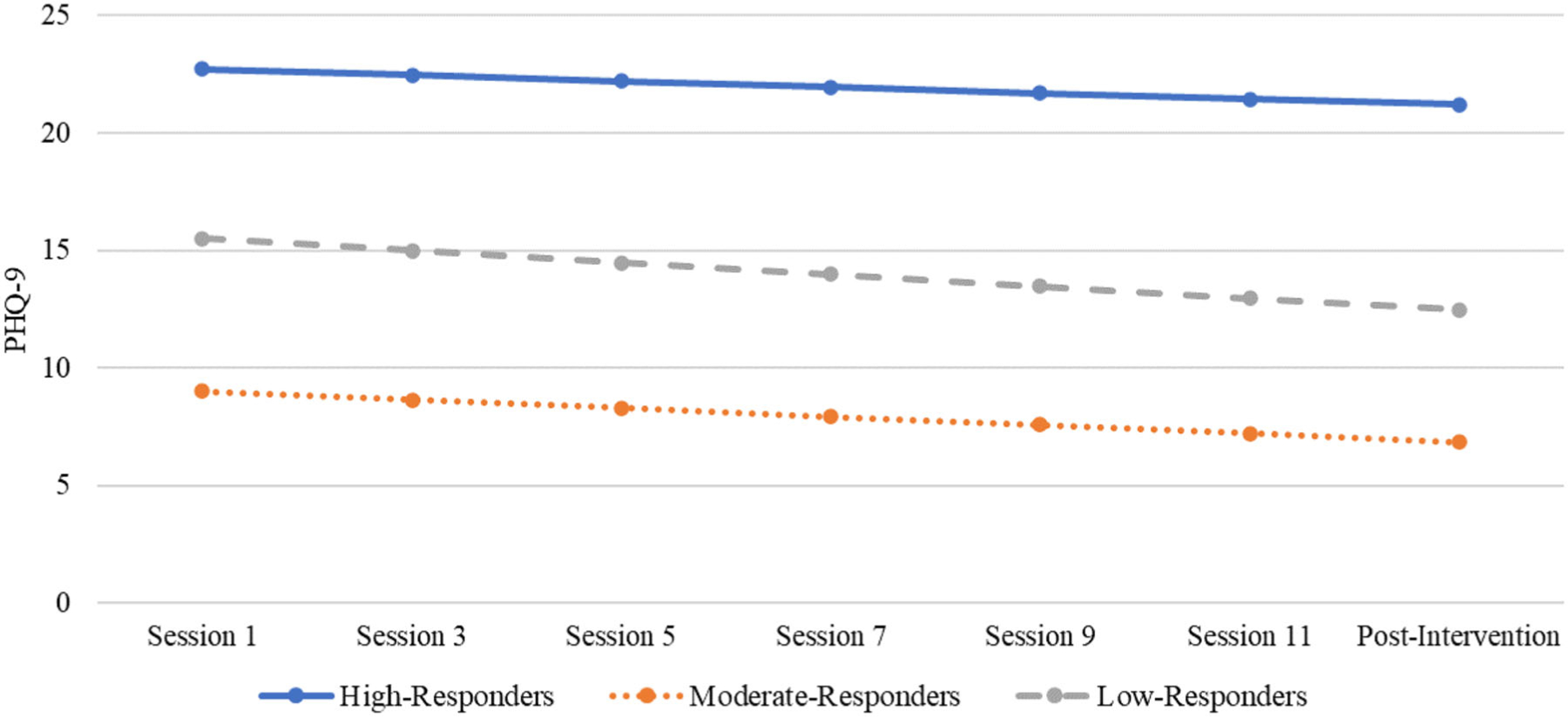
Estimated depressive symptom trajectories of high-responder (n = 22), moderate-responder (n = 64), and low-responder (n = 23) classes
Note: PHQ-9 = nine-item Patient Health Questionnaire.
PTSD
PCL-5 restricted GMM comparisons are presented in Table 3, and all model fit information is presented in Supplementary Table S2. Based on fit information, the six-class linear LCGA was considered the maximum class threshold to test in restricted GMM. The one- and two-class GMMs with intercept and slope variance estimated and the three-class GMM with intercept variance free had similar fit information. However, the BIC was not 10 points lower in the one- and two-class models compared to the three-class model, and the three-class intercept variance freed model was accepted as the best-fitting model.
TABLE 3.
Fit indices for growth mixture models of posttraumatic stress disorder from Session 1 to postintervention
| Model | −2LL | Parameters | AIC | BIC | Entropy | LMR-LRT | BLRT |
|---|---|---|---|---|---|---|---|
| Restricted GMM (intercept variance estimated) | |||||||
| 1 class | −1,774.45 | 10 | 3,568.90 | 3,595.44 | |||
| 2 class | −1,738.31 | 13 | 3,502.62 | 3,537.12 | .65 | 67.45** | 72.28** |
| 3 class | −1,726.21 | 16 | 3,484.42 | 3,526.88 | .58 | 22.59 | 24.21 |
| 4 class | −1,721.46 | 19 | 3,480.91 | 3,531.34 | .59 | 8.87 | 9.51 |
| 5 class | −1,716.95 | 22 | 3,477.90 | 3,536.28 | .71 | 8.41 | 9.01 |
| 6 class | −1,715.16 | 25 | 3,480.32 | 3,546.67 | .71 | 3.34 | 3.58 |
| Restricted GMM (slope variance estimated) | |||||||
| 1 class | −1,855.91 | 10 | 3,731.81 | 3,758.35 | |||
| 2 class | −1,782.50 | 13 | 3,591.00 | 3,625.50 | .78 | 137.00** | 146.81** |
| 3 class | −1,735.47 | 16 | 3,502.94 | 3,545.41 | .87 | 87.77** | 94.06** |
| 4 class | −1,724.87 | 19 | 3,487.74 | 3,538.16 | .87 | 19.78 | 21.20 |
| 5 class | −1,719.61 | 22 | 3,483.21 | 3,541.60 | .78 | 9.83 | 10.53 |
| 6 class | −1,717.00 | 25 | 3,484.01 | 3,550.36 | .75 | 4.86 | 5.20 |
| Restricted GMM (intercept and slope variance estimated) | |||||||
| 1 class | −1,734.29 | 12 | 3,492.59 | 3,524.44 | |||
| 2 class | −1,728.06 | 15 | 3,486.12 | 3,525.93 | .66 | 11.64 | 12.47 |
| 3 class | − 1,723.33 | 18 | 3,482.66 | 3,530.43 | .72 | 8.83 | 9.46 |
| 4 class | −1,716.53 | 21 | 3,475.06 | 3,530.79 | .75 | 12.69 | 13.60 |
| 5 class | −1,712.75 | 24 | 3,473.51 | 3,537.20 | .71 | 7.05 | 7.56 |
Note: Bolding indicates the best-fitting model. GMM = growth mixture modeling; LL = log-likelihood; AIC = Akaike information criterion; BIC = Bayesian information criterion; LMR-LRT = Lo–Mendell–Rubin likelihood ratio test; BLRT = bootstrapped likelihood ratio test.
p < .05.
p < .01.
Figure 2 contains the mean estimated PCL-5 trajectories for the three classes. Class 1, high nonresponders, contained 20 participants, pp = .66, and captured a flat to slightly increasing effect size, d = −0.07. Class 2, high responders, contained 14 participants, pp = .61, and captured a large effect size reduction, d = 1.43. Class 3, moderate responders, contained 71 participants, pp = .93, and captured a medium effect size reduction, d = 0.49. The entropy value was .58 for the overall model, indicating a modest amount of classification misfit.
FIGURE 2.
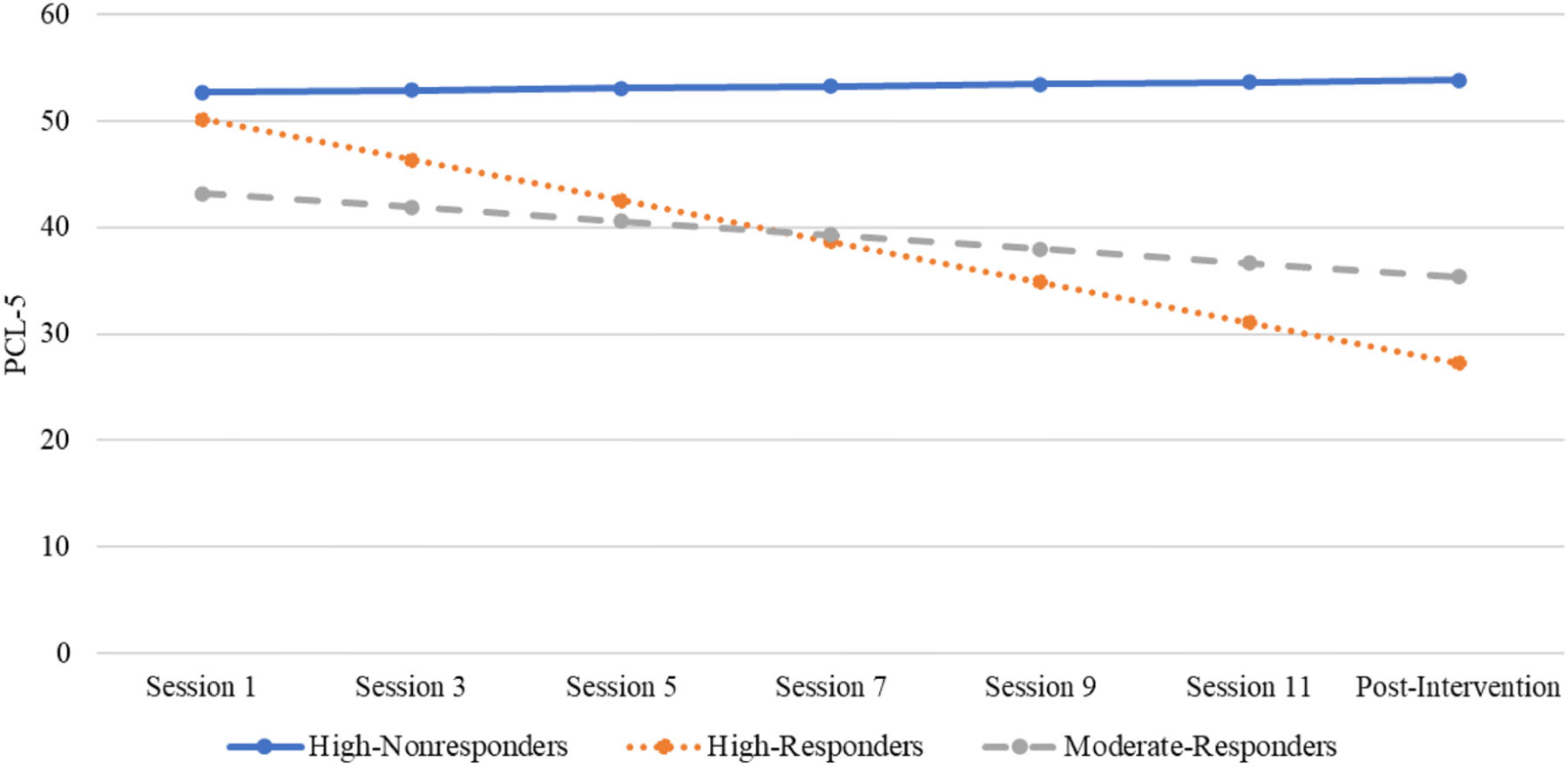
Estimated posttraumatic stress disorder (PTSD) symptom trajectories of high-nonresponder (n = 20), high-responder (n = 14), and moderate-responder (n = 71) classes
Note: PCL-5 = PTSD Checklist for DSM-5.
Panic
PDSS restricted GMM comparisons are presented in Table 4, and all model fit information is presented in Supplementary Table S3. Based on fit information, the four-class LCGA solution indicated that the maximum class threshold to test in the restricted GMM was four classes. Of the less-restricted models, the one-class GMM with intercept and slope variance estimated had the lowest BIC values, followed by the two- and three-class GMMs with intercept variance freed. A comparison of these models favored the three-class GMM with intercept variance freed given that the AIC values were the lowest, the classes had meaningful intercept and slope differences, and BIC values did not differ by 10 or more (Raftery, 1995).
TABLE 4.
Fit indices for growth mixture models of panic from Session 1 to postintervention
| Model | −2LL | Parameters | AIC | BIC | Entropy | LMR-LRT | BLRT |
|---|---|---|---|---|---|---|---|
| Restricted GMM (intercept variance estimated) | |||||||
| 1 class | −1,310.89 | 10 | 2,641.79 | 2,668.33 | |||
| 2 class | −1,298.25 | 13 | 2,622.50 | 2,657.00 | .57 | 23.60 | 25.29 |
| 3 class | −1,293.38 | 16 | 2,618.76 | 2,661.22 | .53 | 9.09 | 9.74 |
| 4 class | −1,286.55 | 19 | 2,611.11 | 2,661.53 | .65 | 12.74 | 13.65* |
| Restricted GMM (slope variance estimated) | |||||||
| 1 class | −1,374.69 | 10 | 2,769.38 | 2,795.92 | |||
| 2 class | −1,320.25 | 13 | 2,666.49 | 2,701.00 | .75 | 101.61* | 108.88** |
| 3 class | −1,299.19 | 16 | 2,630.38 | 2,672.85 | .75 | 39.30 | 42.11 |
| 4 class | −1,291.60 | 19 | 2,621.19 | 2,671.62 | .73 | 14.18 | 15.19 |
| Restricted GMM (intercept and slope variance estimated) | |||||||
| 1 class | −1,298.91 | 12 | 2,621.82 | 2,653.67 | |||
| 2 class | −1,295.77 | 15 | 2,621.53 | 2,661.34 | .59 | 5.87 | 6.29 |
| 3 class | 1,290.22 | 18 | 2,616.43 | 2,664.20 | .70 | 10.36 | 11.10 |
| 4 classa | |||||||
Note: Bolding indicates the best-fitting model. GMM = growth mixture modeling; LL = log-likelihood; AIC = Akaike information criterion; BIC = Bayesian information criterion; LMR-LRT = Lo–Mendell–Rubin likelihood ratio test; BLRT = bootstrapped likelihood ratio test.
The four-class restricted GMM with intercept and slope variance estimated did not converge on a single lowest −2 loglikelihood solution even after increasing the initial starting values to 1,000 and the optimized values to 250.
p < .05.
p < .01.
Figure 3 contains the mean estimated PDSS trajectories for the three classes. Class 1, high nonresponders, contained 21 participants, pp = .71, and captured a flat to slightly increasing effect size, d = −0.13. Class 2, high responders, contained 10 participants, pp = .42, and reflected a large effect size reduction, d = 1.09. Class 3, moderate responders, contained 74 participants, pp = .91, and reflected a small-to-medium effect size symptom reduction, d = 0.36. Entropy was .53 for the overall model, indicating a modest amount of classification misfit.
FIGURE 3.
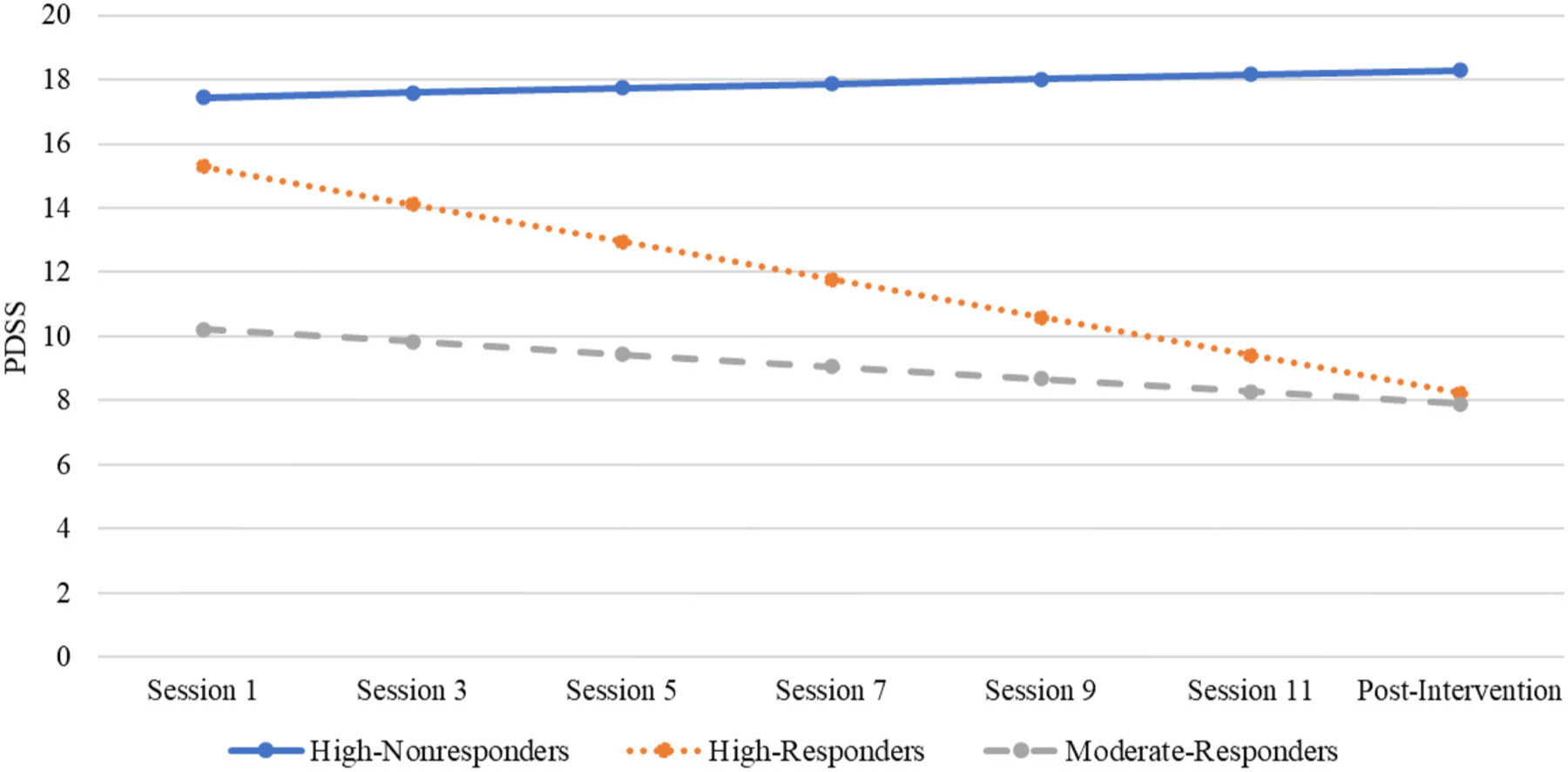
Estimated panic trajectories of high-nonresponder (n = 21), high-responder (n = 10), and moderate-responder (n = 74) classes
Note: PDSS = Panic Disorder Severity Scale.
Comparison of class membership across symptom trajectories
To provide descriptive characteristics on the overlap between depressive symptom, PTSD symptom, and panic classes, crosstabs were calculated to determine the percentage of participants who were classified in similar classes across symptoms (Table 5). For participants in the high nonresponder PTSD symptom class, 50.0% were in the high responder depression class, 45.0% were in the moderate responder depression class, and 5.0% were in the low responder depressive symptom class. For participants in the high nonresponder PTSD class, 57.1% were in the high nonresponder panic class, 5.0% were in the high-responder panic class, and 40.0% were in the moderate responder panic class. Finally, for participants in the high nonresponder panic class, 57.1% were in the high responder depressive symptom class, and 42.9% were in the moderate responder class.
TABLE 5.
Class membership across symptom groups
| Depression | PTSD | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class 1: High responders | Class 2: Moderate resonders | Class 3: Low responders | Class 1: High non-responders | Class 2: High responders | Class 3: Moderate responders | |||||||
| Variable | n | % | n | % | n | % | n | % | n | % | n | % |
| PTSD | ||||||||||||
| Class 1: High nonresponders | 10 | 47.6 | 9 | 14.5 | 1 | 4.5 | ||||||
| Class 2: High responders | 0 | 0.0 | 11 | 17.7 | 3 | 13.6 | ||||||
| Class 3: Moderate responders | 11 | 52.4 | 42 | 67.7 | 18 | 81.8 | ||||||
| Panic | ||||||||||||
| Class 1: High nonresponders | 12 | 57.1 | 9 | 14.5 | 0 | 0.0 | 11 | 55.0 | 1 | 7.1 | 9 | 12.7 |
| Class 2: High responders | 2 | 9.5 | 7 | 11.3 | 1 | 4.5 | 1 | 5.0 | 5 | 35.7 | 4 | 5.6 |
| Class 3: Moderate responders | 7 | 33.3 | 46 | 74.2 | 21 | 95.5 | 8 | 40.0 | 8 | 57.1 | 58 | 81.7 |
Note: PTSD = posttraumatic stress disorder.
Class comparison across risk factors
Results from the comparison of risk factor variables across latent classes are presented in Table 6. Comparing depressive symptom classes, ASI-3, PTQ, and APPQ-A scores were higher among high responders than low responders. ASI-3 and APPQ-A scores were higher among moderate responders than low responders. The likelihood of presenting with a comorbid diagnosis was higher in the high-responder class compared to the moderate- and low-responder classes. Comparing PTSD classes, APPQA scores were higher in the high-nonresponder class than in the high-responder class. Session attendance was lower among moderate responders than high non-responders and high responders. The rate of men and the likelihood of presenting with a comorbid diagnosis were higher in the high-nonresponder and high-responder classes compared to the moderate-responder class. For panic classes, ASI-3 and APPQ-A scores were higher in the high-nonresponders and high-responders classes than in the moderate-responders class. APPQ-A scores were also higher in high nonresponders than high responders. Session attendance was higher among high responders than moderate responders. Homework engagement and session participation scores were higher among high responders than high nonresponders and moderate responders. The likelihood of presenting with a comorbid diagnosis was significantly higher in the high-nonresponder class compared to the moderate-responder class.
TABLE 6.
Examination of class differences in risk factors
| High nonresponders | High responders | Moderate responders | Low responders | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SE | M | SE | M | SE | M | SE | χ2(2, N = 105) |
| Depression b | |||||||||
| Continuous | |||||||||
| ASI-3 | 63.743 | 3.49 | 59.063 | 2.12 | 41.771,2 | 3.52 | 22.66** | ||
| PTQ | 45.173 | 2.64 | 38.97 | 1.77 | 32.351 | 2.73 | 11.47** | ||
| APPQ-A | 35.423 | 4.70 | 26.023 | 2.59 | 15.071,2 | 3.30 | 13.66** | ||
| Age | 42.04 | 2.98 | 49.01 | 1.94 | 49.05 | 3.76 | 4.08 | ||
| Sessions attended | 9.83 | 0.67 | 9.03 | 0.54 | 8.18 | 1.01 | 2.05 | ||
| Session participation | 4.51 | 0.28 | 4.26 | 0.21 | 4.47 | 0.45 | 0.50 | ||
| HW engage | 3.77 | 0.24 | 3.74 | 0.22 | 3.81 | 0.43 | 0.02 | ||
| Categorical | |||||||||
| Sex | 0.72 | 0.09 | 0.65 | 0.06 | 0.72 | 0.09 | 0.73 | ||
| Comorbidity | 0.962,3 | 0.04 | 0.831 | 0.05 | 0.701 | 0.09 | 7.94* | ||
| PTSD | |||||||||
| Continuous | |||||||||
| ASI-3 | 59.75 | 4.37 | 59.62 | 4.90 | 53.97 | 3.26 | 1.05 | ||
| PTQ | 43.55 | 3.49 | 40.12 | 2.36 | 35.38 | 2.79 | 2.54 | ||
| APPQ-A | 34.402 | 5.69 | 19.801 | 4.74 | 23.59 | 3.48 | 4.04 | ||
| Age | 44.90 | 3.83 | 49.70 | 4.56 | 47.59 | 2.60 | 0.69 | ||
| Sessions attended | 11.363 | 0.63 | 10.823 | 0.79 | 7.701,2 | 1.01 | 12.03** | ||
| Session participation | 4.09 | 0.32 | 4.97 | 0.51 | 4.43 | 0.26 | 2.31 | ||
| HW engage | 3.48 | 0.30 | 4.48 | 0.45 | 3.86 | 0.26 | 3.55 | ||
| Categorical | |||||||||
| Sex | 0.893 | 0.06 | 0.843 | 0.08 | 0.551,2 | 0.07 | 15.22** | ||
| Comorbidity | 1.003 | 0.00 | 1.003 | .00 | 0.701,2 | 0.06 | 25.75** | ||
| Panic | |||||||||
| Continuous | |||||||||
| ASI-3 | 71.503 | 4.65 | 65.743 | 4.86 | 47.821,2 | 3.64 | 16.22** | ||
| PTQ | 46.28 | 5.05 | 37.68 | 3.29 | 36.70 | 2.45 | 2.60 | ||
| APPQ-A | 51.342,3 | 6.79 | 26.251 | 5.74 | 16.221 | 3.73 | 19.71** | ||
| Age | 45.18 | 3.85 | 43.95 | 6.65 | 49.08 | 2.65 | 0.73 | ||
| Sessions attended | 10.08 | 0.97 | 12.243 | 1.03 | 8.172 | 0.68 | 9.36** | ||
| Session participation | 4.462 | 0.39 | 5.901,3 | 0.40 | 4.062 | 0.27 | 14.23** | ||
| HW engage | 3.782 | 0.39 | 5.181,3 | 0.29 | 3.562 | 0.26 | 19.36** | ||
| Categorical | |||||||||
| Sex | 0.81 | 0.09 | 0.70 | 0.11 | 0.65 | 0.06 | 2.29 | ||
| Comorbiditya | 0.953 | – | 1.00 | – | 0.771 | – | 8.41* | ||
Note. Sex dummy coded such that 1 = male. Comorbidity dummy coded such that 1 = the presence of any comorbid mental health condition.
The comorbidity outcome did not converge on an acceptable solution in Mplus but did when examined using a multinomial regression in SPSS; these results are reported.
χ2: N = 109.
p < .05.
p < .01. ** p < .05.
DISCUSSION
The present study investigated treatment trajectories for TBT and transdiagnostic predictors of treatment response in veterans with emotional disorders. Across symptoms, a three-class model received the most support for the GMM analyses. However, the pattern of trajectories varied between depressive symptoms compared to PTSD and panic symptoms. All three classes for depressive symptoms responded to TBT and were distinguished by low, moderate, and high baseline symptom levels. In contrast, the classes for PTSD and panic symptoms only distinguished participants with moderate (one class) and high (two classes) baseline symptoms but supported separate classes within the high baseline level for responders and nonresponders. Predictor analyses revealed significant differences in behavioral avoidance between the PTSD and panic symptom high responders and nonresponders wherein nonresponders demonstrated significantly higher behavioral avoidance than responders. These findings for behavioral avoidance were mirrored by trends in the measures of treatment engagement in that PTSD and panic high nonresponders were rated as participating less in session procedures and having lower homework completion than high responders.
Across symptoms and trajectories, the vast majority of patients receiving TBT demonstrated clinically significant and yet moderate diagnostic symptoms at baseline (i.e., above clinical cutoffs) and moderate-to-large effect size reductions from baseline to posttreatment. Although some of these effect sizes were smaller than observed in previous studies of TBT (Gros, 2014; Gros & Allan, 2019) and comparable studies of transdiagnostic interventions (Barlow et al., 2017), the present study investigated disorder-specific measures of depressive symptoms (PHQ-9), PTSD symptoms (PCL-5), and panic disorder (PDSS) across patients with diagnoses of MDD, PTSD, and panic disorder. Thus, for example, the outcomes for patients with PTSD were included in the analyses of the PHQ-9 and PDSS independent of whether comorbid MDD or panic disorder was present. This observation likely had the largest effect on the moderate responder trajectory for the PDSS due to a lower prevalence rate of panic disorder as a principal or comorbid diagnosis. However, despite this potential source of smaller effects, the present findings suggest that most participants with MDD, panic disorder, and PTSD still demonstrated significant symptom reductions across all measures and diagnoses via TBT.
Two identified trajectories were associated with treatment nonresponse in a minority of participants, one each for PTSD and panic symptoms. These participants demonstrated elevated scores at baseline but minimal improvement during treatment. Predictors analyses revealed that nonresponders were associated with elevated behavioral avoidance compared to responders. However, despite TBT’s specific focus on addressing avoidance (Gros, 2014), the findings suggest that these participants’ avoidance may be associated with avoidance of treatment itself, as indicated by poorer participation in session procedures and poorer homework engagement. TBT is heavily reliant on homework participation, with treatment procedures focused on between-session exposure practices and within-session processing and problem-solving of completed exposure practices (Gros, 2014). Of note, homework compliance has been shown to be improved in TBT compared to traditional, disorder-specific therapies that are similarly dependent on homework (e.g., behavioral activation; Shapiro & Gros, 2020). Unfortunately, although clinician-rated measures of in-session procedures and homework engagement did not elucidate the cause for poorer response (e.g., treatment-resistant vs. highly symptomatic), homework compliance consistently has been associated with therapy outcomes across studies and protocols (Mausbach et al., 2010; Rees et al., 2005) and likely contributed to nonresponse in these trajectories for PTSD and panic symptoms.
Given the findings for behavioral avoidance and related treatment participation, clinical implications of the present findings merit discussion for TBT and related treatments. Without knowing the specific cause of increased avoidance and reduced participation, several adaptations should be considered in future implementation of TBT. Mobile applications have been designed for similar behavioral psychotherapies in efforts to improve homework compliance, such as the PE Coach app for prolonged exposure for PTSD (Reger et al., 2013). Similarly, innovative research is investigating whether the incorporation of a peer who has successfully completed exposure-based psychotherapy improves treatment adherence and completion (Hernandez-Tejada et al., 2020). Although motivation and treatment goals are assessed early in TBT (Gros et al., 2023), another approach could be to more fully incorporate motivational interviewing into TBT to better manage patient resistance (Westra & Norouzian, 2018). Although the non-response findings only represent a minority of participants receiving TBT in the present study, these potential adaptations for TBT should be considered to improve outcomes, especially in participants who demonstrate particularly high behavioral avoidance at baseline or initial resistance to within- and between-session procedures.
The findings for the latent classes, effect sizes, and predictors may have been limited by the assessment challenges in completing transdiagnostic psychotherapy research (Gros, 2015). As noted previously, the present study investigated participants with three different principal diagnoses (i.e., MDD, PTSD, and panic disorder) across three separate disorder-specific measures (i.e., the PHQ-9, PCL-5, and PDSS). Though the selection of these measures was important for the parent study investigating TBT and disorder-specific psychotherapies (e.g., participants with PTSD randomized to TBT or cognitive processing therapy and investigated via PCL-5 outcomes), investigating disorder-specific outcomes across all participants, with various diagnoses, has its limitations, as highlighted regarding the potentially smaller observed effect sizes. However, there may be some advantages to this approach as well given the rates of diagnostic comorbidity observed in veterans (Ginzburg et al., 2010). With patients more frequently presenting with multiple diagnoses, understanding the primary and secondary effects of psychotherapeutic practices is essential (Barlow et al., 2004; Gros et al., 2022, 2023). Future transdiagnostic studies should consider incorporating both transdiagnostic and disorder-specific outcome measures, with the studies to date tending to select one or the other (Barlow et al., 2017; Gros & Allan, 2019). Additionally, it is important to note that GMM and similar methodologies are exploratory and hypothesis-generating by nature rather than confirmatory (Muthen, 2003). This need for confirmatory follow-up underscores the importance of continued, comprehensive investigation in transdiagnostic intervention research.
The present study investigated latent classes via GMM in veterans receiving TBT. The analyses revealed that the majority of participants who received TBT demonstrated symptom reductions with medium-to-large effect sizes across depression, PTSD, and panic disorder in a sample of veterans with various diagnoses and comorbidities. The present findings contribute to the growing literature supporting the efficacy of transdiagnostic psychotherapies in the treatment of emotional disorders, including PTSD. Potential adaptations to TBT should be considered in patients with significantly elevated behavioral avoidance at treatment onset to improve treatment engagement and homework completion and further improve outcomes.
Supplementary Material
OPEN PRACTICES STATEMENT.
The study reported in this article was not formally preregistered. Neither the data nor the materials have been made available on a permanent third-party archive; requests for the data or materials can be sent via email to the lead author at grosd@musc.edu.
Funding information
U.S. Department of Veterans Affairs, Grant/Award Number: CX001846
This study was supported by Department of Veterans Affairs Clinical Sciences Research and Development Merit Award I01 CX001846 (PI: Daniel F. Gros). This research was also supported in part by the Department of Veterans Affairs (VA) Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Ann Arbor VA Healthcare System, and the Serious Mental Illness Treatment Resource and Evaluation Center (SMITREC).
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government. There are no conflicts of interest to disclose.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- Adler DA, Possemato K, Mavandadi S, Lerner D, Chang H, Klaus J, Tew JD, Barrett D, Ingram E, & Oslin DW (2011). Psychiatric status and work performance of veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatric Services, 62(1), 39–46. 10.1176/appi.ps.62.1.39 [DOI] [PubMed] [Google Scholar]
- Allan NP, Gros DF, Myers US, Korte KJ, & Acierno R (2017). Predictors and outcomes of growth mixture modeled trajectories across an exposure-based PTSD intervention with veterans. Journal of Clinical Psychology, 73(9), 1048–1063. 10.1002/jclp.22408 [DOI] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling, 21(3), 329–341. 10.1080/10705511.2014.915181 [DOI] [Google Scholar]
- Barlow DH, Allen LB, & Choate ML (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35(2), 205–230. 10.1016/S0005-7894(04)80036-4 [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, & Cassiello-Robbins C (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74(9), 875–884. 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blore JD, Sim MR, Forbes AB, Creamer MC, & Kelsall HL (2015). Depression in Gulf War veterans: A systematic review and meta-analysis. Psychological Medicine, 45(8), 1565–1580. 10.1017/S0033291714001913 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psycho-metric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Brown TA (2014). Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5)-Adult and Lifetime Version: Clinician manual. Oxford University Press. [Google Scholar]
- Coyne AE, & Gros DF (2022). Comorbidity as a moderator of the differential efficacy of transdiagnostic behavior therapy vs. behavioral activation for affective disorders. Psychotherapy Research, 32(7), 886–897. 10.1080/10503307.2021.2022236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Lier PA, van Straten A, & Donker M (2005). Examining differential effects of psychological treatment of depressive disorder: An application of trajectory analyses. Jour nal of Affective Disorders, 89(1–3), 137–146. 10.1016/j.jad.2005.09.001 [DOI] [PubMed] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1(1), 16–29. 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- Dewar M, Paradis A, & Fortin CA (2020). Identifying trajectories and predictors of response to psychotherapy for post-traumatic stress disorder in adults: A systematic review of literature. Canadian Journal of Psychiatry, 65(2), 71–86. 10.1177/0706743719875602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, Zetsche U, Weidacker K, Wahl K, Schönfeld S, & Ehlers A (2011). The Perseverative Thinking Questionnaire (PTQ): Validation of a content-independent measure of repetitive negative thinking. Journal of Behavior Therapy and Experimental Psychiatry, 42(2), 225–232. 10.1016/j.jbtep.2010.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginzburg K, Ein-Dor T, & Solomon Z (2010). Comorbidity of posttraumatic stress disorder, anxiety and depression: A 20-year longitudinal study of war veterans. Journal of Affective Disorders, 123(1–3), 249–257. 10.1016/j.jad.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Gros DF (2014). Development and initial evaluation of trans-diagnostic behavior therapy (TBT) for veterans with affective disorders. Psychiatry Research, 220(1–2), 275–282. 10.1016/j.psychres.2014.08.018 [DOI] [PubMed] [Google Scholar]
- Gros DF (2015). Design challenges in transdiagnostic psychotherapy research: Comparing transdiagnostic behavior therapy (TBT) to existing evidence-based psychotherapy in veterans with affective disorders. Contemporary Clinical Trials, 43, 114–119. 10.1016/j.cct.2015.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, & Allan NP (2019). A randomized controlled trial comparing transdiagnostic behavior therapy (TBT) and behavioral activation in veterans with affective disorders. Psychiatry Research, 281, Article 112541. 10.1016/j.psychres.2019.112541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, Allan NP, Koscinski B, Keller S, & Acierno R (2022). Influence of comorbid social anxiety disorder in PTSD treatment outcomes for prolonged exposure in female military sexual trauma survivors with PTSD. Journal of Clinical Psychology, 79(2), 1039–1050. 10.1002/jclp.23456 [DOI] [PubMed] [Google Scholar]
- Gros DF, Allan NP, & Szafranski DD (2016). Movement towards transdiagnostic psychotherapeutic practices for the affective disorders. Evidence-based Mental Health, 19(3), e10–e12. 10.1136/eb-2015-102286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, Keller S, Allan NP, & Szafranski DD (2023). Application of transdiagnostic behavior therapy (TBT) to diagnostic comorbidity. Psychiatry Research Case Reports, 2(1), Article 100102. 10.1016/j.psycr.2022.100102 [DOI] [Google Scholar]
- Gros DF, Shapiro MO, & Allan NP (2020). Efficacy of transdiagnostic behavior therapy on transdiagnostic avoidance in veterans with emotional disorders. Journal of Clinical Psychology, 76(1), 31–39. 10.1002/jclp.22874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, Szafranski DD, & Shead SD (2017). A real world dissemination and implementation of transdiagnostic behavior therapy (TBT) for veterans with affective disorders. Journal of Anxiety Disorders, 46, 72–77. 10.1016/j.janxdis.2016.04010. [DOI] [PubMed] [Google Scholar]
- Hernandez-Tejada MA, Muzzy W, Price M, Hamski S, Hart S, Foa E, & Acierno R (2020). Peer support during in vivo exposure homework to reverse attrition from prolonged exposure therapy for posttraumatic stress disorder (PTSD): Description of a randomized controlled trial. Trials, 21(1), 1–11. 10.1186/s13063-020-04302-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, & Engel CC (2007). Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry, 164(1), 150–153. 10.1176/ajp.2007.164.1.150 [DOI] [PubMed] [Google Scholar]
- Hoglund MW, & Schwartz RM (2014). Mental health in deployed and nondeployed veteran men and women in comparison with their civilian counterparts. Military Medicine, 179(1), 19–25. 10.7205/MILMED-D-13-00235 [DOI] [PubMed] [Google Scholar]
- Jung T, & Wickrama KAS (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 21(1), 302–317. 10.1111/j.1751-9004.2007.00054.x [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen H-U (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline AC, Cooper AA, Rytwinski NK, & Feeny NC (2021). The effect of concurrent depression on PTSD outcomes in trauma-focused psychotherapy: A meta-analysis of randomized controlled trials. Behavior Therapy, 52(1), 250–266. 10.1016/j.beth.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke J, Spitzer RL, & Williams JBW (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, & Bray BC (2013). Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling: A Multidisciplinary Journal, 20(1), 1–26. 10.1080/10705511.2013.742377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Holder N, Madden E, Li Y, Seal KH, Neylan TC, Lujan C, Patterson OV, DuVall SL, & Shiner B (2020). Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001–2014. Depression and Anxiety, 37(4), 356–364. 10.1002/da.22983 [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Moore R, Roesch S, Cardenas V, & Patterson TL (2010). The relationship between homework compliance and therapy outcomes: An updated meta-analysis. Cognitive Therapy and Research, 34(5), 429–438. 10.1007/s10608-010-9297-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moors A, Ellsworth PC, Scherer KR, & Frijda NH (2013). Appraisal theories of emotion: State of the art and future development. Emotion Review, 5(2), 119–124. 10.1177/1754073912468165 [DOI] [Google Scholar]
- Mott JM, Hundt NE, Sansgiry S, Mignogna J, & Cully JA (2014). Changes in psychotherapy utilization among veterans with depression, anxiety, and PTSD. Psychiatric Services, 65(1), 106–112. 10.1176/appi.ps.201300056 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus user’s guide (7th ed.). Muthén & Muthén. [Google Scholar]
- Muthén B (2003). Statistical and substantive checking in growth mixture modeling: Comment on Bauer and Curran (2003). Psychological Methods, 8(3), 369–377. 10.1037/1082-989X.8.3.369 [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin, 136(1), 128–150. 10.1037/a0018055 [DOI] [PubMed] [Google Scholar]
- Norton PJ, & Paulus DJ (2016). Toward a unified treatment for emotional disorders: Update on the science and practice. Behavior Therapy, 47(6), 854–868. 10.1016/j.beth.2015.07.002 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén M &, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Owen J, Adelson J, Budge S, Wampold B, Kopta M, Minami T, & Miller S (2015). Trajectories of change in psychotherapy. Journal of Clinical Psychology, 71(9), 817–827. 10.1002/jclp.22191 [DOI] [PubMed] [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. 10.2307/271063 [DOI] [Google Scholar]
- Rees CS, McEvoy P, & Nathan PR (2005). Relationship between homework completion and outcome in cognitive behaviour therapy. Cognitive Behaviour Therapy, 34(4), 242–247. 10.1080/16506070510011548 [DOI] [PubMed] [Google Scholar]
- Reger GM, Hoffman J, Riggs D, Rothbaum BO, Ruzek J, Holloway KM, & Kuhn E (2013). The “PE Coach” smart-phone application: An innovative approach to improving implementation, fidelity, and homework adherence during prolonged exposure. Psychological Services, 10(3), 342–349. 10.1037/a0032774 [DOI] [PubMed] [Google Scholar]
- Ruzek JI, Karlin BE, Zeiss A (2012). Implementation of evidence-based psychological treatments in Veterans Health Administration. In McHugh RK, & Barlow DH (Eds.), Dissemination and implementation of evidence-based psychological interventions (pp. 78–96). Oxford University Press. 10.1093/med:psych/9780195389050.003.0013 [DOI] [Google Scholar]
- Santacana M, Arias B, Mitjans M, Bonillo A, Montoro M, Rosado S, Guillamat R, Valles V, Perez V, Forero CG, & Fullana MA (2016). Predicting response trajectories during cognitive-behavioural therapy for panic disorder: No association with the BDNF gene or childhood maltreatment. PloS One, 11, Article e0158224. 10.1371/journal.pone.0158224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer-Zavala S, Boswell JF, Gallagher MW, Bentley KH, Ametaj A, & Barlow DH (2012). The role of negative affectivity and negative reactivity to emotions in predicting outcomes in the unified protocol for the transdiagnostic treatment of emotional disorders. Behaviour Research and Therapy, 50(9), 551–557. 10.1016/j.brat.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schein J, Houle C, Urganus A, Cloutier M, Patterson-Lomba O, Wang Y, King S, Levinson W, Guérin A, Lefebvre P, & Davis LL (2021). Prevalence of post-traumatic stress disorder in the United States: A systematic literature review. Current Medical Research and Opinion, 37(12), 2151–2161. 10.1080/03007995.2021.1978417 [DOI] [PubMed] [Google Scholar]
- Shapiro MO, & Gros DF (2021). Acceptability of a transdiagnostic behavior therapy in veterans with affective disorders. Psychological Services, 18(4), 643–650. 10.1037/ser0000490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, Houck P, & Wang T (2001). Reliability and validity of the Panic Disorder Severity Scale: Replication and extension. Journal of Psychiatric Research, 35(5), 293–296. 10.1016/S0022-3956(01)00028-0 [DOI] [PubMed] [Google Scholar]
- Sorg S, Vögele C, Furka N, & Meyer AH (2012). Perseverative thinking in depression and anxiety. Frontiers in Psychology, 3, Article 20. 10.3389/fpsyg.2012.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Abramowitz JS, Holaway RM, Sandin B, Stewart SH, Coles M, Eng W, Daly ES, Arrindell WA, Bouvard M, & Cardenas SJ (2007). Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index–3. Psychological Assessment, 19(2), 176–188. 10.1037/1040-3590.19.2.176 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmier PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- Westra HA, & Norouzian N (2018). Using motivational interviewing to manage process markers of ambivalence and resistance in cognitive behavioral therapy. Cognitive Therapy and Research, 42(2), 193–203. 10.1007/s10608-017-9857-6 [DOI] [Google Scholar]
- Zeelenberg M, Nelissen RM, Breugelmans SM, & Pieters R (2008). On emotion specificity in decision making: Why feeling is for doing. Judgment and Decision Making, 3(1), 18–27. 10.1017/S1930297500000139 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


