Abstract
Background:
Severe, chronic irritability is receiving increased research attention, and is the cardinal symptom of a new diagnostic category, Disruptive Mood Dysregulation Disorder (DMDD). Although data from epidemiological community samples suggest that childhood chronic irritability predicts unipolar depression and anxiety in adulthood, whether these symptoms are stable and cause ongoing clinical impairment is unknown. The present study presents 4-year prospective, longitudinal diagnostic and impairment data on a clinical sample of children selected for symptoms of severe irritability (operationalized as severe mood dysregulation [SMD]).
Methods:
Youth meeting criteria for SMD (n=200) were evaluated at baseline using standard diagnostic methods. Two (n=78) and four-year (n=46) follow-up diagnostic and clinical impairment ratings collected at 6 month intervals were completed with those youths enrolled in the study for a sufficient period of time.
Results:
Although the number of youth meeting strict categorical SMD criteria declined over time (49% and 40% at 2 and 4 yrs, respectively), many individuals not meeting full criteria continued to display clinically significant irritability symptoms (2yrs: 42%; 4yrs: 37%). Impairment due to these irritability symptoms remained consistently in the moderate range on the Clinical Global Impressions Scale.
Conclusions:
By the four year follow-up, only 40% of youths meet strict SMD criteria; however, most continue to display clinically impairing symptoms and significant impairment warranting psychiatric treatment. These findings provide evidence for the course of irritability, with implications for DMDD. Future research with populations meeting DMDD criteria and followed through the ages of high risk for psychiatric diagnoses is necessary.
Keywords: irritability, longitudinal, DMDD, severe mood dysregulation
Introduction
Characterizing the clinical presentation and longitudinal outcome of severely irritable children is important because irritability is common (~3–5% of youth (1–4)) and predicts poor outcomes (high rates of psychiatric co-morbidity, suicidality, and social and functional impairment (3–6)). Studying severe irritability is especially pressing following the adoption of Disruptive Mood Dysregulation Disorder (DMDD) by DSM 5; however, little research exists. The present study describes the clinical presentation of 200 youths evaluated as part of a longitudinal study of Severe Mood Dysregulation (SMD), the syndrome upon which diagnostic criteria for DMDD were based. We report diagnostic and clinical impairment assessments conducted over a four-year follow up period, focusing on the stability of irritability and irritability-related impairment.
Few studies have examined the course of childhood irritability, including its stability and relationship to future psychopathology. Community and clinical studies suggest that a large percentage of children only meet SMD or DMDD criteria at a single assessment point (1, 7), and that childhood irritability predicts unipolar depression and anxiety, but not bipolar disorder (BD), in adulthood (1, 8–11). However, those studies identified youths with SMD or DMDD retrospectively, and did not examine subthreshold symptoms that continued to cause significant impairment. While criteria for SMD and DMDD identify youths with extreme forms of irritability, the strict criteria may ignore a subset of youths whose irritability is significant and impairing, but falls just below established criteria. Further studies of clinical populations selected for symptoms of severe irritability that track subthreshold irritability symptoms as well as diagnoses throughout childhood and adolescence are essential for informing hypotheses about the longitudinal clinical outcome of such youth.
To date, only one study has prospectively followed severely irritable youth longitudinally. Due to controversy in the literature over the diagnostic criteria for BD in youths, (12), the study compared hypomanic/manic and depressive episodes rates between youths with SMD and those with BD (13). Youth with SMD were less likely to have manic or depressive episodes than those with BD (1.2% vs. 62%). The present study builds on this work by describing a larger sample over a longer period of time to better address the question of whether SMD is a developmental form of BD. In addition, we examine the stability of SMD as well as subthreshold, yet clinically impairing irritability symptoms, in order to take a dimensional approach to the persistence of irritability over time.
Current Study
The present study addressed two clinical questions using data from a sample of 200 youths enrolled in an ongoing longitudinal study of SMD and preliminary data on a subset of participants up to 4 years after their initial evaluation.
First, we examined the longitudinal course of clinically significant irritability at 2 and 4 years by examining the percentage of youths meeting full criteria for SMD, and what percentage continued to report high levels of irritability that caused significant impairment, despite not meeting full criteria for SMD. We expected that the majority of youths would either continue to meet full SMD criteria or would report that irritability symptoms caused significant impairment. That is, we expected very few youths to report minimal or complete absence of irritability. We also retrospectively applied DSM 5 DMDD criteria to explore what percentage of our SMD sample met criteria for DMDD. Second, we prospectively examined rates of new diagnoses to replicate prior associations between childhood irritability and adult unipolar depression and anxiety, but not BD (1, 7–9, 13).
Methods
Participants
Participants were 200 youths (ages 7–17.6 years) enrolled in an IRB-approved study in the NIMH Intramural Program between July 1, 2002 and December 31, 2012. Parents and children provided written informed consent/assent. All youths met published criteria for SMD (14), including severe and chronic irritability, behavioral reactivity, and hyperarousal symptoms with onset prior to 12 years of age. Irritability and behavioral reactivity were consistently present for at least a year prior to evaluation and caused severe impairment in at least one domain and mild impairment in at least one other domain (i.e., home, school, peers). Exclusion criteria included distinct hypomanic or manic episodes lasting ≥1 day, IQ<70, pervasive developmental disorder, unstable medical illness, substance abuse within the past 2 months, psychosis, current posttraumatic stress disorder (PTSD), and irritability only in the context of a major depressive episode.
Overall Study Procedure
Clinical assessments were made during onsite visits at NIMH and by phone follow up (see below and Figure 1 for details about assessments at specific visits). First, participants completed an onsite evaluation visit where study eligibility was determined using a diagnostic interview and global impairment was ascertained. Participants meeting SMD criteria were invited to enroll and returned to the NIMH (M=72.2 days, SD=90.98) for admission into a treatment trial (N=78; 43%) or a “baseline” visit as part of the non-treatment longitudinal study (N=103; 57%). Clinical severity ratings were completed during these visits. Data collected at both initial onsite diagnostic evaluation and the baseline visit are referred to as “baseline” data below. Participants and their parents returned to the NIMH approximately 2 and 4 years after the initial evaluation for diagnostic interviews and clinical severity ratings. Clinicians conducted telephone follow-up assessments of clinical severity and impairment with a parent at 6 month intervals starting 6 months after each onsite visit.
Figure 1.
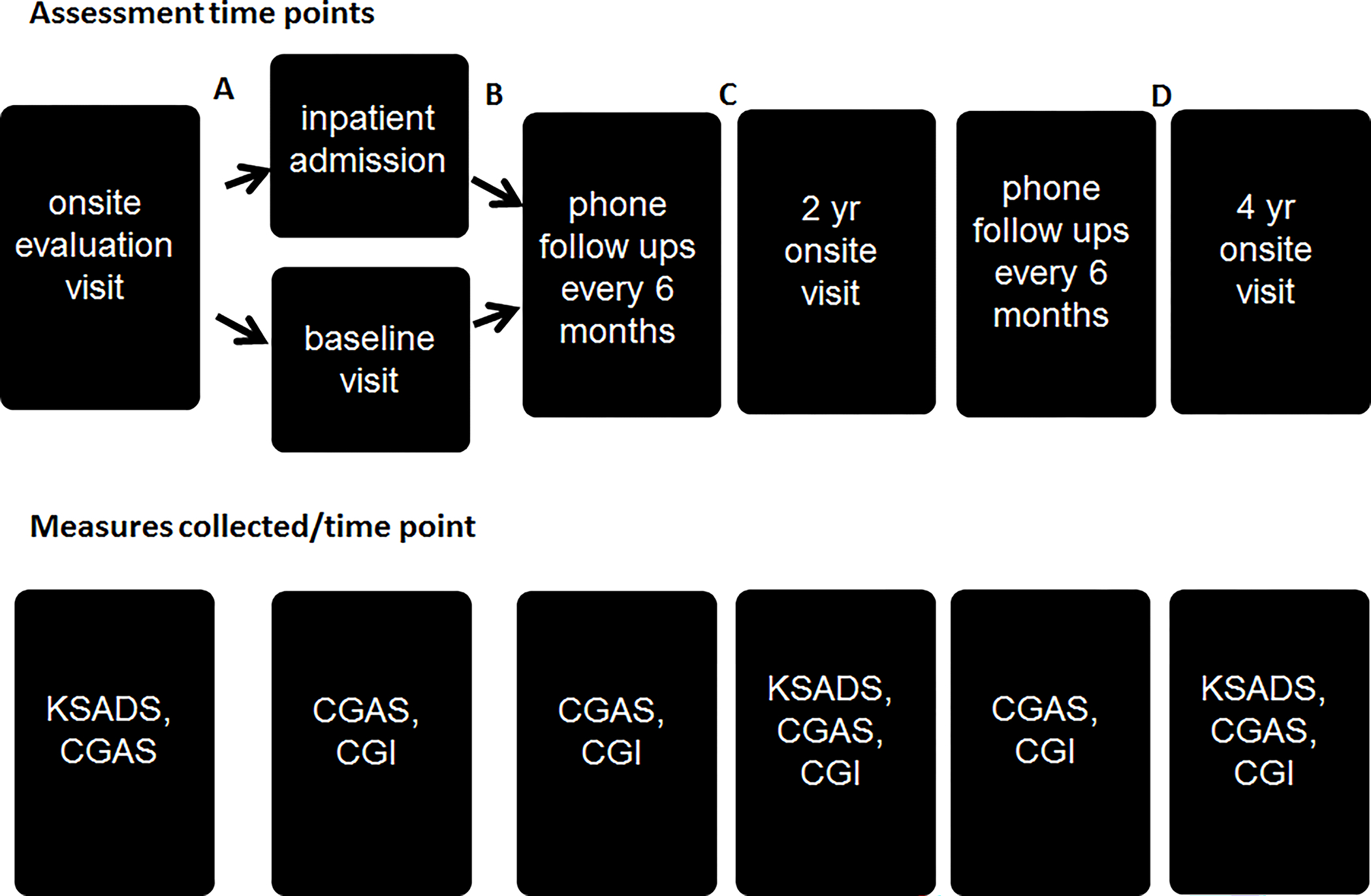
Overall schema of the study protocol. The first line of information describes the terms used for each of the assessment points throughout the study and the number of individuals with data at each time point. The second line includes the diagnostic and clinical measures collected at each time point. Briefly, participants were evaluated for the study at the onsite evaluation and returned shortly thereafter to enroll in the longitudinal protocol and establish baseline clinical severity ratings. After this, they were contacted by phone at 6 month intervals to determine symptom severity and impairment. Participants returned for an onsite evaluation at 2 years and 4 years following study enrollment; diagnostic interviews, assessing psychiatric diagnoses present during the interval since the last onsite assessment were repeated at these visits. Note: letters A-D reflect the time points where retention analyses comparing youths who remained in the study versus those who did not were completed (see supplemental information for details).
Clinical assessments were conducted by graduate level licensed clinicians with 5–25 yrs of post-licensure clinical experience and extensive training involving 20–30 hours of observation, monitored administration of the instrument, and establishing reliability with experienced child research clinicians (κ ≥.9) for all measures.
Diagnostic Measures
Patient diagnoses were determined using the Kiddie Schedule for Affective Disorders – Present and Lifetime Version (K-SADS-PL; (15)) and a specifically developed supplementary module for SMD. Interviews were administered to parents and children separately by different clinicians. Diagnoses were based on best-estimate procedures in a consensus conference led by at least one psychiatrist with extensive experience evaluating children with similar symptoms. For patients following up after their 18th birthday (2yr: n=1; 4yr: n=3), diagnoses were determined using the Structured Interview for the DSM-IV-TR Patient Edition (16) and the SMD supplementary module administered to the patient.
SMD and DMDD.
Because the longitudinal course of irritability was of primary interest, participants not meeting full SMD criteria at follow-up were categorized into three categories based on the presence or absence of core symptoms (i.e., irritability and excess reactivity/outbursts), and the presence or absence of impairment and illness severity (determined by the SMD module and/or by scores on a modified CGI assessing SMD symptoms. These divisions were aimed at distinguishing participants with clinically significant irritability symptoms that would likely warrant treatment in the community (threshold and sub-threshold) from participants with mild irritability not necessarily requiring treatment (partial remission and remission) or whose symptoms were being adequately managed by psychiatric treatment (see supplemental material). Adequate data were unavailable to categorize 5 participants (2yrs: n=2; 4yrs: n=3) who were not included in the SMD stability analysis.
We retrospectively applied DMDD criteria to the prospectively-obtained SMD module. Participants were identified as having DMDD if they had both core irritability/outburst symptoms present at threshold level (score of 3/3), impairment in >1 domain, at least 1yr of consecutive symptoms, and onset before age 10yrs.
Co-Occurring Psychiatric Diagnoses.
Lifetime diagnoses reflect diagnoses present at any time up to the initial diagnostic interview. During the 2 and 4 year follow-ups, four categories were generated per diagnosis: (a) “never existed” (i.e., diagnostic criteria never met); (b) “in remission” (i.e., criteria met at the prior interview but not in the interval between interviews); (c) “new onset” (i.e., criteria met only during the follow-up period) and (d) “continuous” (i.e., diagnostic criteria met at the initial interview and during the follow-up period). We first present the percentage of youths meeting criteria for an illness category for the first time (category onset rate) and then present the percentage of youths meeting criteria for a new illness within that category for the first time (illness onset rate). The latter category captures the true new onset of each illness. For example, some children met criteria for separation anxiety disorder during the initial evaluation and developed GAD during the follow-up period. The first percentage (category onset rate) would consider this youth as having had a continuous lifetime anxiety disorder, while the second percentage would represent the development of a distinct anxiety disorder (illness onset rate).
Clinical Severity Measures
Clinical severity was assessed using the Clinical Global Impression Severity Scale (CGI) (17) – Overall Symptom Score and a SMD-specific rating. This scale ranges from 1 (normal functioning) to 7 (very severe illness/very severe impairment). Scores of 4 and 5 reflect moderate and marked illness severity/impairment, respectively.
The impact of psychiatric illness on general functioning was assessed using the KSADS Children’s Global Assessment of Functioning Scale (CGAS) (18) or the SCID Global Assessment of Functioning (GAF) (19). Both scales range from 0–100. Higher scores reflect better functioning. Scores in the 40–50 range reflect “moderate degree of interference in functioning in most social areas or severe impairment of functioning in one area”. Number of psychiatric medications, outpatient psychiatric treatment, and psychiatric hospitalizations were also considered as indicators of clinical severity and impairment.
Socioeconomic Status
The Two Factor Hollingshead Index of Social Position (20) was used to determine socioeconomic status (SES). The highest reported education and occupational levels of any parent or parental figure was used.
Participant Retention
The present research required clinically severe patients, from all over the country, to participate in several multi-day visits to the NIMH over a period of several years. Importantly, no treatment was provided at these visits and youths ≥18 years had to sign consent forms at follow-up documenting their continued willingness to participate. These factors made maintaining enrollment after the initial evaluation a unique challenge (see Figure S1 for the CONSORT diagram).
Several unique time points were identified for retention analyses (Figure 1). These included: after the initial evaluation and before the baseline visit (Point A), after the baseline visit but before the first phone follow-up (Point B), after phone follow-up but before the 2 year onsite visit (Point C), and after the 2 year but before the 4 year onsite visit (Point D).
Statistical Analyses
Retention Analyses
We conducted multiple retention analyses to examine the effects of attrition on our study findings. Details about these analyses are included in the supplemental material. Briefly, in one group of analyses, t tests or Chi squares compared individuals who completed each assessment versus those who did not on a variety of demographic and clinical variables (including parental psychopathology). Youths who completed the initial diagnostic evaluation but did not enroll in the longitudinal study were taking more psychotropic medications than those who enrolled. Youths that enrolled in the study but did not complete any follow up assessments were older and had a later age of SMD onset than those who completed at least one phone follow up. No significant differences were noted for the remaining demographic and clinical variables (including parental psychopathology).
A second group of analyses used linear regressions to predict CGAS total scores at year 2 and year 4 from baseline CGAS scores using three different methods for handling missing data (see supplemental material). Results suggest that our findings are unlikely to be due to the unique characteristics of the youths who completed the follow-up assessments.
Results
Demographics
Demographic characteristics and psychiatric treatment information at all assessment points are presented in Table 1.
Table 1.
Demographic, Treatment, Socioeconomic, and Clinical Characteristics of Youth with Severe Mood Dysregulation at Baseline and 2 and 4 year Follow-Up Assessments
| Characteristic | Baseline (n=200) |
2yr (n=78) |
4yr (n=46) |
|||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Time since baseline visit (in days) | -- | -- | 871.1 | 97.9 | 1535.58 | 178.11 |
| Age | 11.6 | 2.4 | 13.4 | 2.0 | 15.0 | 2.1 |
| IQ† | 106.1 | 14.4 | 107.0 | 14.8 | 106.8 | 14.3 |
| Socioeconomic Status† | 55.7 | 29.7 | 58.2 | 28.6 | 57.53 | 29.0 |
| Age of onset† | 5.1 | 2.5 | 4.5 | 2.0 | 4.5 | 1.9 |
| Number of medications† | 2.4 | 1.5 | 2.0 | 1.3 | 2.3 | 1.6 |
| Number of co-occurring diagnosesa | 3.9 | 1.8 | 4.6 | 1.7 | 5.0 | 2.1 |
| N | % | N | % | N | % | |
| Male | 130 | 65.0 | 55 | 70.5 | 33 | 73.3 |
| Adopted | 45 | 22.5 | 15 | 19.2 | 8 | 17.4 |
| Race/Ethnicity † | ||||||
| Caucasian | 164 | 82.4 | 67 | 85.9 | 40 | 87.0 |
| Black/African-American | 11 | 5.5 | 2 | 2.6 | 1 | 2.2 |
| Asian | 7 | 3.5 | 2 | 2.6 | 1 | 2.2 |
| Hispanic/Latino | 1 | .5 | 0 | 0 | 2 | 4.3 |
| Other | 16 | 8.4 | 7 | 9.0 | 2 | 4.3 |
| Treatment † | ||||||
| Outpatient | 191 | 97.9 | 57 | 81.4 | 34 | 73.1 |
| Inpatient | 71 | 36.2 | 13 | 16.7 | 8 | 19.0 |
| Medication † | ||||||
| Unmedicated | 26 | 13.0 | 14 | 18.4 | 7 | 15.9 |
| Atypical Antipsychotic | 116 | 58.0 | 36 | 47.4 | 16 | 36.4 |
| Lithium | 26 | 13.0 | 15 | 19.5 | 14 | 31.1 |
| Antiepileptic | 75 | 37.5 | 16 | 21.1 | 16 | 36.4 |
| Antidepressant | 66 | 33.0 | 24 | 31.6 | 14 | 31.8 |
| Anti-ADHD medicationb | 115 | 57.5 | 46 | 60.5 | 25 | 56.8 |
IQ = WASI Full-scale IQ
Self-identified race/ethnicity categories and labels are consistent with current U.S.A. federal guidelines. Hispanic/Latino is defined as an ethnicity that may be of any race, others are divided by racial categories presented. No participant identified as Native Hawaiian/Other Pacific Islander or American Indian/Alaskan Native. “Other” refers to participants who identified as two or more races or other.
Data were not available for all participants for these variables. The following subsample of data was included for the baseline evaluation: IQ (n=124); socioeconomic status (n=162); Race/Ethnicity (n=199); Age of Onset (n=169); Outpatient Treatment (n=195); Hospitalization (n=196); Any Treatment (n=199).
The following subsample of data was included for the 2 yr follow-up: IQ (n=76); Outpatient Treatment (n=70); Hospitalization (n=69). Number of medications (n=76); Lithium (n=77); All other medication (n=76). The following subsample of data was included for the 4 yr follow-up: IQ (n=44); Number of medications (n=44); Lithium (n=45); All other medication (n=44).
For variables with missing data, mean values and percentages are calculated relative to the number of participants with data for this variable.
number of co-occurring diagnoses reflects the number of lifetime co-occurring diagnoses, excluding SMD, that existed at any point up to and including each assessment.
Anti-ADHD medication included stimulants as well as non-stimulants
Socioeconomic Status was determined using the 2- factor Hollingshead index of social position. Due to data availability, the maximum value for parent education and occupation (regardless of parental figure) was used.
SMD Stability
Most youths who completed the 2 and 4 year follow ups continued to have clinically significant irritability (Figure 2). 48.7% of the youths met full SMD criteria and 42.1% met subthreshold SMD criteria at the 2-year follow up. A minority of patients improved significantly (i.e., 6.6% were designated as partial remission and 2.6% considered to have no diagnosis). At the 4 year follow up, 39.5% met full criteria and 37.2% had sub-threshold SMD. Partial remission accounted for 9.3% of participants and 14.0% had no diagnosis. These data suggest that most youth with SMD continue to have clinically significant irritability at follow-up.
Figure 2.
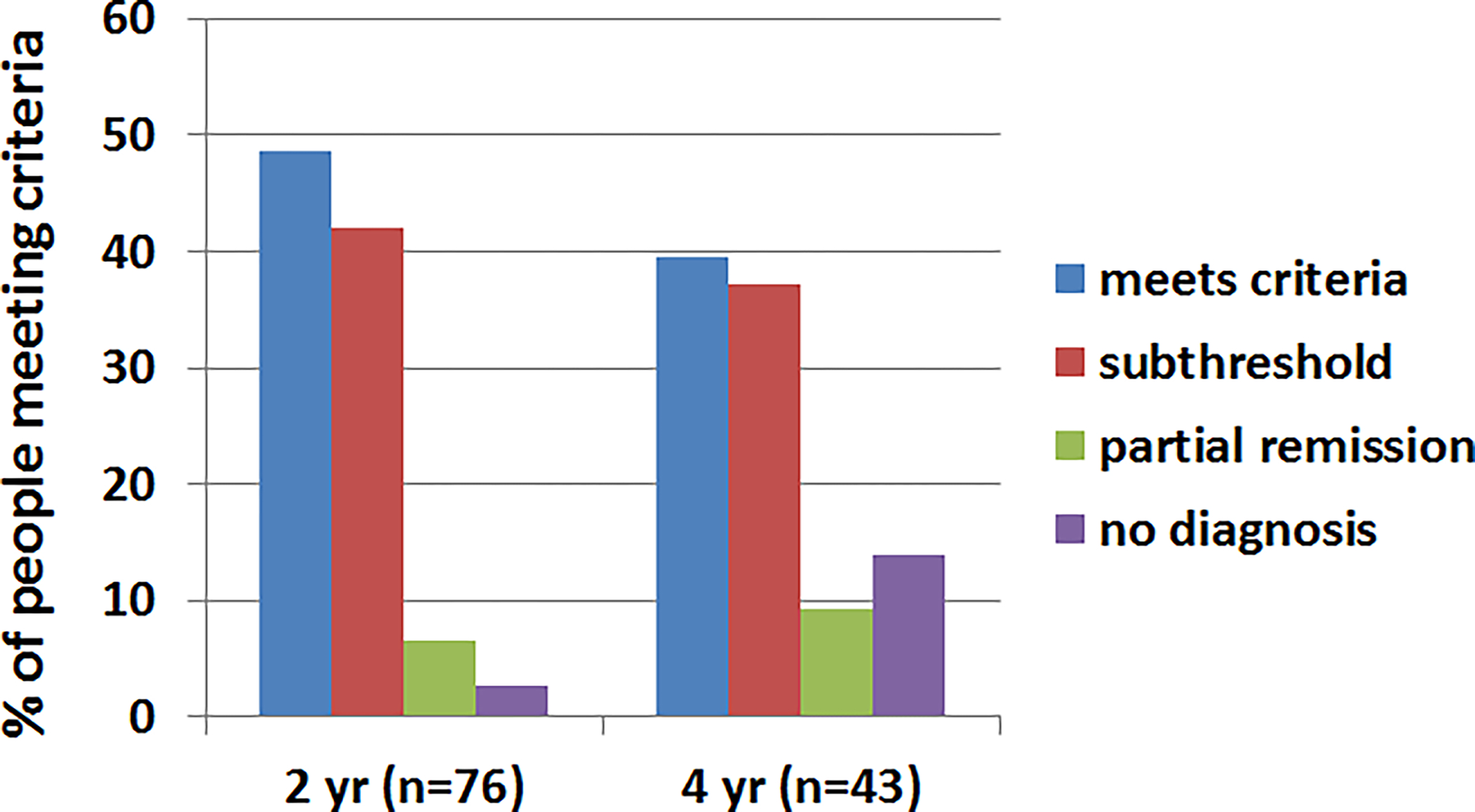
SMD stability over time. Values represent the percent of individuals meeting criteria for each subcategory of SMD within the past 6 months at 2 and 4 year follow-up visits. Values represent the percent of individuals meeting criteria at each time point. Note: 100% of youth (n=200) met criteria for SMD at baseline. N’s at the 2 and 4 year follow-ups reflect the number of individuals with data available to categorize as subthreshold or partial remission.
DMDD
Of the 200 youths who met criteria for SMD, 194 (97%) also met criteria for DMDD. The remaining 6 individuals had an age of onset of 10 or 11 years. Of the youths who met criteria for DMDD at baseline, and completed a follow-up with enough symptom information recorded to make a retrospective DMDD diagnosis, 51.3% and 36.4% continued to meet criteria for DMDD at 2 and 4 years, respectively. The retrospective nature of DMDD diagnoses precluded our ability to assess subthreshold DMDD symptoms over time.
linical Severity and Impairment over Time
Clinical severity data indicated moderate levels of clinical impairment at initial evaluation and across the follow-up period (Figure 3). At the time of initial evaluation, nearly all (97.9%) patients had received outpatient psychiatric treatment, including pharmacotherapy, and 35.7% had a prior psychiatric hospitalization (range 0–9). Psychiatric treatment rates remained high (i.e., ≥ 73.1%) at each follow-up period (Table 1). More than 80% were taking psychotropic medications, including a large percentage of youths taking an atypical antipsychotic medication. Almost 20% were hospitalized for psychiatric reasons during the intervals between follow-up visits.
Figure 3:
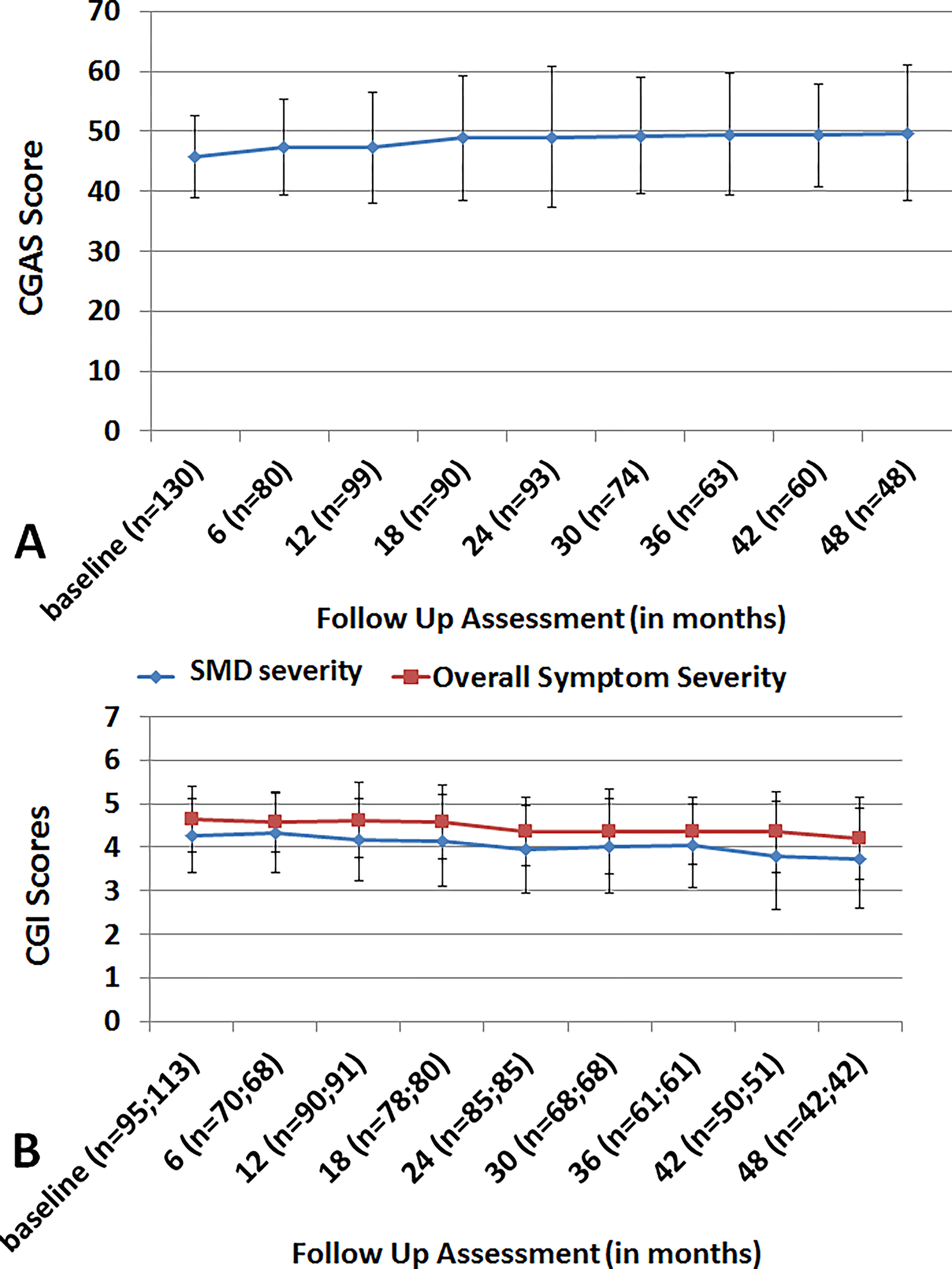
Clinical severity over time. Panel A: Children’s Global Assessment Scale scores at each of the 6 month follow up assessments. Scores between 40 and 50 represent moderate impairment. Panel B: Clinical Global Impressions Scores at each of the 6 month follow up assessments. 1=normal functioning; 7= severe impairment. Overall SMD = impairment due to severe mood dysregulation symptoms. Overall Symptom Severity = impairment due to all psychiatric symptoms. Note: n’s in parentheses refer to the number of available data points at each follow up. For the CGI scores, the first value is the n for SMD severity and the second is the n for Overall Symptom Severity.
Diagnostic Presentation at Initial Evaluation
The most common co-occurring illnesses at initial evaluation were unipolar depressive disorders (primarily major depressive disorder [MDD] and dysthymia), anxiety disorders (primarily separation anxiety disorder, social anxiety disorder [SAD], and generalized anxiety disorder [GAD]), attention deficit hyperactivity disorder [ADHD], and oppositional defiance disorder [ODD] (Figure 4). Youths presented with an average of 3.9 lifetime psychiatric disorders (range 1–8), excluding SMD.
Figure 4.
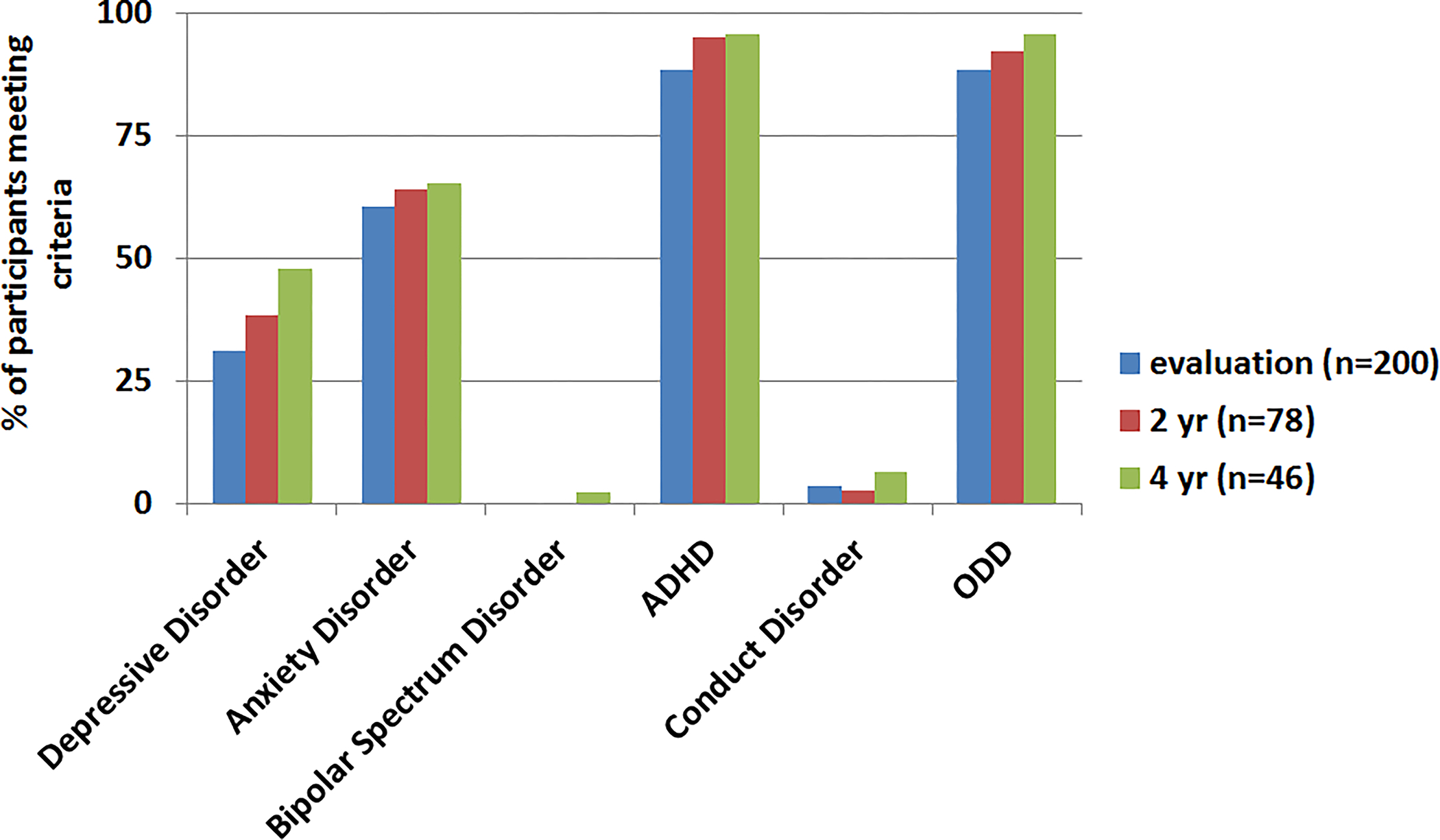
Cumulative lifetime prevalence of Axis I Psychiatric Diagnoses at Each Time Point. The percentage of individuals meeting lifetime criteria for each illness or illness category at each time point. Depressive disorder = MDD, Dysthymia, Depression NOS; Anxiety = Social Phobia, GAD, PTSD, Separation Anxiety Disorder, OCD & Panic Disorder (not specific). Note: At evaluation, 1 person was missing data for Conduct Disorder, ODD and ADHD; therefore the percentage of people meeting criteria was calculated out of 199 patients.
Diagnostic Presentation at 2 and 4 year follow up
Seventy-eight individuals (63.4% of those eligible) returned for the 2-year follow up and 46 individuals (52.3% of those eligible) returned for the 4-year follow up assessments. Lifetime diagnoses and continued need for psychiatric treatment at both points were similar to those in the initial evaluation (Figure 4; Table 1). As with the initial evaluation data, lifetime prevalence rates were highest for depressive disorders, anxiety disorders, ADHD, and ODD at both time points. No participant met criteria for a hypomanic/manic episode at the 2 year follow-up, and a single person (2.2%) met criteria for bipolar disorder (type II) by the 4 year follow up.
Given prior evidence linking childhood irritability with later development of unipolar depression and anxiety (1, 8), we examined rates of “new onsets”, “ongoing illness”, and “remission” of depression and anxiety disorders at each follow up (Figure 5). Depressive and anxiety disorders persisted at the 2 and 4 year follow ups for many, and a number of individuals developed these disorders over time. For example, two youth with no history of any depression in the past experienced a new onset of a depressive disorder by 2 years (5.1% category onset rate). A total of 7 new depression diagnoses (5 MDD; 2 dysthymia) emerged during that time (9.0% illness onset rate). Three additional youth experienced a new onset of any depressive disorder by 4 years (6.5% category onset rate). Four new depression diagnoses (3 MDD; 1 dysthymia) emerged by this time point (8.7% illness onset). The illness category onset rate for anxiety disorders was 7.7% (n=6) at 2 years and 4.3% (n=2) at 4 years. A total of 21 new anxiety disorders (45.7%; 9 SAD; 7 GAD; 4 separation anxiety disorder; 1 PTSD), emerged by the 2 year follow-up and an additional 9 new anxiety diagnoses (19.6%; 5 GAD; 2 SAD; 1 obsessive compulsive disorder; 1 separation anxiety disorder) emerged by the 4 year follow-up.
Figure 5.
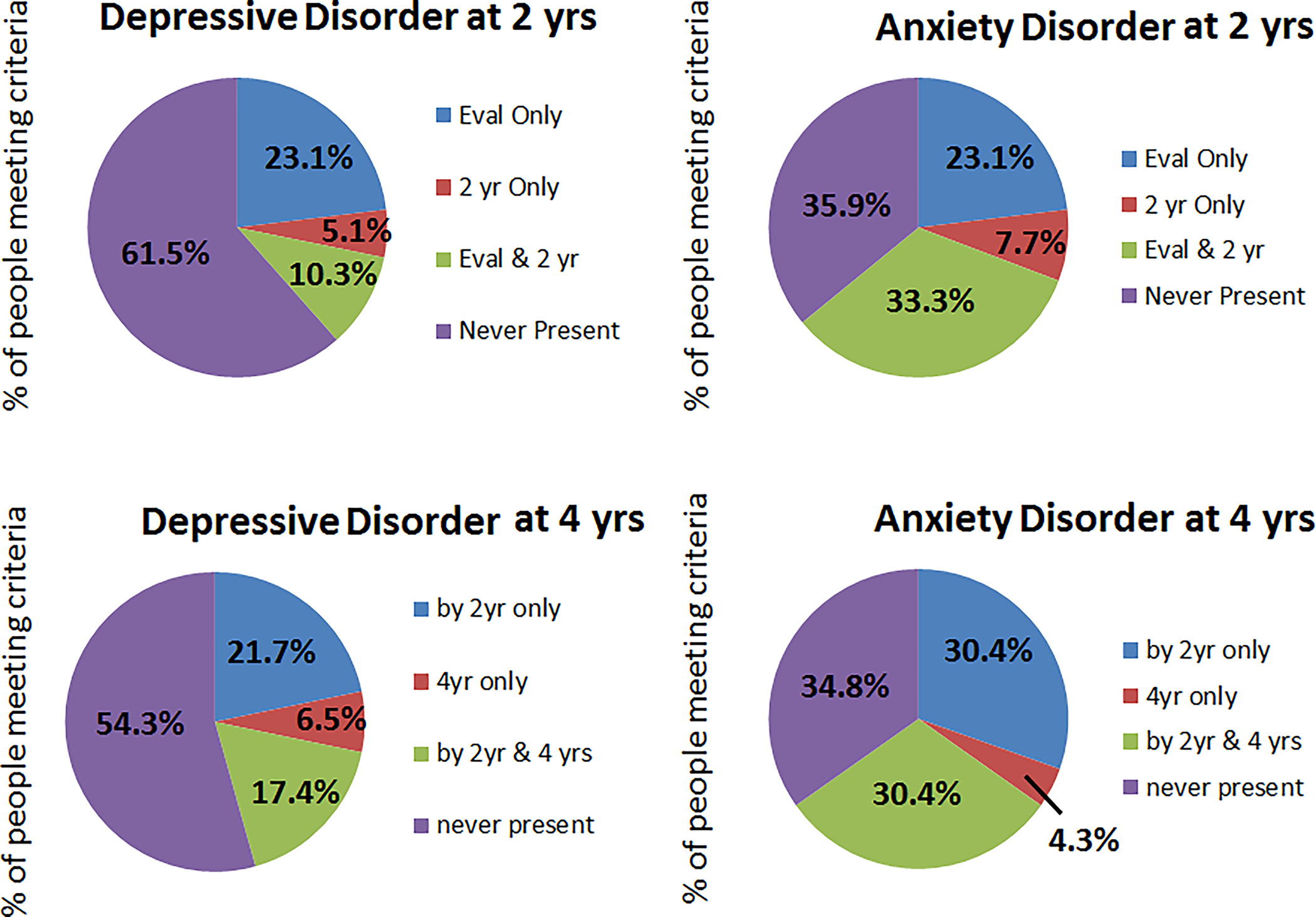
Rates of depressive and anxiety disorders over time. Eval only = diagnosis was only present at the evaluation but criteria were not met during the time period between evaluation and the 2 year follow-up assessment. 2 yr only = diagnosis was not present at the time of the evaluation, but criteria were met between evaluation and the 2 year follow-up assessment. Eval & 2 yr = diagnosis was present at evaluation and criteria continued to be met during the 2 year follow-up period. By 2 yr only = the diagnosis was present by the 2 year assessment (note this percentage could reflect the “eval only”, “2 yr only” and “eval and 2 yr” categories above). 4 yr only = the diagnosis was not present at the initial evaluation or the 2 year follow up, but were met between the 2 and 4 year follow-up assessments. By 2 yr and 4 yrs = criteria were present by the 2 year evaluation and continued to be present during the period between the 2 and 4 year follow-up assessments. Never present = diagnostic criteria were never met.
Discussion
The stability of severe irritability as a psychiatric symptom and its place in psychiatric nosology remain a topic of debate (7, 10, 21). The present study expands upon prior work by prospectively identifying a cohort of youths with severe irritability and conducting rigorous and thorough diagnostic evaluations at two year intervals and regular clinical severity and impairment assessments every 6 months. The majority of youth did not meet strictly defined SMD and DMDD criteria at the 2 and 4 year follow ups. However, most youths continued to exhibit clinically impairing irritability. Indeed, clinical severity ratings (CGI-S) remained in the moderate range across the 4 year interval, indicating that irritability resulted in severe impairment of at least one area of psychosocial functioning or caused moderate impairment in a number of domains. In addition, the majority of youths received psychiatric care at all time points including a substantial proportion of youths taking anti-psychotic medications. These findings speak to the trajectory of severe irritability presenting in childhood, providing data relevant to DMDD. They also suggest the need to identify whether clinical improvement is due to adequate psychiatric treatment or the true remission of symptoms over time.
It is important to highlight several important characteristics about our study participants. First, they traveled from throughout the country to the NIMH to participate in multi-day research visits with no direct benefit to the participants, potentially leading to an ascertainment bias. Second, a large number of participants dropped out during the course of the study. Our retention analyses revealed few demographic and clinical (including parental psychopathology) differences between youths who remained in the study versus those who did not (see supplemental material), although this may reflect limited statistical power. Without clear differences in the retention analyses, it is unclear whether our study underestimates irritability stability because youths with more severe symptoms discontinued the study, or whether it overestimates it because individuals with more severe symptoms were motivated to remain engaged with our research team. The differences observed in our retention analyses suggest that our retained participants might underestimate the severity of the course of irritability or the percentage of new diagnoses developing because they were taking less psychotropic medications at the initial evaluation and were younger than those who dropped out of the study. Finally, series of statistical analyses designed to examine the effects of missing data suggest that participant attrition is unlikely to have an effect on our study findings. In addition, participants were selected based on SMD criteria, which differs slightly from criteria for DMDD, limiting generalizability to other DMDD samples. Since these limitations preclude firm conclusions about the extent to which our findings reflect the unique characteristics of our sample, the findings should be interpreted with caution. An additional limitation is the lack of comparison groups that would help clarify how a) the stability of severe irritability differs from the stability of non-clinical levels of irritability or b) how the stability of severe irritability varies between diagnoses with irritability as the dominant symptom (e.g., SMD or DMDD) versus clinical conditions where irritability is somewhat less pronounced (e.g., GAD). However, this is the first prospectively identified clinical sample of youth with severe irritability to be followed using rigorous diagnostic and clinical assessments over time. Therefore, these data can be used to formulate hypotheses for future research clarifying the longitudinal course and predictors of severe childhood irritability.
Our findings suggest that clinically significant irritability is relatively stable. Only a minority of youths “recover” fully from SMD and decreases in rates of SMD or DMDD over time may reflect the use of a present/not present categorization that classifies individuals with marked, yet categorically sub-threshold, irritability as not having an illness. In addition, across the four years, most youths displayed sustained irritability and moderate impairment that required psychiatric care. The fact that a number of youth continued to display high levels of irritability and impairment, in the absence of meeting full SMD and DMDD criteria, emphasizes the need for dimensional research that identifies empirically-derived cut points that can be used to predict different longitudinal outcomes for childhood irritability. Because a dimensional measure of irritability (such as the Affective Reactivity Index (22)) was not included in the original study methods, we were unable to adopt that approach here. In addition, our use of a population with SMD and operationalization of irritability using items from the SMD module may have obscured our ability to study the stability of irritability as it presents in other illnesses like GAD and ODD. Future work should adopt more rigorous methods like the Multidimensional Assessment of Preschool Disruptive Behavior questionnaire that has been used to identify clinically meaningful cut-points for preschool irritability (23). In addition to clinical measures (including psychiatric treatment history), dimensional neurobiological, genetic, cognitive, and sociodemographic measures (e.g., parental psychopathology, exposure to stress) should be included as possible predictors of individual differences in irritability persistence and remission.
Longitudinal studies of community samples support the association between childhood irritability and unipolar depression and anxiety in adulthood (1, 9, 10, 13, 24). Consistent with those findings, 4–8% of youths developed these disorders during the follow up periods, and the lifetime rates of depressive (39–48%) and anxiety disorders (64–65%) observed were much higher than the rates reported in epidemiologic samples of American youth (25). These data suggest that the incidence of these diagnoses may begin to rise well before the 10 and 20 year follow up assessments examined in other studies (8, 9). In addition, the fact that our participants were younger than the median age of onset for mood disorders and several anxiety disorders (26, 27), suggests that our prevalence rates may represent a conservative estimate, with more youths likely to develop these illnesses as they enter late adolescence and early adulthood. Future studies with this sample will explore this possibility and whether the presence of childhood irritability confers risk in the age of onset of depression and anxiety disorders.
Similarly, the average age of our participants is younger than the typical age of onset for BD (26, 27). Therefore, some subjects in this sample may still go on to develop BD. Nonetheless, the low rate of BD that we observe in children with severe, chronic irritability is consistent with existing studies that fail to demonstrate a link between childhood irritability and mania/hypomania in adulthood (1, 8–10, 13), including at least one that followed adolescents past the typical age of risk for developing BD (8).
Conclusions
The present longitudinal study indicates that severe irritability remains fairly persistent and impairing among youth, although strict diagnostic criteria for SMD are not met by the majority of participants on follow-up. These data highlight the need for more treatment trials to identify effective treatments for severe irritability in youth. Of note, many of these youth receive treatment with atypical antipsychotics, despite the significant side-effects of these medications (28), coupled with limited data for their use in the treatment for irritability (operationalized as disruptive behavior disorders (29)). These youths are also at risk for the development of unipolar depressive disorders and anxiety disorders, but do not show high rates of BD over four years of follow up. These findings represent data upon which future studies of the longitudinal course of irritability and DMDD should be built so that predictors of poor outcomes can be identified and preventative measures employed.
Supplementary Material
Acknowledgments
This research was supported (in part) by the Intramural Research Program of the NIMH. NCT00025935. Protocol 02-M-0021. We gratefully acknowledge the support of the staff of the Emotion and Development Branch, in particular, the dedicated clinicians who conducted all of the assessments. We are also grateful for the time and generosity of our participants and their families.
Footnotes
Note: Ms. Reeves is now at the Counseling Psychology Program at the University of Maryland, Ms. Hinton is now at the Department of Psychology, Vanderbilt University, and Ms. Haring is now at the George Washington University Medical School.
References
- 1.Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60(9):991–7. [DOI] [PubMed] [Google Scholar]
- 2.Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J. Adult outcomes of childhood dysregulation: a 14-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(11):1105–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 2013;170(2):173–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, Maughan B. Predictors of suicidality across the life span: the Isle of Wight study. Psychological medicine. 2010;40(9):1453–66. [DOI] [PubMed] [Google Scholar]
- 5.Andreassi JL. Psychophysiology: Human behavior and psychophysiological response. 3rd ed. Hillsdale, N.J.: Erlbaum; 1995. [Google Scholar]
- 6.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(4):404–12. [DOI] [PubMed] [Google Scholar]
- 7.Axelson D, Findling RL, Fristad MA, Kowatch RA, Youngstrom EA, Horwitz SM, et al. Examining the proposed disruptive mood dysregulation disorder diagnosis in children in the Longitudinal Assessment of Manic Symptoms study. J Clin Psychiatry. 2012;73(10):1342–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166(9):1048–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16(4):456–66. [DOI] [PubMed] [Google Scholar]
- 10.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 2012;169(1):47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Copeland WE, Shanahan L, Egger H, Angold A, Costello EJ. Adult Diagnostic and Functional Outcomes of DSM-5 Disruptive Mood Dysregulation Disorder. Am J Psychiatry. 2014;171(6):668–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leibenluft E Severe Mood Dysregulation, Irritability, and the Diagnostic Boundaries of Bipolar Disorder in Youths. Am J Psychiatry. 2011;168:129–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stringaris A, Baroni A, Haimm C, Brotman M, Lowe CH, Myers F, et al. Pediatric bipolar disorder versus severe mood dysregulation: risk for manic episodes on follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(4):397–405. [PMC free article] [PubMed] [Google Scholar]
- 14.Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS. Defining clinical phenotypes of juvenile mania. Am J Psychiatry. 2003;160(3):430–7. [DOI] [PubMed] [Google Scholar]
- 15.Kaufmann J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children: Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36. [DOI] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York: New York State Psychiatric Insistute, Biometrics Research; 2002. [Google Scholar]
- 17.Guy W Clinical Global Impressions: In ECDEU Assessment Manual For Psychopharmacology. Rockville, M.D.: National Institute of Mental Health; 1976. p. 218–22. [Google Scholar]
- 18.Rothman D, Sorrells J, Heldman P. A Global Assessment Scale for Children. Oakland, C.A.: Alameda County Mental Health Services; 1976. [Google Scholar]
- 19.Luborsky L Clinician’s judgments of mental health. A proposed scale. Archives of general psychiatry. 1962;7:407–17. [DOI] [PubMed] [Google Scholar]
- 20.Hollingshead AB. Two Factor Index of Social Position. 1957.
- 21.Axelson DA, Birmaher B, Findling RL, Fristad MA, Kowatch RA, Youngstrom EA, et al. Concerns Regarding the Inclusion of Temper Dysregulation Disorder With Dysphoria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. J Clin Psychiatry. 2011;72(9):1257–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stringaris A, Goodman R, Ferndinando S, Razdan V, Muhrer EJ, Leibenluft E, et al. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. Journal of child psychology and psychiatry, and allied disciplines. 2012;53(11):1109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, et al. Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(1):82–96 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(5):484–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prevention CfDCa. Mental Health Surveillance Among Children - United States, 2005–2011. MMWR. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- 26.Kessler RC, Angermeyer M, Anthony JC, R DEG, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World psychiatry : official journal of the World Psychiatric Association. 2007;6(3):168–76. [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 28.Vitiello B, Correll C, van Zwieten-Boot B, Zuddas A, Parellada M, Arango C. Antipsychotics in children and adolescents: increasing use, evidence for efficacy and safety concerns. European Neuropsychopharmacology. 2009;19:629–35. [DOI] [PubMed] [Google Scholar]
- 29.Loy JH, Merry SN, Hetrick SE, Stasiak K. Atypical antipsychotics for disruptive behaviour disorders in children and youths (Review). 2012. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


