Abstract
The astounding number of genetic variants revealed in the 15 years of genome-wide association studies of asthma has not kept pace with the goals of translational genomics. Moving asthma diagnosis from a nonspecific umbrella term to specific phenotypes/endotypes and related traits may provide insights into features that may be prevented or alleviated by therapeutical intervention. This review provides an overview of the different asthma endotypes and phenotypes and the genomic findings from asthma studies using patient stratification strategies and asthma-related traits. Asthma genomic research for treatable traits has uncovered novel and previously reported asthma loci, primarily through studies in Europeans. Novel genomic findings for asthma phenotypes and related traits may arise from multi-trait and specific phenotyping strategies in diverse populations.
Keywords: asthma, GWAS, genomics, precision medicine, asthma phenotype, endotype
1. Introduction
Asthma is a major noncommunicable, respiratory disease that affects an estimated 350 million people worldwide and is the most prevalent chronic disease in children globally [1]. It is a heterogeneous and complex disease, characterized by chronic airway inflammation and a history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation [2]. Different environmental, genetic, and behavioral factors interact to modify asthma’s susceptibility and course, which contributes to the disease complexity [2]. Regrettably, despite asthma mortality having decreased in the last decades, still a substantial proportion of asthmatics remain difficult to treat, leading to significant economic consequences, including productivity losses and increased cost of public health expenditure [3,4,5].
Early genetic studies of asthma had limited success in associating genetic variation with asthma susceptibility using linkage analyses in large families with more than one person with asthma, as well as using candidate gene association analyses. Novel genetic signals arose with the advent of genome-wide association studies (GWAS), which are hypothesis-free scans that interrogate genetic variation across the genome for association with a phenotype of interest. Despite GWAS having revealed a large catalog of genetic loci for asthma, the genetic variation uncovered only accounts for a small fraction of asthma heritability, with higher contribution to childhood-onset asthma (33%) than to adult-onset asthma (9.8%), as found in British individuals [6]. Genomic research has investigated several asthma phenotypes or asthma-related traits in an attempt to unravel the complicated etiologic pathways of asthma and features that could be prevented or alleviated by therapeutic interventions such as pulmonary rehabilitation or pharmacological treatment. Here, we provide an overview of the different asthma endotypes and phenotypes along with their clinical characteristics, clinically relevant markers, and molecular mechanisms. We also provide an update on GWAS findings across asthma phenotypes and related traits to identify strategic research opportunities for treatable traits moving forward asthma precision medicine.
2. Asthma Endotypes and Phenotypes
The asthma definition has largely evolved from the early clinical descriptions by Dr. Henry Hyde Salter in the 19th Century [7] to the current understanding of this heterogeneous disease as an umbrella term comprising numerous and different asthma subtypes [8]. A prevailing approach to categorize asthma has been to group patients on observable attributes arising from a complex interplay between hereditary, environmental, and behavioral influences. In fact, the first approach to asthma phenotyping was documented in the late 1940s when Rackemann distinguished between extrinsic—atopic—and intrinsic—unrelated to atopy—asthma [9], and skin tests were often helpful in confirming diagnosis and determining a specific treatment [10]. Since 1999, the clinical and physio-pathological characterization of severe asthmatics—according to the number of eosinophils in the airway—has subsequently inspired a myriad of studies aiming to discriminate between eosinophilic (EA) and non-eosinophilic asthma (NEA). In 2006, Hinks and colleagues assessed the proportion of eosinophils and neutrophils in induced sputum, depicting four asthma phenotypes—EA, NEA, paucigranulocytic asthma (PGA), and mixed-granulocytic asthma (MGA) [11]. Furthermore, gene expression analysis confirmed in 2009, two distinct asthma subgroups—Th2-high and Th2-low—defined by the degree of underlying Th2 inflammation and regardless of patients’ demographic characteristics, lung function, or bronchodilator response [12]. Thus, the definition of the Th2-high asthma phenotype was initially based on atopic predisposition in combination with any of the following surrogate biomarkers for Th2 immune activation: serum immunoglobulin E (IgE) ≥ 100 IU/mL, blood eosinophil count ≥ 300/μL, and exhaled nitric oxide fraction (FENO) ≥ 30 ppb [13]. However, since the production of Th2-related cytokines such as interleukins 4, 5, and 13 (IL-4, IL-5, and IL-13) has been confirmed in further cell populations as type 2 innate lymphoid cells (ILC-2s), mast cells, basophils, and/or eosinophils, the term Th2 has been currently updated to the T2 immune phenotype in asthma [14]. Notably, some of these cytokines may also affect cell counts in asthmatics (i.e., IL5-promoted eosinophilia) [14]. Conventional asthma phenotyping classifies patients according to observable clinical features, including exacerbating factors, age of onset, concomitant comorbidities, and/or response to therapy [15]. As these clinical categories could not discriminate among groups or elucidate the underlying pathobiology, multivariate statistical cluster analysis performed on large asthma cohorts such as SARP [16], U-BIOPRED [17], or ADEPT [18] have greatly contributed to the unbiased description of specific asthma phenotypes [19]. Despite differences in clusters being found, two major groups, namely type 2 (T2)-high and non-T2-high, have been currently defined [20]. These evolving endotypes—associating plausible molecular and cellular mechanisms or therapeutic response to phenotypes—have, nowadays, pioneered asthma into the age of precision medicine [21,22].
2.1. T2-High Asthma
In T2-high asthma, the interaction of the airway epithelium with the external exposome activates the release of specific mediators—epithelial-derived alarmins—as thymic stromal lymphopoietin (TSLP), IL-25, and IL-33, leading to the production of IL-4, IL-5, and IL-13 [23]. Subsequent tT2 immuno-responses include IgE-mediated hypersensitivity to aeroallergens, chemoattraction of mast cells, eosinophils, and basophils, and remodeling of the airway epithelium [14]. T2-high asthma has been clinically classified into three phenotypes, including early-onset allergic asthma, late-onset eosinophilic asthma, and nonsteroidal anti-inflammatory drugs (NSAIDs)-exacerbated respiratory disease (NERD) [20,24].
2.1.1. Early-Onset Atopic Asthma
The early-onset atopic asthma phenotype—most frequently identified in former hierarchical clustering analysis—is predominant in children, responsive to inhaled steroids, and commonly associated with increased T2 cytokines, serum-specific IgE to inhalants, and allergic comorbidities, i.e., allergic rhinitis, atopic dermatitis, and/or food allergy, with a relevant participation in the “atopic march” [8,25]. Multiple environmental factors, including allergens, viral infections, pollutants, and/or cigarette smoke, have been described as potential triggers to activate inflammatory responses, leading to clinical symptoms concerning this asthma phenotype [26,27,28]. Despite asthma symptoms—with variations in severity—that are elicited during childhood and may be resolved in adolescence, this phenotype can persist through life [19,29].
2.1.2. Late-Onset Eosinophilic Asthma
Late-onset eosinophilic asthma phenotype usually starts in adulthood, and its underlying pathobiology is also driven by a preponderant T2 inflammation response with apparently no evidence of atopy but the leading role of ILC-2 in the production of IL-5 and IL-13 [30]. Although this phenotype may show different clinical presentations, including comorbid chronic rhinosinusitis with and without nasal polyps, a significant proportion of patients are older and have a more severe disease, lower pulmonary function, increased blood and sputum eosinophils, and are partially responders to inhaled or systemic steroids [31,32].
2.1.3. Nonsteroidal Anti-Inflammatory Drugs-Exacerbated Respiratory Disease (NERD)
NERD is considered as a subset of the late-onset eosinophilic asthma phenotype—frequently associated with chronic rhinosinusitis with nasal polyps (CRSwNP)—presenting with rapid respiratory exacerbations immediately triggered after the intake of aspirin or other NSAID drugs that inhibit the cyclooxygenase-1 isoenzyme (COX-1). Despite the complete underlying pathogenic mechanism remaining unclear, NERD is characterized by a dysregulation in the arachidonic acid metabolism and a marked overproduction of cysteinyl leukotrienes (cysLTs), a potent lipid inflammatory mediator derived from arachidonic acid [33,34]. Mast cells, eosinophils and platelet-adherent leukocytes, which are present in the respiratory tissue of subjects with NERD have functional 5-lipoxygenase (5-LOX) and leukotriene (LT) C4 synthase enzymes [35]. Arachidonic acid is oxidized by 5-LOX to form short-lived LT mediators, such as LTC4, LTD4, and the stable metabolite LTE4 that has been formerly described as a biomarker in patients with NERD [36,37,38]. Interestingly, innate type 2 mediators from epithelial cells can be also activated after stimulation with cysLTs and further amplified by mast-cell-derived prostaglandin D2 gene (PGD2), leading to the persistent eosinophilic airway inflammation, bronchoconstriction, and mucus secretion related to refractory nasal polyposis and asthma [39,40].
2.2. T2-Low Asthma
Clinically, T2-low asthma—accounting for 33 to 50% of the asthmatics—has been grouped according to obesity, smoking exposure, and age. T2-low asthma is characterized by the activation of non-T2 inflammatory pathways, including helper T-lymphocytes type 1 (Th1) and/or Th17 cells, IL-6, IL-8, IL-17, and IL-22, and epithelial-derived cytokines [41,42]. Despite no validated biomarkers having been confirmed yet, sputum cytology has defined different subsets for T2-low asthma: neutrophilic (sputum neutrophils > 40–60%) and paucigranulocytic (normal sputum levels of neutrophils and eosinophils) asthma [43]. Patients with T2-low asthma usually develop symptoms at adulthood, and they are frequently associated with obesity, cigarette smoke exposure, lower bronchodilator reversibility, chronic infection with atypical bacteria, and a limited response to inhaled and systemic steroids in combination with a metabolic dysfunction [44,45,46]. Comorbidities such as hypertension and diabetes are frequent in this subset of patients with lower lung function and increased blood IL-6 levels, which has been considered a putative biomarker for metabolic dysfunction [22,47].
PGA has been identified as a milder respiratory phenotype in terms of severity, number of clinically relevant exacerbations, and improved lung function compared to EA and neutrophilic asthma (NA) [48]. Patients with PGA show lower levels of biomarkers of both eosinophilic—blood and sputum eosinophils, serum periostin, eosinophilic cationic protein (ECP), and FENO—and neutrophilic inflammation—serum matrix metalloproteinase-9 (MM-9), and IL-8 [48,49]. Despite the immunopathological underlying mechanisms not having been elucidated yet, PGA is characterized by increased airway smooth muscle dysfunction—hyperplasia and hypertrophy—leading to chronic airflow obstruction and release of inflammatory mediators due to specific neurogenic pathways [50,51]. As no biological treatment is available for T2-low asthma, alternative therapy targeting airway smooth muscle dysfunction including mitogen-activated protein kinase inhibitors, tyrosine-kinase inhibitors, phosphatidylinositol 3 kinase inhibitors, or phosphodiesterase inhibitors is currently under investigation [52,53,54].
2.2.1. Obesity-Associated Asthma
Obesity-associated asthma is a complex asthma phenotype more frequently described in nonatopic middle-aged females, presenting with severe respiratory symptoms and a relatively preserved pulmonary function [55,56]. Interestingly, the inflammatory response in obesity is associated with a switch from Th2 cells to Th1, Th17, and cytotoxic T lymphocytes [57]. In addition, the levels of specific cytokines have been positively related to body-mass index (BMI) [58]. Further innate inflammatory pathways involving ILC-3s expressing IL-17 and IL-22 have been also described in obesity-associated asthma [59]. The proinflammatory cytokine IL-6, produced in adipocytes and adipose tissue macrophages, has been associated with obese T2-low asthma but not with obese atopic asthma [59,60]. Moreover, a reduction in arginine and nitric oxide (NO) bioavailability has been related to the increased oxidative stress occurring both in obesity and obese adults with the late-onset asthma phenotype [61].
2.2.2. Smoking-Associated Asthma Phenotype
The estimated prevalence of smokers within asthmatics—about 20%—is similar to that found in the general population [62,63]. Cigarette smoking in asthmatics has been previously related to poor control of symptoms, increased mortality, declined pulmonary function, lower response to steroids, and increased healthcare costs [64,65,66]. The recognition of a smoking-associated asthma phenotype has relevant implications to an improved management of patients afflicted with this specific asthma subtype. In this regard, smoking-associated asthma is considered a T2-low neutrophilic phenotype speculating that persistent exposure to cigarette smoke may induce a predominance of activated macrophages producing proinflammatory molecules, reactive oxygen species, matrix metalloproteinases, and specific chemokines such as IL-8, contributing to the prolonged survival of neutrophils in the lung tissue [67]. In addition, cigarette smoke increases total IgE levels and the risk of sensitization to aeroallergens, thus enhancing a combined Th1/Th2 inflammatory response developing a more severe asthma phenotype and a putative link between asthma and chronic obstructive pulmonary disease (COPD) in subjects with a relevant smoking history, airflow obstruction, and overlapping features of asthma, termed asthma–COPD overlap syndrome (ACO) [53,68,69].
2.2.3. Elderly-Associated Asthma Phenotype
The age cutoff value in this underdiagnosed and sub-optimally treated very-late-onset asthma phenotype is >65 years [70]. Age-related changes in the lung structure such as airway narrowing, reduced elastic recoil, or alveolar dilation may lead to an overall decreased pulmonary function [71,72]. Although the pathobiology of this phenotype has not been totally elucidated the preponderant airway neutrophilic inflammation has been related to both Th1 and Th17 responses [73,74].
2.3. Overlapping in Asthma Phenotypes
An elevated rate of overlapping—above 70%—has been described in mild-to-severe asthmatics, including combinations among different inflammatory asthma phenotypes, such as T2-high, T2-low, and mixed T2/non-T2 [75] (Table 1). In this regard, occupational asthma (OA), a subtype of work-related asthma, currently shows as a challenging respiratory model to clinical phenotyping. As both high-molecular-weight (HMW) proteins and low-molecular-weight (LMW) chemicals can elicit OA, different clinical, physiological, and inflammatory profiles have been described, with HMW agents showing a higher baseline blood eosinophilia and a greater post-challenge elevation in associated FENO levels [76,77]. In fact, asthma has been proposed as a nonlinear complex dynamic system with both clinical and therapeutic implications, suggesting an evolution in the underlying inflammatory status from an initial T2-high profile moving towards an alternative T2-low or mixed T2/non-T2 asthma phenotype [78,79,80].
Table 1.
Overview of asthma endotypes and phenotypes.
| Endotype | Phenotype | Clinical Features | Molecular Mechanism | References |
|---|---|---|---|---|
| T2-high asthma | Early-onset atopic asthma | Trigger-induced phenotypes. Steroid-sensitive. Preserved lung function | Allergy to aeroallergens | [8,13,14,19,25,26,27,28,29] |
| Late-onset eosinophilic asthma | CRSwNP frequently associated. Steroid-refractory |
Staphilococcus aureus enterotoxin | [11,12,30,31,32] | |
| NERD | Samter´s Syndrome. Adult onset. Trigger-induced phenotypes | Arachidonic acid dysregulation | [33,34,35,36,37,38,39,40] | |
| T2-low asthma | Non-atopic asthma | Neutrophilic or paucigranulocytic. | Th1/Th17 inflammation | [22,41,42,43,44,45,46,47,48,49,50,51,52,53,54] |
| Adult onset | ||||
| Smoking-associated asthma | Adult onset. Lower lung function | Oxidative stress | [62,63,64,65,66,67] | |
| Obesity-associated asthma | Metabolic syndrome. Females. Preserved lung function |
Th1/Th17 inflammation. Oxidative stress. IL-6 |
[55,56,57,58,59,60,61] | |
| Elderly-related asthma | Very late onset. Declined lung function | Th1/Th17 inflammation | [70,71,72,73,74] |
3. Genomic Studies
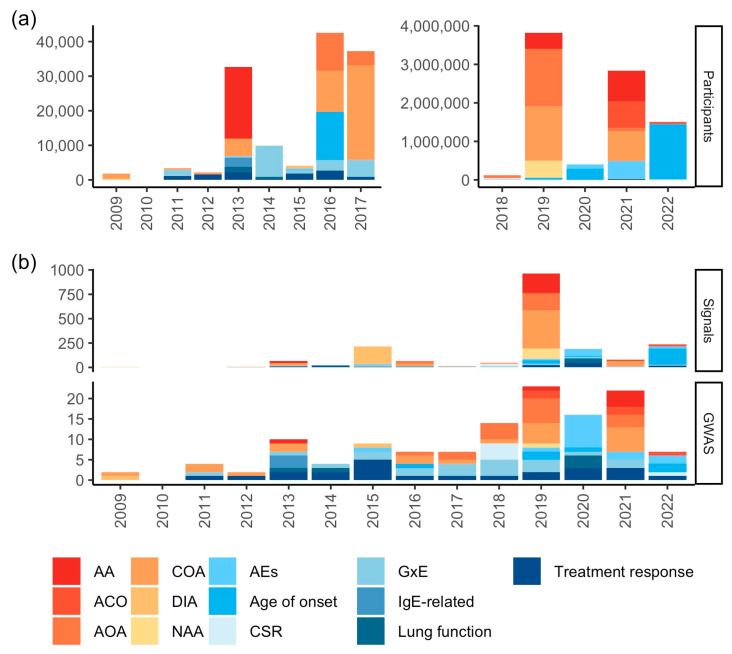
Among genomic studies, GWAS have uncovered a plethora of associations for several diseases and complex human traits and diseases, mainly comprising common genetic variants (usually with a minor allele frequency (MAF) ≥ 1%) of low-to-moderate effect sizes (~0.8 < odds ratio (OR) < ~1.3 for most asthma-related variants) [6,81]. GWAS findings regarding asthma phenotypes and related traits were characterized by querying the latest version of the NHGRI-EBI GWAS Catalog [82] as detailed in Appendix A. As of 7 April 2023, the NHGRI-EBI GWAS Catalog encompasses 31 publications related to asthma phenotypes spanning 52 unique study accession numbers—trait-specific analyses conducted within each publication—across 24 unique outcomes and 973 unique associations. In addition, a total of 51 publications of asthma-related traits comprised 76 unique study accession numbers, 61 unique outcomes, and 464 unique associations. Overall, the outburst of GWAS with a growing number of participants has risen the number of identified genetic signals, except in 2021, when the analysis of more than 2.8 million individuals revealed less than 80 associations across outcomes (Figure 1a,b). The maximum number of GWAS participants included in the discovery stage for an asthma phenotype was 601,193 (for childhood-onset asthma (COA) in Europeans and Japanese [83]), while it amounts up to 730,758 for asthma-related trait findings (specifically, for age of onset in ethnically diverse individuals [84]).
Figure 1.
Characteristics and findings from GWAS of asthma phenotypes and related traits over time, 2009–2022, as curated by the NHGRI-EBI GWAS Catalog. (a) Maximum number of participants in the discovery GWAS stage; (b) number of associations and GWAS. Abbreviations: AA: allergic asthma; ACO: asthma–chronic obstructive pulmonary disease overlap syndrome; AEs: asthma exacerbations; AOA: adult-onset asthma; COA: childhood-onset asthma; CSR: asthma control, severity, or remission; DIA: diisocyanate-induced asthma; GxE: gene–environment interaction; IgE: immunoglobulin E; NAA: nonatopic asthma.
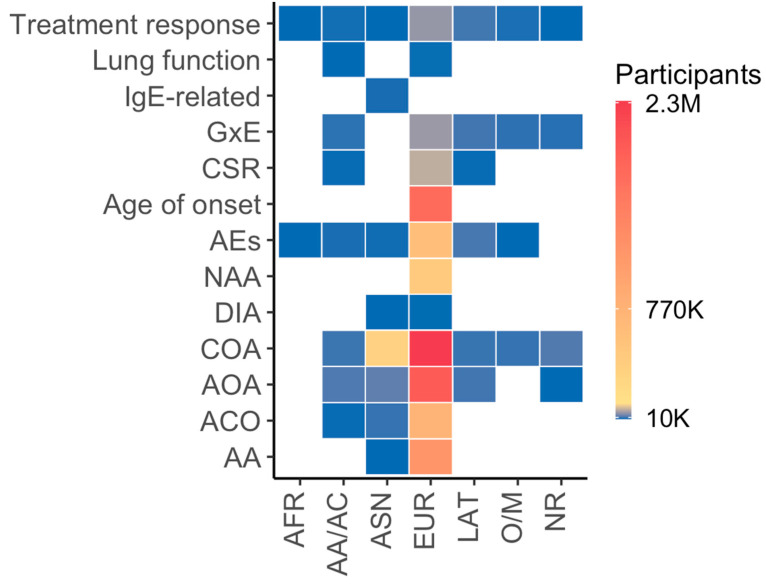
Asthma phenotypes have been widely investigated in Europeans compared with other ancestry groups and asthma-related traits (Figure 2), largely due to the contribution of the population-based United Kingdom Biobank (UKB). Furthermore, asthma-related traits remain widely unexplored across diverse populations, partially because these data might have not been extensively collected in population-based studies. Notably, African populations are poorly represented in both GWAS of asthma phenotypes and related traits. Nevertheless, African-admixed populations, mainly African Americans, have been included in genetic studies of asthma phenotypes and related traits for which African Americans exhibit differential profiles in comparison with other ancestry groups (e.g., asthma exacerbations, treatment response, or lung function). Across all outcomes, lung function, IgE-related phenotypes, asthma control, severity or remission, age of asthma onset, and nonatopic asthma are the least investigated across ancestry groups. Conversely, asthma exacerbations and treatment response have been investigated across most of the ancestry groups, despite the modest sample sizes compared to GWAS of asthma phenotypes in Europeans. Similarly, gene–environment interactions still lag behind compared to GWAS of asthma phenotypes, possibly due to the even large sample size required to detect interaction signals after multiple comparison testing (Figure 2).
Figure 2.
Outcome distribution per “broad” ancestry category and number of participants in GWAS of asthma phenotypes and related traits over time, 2009–2022, as curated by the NHGRI-EBI GWAS Catalog. Abbreviations: AA: allergic asthma; ACO: asthma–chronic obstructive pulmonary disease overlap syndrome; AA/AC: African American or Afro-Caribbean; AEs: asthma exacerbations; AFR: African; AOA: adult-onset asthma; ASN: Asian; COA: childhood-onset asthma; CSR: asthma control, severity, or remission; DIA: diisocyanate-induced asthma; EUR: European; GxE: gene–environment interaction; IgE: immunoglobulin E; LAT: Hispanic/Latin American; NAA: nonatopic asthma; NR: not reported; O/M: Other/Mixed.
3.1. Genomic Studies of Asthma Phenotypes
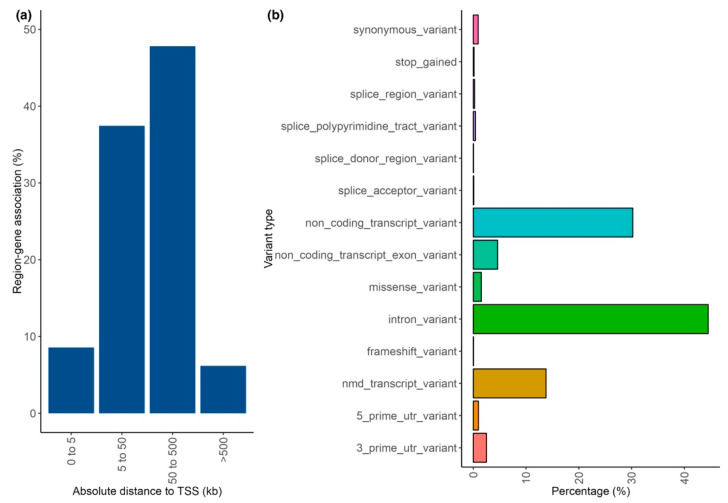
Most GWAS variants from asthma phenotype studies annotate to distal noncoding regions far from the transcription start site (TSS) of the closest gene (less than 500 kb). Functionally, most variants had consequences over introns, noncoding transcripts, or transcripts affected by nonsense-mediated mRNA decay (Figure 3a,b).
Figure 3.
Annotation of genetic variants for asthma phenotypes. (a) Absolute distance (in kilobases) between genetic variants and the transcription start site (TSS) of the nearest gene; (b) variant effect type according to the Sequence Ontology term. Abbreviations: kb: kilobases; NMD: nonsense-mediated mRNA decay: TSS: transcription start site: UTR: untranslated region.
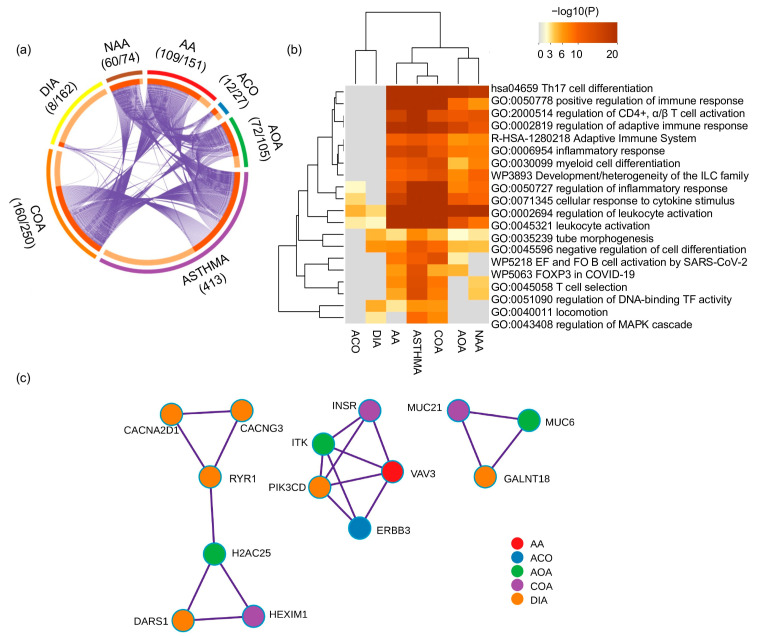
COA and allergic asthma (AA) showed the highest gene overlap with asthma and cluster closely in terms of biological processes and pathways, while toluene diisocyanate-induced asthma (DIA) and ACO show the largest divergence (Figure 4a,b). The most shared terms in the enrichment analyses were related to inflammatory and adaptative immune responses (Figure 4b). A protein–protein interaction network of the most densely connected network components for asthma phenotypes prioritized three subnetworks (Figure 4c). The first subnetwork comprised four DIA, one COA, and one adult-onset asthma (AOA)-related genes implicated in calcium transport (CACNG3, CACNA2D1, and RYR1) or transcriptional/translational control (DARS1, H2AC25, and HEXIM1). The second subnetwork comprised five genes implicated in B-/T-cell receptor and PI3K/AKT signaling pathways (ERBB3, ITK, INSR, PIK3CD, and VAV3). The third subnetwork harbored three genes implicated in O-linked glycosylation of mucins (GALNT18, MUC6, and MUC21). None of these sub-networks contained NA-related genes.
Figure 4.
Genetic findings of asthma phenotypes. (a) Circos plot depicting the overlap of genes annotated based on the genetic variation associated across asthma phenotypes. The outer arc represents the identity of each gene list, whereas the inner arc represents a gene list, where each gene member of that list is assigned a spot on the arc. The dark orange color represents the genes shared by multiple gene lists, and light orange color represents genes specific to that gene list. The number of genes overlapping between each gene list and the 413 genes from the asthma gene list and the total number of genes within each gene list are shown along with each phenotype term. (b) Gene-set enrichment analysis of asthma and asthma phenotype-related genes. (c) Prioritized subnetworks for distinct genes for asthma phenotypes. Abbreviations: AA: allergic asthma; ACO: asthma–chronic obstructive pulmonary disease overlap syndrome; AOA: adult-onset asthma; COA: childhood-onset asthma; DIA: diisocyanate-induced asthma; EF: extrafollicular; FO: follicular; NAA: nonatopic asthma; TF: transcription factor.
3.2. Genomic Studies of Asthma-Related Traits
In recent years, great efforts have been made to characterize the genetic determinants of asthma treatment response and exacerbations, particularly in genetically admixed and historically minoritized populations disproportionately affected by asthma. Since genomic findings for asthma treatment response, asthma exacerbations, or gene–environment interactions have been recently reviewed elsewhere [85,86,87,88], this review will focus on age of asthma onset, moderate-to-severe asthma, asthma remission, T2-low asthma, as well as lung function, total IgE levels, and eosinophil-specific proteins in asthma.
Overall, 10 GWAS of asthma-related traits have been published (Table 2), primarily in European populations, except for GWAS of total serum and mite-specific IgE levels in East Asian individuals. Three GWAS [89,90,91] have investigated the association with age of asthma onset as a linear measurement. A GWAS meta-analysis of 5462 individuals with asthma and 8424 individuals without asthma [89] associated four stablished asthma loci with the age of asthma onset (2q12, 6p21, 9p24, and 17q12–q21) and found a novel association at locus 16q12. Moreover, in a GWAS including 37,846 patients with asthma [90], 19 loci were genome-wide associated with age of asthma onset, along with the genomic regions 2q12 and 9p24, previously detected [89]. Furthermore, a recent study [91] in 25,240 individuals with asthma uncovered novel significant genome-wide signals near genes implicated in the regulation of transcription (TEF), cell growth (MUCL3), and the prognosis of non-small-cell lung carcinoma (SFTA2) [92].
In terms of asthma severity, the largest genome-wide association study of moderate-to-severe asthma published to date identified three novel signals that regulate mucin production (rs10905284, rs11603634, and rs560026225) and validated 24 prior signals for mild asthma [93]. From the three novel signals, the SNP rs11603634 was specific to moderate-to-severe asthma. Moreover, a whole-genome sequencing association study of asthma severity in Europeans evidenced eight genome-wide significant loci previously reported as associated with asthma (IL1RL2, TSLP, HLA-DQA1, BACH2, C11orf30, RAD51B, and GSDMB) and lung function (THSD4) [94]. The inverse genetic correlation between moderate-to-severe asthma risk and lung function (rg < −0.16) provides genetic support for a role of lung function in moderate-to-severe asthma risk. In this sense, only two GWAS of pulmonary function among individuals with asthma have been performed [95,96], focused mainly on Europeans. One study focused only on longitudinal FEV1 in children with asthma that received placebo and with data collected every 2–4 months in a 4-year period. Their work revealed seven suggestively associated SNPs that replicated in individuals that underwent nedocromil treatment (Table 1) [95]. Another study found replication for 7 out of 28 lung function loci (HHIP, FAM13A, THSD4, GSTCD, NOTCH4-AGER, RARB, and ZNF323) previously identified in the general population (p-value < 0.05) supporting a shared basis between phenotypes [96].
Although there are treatments to control asthma symptoms, as of today, there is no cure for asthma. Nonetheless, some individuals with asthma experience remission of their symptoms, which is more common in children than in adults [97]. The first and only GWAS of asthma remission to date [97] reported 25 SNPs suggestively associated in 790 Dutch adults (p-value < 2.5 × 10−4). Four of those associations were replicated in European adults (n = 1132). The top-hit, rs6581895, was found to be an expression quantitative trait locus (eQTL) of FRS2 and CCT2 in lung tissue. FRS2 encodes a protein that belongs to the FRS2 family of adaptor/scaffold proteins and inhibits EGF signaling, which leads to an inhibition of EGF-induced cell proliferation and cell transformation. CCT2 encodes a molecular chaperone which is part of the TCP1 ring complex (TRiC) and participates in the maintenance of cell proliferation. Genetic variants in these genes have been associated with albuminuria [98], which was recently associated with a greater decline in lung function [99]. Nevertheless, considering asthma as a risk factor for renal dysfunction remains controversial [100].
Nowadays, the inflammatory microenvironment in the lower airway remains unclear. Since the identification of biomarkers associated with T2 inflammation, one of the approaches used is to differentiate patients with T2-high from those who have T2-low asthma [20]. The only GWAS of T2-low adult asthma (n = 1350) revealed a genome-wide significant association (rs117639512, OR for A allele = 0.33, p-value = 2.75 × 10−8) in the intergenic region between kallikrein-related peptidase 4 (KLK4) and kallikrein-related peptidase 5 (KLK5) genes [101].
Although several GWAS have investigated genetic factors of IgE levels, only one GWAS of IgE levels in individuals with asthma has been conducted [102]. The analysis of 877 East Asians highlighted suggestive associations in CRIM1, ZNF71, TLN1, and SYNPO2 that had not been previously associated with IgE in non-asthmatic individuals. However, these regions remain to be validated in independent studies to assess their potential interest as clinical markers. Notably, gene expression variation of SYNPO2 has been previously associated with airway hyperresponsiveness in patients with asthma [103]. Similarly, although no GWAS of eosinophil counts has been conducted in asthma patients, two eosinophil-specific proteins released during allergic response have been studied in asthmatic families: ECP and eosinophil-derived neurotoxin (EDN) [104]. This study identified seven distinct signals located in five loci (1p31, 2p13, 7p21, 9q22, and 14q11) associated with ECP and EDN levels and/or the combination of both phenotypes in adults of asthma-ascertained families.
Table 2.
Summary of independent genetic signals from GWAS of asthma-related traits.
| Phenotypes | SNP | Chr. Region a | Genomic Context | Effect Allele | Coefficient Type | Coefficient Value | p-Value | References |
|---|---|---|---|---|---|---|---|---|
| Asthma age onset | rs10208293 | 2q12 | IL1RL1 | G | HR | 1.14 | 3.1 × 10−8 | [89] |
| rs9272346 | 6p21 | HLA-DQA1 | A | HR | 1.13 | 1.6 × 10−8 | ||
| rs928413 | 9p24 | IL33 | G | HR | 1.19 | 6.5 × 10−16 | ||
| rs1861760 | 16q12 | CYLD | A | HR | 1.28 | 4.2 × 10−8 | ||
| rs9901146 | 17q12-q21 | ZPBP2/GSDMB | G | HR | 1.18 | 1.9 × 10−16 | ||
| rs61816761 | 1q21.3 | FLG | A | beta | −4.57 | 8.15 × 10−27 | [90] | |
| rs7518129 | 1q25.1 | TNFSF4 | G | beta | −0.85 | 4.89 × 10−9 | ||
| rs3771175 | 2q12.1 | IL1RL1 | T | beta | −1.73 | 7.66 × 10−17 | ||
| rs10187276 | 2q36.3 | SNRPGP8/CCL20 | T | beta | −0.87 | 1.98 × 10−8 | ||
| rs78147778 | 2q37.3 | D2HGDH | T | beta | −0.91 | 1.64 × 10−8 | ||
| rs2889896 | 3q28 | LPP | C | beta | −0.98 | 8.07 × 10−13 | ||
| rs5743618 | 4p14 | TLR1 | C | beta | −1.58 | 4.53 × 10−22 | ||
| rs4705962 | 5q31.1 | KIF3A | T | beta | −0.99 | 5.57 × 10−10 | ||
| rs12207974 | 6p21.33 | HLA-E/RANP1 | C | beta | −1.07 | 8.86 × 10−11 | ||
| rs1093 | 6p21.33 | HLA-B | G | beta | −0.99 | 8.41 × 10−10 | ||
| rs9274659 | 6p21.32 | HLA-DQB1/MTCO3P1 | A | beta | −1.25 | 6.71 × 10−18 | ||
| rs7848215 | 9p24.1 | IL33 | T | beta | −1.03 | 7.51 × 10−12 | ||
| rs117137535 | 9q34.3 | ARRDC1 | A | beta | −2.46 | 3.42 × 10−8 | ||
| rs61894547 | 11q13.5 | EMSY | T | beta | −2.23 | 4.42 × 10−15 | ||
| rs12365699 | 11q23.3 | CXCR5/DDX6 | G | beta | −1.40 | 4.42 × 10−14 | ||
| rs4795399 | 17q12 | GSDMB | T | beta | −2.29 | 6.76 × 10−65 | ||
| rs11658582 | 17q21.2 | CCR7/SMARCE1 | G | beta | −0.91 | 1.37 × 10−10 | ||
| rs4574025 | 18q21.33 | TNFRSF11A | T | beta | −0.87 | 1.61 × 10−10 | ||
| rs12964116 | 18q21.33 | SERPINB7 | G | beta | −1.92 | 4.87 × 10−8 | ||
| rs5758324 | 22q13.2 | TEF | G | HR | 1.06 | 2.39 × 10−8 | [91] | |
| rs2844649 | 6p21.33 | SFTA2/MUCL3 | A | HR | 1.08 | 4.45 × 10−8 | ||
| Asthma severity | rs560026225 | 4q27 | KIAA1109 | GATT | OR | 1.12 | 3.06 × 10−9 | [93] |
| rs10905284 | 10p14 | GATA3 | A | OR | 0.90 | 1.76 × 10−10 | ||
| rs11603634 | 11p15.5 | MUC5AC | G | OR | 1.09 | 2.32 × 10−8 | ||
| rs7523907 | 1q24.2 | CD247 | T | OR | 1.10 | 4.82 × 10−9 | ||
| rs12479210 | 2q12.1 | IL1RL1 | T | OR | 1.19 | 1.57 × 10−29 | ||
| rs34290285 | 2q37.3 | D2HGDH | A | OR | 0.84 | 2.24 × 10−23 | ||
| rs1837253 | 5q22.1 | TSLP | C | OR | 1.19 | 1.95 × 10−22 | ||
| rs1438673 | 5q22.1 | WDR36 | T | OR | 0.89 | 3.29 × 10−13 | ||
| rs3749833 | 5q31.1 | C5orf56 | C | OR | 1.14 | 5.60 × 10−14 | ||
| rs1986009 | 5q31.1 | RAD50 | A | OR | 1.17 | 2.43 × 10−15 | ||
| rs9273410 | 6p21.32 | HLA-DQB1 | A | OR | 1.21 | 5.62 × 10−32 | ||
| rs144829310 | 9p24.1 | IL33 | T | OR | 1.21 | 2.29 × 10−20 | ||
| rs7936312 | 11q13.5 | C11orf30 | T | OR | 1.17 | 6.18 × 10−24 | ||
| rs703816 | 12q13.3 | STAT6 | C | OR | 1.12 | 3.69 × 10−13 | ||
| rs10519068 | 15q22.2 | RORA | A | OR | 0.85 | 1.84 × 10−12 | ||
| rs72743461 | 15q22.33 | SMAD3 | A | OR | 1.14 | 4.52 × 10−14 | ||
| rs7203459 | 16p13.13 | CLEC16A | C | OR | 0.86 | 4.37 × 10−18 | ||
| rs2941522 | 17q12 | IKZF3 | T | OR | 1.11 | 2.32 × 10−12 | ||
| rs139210940 | 2q12.1 | IL1RL2 | AT | OR | 1.34 | 8.08 × 10−9 | [94] | |
| rs10455025 | 5q22.1 | TSLP | C | OR | 1.30 | 4.36 × 10−13 | ||
| rs17205170 | 6p21.32 | HLA-DQA1 | G | OR | 1.45 | 7.92 × 10−16 | ||
| rs2875584 | 6q15 | BACH2 | C | OR | 1.24 | 1.57 × 10−8 | ||
| rs7130588 | 11q13.5 | C11orf30 | G | OR | 1.24 | 2.46 × 10−9 | ||
| rs2104047 | 14q24.1 | RAD51B | T | OR | 1.25 | 1.28 × 10−8 | ||
| rs11631778 | 15q23 | THSD4 | G | OR | 1.23 | 3.54 × 10−8 | ||
| rs7216558 | 17q12 | GSDMB | T | OR | 1.26 | 1.91 × 10−11 | ||
| Pulmonary function | ||||||||
| FEV1 | rs559389 | 11q13.4 | - | C | beta | −0.03 | 5.28 × 10−5 | [95] |
| rs9366309 | 6p22.3 | - | T | beta | −0.03 | 3.32 × 10−5 | ||
| rs6763931 | 3q23 | ZBTB38 | A | beta | 0.03 | 5.90 × 10−5 | ||
| rs2304725 | 3p25.3 | SLC6A11 | C | beta | 0.03 | 3.87 × 10−5 | ||
| rs17161791 | 7p21.3 | - | C | beta | 0.002 | 3.01 × 10−5 | ||
| rs10795348 | 10p13 | C10orf97 | T | beta | 20.16 | 5.07 × 10−5 | [96] | |
| rs10951730 | 7p13 | HECW1 | A | beta | 20.24 | 9.58 × 10−5 | ||
| rs1291183 | 18p11.32 | YES1 | T | beta | 20.18 | 3.54 × 10−5 | ||
| rs1321267 | 6q23.2 | MOXD1 | A | beta | 20.14 | 5.46 × 10−5 | ||
| rs1843593 | 4q13.2 | GNRHR | T | beta | 20.20 | 5.30 × 10−5 | ||
| rs2040403 | 22q12.3 | SYN3 | A | beta | 0.29 | 1.96 × 10−5 | ||
| rs2063485 | 3q13.11 | ZPLD1 | T | beta | 0.23 | 7.18 × 10−5 | ||
| rs285461 | 1q23.3 | LRRC52 | T | beta | 0.22 | 9.56 × 10−5 | ||
| rs3010301 | 6q24.1 | CITED2 | T | beta | 0.17 | 2.65 × 10−5 | ||
| rs3756089 | 4q35.1 | IRF2 | T | beta | 0.26 | 8.79 × 10−5 | ||
| rs3805383 | 4q12 | NMU | A | beta | 20.17 | 2.35 × 10−5 | ||
| rs388159 | 19p13.11 | IL12RB1 | T | beta | 0.19 | 3.47 × 10−5 | ||
| rs4234121 | 2q37.3 | KIF1A | A | beta | 20.15 | 3.25 × 10−5 | ||
| rs4651208 | 1q25.3 | C1orf21 | T | beta | 20.15 | 6.34 × 10−5 | ||
| rs4735916 | 8p23.3 | ERICH1 | A | beta | 20.24 | 7.02 × 10−5 | ||
| rs5755023 | 22q12.3 | LARGE | A | beta | 20.21 | 1.75 × 10−5 | ||
| rs58667 | 22q13.31 | UPK3A | A | beta | 0.18 | 3.95 × 10−7 | ||
| rs6788848 | 3q13.11 | ZPLD1 | T | beta | 20.18 | 4.99 × 10−5 | ||
| rs7434819 | 4q32.1 | C4orf18 | A | beta | 20.14 | 7.34 × 10−5 | ||
| rs7670758 | 4q31.21 | HHIP | A | beta | 20.14 | 9.50 × 10−5 | ||
| rs7836170 | 8q13.2 | SULF1 | T | beta | 20.16 | 2.15 × 10−5 | ||
| rs925847 | 2q32.2 | STAT4 | T | beta | 0.16 | 8.17 × 10−5 | ||
| rs9364299 | 6q27 | SMOC2 | A | beta | 0.14 | 9.96 × 10−5 | ||
| rs9903394 | 17q24.3 | SOX9 | A | beta | 0.16 | 8.47 × 10−5 | ||
| FVC | rs6482071 | 10p12.31 | BCL11A | T | beta | 20.16 | 6.15 × 10−5 | |
| rs2497714 | 10q25.3 | ALS2CR4 | T | beta | 20.17 | 8.49 × 10−5 | ||
| rs2181563 | 10q25.3 | TNIK | A | beta | 0.20 | 3.50 × 10−5 | ||
| rs10466868 | 12q24.33 | YTHDC1 | T | beta | 0.35 | 1.39 × 10−5 | ||
| rs6500728 | 16p13.3 | KIAA0922 | T | beta | 20.17 | 2.02 × 10−5 | ||
| rs169660 | 16p12.2 | SULF1 | T | beta | 20.17 | 9.77 × 10−5 | ||
| rs1291183 | 18p11.32 | ABLIM1 | A | beta | 0.33 | 4.66 × 10−5 | ||
| rs11085898 | 19p13.12 | PLXDC2 | T | beta | 0.31 | 6.50 × 10−5 | ||
| rs2110565 | 2p16.1 | KIAA1600 | A | beta | 20.17 | 6.72 × 10−5 | ||
| rs1208082 | 2q33.1 | LOC338797 | T | beta | 20.25 | 6.39 × 10−5 | ||
| rs221013 | 20p12.2 | HS3ST2 | T | beta | 20.17 | 4.20 × 10−5 | ||
| rs8115491 | 20q12 | A2BP1 | T | beta | 20.17 | 7.15 × 10−5 | ||
| rs6096573 | 20q13.2 | YES1 | T | beta | 20.18 | 5.47 × 10−5 | ||
| rs9974012 | 20q13.31 | NDUFB7 | A | beta | 0.16 | 4.97 × 10−5 | ||
| rs7281703 | 21q21.1 | PAK7 | T | beta | 0.17 | 3.09 × 10−5 | ||
| rs8140240 | 22q12.3 | ATP9A | T | beta | 0.16 | 5.92 × 10−5 | ||
| rs4133045 | 3q26.2 | PTPRT | T | beta | 0.20 | 7.02 × 10−5 | ||
| rs17592868 | 4q13.2 | BMP7 | T | beta | 0.16 | 8.72 × 10−5 | ||
| rs13119846 | 4q31.3 | C21orf37 | T | beta | 0.33 | 6.98 × 10−5 | ||
| rs7836170 | 8q13.2 | EIF3S7 | A | beta | 20.31 | 9.95 × 10−5 | ||
| FEV1/FVC | rs11032873 | 11p13 | APIP | T | beta | 0.18 | 3.08 × 10−5 | |
| rs11675728 | 2q36.3 | DNER | T | beta | 20.15 | 7.22 × 10−5 | ||
| rs12659620 | 5p15.31 | ADCY2 | T | beta | 0.15 | 5.56 × 10−5 | ||
| rs1406593 | 7p15.2 | SNX10 | T | beta | 20.15 | 7.64 × 10−5 | ||
| rs1416920 | 6p22.1 | ZNF323 | T | beta | 0.16 | 9.46 × 10−5 | ||
| rs17450685 | 10q22.3 | C10orf11 | T | beta | 0.15 | 8.73 × 10−5 | ||
| rs17554448 | 2q31.1 | ZNF650 | A | beta | 0.19 | 8.56 × 10−5 | ||
| rs17646998 | 8q13.2 | SULF1 | T | beta | 20.15 | 3.61 × 10−5 | ||
| rs2063485 | 3q13.11 | ZPLD1 | T | beta | 0.25 | 1.34 × 10−5 | ||
| rs2230739 | 16p13.3 | ADCY9 | A | beta | 0.16 | 6.25 × 10−5 | ||
| rs2705044 | 8p22 | MTMR7 | A | beta | 0.21 | 7.46 × 10−5 | ||
| rs3130696 | 6p21.33 | HLA-C | A | beta | 20.17 | 7.34 × 10−5 | ||
| rs3748540 | 1q43 | GREM2 | A | beta | 0.15 | 7.88 × 10−5 | ||
| rs3809335 | 13q12.13 | MTMR6 | T | beta | 0.28 | 5.40 × 10−5 | ||
| rs4234121 | 2q37.3 | KIF1A | A | beta | 20.15 | 5.32 × 10−5 | ||
| rs5767064 | 22q13.32 | LOC388915 | A | beta | 0.16 | 2.79 × 10−5 | ||
| rs7663065 | 4p15.1 | FLJ45721 | A | beta | 20.15 | 5.43 × 10−5 | ||
| rs8030494 | 15q24.1 | TBC1D21 | A | beta | 0.15 | 7.83 × 10−5 | ||
| rs823673 | 1p34.2 | NFYC | A | beta | 0.19 | 3.94 × 10−5 | ||
| rs9287995 | 2q31.1 | HNRPA3 | T | beta | 0.15 | 6.02 × 10−5 | ||
| rs9362054 | 6q14.3 | C6orf84 | T | beta | 0.14 | 8.68 × 10−5 | ||
| rs9574386 | 13q31.1 | C13orf10 | A | beta | 20.27 | 7.72 × 10−5 | ||
| Asthma remission | [97] | |||||||
| Clinical remission | rs7240102 | 18q21.2 | LOC100130003/C18orf26 | G | OR | 1.99 | 7.9 × 10−5 | |
| Complete remission | rs6581895 | 12q15 | YEATS4/FRS2 | G | OR | 3.83 | 1.3 × 10−5 | |
| rs12405429 | 1q42.2 | FAM89A/TRIM67 | G | OR | 3.10 | 1.0 × 10−4 | ||
| rs1420101 | 2q12.1 | IL18R1/IL1RL1 | A | OR | 0.44 | 3.4 × 10−4 | ||
| T2-low asthma | rs117639512 | 19q13.41 | KLK5 | A | OR | 0.33 | 2.75 × 10−8 | [101] |
| Total IgE | rs10404342 | 19q13.43 | ZNF71 | C | NA | NA | 7.60 × 10−6 | [102] |
| rs4879926 | 9p13.3 | TLN1 | C | NA | NA | 7.74 × 10−60 | ||
| Eosinophil-specific proteins | [104] | |||||||
| EDN | rs72677651 | 1p31.3 | JAK1/AK4 | T | beta | 0.54 | 2.0 × 10−8 | |
| rs76335186 | 7p21.3 | NDUFA4 | G | beta | −0.55 | 4.9 × 10−8 | ||
| rs67049014 | 14q11.2 | RNASE2/METTL17 | A | beta | −0.32 | 3 × 10−12 | ||
| ECP | rs56675562 | 9q22.1 | CDK20/SPATA31C2 | G | beta | −0.56 | 5.1 × 10−9 | |
| ECP-EDN | rs116571378 | 2p13.3 | ARHGAP25 | T | beta | NA | 4.2 × 10−10 | |
| rs67049014 | 14q11.2 | RNASE2/METTL17 | A | beta | NA | 1 × 10−13 | ||
a Positions based on GRCh37/hg19 build. Abbreviations: FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; HR: hazard ratio; IgE: immunoglobulin E; NA: not available; OR: odds ratio.
4. Discussion
Our analysis of the NHGRI-EBI GWAS Catalog highlighted a Eurocentric bias in studies of asthma phenotypes and related traits, as similarly observed for GWAS across human diseases/traits [105] and polygenic scores [106]. Further efforts should be made in ethnically diverse populations, particularly in historically minoritized populations disproportionately affected by asthma susceptibility, mortality, and comorbidities, such as African Americans and Hispanics/Latinos in the United States of America. In this regard, recent studies have characterized the genetic variation implicated in asthma exacerbations and treatment response in admixed populations either by GWAS [85,86], multi-omic approaches [107], or leveraging local ancestry via admixture mapping [108,109,110]. However, functional studies are needed to confirm these findings and prioritize genetic markers for assessment of their predictive capability to guide treatment response or prognosis.
Some of the genes revealed in GWAS of asthma phenotypes and related traits have been also uncovered in non-stratified GWAS of asthma. Therefore, it is likely that many of the previously reported asthma signals actually reflect specific asthma phenotypes present in a large proportion of GWAS participants. Although several studies have focused on asthma phenotypes, there is a limited number of studies considering only asthma patients, especially for clinically relevant phenotypes such as lung function or IgE levels, which could also include healthy individuals. For instance, novel IgE-related genes (CRIM1, ZNF71, TLN1, and SYNPO2) were uncovered by the only GWAS of IgE in asthma patients. Among these, SYNPO2 gene overexpression was previously associated with reduced airway hyperresponsiveness in individuals with asthma after oral corticoid therapy [103]. Another study focused on eosinophil-specific proteins released during allergic response [104] revealed genetic signals in genes involved in pathophysiologic mechanisms common between eosinophil activity and asthma, such as inflammation, oxidative stress, and extracellular matrix remodeling. The research on asthma remission merits special attention, despite the fact that just one study has been conducted so far [97]. In their work, the A-allele of rs1420101 located in IL1RL1 was associated with a lower probability of complete asthma remission in adults. This finding is consistent with a previous study that reported the association of this SNP with higher eosinophil levels in childhood asthma and with a higher risk for asthma [111]. All these together support the necessity of considering asthma-related phenotypes as a strategy to potentiate novel loci discovery and possible new therapeutical targets for precision medicine. Although the characterization of genetic influences on asthma phenotypes still lags behind compared to other omic layers (e.g., proteomics [112], transcriptomics [93,113,114], or epigenetics [115,116]), three studies have discerned asthma-related polygenic phenotypes [117,118,119]. The analysis of comorbidity data from electronic health records as a surrogate of unknown gene–environment contexts distinguished 22 asthma subgroups with distinct comorbidity patterns using approximately six million residents of the United States of America, from which 11 subgroups were validated in the UKB [117]. The GWAS of asthma across the validated subgroups and the whole dataset revealed 14 shared and 6 distinct associations, of which loci for the musculoskeletal and gastrointestinal asthma subgroups remained significant after stringent correction for multiple testing [117]. An analysis of longitudinal data from the UKB revealed multiple age-dependent comorbidity subgroups across complex diseases. In particular, the asthma subgroup characterized by dermatological comorbidities exhibited significant heterogeneity in polygenic risk scores compared to the other asthma subgroups [118]. Another study found suggestive genetic associations for asthma-related phenotypes determined by latent class analysis of clinical and demographic data from 3001 European adults [119].
Other approaches for identification of polygenic subtypes for human complex diseases and traits [120] could be implemented in asthma. Although the effect size gradient is likely to be small for most asthma-related loci [117], clustering of variant effect sizes supported by functional annotation or pleiotropy may also reveal additional insights into the genetic basis of respiratory diseases. Multi-trait genetic analyses of autoimmune and/or allergic diseases have uncovered pleotropic variants in European [121,122] and Japanese individuals [123]. Conversely, the modest differences in minor allele frequencies of most common variants across subgroups may hinder genomic-driven subtype identification in complex diseases [120]. A recent analysis in the UKB overcame this limitation by investigating previous respiratory-health-related loci and incorporating multi-trait data into genetic effect clustering by considering airway diseases, lung function, and other clinical and demographic traits [124]. The evident Eurocentric bias in genomic research of respiratory diseases is likely to lessen with the development of large-scale initiatives integrating both genomic, environmental, and respiratory health data from ethnically diverse populations, such as the Environmental influences on Child Health Outcomes (ECHO) study [125] and the All of Us Research Program [126]. Moore et al. [16] used a clustering approach in the SARP cohort to classify severe asthma cases attending to clinical and demographic data and were able to discriminate several sub-phenotypes within this cohort of patients.
Multi-omics have also been applied to define asthma phenotypes and gain a better comprehension of the disease. For instance, Forno et al. prioritized IL5RA as a candidate gene associated with asthma using vertical integration of several analytical layers [127]. Another potential strategy to integrate several omic layers could be the use of colocalization [128]. In this case, each layer is analyzed separately and then overlapped to evaluate if there are specific genomic regions that associate with a trait of interest through more than one omic layer, implying and reinforcing the association of that region with the phenotype studied. In that regard, it is important that the tissues to be explored are relevant for the trait under study since the transcriptomic and epigenetic profiles may differ between tissues. Nonetheless, these strategies have been scarcely applied to define asthma subgroups or to assess any asthma phenotype individually.
Importantly, one omic layer rarely included in asthma multi-omic analyses despite the amount of linking evidence with asthma development, progression, and asthma exacerbations is the microbiome, defined as the set of microorganisms of a specific niche, which gathers both the human microbiome and the environmental microbiome. In fact, several studies have assessed the implication of the bacterial and fungal communities of the airways and related tissues as the saliva or the oral cavity, highlighting how dysbiosis in those environments associates with risk or protection of developing asthma or asthma exacerbations [129].
An alternative to these integrative methods could be the exploration of the role that genetic variants highlighted in omic studies as associated with a specific trait have in the context of transcriptomic and epigenetic regulation or other contexts such as the RNA maturation or the tridimensional organization of the genetic material in the nucleus (histone modification and DNA packing). These methods have been collectively called quantitative trait locus (QTL) analyses and have been recently incorporated in omic studies to allocate those associations in the cellular context and gain a better understanding with regard to the biological meaning of those associations [130]. An important note for future studies concerns the annotation methodology used to assign genes to genetic variants in order to understand omic results from a functional perspective and as part of a bigger picture. Since this annotation method assigns genes to genetic variants attending to proximity to the TSS, a plausible alternative for future studies could be using annotation methods that rely on functional information instead of only relying on physical distance.
Appendix A
Appendix A.1. Literature and Database Mining
The NHGRI-EBI GWAS Catalog (version 2023-04-07) was downloaded from the GWAS catalog webpage and processed in R 4.2.3. The GWAS Catalog literature mining, inclusion criteria, and curation process is described elsewhere [82,131]. The methodology for categorization of individuals into ancestry groups is detailed elsewhere [132]. Ancestry groups were categorized into seven groups: “African” (AFR), “African American or Afro-Caribbean” (AA/AC), “Asian” (ASN), “European” (EUR), “Hispanic/Latin American” (LAT), “Other/Mixed” (O/M), “Not Reported (NR)”. Outcomes containing the words “asthma” or “Asthma” in the disease/category term were categorized into six groups according to the type of assessed genetic effect: (a) main effects for asthma, (b) main effects for asthma and other diseases/traits (pleiotropy), (c) effects of gene–environment or gene–gene interactions, (d) main effects for asthma subtypes, or (e) main effects for asthma-related phenotypes. Diseases/traits related to asthma were grouped according to the following seven categories: asthma, asthma–chronic obstructive pulmonary disease overlap syndrome (ACO), nonatopic asthma (NAA), allergic asthma (AA), adult-onset asthma (AOA), childhood-onset asthma (COA), and toluene diisocyanate-induced asthma (DIA). Asthma-related diseases/traits were grouped according to the following six categories: asthma remission, control, and severity, age of asthma onset, immunoglobulin E levels, eosinophil-specific protein levels, bronchial hyperresponsiveness, and lung function. Asthma exacerbations, treatment response, and gene–environment interactions on asthma were considered for scientometric analysis but were not reviewed as they have been recently described in depth [85,86,87]. The full list of phenotypes considered for scientometric purposes is detailed in Table A1.
Table A1.
Categorization of diseases/traits for asthma phenotypes and related traits available in the NHGRI-EBI GWAS Catalog (version 2023-04-07).
| Asthma-Related Traits | Asthma Phenotype |
|---|---|
| AES | AA |
| Asthma exacerbations | Atopic asthma |
| Asthma with exacerbation (PheCode 495.2) | Asthma and hay fever |
| Childhood asthma exacerbations in long-acting beta2-agonist treatment | Asthma and eczema |
| Childhood asthma with severe exacerbations | ICD10 J45.0: Predominantly allergic asthma |
| Severe exacerbations in childhood asthma | ICD10 J45.0: Predominantly allergic asthma (Gene-based burden) |
| Exacerbations requiring hospitalization in asthma | ACO |
| Asthma exacerbations in inhaled corticosteroid treatment | Asthma–COPD overlap syndrome |
| Asthma with severe exacerbations | Asthma–chronic obstructive pulmonary disease overlap syndrome in asthma |
| Age of onset | Asthma–COPD overlap syndrome (Gene-based burden) |
| Asthma (time to childhood onset) in early life tobacco smoke exposure) | Asthma–chronic obstructive pulmonary disease overlap syndrome |
| Asthma (time to onset) | AOA |
| Asthma (age of onset) | Adult-onset asthma in non-smokers |
| Age of onset of childhood-onset asthma | Adult-onset asthma in ever-smokers |
| Age of onset of adult-onset asthma | Adult asthma (Gene-based burden) |
| Asthma (time to event) | Asthma (adult onset) |
| CSR | Adult asthma |
| Asthma (moderate or severe) | COA |
| Clinical remission in asthma | Pediatric asthma |
| Complete remission in asthma | Self-reported childhood asthma in adult smokers |
| Asthma control | Asthma (childhood onset) |
| GxE | Childhood asthma |
| Asthma (sex interaction) | Asthma onset (childhood vs. adult) |
| Adult onset asthma (smoking interaction) | DIA |
| Childhood asthma x sex interaction | Asthma (toluene diisocyanate-induced) |
| Asthma (SNP x SNP interaction) | Diisocyanate-induced asthma |
| Asthma control x inhaled corticosteroid treatment interaction (1df) | NAA |
| Asthma control x inhaled corticosteroid treatment interaction (2df) | Nonatopic asthma |
| Asthma x Hispanic interaction (2df) | |
| Bronchodilator response x age interaction in asthma | |
| Bone mineral accretion in asthma (oral corticosteroid dose interaction) | |
| Response to zileuton treatment in asthma (FEV1 change interaction) | |
| Asthma (time to childhood onset) x early life tobacco smoke interaction | |
| Adult onset asthma (smoking interaction) | |
| Asthma (sex interaction) | |
| Asthma (SNP x SNP interaction) | |
| Asthma or atopy (farm exposure interaction) | |
| Asthma x air pollution interaction (2df) | |
| Asthma x Hispanic interaction (2df) | |
| Childhood asthma x sex interaction | |
| Childhood onset asthma (traffic air pollution exposure interaction) | |
| Lung function (FEV1) in asthma (dust mite allergen exposure interaction) | |
| Lung function (FEV1/FVC) in asthma (dust mite allergen exposure interaction) | |
| Adverse response to inhaled corticosteroid treatment x age interaction in asthma | |
| Bronchodilator response in asthma (inhaled corticosteroid treatment interaction) | |
| Post-bronchodilator FEV1 x air pollution (CO) interaction in childhood asthma) | |
| Asthma x air pollution interaction (2df) | |
| Post-bronchodilator FEV1 x air pollution (NO2) interaction in childhood asthma, | |
| Childhood onset asthma (traffic air pollution exposure interaction) | |
| IgE-related | |
| IgE levels in asthmatics | |
| IgE levels in asthmatics (D.f. specific) | |
| IgE levels in asthmatics (D.p. specific) | |
| Lung function | |
| Pulmonary function in asthmatics, | |
| Lung function (FEV1) in asthma | |
| Lung function (FVC) in asthma | |
| Lung function (FEV1/FVC) in asthma | |
| Treatment response | |
| Post-bronchodilator lung function in asthma (FEV1) | |
| Post-bronchodilator lung function in asthma (FVC) | |
| Post-bronchodilator lung function in asthma (FEV1/FVC) | |
| Asthma treatment response | |
| Asthma (bronchodilator response) | |
| Asthma (corticosteroid response) | |
| Response to inhaled corticosteroid treatment in asthma (change in FEV1) | |
| Response to inhaled glucocorticoid treatment in asthma (change in FEV1) | |
| Bronchodilator response in asthma | |
| Response to montelukast in asthma (change in FEV1) | |
| Response to mepolizumab in severe asthma | |
| Response to placebo treatment in childhood asthma (FVC change) | |
| Oral corticosteroid burst in asthma | |
| Recent medication for asthma (UKB data field 22167) | |
| Recent medication for asthma (UKB data field 22167) (Gene-based burden) | |
| Subjective response to placebo treatment in childhood asthma (change in cough/wheeze) |
Abbreviations: 2df: 2 degree of freedom test; AA: allergic asthma; ACO: asthma–chronic obstructive pulmonary disease overlap syndrome; AEs: asthma exacerbations; AOA: adult-onset asthma; CO: carbon monoxide; COA: childhood-onset asthma; COPD: chronic obstructive pulmonary disease; CSR: asthma control, severity, or remission; Dp: Dermatophagoides pteronyssinus; Df: Dermatophagoides farinae; DIA: diisocyanate-induced asthma; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; GxE: gene–environment interaction; IgE: immunoglobulin E; NAA: nonatopic asthma; NO2: nitrogen dioxide; SNP: single-nucleotide polymorphism; UKB: United Kingdom Biobank.
To identify GWAS studies that have yet to be included in the NHGRI-EBI GWAS Catalog, Pubmed was queried using the following command via PubmedR R package [133] in order to retrieve studies from inception up to 19 April 2023: “((((((Genome-Wide Association Study[MeSH Terms]) AND (asthma[MeSH Terms])) AND (asthma[Title])) NOT (exacerbations[Title])) NOT (editorial[Publication Type])) NOT (Review[Publication Type])) NOT (Systematic Review[Publication Type])”. Screening of articles was conducted independently by two reviewers (A.E.-O. and E.H.-L.). Any disputes in data were resolved in a joint meeting between the two reviewers (A.E.-O. and E.H.-L.). Conference or poster abstracts, literature reviews, editorials, or opinion articles, studies not conducted on humans, studies not in English, and studies not designed as genome-wide association were excluded. One article with genome-wide significant signals for COA was identified and incorporated into the database. In addition, we further conducted a systematic search using Pubmed to identify genomic studies for asthma remission, asthma control, asthma severity, age of asthma onset, immunoglobulin E levels, eosinophils count, eosinophil-specific protein levels, bronchial hyperresponsiveness, and lung function. No genomic studies of eosinophils count in asthma have been conducted.
Appendix A.2. Variant Annotation
Genetic variants were annotated to genes via GREAT [134] using the “basal plus extension” procedure, which considers proximal genes as those with a transcription start site (TSS) within 5.0 and 1.0 kilobases (kb) upstream and downstream of the genomic location, respectively, and distal genes as those with a TSS located up to 1000 kb from the genomic location. Variant effect type according to the Sequence Ontology term was investigated using g:SNPsense within the g:Profiler framework [135]. Multi-effect variants were considered in the analysis.
Appendix A.3. Enrichment and Protein–Protein Interaction Network Analyses
Gene-set enrichment analyses were conducted for genes detected only by the specific parent categories or shared across categories using default parameters at Metascape (v3.5.2023-05-01) [136]. The following terms were evaluated using gene-set enrichment analysis on Gene ontology terms (GO) for Cellular Components, Molecular Functions, and Biological Processes, as well as additional pathway data, including the Kyoto Encyclopedia of Genes and Genomes (KEGG) Pathway, Reactome Gene Sets, Canonical Pathways, and WikiPathways datasets. Within the Metascape framework, a protein–protein interaction network was built considering distinct gene sets for asthma phenotypes and physical interactions in STRING [137] and BioGrid [138]. The Molecular Complex Detection (MCODE) algorithm [139] was used to identify densely connected network components.
Author Contributions
Conceptualization, A.E.-O., E.H.-L., P.P.-G. and R.G.-P.; methodology, A.E.-O. and E.H.-L.; validation, A.E.-O. and E.H.-L.; formal analysis, A.E.-O., E.H.-L., E.M.-G., P.P.-G. and R.G.-P.; data curation, A.E.-O., E.H.-L., E.M.-G., P.P.-G. and R.G.-P.; writing—original draft preparation, A.E.-O., E.H.-L., E.M.-G., P.P.-G. and R.G.-P.; writing—review and editing, A.E.-O., E.H.-L., E.M.-G., P.P.-G. and R.G.-P.; visualization, A.E.-O. and E.H.-L.; supervision, E.H.-L., P.P.-G. and R.G.-P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data necessary to evaluate the conclusions of this manuscript are available in the NHGRI-EBI GWAS Catalog and reported in the main text and/or Appendix A.
Conflicts of Interest
P.P.-G. reports personal fees from GSK, AstraZeneca, LETI Pharma, Inmunotek Laboratories, Stallergenes, and Sanofi outside the submitted work. R.G.-P. received grants from Fundación Canaria Instituto de Investigación Sanitaria de Canarias (FIISC), code number PIFIISC22/24 and Sociedad Española de Alergología e Inmunología Clínica (SEAIC), code AGITA. RGP reports personal fees from AstraZeneca, Diater Laboratories, GSK, Inmunotek Laboratories, Leo Pharma, and Sanofi outside the submitted work. The remaining authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
E.H.-L. received support from the National Institute of Health (NIH) National Human Genome Research Institute (NHGRI) (R35HG011944-02). E.M.-G. was supported by a fellowship (TESIS2022010045) co-financed by the Canarian Agency for Research, Innovation and the Information Society of the Ministry of Economy, Knowledge and Employment and by the European Social Fund (ESF) Integrated Operational Program of the Canary Islands 2014–2020, Axis 3 Priority Theme 74 (85%). R.G.-P. received funding support from Sociedad Española de Alergología e Inmunología Clínica (SEAIC), Becas Fundación SEAIC convocatoria 2021, project code AGITA. This manuscript was published free of charge after peer review as part of the Genes 2022 Best PhD Thesis Award, awarded to E.H.-L.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ferkol T., Schraufnagel D. The Global Burden of Respiratory Disease. Ann. Am. Thorac. Soc. 2014;11:404–406. doi: 10.1513/AnnalsATS.201311-405PS. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Asthma Global Strategy for Asthma Management and Prevention. 2023. [(accessed on 27 August 2023)]. Available online: https://ginasthma.org/
- 3.Price D., Fletcher M., Molen T. van der Asthma Control and Management in 8000 European Patients: The REcognise Asthma and Link to Symptoms and Experience (REALISE) Survey. NPJ Prim. Care Respir. Med. 2014;24:14009. doi: 10.1038/npjpcrm.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy M.L. The National Review of Asthma Deaths: What Did We Learn and What Needs to Change? Breathe Sheff. 2015;11:14–24. doi: 10.1183/20734735.008914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadatsafavi M., Rousseau R., Chen W., Zhang W., Lynd L., FitzGerald J.M. The Preventable Burden of Productivity Loss Due to Suboptimal Asthma Control: A Population-Based Study. Chest. 2014;145:787–793. doi: 10.1378/chest.13-1619. [DOI] [PubMed] [Google Scholar]
- 6.Vicente C.T., Revez J.A., Ferreira M.A.R. Lessons from Ten Years of Genome-Wide Association Studies of Asthma. Clin. Transl. Immunol. 2017;6:e165. doi: 10.1038/cti.2017.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakula A. Henry Hyde Salter (1823-71): A Biographical Sketch. Thorax. 1985;40:887–888. doi: 10.1136/thx.40.12.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wenzel S.E. Asthma Phenotypes: The Evolution from Clinical to Molecular Approaches. Nat. Med. 2012;18:716–725. doi: 10.1038/nm.2678. [DOI] [PubMed] [Google Scholar]
- 9.Rackemann F.M. A Working Classification of Asthma. Am. J. Med. 1947;3:601–606. doi: 10.1016/0002-9343(47)90204-0. [DOI] [PubMed] [Google Scholar]
- 10.McFadden E.R. A Century of Asthma. Am. J. Respir. Crit. Care Med. 2004;170:215–221. doi: 10.1164/rccm.200402-185OE. [DOI] [PubMed] [Google Scholar]
- 11.Hinks T.S.C., Levine S.J., Brusselle G.G. Treatment Options in Type-2 Low Asthma. Eur. Respir. J. 2021;57:2000528. doi: 10.1183/13993003.00528-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woodruff P.G., Modrek B., Choy D.F., Jia G., Abbas A.R., Ellwanger A., Koth L.L., Arron J.R., Fahy J.V. T-Helper Type 2-Driven Inflammation Defines Major Subphenotypes of Asthma. Am. J. Respir. Crit. Care Med. 2009;180:388–395. doi: 10.1164/rccm.200903-0392OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Busse W.W., Holgate S.T., Wenzel S.W., Klekotka P., Chon Y., Feng J., Ingenito E.P., Nirula A. Biomarker Profiles in Asthma with High vs Low Airway Reversibility and Poor Disease Control. Chest. 2015;148:1489–1496. doi: 10.1378/chest.14-2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lambrecht B.N., Hammad H., Fahy J.V. The Cytokines of Asthma. Immunity. 2019;50:975–991. doi: 10.1016/j.immuni.2019.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Svenningsen S., Nair P. Asthma Endotypes and an Overview of Targeted Therapy for Asthma. Front. Med. Lausanne. 2017;4:158. doi: 10.3389/fmed.2017.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore W.C., Meyers D.A., Wenzel S.E., Teague W.G., Li H., Li X., Jr R.D., Castro M., Curran-Everett D., Fitzpatrick A.M., et al. Identification of Asthma Phenotypes Using Cluster Analysis in the Severe Asthma Research Program. Am. J. Respir. Crit. Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaw D.E., Sousa A.R., Fowler S.J., Fleming L.J., Roberts G., Corfield J., Pandis I., Bansal A.T., Bel E.H., Auffray C., et al. Clinical and Inflammatory Characteristics of the European U-BIOPRED Adult Severe Asthma Cohort. Eur. Respir. J. 2015;46:1308–1321. doi: 10.1183/13993003.00779-2015. [DOI] [PubMed] [Google Scholar]
- 18.Loza M.J., Djukanovic R., Chung K.F., Horowitz D., Ma K., Branigan P., Barnathan E.S., Susulic V.S., Silkoff P.E., Sterk P.J., et al. Validated and Longitudinally Stable Asthma Phenotypes Based on Cluster Analysis of the ADEPT Study. Respir. Res. 2016;17:165. doi: 10.1186/s12931-016-0482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haldar P., Pavord I.D., Shaw D.E., Berry M.A., Thomas M., Brightling C.E., Wardlaw A.J., Green R.H. Cluster Analysis and Clinical Asthma Phenotypes. Am. J. Respir. Crit. Care Med. 2008;178:218–224. doi: 10.1164/rccm.200711-1754OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuruvilla M.E., Lee F.E.-H., Lee G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2019;56:219–233. doi: 10.1007/s12016-018-8712-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson G.P. Endotyping Asthma: New Insights into Key Pathogenic Mechanisms in a Complex, Heterogeneous Disease. Lancet. 2008;372:1107–1119. doi: 10.1016/S0140-6736(08)61452-X. [DOI] [PubMed] [Google Scholar]
- 22.Ray A., Camiolo M., Fitzpatrick A., Gauthier M., Wenzel S.E. Are We Meeting the Promise of Endotypes and Precision Medicine in Asthma? Physiol. Rev. 2020;100:983–1017. doi: 10.1152/physrev.00023.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Locksley R.M. Asthma and Allergic Inflammation. Cell. 2010;140:777–783. doi: 10.1016/j.cell.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung K.F. Asthma Phenotyping: A Necessity for Improved Therapeutic Precision and New Targeted Therapies. J. Intern. Med. 2016;279:192–204. doi: 10.1111/joim.12382. [DOI] [PubMed] [Google Scholar]
- 25.Akar-Ghibril N., Casale T., Custovic A., Phipatanakul W. Allergic Endotypes and Phenotypes of Asthma. J. Allergy Clin. Immunol. Prac. 2020;8:429–440. doi: 10.1016/j.jaip.2019.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jartti T., Gern J.E. Role of Viral Infections in the Development and Exacerbation of Asthma in Children. J. Allergy Clin. Immunol. 2017;140:895–906. doi: 10.1016/j.jaci.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foronjy R., D’Armiento J. The Effect of Cigarette Smoke-Derived Oxidants on the Inflammatory Response of the Lung. Clin. Appl. Immunol. Rev. 2006;6:53–72. doi: 10.1016/j.cair.2006.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martinez F.D. Childhood Asthma Inception and Progression: Role of Microbial Exposures, Susceptibility to Viruses and Early Allergic Sensitization. Immunol. Allergy Clin. N. Am. 2019;39:141–150. doi: 10.1016/j.iac.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ayers A.B., Henry K., Russell S.B., Steiner R.E. The Microvasculature of the Spleen. Clin. Radiol. 1976;27:259–264. doi: 10.1016/S0009-9260(76)80161-4. [DOI] [PubMed] [Google Scholar]
- 30.Fahy J.V. Type 2 Inflammation in Asthma--Present in Most, Absent in Many. Nat. Rev. Immunol. 2015;15:57–65. doi: 10.1038/nri3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peters M.C., Kerr S., Dunican E.M., Woodruff P.G., Fajt M.L., Levy B.D., Israel E., Phillips B.R., Mauger D.T., Comhair S.A., et al. Refractory Airway Type 2 Inflammation in a Large Subgroup of Asthmatic Patients Treated with Inhaled Corticosteroids. J. Allergy Clin. Immunol. 2019;143:104–113.e14. doi: 10.1016/j.jaci.2017.12.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amelink M., de Groot J.C., de Nijs S.B., Lutter R., Zwinderman A.H., Sterk P.J., Brinke A.T., Bel E.H. Severe Adult-Onset Asthma: A Distinct Phenotype. J. Allergy Clin. Immunol. 2013;132:336–341. doi: 10.1016/j.jaci.2013.04.052. [DOI] [PubMed] [Google Scholar]
- 33.White A.A., Doherty T.A. Role of Group 2 Innate Lymphocytes in Aspirin-Exacerbated Respiratory Disease Pathogenesis. Am. J. Rhinol. Allergy. 2018;32:7–11. doi: 10.2500/ajra.2018.32.4498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laidlaw T.M., Mullol J., Woessner K.M., Amin N., Mannent L.P. Chronic Rhinosinusitis with Nasal Polyps and Asthma. J. Allergy Clin. Immunol. Prac. 2021;9:1133–1141. doi: 10.1016/j.jaip.2020.09.063. [DOI] [PubMed] [Google Scholar]
- 35.Swierczynska M., Nizankowska-Mogilnicka E., Zarychta J., Gielicz A., Szczeklik A. Nasal versus bronchial and nasal response to oral aspirin challenge: Clinical and biochemical differences between patients with aspirin-induced asthma/rhinitis. J. Allergy Clin. Immunol. 2003;112:995–1001. doi: 10.1016/S0091-6749(03)02015-3. [DOI] [PubMed] [Google Scholar]
- 36.Daffern P.J., Muilenburg D., Hugli T.E., Stevenson D.D. Association of urinary leukotriene E4 excretion during aspirin challenges with severity of respiratory responses. J. Allergy Clin. Immunol. 1999;104:559–564. doi: 10.1016/S0091-6749(99)70324-6. [DOI] [PubMed] [Google Scholar]
- 37.Micheletto C., Tognella S., Visconti M., Trevisan F., Dal Negro R.W. Changes in urinary LTE4 and nasal functions following nasal provocation test with ASA in ASA-tolerant and -intolerant asthmatics. Respir. Med. 2006;100:2144–2150. doi: 10.1016/j.rmed.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 38.Laidlaw T.M., Boyce J.A. Pathogenesis of aspirin-exacerbated respiratory disease and reactions. Immunol. Allergy Clin. N. Am. 2013;33:195–210. doi: 10.1016/j.iac.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cavagnero K.J., Doherty T.A. Lipid-Mediated Innate Lymphoid Cell Recruitment and Activation in Aspirin-Exacerbated Respiratory Disease. Ann. Allergy Asthma Immunol. 2021;126:135–142. doi: 10.1016/j.anai.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eastman J.J., Cavagnero K.J., Deconde A.S., Kim A.S., Karta M.R., Broide D.H., Zuraw B.L., White A.A., Christiansen S.C., Doherty T.A. Group 2 Innate Lymphoid Cells Are Recruited to the Nasal Mucosa in Patients with Aspirin-Exacerbated Respiratory Disease. J. Allergy Clin. Immunol. 2017;140:101–108.e3. doi: 10.1016/j.jaci.2016.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fitzpatrick A.M., Chipps B.E., Fernando P.G.H. Woodruff T2-“Low” Asthma: Overview and Management Strategies. J. Allergy Clin. Immunol. Prac. 2020;8:452–463. doi: 10.1016/j.jaip.2019.11.006. [DOI] [PubMed] [Google Scholar]
- 42.Hudey S.N., Ledford D.K., Cardet J.C. Mechanisms of Non-Type 2 Asthma. Curr. Opin. Immunol. 2020;66:123–128. doi: 10.1016/j.coi.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simpson J.L., Scott R., Boyle M.J., Gibson P.G. Inflammatory Subtypes in Asthma: Assessment and Identification Using Induced Sputum. Respirology. 2006;11:54–61. doi: 10.1111/j.1440-1843.2006.00784.x. [DOI] [PubMed] [Google Scholar]
- 44.Carr T.F. Treatment Approaches for the Patient with T2 Low Asthma. Ann. Allergy Asthma Immunol. 2021;127:530–535. doi: 10.1016/j.anai.2021.05.027. [DOI] [PubMed] [Google Scholar]
- 45.Hastie A.T., Moore W.C., Meyers D.A., Vestal P.L., Li H., Peters S.P., Bleecker E.R., Lung N.H., Program B.I.S.A.R. Analyses of Asthma Severity Phenotypes and Inflammatory Proteins in Subjects Stratified by Sputum Granulocytes. J. Allergy Clin. Immunol. 2010;125:1028–1036.e13. doi: 10.1016/j.jaci.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rossios C., Pavlidis S., Hoda U., Kuo C.-H., Wiegman C., Russell K., Sun K., Loza M.J., Baribaud F., Durham A.L., et al. Sputum Transcriptomics Reveal Upregulation of IL-1 Receptor Family Members in Patients with Severe Asthma. J. Allergy Clin. Immunol. 2018;141:560–570. doi: 10.1016/j.jaci.2017.02.045. [DOI] [PubMed] [Google Scholar]
- 47.Peters M.C., McGrath K.W., Hawkins G.A., Hastie A.T., Levy B.D., Israel E., Phillips B.R., Mauger D.T., Comhair S.A., Erzurum S.C., et al. Plasma Interleukin-6 Concentrations, Metabolic Dysfunction, and Asthma Severity: A Cross-Sectional Analysis of Two Cohorts. Lancet Respir. Med. 2016;4:574–584. doi: 10.1016/S2213-2600(16)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ntontsi P., Loukides S., Bakakos P., Kostikas K., Papatheodorou G., Papathanassiou E., Hillas G., Koulouris N., Papiris S., Papaioannou A.I. Clinical, Functional and Inflammatory Characteristics in Patients with Paucigranulocytic Stable Asthma: Comparison with Different Sputum Phenotypes. Allergy. 2017;72:1761–1767. doi: 10.1111/all.13184. [DOI] [PubMed] [Google Scholar]
- 49.Tliba O., Jr R.A.P. Paucigranulocytic Asthma: Uncoupling of Airway Obstruction from Inflammation. J. Allergy Clin. Immunol. 2019;143:1287–1294. doi: 10.1016/j.jaci.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ogawa H., Azuma M., Umeno A., Shimizu M., Murotomi K., Yoshida Y., Nishioka Y., Tsuneyama K. Singlet Oxygen -Derived Nerve Growth Factor Exacerbates Airway Hyperresponsiveness in a Mouse Model of Asthma with Mixed Inflammation. Allergol. Int. 2022;71:395–404. doi: 10.1016/j.alit.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 51.Braun A., Quarcoo D., Schulte-Herbrüggen O., Lommatzsch M., Hoyle G., Renz H. Nerve Growth Factor Induces Airway Hyperresponsiveness in Mice. Int. Arch. Allergy Immunol. 2001;124:205–207. doi: 10.1159/000053711. [DOI] [PubMed] [Google Scholar]
- 52.Kyriakopoulos C., Gogali A., Bartziokas K., Kostikas K. Identification and Treatment of T2-Low Asthma in the Era of Biologics. ERJ Open Res. 2021;7:309–2020. doi: 10.1183/23120541.00309-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nair P., O’Byrne P.M. Measuring Eosinophils to Make Treatment Decisions in Asthma. Chest. 2016;150:485–487. doi: 10.1016/j.chest.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 54.Thomson N.C. Novel Approaches to the Management of Noneosinophilic Asthma. Ther. Adv. Respir. Dis. 2016;10:211–234. doi: 10.1177/1753465816632638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mohan A., Grace J., Wang B.R., Lugogo N. The Effects of Obesity in Asthma. Curr. Allergy Asthma Rep. 2019;19:49. doi: 10.1007/s11882-019-0877-z. [DOI] [PubMed] [Google Scholar]
- 56.Dixon A.E., Que L.G. Obesity and Asthma. Semin. Respir. Crit. Care Med. 2022;43:662–674. doi: 10.1055/s-0042-1742384. [DOI] [PubMed] [Google Scholar]
- 57.Ignacio R.M.C., Kim C.-S., Kim S.-K. Immunological Profiling of Obesity. J. Lifestyle Med. 2014;4:1–7. doi: 10.15280/jlm.2014.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Himmerich H., Fulda S., Linseisen J., Seiler H., Wolfram G., Stephanie K.H., Gedrich, Pollmächer T. TNF-α, Soluble TNF Receptor and Interleukin-6 Plasma Levels in the General Population. Eur. Cytokine Netw. 2006;17:196–201. [PubMed] [Google Scholar]
- 59.Björkander S., Klevebro S., Hernandez-Pacheco N., Kere M., Ekström S., Mikus M.S., van Hage M., James A., Kull I., Bergström A., et al. Obese Asthma Phenotypes Display Distinct Plasma Biomarker Profiles. Clin. Transl. Allergy. 2023;13:e12238. doi: 10.1002/clt2.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li X., Hastie A.T., Peters M.C., Hawkins G.A., Phipatanakul W., Li H., Moore W.C., Busse W.W., Castro M., Erzurum S.C., et al. Investigation of the Relationship between IL-6 and Type 2 Biomarkers in Patients with Severe Asthma. J. Allergy Clin. Immunol. 2020;145:430–433. doi: 10.1016/j.jaci.2019.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Holguin F., Comhair S.A.A., Hazen S.L., Powers R.W., Khatri S.S., Bleecker E.R., Busse W.W., Calhoun W.J., Castro M., Fitzpatrick A.M., et al. An Association between L-Arginine/Asymmetric Dimethyl Arginine Balance, Obesity, and the Age of Asthma Onset Phenotype. Am. J. Respir. Crit. Care Med. 2013;187:153–159. doi: 10.1164/rccm.201207-1270OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barcala F.J.G., de la Fuente-Cid R., Alvarez-Gil R., Tafalla M., Nuevo J., Caamaño-Isorna F. Factores Asociados Con El Control Del Asma En Pacientes de Atención Primaria En España: El Estudio CHAS. Arch. Bronconeumol. 2010;46:358–363. doi: 10.1016/j.arbres.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 63.Esteban-Gorgojo I., Antolín-Amérigo D., Domínguez-Ortega J., Quirce S. Non-Eosinophilic Asthma: Current Perspectives. J. Asthma Allergy. 2018;11:267–281. doi: 10.2147/JAA.S153097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boulet L.-P., Lemière C., Archambault F., Carrier G., Claire F.D.M. Deschesnes Smoking and Asthma: Clinical and Radiologic Features, Lung Function, and Airway Inflammation. Chest. 2006;129:661–668. doi: 10.1378/chest.129.3.661. [DOI] [PubMed] [Google Scholar]
- 65.Kiljander T., Poussa T., Helin T., Jaakkola A., Venho K., Lehtimäki L. Symptom Control among Asthmatics with a Clinically Significant Smoking History: A Cross-Sectional Study in Finland. BMC Pulm. Med. 2020;20:88. doi: 10.1186/s12890-020-1127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tiotiu A., Ioan I., Wirth N., Romero-Fernandez R., González-Barcala F.-J. The Impact of Tobacco Smoking on Adult Asthma Outcomes. Int. J. Environ. Res. Public Health. 2021;18:992. doi: 10.3390/ijerph18030992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Polosa R., Thomson N.C. Smoking and Asthma: Dangerous Liaisons. Eur. Respir. J. 2013;41:716–726. doi: 10.1183/09031936.00073312. [DOI] [PubMed] [Google Scholar]
- 68.Cazzola M., Polosa R. Anti-TNF-α and Th1 Cytokine-Directed Therapies for the Treatment of Asthma. Curr. Opin. Allergy Clin. Immunol. 2006;6:43–50. doi: 10.1097/01.all.0000199798.10047.74. [DOI] [PubMed] [Google Scholar]
- 69.Bujarski S., Parulekar A.D., Amir N.A.S. Hanania the Asthma COPD Overlap Syndrome (ACOS) Curr. Allergy Asthma Rep. 2015;15:509. doi: 10.1007/s11882-014-0509-6. [DOI] [PubMed] [Google Scholar]
- 70.Gibson P.G., McDonald V.M., Marks G.B. Asthma in Older Adults. Lancet. 2010;376:803–813. doi: 10.1016/S0140-6736(10)61087-2. [DOI] [PubMed] [Google Scholar]
- 71.Ducharme M.-E., Prince P., Hassan N., Nair P., Boulet L.-P. Expiratory Flows and Airway Inflammation in Elderly Asthmatic Patients. Respir. Med. 2011;105:1284–1289. doi: 10.1016/j.rmed.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 72.Dunn R.M., Busse P.J., Wechsler M.E. Asthma in the Elderly and Late-Onset Adult Asthma. Allergy. 2018;73:284–294. doi: 10.1111/all.13258. [DOI] [PubMed] [Google Scholar]
- 73.Schmitt V., Rink L., Uciechowski P. The Th17/Treg Balance Is Disturbed during Aging. Exp. Gerontol. 2013;48:1379–1386. doi: 10.1016/j.exger.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 74.Diaz-Guzman E., Mannino D.M. Airway Obstructive Diseases in Older Adults: From Detection to Treatment. J. Allergy Clin. Immunol. 2010;126:702–709. doi: 10.1016/j.jaci.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 75.Han Y.Y., Zhang X., Wang J., Wang G., Oliver B.G., Zhang H.P., Kang D.Y., Wang L., Qiu Z.X., Li W.M., et al. Multidimensional Assessment of Asthma Identifies Clinically Relevant Phenotype Overlap: A Cross-Sectional Study. J. Allergy Clin. Immunol. Prac. 2021;9:349–362.e18. doi: 10.1016/j.jaip.2020.07.048. [DOI] [PubMed] [Google Scholar]
- 76.Quirce S., Sastre J. Occupational asthma: Clinical phenotypes, biomarkers, and management. Curr. Opin. Pulm. Med. 2019;25:59–63. doi: 10.1097/MCP.0000000000000535. [DOI] [PubMed] [Google Scholar]
- 77.Vandenplas O., Godet J., Hurdubaea L., Rifflart C., Suojalehto H., Wiszniewska M., Munoz X., Sastre J., Klusackova P., Moore V., et al. Are high- and low-molecular-weight sensitizing agents associated with different clinical phenotypes of occupational asthma? Allergy. 2019;74:261–272. doi: 10.1111/all.13542. [DOI] [PubMed] [Google Scholar]
- 78.Ricciardolo F.L.M., Guida G., Bertolini F., Stefano A.D., Carriero V. Phenotype Overlap in the Natural History of Asthma. Eur. Respir. Rev. 2023;32:220201. doi: 10.1183/16000617.0201-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Frey U., Suki B. Complexity of Chronic Asthma and Chronic Obstructive Pulmonary Disease: Implications for Risk Assessment, and Disease Progression and Control. Lancet. 2008;372:1088–1099. doi: 10.1016/S0140-6736(08)61450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.González-Pérez R., Poza-Guedes P., Mederos-Luis E., Sánchez-Machín I. Real-Life Performance of Mepolizumab in T2-High Severe Refractory Asthma with the Overlapping Eosinophilic-Allergic Phenotype. Biomedicines. 2022;10:2635. doi: 10.3390/biomedicines10102635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim K.W., Ober C. Lessons Learned from GWAS of Asthma. Allergy Asthma Immunol. Res. 2019;11:170–187. doi: 10.4168/aair.2019.11.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sollis E., Mosaku A., Abid A., Buniello A., Cerezo M., Gil L., Groza T., Güneş O., Hall P., Hayhurst J., et al. The NHGRI-EBI GWAS Catalog: Knowledgebase and Deposition Resource. Nucleic Acids Res. 2023;51:D977–D985. doi: 10.1093/nar/gkac1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sakaue S., Kanai M., Tanigawa Y., Karjalainen J., Kurki M., Koshiba S., Narita A., Konuma T., Yamamoto K., Akiyama M., et al. A Cross-Population Atlas of Genetic Associations for 220 Human Phenotypes. Nat. Genet. 2021;53:1415–1424. doi: 10.1038/s41588-021-00931-x. [DOI] [PubMed] [Google Scholar]
- 84.Tsuo K., Zhou W., Wang Y., Kanai M., Namba S., Gupta R., Majara L., Nkambule L.L., Morisaki T., Okada Y., et al. Multi-Ancestry Meta-Analysis of Asthma Identifies Novel Associations and Highlights the Value of Increased Power and Diversity. Cell Genom. 2022;2:100212. doi: 10.1016/j.xgen.2022.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Herrera-Luis E., Forno E., Celedón J.C., Pino-Yanes M. Asthma Exacerbations: The Genes Behind the Scenes. J. Investig. Allergol. Clin. Immunol. 2023;33:76–94. doi: 10.18176/jiaci.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hernandez-Pacheco N., Pino-Yanes M., Flores C. Genomic Predictors of Asthma Phenotypes and Treatment Response. Front. Pediatr. 2019;7:6. doi: 10.3389/fped.2019.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Perez-Garcia J., Herrera-Luis E., Lorenzo-Diaz F., González M., Sardón O., Villar J., Pino-Yanes M. Precision Medicine in Childhood Asthma: Omic Studies of Treatment Response. Int. J. Mol. Sci. 2020;21:2908. doi: 10.3390/ijms21082908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hernandez-Pacheco N., Kere M., Melén E. Gene-Environment Interactions in Childhood Asthma Revisited; Expanding the Interaction Concept. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2022;33:e13780. doi: 10.1111/pai.13780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sarnowski C., Sugier P.-E., Granell R., Jarvis D., Dizier M.-H., Ege M., Imboden M., Laprise C., Khusnutdinova E.K., Freidin M.B., et al. Identification of a New Locus at 16q12 Associated with Time to Asthma Onset. J. Allergy Clin. Immunol. 2016;138:1071–1080. doi: 10.1016/j.jaci.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 90.Pividori M., Schoettler N., Nicolae D.L., Ober C., Im H.K. Shared and Distinct Genetic Risk Factors for Childhood-Onset and Adult-Onset Asthma: Genome-Wide and Transcriptome-Wide Studies. Lancet Respir. Med. 2019;7:509–522. doi: 10.1016/S2213-2600(19)30055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bi W., Fritsche L.G., Mukherjee B., Kim S., Lee S. A Fast and Accurate Method for Genome-Wide Time-to-Event Data Analysis and Its Application to UK Biobank. Am. J. Hum. Genet. 2020;107:222–233. doi: 10.1016/j.ajhg.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li N., Zhai Z., Chen Y., Li X. Transcriptomic and Immunologic Implications of the Epithelial-Mesenchymal Transition Model Reveal a Novel Role of SFTA2 in Prognosis of Non-Small-Cell Lung Carcinoma. Front. Genet. 2022;13:911801. doi: 10.3389/fgene.2022.911801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shrine N., Portelli M.A., John C., Soler Artigas M., Bennett N., Hall R., Lewis J., Henry A.P., Billington C.K., Ahmad A., et al. Moderate-to-Severe Asthma in Individuals of European Ancestry: A Genome-Wide Association Study. Lancet Respir. Med. 2019;7:20–34. doi: 10.1016/S2213-2600(18)30389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chang D., Hunkapiller J., Bhangale T., Reeder J., Mukhyala K., Tom J., Cowgill A., Vogel J., Forrest W.F., Khan Z., et al. A Whole Genome Sequencing Study of Moderate to Severe Asthma Identifies a Lung Function Locus Associated with Asthma Risk. Sci. Rep. 2022;12:5574. doi: 10.1038/s41598-022-09447-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wu K., Gamazon E.R., Im H.K., Geeleher P., White S.R., Solway J., Clemmer G.L., Weiss S.T., Tantisira K.G., Cox N.J., et al. Genome-Wide Interrogation of Longitudinal FEV1 in Children with Asthma. Am. J. Respir. Crit. Care Med. 2014;190:619–627. doi: 10.1164/rccm.201403-0460OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li X., Hawkins G.A., Ampleford E.J., Moore W.C., Li H., Hastie A.T., Howard T.D., Boushey H.A., Busse W.W., Calhoun W.J., et al. Genome-Wide Association Study Identifies TH1 Pathway Genes Associated with Lung Function in Asthmatic Patients. J. Allergy Clin. Immunol. 2013;132:313–320.e15. doi: 10.1016/j.jaci.2013.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vonk J.M., Nieuwenhuis M.A.E., Dijk F.N., Boudier A., Siroux V., Bouzigon E., Probst-Hensch N., Imboden M., Keidel D., Sin D., et al. Novel Genes and Insights in Complete Asthma Remission: A Genome-Wide Association Study on Clinical and Complete Asthma Remission. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2018;48:1286–1296. doi: 10.1111/cea.13181. [DOI] [PubMed] [Google Scholar]
- 98.Teumer A., Li Y., Ghasemi S., Prins B.P., Wuttke M., Hermle T., Giri A., Sieber K.B., Qiu C., Kirsten H., et al. Genome-Wide Association Meta-Analyses and Fine-Mapping Elucidate Pathways Influencing Albuminuria. Nat. Commun. 2019;10:4130. doi: 10.1038/s41467-019-11576-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Oelsner E.C., Balte P.P., Grams M.E., Cassano P.A., Jacobs D.R., Barr R.G., Burkart K.M., Kalhan R., Kronmal R., Loehr L.R., et al. Albuminuria, Lung Function Decline, and Risk of Incident Chronic Obstructive Pulmonary Disease. The NHLBI Pooled Cohorts Study. Am. J. Respir. Crit. Care Med. 2019;199:321–332. doi: 10.1164/rccm.201803-0402OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bolotova E.V., Dudnikova A.V., Chulkova A.O. Frequency of Albuminuria in Patients with Bronchial Obstructive Diseases. Adv. Gerontol. Uspekhi Gerontol. 2021;34:272–276. [PubMed] [Google Scholar]
- 101.Jackman J.K., Stockwell A., Choy D.F., Xie M.M., Lu P., Jia G., Li H., Abbas A.R., Bronson P.G., Lin W.-Y., et al. Genome-Wide Association Study Identifies Kallikrein 5 in Type 2 Inflammation-Low Asthma. J. Allergy Clin. Immunol. 2022;150:972–978.e7. doi: 10.1016/j.jaci.2022.03.033. [DOI] [PubMed] [Google Scholar]
- 102.Kim J.-H., Cheong H.S., Park J.S., Jang A.-S., Uh S.-T., Kim Y.-H., Kim M.-K., Choi I.S., Cho S.H., Choi B.W., et al. A Genome-Wide Association Study of Total Serum and Mite-Specific IgEs in Asthma Patients. PLoS ONE. 2013;8:e71958. doi: 10.1371/journal.pone.0071958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yick C.Y., Zwinderman A.H., Kunst P.W., Grünberg K., Mauad T., Fluiter K., Bel E.H., Lutter R., Baas F., Sterk P.J. Glucocorticoid-Induced Changes in Gene Expression of Airway Smooth Muscle in Patients with Asthma. Am. J. Respir. Crit. Care Med. 2013;187:1076–1084. doi: 10.1164/rccm.201210-1886OC. [DOI] [PubMed] [Google Scholar]
- 104.Vernet R., Matran R., Zerimech F., Madore A.-M., Lavoie M.-E., Gagnon P.-A., Mohamdi H., Margaritte-Jeannin P., Siroux V., Dizier M.-H., et al. Identification of Novel Genes Influencing Eosinophil-Specific Protein Levels in Asthma Families. J. Allergy Clin. Immunol. 2022;150:1168–1177. doi: 10.1016/j.jaci.2022.05.017. [DOI] [PubMed] [Google Scholar]
- 105.Mills M.C., Rahal C. A Scientometric Review of Genome-Wide Association Studies. Commun. Biol. 2019;2:9. doi: 10.1038/s42003-018-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Martin A.R., Kanai M., Kamatani Y., Okada Y., Neale B.M., Daly M.J. Clinical Use of Current Polygenic Risk Scores May Exacerbate Health Disparities. Nat. Genet. 2019;51:584–591. doi: 10.1038/s41588-019-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Levin A.M., Gui H., Hernandez-Pacheco N., Yang M., Xiao S., Yang J.J., Hochstadt S., Barczak A.J., Eckalbar W.L., Rynkowski D., et al. Integrative Approach Identifies Corticosteroid Response Variant in Diverse Populations with Asthma. J. Allergy Clin. Immunol. 2019;143:1791–1802. doi: 10.1016/j.jaci.2018.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Herrera-Luis E., Mak A.C.Y., Perez-Garcia J., Martin-Gonzalez E., Eng C., Beckman K.B., Huntsman S., Hu D., González-Pérez R., Hernández-Pérez J.M., et al. Admixture Mapping of Severe Asthma Exacerbations in Hispanic/Latino Children and Youth. Thorax. 2023;78:233–241. doi: 10.1136/thorax-2022-218755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Spear M.L., Hu D., Pino-Yanes M., Huntsman S., Eng C., Levin A.M., Ortega V.E., White M.J., McGarry M.E., Thakur N., et al. A Genome-Wide Association and Admixture Mapping Study of Bronchodilator Drug Response in African Americans with Asthma. Pharmacogenomics J. 2019;19:249–259. doi: 10.1038/s41397-018-0042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ortega V.E., Daya M., Szefler S.J., Bleecker E.R., Chinchilli V.M., Phipatanakul W., Mauger D., Martinez F.D., Herrera-Luis E., Pino-Yanes M., et al. Pharmacogenetic Studies of Long-Acting β Agonist and Inhaled Corticosteroid Responsiveness in Randomised Controlled Trials of Individuals of African Descent with Asthma. Lancet Child Adolesc. Health. 2021;5:862–872. doi: 10.1016/S2352-4642(21)00268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gudbjartsson D.F., Bjornsdottir U.S., Halapi E., Helgadottir A., Sulem P., Jonsdottir G.M., Thorleifsson G., Helgadottir H., Steinthorsdottir V., Stefansson H., et al. Sequence Variants Affecting Eosinophil Numbers Associate with Asthma and Myocardial Infarction. Nat. Genet. 2009;41:342–347. doi: 10.1038/ng.323. [DOI] [PubMed] [Google Scholar]
- 112.Schofield J.P.R., Burg D., Nicholas B., Strazzeri F., Brandsma J., Staykova D., Folisi C., Bansal A.T., Xian Y., Guo Y., et al. Stratification of Asthma Phenotypes by Airway Proteomic Signatures. J. Allergy Clin. Immunol. 2019;144:70–82. doi: 10.1016/j.jaci.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 113.Hernandez-Pacheco N., Gorenjak M., Jurgec S., Corrales A., Jorgensen A., Karimi L., Vijverberg S.J., Berce V., Schieck M., Acosta-Herrera M., et al. Combined Analysis of Transcriptomic and Genetic Data for the Identification of Loci Involved in Glucocorticosteroid Response in Asthma. Allergy. 2021;76:1238–1243. doi: 10.1111/all.14552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Singh P., Sharma A., Jha R., Arora S., Ahmad R., Rahmani A.H., Almatroodi S.A., Dohare R., Syed M.A. Transcriptomic Analysis Delineates Potential Signature Genes and MiRNAs Associated with the Pathogenesis of Asthma. Sci. Rep. 2020;10:13354. doi: 10.1038/s41598-020-70368-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhu T., Zhang X., Chen X., Brown A.P., Weirauch M.T., Guilbert T.W., Khurana Hershey G.K., Biagini J.M., Ji H. Nasal DNA Methylation Differentiates Severe from Non-Severe Asthma in African-American Children. Allergy. 2021;76:1836–1845. doi: 10.1111/all.14655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Milger K., Götschke J., Krause L., Nathan P., Alessandrini F., Tufman A., Fischer R., Bartel S., Theis F.J., Behr J., et al. Identification of a Plasma MiRNA Biomarker Signature for Allergic Asthma: A Translational Approach. Allergy. 2017;72:1962–1971. doi: 10.1111/all.13205. [DOI] [PubMed] [Google Scholar]
- 117.Jia G., Zhong X., Im H.K., Schoettler N., Pividori M., Hogarth D.K., Sperling A.I., White S.R., Naureckas E.T., Lyttle C.S., et al. Discerning Asthma Endotypes through Comorbidity Mapping. Nat. Commun. 2022;13:6712. doi: 10.1038/s41467-022-33628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jiang X., Zhang M.J., Zhang Y., Durvasula A., Inouye M., Holmes C., Price A.L., McVean G. Age-dependent topic modelling of comorbidities in UK Biobank identifies disease subtypes with differential genetic risk. Res. Sq. 2022 doi: 10.21203/rs.3.rs-2320352/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Siroux V., González J.R., Bouzigon E., Curjuric I., Boudier A., Imboden M., Anto J.M., Gut I., Jarvis D., Lathrop M., et al. Genetic Heterogeneity of Asthma Phenotypes Identified by a Clustering Approach. Eur. Respir. J. 2014;43:439–452. doi: 10.1183/09031936.00032713. [DOI] [PubMed] [Google Scholar]
- 120.Dahl A., Zaitlen N. Genetic Influences on Disease Subtypes. Annu. Rev. Genom. Hum. Genet. 2020;21:413–435. doi: 10.1146/annurev-genom-120319-095026. [DOI] [PubMed] [Google Scholar]
- 121.Guo H., An J., Yu Z. Identifying Shared Risk Genes for Asthma, Hay Fever, and Eczema by Multi-Trait and Multiomic Association Analyses. Front. Genet. 2020;11:270. doi: 10.3389/fgene.2020.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhu Z., Lee P.H., Chaffin M.D., Chung W., Loh P.-R., Lu Q., Christiani D.C., Liang L. A Genome-Wide Cross-Trait Analysis from UK Biobank Highlights the Shared Genetic Architecture of Asthma and Allergic Diseases. Nat. Genet. 2018;50:857–864. doi: 10.1038/s41588-018-0121-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shirai Y., Nakanishi Y., Suzuki A., Konaka H., Nishikawa R., Sonehara K., Namba S., Tanaka H., Masuda T., Yaga M., et al. Multi-Trait and Cross-Population Genome-Wide Association Studies across Autoimmune and Allergic Diseases Identify Shared and Distinct Genetic Component. Ann. Rheum. Dis. 2022;81:1301–1312. doi: 10.1136/annrheumdis-2022-222460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ziyatdinov A., Hobbs B.D., Kanaan-Izquierdo S., Moll M., Sakornsakolpat P., Shrine N., Chen J., Song K., Bowler R.P., Castaldi P.J., et al. Identifying COPD Subtypes Using Multi-Trait Genetics. medRxiv. 2023 doi: 10.1101/2023.02.20.23286186. [DOI] [Google Scholar]
- 125.Knapp E.A., Kress A.M., Parker C.B., Page G.P., McArthur K., Gachigi K.K., Alshawabkeh A.N., Aschner J.L., Bastain T.M., Breton C.V., et al. The Environmental Influences on Child Health Outcomes (ECHO)-Wide Cohort. Am. J. Epidemiol. 2023;192:1249–1263. doi: 10.1093/aje/kwad071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ramirez A.H., Sulieman L., Schlueter D.J., Halvorson A., Qian J., Ratsimbazafy F., Loperena R., Mayo K., Basford M., Deflaux N., et al. The All of Us Research Program: Data quality, utility, and diversity. Patterns. 2022;3:100570. doi: 10.1016/j.patter.2022.100570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Forno E., Wang T., Yan Q., Brehm J., Acosta-Perez E., Colon-Semidey A., Alvarez M., Boutaoui N., Cloutier M.M., Alcorn J.F., et al. A Multiomics Approach to Identify Genes Associated with Childhood Asthma Risk and Morbidity. Am. J. Respir. Cell Mol. Biol. 2017;57:439–447. doi: 10.1165/rcmb.2017-0002OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Soliai M.M., Kato A., Helling B.A., Stanhope C.T., Norton J.E., Naughton K.A., Klinger A.I., Thompson E.E., Clay S.M., Kim S., et al. Multi-omics colocalization with genome-wide association studies reveals a context-specific genetic mechanism at a childhood onset asthma risk locus. Genome Med. 2021;13:157. doi: 10.1186/s13073-021-00967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gautam Y., Johansson E., Mersha T.B. Multi-Omics Profiling Approach to Asthma: An Evolving Paradigm. J. Pers. Med. 2022;12:66. doi: 10.3390/jpm12010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zheng Z., Huang D., Wang J., Zhao K., Zhou Y., Guo Z., Zhai S., Xu H., Cui H., Yao H., et al. QTLbase: An integrative resource for quantitative trait loci across multiple human molecular phenotypes. Nucleic Acids Res. 2020;48:D983–D991. doi: 10.1093/nar/gkz888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Buniello A., MacArthur J.A.L., Cerezo M., Harris L.W., Hayhurst J., Malangone C., McMahon A., Morales J., Mountjoy E., Sollis E., et al. The NHGRI-EBI GWAS Catalog of Published Genome-Wide Association Studies, Targeted Arrays and Summary Statistics 2019. Nucleic Acids Res. 2019;47:D1005–D1012. doi: 10.1093/nar/gky1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mills M.C., Rahal C. The GWAS Diversity Monitor Tracks Diversity by Disease in Real Time. Nat. Genet. 2020;52:242–243. doi: 10.1038/s41588-020-0580-y. [DOI] [PubMed] [Google Scholar]
- 133.Fantini D. easyPubMed: Search and Retrieve Scientific Publication Records from PubMed. 2019. R Package Version 2.13. [(accessed on 27 August 2023)]. Available online: https://CRAN.R-project.org/package=easyPubMed.
- 134.McLean C.Y., Bristor D., Hiller M., Clarke S.L., Schaar B.T., Lowe C.B., Wenger A.M., Bejerano G. GREAT Improves Functional Interpretation of Cis-Regulatory Regions. Nat. Biotechnol. 2010;28:495–501. doi: 10.1038/nbt.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Raudvere U., Kolberg L., Kuzmin I., Arak T., Adler P., Peterson H., Vilo J. g:Profiler: A web server for functional enrichment analysis and conversions of gene lists (2019 update) Nucleic Acids Res. 2019;47:W191–W198. doi: 10.1093/nar/gkz369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhou Y., Zhou B., Pache L., Chang M., Khodabakhshi A.H., Tanaseichuk O., Benner C., Chanda S.K. Metascape Provides a Biologist-Oriented Resource for the Analysis of Systems-Level Datasets. Nat. Commun. 2019;10:1523. doi: 10.1038/s41467-019-09234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Szklarczyk D., Gable A.L., Lyon D., Junge A., Wyder S., Huerta-Cepas J., Simonovic M., Doncheva N.T., Morris J.H., Bork P., et al. STRING V11: Protein-Protein Association Networks with Increased Coverage, Supporting Functional Discovery in Genome-Wide Experimental Datasets. Nucleic Acids Res. 2019;47:D607–D613. doi: 10.1093/nar/gky1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Stark C., Breitkreutz B.-J., Reguly T., Boucher L., Breitkreutz A., Tyers M. BioGRID: A General Repository for Interaction Datasets. Nucleic Acids Res. 2006;34:D535–D539. doi: 10.1093/nar/gkj109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bader G.D., Hogue C.W.V. An Automated Method for Finding Molecular Complexes in Large Protein Interaction Networks. BMC Bioinform. 2003;4:2. doi: 10.1186/1471-2105-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data necessary to evaluate the conclusions of this manuscript are available in the NHGRI-EBI GWAS Catalog and reported in the main text and/or Appendix A.