Abstract
Pulmonary valve (PV) fibroelastomas are a rare pathology, with limited anecdotal literature surrounding them. Consequently, the natural history is unclear; however, two features have remained salient; they are asymptomatic and found incidentally. Here, we describe a 52-year-old female, presenting with symptoms suggestive pulmonary embolism (PE). Pulmonary angiography revealed a filling deficit in the pulmonary trunk (PT), adjacent to the PV. Subsequent investigation found a large PV fibroelastoma. The presence of symptoms is likely secondary to right ventricular outflow tract obstruction from the lesions large size. We describe our investigation and management of the lesion. The reporting of this case challenges the existing knowledge of PV fibroelastomas.
Keywords: fibroelastoma, pulmonary valve, cardiac surgery, pulmonary embolism, cardiac tumour
Introduction
Papillary fibroelastomas (PFEs) are benign neoplasms of the endocardium, commonly affecting left-sided heart valves. The incidence rate is between 0.0017 and 0.33%, ~95% are on the aortic or mitral valves [1, 2]. Right-sided PFEs are commonly asymptomatic and identified incidentally, least commonly affecting the pulmonary valve (PV). The literature to-date is largely anecdotal and the natural history of right-sided PFE is poorly understood. Consequently, the in-vivo risk of embolization, morbidity, and mortality associated with right-sided PFEs is unknown, noting the increasing observation of these lesions post-mortem [2]. However, due to the morphology of PFEs and known risk of embolic sequelae noted in left-sided PFEs, right-sided PFEs have historically been treated with excision. Shave excision is considered curative for PFEs with low risk of recurrence [3]. Here, we describe an unusual symptomatic presentation of PFE and our surgical technique for excision.
Case summary
A 52-year-old female presented with dyspnoea and atypical chest pain. On a background of alcoholic pancreatitis, type 2 diabetes mellitus and cigarette use, without history of recent surgery, immobilization, malignancy, or travel.
Examination was unremarkable.
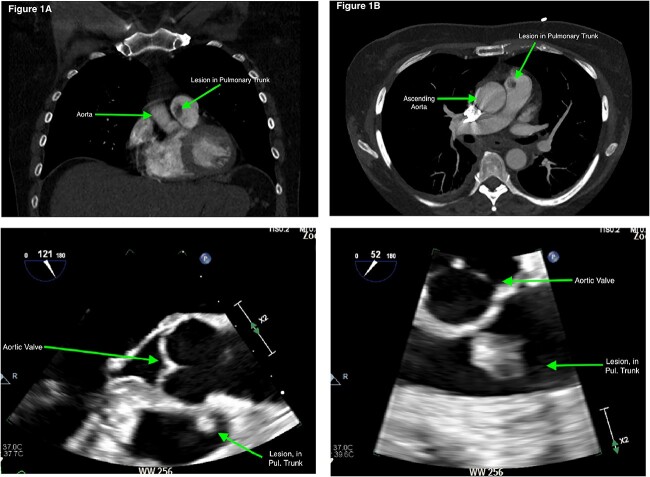
Acute coronary syndrome was excluded. A differential of pulmonary embolism (PE) was considered given the D-dimer was 5.4 mg/L. A computerized tomography of the pulmonary arteries (CTPA) was negative for PE but demonstrated a filling defect in the pulmonary trunk (PT) (Fig. 1a and b). The lesion was closely associated with the PV. Differentials included PV vegetation, thrombus, or cardiac tumour.
Figure 1.
(a) and (b) Computerized tomography scan (coronal and axial slices) demonstrating filling defect in the pulmonary trunk. (c) and (d) TOE images of the PV lesion.
Blood and urine cultures were negative and inflammatory markers were normal. Transthoracic echocardiography (TTE) demonstrated a structurally and functionally normal heart with a mobile echogenic mass on the PV attached to the anterior leaflet. The PV looked morphologically and functionally normal. A transoesophageal echocardiogram (TOE) demonstrated a homogenous hyperechogenic and highly mobile mass on the PV measuring 10 × 13 mm on the anterior leaflet, concerning for a cardiac tumour, its appearance not suggestive of a clot or vegetation (see Video 1, Fig. 1c and d). Given the large size of the tumour urgent cardiothoracic review was sought and excision was recommended.
A median sternotomy was performed. The lesion was identified using intraoperative ultrasound. Routine cardiopulmonary bypass (CPB) was initiated. Anterograde cold-blood cardioplegia was given with passive cooling to 35°C. A longitudinal incision of the PT revealed the mass (Fig. 2a), which appeared gelatinous, and was adherent to the free edge of left cusp of the PV. The lesion was shaved off the PV (Fig. 2b). The PV was macroscopically/morphologically unremarkable. The PT was irrigated with water and closed in layers. The patient was de-aired and weaned from CPB. The cross-clamp time was 16 min and CPB-time of 27 min. Postoperative recovery was unremarkable.
Figure 2.
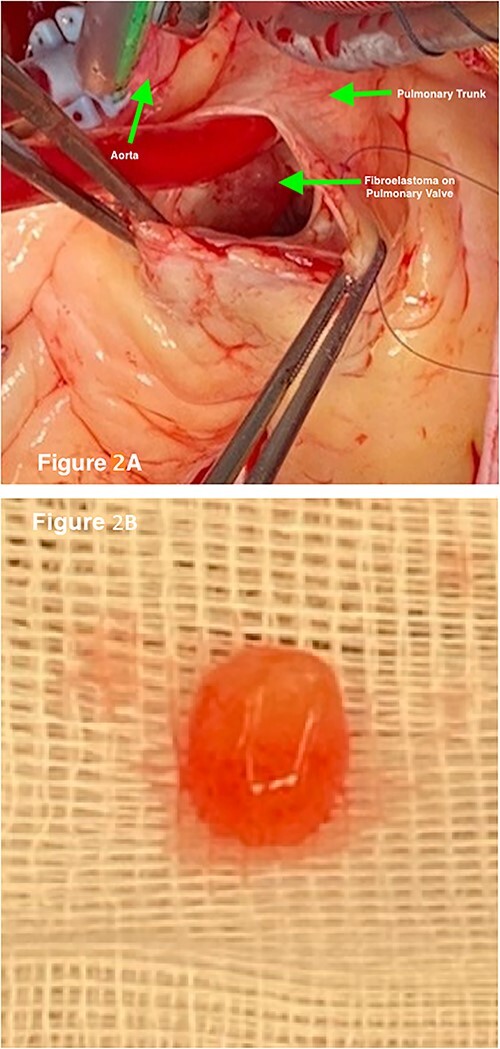
(a) Intraoperative imaging demonstrates the gelatinous lesion on the leaflet of the PV after opening the pulmonary trunk. (b) Excised PV papillary fibroelastoma.
Histology demonstrated endocardium lining branching papillary structures with avascular cores, consistent with a PFE.
Discussion
PFEs have been mistaken for PEs although they are rarely considered as a differential diagnosis for PE [4, 5]. Given the exceeding rarity of PFEs, it is permissible to overlook them in most presentations, but they should be acknowledged to prevent misdiagnosis.
Symptomatic presentations with dyspnoea and chest pain are atypical for PV PFEs. Given the size of the lesion and its location, these symptoms are hypothesized to be due to right ventricular outflow tract obstruction. This is seldom described in the literature, even with similar sized PFEs. The decision for prompt surgical excision in this case was supported by the risk of fatal embolization.
Conclusion
PV PFEs are a rare cardiac tumour. The experience with PFEs to-date and the histological examination of their structure poses a significant risk of morbidity and mortality secondary to embolization and so they should be treated aggressively. In the absence of a robust literature basis or standardized guidelines, we recommend excision of right-sided PFEs to prevent morbidity or mortality from embolization, particularly in symptomatic patients.
Supplementary Material
Footnotes
†Poster presentation at the CSANZ 46th Annual Scientific Meeting, Gold Coast, August 2022.
Contributor Information
Frazer Kirk, Department of Cardiothoracic Surgery, Gold Coast University Hospital, 1 Hospital Boulevard, Southport, QLD 4215, Australia; College of Medicine and Dentistry, Griffith University Hospital, Gold Coast, QLD 4215, Australia.
Matthew S Yong, Department of Cardiothoracic Surgery, Gold Coast University Hospital, 1 Hospital Boulevard, Southport, QLD 4215, Australia; College of Medicine and Dentistry, Griffith University Hospital, Gold Coast, QLD 4215, Australia.
Peter Williams, Department of Cardiac Anaesthesia, Gold Coast University Hospital, 1 Hospital Boulevard, Southport, QLD 4215, Australia.
Andrie Stroebel, College of Medicine and Dentistry, Griffith University Hospital, Gold Coast, QLD 4215, Australia.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
The data underlying this article cannot be shared for the confidentiality/privacy of the patient involved.
Ethical approval
Written consent for publication was provided by the patient. Gold Coast University Hospital and Health Service Human Research Ethics Committee and granted ethical clearance: EX/2022/QGC/81799.
References
- 1. Biocic S, Puksic S, Vincelj J. et al. Pulmonary valve papillary fibroelastoma diagnosed by echocardiography: a case report. Eur J Echocardiogr 2009;10:726–8. [DOI] [PubMed] [Google Scholar]
- 2. Daccarett M, Burke P, Saba S. Incidental finding of a large pulmonary valve fibroelastoma: a case report. Eur J Echocardiogr 2006;7:253–6. [DOI] [PubMed] [Google Scholar]
- 3. Nadal J, Nelson A, Edwards J. Giant papillary fibroelastoma: a case report and review of the literature. Heart, Lung Circulation 2018;27:S572. [Google Scholar]
- 4. Generali T, Tessitore G, Mushtaq S. et al. Pulmonary valve papillary fibroelastoma: management of an unusual, tricky pathology. Interact Cardiovasc Thorac Surg 2013;16:88–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Molnar A, Encica S, Kovacs E. et al. Papillary fibroelastoma of the pulmonary valve: a case report. Rom J Morphol Embryol 2014;55:463–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared for the confidentiality/privacy of the patient involved.