Abstract
Over the past two years, the COVID-19 pandemic has seen multiple waves with high morbidity and mortality. Lockdowns and other prompt responses helped India's situation become less severe. Although Malegaon in the Indian state of Maharashtra has a high population density, poor hygienic standards, and oppositional local community views toward national pandemic addressing measures, it is nevertheless reasonably safe. To understand the possible reasons serosurvey was conducted to estimate the anti-SARS-CoV-2 neutralizing antibody levels in the Malegaon population. Also, we did SUTRA mathematical modeling to the Malegaon daily data on COVID-19 attributable events and compared it with the National and state level. The case fatality rate (CFR) in Malegaon city for the first, second, and third waves was 3.25%, 2.25%, and 0.39%, respectively. The crude death rate (CDR) for Maharashtra ranked first for the initial two waves and India for the third wave. Malegaon, meanwhile, finished second in the first two waves but fared best in the third. The Vaccination coverage for the first dose before the second wave was only 0.34% but had risen to 64.46% by 12 Oct 2022. By then, the second and booster dose coverage was 27.55% and 2.38%, respectively. Serosurvey did between 12 and 18 Jan 2022 showed a 93.93% anti-SARS-CoV-2 neutralizing antibody presence. SUTRA modeling elucidated the high levels of antibodies due to the pandemic-reach over 102% by the third wave. The serosurvey and the model explain why the pandemic severity in terms of duration and CFR during the subsequent waves, especially third wave, was milder compared to the first wave in spite of low vaccination rates.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12088-023-01096-3.
Keywords: COVID-19, SUTRA, Mathematical modeling, Malegaon, Immunity
Introduction
The COVID-19 pandemic has brought the world to its knees, wreaking havoc on both human health and economies. As scientists and researchers continue to grapple with the challenges posed by the virus, various approaches have been explored to understand its spread and control, including the use of mathematical modeling, development of vaccines and treatments, and investigation of the virus' interaction with host cells. Recent research has also shed light on the role of diet and gut microbiota in COVID-19 outcomes [1]. Meanwhile, the emergence of new waves and variants of the virus, such as the hybrid variants BA(x), XE, XD, and XF, have added to the complexity of the pandemic [2, 3]. Despite the development of repurposed and new therapeutic agents, as well as vaccines, the virus continues to pose challenges with increased transmissibility, virulence, and immune escape. The current status of various therapeutic agents being used or undergoing preclinical and clinical trials to manage COVID-19 can shed light on the ongoing efforts to combat the pandemic [4].
In India, the COVID-19 pandemic has seen multiple waves with high morbidity and mortality, and the initial unpreparedness of the public health infrastructure led to the expectation of significant mortality [5, 6]. Timely interventions such as lockdowns helped reduce the magnitude of the problem [7, 8]. However, the second Delta wave, with the increased transmission and higher requirements of oxygen and intensive care for those hospitalized, came like a Tsunami with many deaths and patients suffering [9, 10]. The pandemic has also had a significant impact on the Indian economy, with businesses and individuals suffering losses and struggling to cope with the fallout [11].
Against this backdrop, the city of Malegaon in Maharashtra, with a population of approximately 5.24 lakhs [12], appeared to be doing reasonably well after the initial brutal wave. This was inspite of the fact that the local people continued to have a poor vaccination rate of 56.47% for the first dose and 13.32% for the second dose till Dec 2021. They refused to wear masks, and social distancing was just not possible in view of the people's population density and economic status. As of now (12 Oct 2022), vaccination rates are 64.46%for the first and 27.55% for the second doses [13].
Malegaon has been an area of concern and attention for the health administration since it is characterized by overcrowding, high population density, suboptimal hygienic conditions, relative poverty, contrarian views of the local community towards the use of face masks, and wanting health infrastructure, especially for people working in closed crowded places on power looms. During the first wave, there had been an enormous number of patients with high mortality, and Malegaon stood out as a hotspot that had overwhelmed the healthcare infrastructure [14]. However, during the second pandemic wave, when the number of cases surged across the State, Malegaon had few cases and a low case fatality rate compared to the rest of the country in spite of the Delta wave being more severe [15].
Therefore, the local administration was keen to understand the possible reasons for a relatively protected population despite poor non-pharmacological interventions. This formed the basis of undertaking a study in Malegaon involving a serosurvey of the randomly selected population and using an Indian mathematical model SUTRA to understand the time series data for the spread of the pandemic in Malegaon.
Material and Methods
The urban Malegaon population has been sero-surveyed for anti-COVID antibody levels. In addition, historical time series data of COVID cases was obtained from the local administration of Malegaon. The “SUTRA” mathematical model developed by M Agrawal et al. [8] was used to analyze the time-series data calibrated to the serosurvey data.
Serosurvey Data Collection
During this survey, subjects above 18-year-old who gave consent for interview and blood collection were enrolled from the urban area of Malegaon city in Nashik District of Maharashtra, India. A total of 2720 subjects were selected between 12 and 18 Jan 2022 using the cluster sampling method, where 72 municipal wards were considered cluster and sampling units as individual subjects. Out of 72 clusters, 16 were divided into four zones North, South, East, and West. However, to have a proportionate distribution of sample from uneven zone distribution of population due to geographical boundaries, 170 subjects were selected from each ward out of five wards from the East zone, two wards from the West zone, seven wards from the South Zone, and two wards from North zone by simple random sample lottery method. Pre-validated case record forms were used, and informed consent was obtained from all individuals.
IgG-Antibody Levels Estimation
Three (03) ml of venous blood was drawn in a plain vacutainer taking aseptic precautions. The separated serum was processed for the detection of IgG antibody levels using J. Mitra & Co.'sCOVID-19 Neutralizing Antibody Micro-ELISA Kit. Individuals with > 30% inhibition on testing were labeled as antibody positive. Data were analyzed using Microsoft excel Sheet and Graph Pad Prism 9 for windows [version 9.0.0 (121)].
Historical Data Collection-
Daily data (till 12 Oct 2022) on the number of individuals taking first, second, and booster vaccination doses, confirmed, recovered, and deceased cases in Malegaon due to COVID-19 were collected from the authorities of Malegaon Municipal Corporation, Malegaon. This data was used to calculate the percentage of total vaccinated individuals and deaths in Malegaon city after the COVID-19 pandemic. In addition, the India and Maharashtra state-level time series for confirmed, recovered, and deceased cases (till 12 Oct 2022) were taken from the data published by the Indian Institute of Technology, Hyderabad [15].
Application of the SUTRA Model
SUTRA is an acronym for Susceptible Undetected Tested Positive (symptomatic and asymptomatic) Removed (recovered or died) Approach and applied to estimate the four parameters viz. β, γ, η, and ε. Where β shows the likelihood of the susceptible individual getting infected, γ shows the recovery rate of patients, η measures the rate at which infected patients die (the presumption is that all asymptomatic patients recover), and ε measures the ratio between infected symptomatic and asymptomatic patient populations. The mathematical model derived its equations through the relationship between total cases, active cases, and mortality in the population obtained as a time series data available in the public domain. The same was calibrated against serosurvey data as well.
Results
Socio-Demographic Characteristics
The demographic characteristics of 2454 subjects are provided in supplementary Table S1. Out of 2454 individuals surveyed, males accounted for 51.26% of the population. The age category of 26–35 years comprised the most proportion with 26.98%, and subjects with 36–45 years came in second (22.66%), while those above 55 years (17.89%) placed in the fourth position. Muslims comprised 75.35% of the population, while Hindus numbered 594 (24.21%).Interestingly, this compared well with the age and religious demographics of the region.
Time Series
Supplementary Table S2 shows the estimated events for the 10 phases' time series data and summarizes daily phase-wise (Mean ± SEM) time series data of Malegaon citizens on COVID-19 confirmed, recovered, and deceased cases from Apr 2020 to Feb 2022. For the Malegaon, the first Phase started on 09 Apr 2020, and a phase change was registered whenever there was a drift of the mathematical model's derived parameters, and the model recalibrated itself. Cumulative records in Malegaon revealed 12,252 confirmed, 11,643 hospitalized, 7666 recovered, and 315 deceased cases between the selected phases.
Wave-wise COVID-19 Attributable Events in Malegaon
The first, second, and third waves for Malegaon approximately lay between 09 Apr 2020 to 14 Nov 2020, 03 Feb 2021 to 06 Jun 2021, and 09 Jan 2022 to 09 Feb 2022, respectively. Table 1 shows the wave-wise comparison of COVID-19-attributable events in Malegaon. Here results showed that the COVID-19 second wave’s mean attributable events were significantly higher than the first and third waves.
Table 1.
Wave-wise comparison of COVID-19 attributable events in Malegaon
| COVID-19 attributable events | Comparison between wavesa | Mean difference | Confidence interval | S.E. of diff | P valueb | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Confirmed | First–Second | − 32.27 | − 41.31 | − 23.22 | 3.843 | < 0.0001* |
| First–Third | − 13.23 | − 28.46 | 2.009 | 6.475 | 0.1035 | |
| Second–Third | 19.04 | 3.072 | 35.01 | 6.786 | 0.0146* | |
| Recovered | First–Second | − 14.68 | − 18.58 | − 10.78 | 1.658 | < 0.0001* |
| First–Third | 2.124 | − 4.448 | 8.695 | 2.793 | 0.7274 | |
| Second–Third | 16.80 | 9.913 | 23.69 | 2.927 | < 0.0001* | |
| Deceased | First–Second | − 0.535 | − 0.8166 | − 0.2535 | 0.1197 | < 0.0001* |
| First–Third | 0.493 | 0.01879 | 0.9676 | 0.2016 | 0.0394* | |
| Second–Third | 1.028 | 0.5311 | 1.525 | 0.2113 | < 0.0001* | |
aDate range for the First wave: 09 Apr 2020 to 14 Nov 2020, Second wave: 03 Feb 2021 to 06 Jun 2021, and Third wave: 09 Jan 2022 to 09 Feb 2022
bAnalyzed by One-way ANOVA Post hoc Tuckey Test
*Statistically significant at 95% confidence interval
COVID-19 Attributable Events at National Versus State Versus Malegaon Level
Supplementary Table S3 shows mean-wise comparisons of daily confirmed, recovered, and deceased cases of COVID-19 disease in India, Maharashtra, and Malegaon levels. Here, the data were rescaled per 100 M population to bring them on the same platform. It was found that Maharashtra had significantly higher average daily confirmed, recovered, and deceased cases than India and Malegaon (p < 0.0001).
Total infections, deceased, case fatality rate (CFR), and Crude Death Rate (CDR-mortality rate per thousand population) during the three COVID- 19 waves at the National (India), State (Maharashtra), and Malegaon city levels are depicted in Table 2. The waves at Malegaon lasted approximately 220, 123, and 31 days for the first, second, and third waves, respectively. However, the second wave in Malegaon lasted a bit longer, and the other two waves stretched over fewer days than the rest of the State.
Table 2.
National versus state versus Malegaon level COVID-19 attributable events at the different waves
| Sr. no | Wave | Region | Start date | End date | Infections | Deceased | CFRa (%) | CDRb |
|---|---|---|---|---|---|---|---|---|
| 1 | First | India | 16-03-2020 | 28-12-2020 | 1,02,24,687 | 1,48,189 | 1.45 | 0.11 |
| Maharashtra | 21-03-2020 | 09-11-2020 | 1,723,083 | 45,325 | 2.63 | 0.36 | ||
| Malegaon | 09-04-2020 | 14-11-2020 | 4185 | 136 | 3.25 | 0.20 | ||
| 2 | Second | India | 11-02-2021 | 19-07-2021 | 2,03,01,942 | 2,59,113 | 1.28 | 0.20 |
| Maharashtra | 01-02-2021 | 02-06-2021 | 37,49,785 | 45,669 | 1.22 | 0.37 | ||
| Malegaon | 03-02-2021 | 06-06-2021 | 6360 | 143 | 2.25 | 0.27 | ||
| 3 | Third | India | 25-12-2021 | 21-03-2022 | 82,32,016 | 36,983 | 0.45 | 0.03 |
| Maharashtra | 04-12-2021 | 01-03-2022 | 12,25,613 | 2548 | 0.21 | 0.02 | ||
| Malegaon | 09-01-2022 | 09-02-2022 | 1032 | 4 | 0.39 | 0.01 |
aCFR-case fatality rate
bCDR-mortality rate per thousand population
However, CDR levels in Maharashtra ranked first for the initial two waves and India for the third wave. At the same time, Malegaon ranked second in the initial two waves and lasted in the third wave for CDR levels.
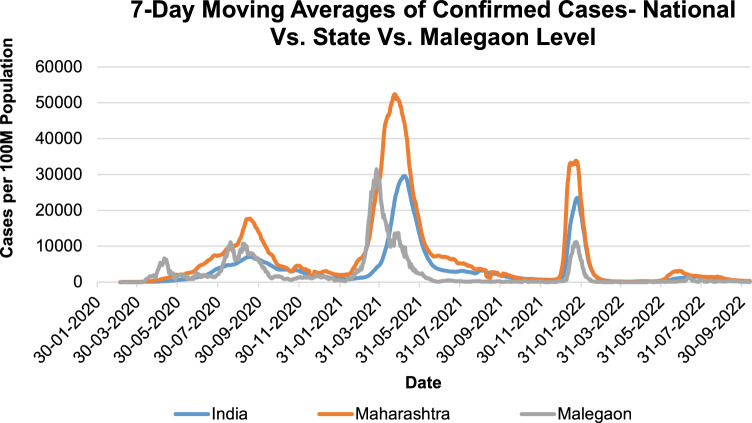
The National versus State versus Malegaon level seven-day moving averages of confirmed cases rescaled data to 100 M per population of the respective region is shown in Fig. 1. Here, the wave-III peak for the Malegaon infections founds around the 3rd week of Jan 2022 was low with a value of 11,207.95, which is only 33.08% and 47.72% of the value shown by Maharashtra (22 Jan 2022) and India (25 Jan 2022) level, respectively.
Fig. 1.
A seven-day moving averages of confirmed cases at National versus State versus Malegaon level. The data for confirmed cases for all the levels, i.e., National, State, and Malegaon, were rescaled and shown in 100 M per population
Vaccination Status
The daily vaccination at Malegaon city from 16 Jan 2021 to 12 Oct 2022 is shown in supplementary Fig S1. In this study period, of the 5.24 lakh individuals in Malegaon city, the first dose coverage was around 64.46%, while the second dose coverage was barely 27.55%. However, the cumulative vaccination count for the booster dose is only 11,928 (2.28%).
In a single day, Malegaon health administrators vaccinated 12,215 individuals with the first dose on 29 Dec 2021, displaying a peak in the vaccination drive. The peak day for the second dose was 28 Mar 2022 (1921 individuals), and the booster dose was 22 Jul 2022 (360 individuals) for the duration studied.
Levels of Anti-SARS-CoV-2 Neutralizing Antibodies in the Individuals
Supplementary Fig. S2. depicts the status of anti-COVID-19 antibodies in the study individuals. Only 6.07% of the subjects were negative for the COVID-19 neutralizing antibody, and 93.93% had significant levels of antibodies (> 30% inhibition).
SUTRA Analysis of Disease Progression in the Urban Malegaon
The SUTRA parameters for the spread of COVID-19 between Apr 2020 and Feb 2022 across phases are depicted in Table 3. There was a significant drift of data values over the period from Apr 2020 to Dec 2021. Thus, this resulted in a phase change reflected in a shift in β and ρ.
Table 3.
Modeling the phases and parameters for a spread of COVID-19 between Apr 2020 and Feb 2022
| Phases | Start date | End date | βa | 1/ϵb | ρc |
|---|---|---|---|---|---|
| Phase 1 | 09-04-2020 | 25-04-2020 | 0.37 ± 0 | 59 | 1.3 ± 0 |
| Phase 2 | 26-04-2020 | 26-05-2020 | 0.31 ± 0.01 | 58.8 ± 0.1 | 7.1 ± 0.3 |
| Phase 3 | 27-05-2020 | 20-06-2020 | 0.2 ± 0.02 | 58.8 ± 0 | 11.7 ± 7.1 |
| Phase 4 | 21-06-2020 | 25-07-2020 | 0.32 ± 0.02 | 58.8 ± 0.1 | 13.9 ± 3.1 |
| Phase 5 | 26-07-2020 | 27-08-2020 | 0.43 ± 0.03 | 58.4 ± 0 | 24.2 ± 2.3 |
| Phase 6 | 28-08-2020 | 17-11-2020 | 0.25 ± 0.01 | 57.9 ± 0 | 45 ± 2.7 |
| Phase 7 | 18-11-2020 | 10-02-2021 | 0.76 ± 0.04 | 57.8 ± 4.3 | 43.8 ± 5 |
| Phase 8 | 11-02-2021 | 11-04-2021 | 0.48 ± 0.01 | 57.4 ± 4.3 | 84.5 ± 4.4 |
| Phase 9 | 12-04-2021 | 30-11-2021 | 0.47 ± 0.02 | 57.4 ± 0.1 | 103.6 ± 4.8 |
| Phase 10 | 01-12-2021 | 19-02-2022 | 3.92 ± 0.11 | 56.4 ± 1.8 | 102.6 ± 2.9 |
aShows the likelihood of the susceptible individual getting infected
bMeasures the ratio between infected symptomatic and asymptomatic patient populations,
cShows the reach of the pandemic
The present serosurvey was used to calibrate the 1/ϵ. Drift in data and parameters correlates with the spread of diseases and the non-pharmacological interventions if any. For example, during the first Wave in Apr 2020, the mortality was high, but by Aug 2020, the reach was around 30%. Then, with the lockdown lifted, the β increased significantly, resulting in high transmission.
During the second wave, the reach increased rapidly to 86% by April 2021. However, after that, it decreased slightly due to possibly waning immunity and not adequate vaccination. Third-wave was relatively small, suggesting high immunity among the population.
The mathematical model and predictions are further depicted in supplementary Fig S3 for Malegaon city, which illustrates that the projected trajectory superimposes the actual time series, thereby validating the parameters derived through 'SUTRA.’ Similarly supplementary Fig S4 shows the model predictions for India.
Discussion
COVID-19 has become the most prominent health catastrophe of the twenty-first century [16]. Until 17 Jul 2022; COVID-19 has caused approximately 0.63 billion infections and 6.59 million fatalities. At the same time, India has reported 44.65 illnesses and 0.53 million losses of life attributable to COVID-19 [17]. The global distribution of COVID-19 disease and associated mortality has been incredibly unequal between and across nations [16]. So, to understand COVID-19, several research institutions have conducted serosurveys in different districts of Maharashtra [18, 19].
However, to the best of our knowledge, this is the first Mathematical modeling study using a serosurvey with a generalizable sample size focusing on Malegaon and the SUTRA model. Malegaon is a densely populated city in Maharashtra's Nashik district [20]. Therefore, implementing the lockdown in Malegaon city was a very challenging task for the Government officials considering the population and way of life in Malegaon. Our survey showed that Malegaon has a diverse socio-demography, with a Muslim community residing approximately 75%.
The Nation, State, and Malegaon region got affected by three significant waves, first by COVID-19 native strain, second by Delta variant, and third by Omicron. In the first wave, Malegaon was a focus of infection with 3.25% CFR. A total of 136 out of 4185 COVID-19 cases died. Of 6360 cases diagnosed during the second wave 143 died, representing a CFR of 2.25%. At the same time, the National CFR was 1.45% and 1.28%, respectively. The CFR in Malegaon was significantly higher than the National and State figures during the first two waves. Important to note was that only four deaths were noted among 1032 infected in Malegaon, with a markedly lower CFR of 0.39% in the third wave of pandemic.
Analysis of the COVID-19 attributable events from 09 Apr 2020 to 19 Feb 2022 in Malegaon showed that in the initial phases, the hospital admissions were more than the infected cases, which might be the effect of the preventive measures taken by the Malegaon Corporation for the suspected cases. Also, the cumulative records in the phases studied revealed that, out of the 12,252 who had a positive outcome, death occurred in 2.57%. It shows that COVID-19 severely impacted this city compared to the global data. However, if we look at the statistics from the entire Malegaon population view, only 2.22% of the population required hospitalization, and 0.06% died by 19 Feb 2022. Similarly, 0.026%, 0.027%, and 0.001% deaths were noted in the first, second, and third waves against the Malegaon population. Findings show that the effect of COVID-19 was more severe during the first and second waves at Malegaon.
Initially, there seemed to be a lot of misunderstanding in this area about the subject of Corona as a whole. Simultaneously, communally-sensitive WhatsApp messages were doing the rounds. As a result, people with symptoms stopped going to doctors for fear of the entire family being quarantined [20]. During the survey, a large number of residents mentioned trying out home and other remedies such as Unani Kadha, Ayurvedic formulations, Vitamin C and Zinc tablets, and Arsenic album (homeopathic formulation), and not presenting for a vaccination drive run by the government.
Even during all three waves of the pandemic, locals on a colossal scale violated COVID-19 appropriate behavior [21]. We also observed large crowds at weddings, public functions, and markets during the survey. We found that they had forgotten the use of masks, safe distances, and sanitizers. Additionally, Malegaon's vaccination rate has been significantly lower. The first dose coverage was roughly 64.46%, and the second dose coverage was only 27.55% of the 5.24 lakh beneficiaries in Malegaon town, even at the time of the second wave. Most of the town's recipients in the eastern district especially had reservations about the vaccine, which could have contributed to not completing even 70% first dose of vaccination.
When we observed the data for CDR, Malegaon contributed more than the national average for the first and second waves but showed a very negligible contribution for the third. However, the number of individuals affected by COVID-19 was less in the third wave, contributing to the lower number of the denominator in CFR calculation. The reasons for this are well explained by the high seroprevalence and its effect on the SUTRA parameters.
Remarkably, the Indian Council of Medical Research serosurvey showed a higher antibody presence in 2021 in the individuals (89.8%, 95% CI 88.4–91.1%) who received two doses of the COVID-19 vaccine than those who were unvaccinated (62.3%, 95% CI 60.9–63.7%) [22]. In contrast to other studies [23, 24], though vaccination status is low, our study found that 94% of the population had positive neutralizing antibody status. According to earlier surveys conducted in India, the COVID-19 seroprevalence is increasing every month [25–33]. The SUTRA parameters also support the same, in which the reach of a pandemic was more than 102% by December 2021. Despite having a low COVID-19 vaccination status, the general population in Malegaon has developed background immunity due to a markedly higher natural infection during the second wave. The COVID-19 pandemic, like all other pandemics, is affected by complexities such as the differential evolution of the infection in separate geographical regions and distinct communities. Intrinsic epidemiological factors may often outweigh the infectivity potential of the microbe and host vulnerability. In this context, human behavior and community response, with particular reference to general awareness, play a significant role in the success or failure of any healthcare strategy [34].
To summarize, the high infection rate in the first wave with high seroprevalence due to natural infection did not wane with time compared to the rest of the country; the population of Malegaon remains relatively protected from the severity of the disease.
Conclusions
Malegaon was affected by the COVID-19 Native strain sometime around Apr 2020, with relatively high mortality. Still, the reach of the pandemic was just about 30% of the population by the time the wave ebbed. The Delta wave peaked around Apr 2021, taking the reach to 85% population. The mortality was much lower despite poor vaccination status. A rapid increase in β due to high transmission resulted in the reach covering a large population. By Dec 2021, the reach increased to 102.6, suggesting a fair number of cases of reinfection, keeping mortality low. The omicron wave was very small and short as the population's immunity was high and well sustained after the first and second waves.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge Municipal Corporation of Malegaon, Nashik; Motiwala (National) Homoeopathic Medical College & Hospital, Nashik; Mohammadia Tibbia College and Assayer Hospital, Malegaon; KC Ajmera Ayurved College, Dhule; Alameen Unani Medical College, Malegaon; JMF’s ACPM Medical College and Hospital, Dhule for their unrelenting help in serosurvey data collection and Shree Bhausaheb Hire Govt. Medical College, Dhule, for their contribution to estimating IgG antibody levels. We are very grateful to Mr. Yogesh Raut and Mr. Pravin Ghatekar from Maharashtra University of Health Sciences Nashik for the statistical assistance.
Author Contributions
Conceptualization: Dr. MK; Design: Mr. PS, Dr. MK; Data Curation: Mr. PS, Dr. SS, Dr. MK, Dr. MA, Dr. MV; Literature search: Mr. PS; Data acquisition: Mr. PS, Dr. ST, Dr. MK, Dr. MA, Dr. VM; Data analysis: Mr. PS, Dr. SS, Dr. MK, Dr. MA, Dr. VM; Statistical analysis: Mr. PS; Project Administration: Mr. PS; Supervision: Dr. MK; Validation: Mr. PS, Dr ST, Visualization: Mr. PS, Writing—Original Draft Preparation: Mr. PS; Writing—Review and Editing: Dr. SS, Dr. MK,; Manuscript review: Dr. MA, Dr. MV.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The Institutional Ethics Committee approved this study's survey protocol at Maharashtra University of Health Sciences, Nashik (Approval No.: MUHS/IEC/2022/01).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
Sapana Thakare: Died March 13, 2023.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rishi P, Thakur K, Vij S, Rishi L, et al. Diet, gut microbiota and COVID-19. Indian J Microbiol. 2020;60:420–429. doi: 10.1007/s12088-020-00908-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thakur V, Bhola S, Thakur P, Kumar S, et al. Waves and variants of SARS-CoV-2: understanding the causes and effect of the COVID-19 catastrophe. Infection. 2022;50:309–325. doi: 10.1007/s15010-021-01734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thakur P, Thakur V, Kumar P, et al. Emergence of novel omicron hybrid variants: BA(x), XE, XD, XF more than just alphabets. Int J Surg. 2022;104:106727. doi: 10.1016/j.ijsu.2022.106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen S, Kumar N. SARS CoV2 pandemic: therapeutics in warp speed. Recent Adv Antiinfect Drug Discov. 2023 doi: 10.2174/2772434418666230119101350. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (2021) Index @ Covid19.Who.Int. In: https://covid19.who.int/
- 6.Singh A, Deedwania P, Vinay K, et al. Is India’s health care infrastructure sufficient for handling COVID 19 pandemic? Int Arch Public Health Community Med. 2020;4:1–4. doi: 10.23937/2643-4512/1710041. [DOI] [Google Scholar]
- 7.Ghosh A, Nundy S, Mallick TK. How India is dealing with COVID-19 pandemic. Sens Int. 2020;1:1–8. doi: 10.1016/j.sintl.2020.100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agrawal M, Madhuri K, Vidyasagar M. Modelling the spread of SARS-CoV-2 pandemic: impact of lockdowns & interventions. Indian J Med Res. 2021;153:175–181. doi: 10.4103/ijmr.IJMR_4051_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barber RM, Sorensen RJD, Pigott DM, et al. Articles Estimating global, regional, and national daily and cumulative infections with SARS-CoV-2 through 14 Nov, 2021: a statistical analysis. The Lancet. 2022 doi: 10.1016/S0140-6736(22)00484-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Babu GR, Ray D, Bhaduri R, et al. COVID-19 pandemic in India: through the lens of modeling. Glob Health Sci Pract. 2021;9:220–228. doi: 10.9745/GHSP-D-21-00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SKS, Kalia VC, Lee J. Deploying biomolecules as anti-COVID-19 agents. Indian J Microbiol. 2020;60:263–268. doi: 10.1007/s12088-020-00893-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nashik Population 2022. https://www.indiacensus.net/district/nashik. Accessed 27 Oct 2022
- 13.Municipal Corporation of Malegaon. COVID 19 daily reporting data
- 14.Kulkarni M, Amale P (2022) Malegaon pattern :काय आहे कोरोना नियंत्रणाचा मालेगाव पॅटर्न? ABP Maza live 12:21–23. https://marathi.abplive.com/news/maharashtra/maharashtra-nashik-malegaon-pattern-what-is-the-malegaon-pattern-of-corona-control-1024925
- 15.Aggregated Sheets C (2022) COVID19-tracker API. Indian Institute of Technology, Hyderabad. https://covid19tracker.in/data. Accessed 27 Oct 2022
- 16.Vasishtha G, Mohanty SK, Mishra US, et al. Impact of COVID-19 infection on life expectancy, premature mortality, and DALY in Maharashtra, India. BMC Infect Dis. 2021;21:1–11. doi: 10.1186/s12879-021-06026-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Worldometer (2022) COVID live: Coronavirus statistics—worldometer. https://www.worldometers.info/coronavirus/. Accessed 29 Oct 2022
- 18.Chakraborty R (2022) 23 districts in Maharashtra record seven-day positivity rate above 10 per cent. In: The Indian Express e-paper. https://indianexpress.com/article/cities/mumbai/23-districts-in-maharashtra-record-seven-day-positivity-rate-above-10-per-cent-7730532/
- 19.Madaan N, Jain B (2021) Maharashtra: immunity in 50% population in six districts, indicates sero-survey. In: The Times of India. https://timesofindia.indiatimes.com/city/mumbai/maharashtra-immunity-in-50-population-in-six-dists-indicates-sero-survey/articleshowprint/84719966.cms
- 20.Phadke M (2020) How congested, communally-sensitive Malegaon went from Covid hotspot to just 75 cases. In: The print. https://theprint.in/statedraft/how-congested-communally-sensitive-malegaon-went-from-covid-hotspot-to-just-75-cases/447964/
- 21.(2022) No active Covid case in Malegaon since 16 Mar; civic admin still on guard. In: The Times of India epaper. https://timesofindia.indiatimes.com/city/nashik/no-active-covid-case-in-malegaon-since-march-16-civic-admin-still-on-guard/articleshow/90342022.cms
- 22.Murhekar M, Bhatnagar T, Thangaraj JWV, et al. Seroprevalence of IgG antibodies against SARS-CoV-2 among the general population and healthcare workers in India, June–July 2021: a population-based cross-sectional study. PLoS Med. 2021;18:1–17. doi: 10.1371/journal.pmed.1003877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma SK, Rathod PG, Ukey UU, et al. Sero prevalence of SARS-CoV-2 in general population of Nagpur district. Int J Community Med Public Health. 2021;8:3952. doi: 10.18203/2394-6040.ijcmph20213027. [DOI] [Google Scholar]
- 24.Murhekar M, Bhatnagar T, Thangaraj JWV, et al. SARS-CoV-2 seroprevalence among the general population and healthcare workers in India, December 2020–January 2021. Int J Infect Dis. 2021;108:145–155. doi: 10.1016/j.ijid.2021.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murhekar M, Bhatnagar T, Selvaraju S, et al. SARS-CoV-2 antibody seroprevalence in India, August–September, 2020: findings from the second nationwide household serosurvey. Lancet Glob Health. 2021;9:e257–e266. doi: 10.1016/S2214-109X(20)30544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aggarwal A, Mehta S, Gupta D, et al. Healthcare workers & SARS-CoV-2 infection in India: a case-control investigation in the time of COVID-19. J Dent Educ. 2012;76:1532–1539. doi: 10.4103/ijmr.IJMR_2234_20. [DOI] [PubMed] [Google Scholar]
- 27.Murhekar M, Bhatnagar T, Selvaraju S, et al. Prevalence of SARS-CoV-2 infection in India: findings from the national serosurvey, May–June 2020. Indian J Med Res. 2020;152:48–60. doi: 10.4103/ijmr.IJMR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aggarwal A, Mehta S, Gupta D, et al. Seroprevalence of antibodies to SARS-CoV-2 in healthcare workers & implications of infection control practice in India. Indian J Med Res. 2021;153:207–213. doi: 10.4103/ijmr.IJMR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.George CE, Inbaraj LR, Rajukutty S, et al. Seroprevalence of COVID-19 infection among vaccine naïve population after the second surge (June 2020) in a rural district of South India: a community-based cross-sectional study. PLoS ONE. 2022;17:1–11. doi: 10.1371/journal.pone.0265236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kallathiyan K, Velumani A, Iyer S, et al. COVID-19 seroprevalence study of an Indian Diagnostic Laboratory: report on gender and age analysis. Asian J Health Sci. 2020;6:1–5. doi: 10.15419/ajhs.v6i2.478. [DOI] [Google Scholar]
- 31.Ramaswamy S, Athotra A, Kasar PK, et al. Cross-sectional study on sero-prevalence of SARS-CoV-2 infection in Jabalpur, Madhya Pradesh, India. J Commun Dis. 2021;53:82–88. doi: 10.24321/0019.5138.202114. [DOI] [Google Scholar]
- 32.Kshatri JS, Bhattacharya D, Kanungo S, et al. Serological surveys to inform SARS-CoV-2 epidemic curve: a cross-sectional study from Odisha, India. Sci Rep. 2021;11:1–10. doi: 10.1038/s41598-021-89877-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Babu GR, Sundaresan R, Athreya S, et al. The burden of active infection and anti-SARS-CoV-2 IgG antibodies in the general population: results from a statewide sentinel-based population survey in Karnataka, India. Int J Infect Dis. 2021;108:27–36. doi: 10.1016/j.ijid.2021.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adalja AA, Watson M, Toner ES, et al. Characteristics of microbes most likely to cause pandemics and global catastrophes. Curr Top Microbiol Immunol. 2019;424:1–20. doi: 10.1007/82_2019_176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.