Abstract
Background
Clinical airway screening tests intend to predict difficult airways, but none have a high predictive value. Recent systematic reviews correlate ultrasound with difficult laryngoscopy. This study aimed primarily to correlate ultrasound measurements of anatomical upper airway structures in the sniffing position with difficult direct laryngoscopy. The secondary aim was to observe gender-based differences.
Methods
This prospective, cross-sectional, single-center observational study included 209 patients requiring general anesthesia for elective surgery. Preoperatively, we performed six clinical airway assessments and three ultrasound measurements, which were the Distance from Skin to the Hyoid Bone (DSHB), to the Epiglottis (DSE), and to the anterior commissure of the vocal cords (DSAC) in a sniffing position. Benumof's criteria for the “best view at the first attempt” for direct laryngoscopy assessed the difficulty of laryngoscopy.
Results
The distance from skin to the epiglottis was the best predictor of direct difficult laryngoscopy (defined as Cormack-Lehane grade ≥ 2b) with a minimum thickness cut-off at 2.70 ± 0.19 cm (sensitivity 91.3%; specificity 96.9%). The skin to the hyoid bone distance cut-off was 1.41 ± 0.30 cm with moderate correlation (sensitivity 80.4%; specificity 60.1%). No correlation was found for the distance to the anterior commissure of the vocal cords. In women compared to men, the skin to the epiglottis distance was more sensitive (92.3% vs. 90.9%) and specific (98.8% vs. 95.2%).
Conclusions
DSE in the sniffing position is the most reliable parameter for preoperative airway ultrasound assessment in the Caucasian population, with higher sensitivity and specificity in women, and might be considered as an independent predictor for direct difficult laryngoscopy.
KEYWORDS: Anesthesia, Airway management, Intubation, Laryngoscopy, Position, Ultrasonography
Introduction
Unanticipated difficult airway is a potentially life-threatening event during airway management. Physicians must act quickly and safely in order to avoid increased morbidity and mortality.1 The NAP4 study on complications of airway management in Great Britain revealed the inability of physical airway examination to identify difficult airways as a risk factor.2 Two recent Cochrane meta-analyses found no reliable clinical screening tests to predict difficult laryngoscopy or difficult tracheal intubation.3,4 A meta-analysis5 and a systematic review6 found limited sensitivity to predict a difficult airway of single clinical airway exams, as well as for multivariate tests.
Recently, point-of-care ultrasound of the airway entered routine clinical practice.7 Prasad et al8 found good anatomical correlation of the airway comparing computerized axial tomography with ultrasound. Ultrasonography reliably measured pre-tracheal tissues and infra-hyoid structures but was less robust for suprahyoid structures that might be affected by neck flexo-extension.
Several ultrasound predictors intended to evaluate prediction of difficult airways.9, 10, 11, 12 Three systematic reviews correlated the “skin thickness at the epiglottis and hyoid levels”, and “the hyomental distance and ratio” with difficult laryngoscopy.13, 14, 15 The limitations of these studies affecting generalizability are the small sample size, the absence of standardized ultrasonographic and laryngoscopy evaluation methods,13 and no specific analysis of the differences in neck tissue between men and women.16 To overcome such limitations we propose standardized ultrasound measurements of the airways in the sniffing position to allow optimal alignment of the axes of vision for direct laryngoscopy,17,18 thus avoiding the neutral neck position in previous studies. The proposed laryngoscopy protocol follows Benumof's criteria.19
The primary goal of this study was to predict a Cormack-Lehane grade ≥ 2b with three standardized ultrasound airway measurements having reasonable high sensitivity and specificity: Distance from the Skin to the Hyoid Bone (DSHB), from the Skin to Epiglottis (DSE), and from the Skin to the Anterior Commissure of the vocal cords (DSAC). Secondarily, we aimed to investigate differences between men and women.
Methods
Ethical approval for this study was provided by the Ethical Committee of Navarra University Hospital (Pamplona, Spain) (Chairperson Beatriz González) (Project 2019.14) on March 14th, 2019. This prospective, cross-sectional, single-center observational study was registered on Clinical Trial.gov (NCT04168840). All participants signed a written informed consent. The study was conducted in accordance with the Helsinki Declaration, Good Clinical Practice guidelines, and the Spanish legislation for biomedical research.
A cohort of consecutive American Society of Anesthesiologists (ASA) physical status I to III patients, aged 18‒90 years, undergoing general anesthesia for elective surgery between May 2019 and January 2020 were included. Exclusion criteria were a Body Mass Index (BMI) > 35 Kg.m−2(the ramping position in these patients is not considered as a sniffing position), pregnancy, cervical tumors, goiter, or a history of cervical radiation therapy, maxillofacial or cervical abnormalities, and inability or unwillingness to provide consent.
During the preanesthesia evaluation, we collected demographic variables (age, sex, weight, height, BMI, and ASA physical status) and performed several clinical airway screening measurements by the principal investigator: modified Mallampati (Samsoon and Young) score (MMS), Thyromental Distance (TMD), Sternomental Distance (SMD), Interincisal Distance (IID), Upper Lip Bite Test (ULBT) and Cervical Perimeter (CP).
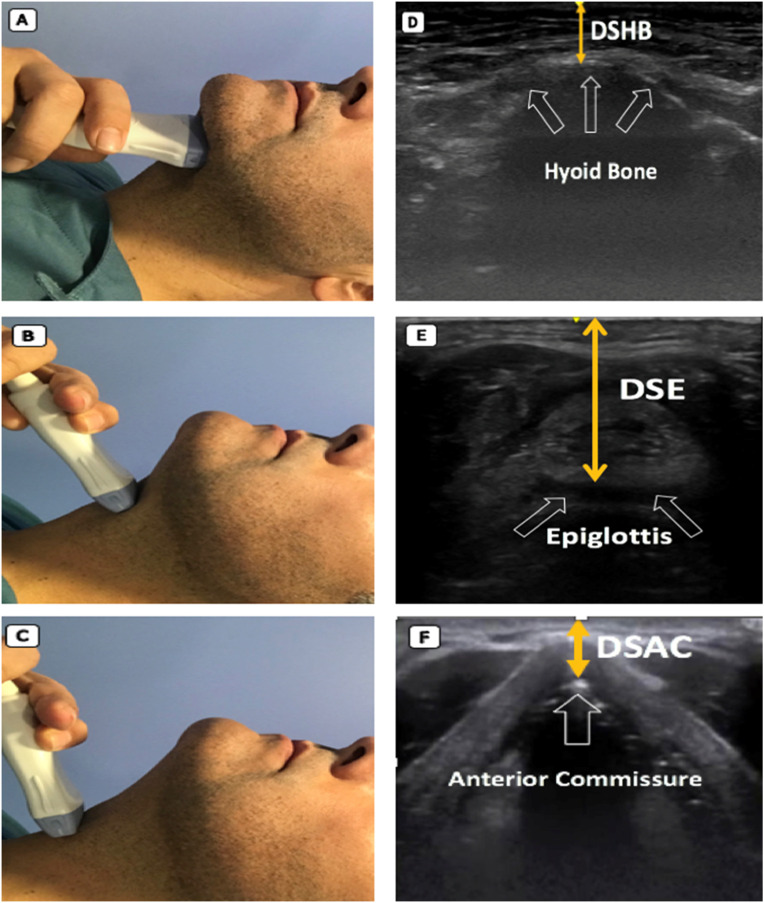
Ultrasound measurements were performed in the operating room by the principal investigator. Patients were in supine position with the head in the “sniffing” position on a slightly compressible foam pillow (TRUMPF Medizin Systeme, Saalfeld, Germany). This is the best position to perform direct laryngoscopy according to Benumof,19 the Difficult Airway Society (DAS) guidelines,17 and the anatomical model described by Greenland.18 A high frequency linear probe (6–12 MHz) with the recommended penetration depth of 2–3 cm for superficial structures7 was placed in the transverse plane of the neck to measure the thickness of the anterior cervical tissues (General Electric Logiq V2, GE Medical Systems, Jiangsu, China). Three easy and quick to implement ultrasound distances were measured: the minimum Distance from the Skin to the Hyoid Bone (DSHB), the Skin to the medium Epiglottis line distance (DSE), and the Distance Skin to the Anterior Commissure of the vocal cords (DSAC) (Fig. 1).
Figure 1.
Ultrasound measurements of pre-tracheal tissues. Left panel different neck levels with ultrasound probe in transverse plane in the sniffing position: (A) Hyoid bone level; (B) thyrohyoid membrane level; (C) Anterior Commissure of vocal cords level. Right panel corresponding ultrasound images: (D) white empty arrows denote hyoid bone, orange arrow denotes minimum Distance from Skin to Hyoid Bone (DSHB); (E) white empty arrows denote hypoechoic image of epiglottis, orange arrow denotes Distance from Skin to Epiglottis midway (DSE); (F) white empty arrows denote anterior commissure of vocal cords, orange arrow denotes minimum Distance from Skin to Anterior Commissure (DSAC).
Standard noninvasive anesthesia monitoring was installed (ECG, SpO2, noninvasive blood pressure, capnography, accelerometric neuromuscular monitoring) before the induction of general anesthesia according to the departmental standardized protocol. After adequate preoxygenation was confirmed by an ETO2 greater than 90%, general anesthesia was induced with propofol (2–2.5 mg.Kg−1), fentanyl (2–4 µg.Kg−1) and rocuronium (0.6–1 mg.Kg−1). After verifying adequate hypnotic depth (Entropy below 50, GE Healthcare, Helsinki, Finland) and neuromuscular relaxation (TOF = 0), direct laryngoscopy with a Macintosh blade n° 4 (Riester, Jungigen, Alemania) was performed in the sniffing position to evaluate the Cormack-Lehane (C-L) grade followed by tracheal intubation. A SpO2 of less than 91% was the stopping criterion of the rating. A maximum of two intubation attempts were allowed before declaring a failed direct laryngoscopy intubation, and an optical or videolaryngoscope (Airtraq® Prodol Meditec, Vizcaya, Spain or Kingvision®, King Systems, Indiana, USA) was used as a rescue device.
All Benumof's19 criteria were used for “best view at the first attempt”, which include the sniffing position (7–8 cm height slightly compressible foam pillow for flexion of the neck), the BURP maneuver, complete muscle relaxation (TOF = 0), and an appropriate laryngoscope blade (on our case a Macintosh blade n° 4). Four anesthesiologists with more than 5 years of clinical experience (including the principal investigator) performed the direct laryngoscopy and assessed the C-L grade with and without the Backward-Upward-Rightward-Pressure (BURP) maneuver.20 For direct laryngoscopy, we used Cook's modified scale because of its greater sensitivity and specificity in predicting a difficult intubation.21 Yentis et al. concluded that the classic C-L system was insufficient to describe visualization in direct laryngoscopy, reporting that up to 67.4% of grade 2b intubations were considered difficult.22 Finally, DAS also describes in its difficult airway guidelines that Cook modified scale gives more information in airway management.17 It rates a grade 1 (complete vision of the glottis) and a 2a (partial vision of the glottis) as an easy direct laryngoscopy. Grade 2b (only the arytenoids are visible) and grade 3a (only epiglottis visible, but it can be elevated) were rated as restricted laryngoscopy. Grade 3b (only epiglottis visible and no elevation possible) and grade 4 (base of the tongue visible) were rated as difficult laryngoscopy.21 Therefore, this classification gives information about the technique necessary to most probably achieve successful intubation.
We dichotomized laryngoscopy into easy (comprised of C-L grades 1 and 2a) and restricted/difficult laryngoscopy (composed of C-L grades 2b, 3a, 3b, and 4), as studies reported a 5% to 10% increased incidence of airway management complications with these higher C-L grades.2,17
Because the airway management as well as the ultrasound measurements were performed on patients during daily clinical care, blinding of the operators was not possible, but the different results of the ultrasound measurements were not communicated to the anesthesiologist who performed the laryngoscopy and intubations.
Statistics
The sample size calculations were based on literature of ultrasound measurements predicting difficulty in at least 80–85% of direct laryngoscopy and intubation that are really difficult (C-L ≥ 2b).23,24 Unexpected difficult intubation due to inadequate larynx view during direct laryngoscopy is reported in 5% to 10%.17 Accepting an alpha error of 0.05 and beta error of 0.15, we needed 196 patients to obtain statistically significant differences between easy and restricted/difficult laryngoscopy.
Descriptive statistics analyzed quantitative variables. Pearson's χ2 test or Fisher's exact test for qualitative variables and the Student's t-test or Mann-Whitney U test for quantitative variables compared results, and a logistic regression analysis evaluated the Odds Ratio (OR) with their corresponding 95% Confidence Interval.
The area under the Receiver Operating Characteristic Curve (ROC AUC) established sensitivity and specificity of the clinical tests and ultrasound measurements. Then the Youden's Index estimated the optimal cut-off point values. The accuracy, sensitivity, specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of the indicators were calculated with Epidat 3.1(SERGAS, Galicia, Spain), otherwise we used SPSS software version 25.0 (IBM, Armonk, New York), and reported continuous variables as mean ± Standard Deviation (SD) and categorical variables as absolute (n) and relative frequencies (%). A p-value < 0.05 was considered statistically significant.
Results
This study included 209 patients and their demographic data are presented in Table 1. The C-L was restricted/difficult in 57 patients (27.3%) without BURP maneuver, and in 46 patients (22%) with BURP maneuver, an improved view in 11 patients (5.3%). Direct laryngoscopy was classified as easy in 163 patients (78.0%), and as restricted/difficult in 46 patients (22.0%). CL grade 1: 123 patients (58.9%), 2a: 40 patients (19.1%), 2b: 36 patients (17.2%), 3a: 8 patients (3.8%) and 3b: 2 patients (1.0%).
Table 1.
Demographic patient variables, clinical airway assessment, and ultrasound measurements.
| Variables | Easy laryngoscopy (n = 163) | Restricted/difficult laryngoscopy (n = 46) | p-value |
|---|---|---|---|
| Sex (Female) n (%) | 80 (86%) | 13 (14%) | <0.012 |
| Age (years) | 54.8 ± 15.5 | 64.6 ± 9.4 | <0.001 |
| BMI (Kg.m−1) | 24.8 ± 3.4 | 27.5 ± 3.2 | <0.001 |
| ASA, n (%) | 0.054 | ||
| I | 45 (88.2%) | 6 (11.8%) | |
| II | 100 (73%) | 37 (27%) | |
| III | 18 (85.7%) | 3 (14.3%) | |
| MMS, n (%) | <0.001 | ||
| I | 90 (92.8%) | 7 (7.2%) | |
| II | 60 (71.4%) | 24 (28,6%) | |
| III | 12 (52.2%) | 11 (47.8%) | |
| IV | 1 (20%) | 4 (80%) | |
| TMD (cm) | 7.6 ± 0.9 | 7.3 ± 0.9 | 0.310 |
| STM (cm) | 13.3 ± 1.4 | 12.8 ± 1.1 | 0.034 |
| IID (cm) | 4.7 ± 0.5 | 4.5 ± 0.6 | 0.090 |
| ULBT, n (%) | <0.001 | ||
| I | 139 (83.2%) | 28 (16.8%) | |
| II | 23 (57.5%) | 17 (42.5%) | |
| III | 1 (50%) | 1 (50%) | |
| CP (cm) | 39.27 ± 4.53 | 43.46 ± 4.56 | <0.001 |
| DSHB (cm) | 1.15 ± 0.27 | 1.41 ± 0.30 | <0.001 |
| DSE (cm) | 2.16 ± 0.29 | 2.70 ± 0.19 | <0.001 |
| DSAC (cm) | 0.77 ± 0.24 | 0.92 ± 0.27 | <0.001 |
BMI, Body Mass Index; ASA, American Society of Anesthesiologists physical status classification system; MMS, Modified Mallampati Score; TMD, Thyromental Distance; STM, Sternomental Distance; IID, Interincisor Distance; ULBT, Upper Lip Bite Test; CP, Cervical Perimeter; DSHB, Distance from Skin to Hyoid Bone; DSE, Distance from Skin to Epiglottis; DSAC, Distance from Skin to Anterior Commissure of the vocal cords.
For patients with C-L ≥ 2b, 9 (19.5%) required 2 attempts of direct laryngoscopy and a stylet, 19 (41.3%) needed a Frova®-type intubation guide (Cook Medical, Indiana, USA), 16 (34.8%) required video laryngoscopy (Airtraq® or Kingvision®), and 2 patients (4.4%) (C-L grade 3b) were intubated asleep with a flexible bronchoscope. There were 18 cases of difficult tracheal intubation as defined as ASA practice guidelines25 (8.6% of total study population, and 39.1% of restricted/difficult laryngoscopy group), nonetheless all patients were successfully intubated without complications.
The 46 restricted/difficult laryngoscopy patients were more men (restricted/difficult laryngoscopy 33 men/13 women vs. easy laryngoscopy 83 men/80 women; p < 0.012), older (restricted/difficult laryngoscopy 64.6±9.4 years vs. easy laryngoscopy 54.8 ± 15.5 years; p < 0.001), and with higher BMI (restricted/difficult laryngoscopy 27.5 ± 3.2 Kg.m−2 vs. easy laryngoscopy 24.8 ± 3.4 Kg.m−2; p < 0.001), without difference for ASA physical status (Table 1). The Mallampati score, sternomental distance, upper lip bite test, and cervical perimeter were statistically significant worse. No differences were found for the thyromental distance and the interincisal distance. Ultrasound measures revealed statistically significant greater thickness for the distance from skin to the hyoid bone, the distance from skin to the epiglottis, and the distance from skin to the anterior commissure of the vocal cords (Table 1).
The diagnostic accuracy expressed as ROC AUC to detect a restricted/difficult laryngoscopy were best for the distance from skin to the epiglottis DSE (0.96 [95% CI 0.94‒0.99]; p < 0.001) and the distance from skin to the hyoid bone (0.74 [95% CI 0.66‒0.82]; p < 0.001), which was in the same range as the Mallampati score (0.74 [95% CI 0.66‒0.82]; p < 0.001) and the cervical perimeter (0.73 [95% CI 0.66‒0,81]; p < 0.001) (Table 2).
Table 2.
Diagnostic accuracy of clinical airway screening tests and ultrasound measurements for predicting a restricted/difficult laryngoscopy.
| Variables | AUC (95% CI) | Sensitivity | Specificity | PPV | NPV | Youden Index | p-value |
|---|---|---|---|---|---|---|---|
| MMS | 0.74 (0.66‒0.82) | 32.61 | 92.02 | 53.57 | 82.87 | 0.25 | <0.001 |
| TMD | 0.46 (0.37‒0.55) | 15.22 | 87.12 | 25.00 | 78.45 | 0.02 | 0.5 |
| STM | 0.38 (0.29‒0.47) | 47.83 | 72.39 | 32.84 | 83.10 | 0.20 | 0.017 |
| IID | 0.40 (0.31‒0.50) | 6.52 | 98.16 | 50.00 | 78.82 | 0.05 | 0.058 |
| ULBT | 0.39 (0.29‒0.49) | 2.17 | 99.39 | 50.00 | 78.26 | 0.02 | 0.027 |
| CP | 0.73 (0.66‒0.81) | 50.00 | 76.07 | 37.10 | 84.35 | 0.26 | <0.001 |
| DSHB | 0.74 (0.66‒0.82) | 80.43 | 60.12 | 36.27 | 91.59 | 0.41 | <0.001 |
| DSE | 0.96 (0.94‒0.99) | 91.30 | 96.93 | 89.36 | 97.53 | 0.88 | <0.001 |
| DSAC | 0.66 (0.57‒0.75) | 67.39 | 65.64 | 35.63 | 87.70 | 0.33 | <0.001 |
AUC, Area Under ROC Curve; MMS, Modified Mallampati Score; TMD, Thyromental Distance; STM, Sternomental Distance; IID, Interincisor Distance; ULBT, Upper Lip Bite Test; CP, Cervical Perimeter; DSHB, Distance from Skin to Hyoid Bone; DSE, Distance from Skin to Epiglottis; DSAC, Distance from Skin to Anterior Commissure of the vocal cords; PPV, Positive Predictive Value; NPV, Negative Predictive Value.
Using binary logistic regression to maximize the Youden's index, sensitivity, specificity, Positive Predictive Value (PPV), the Negative Predictive Value (NPV) for the diagnosis of restricted/difficult laryngoscopy, and the cut-off points for the distance from skin to hyoid bone, the distance from skin to epiglottis and the distance from skin to anterior commissure of the vocal cords were established. The distance from skin to hyoid bone with a cut-off point at 1.19 cm could be predicted with a PPV of 36.3% (95% CI 26.5‒46.1%] and a NPV of 91.6% (95% CI 85.9‒97.3%). The distance from skin to epiglottis with a cut-off at 2.48 cm had a PPV of 89.4% (95% CI 79.5‒99.2%) and a NPV of 97.5% [95% CI 94.8‒100.00%). The distance from skin to anterior commissure of the vocal cords had a cut-off of 0.82 cm with a PPV of 35.6% (95% CI 25.0‒46.3%) and a NPV of 87.7% (95% CI 81.5‒93.9%) (Table 2).
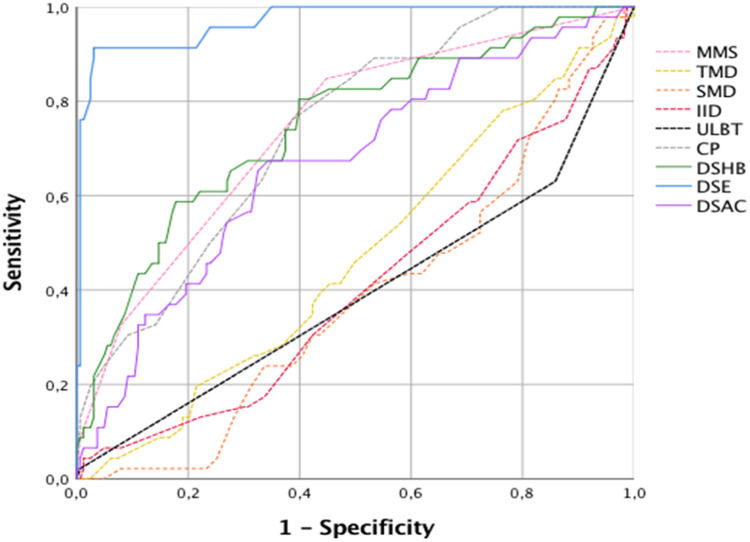
The correlation between clinical airway assessment tests, ultrasound measurements and C-L ≥ 2b (restricted/difficult laryngoscopy) is shown as Area Under the ROC Curves (AUC), which is for the distance from skin to epiglottis with 0.96 the closest to 1 (95% CI 0.94‒0.99), sensitivity 91.30%, specificity 96.93% as the best ultrasound predictor performing better than any clinical airway assessment parameter. The AUC for the modified Mallampati score was 0.74 (95% CI 0.66‒0.82, sensitivity 32.61%, specificity of 92.02%) as the best clinical airway assessment predictor (Fig. 2).
Figure 2.
Receiver Operating Characteristic (ROC) for clinical test and ultrasound measurements for a C-L ≥ 2b. MMS modified Mallampati score (pink dotted line), TMD, Thyromental Distance (yellow dotted line); STM, Sternomental Distance (orange dotted line); IID, Interincisor Distance (red dotted line); ULBT, Upper Lip Bite Test (black dotted line); CP, Cervical Perimeter (grey dotted line); DSHB, Distance from Skin to Hyoid Bone (solid green line); DSE, Distance from Skin to Epiglottis (solid blue line) and DSAC, Distance from Skin to Anterior Commissure of the vocal cords (solid purple line).
Comparing sex and ultrasound variables, we found slightly higher values for the AUC for all three ultrasound parameters in women for the same cut-off points. These show that the distance from skin to anterior commissure of the vocal cords could also be a predictor in women, but not stronger than the distance from skin to epiglottis. (Table 3).
Table 3.
Diagnostic accuracy of ultrasound for predicting a restricted/difficult laryngoscopy by sex.
| Variables | AUC (95% CI) | Cut-Off | Sensitivity | Specificity | p-value |
|---|---|---|---|---|---|
| DSHB (M) | 0.74 (0.63‒0.84) | 1.19 cm | 78.8 | 61.4 | <0.001 |
| DSHB (F) | 0.75 (0.60‒0.89) | 1.19cm | 84.6 | 56.2 | 0.004 |
| DSE (M) | 0.94 (0.89‒0.99) | 2.48 cm | 90.9 | 95.2 | <0.001 |
| DSE (F) | 0.99 (0.97‒1) | 2.48 cm | 92.3 | 98.8 | <0.001 |
| DSAC (M) | 0.64 (0.53‒0.75) | 0.82 cm | 60.6 | 71.1 | 0.015 |
| DSAC (F) | 0.78 (0.65‒0.91) | 0.82 cm | 84.6 | 60.0 | <0.001 |
AUC, Area Under ROC Curve; DSHB, Distance from Skin to Hyoid Bone; DSE, Distance from Skin to Epiglottis; DSAC, Distance from Skin to Anterior Commissure of the vocal cords, (M) Men and (F) Women.
Discussion
This prospective observational study comparing clinical airway assessment parameters and ultrasound measurements showed the best and strong correlation for the ultrasound distance from skin to epiglottis and a moderate correlation for the distance from skin to hyoid bone measured in the sniffing position to predict restricted/difficult laryngoscopy defined as a Cormack-Lehane grade ≥2b at direct laryngoscopy with a Macintosh blade. The distance from skin to anterior commissure of the vocal cords had a similar ROC AUC as all the clinical airway assessment measurements. These results are similar to recent reviews and meta-analyses13, 14, 15 that recommended to introduce ultrasonography for preoperative airway assessment in anesthesiology curriculum training. Interestingly, the distance from skin to epiglottis was the strongest independent predictor for difficult laryngoscopy for men and women. Therefore, this ultrasound parameter with a cut-off value of 2.48 cm, having a sensitivity of 91.3% and a specificity of 96.9%, is able to predict difficulty in airway management in routine clinical practice and therefore has the potential to improve patient safety.21
Our results about the distance from skin to epiglottis are comparable to the findings of others but all with a slightly lower sensitivity and specificity: Falcetta et al.12 described a cut off at 2.54 cm (sensitivity 82%; specificity 91%), Pinto et al.,11 2.75 cm (sensitivity 64.7%; specificity 77.1%), and Martinez et al.,26 3.0 cm (sensitivity 56.3%; specificity 88.2%) in similar population. Adhikari et al.,9 described a cut-off point of 2.8 cm in a Caucasian and African American population, Wu et al.,10 a cut-off of 1.78 cm (sensitivity 100%; specificity 66.3%) in a Chinese population, and Parameswari et al.,24 found a cut-off of 1.8 cm (sensitivity 75%; specificity 63.6%) in an Indian population. All authors propose the distance from skin to epiglottis as the most promising independent ultrasound predictor of a difficult laryngoscopy. The variable is robust, valid in different ethnicities, and far better than any other clinical predictors are. However, methodology heterogeneity in ultrasound measurements and in laryngoscopy technique might result in a bias (Table 4).
Table 4.
Cut-off points, sensitivity, specificity, ultrasound-measured position, and laryngoscopy method in publications by various authors.
| Author | Adhikari 2011 | Wu 2014 | Pinto 2016 | Parameswari 2017 | Falcetta 2018 | Martinez 2019 | Fernández-Vaquero 2019 |
|---|---|---|---|---|---|---|---|
| DSE cut-off point | 2.8 cm | 1.78 cm | 2.75 cm | 1.8 cm | 2.54 cm | 3 cm | 2.48 cm |
| Sensitivity | Not showed | 100% | 64.7% | 75% | 82% | 56.3% | 91.3% |
| Specificity | Not showed | 66.3% | 77.1% | 63.3% | 91% | 88.2% | 96.9% |
| Ultrasound measurement position | Neutral neck position | Neutral neck position | Neutral neck position | Neutral neck position | Neutral neck position | Sniffing position | Sniffing position |
| Laryngoscopy (Benumof's criteria) | |||||||
| 1. BURP | Not BURP applied. | Not BURP applied. | Not BURP applied. | Not BURP applied. | BURP only if necessary. | Not BURP applied. | BURP applied. |
| 2. Experience | Physician resident/ nurse. | 2-years experienced physicians. | Experience not specified. | Experience not specified. | 5-years experienced physicians. | 10-years experienced physicians. | 5-years experienced physicians. |
| 3. TOF | TOF not Specified. | TOF not Specified. | TOF not Specified. | TOF not Specified. | TOF 0. | TOF 0. | TOF 0. |
| 4. Neck position | Neck position not specified. | Neck position not specified. | Neck position not specified. | Neck position not specified. | Neck position not specified. | Sniffing position. | Sniffing position. |
| Population | Caucasian African-American | Chinese | Portuguese | Indian | Italian | Spanish | Spanish |
| Portuguese | |||||||
| Sample size (n) | 51 | 203 | 74 | 130 | 301 | 50 | 209 |
Anatomical differences between men and women seems to be an issue. We found that the distance from skin to epiglottis is a better parameter in women (sensitivity of 92.3% and specificity of 98.8%, compared to sensitivity of 90.9% and specificity of 95.2% in men). Falcetta et al., described also higher values for women (sensitivity 100% and specificity 83%) compared to men (sensitivity 75% and specificity 92%). Unfortunately, no other authors have analyzed the differences between men and women.
Our data about the distance from skin to hyoid bone (cut-off at 1.19 cm; sensitivity 80.4%, specificity 60.1%) are similar to findings by Wu et al.10 (cut-off point 1.28 cm; sensitivity 85.7 %, specificity 85.1%) and Adhikari et al.9 (with a cut-off at 1.69 cm). However, a similar analysis by Martinez et al.26 in a Spanish population showed a non-significant association (p = 0.580), probably due to an underpowered sample size of the study (50 patients). Interestingly, the distance from skin to anterior commissure of the vocal cords was the weakest predictor of difficult laryngoscopy in our study, which is in line with previous data by Falcetta et al.12 and Martinez et al.26 (same ethnicity), but contrary to Ezri et al.27 (in an obese population) and Wu et al.10 (in a Chinese population).
The modified Mallampati score and the cervical perimeter were the best clinical airway assessment tests with an AUC of 0.74 and 0.73, respectively, similar to reports by Pinto et al.11 (Portuguese population) and Martinez et al.26 (Spanish population), but in contrast to Ezri et al.27 (Middle-East obese population, Israel) or Komatsu et al.28 (Caucasian and African-American obese population, USA). Differences among ethnicities, methodology, and experience of physicians may explain such different results, as age, sex, and BMI, presented statistically significant differences according to Martinez,26 Adhikari,9 Komatsu,28 Pinto,11 Ezri,27 and Wu,10 respectively.
A strength of our study is the standardized ultrasound measurements (sniffing position, the final position for endotracheal intubation), and the standardized laryngoscopy applying the Benumof19 criteria for “best view at the first attempt”. Furthermore, the analysis of differences between men and women confirming the value of ultrasound in predicting airway management difficulties in female patients. All clinical airway assessments and the ultrasound measurements were taken by the same investigator which improves inter-rated reliability but also might introduce a bias driven by the competence of experts. As far as we know, to date there is no international endorsed ultrasound airway assessment certification, but in this study all ultrasound measurements were taken by an investigator who has eight years of experience in teaching airway ultrasound in national and international courses. Regardless, point-of-care ultrasonography of the airways has a steep learning curve.7,28 We favored direct laryngoscopy as a relevant outcome parameter over tracheal intubation because best view on the glottis is the first step to facilitate easy tracheal intubation. Proper laryngoscopy depends a bit on the skill of the clinician who performs it,29 but we are aware of the differences between laryngoscopy and tracheal intubation, which is even more prominent during video laryngoscopy with the well-known “you-see-that-you-fail” phenomenon.30 The results of our study cannot be related to tracheal intubation success.
The trial was registered in November 2019, about 6 months into the recruitment period. Another limitation of our study relates to the impossibility of blinding airway management and ultrasound measurements, as well as the non-randomized design and the single-center study in a specific European population, which might limit generalization. Therefore, future research should aim to validate our findings and quantify generalizability across different populations and operators.
In conclusion, this study correlated ultrasound measurements of pre-tracheal tissue with difficult laryngoscopy and showed that the distance from the skin to the epiglottis, measured in the sniffing position, is the most reliable parameter for preoperative airway assessment predicting difficult laryngoscopy (defined as Cormack/Lehane grade ≥ 2b) in men and women with a cut-off value of 2.48 cm having a sensitivity of 91.3% and a specificity of 96.9%.
Acknowledgements
No professional medical writer was involved in the writing process of the manuscript. No industrial or other grant body provided financial support to the study. None of the authors has a financial conflict of interest with the study. PCM is Board Member and Secretary of the European Airway Management Society (EAMS). RG is Board Member and Treasurer of EAMS. The results of the study were not presented elsewhere before.
The authors declare no conflicts of interest.
Footnotes
Clinical Trial.gov identified NCT04168840. https://clinicaltrials.gov/ct2/show/NCT04168840.
References
- 1.Joffe AM, Aziz MF, Posner KL, Duggan LV, Mincer SL, Domino KB. Management of difficult tracheal intubation: a closed claims analysis. Anesthesiology. 2019;131:818–829. doi: 10.1097/ALN.0000000000002815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br J Anaesth. 2011;106:617–631. doi: 10.1093/bja/aer058. [DOI] [PubMed] [Google Scholar]
- 3.Detsky ME, Jivraj N, Adhikari NK, et al. Will this patient be difficult to intubate? the rational clinical examination systematic review. JAMA ‒ J Am Med Assoc. 2019;321:493–503. doi: 10.1001/jama.2018.21413. [DOI] [PubMed] [Google Scholar]
- 4.Roth D, Nl P, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients (Review) Summary of findings for the main comparison. Cochrane Database Syst Rev. 2018;15:5. doi: 10.1002/14651858.CD008874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nørskov AK, Rosenstock C V, Wetterslev J, Astrup G, Afshari A, Lundstrøm LH. Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia. 2015;70:272–281. doi: 10.1111/anae.12955. [DOI] [PubMed] [Google Scholar]
- 6.Vannucci A, Cavallone LF. Bedside predictors of difficult intubation: A systematic review. Minerva Anestesiol. 2016;82:69–83. [PubMed] [Google Scholar]
- 7.Kristensen MS, Teoh WH, Graumann O, Laursen CB. Ultrasonography for clinical decision-making and intervention in airway management: From the mouth to the lungs and pleurae. Insights Imaging. 2014;5:253–279. doi: 10.1007/s13244-014-0309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prasad A, Yu E, Wong DT. Karkhanis R. Comparison of sonography and computed tomography as imaging. J Ultrasound Med. 2011;30:965–972. doi: 10.7863/jum.2011.30.7.965. [DOI] [PubMed] [Google Scholar]
- 9.Adhikari S, Zeger W, Schmier C, et al. Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad Emerg Med. 2011;18:754–758. doi: 10.1111/j.1553-2712.2011.01099.x. [DOI] [PubMed] [Google Scholar]
- 10.Zheng J. Role of anterior neck soft tissue quantifications by ultrasound in predicting difficult laryngoscopy. Med Sci Monit. 2014;18:2343–2350. doi: 10.12659/MSM.891037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinto J, Cordeiro L, Pereira C, Gama R, Fernandes HL, Assunção J. Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J Crit Care. 2016;33:26–31. doi: 10.1016/j.jcrc.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 12.Falcetta S, Cavallo S, Gabbanelli V, et al. Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy. Eur J Anaesthesiol. 2018;35:605–612. doi: 10.1097/EJA.0000000000000832. [DOI] [PubMed] [Google Scholar]
- 13.Gomes SH, Simões AM, Nunes AM, et al. Useful ultrasonographic parameters to predict difficult laryngoscopy and difficult tracheal intubation ‒ a systematic review and meta-analysis. Front. Med. 2021;8 doi: 10.3389/fmed.2021.671658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sotoodehnia M, Rafiemanesh H, Mirfazaelian H, Safaie A, Baratloo A. Ultrasonography indicators for predicting difficult intubation: a systematic review and meta-analysis. BMC Emerg Med. 2021;21:76. doi: 10.1186/s12873-021-00472-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carsetti A, Sorbello M, Adrario E, Donati A, Falcetta S. Airway Ultrasound as Predictor of Difficult Direct Laryngoscopy: A Systematic Review and Meta-analysis. Anesth Analg. 2021:1–11. doi: 10.1213/ANE.0000000000005839. Publish Ah. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ. Neck soft tissue and fat distribution: Comparison between normal men and women by magnetic resonance imaging. Thorax. 1999;54:323–328. doi: 10.1136/thx.54.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–848. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenland KB. Airway assessment based on a three-column model of direct laryngoscopy. Anaesth Intensive Care. 2010;38:14–19. doi: 10.1177/0310057X1003800104. [DOI] [PubMed] [Google Scholar]
- 19.Benumof JL. Difficult laryngoscopy: obtaining the best view. Can. J. Anaesth. 1994;41:361–365. doi: 10.1007/BF03009856. [DOI] [PubMed] [Google Scholar]
- 20.Takahata O, Kubota M, Mamiya K, et al. The efficacy of the ‘BURP’ maneuver during a difficult laryngoscopy. Anesth Analg. 1997;42:48. doi: 10.1097/00000539-199702000-00033. [DOI] [PubMed] [Google Scholar]
- 21.Cook TM. A new practical classification of laryngeal view. Anaesthesia. 2000;55:274–279. doi: 10.1046/j.1365-2044.2000.01270.x. [DOI] [PubMed] [Google Scholar]
- 22.Yentis SM, Lee DJH. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia. 1998;53 doi: 10.1046/j.1365-2044.1998.00605.x. 104-4. [DOI] [PubMed] [Google Scholar]
- 23.Andruszkiewicz P, Wojtczak J, Sobczyk D, Stach O, Kowalik I. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J Ultrasound Med. 2016;35:2243–2252. doi: 10.7863/ultra.15.11098. [DOI] [PubMed] [Google Scholar]
- 24.Parameswari A, Govind M, Vakamudi M. Correlation between preoperative ultrasonographic airway assessment and laryngoscopic view in adult patients: A prospective study. J Anaesthesiol Clin Pharmacol. 2017;33:353–358. doi: 10.4103/joacp.JOACP_166_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway*. Anesthesiology. 2021 doi: 10.1097/ALN.0000000000004002. [DOI] [PubMed] [Google Scholar]
- 26.Martínez-García A, Guerrero-Orriach JL, Pino-Gálvez MA. Ultrasonography for predicting a difficult laryngoscopy. Getting closer. J Clin Monit Comput. 2021;35:269–277. doi: 10.1007/s10877-020-00467-1. [DOI] [PubMed] [Google Scholar]
- 27.Ezri T, Gewürtz G, Sessler DI, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58:1111–1114. doi: 10.1046/j.1365-2044.2003.03412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Komatsu R, Sengupta P, Wadhwa A, et al. Ultrasound quantification of anterior soft tissue thickness fails to predict difficult laryngoscopy in obese patients. Anaesth Intensive Care. 2007;35:32–37. doi: 10.1177/0310057X0703500104. [DOI] [PubMed] [Google Scholar]
- 29.Jung W, Kim J. Factors associated with first-pass success of emergency endotracheal intubation. Am J Emerg Med. 2020;38:109–113. doi: 10.1016/j.ajem.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Hwang SM. A good laryngeal view does not guarantee perfectly successful tracheal intubation. Korean J Anesthesiol. 2016;69:111–112. doi: 10.4097/kjae.2016.69.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]