Abstract
Background:
Fertility awareness-based methods have been linked to shorter time to conception; however, little is known about the predictors of fertility awareness-based method use among women who are currently or will soon be trying to conceive.
Objective:
To identify predictors of fertility awareness-based methods use among women trying to conceive or contemplating pregnancy within the next year.
Methods:
Women participating in the Nurses’ Health Study 3 were asked if they were trying to become pregnant or contemplating pregnancy and whether they are using fertility awareness-based methods. Multivariable negative binomial regression was used to identify predictors for a number of fertility awareness-based methods used.
Results:
Among the 23,418 women asked about pregnancy intention since 2015, 955 were trying to conceive, and 2,282 were contemplating pregnancy within the next year. The three most used fertility awareness-based methods among women trying to conceive were menstrual cycle tracking, ovulation prediction kits, and cervical mucus monitoring. Among women contemplating pregnancy, the three most commonly used methods were menstrual cycle tracking, cervical mucus monitoring, and basal body temperature monitoring. The ongoing duration of pregnancy attempts and gravidity were associated with the number of methods used among women actively trying to conceive. When compared to women who were trying for 2 months or less, the number of methods was 29% higher when trying for 3–5 months, 45% higher when trying for 6–12 months, and 38% higher when trying for more than 1 year. Compared to nulligravid women, the number of methods was lower for women with a history of two or more pregnancies. Among women contemplating pregnancy, those who were married or in a domestic partnership used more fertility awareness-based methods than unpartnered women. No other significant predictors of fertility awareness-based methods use were identified.
Discussion:
Duration of ongoing pregnancy attempt and gravidity were the only significant predictors for the number of fertility awareness-based methods used among women actively trying to conceive, whereas partnership was the only significant predictor of the number of fertility awareness-based methods among women contemplating pregnancy.
Keywords: family planning, fertility, reproduction
Fertility awareness-based methods (FABMs) are a group of techniques that can help women identify the most fertile days of their menstrual cycles to either avoid pregnancy or increase the chances of conception. Women may observe and track external signs of ovulation that reflect hormonal changes in the cycle, such as changes in cervical fluid, basal body temperature, and saliva, or directly measure reproductive hormone levels in urine or saliva. The recognition and understanding of these signs have increased in recent years, leading to the development of various FABMs. Each FABM uses distinctive signs and sets of instructions to help women identify the fertile time in the menstrual cycle (Duane et al., 2022).
Emerging evidence indicates using FABMs while attempting conception is related to a shorter time to conception, suggesting it may also reduce the risk of infertility and its societal burden (Stanford et al., 2002, 2019). Infertility is no small problem. According to the Centers for Disease Control and Prevention (CDC), among heterosexual women aged 15 to 49 years with no prior births living in the United States, about 1 in 5 (19%) are unable to get pregnant after 1 year of trying (CDC, 2023), and 12.2% have used infertility services (National Center for Health Statistics, 2021). Previous studies have shown that among infertile women and women seeking pregnancy, there is limited knowledge regarding the menstrual cycle, ovulation, and the fertile window (Capotosto, 2021;Hampton et al., 2013; Mahey et al., 2018; Righarts et al., 2017). Although the Practice Committee of the American Society for Reproductive Medicine, in collaboration with the Society of Reproductive Endocrinology and Infertility, states that devices designed to determine or predict the time of ovulation may be useful for people trying to conceive (Pfeifer et al., 2017), there is no standard practice for how health care providers review a woman’s ovulation tracking methods that are needed to establish evidence of ovulation before referral for infertility care. Additionally, referral to infertility services may not always be feasible as a result of the lack of availability of specialized care in many areas of the country, financial barriers to access, limited medical insurance coverage for these services in most of the U.S., or moral/ethical objections to some forms of infertility treatment, among other reasons (Ethics Committee of the American Society for Reproductive Medicine, 2015; Sallam & Sallam, 2016; Shreffler et al., 2010; Weigel et al., 2020). Hence, for women trying to conceive, using FABMs could be an initial intervention for optimizing fertility.
There has been a gradual decline in annual births in the U.S. from about 4.1 million annual births in 1990 to 3.7 million in 2019, so it is important to understand trends in fertility. Fertility rates among women ages 20–24 declined by 43%, while there was an increase of 67% for women aged 35–39 (Morse, 2022). Additionally, there is currently little data on the patterns of use of FABMs and the characteristics of women who use them while trying to conceive. Therefore, this study aimed to identify the patterns and predictors of the use of FABMs among women actively trying to achieve conception and among women contemplating pregnancy within the next year.
Methods
The Nurses’ Health Study 3 (NHS 3; www.nhs3.org) is an ongoing, prospective, internet-based cohort study of nurses living in the U.S. and Canada (Bao et al., 2016). Female and male nurses—including nursing students, licensed practical/vocational nurses, registered nurses, and advanced practice nurses—aged 18 or older, born on or after January 1, 1965, and living in the U.S. or Canada, are eligible to enroll. Recruitment began in 2010, and more than 49,000 participants had joined as of November 2021. Participants receive follow-up questionnaires approximately every 6 months to update information on lifestyle and medical characteristics. In each follow-up questionnaire, participants answering the female questionnaire are asked about their pregnancy status, and nonpregnant participants are asked if they are currently trying to conceive or contemplating pregnancy. Starting in January 2015, participants who reported that they were trying to conceive or contemplating pregnancy were also asked questions about the use of FABMs. As of November 2021, 23,418 women had been asked about their pregnancy and pregnancy intention statuses and their use of FABMs on at least one occasion. Participants were eligible for this analysis if they chose to answer the female questionnaire at registration and had reported that they were either actively trying to achieve pregnancy (n = 955) or contemplating pregnancy within the next year (n = 2,282). For women reporting actively trying to conceive or contemplating pregnancy multiple times during this period, we only included their initial report in the analysis (Supplemental Figure 1). The study was approved by the Mass Brigham Committee for the Protection of Human Subjects in Research.
Assessment of Pregnancy Intention
Nonpregnant women were asked, “Are you actively trying to become pregnant, or do you think that you may become pregnant at some point within the next year?” Women endorsing either option were asked about their use of FABMs, and those answering affirmatively were asked to select from a list of seven FABMs, as well as the option to choose “other.” Women were allowed to report use of more than one FABM. The seven FABMs were: (a) tracking menstrual cycle length, (b) basal body temperature monitoring, (c) cervical mucus monitoring, (d) ovulation prediction kits, (e) fertility monitors that use urine samples, (f) fertility monitors that use saliva samples, and (g) saliva “ferning” microscopes. A brief description of these FABMs is included in Supplemental Table 1.
Information on potential predictors of FABM use was assessed on the enrollment questionnaire, including age, marital status, education, employment, lifetime number of pregnancies, history of infertility, height, and weight from which we calculated BMI, smoking, as well as self-reported chronic health conditions such as anxiety, depression, uterine fibroids, endometriosis, Graves’ disease, hypothyroidism, high blood pressure, elevated cholesterol, diabetes, and polycystic ovarian syndrome (PCOS). In addition, women trying to become pregnant were asked to report the current duration of their ongoing pregnancy attempt. We identified these variables a priori based on other factors in previous studies that have been shown to affect women’s desires, intentions, and behaviors related to family planning decisions and FABM use (Mynarska & Rytel, 2018).
We first calculated frequencies of use for each FABM overall and separately for women actively trying to conceive and women contemplating pregnancy. We then compared baseline demographic and reproductive characteristics between these two groups of women using t-tests for continuous variables and chi-square tests for categorical variables. Associations between the number of fertility awareness-based methods used and potentially predictive factors were evaluated using negative binomial regression models, which were fit separately for both the actively trying and contemplating pregnancy groups. Specifically, we first fit univariate negative log-binomial models where the number of FABMs used was the outcome, and each potential predictor was the model’s sole term. We then fit multivariable models where all the potential predictors were simultaneously included in the model. Duration of ongoing pregnancy attempts were grouped into 2 months or less, 3–5 months, 6–12 months, and 1 year or more. Marital status was grouped into women who were partnered (married or domestic partnership) and those unpartnered (never married, separated, divorced, and widowed). BMI was grouped according to the standard weight status categories. The number of pregnancies was grouped into never been pregnant, history of one pregnancy, and history of two or more pregnancies. All analyses were conducted using Stata software (Release 17; StataCorp LLC, 2021). A significance level of p < .05 was used for all analyses.
Results
Of the 23,418 women asked about pregnancy status and intention between 2015 and 2021, 3,237 women were eligible for our analysis: 955 women who reported being actively trying to conceive and 2,282 women who reported they might become pregnant within the next year. Characteristics of these two groups of women are summarized in Table 1. Women in the study sample were primarily non-Hispanic White (88.1%) and had a mean (SD) age of 29.5 ±4.3 years. Most were employed (92.3%) and married or in a domestic partnership (57.9%). Women who stated they were contemplating pregnancy were slightly younger than women actively trying to achieve conception (29.3 years vs. 30.3 years) and less likely to be married or in a domestic partnership (55.4% vs. 63.8%). Women actively trying to conceive had a slightly higher BMI (26.0 kg/m2 vs. 25.5 kg/m2) and were more likely to report PCOS (11.8% vs. 8.3%), endometriosis (4.6% vs. 2.4%), and hypothyroidism (3.1% vs. 1.8%) than the women who were contemplating pregnancy. A history of infertility was significantly more common in women trying to conceive than in women contemplating pregnancy (23.8% vs. 8.1%). No other major differences were observed between these groups of women (Table 1).
Table 1.
Characteristics of the Study Participants According to Pregnancy Intention Status
| Actively Trying n = 955 | Contemplating Pregnancy n = 2,282 | p | |
|---|---|---|---|
| Mean (N%) | Mean (N%) | ||
| Demographics | |||
| Age, years | SD = 30.3 ± 4.5 | SD = 29.2 ± 4.3 | < .001 |
| Less than 35 years | 807 (84.5) | 2,055 (90.1) | |
| 35 years or more | 147 (15.4) | 227 (9.9) | |
| Not reported | 1 (0.1) | 0 (0) | < .001 |
| Ethnicity | |||
| Hispanic or Latina | 43 (4.5) | 101 (4.4) | |
| Not reported | 4 (0.4) | 5 (0.2) | .61 |
| Race | |||
| American Indian or Alaska Native | 6 (0.6) | 6 (0.3) | |
| White | 876 (91.7) | 2,084 (91.3) | |
| Black or African American | 16 (1.7) | 57 (2.5) | |
| Asian | 33 (3.5) | 79 (3.5) | |
| Native Hawaiian or other Pacific Islander | 7 (0.7) | 13 (0.6) | |
| Middle Eastern or North African | 3 (0.3) | 5 (0.2) | |
| Other | 9 (0.9_ | 19 (0.8) | |
| Not reported | 5 (0.5) | 19 (0.8) | .55 |
| Marital Status | |||
| Partnered | 610 (63.9) | 1,265 (55.4) | |
| Not reported | 1 (0.1) | 5 (0.2) | < .001 |
| Region | |||
| Northeast, USA | 194 (20.3) | 572 (25.1) | |
| Midwest, USA | 273 (28.6) | 615 (26.9) | |
| South, USA | 222 (23.3) | 471 (20.6) | |
| West, USA | 214 (22.4) | 501 (21.9) | |
| Canada | 39 (4.1) | 69 (3.0) | |
| Not reported | 13 (1.4) | 54 (2.4) | .01 |
| Education | |||
| Diploma in Nursing | 2 (0.2) | 5 (0.2) | |
| Associate’s degree | 36 (3.8) | 91 (4.0) | |
| Bachelor’s degree | 564 (59.1) | 1,370 (60.0) | |
| Master’s degree | 184 (19.3) | 429 (18.8) | |
| Doctorate degree | 17 (1.8) | 24 (1.0) | |
| Not reported | 152 (15.9) | 363 (15.9) | .69 |
| Employed Outside the Home | |||
| Yes | 887 (92.9) | 2,102 (92.1) | |
| Not reported | 19 (2.0) | 41 (1.8) | .54 |
| Physical Characteristics | |||
| BMI, kg/m2 | SD = 26.0 ± 6.6 | SD = 25.5± 5.9 | .04 |
| Underweight | 24 (2.5) | 54 (2.4) | |
| Normal weight | 520 (54.5) | 1,277 (56.0) | |
| Overweight | 219 (22.9) | 504 (22.1) | |
| Obese | 127 (13.3) | 366 (16.0) | |
| Severe Obese | 54 (5.7) | 61 (2.7) | |
| Not reported | 11 (1.2) | 20 (0.9) | .001 |
| Current Smoker | |||
| Yes | 6 (0.6) | 5 (0.2) | .17 |
| Self-Reported | |||
| Chronic Health Conditions | |||
| Anxiety | 27 (2.8) | 64 (2.8) | .97 |
| Depression | 282 (29.5) | 609 (26.7) | .10 |
| Uterine Fibroids | 30 (3.1) | 52 (2.3) | .15 |
| Endometriosis | 44 (4.6) | 56 (2.4) | .001 |
| Grave’s Disease | 7 (0.7) | 12 (0.5) | .48 |
| Hypothyroidism | 29 (3.0) | 40 (1.7) | .02 |
| High blood pressure | 53 (5.6) | 101 (4.4) | .17 |
| Elevated cholesterol | 118 (12.4) | 246 (10.8) | .20 |
| Diabetes (Type I or Type II) | 11 (1.2) | 25 (1.0) | .89 |
| PCOS | 108 (11.3) | 183 (8.0) | .003 |
| Pregnancy History | |||
| Gravidity | |||
| 0 | 658 (68.9) | 1,575 (69.0) | |
| 1 | 174 (18.2) | 384 (16.8) | |
| 2 or more | 109 (11.4) | 291 (12.8) | |
| Not reported | 14 (1.5) | 32 (1.4) | .63 |
| History of infertility | 228 (23.9) | 187 (8.2) | |
| Not Reported | 33 (3.5) | 54 (2.4) | < .001 |
| Ongoing duration of time trying to conceive | SD= 7.45 ± 5.02 | N/A* | |
| 2 months or less | 264 (27.6) | ||
| 3–5 months | 149 (15.6) | ||
| 6–12 months | 230 (24.1) | ||
| 1–3 years | 311 (32.6) | ||
| Not reported | 1 (0.1) | ||
| Actively monitor the cycle for signs of ovulation | 674 (70.6) | 811 (35.5) | |
| Not reported | 58 (6.1) | 267 (11.7) | < .001 |
Note. SD= standard deviation; USA= United States of America; BMI= body mass index; PCOS= polycystic ovarian syndrome
Women actively trying to conceive had a higher frequency of FABM use than women contemplating pregnancy. Women actively trying to conceive used, on average, 1.84 FABMs, whereas women contemplating pregnancy used, on average, 0.75 FABMs (Supplemental Figure 2) and were more likely to use each of the seven FABMs included in the questionnaire (Figure 1). The three most commonly used FABMs among women trying to conceive were menstrual cycle tracking, ovulation prediction kits, and cervical mucus monitoring; in contrast, the three most used methods among women contemplating pregnancy were menstrual cycle tracking, cervical mucus monitoring, and basal body temperature monitoring (Figure 1).
Figure 1.
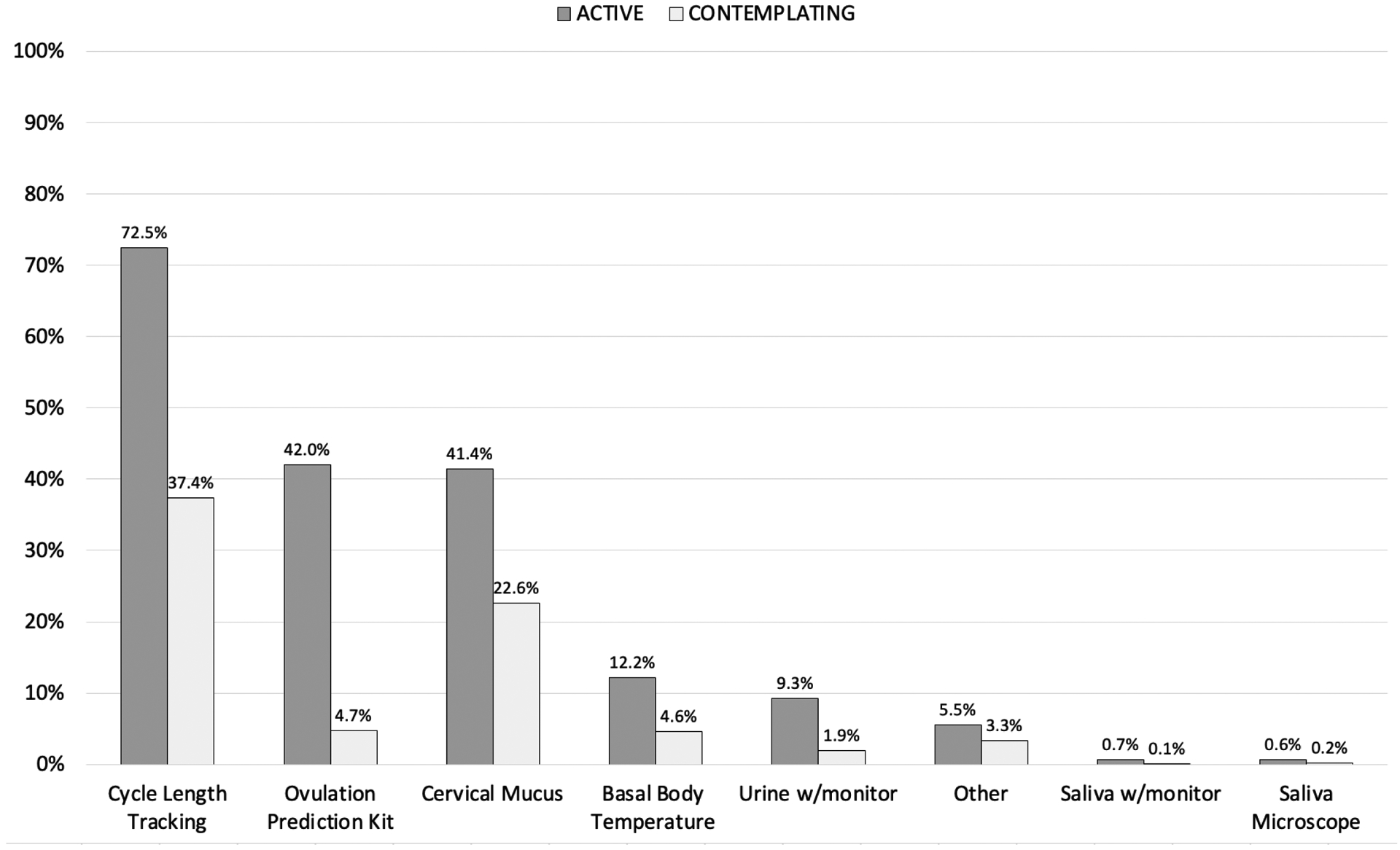
Frequency of FABM use among women actively trying to conceive and women contemplating pregnancy within the next year.
Among women actively trying to conceive, the ongoing duration of pregnancy attempt was the only factor associated with the number of FABMs used in both univariate and multivariable analyses (Table 2). Compared to women who had been trying for 2 months or less, the number of FABMs was 29% (95% CI = 1.11, 1.51), 45% (95% CI = 1.27, 1.66), and 38% (95% CI = 1.20, 1.58) higher for women who had been trying for 3–5 months, 6–12 months, or more than 1 year, respectively (Table 2). Compared to nulligravid women, the number of fertility-awareness-based methods was 17% (95% CI, 0.70–0.98) less for women with a history of two or more pregnancies. Among women contemplating pregnancy, age, and marital status were associated with the number of FABMs used in univariate analyses. In multivariable analysis, women who were partnered (either married or in a domestic partnership) used, on average, 39% (95% CI = 1.23, 1.57) more FABMs than unpartnered women (Table 2). No other a priori selected factors were associated with FABM use in these analyses.
Table 2.
Predictors of the Number of FABMs Used Among Women Actively Trying to Conceive and Women Contemplating Pregnancy
| Univariate IRR | Univariate 95% CI | Multivariate IRR | Multivariate 95% CI | Univariate IRR | Univariate 95% CI | Multivariate IRR | Multivariate 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Actively Trying to Conceive (N = 955) | Contemplating Pregnancy (N = 2,282) | |||||||
| Age, years | ||||||||
| Less than 35 years | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| 35 years or more | 0.98 | 0.86, 1.12 | 1.01 | 0.87, 1.16 | 1.24 | 1.04, 1.49 | 1.14 | 0.94,1.39 |
| Not reported | 1.08 | 0.27, 4.33 | 0.78 | 0.17, 3.47 | ---- | ---- | ---- | ---- |
| Marital status | ||||||||
| Unpartnered | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Partnered | 1.01 | 0.92, 1.11 | 1.02 | 0.92, 1.14 | 1.40 | 1.24, 1.57 | 1.37 | 1.21, 1.55 |
| Not reported | 1.09 | 0.27, 4.38 | 1 | ---- | 0.98 | 0.26, 3.66 | 0.95 | 0.25, 3.59 |
| Education | ||||||||
| Diploma | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Associates | 1.67 | 0.41, 6.82 | 1.94 | 0.47, 8.00 | 1.84 | 0.38, 8.91 | 2.26 | 0.47, 10.95 |
| Bachelor | 1.90 | 0.47, 7.59 | 2.21 | 0.55, 8.91 | 1.82 | 0.38, 8.60 | 2.29 | 0.48, 10.81 |
| Master | 1.68 | 0.42, 6.77 | 2.01 | 0.50, 8.14 | 1.94 | 0.41, 9.23 | 2.31 | 0.49, 10.98 |
| Doctorate | 2.00 | 0.48, 8.32 | 2.44 | 0.58, 10.27 | 1.98 | 0.38, 10.26 | 2.39 | 0.46, 12.41 |
| Not reported | 1.86 | 0.46, 7.51 | 2.23 | 0.55, 9.04 | 1.98 | 0.42, 9.38 | 2.57 | 0.54, 12.23 |
| Employment | 1.04 | 0.87–1.25 | 1.01 | 0.83–1.25 | 0.97 | 0.79–1.20 | 1.04 | 0.82–1.31 |
| BMI, kg/m2 | ||||||||
| Underweight | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| Normal weight | 0.98 | 0.73, 1.32 | 0.98 | 0.73, 1.32 | 0.94 | 0.65, 1.37 | 0.93 | 0.64, 1.34 |
| Overweight | 0.94 | 0.69, 1.28 | 0.95 | .70, 1.30 | 0.84 | 0.57, 1.24 | 0.81 | 0.55, 1.19 |
| Obese | 0.96 | 0.70, 1.31 | 0.96 | 0.70, 1.33 | 1.03 | 0.70, 1.52 | 0.97 | 0.65, 1.43 |
| Severe Obese | 0.83 | 0.58, 1.19 | 0.80 | 0.55, 1.16 | 0.95 | 0.57, 1.57 | 0.84 | 0.51, 1.40 |
| Not reported | 0.95 | 0.56, 1.60 | 0.89 | 0.51, 1.56 | 1.23 | 0.64, 2.45 | 1.21 | 0.62, 2.35 |
| Smoking | 1.06 | 0.87, 1.30 | 1.02 | 0.82, 1.26 | 0.72 | 0.40, 1.32 | 0.68 | 0.37, 1.25 |
| Anxiety | 1.09 | 0.83, 1.43 | 1.11 | 0.83, 1.49 | 1.17 | 0.84, 1.64 | 1.13 | 0.81, 1.59 |
| Depression | 0.96 | 0.87, 1.07 | 0.98 | 0.88, 1.09 | 1.04 | 0.92, 1.19 | 1.01 | 0.89, 1.16 |
| Uterine Fibroids | 0.96 | 0.73, 1.26 | 0.95 | 0.73, 1.27 | 1.37 | 0.97, 1.95 | 1.28 | 0.90, 1.82 |
| Endometriosis | 0.96 | 0.76, 1.20 | 0.93 | 0.73, 1.18 | 1.00 | 0.69, 1.45 | 1.01 | 0.70, 1.47 |
| Grave’s Disease | 0.70 | 0.36, 1.34 | 0.70 | 0.36, 1.36 | 0.44 | 0.15, 1.31 | 0.38 | 0.13, 1.12 |
| Hypothyroidism | 0.97 | 0.74, 1.28 | 1.01 | 0.75, 1.34 | 1.17 | 0.77, 1.78 | 1.04 | 0.68, 1.58 |
| High Blood Pressure | 1.05 | 0.86, 1.28 | 1.09 | 0.88, 1.34 | 1.04 | 0.79, 1.38 | 0.94 | 0.71, 1.24 |
| Elevated Cholesterol | 0.99 | 0.85, 1.14 | 1.02 | 0.88, 1.18 | 1.04 | 0.87, 1.25 | 1.05 | 0.87, 1.26 |
| Diabetes | 0.94 | 0.59, 1.47 | 1.00 | 0.63, 1.60 | 1.18 | 0.70, 1.99 | 1.12 | 0.66, 1.90 |
| PCOS | 0.89 | 0.77, 1.05 | 0.88 | 0.75, 1.04 | 1.10 | 0.89, 1.35 | 0.97 | 0.78, 1.21 |
| Gravidity | ||||||||
| 0 | Referent | Referent | Referent | Referent | Referent | Referent | Referent | Referent |
| 1 | 0.91 | 0.81, 1.04 | 0.92 | 0.81, 1.04 | 1.11 | 0.96, 1.30 | 1.01 | 0.86, 1.18 |
| 2 or more | 0.83 | 0.71,0.98 | 0.83 | 0.70, 0.98 | 1.19 | 1.01, 1.41 | 1.05 | 0.87, 1.25 |
| Not reported | 1.20 | 0.85, 1.70 | 1.23 | 0.80, 1.89 | 0.70 | 0.39, 1.22 | 0.67 | 0.36, 1.23 |
| History of Infertility | 1.03 | 0.92, 1.15 | 1.03 | 0.90, 1.17 | 1.37 | 1.13, 1.66 | 1.20 | 0.98, 1.48 |
| Not reported | 1.05 | 0.81, 1.35 | 1.02 | 0.79, 1.32 | 0.94 | 0.64, 1.39 | 0.94 | 0.64, 1.39 |
| Ongoing duration of time trying to conceive | N/A* | N/A* | N/A* | N/A* | ||||
| 2 months or less | Referent | Referent | Referent | Referent | ||||
| 3–5 months | 1.29 | 1.11, 1.51 | 1.29 | 1.11, 1.51 | ||||
| 6–12 months | 1.44 | 1.26, 1.64 | 1.45 | 1.27, 1.66 | ||||
| 1–3 years | 1.37 | 1.20, 1.55 | 1.38 | 1.20, 1.58 | ||||
Note. CI= confidence interval, IRR= incidence rate ratio, BMI= body mass index, PCOS= polycystic ovarian syndrome
Women contemplating pregnancy were not asked to report the ongoing duration of pregnancy attempt.
Results were also comparable when we fit models for using any one FABM rather than for the number of FABMs used (Supplemental Table 2). In this model, however, history of PCOS was associated with a lower frequency of FABM use among women actively trying to conceive.
Discussion
Results from this study highlight two important issues for preconception counseling. First, the frequency, pattern, and predictors of FABM use differ between women actively trying to conceive and women contemplating pregnancy. FABM use was more common among women trying to conceive than women contemplating pregnancy. Moreover, women trying to conceive used more and different FABM methods than women contemplating pregnancy. Second, very few predictors of FABM use differ between these two groups of women and do not entirely overlap with factors that may be at the forefront of a clinician’s mind when providing preconception counseling, such as age and comorbidities. The duration of ongoing pregnancy attempt and gravidity were the only significant predictors for FABM use among women actively trying to conceive; however, partnership was the only significant predictor for increase in FABM among women contemplating pregnancy within the next year.
Results in the Context of What Is Known
There is not extensive literature on the frequency and patterns of FABM use among women seeking or contemplating pregnancy. Nevertheless, our results on method use and frequency are similar to those reported by Stanford et al. (2019) among participants of the Pregnancy Study Online (PRESTO), which also found that among women seeking pregnancy, the most frequently used fertility method was keeping track of the menstrual cycle length (71% in PRESTO vs. 72% in our study). The reported frequencies of the next most commonly used method in PRESTO, monitoring cervical mucus, were also similar in both studies (39% vs. 41%); however, we observed a higher frequency of use of ovulation prediction kits in our study (32% vs. 41%). In both studies, the prevalence of use for each FABM increased over time, although the frequency of use appeared to plateau among participants in the PRESTO study. In contrast, in our study, there was less evidence of a plateau within the observed range of ongoing duration of pregnancy attempts. Although the similarities in findings between the two cohorts are encouraging, it is essential to point out that the demographic characteristics of both cohorts raise concerns regarding the extent to which these findings may generalize to women of more diverse socioeconomic and racial/ethnic backgrounds.
We did not find any difference in number of methods used among younger or older women, suggesting that age—although a critical clinical consideration when referring a woman to infertility services—is not predictive of FABM use; this held true in women trying to conceive and women contemplating pregnancy within the next year. This finding is similar to the PRESTO findings, which also did not find differences in FABM use when stratified by age (Stanford et al., 2019). No other factors were significant predictors for number of fertility methods used among women actively trying, suggesting that all women who are actively trying to conceive, regardless of medical history, demographic, or physical characteristics, may be making decisions about FABMs use solely on their current duration of pregnancy attempt and gravidity. Asking women trying to conceive about the use of FABMs and how accurately they implement and interpret the methods could initiate conversations with patients about expectations about fertility based on their individual characteristics, and information gathered while using FABMs may facilitate referral to specialized fertility services, if necessary.
We identified that duration of time trying to conceive was predictive of how many fertility-awareness-based methods were used. Future research is needed to identify if there is a trend in method use progression. Both the PRESTO study and our study found that most women used multiple fertility-awareness-based methods in combination with one another (Stanford et al., 2019). Nevertheless, it is possible that women could take a trial-and-error approach rather than adding more methods; future research can consider if and what the trend in method progression is and which methods shorten time to pregnancy. There is also an opportunity for future research to consider which methods are discussed during preconception counseling visits or well-women visits and which methods providers feel confident educating women to use. Results from continued research in this area can inform future educational-based interventions for increasing fertility awareness.
Limitations and Strengths
Although the NHS3 includes participants from across the U.S. and Canada, findings may not be generalizable to groups of women underrepresented in the study population, including racial/ethnic minorities and women with lower educational achievement. Of key concern for this particular study, nurses’ education may influence their knowledge and use of FABMs, and nurses’ schedules may potentially alter the success or ease of using FABMs. The data do not include how women interpreted and implemented FABMs, as different levels of understanding would affect pregnancy rate. Nevertheless, the similarities in findings for frequency and patterns of use in our study and PRESTO—which does not exclusively recruit nurses or other health professionals—suggest that specific education may not be of great concern for generalizability. Furthermore, validity of self-reported duration of pregnancy attempt has not been assessed in this population, although there is extensive documentation in the literature on its reproducibility and validity (Gaskins, Rich-Edwards, Lawson et al., 2015; Gaskins, Rich-Edwards, Missmer et al., 2015).
Because we were able to identify approximately twice as many women endorsing not trying to get pregnant at the moment while stating they were likely to get pregnant within a year than women endorsing being actively trying to get pregnant suggests that relatively minor changes in the way pregnancy intention is assessed could identify a broad spectrum of intention. This suggests that pregnancy intention is a much broader and more fluid concept than currently operationalized in retrospective assessments of pregnancy intention among pregnant women or when prospectively identifying participants for preconception studies. This research did not focus on understanding what affects women’s fertility monitoring behaviors over time in the group who are contemplating pregnancy, as understanding this group has implications for both contraceptive and preconception counseling.
Strengths of this study were use of data obtained from a relatively large sample of women with pregnancy intention (n = 3,237). In contrast to many studies focusing solely on women trying to conceive or women with a history of infertility, our study population included women who stated they were contemplating future pregnancy. The findings provide new knowledge about the fertility method behaviors of this group of women; they can be used to design future research studies which focus on this group’s pregnancy intentions.
Conclusion
Results from this study found that duration of ongoing pregnancy attempt and gravidity is predictive of which and how many FABMs women use. Establishing the length of time a woman has been trying to conceive, as well as what she is currently using for a FABM, may improve her pregnancy attempt because she can share her observations and receive optimized guidance if needed. This may not only contribute to her success but could also spare her the cost, emotional strain, and potential complications of unnecessary infertility referral.
Supplementary Material
Figure 2.
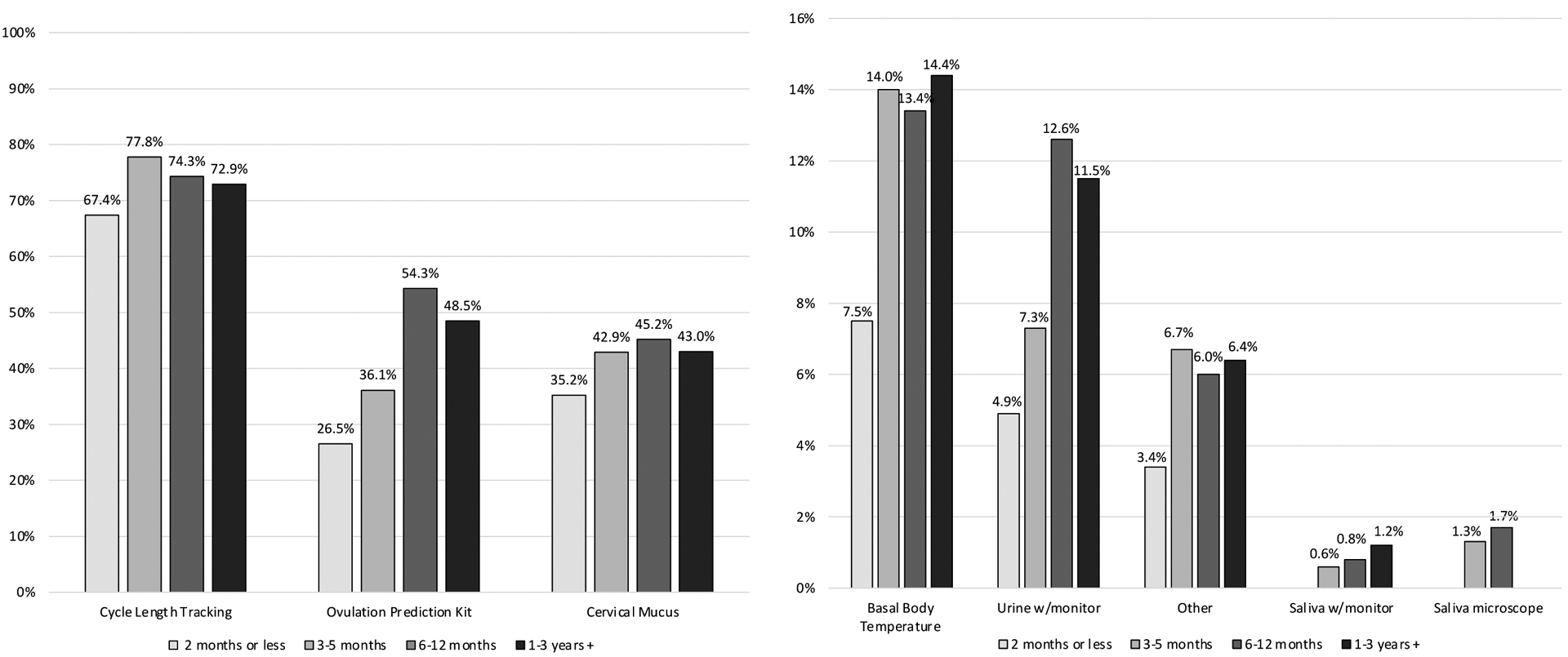
Frequency of FABM use by duration of ongoing attempt trying to conceive among women actively trying to conceive
Acknowledgement:
The authors would like to acknowledge the Channing Division of Network Medicine. Research reported in this publication was supported by grants R24ES028521 and U01HL145386 from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of health.
Footnotes
Disclosure of Interests: The authors report no conflicts of interest.
Ethical Conduct of Research: The study was approved by the MassGeneral Brigham Committee for the Protection of Human Subjects in Research. IRB Protocol Title: A Web-based Questionnaire to Assess Women’s and Men’s Health: The Nurses’ Health Study 3. IRB Protocol Number: 2006P00473
Contributor Information
Melissa Pérez Capotosto, W.F. Connell School of Nursing, Boston College, Chestnut Hill, MA, USA.
Christopher S. Lee, W.F. Connell School of Nursing, Boston College, Chestnut Hill, MA, USA.
Corrine Y. Jurgens, W.F. Connell School of Nursing, Boston College, Chestnut Hill, MA, USA.
Siwen Wang, Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA.
Makiko Mitsunami, Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA.
Brittany M. Charlton, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care; Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA.
Jorge E. Chavarro, Department of Nutrition, Harvard T.H. Chan School of Public Health; Department of Epidemiology, Harvard T.H. Chan School of Public Health, Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts, USA.
References
- Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, & Chavarro JE (2016). Origin, methods, and evolution of the three Nurses’ Health Studies. American Journal of Public Health, 106, 1573–1581. 10.2105/AJPH.2016.303338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duane M, Stanford JB, Porucznik CA, & Vigil P (2022). Fertility awareness-based methods for women’s health and family planning. Frontiers in Medicine, 9, 1359. 10.3389/fmed.2022.858977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capotosto MP (2021). An integrative review of fertility knowledge and fertility-awareness practices among women trying to conceive. Nursing for Women’s Health, 25, 198–206. 10.1016/j.nwh.2021.04.001 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2023). Infertility FAQs. https://www.cdc.gov/reproductivehealth/infertility/index.htm
- Ethics Committee of the American Society for Reproductive Medicine. (2015). Disparities in access to effective treatment for infertility in the United States: An ethics committee opinion. Fertility and Sterility, 104, 1104–1110. 10.1016/j.fertnstert.2015.07.1139 [DOI] [PubMed] [Google Scholar]
- Gaskins AJ, Rich-Edwards JW, Lawson CC, Schernhammer ES, Missmer SA, & Chavarro JE (2015). Work schedule and physical factors in relation to fecundity in nurses. Occupational and Environmental Medicine, 72, 777–783. 10.1136/oemed-2015-103026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskins AJ, Rich-Edwards JW, Missmer SA, Rosner B, & Chavarro JE (2015). Association of fecundity with changes in adult female weight. Obstetrics and Gynecology, 126, 850–858. 10.1097/AOG.0000000000001030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampton KD, Mazza D, & Newton JM (2013). Fertility-awareness knowledge, attitudes, and practices of women seeking fertility assistance. Journal of Advanced Nursing, 69, 1076–1084. 10.1111/j.1365-2648.2012.06095.x [DOI] [PubMed] [Google Scholar]
- Mahey R, Gupta M, Kandpal S, Malhotra N, Vanamail P, Singh N, & Kriplani A (2018). Fertility awareness and knowledge among Indian women attending an infertility clinic: A cross-sectional study. BMC Women’s Health, 18, 177. 10.1186/s12905-018-0669-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse A (2022, April 6). Stable fertility rates 1990–2019 mask distinct variations by age. U.S. Census Bureau. https://www.census.gov/library/stories/2022/04/fertility-rates-declined-for-younger-women-increased-for-older-women.html [Google Scholar]
- Mynarska M, & Rytel J (2018). From motives through desires to intentions: Investigating the reproductive choices of childless men and women in Poland. Journal of Biosocial Science, 50, 421–433. 10.1017/S0021932017000190 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2021). National Survey of Family Growth: Key statistics. https://www.cdc.gov/nchs/nsfg/keystatistics.htm
- Pfeifer S, Butts S, Fossum G, Gracia C, La Barbera A, Mersereau J, Odem R, Paulson R, Penzias A, Pisarska M, Rebar R, Reindollar R, Rosen M, Sandlow J, & Vernon M (2017). Optimizing natural fertility: A committee opinion. Fertility and Sterility, 107, 52–58. 10.1016/j.fertnstert.2016.09.029 [DOI] [PubMed] [Google Scholar]
- Righarts AA, Gray A, Dickson NP, Parkin L, & Gillett WR (2017). Resolution of infertility and number of children: 1386 couples followed for a median of 13 years. Human Reproduction, 32, 2042–2048. 10.1093/humrep/dex271 [DOI] [PubMed] [Google Scholar]
- Sallam HN, & Sallam NH (2016). Religious aspects of assisted reproduction. Facts, Views & Vision in ObGyn, 8, 33–48. [PMC free article] [PubMed] [Google Scholar]
- Shreffler KM, Johnson DR, & Scheuble LK (2010). Ethical problems with infertility treatments: Attitudes and explanations. Social Science Journal, 47, 731–746. 10.1016/j.soscij.2010.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford JB, White GL Jr., & Hatasaka H (2002). Timing intercourse to achieve pregnancy: Current evidence. Obstetrics & Gynecology, 100, 1333–1341. 10.1016/S0029-7844(02)02382-7 [DOI] [PubMed] [Google Scholar]
- Stanford JB, Willis SK, Hatch EE, Rothman KJ, & Wise LA (2019). Fecundability in relation to use of fertility awareness indicators in a North American preconception cohort study. Fertility and Sterility, 112, 892–899. 10.1016/j.fertnstert.2019.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigel G, Ranji U, Long M, & Salganicoff A (2020). Coverage and use of fertility services in the U.S. Kaiser Family Foundation
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


