Version Changes
Revised. Amendments from Version 1
In the second version, the manuscript has been updated as follows: Percentages have been added to the figure to highlight that 67% of the eligible participants were included. We have also included in the description of the sociodemographic data that the 203 children have similar sociodemographic characteristics to the rest of the cohort. We have added the suggested alternative explanations for the pattern of decrease in domestic violence exposure in the discussion. We have added the lack of data on racial violence in our sample as a limitation. We have also discussed the implications of violence exposure on developmental outcomes and highlighted the importance of our descriptive paper in aiding future research investigating these outcomes in young children.
Abstract
Background: Research has highlighted high rates of exposure to violence among South African youth. However, work to date has been largely cross-sectional, focused on violence exposure during the adolescence period, and has been limited to specific types of violence exposure. We examined violence exposure in South African preschool children between 3 and 6 years of age, capturing both direct and indirect forms of violence, and tested for potential sex differences across the several types of exposures.
Methods: Lifetime direct and indirect exposure to domestic and community violence was measured by parental report when children were 3.5 years (N = 530), 4.5 years (N = 749) and 6 years of age (N= 417) in a South African birth cohort located in a peri-urban community.
Results: There are three main findings. First, a large proportion of children (72%-75%) were reported as having been exposed to some form of direct or indirect violent experience in their homes or communities from a young age. Second, there was significant polyvictimization, with 49% of the children being exposed to more than one type of violence by age 6. Third, by 4.5 years of age, there was evidence that boys were more likely than girls to be exposed to domestic victimisation (28% vs. 17%) and polyvictimization (38% vs. 28%).
Conclusions: These findings highlight the high levels of violence exposure in young South African children, particularly among boys, and the need for prevention at both the community and individual levels.
Keywords: childhood exposure to violence, interpersonal violence, community violence, domestic violence; polyvictimization, South Africa, preschoolers
Introduction
Research conducted by the WHO indicates that homicide rates of children under the age of 5 years in South Africa (14.0 and 11.7 per 100 000 for boys and girls, respectively) were more than twice as high as the average for low and middle-income countries (LMICs; ( Krug et al., 2002). Moreover, the estimated economic burden of violence against children in South Africa is high. In 2015, an estimated 2.3 million disability-adjusted life years (DALYs) were lost in South Africa due to non-fatal violence against children, and 84,287 due to fatal child-focused violence. The estimated economic cost of DALYs lost to violence against children in 2015 was ZAR173 billion (USD 13.5 billion)—or 4.3% of the country’s gross domestic product that year ( Fang et al., 2017).
The causes of violence in South Africa are multifaceted. It is considered to be embedded in the colonial history and legacy of apartheid as under the apartheid government violence was widely accepted and normalised ( Bruce, 2009; Ward et al., 2013). Extensive poverty, inequality, high unemployment rates together with a fragile law enforcement system, the rise of urbanisation, poor housing and education outcomes all play a role in the perpetuation of community violence ( Bruce et al., 2007; Seedat et al., 2009). Furthermore, intimate partner violence (IPV) and physical disciplining methods such as corporal punishment are widely tolerated and accepted as social norms and are intergenerationally transferred. For example, in one study, 58% of South African caregivers reported having smacked their children at least once and 33% reported using an object such as a belt ( Dawes et al., 2005). A cycle of vulnerability to violence may also exist, with maltreatment among mothers in childhood being linked with an increased risk of experiencing IPV in pregnancy, and adulthood ( Barnett et al., 2018). Sex differences in violence exposure types have also been reported, where teenage boys have a higher risk of becoming victims of homicide and community violence than girls ( Mathews et al., 2013).
Despite compelling evidence of substantial violence exposure among South African youth, and in other LMIC populations, substantial gaps exist in our knowledge. First, existing studies have focused on adolescents rather than younger children, with little evidence on preschool children in particular. Second, most work has been cross-sectional, with few longitudinal studies. Understanding how patterns of violence exposure may change with age is relevant to developing targeted prevention strategies. Third, studies have often focused on single forms of violence exposure (e.g., IPV), and there is a need to explore a range of direct and indirect forms of trauma exposure to provide a full picture of the risks to children. Relatedly, there is limited research on polyvictimisation - the phenomenon where individuals are exposed to multiple forms of trauma - despite evidence that polyvictimisation is a particular risk factor for poor child outcomes ( De Bellis et al., 2013; Finkelhor et al., 2015; Ford, 2021; Haahr-Pedersen et al., 2020a; Kaminer et al., 2013a; Le et al., 2018). Finally, little work has described sex differences in exposure to violence, which may be important to consider in the development of targeted intervention strategies. In sum, research investigating the exact patterns of violence exposure in the day-to-day lives of preschool children is needed. This is essential in South Africa where interpersonal violence is particularly high.
We addressed the above research gaps using a longitudinal South African birth cohort, the Drakenstein Child Health Study (DCHS), which provides a unique resource for doing so. Previous studies using the DCHS cohort found high levels of IPV and childhood trauma among mothers ( Stein et al., 2015). Here we explored the violence exposure patterns in the DCHS children born to these mothers, who consisted of males and females aged between 3 to 6 years, and where both direct and indirect forms of violence were longitudinally measured across 3 different time points. Sex differences in exposure patterns were also examined as well as the extent of polyvictimisation in this young age group.
Research Methods
Study Design
The DCHS is a longitudinal study employing a multidisciplinary approach to investigate the early-life determinants of child health in two peri-urban communities in the Drakenstein sub-district of the Cape Winelands, Western Cape, South Africa ( Zar et al., 2015). Longitudinal measurements of risk factors in seven domains (environmental, infectious, nutritional, genetic, psychosocial, maternal and immunological) are used to investigate child health in addition to maternal and paternal health. The early-life component of the study centres on a wide range of developmental outcomes in domains that include physical health and growth as well as neurodevelopmental, cognitive and psychological health ( Donald et al., 2018).
Study Setting
The study population is characterised by low-socioeconomic status (SES) and multiple psychosocial risk factors are prevalent, such as single-parent households, high rates of psychological distress and violence exposure, HIV and illicit drug use, high levels of violence and intimate partner violence ( Groves et al., 2015) and low levels of employment and educational achievement ( Stein et al., 2015). The population is a stable one, with low immigration or emigration and over 90% of the inhabitants use the public health care systems. In view of the factors above, the DCHS cohort can be considered representative of other South African and LMICs peri-urban communities.
Participants
Pregnant women were recruited whilst attending one of the two primary healthcare clinics in the area, Mbekweni (serving a predominantly Black African ancestry community) and TC Newman (serving a predominantly mixed ancestry community 1 ) between March 2012 and March 2015. Pregnant women were enrolled if they were at least 18 years of age, received their antenatal care at either of the two clinics and planned on remaining in the area for at least one year. Mothers who consented were enrolled at 20–28 weeks’ gestation and mother-child dyads have been followed longitudinally; to date, the oldest children are 10 years of age. At enrolment, mothers provided informed written consent and were further re-consented annually after childbirth. Mother-child dyads attended follow-up visits at the two clinics and Paarl Hospital ( Stein et al., 2015). Trained study staff from the community guided the informed consent process with the mothers in the mothers’ language of choice, isiXhosa, Afrikaans or English.
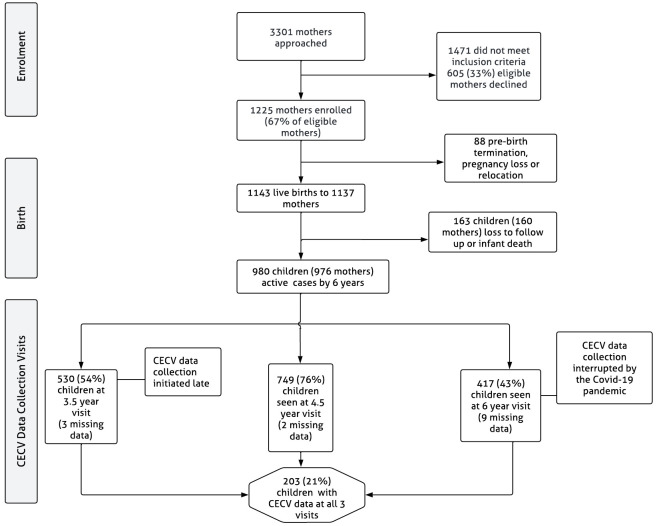
A total of 1137 mother-child dyads were enrolled in the study, from these, four mothers had twins and one had triplets. Therefore, the total number of children who were enrolled in the study is 1143. Due to attrition (see Figure 1 for details), the current sample in the DCHS is 980. All the children were born at the main hospital and child sex was established at birth. Here, sex, classified as female or male, refers to a set of biological attributes in humans linked with physical and physiological features including chromosomes, gene expression, hormone function and reproductive/sexual anatomy ( Coen & Banister, 2012).
Figure 1. DCHS flowchart for CECV data collection.
Procedures and Data Collection Measures
Sociodemographic characteristics. A questionnaire adapted from the South African Stress and Health (SASH) Study ( Myer et al., 2008) was used to collect data on sociodemographic variables such as household income, employment status and education. The questionnaire was administered by trained study staff in interview format antenatally at 28 to 32 weeks’ gestation and during annual study visits.
Violence Exposure. The Child Exposure to Community Violence Checklist (CECV) is a parent-report measure comprised of 35 items assessing the children’s lifetime exposure to domestic, school and community violence.
A standard forward and backward approach ( Smit et al., 2006) was used to translate the measure from English to isiXhosa and Afrikaans. Translations were further cross-checked with study staff based in study communities to ensure that the appropriate dialect was used. The measure was administered by trained research assistants in Afrikaans for the Afrikaans-speaking participants and isiXhosa through the aid of interpreters for the isiXhosa-speaking participants. An interview format was adopted due to the low levels of literacy in the sample, such that mothers were afforded the means to request for clarification when needed.
The CECV version used in the study was adapted to more correctly target the South African population ( Bruwer et al., 2008; Fincham et al., 2009) as well as the study focus. It has shown good psychometric properties such as good internal reliability in previous South African studies such as r = .93 ( Fincham et al., 2009), r =.86 ( Kaminer et al., 2013d) and r = .85 - .87 ( Kaminer et al., 2013b). The checklist is coded on a four-point Likert scale rating the frequency of exposure ranging from “0” (never), to “3” (many times). Here we collapsed the responses to create a binary yes/no indicator of exposure for each item by combining exposure to violence ratings “once”, “a few times” and “many times” to indicate “yes” to violence exposure and retained the rating “never” as an indication of no exposure. This was done to enable us to create subscales and a total exposure score, that clearly reflect the number of types of violence exposures, as opposed to conflating exposure frequency and type.
The total exposure score ( Overall Violence Exposure, α = 0.88) was generated from the CECV by summing over the 35 items with high scores indicating a greater frequency of exposure (range 0–35). We also created four subscales from the CECV items to characterise violence exposure patterns in this cohort, namely, Witnessing Community Violence (10 items, α = .72), Community Victimisation (8 items, α = .75), Witnessing Domestic Violence (6 items, α = .75) and Domestic Victimisation (11 items, α = .79) consistent with previous studies that used this measure ( Kaminer et al., 2013c; Kaminer et al., 2013d). We defined polyvictimisation as a score of 1+ on two or more subscales.
Ethical considerations
All procedures performed were in accordance with the ethical standards of the Medical Research Council in South Africa and with the Helsinki Declaration (2013. The study protocol including consent forms was approved by the Faculty of Health Sciences Research Ethics Committee, University of Cape Town (401/2009), and by the Western Cape Provincial Research committee (2011RP45). Given the content of the CECV scale, a key obligation in the study was to flag instances of abuse, trauma and mental health issues. An active referral system was in place for both mothers and children supported by close relationships between study staff and provincial health staff. Furthermore, all women participating in the study, regardless of specific mental or physical health problems, were informed about social and support service providers available to them.
Data analysis
Data analysis was performed using R Statistical Software (version 4.0.2) and R Studio (version 1.3.1073) for Mac. Given that the exact timing of violence exposure was not measured, each timepoint was cross-sectionally analysed. Prevalence of Overall violence Exposure and subtypes of violence were descriptively summarised using counts and proportions. We examined the distributions of subscales and Overall violence Exposure using the Shapiro-Wilk test of normality. The frequency of polyvictimisation was also explored. Chi-square analyses were conducted to explore sex and sociodemographic differences in violence exposure.
Missing Data
Item nonresponse occurred on the CECV scale in some of the cases where the CECV was completed at each visit. At the 3.5-year visit (N = 530), 3 cases (0.6%) had incomplete data, at the 4.5-year visit (N = 749), 2 cases (0.3%) had incomplete data and at the 6-year visit (N = 417), 9 cases (2.2%) had incomplete data ( Figure 1).
In these cases, item nonresponse was handled by imputing missing values using the single modal imputation method for each measurement occasion separately. Modal imputation was carried out using Base R functions of R Statistical Software (version 4.0.2)
Results
The sample sizes at each age/visit differ from the current total DCHS sample ( N = 980). This is due to late CECV data collection initiation at the first study visit (age 3.5), data collection interruptions at the 6-year visit due to the COVID-19 pandemic, and non-response at any one of the time points. Only 203 children had CECV data at all 3 visits ( Figure 1). Participants’ sociodemographic characteristics are summarized in Table 1. Most of the households are from a low SES, with 49% having a monthly household income between 1000–5000 ZAR (62 - 310 USD), and 38% earning less than 1000 ZAR (62 USD) per month. Many children came from single-parent households and lived with on average 4 to 5 people. Furthermore, mothers reported high levels of unemployment and low levels of educational attainment. The distribution of characteristics was similar in participants who attended the 3.5, 4.5- and 6-year clinics, the 203 children with CECV data at all 3 visits and the cohort overall.
Table 1. Demographic profiles and baseline descriptive statistics of the sample stratified by visit.
| 3.5 years
( N = 530) |
4.5 years
( N = 749) |
6 years
( N = 417) |
Subsample
(N=203) |
Full cohort
( N = 1137) |
|
|---|---|---|---|---|---|
| Sex | |||||
| Female | 262 (49%) | 371 (50%) | 198 (48%) | 95 (47%) | 550 (48%) |
| Average household income per month | |||||
| <1000 ZAR (62 USD) | 179 (34%) | 272 (36%) | 162 (39%) | 76 (37%) | 430 (38%) |
| 1000–5000 ZAR (62 – 310 USD) | 282 (53%) | 388 (52%) | 199 (48%) | 97 (48%) | 553 (49%) |
| >5000 ZAR (310 USD) | 69 (13%) | 89 (12%) | 56 (13%) | 30 (15%) | 154 (14%) |
| Mother's Education | |||||
| Primary | 38 (7%) | 60 (8%) | 42 (10%) | 8 (9%) | 86 (8%) |
| Some Secondary | 292 (55%) | 411 (55%) | 213 (51%) | 100 (49%) | 606 (53%) |
| Completed Secondary | 171 (32%) | 235 (31%) | 146 (35%) | 75 (37%) | 372 (33%) |
| Any tertiary | 29 (6%) | 43 (6%) | 16 (4%) | 10 (5%) | 73 (6%) |
| Mother’s Employment Status | |||||
| Unemployed | 388 (73%) | 560 (75%) | 313 (75%) | 149 (73%) | 831(73%) |
| Mother’s Partnership status | |||||
| Married/cohabiting | 223 (42%) | 301 (40%) | 164 (39%) | 77 (38%) | 458 (40%) |
| Number of people in the household | |||||
| Median (IQR) | 4(3–6) | 5 (3–6) | 4 (3–6) | 4(3–6) | 4 (3–6) |
Violence exposure patterns
The proportions of children exposed to any form of violence, as well as subscale scores and item level exposure by age at measurement are presented in Table 2. Exposure to any form of violence by each of the visits was 72%, 75% and 76%, at ages 3.5, 4.5 and 6 years respectively. Witnessing Community Violence was the most prevalent trauma: (62%, 67% and 69%), followed by Domestic Victimisation (24%, 23% and 31%), Witnessing Domestic Violence (28%, 24% and 21%) and Community Victimisation (9%, 9% and 14%). Similar prevalence rates are reported in the subsample (N = 203) of those participants consistently seen at all visits, see Supplementary Table 1.
Table 2. Prevalence of Exposure to Specific Violence Types at Each Study Visit.
| 3.5 years
( N = 530) |
4.5 years
( N = 749) |
6 years
( N = 417) |
|
|---|---|---|---|
| Exposure at Least Once | |||
| Exposure to any form of violence | 383 (72.3%) | 562 (75.0%) | 318 (76.3%) |
| Witnessing community violence | 329 (62.1%) | 499 (66.6%) | 287 (68.8%) |
| Heard gunshots | 199 (37.5%) | 315 (42.1%) | 201 (48.2%) |
| Seen someone beaten up in the neighbourhood | 219 (41.3%) | 341 (45.5%) | 184 (44.1%) |
| Seen dead body in the neighbourhood | 35 (6.6%) | 64 (8.5%) | 39 (9.4%) |
| Seen somebody point a gun at another in the neighbourhood | 31 (5.8%) | 42 (5.6%) | 34 (8.2%) |
| Seen somebody get shot in the neighbourhood | 8 (1.5%) | 22 (2.9%) | 22 (5.3%) |
| Seen somebody point a knife at another in the neighbourhood | 75 (14.2%) | 119 (15.9%) | 72 (17.3%) |
| Seen somebody get stabbed in the neighbourhood | 47 (8.9%) | 65 (8.7%) | 50 (12.0%) |
| Seen someone forced to do something sexual neighbourhood | 3 (0.6%) | 1 (0.1%) | 7 (1.7%) |
| Child known someone killed by another | 15 (2.8%) | 30 (4.0%) | 22 (5.3%) |
| Seen someone being killed by another person elsewhere | 7 (1.3%) | 11 (1.5%) | 9 (2.2%) |
| Community victimisation | 45 (8.5%) | 68 (9.1%) | 58 (13.9%) |
| House robbery child present | 24 (4.5%) | 27 (3.6%) | 34 (8.2%) |
| Someone threatened to beat up the child at school or creche | 12 (2.3%) | 14 (1.9%) | 22 (5.3%) |
| Someone threatened to beat up the child elsewhere | 12 (2.3%) | 15 (2.0%) | 13 (3.1%) |
| Child been beaten up elsewhere | 7 (1.3%) | 22 (2.9%) | 13 (3.1%) |
| Someone elsewhere threatened to kill the child | 1 (0.2%) | 3 (0.4%) | 4 (1.0%) |
| Someone at school or creche threatened to shoot or stab the
child |
2 (0.4%) | 1 (0.1%) | 7 (1.7%) |
| Someone elsewhere threatened to shoot or stab the child | 2 (0.4%) | 1 (0.1%) | 5 (1.2%) |
| Someone shot or stabbed the child elsewhere | 2 (0.4%) | 1 (0.1%) | 4 (1.0%) |
| Witnessing domestic violence | 147 (27.7%) | 179 (23.9%) | 86 (20.6%) |
| Seen grownups at home hit each other | 138 (26.0%) | 169 (22.6%) | 73 (17.5%) |
| Seen somebody point gun at another at home | 10 (1.9%) | 5 (0.7%) | 10 (2.4%) |
| Seen someone at home get stabbed | 21 (4.0%) | 22 (2.9%) | 22 (5.3%) |
| Seen someone at home get shot | 3 (0.6%) | 2 (0.3%) | 5 (1.2%) |
| Seen someone forced to do something sexual | 2 (0.4%) | 2 (0.3%) | 9 (2.2%) |
| Seen someone being killed by another person at home | 2 (0.4%) | 7 (0.9%) | 6 (1.4%) |
| Domestic victimisation | 125 (23.6%) | 169 (22.6%) | 130 (31.2%) |
| Someone threatened to beat up the child at home | 12 (2.3%) | 15 (2.0%) | 25 (6.0%) |
| Child been beaten up at home | 12 (2.3%) | 16 (2.1%) | 15 (3.6%) |
| Someone at home threatened to kill the child | 4 (0.8%) | 3 (0.4%) | 8 (1.9%) |
| Family member threatened to shoot or stab the child | 1 (0.2%) | 1 (0.1%) | 5 (1.2%) |
| Someone shot or stabbed the child at home | 2 (0.4%) | 3 (0.4%) | 4 (1.0%) |
| Someone made the child do something sexual | 5 (0.9%) | 6 (0.8%) | 10 (2.4%) |
| Family member shouts at the child fiercely and loudly | 60 (11.3%) | 60 (8.0%) | 39 (9.4%) |
| Anyone at home used a stick or belt or hard item to hit the
child |
34 (6.4%) | 50 (6.7%) | 54 (12.9%) |
| Anyone at home hit the child so hard they were hurt | 19 (3.6%) | 26 (3.5%) | 23 (5.5%) |
| Anyone at home said the child would be sent away or kicked
out |
12 (2.3%) | 17 (2.3%) | 31 (7.4%) |
| Anyone at home called the child horrible names | 43 (8.1%) | 66 (8.8%) | 53 (12.7%) |
Looking at all three time points, the most prevalent exposures in the Witnessing Community Violence subscale were hearing gunshots (38% – 48%) and seeing someone beaten up in the neighbourhood (41% – 46%). In the Community Victimisation subscale, the most common exposure was House robbery occurring whilst the child was present (4% – 8%). Seeing grownups fighting (18% – 26%) was the most common exposure in the Witnessing Domestic Violence subscale. The most prevalent Domestic Victimisation subtypes were the child being hit by a stick, belt or another hard item at home (6% – 13%), the child being shouted at fiercely and loudly by a family member (8% – 11%) and child being called horrible names by someone at home (8% – 13%).
Table 3 provides summary statistics (proportion exposed, median, IQR and range) for the overall violence score and subscales by age and sex. The only evidence for sex differences was seen for reported exposure to Domestic Victimisation by age 4.5, where more boys than girls had reports of exposure (28% vs. 17%).
Table 3. Prevalence of forms of violence by each visit stratified by sex.
p-value: Chi-square test.
| 3.5 Years ( N = 530) | 4.5 Years ( N = 749) | 6 Years ( N = 417) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female
( n = 262) |
Male
( n = 268) |
p-value | Female
( n = 371) |
Male
( n = 378) |
p-value | Female
( n = 198) |
Male
( n = 219) |
p-value | |
| Overall Violence Exposure | |||||||||
| Exposed | 179 (68%) | 203 (77%) | 0.07 | 273 (74%) | 288 (76%) | 0.46 | 148 (75%) | 164 (75%) | 1.00 |
| Min / Max | 0 / 35 | 0 / 15 | 0 / 14 | 0 / 35 | 0 / 34 | 0 / 35 | |||
| Med (IQR) | 1 (0;3) | 2 (1;3) | 1 (0;2) | 2(1;3) | 1(1;3) | 2(1;4) | |||
| Witnessing Community Violence | |||||||||
| Exposed | 153 (58%) | 175 (65%) | 0.12 | 237 (64%) | 261 (69%) | 0.16 | 129 (65%) | 154 (70%) | 0.31 |
| Min / Max | 0 / 10 | 0 / 8.0 | 0 / 6 | 0 / 10 | 0 / 9 | 0 / 10 | |||
| Med (IQR) | 1 (0;2) | 1.0 (0;2) | 1(0;2) | 1 (0;2) | 1 (0;2) | 1 (0;3) | |||
| Community Victimisation | |||||||||
| Exposed | 19 (7%) | 24 (9%) | 0.58 | 28 (8%) | 39 (10%) | 0.23 | 19 (10%) | 32 (15%) | 0.16 |
| Min / Max | 0 / 8 | 0 / 3.0 | 0 / 2 | 0 / 8 | 0 / 8 | 0 / 8 | |||
| Med (IQR) | 0 (0;0) | 0 (0;0) | 0 (0;0) | 0 (0;0) | 0 (0;0) | 0 (0;0) | |||
| Witnessing Domestic Violence | |||||||||
| Exposed | 66 (25%) | 80 (30%) | 0.27 | 82 (22%) | 96 (25%) | 0.33 | 39 (20%) | 41 (19%) | 0.90 |
| Min / Max | 0 / 6 | 0 / 4 | 0 / 4 | 0 / 6 | 0 / 6 | 0 / 6 | |||
| Med (IQR) | 0 (0;1) | 0 (0;1) | 0 (0;0) | 0 (0;1) | 0 (0;0) | 0 (0;0) | |||
| Domestic Victimisation | |||||||||
| Exposed | 54 (21%) | 69 (26%) | 0.19 | 64 (17%) | 104 (28%) | 0.001 | 51 (26%) | 73 (33%) | 0.11 |
| Min / Max | 0 / 11 | 0 / 6 | 0 / 5 | 0 / 11 | 0 / 11 | 0 / 11 | |||
| Med (IQR) | 0 (0;0) | 0 (0;1) | 0 (0;0) | 0 (0;1) | 0 (0;1) | 0 (0;1) | |||
Table 4 provides frequencies of violence exposure by marital status, household income and age. There was no evidence of associations between violence exposure and maternal marital status or social economic status (indicated by household income).
Table 4. Violence Exposure by Marital Status and Household Income.
p-value: Chi-square test.
| Overall Viole
nce
Exposure |
Witnessing
Community Violence |
Community
Victimization |
Witnessing
Domestic Violence |
Domestic
Victimization |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3.5 years ( N = 530) | ||||||||||
| Exposed
( n = 382) |
p-value | Exposed
( n = 328) |
p-value | Exposed
( n = 43) |
p-value | Exposed
( n = 146) |
p-value | Exposed
( n = 123) |
p-value | |
| Mother's Marital Status | ||||||||||
| Married/cohabiting
(n = 223) |
170 (76%) | 0.09 | 143 (64%) | 0.41 | 22 (10%) | 0.27 | 65 (29%) | 0.55 | 54 (24%) | 0.72 |
| Single (n = 307) | 212 (69%) | 185 (60%) | 21 (7%) | 81 (26%) | 69 (22%) | |||||
| Household Income | ||||||||||
| < R1000/m (n = 179) | 133 (74%) | 0.59 | 121 (68%) | 0.15 | 10 (6%) | 0.15 | 46 (26%) | 0.62 | 40 (22%) | 0.54 |
| R1000–5000/m (n = 282) | 198 (70%) | 167 (59%) | 24 (9%) | 78 (28%) | 70 (25%) | |||||
| >R5000/m (n = 69) | 51 (74%) | 40 (58%) | 9 (13%) | 22 (32%) | 13 (19%) | |||||
| 4.5 years ( N = 749) | ||||||||||
| Exposed
(n = 561) |
Exposed
(n = 498) |
Exposed
(n = 67) |
Exposed
(n = 178) |
Exposed
(n = 168) |
||||||
| Mother's Marital Status | ||||||||||
| Married/ cohabiting
(n = 301) |
230 (76%) | 0.49 | 202 (67%) | 0.83 | 23 (8%) | 0.37 | 78 (26%) | 0.30 | 61 (20%) | 0.28 |
| Single (n = 448) | 331 (74%) | 296 (66%) | 44 (10%) | 100 (22%) | 107 (24%) | |||||
| Household Income | ||||||||||
| < R1000/m (n = 272) | 207 (76%) | 0.82 | 185 (68%) | 0.65 | 26 (10%) | 0.50 | 58 (21%) | 0.49 | 64 (24%) | 0.09 |
| R1000–5000/m (n = 388) | 287 (74%) | 252 (65%) | 36 (9%) | 97 (25%) | 77 (20%) | |||||
| >R5000/m (n = 89) | 67 (75%) | 61 (69%) | 5 (6%) | 23 (26%) | 27 (30%) | |||||
| 6 years ( N = 417) | ||||||||||
| Exposed
(n = 312) |
Exposed
(n = 283) |
Exposed
(n = 51) |
Exposed
(n = 80) |
Exposed
(n = 124) |
||||||
| Mother's Marital Status | ||||||||||
| Married/ cohabiting
(n = 164) |
125 (76%) | 0.68 | 113 (69%) | 0.80 | 19 (12%) | 0.87 | 30 (18%) | 0.81 | 50 (30%) | 0.87 |
| Single (n = 253) | 187 (74%) | 170 (67%) | 32 (13%) | 50 (20%) | 74 (29%) | |||||
| Household Income | ||||||||||
| < R1000/m (n = 162) | 118 (73%) | 0.21 | 103 (64%) | 0.17 | 22 (14%) | 0.77 | 29 (18%) | 0.61 | 41 (25%) | 0.16 |
| R1000-5000/m (n = 199) | 156 (78%) | 144 (72%) | 22 (11%) | 42 (21%) | 68 (34%) | |||||
| >R5000/m (n = 56) | 38 (68%) | 36 (64%) | 7 (12%) | 9 (16%) | 15 (27%) | |||||
Prevalence of Polyvictimisation
Table 5 reports rates of polyvictimisation in the sample by each visit. By the age of 6 years, 49% of participants who were exposed to some form of violence, were exposed to multiple types of violence. Furthermore, sex differences were observed at the 4.5-year visit, where more boys (37%) experienced significantly more lifetime polyvictimisation than girls (31%).
Table 5. Prevalence of Polyvictimization Stratified by Sex.
p-value: Chi-square test.
| Polyvictimisation | 3.5 years ( N = 530) | 4.5 years (N = 749) | 6 years (N = 417) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Female
(n = 262) |
Male
(n = 268) |
p-value | Female
(n = 371) |
Male
(n = 378) |
p-value | Female
(n = 198) |
Male
(n = 219) |
p-value | |
| Any Polyvictimisation | 80 (31%) | 99 (37%) | 0.14 | 105 (28%) | 145 (38%) | 0.00 | 64 (32%) | 91 (42%) | 0.06 |
| Number of different types of violence exposure | |||||||||
| None | 82 (31%) | 65 (24%) | 0.32 | 98 (26%) | 89 (24%) | 0.01 | 48 (24%) | 51 (23%) | 0.25 |
| One type | 98 (37%) | 104 (39%) | 168 (45%) | 143 (38%) | 84 (42%) | 72 (33%) | |||
| Two types | 52 (20%) | 60 (22%) | 75 (20%) | 91 (24%) | 42 (21%) | 56 (26%) | |||
| Three types | 24 (9%) | 32 (12%) | 27 (7%) | 41 (11%) | 18 (9%) | 29 (13%) | |||
| Four types | 6 (2%) | 7 (3%) | 3 (1%) | 14 (4%) | 6 (3%) | 11 (5%) | |||
Discussion
In this South African birth cohort, we found that a large proportion of children (72%-75%) were exposed to direct and indirect violent experiences in their homes as well as in the community from a very young age with substantial numbers experiencing polyvictimization. Boys and girls were similarly exposed to violence overall, but there was some evidence that boys were more vulnerable to Domestic Victimisation and polyvictimization by age 4.5 years of age.
By the age of 3.5 years, 72% of the children in this cohort had been exposed to some form of violence with Witnessing Community Violence as the most prevalent form of violence reported. This is consistent with the reports of high homicide rates and gang-related violence in the Western Cape region ( South African Police Service, 2021). Other studies with older children in the Western Cape also reported high exposure to community violence. One study found that 98.9% of their sample (aged 12–15 years) had witnessed community violence ( Kaminer et al., 2013c) whilst another found that 84.1% of their sample ( Mean age = 14.2 years) had been exposed to violence ( Stansfeld et al., 2017). A study providing national estimates of trauma exposure in South African adults also found high levels of witnessing violence ( Atwoli et al., 2013), suggesting that this form of trauma is potentially pervasive across the life span in some South African contexts.
Domestic violence was also commonly reported, consistent with earlier reports on IPV during pregnancy in this cohort ( Barnett et al., 2018). Similar prevalence estimates (20% – 31%) were reported on average for both witnessed domestic violent acts as well as violent acts directed at the child at home. Finding that reports of witnessed domestic violence decreased with age, unlike the other forms of violence, may however suggest underreporting of IPV. IPV and domestic violence are typically considered private matters and rely on people feeling able to divulge this sensitive information. Nonetheless, child exposure to IPV is limited, despite its occurrence; or many caregivers may be of the impression that their children are not being exposed to violence in the home, nor attending to or being affected by the incidences of IPV and domestic violence in the family. Furthermore, children’s social-emotional and cognitive development becomes more apparent to caregivers as the children grow older such that parents may appreciate the impact of domestic violence on the children and as such underreport children’s exposure to it. Additionally, it is possible that caregivers under-estimate the extent to which young children are aware of the violence occuring in parts of the home or after the child has gone to bed. Indeed preivous studies have found descripencies between parent and child reports of domestic violence exposure. Alternatively, it is also possible that children in our sample were witnessing less violence with age, given that younger children require more attention which places strain on caregiver relationships subsequently resulting in domestic violence. As such children may be at a greater risk of witnessing domestic violence at younger ages.
Although Community Victimisation is the least prevalent form of reported violence exposure in these early years, it is likely to increase in prevalence as the children get older and spend more time outside the home. Indeed other studies conducted in South Africa in older children found this type of violence highly prevalent in adolescents ( Haahr-Pedersen et al., 2020b; Kaminer et al., 2013e). The finding that a majority of children were exposed to community violence from as young as 3.5 years of age is particularly concerning, given associations between community violence exposure and later aggression ( Grasso et al., 2016), other mental health problems including posttraumatic stress disorder (PTSD) and internalising and externalizing behavioural problems in children and adolescents, respectively ( Fowler et al., 2009a).
Polyvictimisation was reported in this cohort, especially at the 6.5-year visit, where 49% of the children were reported to have been exposed to more than one type of violence, while at the 3.5- and 4.5-year visits the prevalence rates were 34% and 33% respectively. The higher prevalence at the later visit is possibly a result of older children being exposed to different settings beyond the family home such as school and the community where they may experience violence in these contexts in addition to that in the domestic environment. Indeed, even higher polyvictimisation prevalence has been reported in older children, for example, 93% of adolescents aged 12–15 years reported experiencing polyvictimisation in a Cape Town study ( Kaminer et al., 2013c) whilst another more recent national South African study reported polyvictimisation in 64% adolescents aged 15 – 17 years ( Leoschut & Kafaar, 2017). Finding high rates of polyvictimisation in our sample of such young children is important, given that research has shown that polyvictimisation may contribute to the experience of cumulative stress, aggravating later health outcomes and potentially altering developmental trajectories ( Appleyard et al., 2005; Teicher et al., 2006). Furthermore, polyvictimisation has been found to be a stronger risk factor for mental health problems than single forms of victimization (see review by ( Haahr-Pedersen et al., 2020c).
More boys than girls in this cohort were reportedly exposed to polyvictimisation by age 4.5 years. Studies have reported mixed findings regarding the relationship between sex and children’s exposure to violence. While our study used parent reports, other studies using self-report measures also found that older boys reported more exposure to violence than girls ( Falconer et al., 2021; Kamine et al., 2013c; Kaminer et al., 2013e; Shields et al., 2008) whilst others found no differences in reported exposure to violence ( Asagba et al., 2021; Finkelhor et al., 2015; Sternberg et al., 2006). Although research on sex differences in polyvictimization prevalence patterns is very limited, one other study also found that polyvictimization was higher in boys in their sample of adolescents aged 12–15 years living in Cape Town ( Kaminer et al., 2013c). Differential socialization of the sexes may explain this discrepancy as boys may be less protected than girls allowing them to spend more time outside the home, making them more vulnerable to other forms of violence. There was also some evidence in our study that boys experience more domestic victimisation, suggesting there could also be differences in parental perceptions of the suitability of harsh discipline practices for girls versus boys. Some studies have shown that boys are punished more frequently than girls due to differences in gender roles and expectations between the two sexes (see review by Lokot et al., 2020). Here, gender refers to the socially constructed roles, behaviours and identities of female, male and gender-diverse people( Coen & Banister, 2012).
South Africa’s political history of oppression and the structural and socioeconomic inequalities that have persisted in society are likely to contribute to the high levels of violence in these communities. These rates of violence exposure may not be generalisable to all South African communities. However, this cohort is representative of many communities in low and middle-income countries, with high rates of poverty, unemployment, and low levels of educational attainment among women. Given that the majority of studies reporting on children’s exposure to violence have mostly used samples of older children ( Falconer et al., 2021; Hillis et al., 2016; Hinsberger et al., 2016; Kaminer et al., 2013c; Kaminer et al., 2013e; Shields et al., 2008) finding that violence exposure is common in this sample of pre-schoolers suggests that many children experience the persistent threat of violence throughout the life course and importantly, during early formative years.
Finding no evidence of associations between violence exposure and maternal marital status or socioeconomic status in this cohort suggests that children in our study are similarly exposed to violence regardless of their background. This may be expected given that the DCHS children live in similar contexts where community violence is a common phenomenon. Furthermore, certain types of violence such as intimate partner violence and corporal punishment are widely accepted in the South African society ( Mathews et al., 2014). As such, children in our sample are exposed to similar rates of domestic violence regardless of their mother’s socioeconomic context.
Notably, violence exposure in early childhood occurs during sensitive and critical periods of development lasting from infancy to adolescence and can disrupt brain development and consequently impacting affective and neurocognitive systems ( Hertzman & Boyce, 2010) . Young children such as those in our sample experiencing violence during this period have increased risk of short term and long term poor developmental outcomes such as impaired socio-emotional development, mental health problems, poor cognitive functions and physical health problems in adulthood (see reviews: Fowler et al., 2009b; Maguire et al., 2015; Norman et al., 2012; Young-Southward et al., 2020). Previous research has highlighted the early childhood period as a key developmental stage where violence exposure occurring here is associated with greater health problems than violence occurring in other periods ( Cowell et al., 2015; Dunn et al., 2020; Vu et al., 2016). This is important given that existing literature investigating violence exposure has focused particularly on adolescents and adults, neglecting young children. As such, this, together with our findings, emphasize the need for closer attention to be paid to young children such as those in our sample, whose development is taking place in violent contexts. Notably, this descriptive study has provided context for future research to investigate the relatioships between violence exposure and socio-emotional, mental health and cognitve outcomes in young children in the DCHS and similar settings.
The findings of this study should be considered in view of some methodological limitations. Firstly, only a subsample of children was consistently seen at all three visits, such that the sample sizes differ at each visit and comprise different children. Secondly, there is no information about the exact timing of exposure to violence. Thirdly, given that violence exposure relied on caregiver reports and recall; exposure was likely underreported due to social desirability biases. This is a common limitation of studies that examine trauma exposure or maltreatment in children given that young children are unlikely to be developmentally capable of understanding the concept of a ‘violent act’ and reporting it adequately ( Shahinfar et al., 2000). Furthermore, obtaining reports of violence exposure from young children may risk re-traumatising them. The high prevalence rates of violence exposure reported are particularly important given the likelihood of underreporting in some domains. Fourthly, given that the 6-year visit had the smallest sample, the power to detect sex differences in polyvictimisation exposure patterns is limited. Lastly, we did not capture racial discrimination, another type of violence children in the DCHS communities may be experiencing given the persistent occurrence of racial discrimination in South Africa ( South African Human Rights Commission, 2021). Future research is needed to investigate the prevalence of this phenomenon in young South African children.
Conclusion
These findings further highlight the high levels of violence exposure in South African children. They indicate that many pre-schoolers in our sample experience a pervasive threat of danger in their homes and communities. Interventions aimed at the community, family and individual levels, are crucial, not only to stop the cycle of violence but to help children deal with this trauma. Interventions aimed at building resilience in children may help them adapt psychologically. Over and above this, systematic factors that likely contribute to this picture such as poverty, socioeconomic inequality, high unemployment rates, low levels of educational attainment and weak police enforcement need to be mitigated to change this picture.
Statements and declarations
1. The current analyses were funded by the Medical Research Council (MRC), grant ref. MR/T002816/1
2. The study was funded by the Bill and Melinda Gates Foundation (OPP 1017641). Additional funding was provided by the SA Medical Research Council, National Research Foundation, Academy of Medical Sciences Newton Advanced Fellowship (NAF002/1001) funded by the UK Government’s Newton Fund, by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) via (R21AA023887, R01 AA026834-01), by a US Brain and Behaviour Foundation Independent Investigator grant (24467),
3. LT was supported by the University of Bristol’s (i) Pro Vice-Chancellor (PVC)-Research and Enterprise Strategic Research Fund and (ii) The Quality-related Research Global Challenges Research Fund (QRGCRF) Strategy funded by Research England.
Patient consent
Parental/guardian consent was obtained.
Ethics approval
The study protocol including consent forms was approved by the Faculty of Health Sciences Research Ethics Committee, University of Cape Town (401/2009), and by the Western Cape Provincial Research committee (2011RP45).
Acknowledgements
We would like to thank the study staff in Paarl, the study data team and lab teams, the clinical and administrative staff of the Western Cape Government Health Department at Paarl Hospital and the clinics for support of the study. We would like to thank the families and children who participated in this study
This study requires multidisciplinary expertise in the execution of measures of this type. DJ is the PI of the psychosocial aspects of the Drakenstein Child Health Study (DCHS) cohort and contributed to the design and decision-making involving psychosocial tools and measures used as well as general study design. HJZ is the PI of the umbrella DCHS cohort and played a central role in the operational aspects and design of the study. KAD, PI of the child psychosocial aspects of the study, was involved in the design of the study and operational aspects of the study and played a key role in the child psychosocial measures used. SM-S contributed to decision-making involving tools used, training and operational aspects of the child assessments. NH contributed to the operational aspects of the study, QC of data described and data management. MR contributed to data management and analysis. JH contributed to data analysis. LT contributed to the writing of the original draft and preparation, data analyses and interpretations. KAD, AF and SH supervised LT. Authors contributed to sections relating to their area of expertise in the manuscript. All authors reviewed and approved the final version of this manuscript.
Funding Statement
The study was funded by the Bill and Melinda Gates Foundation (OPP 1017641). Additional funding was provided by the SA Medical Research Council, National Research Foundation, Academy of Medical Sciences Newton Advanced Fellowship (NAF002/1001) funded by the UK Government’s Newton Fund, by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) via (R21AA023887, R01 AA026834-01), by a US Brain and Behaviour Foundation Independent Investigator grant (24467), LT was supported by the University of Bristol’s (i) Pro Vice-Chancellor (PVC)-Research and Enterprise Strategic Research Fund and (ii) The Quality-related Research Global Challenges Research Fund (QRGCRF) Strategy funded by Research England.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; peer review: 2 approved]
Footnotes
1 The terms, Black African and mixed ancestry are not used here to reify them, but to contribute to the literature on ongoing socioeconomic disparities.
Data availability statement
Data are not publicly available. Collaborations for the analysis of data are welcome; the parent study has a large and active group of investigators and postgraduate students and many have successfully partnered with students or researchers from other institutions. Researchers who are interested in collaborations can find more information on our website [ http://www.paediatrics.uct.ac.za/scah/dclhs].
Author’s information
LT is a Cotutelle PhD candidate at the University of Bristol and the University of Cape Town.
Supplementary
Supplementary Table 1. Prevalence of Violence Exposure in Subsample.
| 3.5 years | 4.5 years | 6. years | |
|---|---|---|---|
| N = 203 | |||
| Subscales | |||
| Overall Violence Exposure | 153 (75.4%) | 148 (72.9%) | 146 (71.9%) |
| Witnessing Community violence | 132 (65.0%) | 136 (67.0%) | 134 (66.0%) |
| Community victimisation | 12 (5.9%) | 16 (7.9%) | 26 (12.8%) |
| Witnessing Domestic Violence | 56 (27.6%) | 46 (22.7%) | 36 (17.7%) |
| Domestic Victimisation | 49 (24.1%) | 45 (22.2%) | 59 (29.1%) |
Values indicate proportions of those with reports of violence exposure only
References
- Appleyard K, Egeland B, van Dulmen MHM, et al. : When more is not better: The role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46(3):235–245. 10.1111/j.1469-7610.2004.00351.x [DOI] [PubMed] [Google Scholar]
- Asagba RB, Noibi OW, Ogueji IA: Gender Differences in Children’s Exposure to Domestic Violence in Nigeria. J Child Adolesc Trauma. 2021;15(2):423–426. 10.1007/s40653-021-00386-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atwoli L, Stein DJ, Williams DR, et al. : Trauma and posttraumatic stress disorder in South Africa: analysis from the South African Stress and Health Study. BMC Psychiatry. 2013;13(1):182. 10.1186/1471-244X-13-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett W, Halligan S, Heron J, et al. : Maltreatment in childhood and intimate partner violence: A latent class growth analysis in a South African pregnancy cohort. Child Abuse Negl. 2018;86(3):336–348. 10.1016/j.chiabu.2018.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce D: Dictating the local balance of power: Election-related violence in South Africa. SA Crime Quarterly. 2009;2009(28):3–9. Reference Source [Google Scholar]
- Bruce D, Dissel A, Menziwa M: The violent nature of crime in South Africa: a concept paper for the Justice, Crime Prevention and Security Cluster. Braam-fontein: Centre for the Study of Violence and Reconciliation (CSVR). 2007. Reference Source [Google Scholar]
- Bruwer B, Emsley R, Kidd M, et al. : Psychometric properties of the Multidimensional Scale of Perceived Social Support in youth. Compr Psychiatry. 2008;49(2):195–201. 10.1016/j.comppsych.2007.09.002 [DOI] [PubMed] [Google Scholar]
- Coen S, Banister E: What a difference sex and gender make: a gender, sex and health research casebook. 2012. Reference Source
- Cowell RA, Cicchetti D, Rogosch FA, et al. : Childhood maltreatment and its effect on neurocognitive functioning: Timing and chronicity matter. Dev Psychopathol. 2015;27(2):521–533. 10.1017/S0954579415000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawes A, de Sas Kropiwnicki Z, Kafaar Z, et al. : Survey examines South Africa’s attitude towards corporal punishment. Article. 2005;19(1):1–3. [Google Scholar]
- De Bellis MD, Woolley DP, Hooper SR: Neuropsychological Findings in Pediatric Maltreatment: Relationship of PTSD, Dissociative Symptoms, and Abuse/Neglect Indices to Neurocognitive Outcomes. Child Maltreat. 2013;18(3):171–183. 10.1177/1077559513497420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donald KA, Hoogenhout M, du Plooy CP, et al. : Drakenstein Child Health Study (DCHS): investigating determinants of early child development and cognition. BMJ Paediatr Open. 2018;2(1): e000282. 10.1136/bmjpo-2018-000282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Neumann A, et al. : Time-Dependent Effects of Exposure to Physical and Sexual Violence on Psychopathology Symptoms in Late Childhood: In Search of Sensitive Periods in Development. J Am Acad Child Adolesc Psychiatry. 2020;59(2):283–295. e4. 10.1016/j.jaac.2019.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falconer NS, Casale M, Kuo C, et al. : Factors That Protect Children From Community Violence: Applying the INSPIRE Model to a Sample of South African Children. J Interpers Violence. 2021;36(23–24):11602–11629. 10.1177/0886260519898425 [DOI] [PubMed] [Google Scholar]
- Fang X, Zheng X, Fry DA, et al. : The economic burden of violence against children in South Africa. Int J Environ Res Public Health. 2017;14(11):1431. 10.3390/ijerph14111431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fincham DS, Altes LK, Stein DJ, et al. : Posttraumatic stress disorder symptoms in adolescents: Risk factors versus resilience moderation. Compr Psychiatry. 2009;50(3):193–199. 10.1016/j.comppsych.2008.09.001 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, et al. : Prevalence of Childhood Exposure to Violence, Crime, and Abuse: Results From the National Survey of Children's Exposure to Violence. JAMA Pediatr. 2015;169(8):746–754. 10.1001/jamapediatrics.2015.0676 [DOI] [PubMed] [Google Scholar]
- Ford JD: Polyvictimization and developmental trauma in childhood. Eur J Psychotraumatol. 2021;12(sup1):1866394. 10.1080/20008198.2020.1866394 [DOI] [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, et al. : Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol. 2009a;21(1):227–259. 10.1017/S0954579409000145 [DOI] [PubMed] [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, et al. : Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev Psychopathol. 2009b;21(1):227–259. 10.1017/S0954579409000145 [DOI] [PubMed] [Google Scholar]
- Grasso DJ, Dierkhising CB, Branson CE, et al. : Developmental patterns of adverse childhood experiences and current symptoms and impairment in youth referred for trauma-specific services. J Abnorm Child Psychol. 2016;44(5):871–886. 10.1007/s10802-015-0086-8 [DOI] [PubMed] [Google Scholar]
- Groves AK, Moodley D, McNaughton-Reyes L, et al. : Prevalence, rates and correlates of intimate partner violence among South African women during pregnancy and the postpartum period. Matern Child Health J. 2015;19(3):487–495. 10.1007/s10995-014-1528-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haahr-Pedersen I, Ershadi AE, Hyland P, et al. : Polyvictimization and psychopathology among children and adolescents: A systematic review of studies using the Juvenile Victimization Questionnaire. Child Abuse Negl. 2020a;107:104589. 10.1016/j.chiabu.2020.104589 [DOI] [PubMed] [Google Scholar]
- Haahr-Pedersen I, Ershadi AE, Hyland P, et al. : Polyvictimization and psychopathology among children and adolescents: A systematic review of studies using the Juvenile Victimization Questionnaire. Child Abuse Negl. 2020b;107:104589. 10.1016/j.chiabu.2020.104589 [DOI] [PubMed] [Google Scholar]
- Haahr-Pedersen I, Ershadi A, Hyland P, et al. : Polyvictimization and psychopathology among children and adolescents: A systematic review of studies using the Juvenile Victimization Questionnaire.In: Child Abuse and Neglect. Elsevier Ltd; 2020c;107(1): 104589. 10.1016/j.chiabu.2020.104589 [DOI] [PubMed] [Google Scholar]
- Haahr-Pedersen I, Ershadi A, Hyland P, et al. : Polyvictimization and psychopathology among children and adolescents: A systematic review of studies using the Juvenile Victimization Questionnaire. Child Abuse and Neglect. Elsevier Ltd; 2020c;107(1): 104589. 10.1016/j.chiabu.2020.104589 [DOI] [PubMed] [Google Scholar]
- Hertzman C, Boyce T: How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health. 2010;31:329–347. 10.1146/annurev.publhealth.012809.103538 [DOI] [PubMed] [Google Scholar]
- Hillis S, Mercy J, Amobi A, et al. : Global Prevalence of Past-year Violence Against Children: A Systematic Review and Minimum Estimates. Pediatrics. 2016;137(3): e20154079. 10.1542/peds.2015-4079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinsberger M, Sommer J, Kaminer D, et al. : Perpetuating the cycle of violence in South African low-income communities: attraction to violence in young men exposed to continuous threat. Eur J Psychotraumatol. 2016;7(1): 29099. 10.3402/ejpt.v7.29099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer D, du Plessis B, Hardy A, et al. : Exposure to violence across multiple sites among young South African adolescents. Peace and Conflict. 2013a;19(2):112–124. 10.1037/a0032487 [DOI] [Google Scholar]
- Kaminer D, du Plessis B, Hardy A, et al. : Exposure to violence across multiple sites among young South African adolescents. Peace and Conflict: Journal of Peace Psychology. 2013b;19(2):112. 10.1037/a0032487 [DOI] [Google Scholar]
- Kaminer D, du Plessis B, Hardy A, et al. : Exposure to violence across multiple sites among young South African adolescents. Peace and Conflict: Journal of Peace Psychology, 2013c;19(2):112. 10.1037/a0032487 [DOI] [Google Scholar]
- Kaminer D, Hardy A, Heath K, et al. : Gender patterns in the contribution of different types of violence to posttraumatic stress symptoms among South African urban youth. Child Abuse Negl. 2013d;37(5):320–330. 10.1016/j.chiabu.2012.12.011 [DOI] [PubMed] [Google Scholar]
- Kaminer D, Hardy A, Heath K, et al. : Gender patterns in the contribution of different types of violence to posttraumatic stress symptoms among South African urban youth. Child Abuse Negl. 2013e;37(5):320–330. 10.1016/j.chiabu.2012.12.011 [DOI] [PubMed] [Google Scholar]
- Krug EG, Mercy JA, Dahlberg LL, et al. : The world report on violence and health. Lancet. 2002;360(9339):1083–1088. 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- Le MTH, Holton S, Romero L, et al. : Polyvictimization among children and adolescents in low- and lower-middle-income countries: A systematic review and meta-analysis. Trauma Violence Abuse. 2018;19(3):323–342. 10.1177/1524838016659489 [DOI] [PubMed] [Google Scholar]
- Leoschut L, Kafaar Z: The frequency and predictors of poly-victimisation of South African children and the role of schools in its prevention. Psychol Health Med. 2017;22(sup1):81–93. 10.1080/13548506.2016.1273533 [DOI] [PubMed] [Google Scholar]
- Lokot M, Bhatia A, Kenny L, et al. : Corporal punishment, discipline and social norms: A systematic review in low- and middle-income countries. Aggress Violent Beh. 2020;55: 101507. 10.1016/j.avb.2020.101507 [DOI] [Google Scholar]
- Maguire SA, Williams B, Naughton AM, et al. : A systematic review of the emotional, behavioural and cognitive features exhibited by school-aged children experiencing neglect or emotional abuse. Child Care Health Dev. 2015;41(5):641–653. 10.1111/cch.12227 [DOI] [PubMed] [Google Scholar]
- Mathews S, Abrahams N, Jewkes R, et al. : The epidemiology of child homicides in South Africa. Bull World Health Organ. 2013;91(8):562–568. 10.2471/BLT.12.117036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews S, Benvenuti P, Africa S: Violence against children in South Africa: Developing a prevention agenda. South African Child Gauge. 2014;1(2):26–34. Reference Source [Google Scholar]
- Myer L, Stein DJ, Grimsrud A, et al. : Social determinants of psychological distress in a nationally-representative sample of South African adults. Soc Sci Med. 2008;66(8):1828–1840. 10.1016/j.socscimed.2008.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, et al. : The Long-Term Health Consequences of Child Physical Abuse, Emotional Abuse, and Neglect: A Systematic Review and Meta-Analysis. PLoS Med. 2012;9(11): e1001349. 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat M, van Niekerk A, Jewkes R, et al. : Violence and injuries in South Africa: prioritising an agenda for prevention. Lancet. 2009;374(9694):1011–1022. 10.1016/S0140-6736(09)60948-X [DOI] [PubMed] [Google Scholar]
- Shahinfar A, Fox NA, Leavitt LA: Preschool children’s exposure to violence: Relation of behavior problems to parent and child reports. Am J Orthopsychiatry. 2000;70(1):115–125. 10.1037/h0087690 [DOI] [PubMed] [Google Scholar]
- Shields N, Nadasen K, Pierce L: The effects of community violence on children in Cape Town, South Africa. Child Abuse Negl. 2008;32(5):589–601. 10.1016/j.chiabu.2007.07.010 [DOI] [PubMed] [Google Scholar]
- Smit J, van den Berg CE, Bekker LG, et al. : Translation and cross-cultural adaptation of a mental health battery in an African setting. Afr Health Sci. 2006;6(4):215–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South African Human Rights Commission: Trend analysis report 2020/ 2021.2021. Reference Source [Google Scholar]
- South African Police Service: Crime statistics of Republic of South Africa. 2021. [Google Scholar]
- Stansfeld SA, Rothon C, Das-Munshi J, et al. : Exposure to violence and mental health of adolescents: South African Health and Well-being Study. BJPsych Open. 2017;3(5):257–264. 10.1192/bjpo.bp.117.004861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein DJ, Koen N, Donald KA, et al. : Investigating the psychosocial determinants of child health in Africa: The Drakenstein Child Health Study. J Neurosci Methods. 2015;252:27–35. 10.1016/j.jneumeth.2015.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternberg KJ, Baradaran LP, Abbott CB, et al. : Type of violence, age, and gender differences in the effects of family violence on children’s behavior problems: A mega-analysis. Dev Rev. 2006;26(1):89–112. 10.1016/j.dr.2005.12.001 [DOI] [Google Scholar]
- Teicher MH, Tomoda A, Andersen SL: Neurobiological consequences of early stress and childhood maltreatment: are results from human and animal studies comparable? Ann N Y Acad Sci. 2006;1071(1):313–323. 10.1196/annals.1364.024 [DOI] [PubMed] [Google Scholar]
- Vu NL, Jouriles EN, McDonald R, et al. : Children’s exposure to intimate partner violence: A meta-analysis of longitudinal associations with child adjustment problems. Clin Psychol Rev. 2016;46:25–33. 10.1016/j.cpr.2016.04.003 [DOI] [PubMed] [Google Scholar]
- Ward CL, Dawes A, Matzopoulos R: Youth violence in South Africa: Setting the scene. Youth Violence. 2013;1. Reference Source [Google Scholar]
- Young-Southward G, Eaton C, O’Connor R, et al. : Investigating the causal relationship between maltreatment and cognition in children: A systematic review. Child Abuse Negl. 2020;107: 104603. 10.1016/j.chiabu.2020.104603 [DOI] [PubMed] [Google Scholar]
- Zar HJ, Barnett W, Myer L, et al. : Investigating the early-life determinants of illness in Africa: the Drakenstein Child Health Study. Thorax. 2015;70(6):592–594. 10.1136/thoraxjnl-2014-206242 [DOI] [PMC free article] [PubMed] [Google Scholar]