Abstract
Background
Community pharmacies have changed during the COVID-19 pandemic, and new routines have been introduced to address the needs of customers and staff and to reduce the risk of spreading infection. Burnout has been described among staff possibly due to a changed working climate. However, little research has focused on the pandemic's effect on patient safety in community pharmacies.
Objective
To examine pharmacists' perceptions of the impact of the COVID-19 pandemic on workload, working environment, and patient safety in community pharmacies.
Methods
A survey was distributed to all Swedish community pharmacists, constituting a census study. Questions regarding the pharmacists' perception of the impact of the pandemic on workload, working environment, and patient safety were included. Respondents were asked to provide comments on their working situation. Quantitative results were analysed using descriptive statistics, and comments were analysed using qualitative content analysis.
Results
The response rate was 41% (2034 responses). Most pharmacists (62%) considered the workload to be increased during the pandemic while work environment deteriorated (physical work environment was considered worse by 47% of respondents while psychosocial work environment was considered worse by 59%). Despite this, many respondents (55%) believed that patient safety was not affected. Neither having had COVID-19 nor being afraid of contracting it, influenced these perceptions in any substantial way. Findings were consistent regardless of education, professional role, number of years in community pharmacies, or special assignments in the pharmacies. According to the respondents, the communication within pharmacy companies during the pandemic was inadequate.
Conclusions
The impact of the pandemic on working conditions is in line with previous findings but the effect on patient safety needs further studies. The respondents felt the management had a limited understanding of the conditions during the pandemic, which stresses the importance of good and clear communication during a crisis.
Keywords: COVID-19, Community pharmacy, Workload, Work environment, Patient safety
Highlights
-
•
This was a national census study, encompassing all community pharmacists
-
•
Workload increased and working conditions deteriorated during the COVID-19 pandemic
-
•
Patient safety was not perceived to be affected in community pharmacies
-
•
Pharmacists felt lack of understanding from management regarding working conditions
1. Introduction
The workload in the healthcare sector during the COVID-19 pandemic has increased.1, 2, 3, 4 The pandemic's impact on the physical working environment has been significant, and the need for new ways of working with more extensive protective measures and equipment has escalated. However, in addition to this increased workload and changes to the working environment, there is a risk of exposure to infected patients because the protection of the staff in the health care sector has been suboptimal.5,6 Consequently, the psychosocial work environment has also been affected by the pandemic, resulting in anxiety, distress, and depression.1,4,6
Although the situation in pharmacies in many ways is not comparable to the conditions in healthcare, the pharmacies were still influenced by the pandemic. The community pharmacies played an important role in the COVID-19 pandemic as an easily accessible health care provider to the public.7, 8., 9 In response to public health needs during the pandemic, new pharmacy tasks and assignments have been introduced over a short time span.9, 10, 11 These have included patient education and information about the pandemic in addition to physical changes such as changes in stock supplies of essential medicines and products of particular interest during the pandemic such as hand sanitizers.10 New logistical procedures, such as home delivery of medicines, have been introduced.12
The consequences of these new tasks and assignments for pharmacists have been shown to for example involve increased workloads and overtime,13 and higher burnout rates.14 It has been demonstrated that community pharmacists displayed a higher degree of burnout than pharmacists in hospitals with a more business-as-usual approach.15 Drug shortages and inappropriate behaviour by customers have also added to problems of burnout.13
In Canada, 85% of community pharmacy professionals reported that their mental health had suffered during the pandemic.16 As many general practitioners' offices were closed, the pressure on pharmacists increased, which could increase the risk of problems with patient safety, according to a study from Ireland.9
The WHO has, in brief, described patient safety as delivering effective, safe, and people-centred health services.17 In a qualitative study in England and Scotland about the response and adaption among community pharmacist to maintain patient safety during the first year of the pandemic, the dedication of the staff was found to be the main explanation for the claim that patient safety was not compromised.18 Managing the initially intense workload was prioritised, and services not recognised as crucial to patient safety such as retail work were reduced according to the study.
Patient safety has also been described by the WHO as the absence of unnecessary errors.19 In community pharmacies most unsafe acts are dispensing errors, defined as “a discrepancy between a prescription and the medicine that the pharmacy delivers to the patient”.20
The association between dispensing errors in pharmacies and various parameters have been studied prior to the pandemic.21,22 In the UK a high workload has been linked to an increase in the numbers of self-reported dispensing errors,23 and Finnish and American pharmacists have reported high workload as an important contributor to dispensing errors.24,25
The association between patient safety and workload is unclear. According to a review, patient safety is not affected by high workload and pharmacists' poor well-being.26 On the other hand, a study among health care staff showed an association between poor well-being and burnout in staff and negative patient safety outcomes.27
One of the hidden factors affecting patient safety in community pharmacies was limited possibilities to anticipate the workload.28 Another factor was community pharmacies being for-profit organisations leading to less transparency regarding policies and internal business practices.28 In accordance with this, research conducted after de the de-regulation of the state-owned monopoly of pharmacies in Sweden indicated that staff had experienced a negative trend regarding the patient safety climate in community pharmacies.29,30
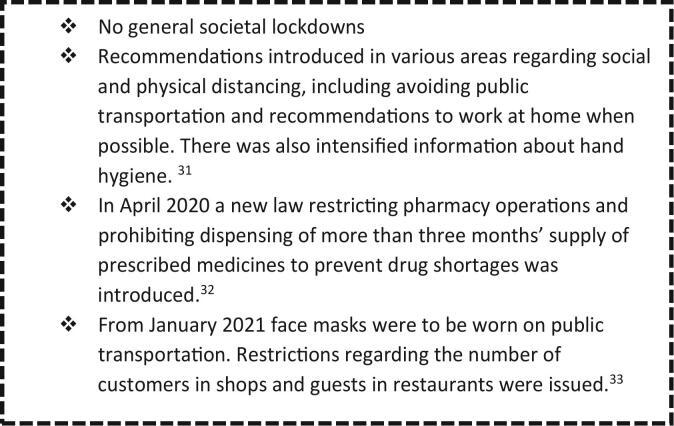
The pandemic forced society to implement several major changes. Sweden in some ways handled the pandemic differently than many other countries (Fig. 1), impacting both healthcare in general and pharmacies. The main difference between Sweden and other countries was the absence of a general lockdown. However, during the latter part of the pandemic the similarities with the restrictions imposed by other countries increased.
Fig. 1.
Swedish recommendations during the pandemic (31., 32., 33.).
As the COVID-19 pandemic has gradually loosened its grip, it has been possible to summarise experiences and to identify lessons learned. Countries have dealt with the pandemic in various ways, resulting in different challenges. The impact of a global crisis such as this pandemic on workloads, working environments, and patient safety in pharmacies needs to be studied further to prepare for future pandemics.
2. Aim
The aim of this work was to examine pharmacists' perceptions of working during the COVID-19 pandemic and the impact of the COVID-19 pandemic on the workload, working environment, and patient safety in community pharmacies.
3. Methods
3.1. Setting and design
The study was carried out among Swedish community pharmacists. The design was a cross-sectional, one-point-in-time survey. This was also a census study as all pharmacists working in community pharmacies in Sweden were invited to participate in the study and no sampling was performed.
3.2. Respondents
All pharmacists in Sweden are registered in the Swedish Occupational Register managed by Statistics Sweden.34 The Swedish Occupational Register has a two-year delay in recording data. As a result, the data used in this study were derived from pharmacists included in the register in 2019 and pharmacists included after 2019 could thus not be identified at the time of the study. Pharmaceutical educations in Sweden include pharmacists with a 5-year university education and prescriptionists with a 3-year university education, and thus a distinction regarding education was made. Both educations, however, have medication dispensing certifications corresponding to that of an international pharmacist degree. There are no substantial differences between pharmacists and prescriptionists regarding the work these professions carry out in Swedish community pharmacies, but the length of training may have an impact on the handling of the pandemic and its consequences. However, the term pharmacist is used throughout this paper and includes both pharmacists and prescriptionists if not otherwise specified.
The inclusion criteria for this study were being a licensed pharmacist and working in a community pharmacy. Pharmacists working in online pharmacies were excluded.
The register included 5364 presumptive respondents. Out of these, 83 were found to be deceased, emigrated, or for other reasons not eligible for the survey (N = 5281). The design of the register made it necessary to incorporate pharmacists, prescriptionists, and pharmacy managers in the presumptive respondent group in order to reach all pharmacists. According to the register holder, pharmacists and prescriptionists can appear in any of these three groups but pharmacy managers could also hold other professions, thus selection questions were needed.
All 5281 possible respondents received the survey. To ensure they fulfilled the inclusion criteria, selection questions were used, namely “Are you a licensed pharmacist?” and “Do you work in a pharmacy?”. Only licensed pharmacists are allowed to work as pharmacists in a pharmacy. Also, only those working in pharmacies at the time of the study were eligible. They were asked to specify which kind of pharmacy they worked in, as only pharmacists in pharmacies where staff meet customers face to face were included.
3.3. Ethical considerations
Ethical consent for the survey was given by the Swedish Ethical Review Authority in August 2021. Statistics Sweden process personal data in accordance with applicable data protection legislation, and thus no ethical principles were compromised.35
3.4. The questionnaire
The survey consisted of a new set of questions, designed by the research group, and included the pharmacists' perception of the impact of the pandemic on the workload, working environment, and patient safety in community pharmacies.
The pilot testing of the questionnaire was done by discussing the questions with a group of pharmacists in academia with some experience as pharmacists in community pharmacies and extensive knowledge in making questionnaires. This resulted in minor revisions prior to the dissemination of the questionnaire.
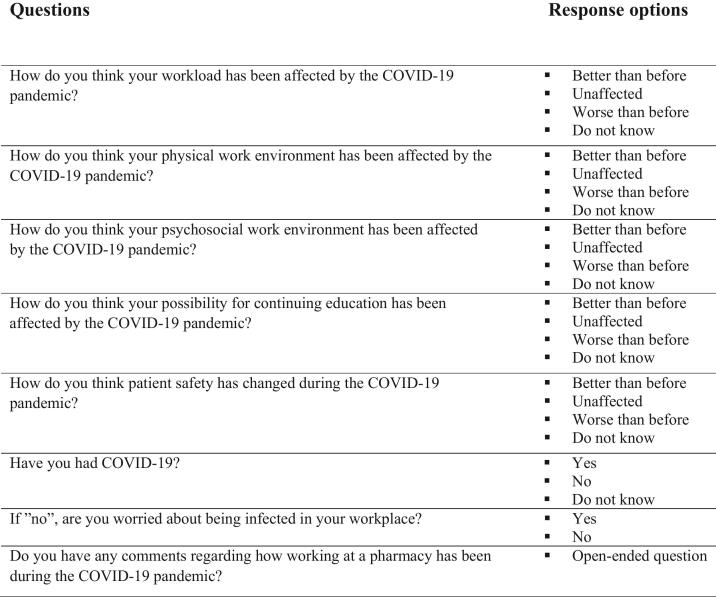
The respondents were also asked to comment on their perception of the working situation in community pharmacies during the COVID-19 pandemic in order to provide a broader understanding of this phenomenon. The questionnaire was in Swedish, but an English translation of the questions was made for publication purposes, as shown in Fig. 2.
Fig. 2.
Questions regarding pharmacists' perception of the impact of the COVID-19 pandemic on work environment, workload, and patient safety.
Questions on respondent characteristics were included, such as education (pharmacists vs. prescriptionists), one's role in the pharmacy (i.e., manager, pharmacist with quality responsibilities, or pharmacist without special responsibilities), and the number of years working in community pharmacies.
3.5. Survey methodology
All possible respondents were approached by Statistics Sweden and sent an invitation letter describing the study and study rationale. The letter also included login details to the web survey. The invitation was sent to their digital public authority mail, and for those who did not have such a digital mailbox the invitation letter was sent by mail to their home address. Many of Sweden's public authorities and municipalities use a personal digital mailbox for communication. Approximately 75% had a digital mailbox. Three reminders were sent to the participants who had not replied. The first and third reminders were digital or postal (i.e., via the same route as the invitation letter was originally sent to the participant). The second reminder was sent by post to all participants. Data was collected between November 2021 and February 2022 i.e. 13 weeks.
Statistics Sweden conducted the web survey on behalf of the research group and was also responsible för compiling the results. To ensure anonymity, Statistics Sweden removed all names of staff, pharmacies, or pharmacy companies appearing in the results prior to handing over the results to the research group. Three months after the end of the survey, all identification keys were deleted by Statistics Sweden.
3.6. Data analysis
The data were analysed with mixed methods approach. Because the qualitative and quantitative data were collected simultaneously, this can be described as a concurrent mixed method design.36
The quantitative results were analysed with SPSS Version 29.0 (SPSS, Inc., Chicago, IL). Descriptive statistics were deemed appropriate because this was a census study37 and the entire population of pharmacists working in Swedish community pharmacies in 2019 was included and no sampling was performed. Because the results are not generalized beyond the target population of this census, statistical inference is not applicable.38
The qualitative results (i.e. the comments regarding perception of the working situation in community pharmacies during the pandemic) were analysed using qualitative manifest content analysis.39,40
The comments were first read and re-read by all co-authors to gain a general understanding. Meaning units and key phrases were then identified and subsequently coded using NVivo software (Version 12 Plus, QSR International Pty Ltd. 2019). The coded data were merged into mutually exclusive categories labelled with short descriptions of their contents. The categories were interpreted and sorted using the framework as provided in the questionnaire, namely Workload, Physical work environment, Psychosocial work environment, Continuing education, and Patient safety. This was inspired by framework analysis.41 The analysis was carried out by two of the researchers (CLP and BS), and disagreements in the analysis were discussed until consensus was reached.
The comments were given in Swedish and thus the quotes were translated into English only for publication purposes. Quotes included in this paper were selected to illustrate the contents of each theme.
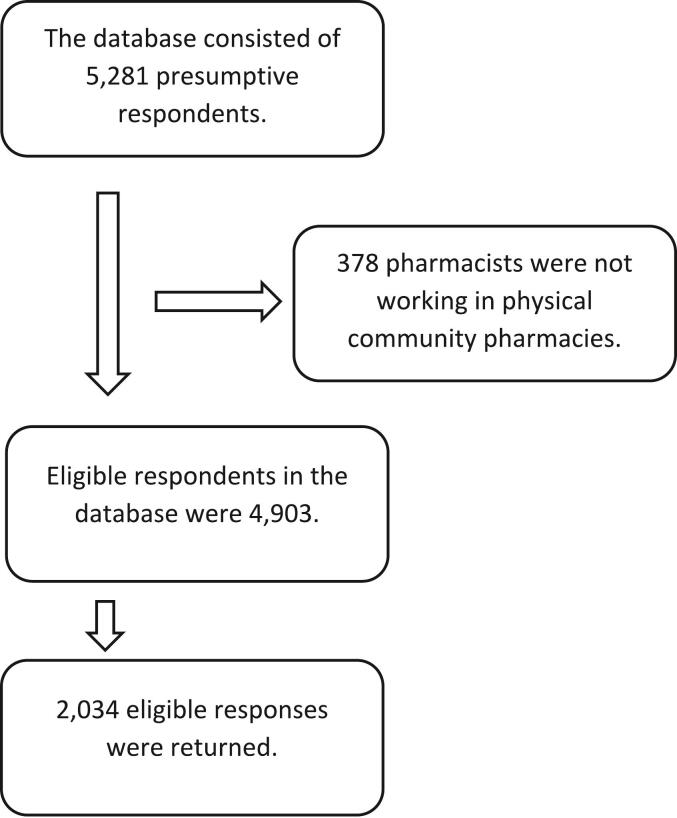
4. Results
Out of the 5281 presumptive respondents who received the survey, 4903 were eligible for inclusion in this study (Fig. 3). A total of 2034 surveys that met the inclusion criteria were returned, thus giving a response rate of 41%.
Fig. 3.
Eligible respondents.
The characteristics of the respondents are presented in Table 1.
Table 1.
Details of the respondents; N = 2034.
| Respondents % | |||
|---|---|---|---|
| Education | |||
| Pharmacist | 30 | (n = 608) | |
| Prescriptionist | 66 | (n = 1341) | |
| Other | 4 | (n = 83) | |
| Missing | 0 | (n = 2) | |
| Professional role | |||
| Pharmacy manager | 6 | (n = 131) | |
| Pharmacist responsible for quality | 21 | (n = 436) | |
| Pharmacist without special responsibilities | 70 | (n = 1415) | |
| Other | 3 | (n = 52) | |
| Missing | 0 | (n = 0) | |
| Time in pharmacy | |||
| Fewer than 4 years | 9 | (n = 189) | |
| More than 4 years | 91 | (n = 1843) | |
| Missing | 0 | (n = 2) | |
| Been infected with COVID-19 | |||
| Yes | 26 | (n = 525) | |
| No | 64 | (n = 1297) | |
| Do not know | 10 | (n = 207) | |
| Missing | 0 | (n = 5) | |
| Fear of contracting COVID-19 | |||
| Yes | 49 | (n = 1002) | |
| No | 50 | (n = 1022) | |
| Missing | 1 | (n = 10) | |
In the total population, 86% were women, as compared to 89% of the respondents. Because most of the respondents were female (89%), potential gender differences were not analysed.
When comparing ages distribution, 37% were 20–39 years in the total population versus 31% of the respondents; 45% were 40–59 years in the total population versus 48% of the respondents, and 18% were 60 years and older in the total population versus 21% of the respondents.
In the total population of pharmacists, prescriptionists, and pharmacy managers, 27% were registered as having a pharmacist education, 56% as having a prescriptionist education, and 17% as having other education. “Other” includes pharmacists with further education, i.e. prescriptionists with a master's degree or pharmacists with a PhD but who work in the pharmacy as either licensed pharmacists or prescriptionists. Further education is more common for prescriptionists, therefore the number of prescriptionists is underestimated in the total population because part of them are included in “other” education. A small number of respondents chose the option “other” education and indicated a higher education such as PhD but did not submit information about their license. Regarding professional role, those choosing the option “other” conveyed more detailed information than the fixed answer options allowed for. This proportion was also small.
The results of the questionnaire are presented below along with the results of the subgroup analyses (i.e., education, professional role in the pharmacy, number of years in community pharmacy, having been infected by COVID-19, and being afraid of being infected by COVID-19).
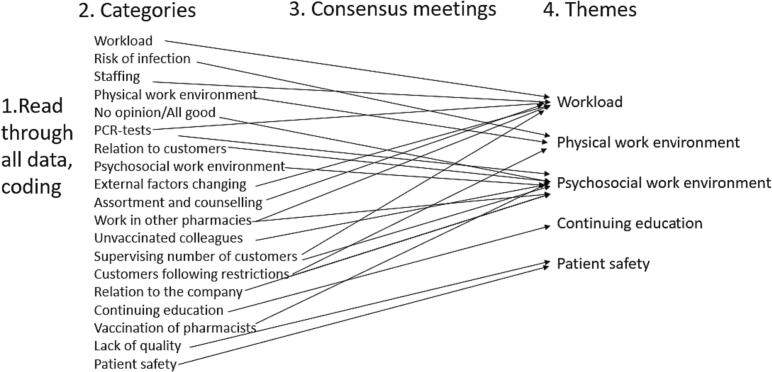
All 880 comments were analysed. The final version of the qualitative analysis had 19 categories (see Fig. 4) that could be merged into the five themes of the questionnaire.
Fig. 4.
The qualitative analysis process.
The results of the qualitative analysis are reported after each quantitative result under the themes Workload, Physical work environment, Psychosocial work environment, Continuing education, and Patient safety to provide a joint display.36
4.1. Workload
Most of the respondents (62%) felt that the workload had increased (become worse) as compared to before the pandemic, while 9% felt that it had decreased (become better), 22% considered the workload unaffected.
The analysis of the possible influence of education, professional role, and having been infected by COVID-19 on the perception of workload during the pandemic showed no major differences compared to the overall results (Table 2).
Table 2.
Perceived impact of the COVID-19 pandemic on the workload analysed per subgroup (N = 2021).
| Better % | Unaffected % | Worse % | Do not know % | Total % | |||
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Pharmacist | 9 | 19 | 66 | 6 | 100 | (n = 605) | |
| Prescriptionist | 10 | 24 | 59 | 8 | 100 | (n = 1332) | |
| Other | 6 | 19 | 69 | 6 | 100 | (n = 83) | |
| Professional role | |||||||
| Pharmacy manager | 11 | 18 | 68 | 4 | 100 | (n = 130) | |
| Pharmacist responsible for quality | 8 | 24 | 62 | 6 | 100 | (n = 432) | |
| Pharmacist without special responsibilities | 9 | 21 | 61 | 8 | 100 | (n = 1407) | |
| Other | 8 | 33 | 48 | 12 | 100 | (n = 52) | |
| Time in community pharmacy | |||||||
| Fewer than 4 years | 6 | 18 | 72 | 4 | 100 | (n = 188) | |
| More than 4 years | 9 | 22 | 61 | 8 | 100 | (n = 1829) | |
| Been infected with COVID-19 | |||||||
| Yes | 8 | 16 | 69 | 7 | 100 | (n = 522) | |
| No | 9 | 25 | 59 | 7 | 100 | (n = 1290) | |
| Do not know | 11 | 18 | 62 | 9 | 100 | (n = 207) | |
| Fear of contracting COVID-19 | |||||||
| Yes | 7 | 15 | 72 | 6 | 100 | (n = 996) | |
| No | 11 | 29 | 51 | 8 | 100 | (n = 1017) | |
However, both those respondents having worked fewer than four years in pharmacies as well as those being afraid of contracting COVID-19 were more likely to perceive the workload as increased (72% for both) compared to the overall results. In contrast, those not afraid of being infected were more likely to consider the workload to have decreased (51%).
The qualitative analysis showed that the workload was perceived by the respondents as having changed negatively during the pandemic. The spring of 2020 was described as very hectic because customers wanted to buy face masks, hand sanitizers, and disposable gloves. The customers also stockpiled prescription and over the counter medicines. At the same time, new extra cleaning routines were introduced in the pharmacies. Even though more extensive procedures for cleaning and disinfection were implemented, the respondents thought that these procedures were not always followed. These tasks were to be carried out by the ordinary pharmacy staff, but they did not have time. In parallel, new services such as curb side pick-up and home delivery were introduced quickly, sometimes with insufficient training of staff. Respondents also said that there were no staff substitutes in case of vacation or sick leave. Instead, pharmacists skipped lunch breaks or helped on days off to keep the pharmacies open. Staff were also transferred from one pharmacy to another causing shortages in staff. The customer flow was different during the pandemic compared to what the staff was used to, and the normally busier pharmacies in the city centres had fewer customers, while pharmacies outside the cities experienced an increase as many were working remotely.
During the summer of 2020 the workload increased as the number of people who fell ill decreased and the flow of customers normalised, according to the respondents. However, by then the companies had reduced the staff in some pharmacies, and the number was not increased when the customer flow increased again.
“When the number of customers increased the staff did not and was kept at minimal level. As soon as a pharmacist gets sick or must take care of sick children, this results in a crisis at work and the other pharmacists feel pressured to work overtime for it to be a functioning working day for their colleagues. Recovery becomes more difficult, stress levels are higher, and fewer persons carry out the same work as previously. It is necessary to prioritise the most important/most acute tasks. I know of several assignments that should be done once a month but that might be done once every half year if it is even done then…”.
New regulations, put in place in January 2021, limited the number of customers allowed in public areas such as pharmacies.33 This further increased the workload for the pharmacy staff because the customers had to be constantly counted and some asked to leave if they were too many. Some respondents expressed disappointment with not being assigned extra staff for this task.
In twelve out of Sweden's 21 counties some pharmacies helped the local health care system to distribute free PCR COVID-19 tests, according to personal communication with all counties. This was described as causing a major increase in workload. The complexity of dispensing drugs also increased when the elderly, other people at risk, and people in quarantine sent friends or family to pick up their prescriptions. These representatives did not always have information about the patient's drug therapy, so the dispensing pharmacist would have to take extra care and sometimes had to call the patient before dispensing.
4.2. Physical work environment
Most of the respondents (47%) considered their physical work environment at the time of completing the survey to be worse compared to before the pandemic. Roughly 20% and 21%, respectively, considered the physical work environment to be unaffected or better.
When analysing how education, professional role, number of years working in community pharmacies, and having been infected by COVID-19 have impacted the perception of influence of COVID-19 on the physical working environment, no large differences could be found compared to the overall result (Table 3).
Table 3.
Perceived impact of the COVID-19 pandemic on the physical working environment analysed per subgroup (N = 2029).
| Better % | Unaffected % | Worse % | Do not know % | Total % | |||
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Pharmacist | 17 | 22 | 51 | 10 | 100 | (n = 606) | |
| Prescriptionist | 24 | 19 | 45 | 12 | 100 | (n = 1339) | |
| Other | 18 | 19 | 48 | 14 | 100 | (n = 83) | |
| Professional role | |||||||
| Pharmacy manager | 25 | 19 | 46 | 10 | 100 | (n = 131) | |
| Pharmacist responsible for quality | 20 | 23 | 48 | 9 | 100 | (n = 436) | |
| Pharmacist without special responsibilities | 21 | 19 | 47 | 12 | 100 | (n = 1408) | |
| Other | 21 | 15 | 48 | 15 | 100 | (n = 52) | |
| Time in pharmacy | |||||||
| Fewer than 4 years | 17 | 19 | 52 | 11 | 100 | (n = 187) | |
| More than 4 years | 22 | 20 | 47 | 12 | 100 | (n = 1838) | |
| Been infected with COVID-19 | |||||||
| Yes | 18 | 16 | 53 | 13 | 100 | (n = 524) | |
| No | 23 | 22 | 44 | 11 | 100 | (n = 1296) | |
| Do not know | 18 | 17 | 54 | 11 | 100 | (n = 207) | |
| Fear of contracting COVID-19 | |||||||
| Yes | 17 | 13 | 59 | 11 | 100 | (n = 999) | |
| No | 25 | 26 | 36 | 12 | 100 | (n = 1022) | |
Of the respondents who were afraid of getting COVID-19, a larger proportion (59%) considered the physical environment to have been impaired during the pandemic as compared to the overall result of 47%. Also, those not afraid of becoming infected deviated from the overall results, and only 36% considered the working environment to be worse.
According to the qualitative part of the survey, the employers had not introduced sufficient safety measures, and this might have influenced the respondents' perceptions of their physical working environment.
In the beginning of the pandemic the pharmacy staff was advised not to use masks or face shields because it was believed by the employer to scare customers, and some respondents said that facemasks were forbidden altogether and some reported that it took a long time before plexiglass barriers were installed in some pharmacies. When in place, many respondents appreciated the barriers because they were believed to protect not only against COVID-19, but also against other viruses. Some even hoped the barriers would remain after the pandemic had ended. The barriers were, however, not appreciated by all:
“Relatively quickly we got plexiglass barriers at the counters …. Which certainly contributed to some sense of safety, but at the same time an unfamiliar distance was created to the customers with whom we usually have a close relationship, in addition to problems with hearing, both for customers and staff (masks were sometimes used and contributed further to hearing problems). …. The workplace was getting ‘colder’, but of course it was necessary.”
Physical barriers were obviously needed because the pharmacists described customers with symptoms of COVID-19 visiting the pharmacy, probably considering it easier accessible than other health care:
” When people with cough/common cold are not allowed to enter the usual health care facilities due to their symptoms, they came to the pharmacy instead to ask for advice or information regarding where to turn to get tested. Infected persons have come in person to buy their cough medicines and COVID tests.”
4.3. Psychosocial work environment
The psychosocial work environment was considered worse than prior to the pandemic by 59% of the respondents, while 28% believed the environment to be unaffected and only 3% found it improved.
The general opinion regarding the psychosocial working environment was not impacted by the respondents' level of education, professional role, number of years working in pharmacies, or having been infected by COVID-19 (Table 4).
Table 4.
Perceived impact of the COVID-19 pandemic on psychosocial working environment analysed per subgroup (N = 2014).
| Better % | Unaffected % | Worse % | Do not know % | Total % | |||
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Pharmacist | 3 | 27 | 61 | 9 | 100 | (n = 605) | |
| Prescriptionist | 3 | 29 | 57 | 10 | 100 | (n = 1327) | |
| Other | 1 | 27 | 62 | 10 | 100 | (n = 81) | |
| Professional role | |||||||
| Pharmacy manager | 6 | 33 | 55 | 6 | 100 | (n = 129) | |
| Pharmacist responsible for quality | 3 | 30 | 60 | 8 | 100 | (n = 433) | |
| Pharmacist without special responsibilities | 3 | 28 | 59 | 11 | 100 | (n = 1398) | |
| Other | 4 | 35 | 48 | 13 | 100 | (n = 52) | |
| Time in pharmacy | |||||||
| Fewer than 4 years | 4 | 25 | 62 | 9 | 100 | (n = 188) | |
| More than 4 years | 3 | 29 | 58 | 10 | 100 | (n = 1822) | |
| Been infected with COVID-19 | |||||||
| Yes | 4 | 25 | 61 | 11 | 100 | (n = 520) | |
| No | 3 | 31 | 57 | 9 | 100 | (n = 1286) | |
| Do not know | 3 | 20 | 65 | 11 | 100 | (n = 206) | |
| Fear of contracting COVID-19 | |||||||
| Yes | 2 | 15 | 75 | 8 | 100 | (n = 997) | |
| No | 4 | 42 | 43 | 12 | 100 | (n = 1009) | |
However, this did not apply for the respondents both afraid of and not afraid of contracting COVID-19. A larger proportion (75%) of those afraid stated that the psychosocial work environment was worse than prior to the pandemic compared to 59% among the respondents in total. However, only 43% of those not afraid of contracting COVID-19 found that the psychosocial environment was worse.
The respondents considered the psychosocial working environment to be affected by the pandemic in several ways according to the qualitative results. The previously mentioned increased workload combined with high levels of sick leave among staff in parallel with unpredictable customer flows was considered stressful.
The temporary regulations regarding refills of prescriptions, the new task of reminding people to maintain physical distance in the pharmacy and asking people to wait outside in order not to exceed the allowed number of customers made the respondents feel like police officers. The staff experienced a need not only to interrupt dispensing medications to fulfil these new tasks, and they also felt pressured to work faster to keep down the waiting time for people in line – all described as very stressful. However, others described the pharmacy as calmer because fewer customers were allowed inside.
Some customers felt lonelier during the pandemic than usual and wanted to talk, but the pharmacists had little time to do so.
The respondents also had to deal with customers' annoyance and anger with new rules and increased waiting times. Conflicts with customers arose because some people had a lack of understanding of the restrictions. For example, customers with symptoms got angry when asked to leave the pharmacy while other customers did not keep a physical distance and bypassed the plexiglass barriers. The distribution of PCR tests was considered challenging, and some pharmacists described people with symptoms coming into the pharmacy to pick up tests even though this was not allowed. Some vaccinated customers believed they were immune to COVID-19 and thus could not infect others.
”Lots of displeased customers, and many complained to us about the situation. Like if it was us who had released the virus and decided on all the restrictions. We only did what we have been told. Many customers did not understand the situation.”
One pharmacist describes how the psychosocial interactions among colleagues in the pharmacy changed:
“From being a good pharmacy with a good atmosphere among staff, we have reached the bottom. Everyone is tired and stressed and feeling mentally tired. I am in the middle of resigning because of this. I can't take it anymore.”
Many described how they had collaborated well with their colleagues during the pandemic and emphasised how important the feeling of teamwork had been. However, some respondents expressed a feeling of having been let down by the pharmacy company they worked for. Bonuses and increases in wages for pharmacies with increasing sales were cancelled due to decreased sales in general.
”The most negative aspect has been that the managers have told us that there are unprofitable parts of our company due to COVID and this leads to an extra focus on selling.”
When compared to other health care staff, pharmacy staff had less protective equipment. This together with the pharmacy companies advising against the use of face masks in combination with the perceived delay in introducing protective barriers was sometimes considered as a lack of care for pharmacy staff:
”In the beginning we were told not to use face masks because it could ‘be frightening for the customers’…this is pharmacies in a nut shell, the customers are more important than staff.”
The fear of being infected by co-workers contributed to creating stress asit was sometimes difficult to maintain distance between staff members, for example, in the lunchroom and backspace areas. Unvaccinated co-workers who came to work with symptoms of COVID-19 were described with resentment. At the same time, respondents perceived it as unacceptable to stay at home, even with symptoms, because they knew there was no one to fill in for them at the pharmacy. Staff were often sent between pharmacies to work, sometimes just for a few hours to cover lunch breaks, and there was a worry that this could help spread COVID-19 infections between staff, especially because one would have to travel on public transportation.
” We had staff who were infected in different pharmacies…What made me upset was that pharmacy staff were sent to different pharmacies (other than the pharmacy where they were employed)…just to be able to keep the pharmacies open or to not reduce the opening hours.”
The pharmacists expressed feelings of being let down by society in general. Pharmacy personnel were not prioritised like other health care personnel in the national vaccination programme, even though a large part of the public was seeking help in pharmacies because other parts of the health care were less accessible and were overloaded. Some respondents also considered that the pharmacy companies had not worked for a prioritisation of pharmacy staff regarding vaccinations thus not standing up for their staff. Also, being infected by COVID-19 in the pharmacy was not considered to be an occupational injury from an insurance perspective, as it was for other health care personnel in Sweden:
” Ungrateful. The health care has received all the cred, but we in the pharmacies that meet customers who ‘just tested positive and need help’ do not get any help at all. Not even compensation.”
“We are not considered health care staff, but we meet sick people every day. It was challenging to work like this during the worst periods of the pandemic. We are essential for the customers and for the society, yet still we are counted as nothing. That was how it felt. We are, however, proud of being able to help so many people during the pandemic.”
4.4. Continuing education
The majority (47%) felt that the possibility for continuing education was unaffected, while 37% thought that this possibility had become worse and 2% thought that it had improved.
The impact of COVID-19 on the possibility for continuing education was not perceived to be differently affected at any level (i.e., the level of education, professional role, length of working time in pharmacy, having been infected, or being afraid of getting infected) compared to the total, as shown in Table 5.
Table 5.
Perceived impact of the COVID-19 pandemic on continuing education as analysed per subgroup (N = 2023).
| Better % | Unaffected % | Worse % | Do not know % | Total % | |||
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Pharmacist | 3 | 42 | 40 | 15 | 100 | (n = 604) | |
| Prescriptionist | 2 | 49 | 36 | 13 | 100 | (n = 1335) | |
| Other | 1 | 47 | 37 | 14 | 100 | (n = 83) | |
| Professional role | |||||||
| Pharmacy manager | 4 | 47 | 42 | 4 | 100 | (n = 130) | |
| Pharmacist responsible for quality | 2 | 49 | 40 | 9 | 100 | (n = 435) | |
| Pharmacist without special responsibilities | 2 | 46 | 36 | 16 | 100 | (n = 1406) | |
| Other | 4 | 42 | 23 | 31 | 100 | (n = 52) | |
| Time in pharmacy | |||||||
| Fewer than 4 years | 2 | 39 | 37 | 22 | 100 | (n = 188) | |
| More than 4 years | 2 | 48 | 37 | 13 | 100 | (n = 1832) | |
| Been infected with COVID-19 | |||||||
| Yes | 3 | 43 | 38 | 16 | 100 | (n = 522) | |
| No | 2 | 49 | 36 | 13 | 100 | (n = 1293) | |
| Do not know | 4 | 46 | 39 | 11 | 100 | (n = 206) | |
| Fear of contracting COVID-19 | |||||||
| Yes | 2 | 41 | 43 | 14 | 100 | (n = 995) | |
| No | 2 | 53 | 31 | 14 | 100 | (n = 1020) | |
The comments described lack of time for all tasks in general. It was considered as positive by the respondents that continuing education as well as meetings were made digital, which meant that more staff could more easily participate.
4.5. Patient safety
The majority (55%) considered that patient safety in the pharmacies was unaffected by the pandemic, while 24% found that patient safety was worse and 8% found it to be better.
Analysing the impact of all the different subgroups on patient safety showed no major differences compared to the overall results (Table 6).
Table 6.
Perceived impact of the COVID-19 pandemic on patient safety analysed per subgroup (N = 2019).
| Better % | Unaffected % | Worse % | Do not know % | Total % | |||
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Pharmacist | 9 | 54 | 26 | 11 | 100 | (n = 604) | |
| Prescriptionist | 8 | 56 | 23 | 14 | 100 | (n = 1331) | |
| Other | 7 | 52 | 29 | 12 | 100 | (n = 83) | |
| Professional role | |||||||
| Pharmacy manager | 15 | 57 | 22 | 5 | 100 | (n = 131) | |
| Pharmacist responsible for quality | 7 | 60 | 26 | 7 | 100 | (n = 435) | |
| Pharmacist without special responsibilities | 8 | 54 | 24 | 15 | 100 | (n = 1403) | |
| Other | 16 | 58 | 12 | 14 | 100 | (n = 50) | |
| Time in pharmacy | |||||||
| Fewer than 4 years | 11 | 51 | 22 | 17 | 100 | (n = 186) | |
| More than 4 years | 8 | 56 | 24 | 12 | 100 | (n = 1831) | |
| Been infected with COVID-19 | |||||||
| Yes | 8 | 51 | 26 | 15 | 100 | (n = 522) | |
| No | 8 | 58 | 23 | 11 | 100 | (n = 1289) | |
| Do not know | 6 | 51 | 24 | 18 | 100 | (n = 206) | |
| Fear of contracting COVID-19 | |||||||
| Yes | 7 | 47 | 32 | 14 | 100 | (n = 998) | |
| No | 9 | 64 | 16 | 11 | 100 | (n = 1013) | |
The comments specifically mentioning patient safety were related to factors already presented in the results such as low staffing in combination with a high workload. Also, circumstances that added to stress such as working in an unfamiliar environment due to lending pharmacists between pharmacies and the necessity of communicating with the patient's representative rather than the patient directly.
“Fewer customers and fewer prescriptions, but the introduction of new services on short notice has sometimes compromised patient safety. Not fully thought through, it [the service] should just be done quickly to meet needs or financial opportunities.”
“Stressful! You are constantly thinking about how to move, how to keep your distance from both colleagues and customers. At the same time, you think about patient safety and dispensing correctly. One feels divided and insufficient. Understaffing due to sickness makes it even worse.”
5. Discussion
This study is to our knowledge the largest survey regarding the perceived impact of the COVID-19 pandemic on pharmacists working in community pharmacies.
The results show that most of the pharmacists considered the workload to have increased during the pandemic while at the same time the physical and psychosocial work environments were considered to have deteriorated. Despite these findings, many respondents stated that patient safety was not affected.
No action appears to have been implemented by the pharmacy companies to deal with the increased workload. On the contrary, new pharmacy services were added to the existing workload in addition to following guidelines issued by the authorities such as keeping track of the number of customers in the pharmacy. The change in workload was handled differently in other countries. In England and Scotland, the pharmacy opening hours were reduced during the pandemic on the initiative of the pharmacy companies. This reduction in opening hours was used to “catch up” on backlogs of tasks in order to ensure patient safety in dispensing.18
According to respondents, the intention of the pharmacy companies was to keep pharmacies open as much as possible. Only a few pharmacies were closed, and then only for short periods due to staff shortage or due to reduced opening hours in the shopping centre the pharmacy was located in.42 The staff was also expected to prioritise retail activities in order to maintain earnings. This focus may be due to the disparity in views that pharmacists, pharmacy companies, and society seem to have regarding the purpose of pharmacies in Sweden. While the pharmacists see themselves as providers of health care, the pharmacy owners in general have a more commercial perspective focusing on sales, according to our respondents. This is in line with previous research in Sweden where many stakeholders see the pharmacies mainly as retail shops.43 These differences in opinions probably had a decisive impact on how pharmacies were governed to handle the pandemic.
The pharmacists considered the provision of PCR tests for COVID-19 to increase the workload, as well as increasing the risk of infection. One pharmacy company distributing tests reported that they indeed saw increased customer flows in the pharmacies while handing out tests.44 They did not, however, see an increase in incident reports regarding infected customers coming to collect tests, and thus no further actions were taken.44 In Queensland and South Australia a similar situation arose, although the topic was about performing PCR testing in pharmacies. In addition to the risk of contributing to spreading the disease, the intervention in Australia caused a fear of pharmacies prioritising financial and professional interests rather than public health interests.45 To our knowledge, no such debate emerged in Sweden.
In the beginning of the pandemic the pharmacy staff in Sweden was, according to the respondents, not allowed to use face masks by the employer. This was explained by one Swedish pharmacy company as a way of not drawing resources from health care when there was a shortage of masks.46 A recommendation to avoid close physical contacts with others was in place in February of 2020 in Sweden. Considering that it is hard to keep physical distances in the pharmacies that often are crowded and have small back offices, the message from the pharmacy companies about face masks was questionable. FIP (Federation Internationale Pharmaceutique) recommended pharmacy staff to wear face masks already in March 2020.47 In most European countries disposable face masks were in general use early during the pandemic10 but not recommended until 2021 in Sweden. More communication from the head offices of the pharmacy companies explaining why certain strategies were – or were not – adopted might have reduced the negative feelings reported by the respondents.
Many respondents described their work during the pandemic as stressful, which is in line with the experiences reported in other studies.9,13,14,16 The job demands-resource model has been applied regarding burnout among pharmacists during the pandemic.13,48 Demands such as increased workload, managing medication supplies, and dealing with poor costumer behaviour were similar to those described by Johnston et al.13 as well as those relayed by the Swedish pharmacists. Conflicts regarding restrictions that arose in pharmacies between customers and staff further contributing to experienced stress and pressure . This has also been described in Australia where controversies arose stemming from a lack of understanding of the need for COVID-related restrictions among the public.49 Lack of understanding among customers regarding restrictions has also been noted in, for example, Saudi Arabia.50 Neither the rate of burnout nor the level of sick leave were measured in this study, but a higher rate of burnout among pharmacists in Australia during the pandemic has been reported.14 Some respondents in our study noted feelings of stress, and job stress has been shown to correlate with workplace burnout, and these factors show a negative correlation with the intention to remain in one's workplace.51 Also in this study, some respondents stated that they were planning on quitting their job – which might be an indication of perceived substandard conditions in their workplace.
Both in Australia and in our study, the increased demands during the pandemic were combined with reduced job resources, a perceived lack of support from management, and a feeling of not being appreciated or recognised.13 This lack of appreciation was also highlighted in the UK where more than 90% of the pharmacists felt that their contribution during the pandemic was not recognised by other healthcare services, the government, the public, or pharmacy owners.52 In some other countries the pandemic led to the introduction of new services in pharmacies; for instance, in Australia pharmacists have been given new rights and roles they hope to retain such as providing pharmaceutical care in a non-pharmacy environment and providing pharmacist-administered vaccinations.45,53 This development does not appear to have taken place in Sweden.
The impact of the pandemic on patient safety are somewhat surprising. Patient safety was perceived as unaffected in the pharmacies, regardless of the otherwise stated effect of the pandemic on workload, work environment, and continuing education. This is in line with some studies26 in community pharmacies but contradictory to other studies where burnout and poor well-being in health care staff has been shown to be associated with negative patient safety outcomes.27 However, as many as 24% in this survey thought that patient safety had been impaired. In Sweden a negative development regarding patient safety issues in community pharmacies was reported some years ago after the de-regulation of the Swedish pharmacy market.29,30 As previously noted, pharmacies as for-profit organisations can be a hidden threat to patient safety.28 If patient safety has continued to deteriorate during latter years, an already exhausted staff might have difficulties perceiving a difference during the pandemic.
Another possibility is that patient safety was defined as a lack of error reports and that a possible connection to workload and work environment was overlooked by the respondents. In Swedish pharmacies serious errors are to be reported to the authorities. Neither the number of reports to the Medical Products Agency nor to the Health and Social Care Inspectorate increased during the pandemic (personal communications). In fact, the number of reports to the latter authority decreased during 2020 and 2021. High incident reporting rates are positively associated with well-functioning patient safety work,54 and the low reporting of serious errors during the pandemic does not support the perception of an unaffected level of patient safety.
A study of mortality in hospitals showed a correlation between workload and patient safety and suggested that there is a “tipping point” in patient safety.55 When the workload is high, the organisation initially has the ability to respond using, for example, staffing pools, to promote the prioritisation of patients and to motivate staff to go the extra mile, a mindset that can probably also be applied to pharmacists. When the workload becomes too intense, the organisation has less ability to respond as the buffers of staff become depleted, and this affects the staff with stress that impairs their cognitive abilities, thus impacting patient safety.55 Because most of the pharmacists in our study considered patient safety to be unaffected, they probably have not reached the “tipping point”. However, being able to uphold patient safety can come with a cost in effort. Perhaps the tipping point was reached for almost a quarter of the pharmacists who perceived patient safety as having deteriorated during the pandemic.
Another possible explanation might be that the results are influenced by the concept of social desirability.56 In this context, social desirability is to be interpreted as the pharmacists wanting to present themselves, their colleagues, or their pharmacy in a favourable way. As a pharmacist, who should protect patient safety, it might be hard to admit to having carried out less than safe actions, regardless of the circumstances. Another, even more troubling explanation, is the possibility that the atmosphere in pharmacies is perceived as oppressive by some respondents. The contact person for this study received both e-mails and phone calls from respondents who expressed fear of their responses being leaked and anonymity not being maintained. The questionnaires were numbered, and this might have been perceived as if the surveys were not anonymous by the respondents. Numbering has previously been shown to affect response rates negatively.57 A questionnaire to Swedish doctors, who are members of the Swedish Medical Association, revealed similar problems with their work climate where only half of the respondents dared to voice criticism.58 These signals stemming from different parts of the Swedish health care system need to be taken seriously.
6. Strengths and limitations
The main strength of this study is that it is a census as all Swedish community pharmacists registered in the Swedish Occupational Register were invited to participate and thus no sampling took place.
Another strength of the study is that all pharmacists in the study were working already before the pandemic and hence were able to make comparisons to the situation in community pharmacies prior to the pandemic.
The gender ratio and age distribution were similar in the respondent group and the registry, thereby further strengthening the credibility of the results and indicating that respondents did not seem to differ from non-respondents. In addition, the number of respondents stating that they had had COVID-19 was 26%, a number that is on par with the overall value of confirmed COVID-19 cases in the population 25–65 years of age, which was 28% at the end of February 2022 according to personal communication with the Public Health Agency in Sweden and population statistics.59
The quality of the data and the delay in data collection of two years in the Swedish Occupational Register are concerns. The group of respondents as provided by Statistics Sweden also included some non-pharmacists. Some data in the register are submitted by the pharmacy companies, and this impacts the quality of the register. This problem was foreseen, and selection questions were added in the survey. In addition, there is also a risk of licensed pharmacists in community pharmacies not being included in the register. This is, however, the only available register of all pharmacists in Sweden.
The aim of this study was to examine community pharmacists' perceptions of the impact of the pandemic on the workload, physical working environment, psychosocial working environment, and patient safety in community pharmacies. Pharmacists are university educated and were therefore expected to understand these concepts. The validation of this questionnaire was unfortunately limited because it was feared that the pandemic would end shortly and that recall bias could possibly increase. However, the questions in the survey were discussed in depth with pharmacists in academia, all with some experience from community pharmacies. Also, one of the members of the research group had recent extensive experience in community pharmacy. It cannot be ruled out that some pharmacists did not understand the wording of the questions. However, this is believed to be limited because the partial non-response in this study was low (0%–1% percent) indicating that the questions were neither hard to understand nor sensitive.
It is likely that negative respondents were more engaged in providing comments, and it has been shown that situations that produce negative emotions also tend to be better remembered than positive situations.60 Several respondents were satisfied with the way the pharmacies and their colleagues had handled the pandemic. However, the comments described mainly negative aspects.
The generalizability of the findings is dependent on the pandemic and national recommendations regarding how to handle the pandemic. Because Sweden handled the pandemic differently than many other countries, the generalizability is, from that point of view, limited. The results, however, could provide guidance to community pharmacies in the management of future pandemics.
7. Recommendations for future research
Considering the criticism raised by the respondents regarding how the pharmacy companies handled the pandemic and its influence on their operations, it is of interest to also study the companies' views.
The results regarding patient safety were surprising and deserve further examination. This could be done by studying the patient safety climate using questionnaires as well as qualitative studies on how patient safety is interpreted by community pharmacists. Further qualitative studies should explore the strategies of pharmacists for handling increased workload and a deterioration in work environment in parallel to maintaining patient safety during such events as a pandemic.
A general approach to communication within pharmacy companies, i.e., not only in times of crisis, might be of interest because this study revealed that there is a lack of understanding of each other's perspectives.
8. Conclusion
The respondents were clear that the workload had increased and that the working environment, both physical and psychosocial, had deteriorated. However, the respondents did not consider that patient safety had been influenced by the external factors that had pronouncedly affected working conditions in general. The management was considered to not understand the working conditions during the pandemic. The importance of good and clear communication within the pharmacy companies cannot be overemphasised.
Funding
This study was funded by a research grant from Sahlgrenska Academy, Gothenburg University. This funding source was not involved in the conduct of the research or the presentation of the results. This research did not receive any other grants from agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
C. Ljungberg Persson: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Visualization, Project administration, Funding acquisition. A. Nordén Hägg: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Visualization. B. Södergård: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
Björn Södergård is employed by Sveriges Farmaceuter, The Swedish Pharmacists Association, a trade union for university graduates in pharmacy, and Christina Ljungberg Persson is a board member of the same organisation. Sveriges Farmaceuter had no role in the research process or in the process of writing his paper. Declarations of interest: none.
Acknowledgements
The authors would like to thank all the pharmacists for participating in this study and Karolina Andersson Sundell for valuable contributions in the planning of the data collection.
Contributor Information
C. Ljungberg Persson, Email: christina.ljungberg.persson@gu.se.
A. Nordén Hägg, Email: annikanordn.h@telia.com.
References
- 1.Koontalay A., Suksatan W., Prabsangob K., Sadang J.M. Healthcare’Workers’ burdens during the COVID-19 pandemic: a qualitative systematic review. J Multidiscip Healthc. 2021;14:3015–3025. doi: 10.2147/JMDH.S330041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Souza D.O. Health of nursing professionals: workload during the COVID-19 pandemic. Rev Bras Med Trab. 2021;18:464–471. doi: 10.47626/1679-4435-2020-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoogendoorn M.E., Brinkman S., Bosman R.J., Haringman J., de Keizer N.F., Spijkstra J.J. The impact of COVID-19 on nursing workload and planning of nursing staff on the intensive care: a prospective descriptive multicenter study. Int J Nurs Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Sio S., Buomprisco G., La Torre G., et al. The impact of COVID-19 on’doctors’ well-being: results of a web survey during the lockdown in Italy. Eur Rev Med Pharmacol Sci. 2020;24:7869–7879. doi: 10.26355/eurrev_202007_22292. [DOI] [PubMed] [Google Scholar]
- 5.Lake E.T., Narva A.M., Holland S., et al. Hospita’ nurses’ moral distress and mental health during COVID-19. J Adv Nurs. 2022;78:799–809. doi: 10.1111/jan.15013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaukat N., Ali D.M., Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. 2020;13:40. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res Soc Adm Pharm. 2021;17:2032–2035. doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.International Pharmaceutical Federation COVID-19: guidelines for pharmacists and the pharmacy workforce. https://www.fip.org/files/content/priority-areas/coronavirus/COVID-19-Guidelines-for-pharmacists-and-the-pharmacy-workforce.pdf Available from. Accessed 29.08.22.
- 9.Gleeson L.L., Ludlow A., Clyne B., et al. Pharmacist and patient experiences of primary care during the COVID-19 pandemic: an interview study. Explor Res Clin Soc Pharm. 2022;8 doi: 10.1016/j.rcsop.2022.100193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costa S., Romão M., Mendes M., et al. Pharmacy interventions on COVID-19 in Europe: mapping current practices and a scoping review. Res Soc Adm Pharm. 2022;18:3338–3349. doi: 10.1016/j.sapharm.2021.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kua K.P., Lee S.W.H. The coping strategies of community pharmacists and pharmaceutical services provided during COVID-19 in Malaysia. Int J Clin Pract. 2021;75 doi: 10.1111/ijcp.14992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koster E.S., Philbert D., Bouvy M.L. Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Res Soc Adm Pharm. 2021;17:2002–2004. doi: 10.1016/j.sapharm.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston K., O’Reilly C.L., Scholz B., Mitchell I. The experiences of pharmacists during the global COVID-19 pandemic: a thematic analysis using the jobs demands-resources framework. Res Soc Adm Pharm. 2022;18:3649–3655. doi: 10.1016/j.sapharm.2022.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnston K., O’Reilly C.L., Scholz B., Georgousopoulou E.N., Mitchell I. Burnout and the challenges facing pharmacists during COVID-19: results of a national survey. Int J Clin Pharm. 2021;43:716–725. doi: 10.1007/s11096-021-01268-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston K., O’Reilly C.L., Scholz B., Georgousopoulou E.N., Mitchell I. The “affected” pharmacist and the “business as usual” pharmacist: Exploring the experiences of pharmacists during COVID-19 through cluster analysis. J Am Pharm Assoc. 2003;2023(63):144–150.e2. doi: 10.1016/j.japh.2022.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Etezad S., Fleming M., Weigand H.A., et al. Exploring the well-being of community pharmacy professionals, turnover intention and patient safety: time to include operational responsibility. Can Pharm J (Ott) 2023;156:71–84. doi: 10.1177/1715163523115217017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Patient safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety Available from. Accessed 20.01.23.
- 18.Peat G., Olaniyan J., Fylan B., et al. Mapping the resilience performance of community pharmacy to maintain patient safety during the Covid-19 pandemic. Res Soc Adm Pharm. 2022;18:3534–3541. doi: 10.1016/j.sapharm.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO What is patient safety? https://www.who.int/teams/integrated-health-services/patient-safety/about Available from. Accessed 15.01.23.
- 20.Cheung K.C., Bouvy M.L., De Smet P.A. Medication errors: the importance of safe dispensing. Br J Clin Pharmacol. 2009;67:676–680. doi: 10.1111/j.1365-2125.2009.03428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ashcroft D.M., Quinlan P., Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf. 2005;14:327–332. doi: 10.1002/pds.1012. [DOI] [PubMed] [Google Scholar]
- 22.Phipps D., Ashour A., Riste L., Lewis P., Ashcroft D. Understanding dispensing errors and risk. Pharm J. 2020:305. doi: 10.1211/PJ.2020.20208528. [DOI] [Google Scholar]
- 23.Johnson S.J., O’Connor E.M., Jacobs S., Hassell K., Ashcroft D.M. The relationships among work stress, strain and self-reported errors in UK community pharmacy. Res Soc Adm Pharm. 2014;10:885–895. doi: 10.1016/j.sapharm.2013.12.00. [DOI] [PubMed] [Google Scholar]
- 24.Teinilä T., Grönroos V., Airaksinen M. A system approach to dispensing errors: a national study on perceptions of the Finnish community pharmacists. Pharm World Sci. 2008;30:823–833. doi: 10.1007/s11096-008-9233-4. [DOI] [PubMed] [Google Scholar]
- 25.Szeinbach S., Seoane-Vazquez E., Parekh A., Herderick M. Dispensing errors in community pharmacy: perceived influence of sociotechnical factors. Int J Qual Health Care. 2007;19:203–209. doi: 10.1093/intqhc/mzm018. [DOI] [PubMed] [Google Scholar]
- 26.Hassell K., Seston E.M., Schafheutle E.I., Wagner A., Eden M. Workload in community pharmacies in the UK and its impact on patient safety and pharmacists’ well-being: a review of the evidence. Health Soc Care Comm. 2011;19:561–575. doi: 10.1111/j.1365-2524.2011.00997.x. [DOI] [PubMed] [Google Scholar]
- 27.Hall L.H., Johnson J., Watt I., Tsipa A., O’Connor D.B. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. 2016;11 doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jairoun A.A., Al-Hemyari S.S., Jairoun M., El-Dahiyat F., Al-Ani M., Habeb M. Hidden factors in community pharmacy related to medication safety risks: pushing patient safety to breaking point. Res Soc Adm Pharm. 2022;18:3217–3219. doi: 10.1016/j.sapharm.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 29.Nordén-Hägg A., Sexton J.B., Kälvemark-Sporrong S., Ring L., Kettis-Lindblad Å. Assessing safety culture in pharmacies: the psychometric validation of the safety attitudes questionnaire (SAQ) in a national sample of community pharmacies in Sweden. BMC Clin Pharmacol. 2010;10:8. doi: 10.1186/1472-6904-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kälvemark Sporrong S., Nordén-Hägg A. Trends in pharmacy staff’s perception of patient safety in Swedish community pharmacies after re-regulation of conditions. Pharm Pract (Granada) 2014;12:502. doi: 10.4321/s1886-36552014000400010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Public Health Agency of Sweden The Swedish strategy about COVID-19. https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/covid-19/covid-19-more-information/covid-19--the-swedish-strategy/ Available from. Accessed 27.06.22.
- 32.Government Offices of Sweden Förordning om ändring i förordningen (2009:659) om handel med läkemedel. https://svenskforfattningssamling.se/sites/default/files/sfs/2020-03/SFS2020-164.pdf Available from. Accessed 27.06.22.
- 33.The Swedish Parliament Lag (2021:4) om särskilda begränsningar för att förhindra spridning av sjukdomen covid-19. https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-20214-om-sarskilda-begransningar-for-att_sfs-2021-4 Available from. Accessed 27.06.22.
- 34.Statistics Sweden The Swedish Occupational Register with statistics. https://www.scb.se/en/finding-statistics/statistics-by-subject-area/labour-market/employment-and-working-hours/the-swedish-occupational-register-with-statistics/ Available from. Accessed 28.06.22.
- 35.Statistics Sweden Data protection policy. https://www.scb.se/contentassets/b3ecb07ca2b14f06b8424f59929831de/data_protection_policy_2021_en.pdf Available from. Accessed 25.04.23.
- 36.Rao D., Shiyanbola O.O. Best practices for conducting and writing mixed methods research in social pharmacy. Res Soc Adm Pharm. 2022;18:2184–2192. doi: 10.1016/j.sapharm.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 37.eurostat Statistics Explained Glossary:Census. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Glossary:Census Available from. Accessed 17.02.23.
- 38.Alexander N. What’s more general than a whole population? Emerg Themes Epidemiol. 2015;12:11. doi: 10.1186/s12982-015-0029-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elo S., Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 40.Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14. [Google Scholar]
- 41.Gale N.K., Heath G., Cameron E., Rashid S., Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sveriges Apoteksförening Branschrapport. 2021. http://www.sverigesapoteksforening.se/wp-content/uploads/2021/03/Branschrapport-2021.pdf2021 Available from. Accessed 24.01.22.
- 43.Wisell K., Sporrong S.K. The raison D’être for the community pharmacy and the community pharmacist in Sweden: a qualitative interview study. Pharmacy (Basel) 2015;4:3. doi: 10.3390/pharmacy4010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Falk A. Svensk Farmaci; 2022. Apotekssektionen: Fortsatt risk för smitta på jobbet.https://www.svenskfarmaci.se/2021/03/30/apotekssektionen-fortsatt-risk-for-smitta-pa-jobbet/ Available from. Accessed 02.09.22. [Google Scholar]
- 45.Chiu K., Thow A.M., Bero L. “never waste a good crisis”: opportunities and constraints from the COVID-19 pandemic on pharmacists’ scope of practice. Res Soc Adm Pharm. 2022;18:3638–3648. doi: 10.1016/j.sapharm.2022.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hedberg F. Svensk farmaci; 2022. Plexiglas installeras på många svenska apotek.https://www.svenskfarmaci.se/2020/03/27/plexiglas-installeras-pa-manga-svenska-apotek/ Available from. Accessed 17.06.22. [Google Scholar]
- 47.International Pharmaceutical Federation COVID-19 SUMMARY GUIDANCE #8 Use of masks. https://www.fip.org/file/4755 Available from. Accessed 19.10.22.
- 48.Abdelsadig Mohammed H., et al. Use of the job demands-resource model to understand community pharmacists’ burnout during the COVID-19 pandemic. Res Soc Adm Pharm. 2022;18(9):3568–3579. doi: 10.1016/j.sapharm.2022.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lam W., Mey A., King M.A., Woods P. The nature of conflict in community pharmacy - a pilot study of pharmacists’ experiences during the COVID-19 pandemic. Res Soc Adm Pharm. 2022;18:3164–3173. doi: 10.1016/j.sapharm.2021.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khojah H.M.J. Community pharmacy services and preparedness during COVID-19 outbreak in Madinah, Saudi Arabia. Saudi Pharm J. 2020;28:1402–1407. doi: 10.1016/j.jsps.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lan Y.L., Huang W.T., Kao C.L., Wang H.J. The relationship between organizational climate, job stress, workplace burnout, and retention of pharmacists. J Occup Health. 2020;62 doi: 10.1002/1348-9585.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zaidi S.T.R., Hasan S.S. Personal protective practices and pharmacy services delivery by community pharmacists during COVID-19 pandemic: results from a national survey. Res Soc Adm Pharm. 2021;17:1832–1837. doi: 10.1016/j.sapharm.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parajuli D.R., Khanal S., Wechkunanukul K.H., Ghimire S., Poudel A. Pharmacy practice in emergency response during the COVID-19 pandemic: lessons from Australia. Res Soc Adm Pharm. 2022;18:3453–3462. doi: 10.1016/j.sapharm.2021.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hutchinson A., Young T.A., Cooper K.L., et al. Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and learning system. Qual Saf Health Care. 2009;18:5–10. doi: 10.1136/qshc.2007.022400. [DOI] [PubMed] [Google Scholar]
- 55.Kuntz L., Mennicken R., Scholtes S. Stress on the ward: evidence of safety tipping points in hospitals. Manag Sci. 2015;61:754–771. doi: 10.1287/mnsc.2014.1917. [DOI] [Google Scholar]
- 56.Freeth D., Sandall J., Allan T., et al. A methodological study to compare survey-based and observation-based evaluations of organisational and safety cultures and then compare both approaches with markers of the quality of care. Health Technol Assess. 2012;16:iii–184. doi: 10.3310/hta16250. [DOI] [PubMed] [Google Scholar]
- 57.Perneger T.V., Cullati S., Rudaz S., et al. Effect of numbering of return envelopes on participation, explicit refusals, and bias: experiment and meta-analysis. BMC Med Res Methodol. 2014:14. doi: 10.1186/1471-2288-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sveriges läkarförbund . Arbetsmiljöenkäten. 2022. Tystnadskultur –bara hälften vågar framföra kritik.https://slf.se/app/uploads/2022/10/arbetsmiljoenkaten-2022-tystnadskultur.pdf Available from. Accessed 01.12.22. [Google Scholar]
- 59.Statistics Sweden Statistical database . Official statistics of Sweden; 2022. Population per month by region, age and sex. Year 2000M01 - 2022M08.https://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__BE__BE0101__BE0101A/BefolkManad/ Available from. Accessed 19.10.22. [Google Scholar]
- 60.Kensinger E.A. Remembering the details: effects of emotion. Emot Rev. 2009;1:99–113. doi: 10.1177/1754073908100432. [DOI] [PMC free article] [PubMed] [Google Scholar]