Abstract
Vaccination plays a crucial role in combating the global COVID-19 pandemic. Immunizing all healthcare workers (HCWs) is essential for increasing vaccine confidence and acceptance within the general population. Understanding the factors that hinder or facilitate vaccine uptake among HCWs is of utmost importance, considering they are among the first to be vaccinated. This review follows Arksey and O’Malley’s five-stage methodological framework. We searched PubMed, Web of Science, ProQuest, WorldCat Discovery, and Google Scholar for peer-reviewed articles published from 2020 to 2023. A descriptive analysis and narrative synthesis approach were employed to collect and synthesize data. Using the social-ecological model as a framework, the literature was categorized into themes at the intrapersonal, interpersonal, organizational, community, and policy levels. We reviewed a total of fifty-three published academic articles, with the majority of studies conducted in Ethiopia and Nigeria. The intention for vaccine uptake resulted in an unsatisfactory (52%) overall uptake rate among HCWs. Individual-level determinants associated with vaccine uptake included being male, middle-aged, being a physician, having a higher level of education, and having a chronic illness. This review identified significant barriers at each level, such as safety concerns, perceived scientific uncertainty, vaccine ineffectiveness, lack of trust in stakeholders, and religious beliefs. Additionally, we identified facilitators at each level, with the most common factors promoting intention to uptake being the desire to protect oneself and others and a high perceived susceptibility to contracting COVID-19. This review highlights the existence of significant barriers to vaccine uptake on the African continent. Given that HCWs play a crucial role in guiding the public’s vaccination decisions, it is imperative to prioritize education and training efforts about the safety and effectiveness of COVID-19 vaccines.
Keywords: HCWs, COVID-19 vaccines, Africa, Social Ecological Model, barriers, facilitators, scoping review
1. Introduction
The World Health Organization (WHO) approved several vaccines against COVID-19 for global distribution in various regions [1,2]. Vaccines manufactured by Pfizer, Oxford/AstraZeneca, Moderna, Janssen, Sputnik V, Sinovac, and Sinopharm, among others, were authorized and made available in Africa [2,3]. In the first quarter of 2021, mass vaccination programs commenced in several African countries [2,3,4]. These campaigns were planned in 31 African countries until 2022 [5]. Egypt was the first African country to begin vaccination on 24 January 2021, followed by South Africa on 17 February 2021, and Zimbabwe on 18 February 2021 [4]. During the distribution of the COVID-19 vaccination, there have been substantial problems with vaccine nationalism and access equity [6] Hence, Africa and other low-and middle-income countries (LMICs) have low COVID-19 vaccine coverage [7]. As a result, the COVAX global initiative was established to ensure equitable and timely access to vaccines worldwide [8]. The continent received more than 892 million vaccine doses, with the COVAX facility accounting for 64% of the total vaccinations received [9]. Much progress has been made in increasing vaccine shipments to countries [10,11]. Despite greater access to COVID-19 vaccinations, the COVID-19 pandemic has exposed numerous flaws in African healthcare systems, particularly in the aftermath of the Delta and Omicron variants [10,12]. As of 16 October 2022, only 24% of the African continent’s population had been vaccinated, compared to a global coverage of 64% [13]. According to the WHO, Africa is on track to reach the global vaccination coverage target of 70% by April 2025 [13]. As vaccine supply has increased worldwide, it has become clear that COVID-19 vaccine hesitancy (VH) challenges vaccine uptake [14,15] in Africa [8,16], particularly in Western and Central Africa [17]. The WHO ranked VH as one of the top ten threats to global health [14,16] and defines it as “a delay in acceptance or refusal of vaccines despite availability of vaccination services” [18] (p. 899). This broad definition highlights variability by stating that VH varies between vaccine types, contexts, geographical regions, and over time. This phenomenon has been exacerbated by the current COVID-19 pandemic [15,19].
Due to a global shortage of COVID-19 vaccines, governments have prioritized high-risk groups for vaccination [11,20,21]. Despite African countries prioritizing healthcare workers (HCWs), vaccine coverage remains low due to VH and a lack of vaccination services and fear of its side effects, especially in rural areas, leaving the vast majority of front-line workers unprotected [4,11,22]. Studies showed that not all HCWs are prepared to receive the COVID-19 vaccine when it becomes available in their country [8,22,23]. Concerns have been raised about VH among HCWs throughout Africa [11,22]. Vaccine acceptance (VA) and hesitancy have been a global problem, particularly in African settings [16,24,25]. Historical, structural, and other systemic dynamics contribute to VH in the African continent [7,8], and are a remaining threat to Africa’s vaccination programmes [17]. The increased polio outbreaks in Nigeria have been argued to stem from misinformation and public distrust in vaccination between 2002 and 2006 and subsequent polio outbreaks on three continents [8,26]. Furthermore, mass deworming programmes in Ghana were rejected due to community misconceptions [8]. Furthermore, trust in current vaccines has been eroded by a history of colonial medical and vaccine research abuse in Africa [7]. African populations were frequently subjected to unethical testing in the name of scientific advancement [7,27]. At the beginning of 2021, Tanzania’s health minister announced that the country would forgo COVID-19 vaccination due to concerns about vaccine safety and would instead depend on traditional and household herbs and medicines for prevention and cure [28,29].
There are numerous barriers and drivers that influence vaccination intention (VI) and uptake, ranging from individual psychological, socio-cultural, and environmental factors that influence HCW’s willingness to be vaccinated [30,31,32,33]. The Social Ecological Model (SEM) was initially developed by Urie Bronfenbrenner [34] and later adapted by McLeroy and colleagues [35]. This framework, widely used in public health and social sciences, aims to comprehend the various factors influencing human behaviour and health outcomes [34,35]. It acknowledges that individuals exist within different social systems and that multiple levels of influence interact to shape their behaviours [35]. These levels are as follows: Intrapersonal Level: this level focuses on the characteristics and attributes of individuals, including factors such as knowledge, attitudes, beliefs, skills, and biological factors. Interpersonal Level: The interpersonal level involves the impact of relationships and social networks on an individual. It includes family, friends, peers, co-workers, and other social connections. Organizational Level: The organizational level pertains to formal and informal rules, policies, and practices. It can encompass schools, workplaces, community organizations, and religious institutions. Organizational factors can affect access to resources, opportunities, and social norms. Community Level: The community level encompasses the physical and social environment in which individuals reside. It includes the characteristics of the community, such as its infrastructure, social capital, and cultural norms. Community factors can influence social norms, social networks, and the availability of resources and services. Policy Level: The policy level represents the broader social, economic, and political context in which individuals and communities are situated. It encompasses public policies, laws, social inequality, and cultural values.
In light of continuous COVID-19 infections and the likelihood of future pandemics, HCW’s hesitation in vaccination uptake remains an area of concern. Given that HCWs are among the first to be vaccinated, it is critical to understand factors that pose barriers or facilitate vaccine uptake. In light of this, we used the five-level SEM to segment the levels of influence (intrapersonal, interpersonal, organizational, community, and policy level) to provide a more comprehensive and nuanced understanding of how these factors shape vaccine-related behaviours. The identified factors were organized into barriers and facilitators to clarify their influence on VA and VH. While a review had been conducted on VA on the African continent among HCWs [36], this review focused on factors and barriers influencing COVID-19 vaccine acceptance, intention for uptake, and hesitancy among HCWs on the African continent in lieu of informing intervention approaches to address likely barriers in future immunization programmes.
2. Methods
This scoping review was conducted using Arksey and O’Malley’s methodological framework [37]. The following five-stage framework proposed was as follows: “(1) Identifying the research questions, (2) Searching for relevant studies, (3) Selecting studies, (4) Charting the data, and (5) Collating, summarising, and reporting the results” [37] (p. 22). This review includes the Preferred Reporting Items for Systematic Review and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) checklist (Supplementary Materials S1) [38]. A review protocol was submitted to the University of KwaZulu-Natal (UKZN) Humanities and Social Sciences Research Ethics Committee (HSSREC)—Application number: 00013262.
2.1. Identifying the Research Questions
What is the rate of uptake of COVID-19 vaccinations among HCWs?
What socio-demographic factors are associated with VA or VH among HCWs?
What factors act as barriers or facilitators for vaccine uptake among HCWs?
2.2. Searching for Relevant Studies
A comprehensive literature search was conducted in five databases: Web of Science, WorldCat Discovery, PubMed, Google Scholar, and ProQuest to retrieve studies related to the above research questions, and the search period for the review spanned from 2020 to 2023. The final search was completed in May 2023. The COVID-19 pandemic was the motivating factor behind this timeline. The following search terms were applied, using a variation of MEsH terms and keywords for each database: “COVID-19 vaccines”, “COVID-19”, “SARS-CoV-2 vaccines”, “associated factors”, “intention”, “barriers”, “drivers”, “acceptance”, “hesitancy”, “Africa”, “Healthcare workers”, “vaccine uptake”, “vaccine refusal”, “HCWs”, “COVID-19 vaccination uptake”, “COVID-19 vaccination intention”, “COVID-19 vaccine willingness”. The final search strategies for WorldCat Discovery and PubMed are in Appendix A, Table A1, Table A2 and Table A3.
2.3. Study Selection
After thoroughly screening the titles and abstracts, inclusion and exclusion criteria were established initially and studies were considered using the Population–Concept–Context (PCC) framework to determine their eligibility for this review. Full-text eligible studies met the following inclusion criteria: (1) literature type: academic/published journals (peer-reviewed journals); (2) language: studies that were published in the English language; (3) timeline: studies that were published between 2021 and 2023, (4) location: studies conducted in Africa; (5) vaccines: COVID-19 vaccines; (6) populations: HCWs—using the WHO definition of HCWs [39] (7) study designs: quantitative, qualitative, or mix-methods studies; (8) studies that specifically address the research questions. The following were excluded: grey literature (unpublished journals, reports and documents, conference papers, memoranda, theses, letters, and protocols) and reviews (scoping and systematic).
2.4. Charting Data
Data extraction from the included peer-reviewed studies was conducted using a standardized Microsoft Excel data collection sheet. A reviewer (D.N) extracted data from included reviews, which was then independently verified by a second reviewer (A.M-W). The following data fields were extracted from each study: author, year of publication, country, data collection period, methodology and study design, population characteristics, sample size, and measurement scales. The VI, VH, and VA levels among HCWs were analysed, summarised, and compared using simple descriptive statistics (percentages). A narrative synthesis approach [40] was utilized to acquire, synthesize, and map the literature utilizing the SEM to group facilitators and barriers to the uptake of the COVID-19 vaccine. All data were reported using thematic narratives [41].
2.5. Collating, Summarising, and Reporting the Results
The results have been compiled and summarized. Following a description of the study’s characteristics, the relevant influencing factors are presented using the SEM. Barriers and facilitators impacting the uptake of COVID-19 vaccines were categorized into various levels, including socio-demographic characteristics, individual factors, social factors, institutional factors, community factors, and policy factors.
3. Results
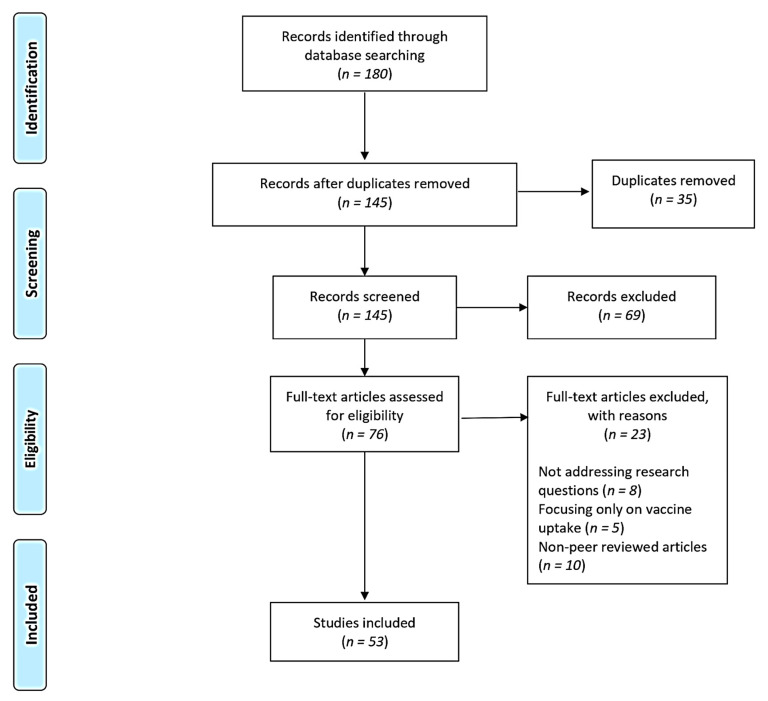
A total of 180 records were identified from the five database searches: Web of Science (n = 20), WorldCat Discovery (n = 16), PubMed (n = 41), Google Scholar (n = 55) and ProQuest (n = 48). After removing duplicates using EndNote (V.X9), 145 records remained for a title and abstract screening. We excluded 69 articles that did not meet the selection criteria, leaving 76 for a review of the full-text articles. The full-text screening was conducted to assess eligibility before further data extraction. Following the inclusion and exclusion assessment criteria, studies were further excluded because they did not address research questions (n = 8), focused solely on vaccine uptake (n = 5), and were non-peer-reviewed (n = 10), resulting in 53 articles included in the final review. The PRISMA flow diagram below illustrates the selection process in Figure 1.
Figure 1.
PRISMA flow diagram: selection of included studies. Adapted from [42].
3.1. Descriptive Analysis of Articles
The majority of the articles included in this review were conducted in Ethiopia (23%), followed by Nigeria (17%), Egypt (13%), South Africa (8%), and Ghana (8%). The remaining articles were conducted in Cameroon, Uganda, Somalia, Tanzania, Namibia, Malawi, Zambia, The Democratic Republic of Congo (DRC), Guinea, Sudan, Sierra Leone, and Tunisia. Two articles focused on multiple African countries, including Nigeria, Cameroon, Sierra Leone, DRC, and Uganda. Please refer to Table 1 for the number of countries reviewed and Appendix B, Table A4 for the included study characteristics.
Table 1.
Illustrates the number of countries reviewed.
| Country of Focus | Number of Studies |
|---|---|
| Ethiopia | 12 |
| Nigeria | 9 |
| South Africa (SA) | 4 |
| Ghana | 4 |
| Tanzania | 1 |
| Namibia | 1 |
| Somalia | 2 |
| Egypt | 7 |
| Uganda | 2 |
| Malawi | 1 |
| Zambia | 1 |
| Cameroon | 2 |
| The Democratic Republic of Congo (DRC) | 1 |
| Guinea | 1 |
| Sudan | 1 |
| Sierra Leone | 1 |
| Tunisia | 1 |
| Multiple African countries | 2 |
The majority of the studies used a quantitative cross-sectional design (88%), while six studies employed a mixed-method design (8%), and one used a qualitative design (4%). This review specifically focused on HCWs, with the exception of a study conducted by Toure and colleagues [43], which also surveyed the general adult population. Since this review had specific exclusion criteria, only the sampled population of HCWs was considered. The sample size of the included studies varied from 15 to 7763 participants. Among the sampled HCWs, the majority were physicians (83%), followed by nurses (73%), pharmacists (49%), medical laboratory technicians (47%), and midwives (42%).
3.2. Survey Instruments/Measurement Scales
There are various types of measurement scales or survey instruments used in research. The articles reviewed in this study employed two types of measurement scales, dichotomous scales and Likert scales, to assess VH or VA. A dichotomous question presents only two possible answer options [44]. This type of question is considered closed-ended because the options are predetermined by the investigator. Dichotomous questions are used when there are only two possible values for the subject being examined [44]. On the other hand, a Likert scale is a rating scale used to evaluate opinions, attitudes, or behaviours. It consists of a statement or question followed by a set of answer statements, typically five, seven, or nine in number [45].
In this review, 12 studies utilized Likert scales, while 36 studies utilized dichotomous scales to measure vaccine uptake. Upon screening the articles, variations in measurement approaches were identified. For example, authors assessed VH or VA using a Likert scale in the following ways. El-Sokkary and colleagues [46] measured vaccination intention by asking participants to indicate their intention to undergo COVID-19 vaccination on a three-point scale: “agree”, “neutral”, or “disagree”. Fares and colleagues [47] measured the decision to receive the COVID-19 vaccine with three options: “yes”, “no”, or “undecided”. In their study, the term “hesitant” was used for the undecided group. Wiysonge and colleagues [48] assessed vaccine acceptance by using the statement, “I will take the COVID-19 vaccine when one becomes available”. This statement had seven response options ranging from “strongly disagree” to “strongly agree”. The responses were later transformed into a binary variable, with responses 1 to 4 categorized as “vaccine hesitancy” and responses 5 to 7 categorized as “vaccine acceptance”.
In terms of dichotomous scales, VH and VA were assessed as follows, Adejumo and colleagues [49] evaluated participants’ willingness to receive the COVID-19 vaccine using single-item questions with “yes” or “no” responses. Yilma and colleagues [50] assessed vaccine acceptability by asking, “If a COVID-19 vaccine is proven safe and effective and is available, will you get vaccinated?” Participants who responded with “definitely not” or “probably not” were categorized as having vaccine non-acceptance, while those who responded with “probably” or “definitely” were categorized as willing to accept the COVID-19 vaccination.
3.3. The Uptake Rate of the COVID-19 Vaccines among HCWs
Table 2 presents the characteristics and COVID-19 vaccine uptake rates among HCWs represented in studies contained in this review.
Table 2.
COVID-19 vaccine uptake rates by author and country.
| Author(s) & Publication Year | Country | Vaccine Intention (VI) |
Vaccine Hesitant (VH) |
Vaccine Acceptance (VA) |
|---|---|---|---|---|
|
Adane et al., 2022
[51] |
Ethiopia | 64.0% | 36.0% | |
|
Adejumo et al., 2021
[49] |
Nigeria | 55.5% | ||
|
Adeniyi et al., 2021
[52] |
South Africa | 90.1% | ||
|
Aemro et al., 2021
[53] |
Ethiopia | 45.9% | ||
|
Agyekum et al., 2021
[23] |
Ghana | 39.6% | 60.7% | |
|
Ahmed et al., 2021
[54] |
Ethiopia | 33.2% | ||
|
Alhassan et al., 2021
[55] |
Ghana | 70.0% | ||
|
Allagoa et al., 2021
[56] |
Nigeria | 44.5% | ||
|
Amour et al., 2023
[57] |
Tanzania | 53.4% | ||
|
Amuzie et al., 2021
[58] |
Nigeria | 50.5% | ||
|
Angelo et al., 2021
[59] |
Ethiopia | 48.4% | 51.6% | |
|
Annan et al., 2021
[60] |
Ghana | 66.9% | ||
|
Asefa et al., 2023
[61] |
Ethiopia | 61.9% | ||
|
Aseneh et al., 2023
[62] |
Multiple countries Cameroon & Nigeria |
50.7% | ||
|
Ashipala et al., 2023
[63] |
Namibia | |||
|
Berhe et al., 2022
[64] |
Ethiopia | 35.8% | ||
|
Dahie et al., 2022
[65] |
Somalia | 48.7% | ||
|
Ekwebene et al., 2021
[66] |
Nigeria | 53.5% | ||
|
El-Ghitany et al., 2022
[67] |
Egypt | 33.5% | 66.5% | |
|
El-Sokkary et al., 2021
[46] |
Egypt | 26% | 32.1% | |
|
Fares et al., 2021
[47] |
Egypt | 21% | 79% | |
|
George et al., 2023
[68] |
South Africa | 89% | ||
|
Guangul et al., 2021
[69] |
Ethiopia | 72.2% | ||
|
Ibrahim et al., 2023
[70] |
Somalia | 38.2% | ||
|
Iwu et al., 2022
[71] |
Nigeria | 64.6% | 34.5% | |
|
Kanyike et al., 2021
[72] |
Uganda | 37.3% | 62.7% | |
|
Mohammed et al., 2021
[73] |
Ethiopia | 60.3% | ||
|
Mohammed et al., 2023
[74] |
Ghana | 73.6% | ||
|
Moucheraud et al., 2022
[75] |
Malawi | 82.5% | ||
|
Mudenda et al., 2022
[76] |
Zambia | 24.5% | ||
|
Ngasa et al., 2021
[77] |
Cameroon | 45.4% | ||
|
Niguse et al., 2023
[78] |
Ethiopia | 71% | ||
|
Nnaemeka et al., 2022
[79] |
Nigeria | 59.3% | ||
|
Nzaji et al., 2020
[80] |
The Democratic Republic of Congo | 27.7% | ||
|
Oriji et al., 2021
[81] |
Nigeria | 72.5% | ||
|
Orok et al., 2022
[25] |
Nigeria | 41.2% | ||
|
Ouni et al., 2023
[82] |
Uganda | 86.7% | 13.3% | |
|
Robinson et al., 2021
[83] |
Nigeria | 48.8% | 39.7% | |
|
Saied et al., 2021
[84] |
Egypt | 34.9% | 65.1% | |
|
Sharaf et al., 2022
[85] |
Egypt | 45.6% | 54.3% | |
|
Shehata et al., 2022
[86] |
Egypt | 75.5% | 22% | |
|
Terefa et al., 2021
[87] |
Ethiopia | 62.1% | ||
|
Tharwat et al., 2022
[88] |
Egypt | 70.5% | 29.5% | |
|
Toure et al., 2022
[43] |
Guinea | 65% | ||
|
Voundi-Voundi et al., 2023
[89] |
Cameroon | 34% | ||
|
Watermeyer et al., 2022
[90] |
South Africa | 90% | ||
|
Whitworth et al., 2022
[91] |
Multiple countries Sierra Leone DRC Uganda |
53.9% | 21% | |
|
Wiysonge et al., 2022
[48] |
South Africa | 59% | 41% | |
|
Yassin et al., 2022
[92] |
Sudan | 63.8% | ||
|
Yendewa et al., 2022
[93] |
Sierra Leone | 60.1% | 38.3% | |
|
Yilma et al., 2022
[50] |
Ethiopia | 25.5% | ||
|
Zammit et al., 2022
[94] |
Tunisia | 51.9% | ||
|
Zewude & Belachew, 2021
[95] |
Ethiopia | 46.9% | 63.4% |
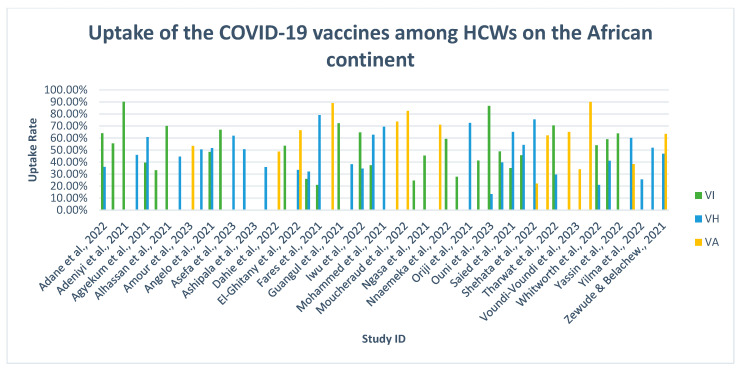
Fifty-two studies reported on COVID-19 vaccination acceptability, intention, and hesitancy. In this review, most of these studies reported HCWs’ hesitation to accept the COVID-19 vaccines on the African continent. A qualitative study conducted by Ashipala and colleagues [63] did not provide information on nurses’ uptake of COVID-19 vaccines.
Twenty-seven studies reported on the intention to accept the COVID-19 vaccine. Intention to accept the vaccine varied dramatically from 21% to 90.1%. Notably, Fares and colleagues [47] found that Egypt (21%) had the lowest intention rate, while Adeniyi and colleagues [52] reported that South Africa (90.1%) had the highest intention rate. Based on the included studies in this review, the intention rate to uptake the COVID-19 vaccine among HCWs was below average [23,25,46,47,54,59,76,77,80,83,88]. Conversely, fourteen studies reported an above-average intention rate [48,49,51,52,55,60,69,71,79,82,88,91,92]. The overall average intention rate for HCWs to uptake the COVID-19 vaccines across all included studies was approximately 52%, indicating a suboptimal level of uptake among this population.
Medical students expressed a lack of willingness to accept the COVID-19 vaccine, with an acceptance rate ranging from 34.7% to 45.4%. A study conducted by Saied and colleagues [83] in Egypt found that only 34.7% of medical students were willing to accept the vaccine, which was disappointing. Most (45.7%) medical students hesitated to accept the vaccine. In addition, 71% intended to take the vaccine but would postpone doing so to wait and observe its effects on those who received it before making a decision themselves.
Twenty-nine studies examined HCWs’ hesitancy towards receiving the COVID-19 vaccine. The degree of hesitancy varied across these studies, ranging from 13.3% to 79%. Fares and colleagues [47] reported the highest VH rate (79%) in Egypt.
Subsequent studies reported HCWs’ acceptance towards the COVID-19 vaccines [43,57,65,68,74,75,78,86,87,89,90,93,95]. Among these ten studies, over half of the participants were vaccinated with at least one dose (see Figure 2). A study by Watermeyer and colleagues [90] reported the highest vaccination rate (90%) in South Africa. Additionally, a study conducted in Ethiopia by Zewude and Belachew [95] further depicted the intention to accept the second dose. Approximately 28.3% of HCWs were VH to accept the second dose.
Figure 2.
An illustration of COVID-19 vaccine uptake rates among the included studies in Africa [23,47,50,51,52,55,57,59,61,63,65,67,69,71,73,75,77,79,81,82,84,86,88,89,91,92,95].
3.4. Socio-Demographic Determinants Associated with VA or VH
Table 3 reports various socio-demographic (individual level) factors influencing vaccine uptake. These factors varied across HCWs on the African continent. Twelve socio-demographic factors were associated with vaccine uptake in this review. Seven socio-demographic factors were prominent in influencing vaccine uptake. These included gender, age, level of education, marital status, presence of chronic illness, living area, and cadre. These factors were further divided into two categories, which include COVID-19 vaccine uptake associated with hesitancy and associated with acceptance. Factors associated with COVID-19 vaccine uptake included being male, middle-aged (older than 40), being a physician, and having a tertiary-level education. In contrast, factors associated with hesitancy towards the COVID-19 vaccine were females younger than 40 and having a tertiary education. Interestingly, a tertiary-level education was a significant factor associated with VA and VH among HCWs.
Table 3.
Socio-demographic determinants associated with vaccine uptake.
| Factors | Associated with Hesitancy | Associated with Acceptance |
|---|---|---|
| Gender | Being female [50,55,85,86,89,94] |
Being female [47] Being male [23,46,56,65,67,72,74,76,77,79,80,87] |
| Age | Younger [50] <30 years [53,58] <35 years [64] <40 years [73,86,94] |
Age [54] >30 years [57] >40 years [65,74,87,94] Older [43,46,48,56] |
| Ethnicity | Amhara [64] | |
| Education level | Tertiary level [50,55,70,86] | Secondary level [43,67] Tertiary level [46,50,52,65,78] |
| Religion | Christian—Pentecostal denomination [71] | Not specified [48] Christian [74] |
| Marital status | Single [58] | Single [72,76] Married [43,77,78] |
| Family status | Being a parent [95] | |
| Pregnancy status | Not being pregnant [43] | |
| Medical condition | Presence of chronic illness [62] | Presence of chronic illness [43,56,59,77] |
| Residential settings | Not specified [65,79] Rural [67] Urban [77] |
|
| Cadre | Nurses & midwives [50,58] Physicians [58,84] Medical laboratory technicians [50,64,71] Environmental health specialist [64] Medical students [93] |
Not specified [53,73] Nurses & midwives [43,51,65] Physicians [23,48,57,59,61,65,79,80] Clinical health workers [50] Public health specialist [65] Academic staff working in hospitals [87] |
| Income level | Average [58] | Not specified [43,46] |
The following factors associated with VA were gender [23,46,56,65,67,72,74,76,77,79,80,87], age [43,46,48,54,56,57,65,74,87,94], education level [43,46,50,52,67,75,78], belonging to religion [48,74], marital status [43,72,76,77,78], being a parent [95], absence of pregnancy [43], presence of chronic illness [43,56,59,77], living area [65,67,77,79], cadre [23,43,48,49,51,53,57,59,61,65,73,79,80,87], and income level [43,46].
In contrast, the following factors were associated with VH, gender [50,55,85,86,89,94], age [50,53,58,64,73,86,94], ethnicity [64], education level [50,55,70,85], religion [71], marital status [58], presence of chronic illness [62], cadre [50,58,64,71,84,93], and income level [58].
3.5. Barriers and Facilitators Affecting Vaccine Uptake among HCWs
At the intrapersonal level, three themes emerged: vaccine-related factors, COVID-19, and psychosocial factors. Within the theme of COVID-19 vaccines, ten sub-themes were identified, all acting as barriers to vaccine uptake. The most prominent sub-theme was safety concerns, which was reported as the primary barrier [23,25,43,47,50,51,55,56,57,60,61,65,66,67,68,69,70,72,74,75,76,77,78,81,82,83,84,85,86,88,90,91,92,95]. However, only three studies mentioned confidence in the COVID-19 vaccines, facilitating uptake [47,52,88]. Numerous studies [23,47,55,56,61,66,68,69,70,74,75,77,81,82,85,90,91] highlighted the prevalent mistrust in science among HCWs, often rooted in the belief that the COVID-19 vaccine has not undergone sufficient clinical trials. Concerns about the vaccine’s effectiveness were reported in 16 studies [23,25,65,67,69,70,76,77,78,82,84,85,86,88,92,95], with some expressing doubts about its ability to protect against COVID-19, particularly in Africa. In contrast, only one study reported that the vaccine was effective against COVID-19 [74]. Three studies mentioned that HCWs preferred alternative treatments to the COVID-19 vaccine, such as hydroxychloroquine, azithromycin, and ivermectin [61,81,94]. The subsequent studies reported on other COVID-19 vaccine-related barriers, which included poor vaccine knowledge [66], negative perceptions toward the vaccine [43], preference for waiting for another type of vaccine [70], and not considering the vaccine a priority [70]. Vaccine safety, mistrust in science, and efficacy were major concerns among HCWs within this theme. The following study [95] reported barriers to the uptake of the second vaccine dose, such as discomfort during the first dose and the belief that sufficient immunity had already been acquired.
The second theme in this level was COVID-19, with four sub-themes identified. The perception of susceptibility to contracting COVID-19 among HCWs was mentioned as both a barrier and a facilitator for vaccine uptake. HCWs who perceived themselves to be at a higher risk of contracting COVID-19 [25,47,59,63,88,92] were more willing to get vaccinated compared to those who perceived themselves to have a low risk [23,66,67,78,91]. HCWs who believed they needed the vaccine for protection were more likely to get vaccinated than those who relied on their immune system to prevent infection [65,68,76,77,95]. A prior diagnosis of COVID-19 was mentioned as a barrier to vaccine uptake as some HCWs believed that they had gained natural immunity and did not need the vaccine [23,67,91,92]. Side effects of COVID-19, such as loss of smell and taste, were mentioned as facilitators for vaccine uptake [56].
The final sub-theme at this level was psychosocial factors, which are individual factors that affect vaccine uptake. In separate studies, HCWs with pre-existing health conditions were mentioned as barriers and facilitators [56,59]. Female HCWs planning to conceive were less likely to get vaccinated [67,70,91]. Religious beliefs also played a role as a barrier, with Christian HCWs expressing concerns about the vaccine containing the mark of the beast [55,56,61,66,70,81,95]. Other barriers to uptake at this level included prior adverse reactions to vaccines [23,61], fear of needles and injections [70], and opposition to vaccinations in general [91].
At the interpersonal level, a significant factor relating to influences was discovered. HCWs reported that their relationships with colleagues played a role in encouraging vaccine uptake [63]. HCWs mentioned that their colleagues influenced their decision to get vaccinated. The connection between HCWs and their families also emerged as a crucial sub-theme. The desire to protect their loved ones motivated HCWs to receive the COVID-19 vaccine, as mentioned in eight studies [25,60,72,78,84,88,91,92].
Moreover, one study found that HCWs who had experienced the loss of a loved one due to COVID-19 were more likely to get vaccinated [55]. Within this theme, two barriers were identified. In one study, HCWs expressed the need for permission from their families before getting the COVID-19 vaccine [70]. In another study, HCWs reported facing disapproval from their families regarding the COVID-19 vaccine [66]. The last sub-theme explored religious leaders’ influences on HCWs, indicating that discouragement from religious leaders also acted as a barrier [66].
At the institutional level, there are significant challenges in the environmental structures. One identified barrier is the lack of trust in stakeholders, such as government and pharmaceutical companies [25,43,56,57,68,81,90]. Furthermore, a study [66] found that some HCWs would refuse the vaccine because government officials themselves did not accept it. The accessibility of the vaccine was mentioned as a barrier in four studies [63,65,70,75]. In contrast, one study suggested that the easy availability of the COVID-19 vaccine could be a reason for its uptake [63]. The workplace environment of HCWs also influences vaccine uptake. Lack of support from employers was identified as a barrier, leading HCWs to reject the vaccine [66]. Conversely, another study revealed that some HCWs felt compelled to accept the COVID-19 vaccine to continue working, per their company’s policy [91].
At the community level, a prevailing theme was centred around shared norms and myths. Within this overarching theme, three sub-themes were identified. Multiple studies [52,78,91,92] emphasized that HCWs viewed the uptake of the COVID-19 vaccine as a crucial public health responsibility for ending the pandemic. However, specific barriers to vaccine uptake were also identified. Several studies [23,25,57,61,63,67,70,78] observed that limited access to reliable information hindered the willingness of HCWs to receive the vaccine. Social media emerged as a significant influencer, with seven studies [57,60,63,68,70,72,90] reporting that HCWs subscribed to misinformation or conspiracy theories. These theories included beliefs that the vaccine was intentionally designed to cause harm to people in Africa, sterilize the African population, or even cause COVID-19.
At the policy level, an important theme that emerged was the implementation of COVID-19 policies. Within this theme, two specific sub-themes were identified. The first sub-theme focused on strategies to encourage HCWs to get vaccinated. It was supported by three studies, which highlighted that HCWs would be required to receive the vaccine to travel in the future [47,60,63]. Additionally, two studies indicated that HCWs are willing to accept the COVID-19 vaccine because it is free of charge [74,88]. However, it is worth noting that there is also a barrier at this level. This barrier stems from mandatory vaccination policies, which make HCWs feel coerced into accepting the vaccines [82,89]. HCWs believe they lack control over their health-related behaviours and refuse to be controlled by others, resulting in their rejection of the COVID-19 vaccine. Table 4 summarizes the factors influencing vaccine uptake.
Table 4.
Factors influencing vaccine uptake.
| Table | Factors | Barriers | Facilitators |
|---|---|---|---|
| Intrapersonal Level | |||
| Vaccine related factors | Vaccine safety | Safety concerns [23,25,33,48,50,51,55,56,57,60,61,65,66,67,68,69,70,72,74,75,76,77,78,81,82,83,84,85,86,88,91,92,95] | Confident in the COVID-19 vaccines [47,52,88] |
| Vaccine efficacy | Concerns about the effectiveness of the vaccine [23,25,65,67,69,70,76,77,78,82,84,85,86,88,92,95] | Belief that the vaccine is effective in protecting against COVID-19 [74] | |
| Vaccine knowledge | Having poor knowledge [66] | ||
| Vaccine perception | Having a negative perception [43] | ||
| Vaccine preference | Prefer to wait for another type of COVID-19 vaccine [70] | ||
| Vaccine necessity | Not a priority [70] | ||
| Vaccine experiences | Experiences of discomfort while receiving the first dose [95] | ||
| Vaccine immunity against COVID-19 | Sufficient immunity with the first dose [95] | ||
| Vaccine vs. alternative treatment | Preferred alternative treatment to the COVID-19 vaccine [61,81,95] | ||
| Vaccine development | Mistrust in science [23,47,55,56,61,66,68,69,70,74,75,77,81,82,85,90,91] | ||
| COVID-19 | Diagnosis of COVID | Prior diagnosis [23,67,91,92] | |
| Susceptibility of contracting COVID | Low perceived susceptibility [23,66,67,78,91] | High perceived susceptibility [25,47,59,63,87,92] | |
| Side-effects of COVID | Previous history of loss of smell & taste [56] | ||
| Protection against COVID | Belief in one’s immune system [65,68,76,77,95] | Requires the vaccine to protect oneself [60,72,74,78,84,88,91] | |
| Psychosocial factors | Chronic illness | Presence of chronic illness [56] | Presence of chronic illness [59] |
| Family planning | Planning pregnancy [67,70,91] | ||
| Religion | Religious beliefs [55,56,61,66,70,81,95] | ||
| Experiences with vaccines | Prior adverse reactions to vaccines [2,61] | ||
| Fear of needles & injections [70] | |||
| Against vaccinations in general [91] | |||
| Interpersonal Level | |||
| Influences | Relationship with colleagues | Being influenced by colleagues [63] | |
| Relationship with family | Requires permission from their family before taking the COVID-19 vaccine [70] | ||
| Disapproval from family [66] | |||
| Desire to protect loved ones [25,60,72,78,84,88,91,92] | |||
| Loss of someone to COVID-19 [55] | |||
| Relationship with religious leaders | Discouragement from Religious leaders [66] | ||
| Organizational Level | |||
| Institutional structures | Government & stakeholders | Lack of trust [25,43,56,57,68,81,90] | |
| Government officials not accepting vaccine uptake [66] | |||
| Vaccine accessibility | COVID-19 vaccine inaccessible [63,65,70,75] | COVID-19 vaccine accessible [63] | |
| Workplace environment | Company policy | To keep working [91] | |
| Leadership & support | Lack of support by employer [66] | ||
| Community Level | |||
| Shared norms & myths | Public health responsibility | To end the pandemic [52,78,91,92] | |
| Access to information | Lack of information [23,25,57,61,63,67,70,78] | ||
| Social media | Subscribing to misinformation or conspiracies [57,60,63,68,70,72,90] | ||
| Policy Level | |||
| Vaccination policies | Travel requirements | Requires the vaccine for future travel [47,60,63] | |
| Vaccination cost | Vaccines are provided free of charge [74,88] | ||
| Mandatory policies | Feeling coerced into accepting vaccines [82,89] | ||
4. Discussion
VH and refusal continue to jeopardize COVID-19 vaccination coverage in LMICs [23]. The fight against COVID-19 requires widespread vaccination uptake and acceptance [96]. In this review, 53 articles were selected and analysed, focusing on the intention, socio-demographical determinants, and factors influencing vaccine uptake. In this review, most studies were conducted in Ethiopia and Nigeria. The intention to take the COVID-19 vaccine is a challenge globally. We found that the proportion of HCWs who intend to take the COVID-19 vaccine was unsatisfactory (52%), with the intention rate ranging from 21% to 90.1%. This finding aligns with a global review by Li and colleagues [97] and Ghare and colleagues [98], who found similar acceptance rates among HCWs ranging from 27.7% to 77.3% and 30% to 98.9% (respectively). HCWs in Africa, particularly in countries such as Egypt, Uganda, and the DRC, seem hesitant about the uptake of the COVID-19 vaccination.
The results pertaining to VH in the studies are likely to be influenced to some extent by the timing of various Information, Education, and Communication (IEC) interventions within the different African countries and vaccine availability at the time of the respective studies. It should also be considered that despite the timing of the studies and vaccine availability in the respective African countries, research findings on vaccine side effects are likely to have played and continue to play a role in VH in particular African countries [99]. Furthermore, as outlined earlier, the previous negative experiences of many African countries with vaccines impact views about the desirability and safety of vaccines [100].
A better understanding of the factors influencing the uptake of COVID-19 vaccines is required to improve vaccine acceptance. Accordingly, this review was conducted using the SEM, which identified several factors that influence the uptake of COVID-19 vaccines. These factors were classified into five levels: intrapersonal, interpersonal, organizational, community, and policy. We found that socio-demographic determinants (intrapersonal level factors) were associated with COVID-19 vaccination. Li and colleagues’ [97] systematic review and Ghare and colleagues’ review [98] aligns with the findings of this scoping review. Socio-demographic determinants associated with COVID-19 vaccine uptake included being male, older age, physician, level of education, and presence of chronic illness. Studies have identified gender differences as a significant cause of VH in low-income countries [56,101]. VA was found to be significantly associated with gender, and specifically the male gender. Naidoo and colleagues’ [102] review reported that men were more accepting of the COVID-19 vaccines among the general African population. This finding is highly noteworthy in African society, where men make most family decisions, regardless of profession or social status [56]. In this review, we found that women were more likely than men to reject the COVID-19 vaccine. While Saied and colleagues [84] noticed that HCWs’ age could explain the difference in uptake; older HCWs appear more accepting due to the prevalence of co-morbidities and a high perceived susceptibility to contracting COVID [99].
Using the SEM, we have identified significant barriers within the five levels. Prominent individual-level barriers include vaccine safety and efficacy concerns and HCWs’ mistrust of science. Contrary to common assumptions that HCWs would have a positive attitude toward COVID-19 vaccines because of their expertise, Verger and colleagues [103] and El-Sokkary and colleagues [46] point out that HCWs are not a homogeneous group and that the vast majority are not immunization experts. Various information sources shape the general public’s vaccine knowledge, influencing vaccination attitudes, perceptions, and uptake [104]. Many studies have shown that individuals who lack adequate knowledge about vaccines or vaccine-preventable diseases (VPDs) are more prone to harbour a negative attitude towards vaccination [105,106]. The development of COVID-19 vaccines exposed a lack of knowledge in immunology among HCWs [46]. Two studies [25,81] cited that HCWs preferred using alternative treatments over accepting the COVID-19 vaccine. According to Oriji and colleagues [81], some (17%) respondents have already taken Hydroxychloroquine and Azithromycin as prophylaxis treatment for COVID-19. Allagoa and colleagues [56] and Oriji and colleagues [81] reported that most respondents who received the COVID-19 vaccine preferred a single-dose vaccine. The number of vaccine doses may have a negative impact on vaccination uptake. Religious beliefs were among the factors associated with vaccine refusal. Studies reviewed [55,56,81] discovered that those of Christian faith were more risk-averse regarding the uptake of the COVID-19 vaccines. However, fatalistic ideas combined with religious beliefs have been found to facilitate questioning about the efficacy of COVID-19 vaccines and that religious fatalism negatively impacts the acceptance of the SARS-CoV-2 vaccine [107].
Misinformation, primarily spread through social media, has fostered distrust in government officials, regulatory agencies, and pharmaceutical companies [102]. The media, particularly social media, has been a significant source of speculation and misinformation about the pandemic and COVID-19 vaccines [108]. According to some HCWs, the media has exaggerated the severity of the side effects of the vaccines [108]. HCWs are a trustworthy source of health information. Their acceptance or rejection of COVID-19 vaccines may impact the broader population’s acceptance and uptake of COVID-19 vaccines [23]. The low intention rate is due to the rapid development of COVID-19 vaccines, concerns about the vaccines’ safety and effectiveness, and cultural and social norms.
On a positive note, our review also identified facilitators at each level. At the intrapersonal level, HCWs’ high perceived susceptibility to COVID-19 and the desire to protect themselves were prominent factors. The African concept of ubuntu, which emphasizes interconnectedness and collective responsibility, influenced COVID-19 vaccine uptake at the interpersonal and community levels. HCWs were eager to receive the vaccine to protect their loved ones and saw it as a public responsibility to end the pandemic.
Governments, public health agencies, and private healthcare systems should collaborate in making educational resources available to inform HCWs about the vaccine’s safety, importance, and the negative consequences of refusing or delaying vaccination [69]. Most studies emphasized how crucial it is for stakeholders to inform and increase HCW awareness of COVID-19 vaccines. It is now up to various stakeholders and policymakers to take effective action to spread as much knowledge as possible among HCWs to increase vaccine acceptance and, thereby, address the pandemic’s detrimental effects on healthcare systems and socio-economic conditions. When tailored education campaigns are targeted to specific attitudes, beliefs, and experiences, they are beneficial [100]. The findings from this review will assist in the roll-out of other vaccination programmes.
Strengths and Limitations
The majority of articles reviewed adopted a quantitative approach. The present review investigates factors influencing HCWs’ intention and uptake of COVID-19 vaccines. Limitations are inherent in a scoping review approach. Some limitations should be considered in this review. This review did not undertake a quality or risk assessment bias of the included studies. Only studies published in English were considered. There is a bias in the body of literature towards VH. Due to the heterogeneity in the definition and assessment of VH in different studies, not all studies reported VH rates among HCWs. In some studies, the measurement scales used to assess the intention to uptake and VH rates for COVID-19 vaccines were either dichotomous or Likert. The varied sample size would be attributed to selection bias in studies focusing on HCWs. Social desirability on self-reported VH among the HCWs can also not be ruled out. At the time of data collection, some studies did not receive the COVID-19 vaccine. Therefore, intentions and VH may have influenced participants’ responses. The trends in acceptance might have changed after the vaccination programmes were implemented.
5. Conclusions
Preventive measures are essential to the global effort to mitigate the pandemic’s consequences. As a result, enormous resources have been dedicated to developing effective and safe COVID-19 vaccines. Using the SEM, this review explored various factors affecting the uptake, allowing for a more comprehensive understanding of vaccine uptake and the development of effective interventions. VI and VH rates vary greatly across countries or regions within the same country. Furthermore, the VI and VH rate is influenced by various factors. Most studies reviewed found significant barriers that affected vaccine uptake on the African continent among HCWs, resulting in a subpar intention to use COVID-19 vaccines. The low level of trust in COVID-19 vaccines and the concerns about the long-term efficacy of the vaccines, as well as the possible long-term side effects associated with the vaccine uptake, play a role in decision-making regarding vaccination. HCWs are influential in informing the general public about vaccines. Therefore, it is crucial to prioritize engagement with key stakeholders to address HCWs’ negative perceptions about vaccines and where they exist in efforts to increase vaccine uptake.
To improve vaccine uptake using the SEM, interventions should target multiple levels simultaneously. At an individual level, understand their concerns and reasons for hesitancy. Provide accurate information to address myths and misconceptions by implementing strategies addressing knowledge gaps and building trust among HCWs. At an organizational level, healthcare facilities should prioritize vaccination by educating staff, offering paid time off for vaccination and side effects, improving access by getting vaccinated as quickly and conveniently as possible, and incentivizing vaccination. They set the culture—if the leadership gets vaccinated, others will follow and leverage social networks and community influencers can have a synergistic effect on increasing vaccine acceptance and uptake. By considering the various levels of influence, the SEM provides a comprehensive framework for understanding and addressing VH and holistically promoting vaccine uptake.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11091491/s1, Supplementary Materials S1: PRISMA-ScR-Fillable-Checklist—HCWs.
Appendix A. Search Strategy
Table A1.
WorldCat Discovery search strategy.
| Search Terms | Filters | Results |
|---|---|---|
| kw: COVID-19 vaccine AND | Format: Article | 16 |
| kw: Vaccine Hesitancy AND | ||
| kw: Vaccine acceptance AND | Language: English | |
| kw: Africa AND | ||
| kw: Healthcare workers | Publication Year: 2020–2023 |
Table A2.
PubMed search strategy.
| Search Number | Query | Filters | Search Details | Results | Time |
|---|---|---|---|---|---|
| 10 | ((((((COVID-19 vaccines[MeSH Terms]) AND (COVID-19)) AND (vaccines)) OR (covid vaccines)) OR (intention)) OR (vaccine hesitancy)) AND (vaccine acceptance) AND (healthcare workers) AND (Africa) | Full text, Humans, English, from 2020–2023 | (((“covid 19 vaccines” [MeSH Terms] AND (“covid 19” [All Fields] OR “covid 19” [MeSH Terms] OR “covid 19 vaccines” [All Fields] OR “covid 19 vaccines” [MeSH Terms] OR “covid 19 serotherapy” [All Fields] OR “covid 19 nucleic acid testing” [All Fields] OR “covid 19 nucleic acid testing” [MeSH Terms] OR “covid 19 serological testing” [All Fields] OR “covid 19 serological testing” [MeSH Terms] OR “covid 19 testing” [All Fields] OR “covid 19 testing” [MeSH Terms] OR “sars cov 2” [All Fields] OR “sars cov 2” [MeSH Terms] OR “severe acute respiratory syndrome coronavirus 2” [All Fields] OR “ncov” [All Fields] OR “2019 ncov” [All Fields] OR ((“coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] OR “cov” [All Fields]) AND 2019/11/01:3000/12/31[Date—Publication])) AND (“vaccin” [Supplementary Concept] OR “vaccin” [All Fields] OR “vaccination” [MeSH Terms] OR “vaccination” [All Fields] OR “vaccinable” [All Fields] OR “vaccinal” [All Fields] OR “vaccinate” [All Fields] OR “vaccinated” [All Fields] OR “vaccinates” [All Fields] OR “vaccinating” [All Fields] OR “vaccinations” [All Fields] OR “vaccinations” [All Fields] OR “vaccinator” [All Fields] OR “vaccinators” [All Fields] OR “vaccines” [All Fields] OR “vaccined” [All Fields] OR “vaccines” [MeSH Terms] OR “vaccines” [All Fields] OR “vaccine” [All Fields] OR “vaccins” [All Fields])) OR ((“sars cov 2” [MeSH Terms] OR “sars cov 2” [All Fields] OR “covid” [All Fields] OR “covid 19” [MeSH Terms] OR “covid 19” [All Fields]) AND (“vaccin” [Supplementary Concept] OR “vaccin” [All Fields] OR “vaccination” [MeSH Terms] OR “vaccination” [All Fields] OR “vaccinable” [All Fields] OR “vaccinal” [All Fields] OR “vaccinate” [All Fields] OR “vaccinated” [All Fields] OR “vaccinates” [All Fields] OR “vaccinating” [All Fields] OR “vaccinations” [All Fields] OR “vaccinations” [All Fields] OR “vaccinator” [All Fields] OR “vaccinators” [All Fields] OR “vaccines” [All Fields] OR “vaccined” [All Fields] OR “vaccines” [MeSH Terms] OR “vaccines” [All Fields] OR “vaccine” [All Fields] OR “vaccins” [All Fields])) OR (“intention” [MeSH Terms] OR “intention” [All Fields] OR “intent” [All Fields] OR “intentions” [All Fields] OR “intentional” [All Fields] OR “intentioned” [All Fields] OR “intents” [All Fields]) OR (“vaccination hesitancy” [MeSH Terms] OR (“vaccination” [All Fields] AND “hesitancy” [All Fields]) OR “vaccination hesitancy” [All Fields] OR (“vaccine” [All Fields] AND “hesitancy” [All Fields]) OR “vaccine hesitancy” [All Fields])) AND ((“vaccin” [Supplementary Concept] OR “vaccin” [All Fields] OR “vaccination” [MeSH Terms] OR “vaccination” [All Fields] OR “vaccinable” [All Fields] OR “vaccinal” [All Fields] OR “vaccinate” [All Fields] OR “vaccinated” [All Fields] OR “vaccinates” [All Fields] OR “vaccinating” [All Fields] OR “vaccinations” [All Fields] OR “vaccinations” [All Fields] OR “vaccinator” [All Fields] OR “vaccinators” [All Fields] OR “vaccines” [All Fields] OR “vaccined” [All Fields] OR “vaccines” [MeSH Terms] OR “vaccines” [All Fields] OR “vaccine” [All Fields] OR “vaccins” [All Fields]) AND (“accept” [All Fields] OR “acceptabilities” [All Fields] OR “acceptability” [All Fields] OR “acceptable” [All Fields] OR “acceptably” [All Fields] OR “acceptance” [All Fields] OR “acceptances” [All Fields] OR “acceptation” [All Fields] OR “accepted” [All Fields] OR “accepter” [All Fields] OR “accepters” [All Fields] OR “accepting” [All Fields] OR “accepts” [All Fields])) AND (“health personnel” [MeSH Terms] OR (“health” [All Fields] AND “personnel” [All Fields]) OR “health personnel” [All Fields] OR (“healthcare” [All Fields] AND “workers” [All Fields]) OR “healthcare workers” [All Fields]) AND (“africa” [MeSH Terms] OR “africa” [All Fields] OR “africa s” [All Fields] OR “africas” [All Fields])) AND ((fft[Filter]) AND (humans[Filter]) AND (english[Filter]) AND (2020:2023[pdat])) | 41 | 9:28:21 |
Table A3.
ProQuest search strategy.
| Set No. | Searched for | Databases | Results |
|---|---|---|---|
| S9 | ((factors associated with covid- 19 vaccine hesitancy among HCWs in Africa) AND (location.exact(“Africa” OR “South Africa” OR “Nigeria” OR “Ethiopia” OR “Egypt” OR “Ghana” OR “Uganda” OR “Central Africa” OR “North Africa” OR “Sierra Leone” OR “West Africa” OR “Zambia” OR “Zimbabwe” OR “Burkina Faso” OR “Cape Town South Africa” OR “Congo-Democratic Republic of Congo” OR “East Africa” OR “Eastern Cape South Africa” OR “Kano Nigeria” OR “Kenya” OR “Malawi” OR “Mozambique”) AND at.exact(“Article”) AND la.exact(“ENG”) AND PEER(yes))) AND ((factors associated with covid-19 vaccine uptake among HCWs in Africa) AND (location.exact(“Africa” OR “South Africa” OR “Nigeria” OR “Ethiopia” OR “Egypt” OR “Ghana” OR “Uganda” OR “Central Africa” OR “North Africa” OR “Sierra Leone” OR “West Africa” OR “Zambia” OR “Zimbabwe” OR “Burkina Faso” OR “Cape Town South Africa” OR “Congo-Democratic Republic of Congo” OR “East Africa” OR “Eastern Cape South Africa” OR “Kano Nigeria” OR “Kenya” OR “Malawi” OR “Mozambique”) AND at.exact(“Article”) AND la.exact(“ENG”) AND PEER(yes))) |
Coronavirus Research Database, Ebook Central, Health Research Premium Collection, Publicly Available Content Database These databases are searched for part of your query. |
48 |
Appendix B
Table A4.
Included Study Characteristics.
| Author(s) & Publication Year |
Country & Data Collection Period |
Methodology |
|---|---|---|
| Adane et al., 2022 [51] |
Ethiopia May 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Medical Laboratory Technicians Nurses & Midwives Pharmacists Radiologists Anaesthesiologists Public Health Specialist Non-medical Auxiliary Staff Sample size: 404 Measurement scale: Likert scale |
| Adejumo et al., 2021 [49] |
Nigeria October 2020 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses Medical Laboratory Technicians Pharmacists Physiotherapists Other Sample size: 1470 Measurement scale: Dichotomous scale |
| Adeniyi et al., 2021 [52] |
South Africa November to December 2020 |
Study design: A quantitative cross-sectional study Population target: Physicians Pharmacists Nurses Allied Health Professionals Support Staff Sample size: 1380 Measurement scale: Dichotomous scale |
| Aemro et al., 2021 [53] |
Ethiopia May to June 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Pharmacists Nurses Allied Health Professionals Support Staff Sample size: 418 Measurement scale: Dichotomous scale |
| Agyekum et al., 2021 [23] |
Ghana January to February 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Allied Health Professionals Physicians Sample size: 234 Measurement scale: Dichotomous scale |
| Ahmed et al., 2021 [54] |
Ethiopia January to March 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Psychiatrists Optometrists Physicians Health Officers Anaesthetics Medical Laboratory Technicians Radiologists Physiotherapists Pharmacists Other Sample size: 409 Measurement scale: Dichotomous scale |
| Alhassan et al., 2021 [55] |
Ghana September to October 2020 |
Study design: A quantitative cross-sectional study Population target: Pharmacists Other Sample size: 1605 Measurement scale: Dichotomous scale |
| Allagoa et al., 2021 [56] |
Nigeria April 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Sample size: 182 Measurement scale: Dichotomous scale |
| Amour et al., 2023 [57] |
Tanzania October to November 2021 |
Study design: A mixed-method study Population target: Physicians Nurses & Midwives Pharmacists Medical Laboratory Technicians Administrative Staff Other Sample size: 1368 |
| Amuzie et al., 2021 [58] |
Nigeria March 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses Pharmacists Medical Laboratory Technicians Administrative Staff Allied Health Professionals Sample size: 422 Measurement scale: Dichotomous scale |
| Angelo et al., 2021 [59] |
Ethiopia March 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses & Midwives Medical Laboratory Technicians Pharmacist Sample size: 405 Measurement scale: Dichotomous scale |
| Annan et al., 2021 [60] |
Ghana |
Study design: A quantitative cross-sectional study Population target: Junior Physicians Sample size: 305 Measurement scale: Dichotomous scale |
| Asefa et al., 2023 [61] |
Ethiopia July to August 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Pharmacists Sample size: 421 Measurement scale: Dichotomous scale |
| Aseneh et al., 2023 [62] |
Multiple countries Cameroon & Nigeria May to June 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses & Midwives Administrative Staff Paramedics Pharmacists CHWs Dentists Medical Laboratory Technicians Nurse Assistants Public Health Specialist Physiotherapists Radiologists Other Sample size: 598 Measurement scale: Dichotomous scale |
| Ashipala et al., 2023 [63] |
Namibia September to October 2021 |
Study design: A qualitative study Population target: Nurses Sample size: 15 |
| Berhe et al., 2022 [64] |
Ethiopia July 2022 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Pharmacist Psychiatrist Environmental Health Specialist Public Health Specialist Others Sample size: 403 Measurement scale: Dichotomous scale |
| Dahie et al., 2022 [65] |
Somalia December 2021 to February 2022 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Public Health Specialist Dentist Pharmacist CHWs Nutritionists Other Sample size: 1281 Measurement scale: Dichotomous scale |
| Ekwebene et al., 2021 [66] |
Nigeria |
Study design: A quantitative cross-sectional study Population target Physicians Nurses Public Health Specialist Radiologist Dentists Optometrist Medical Laboratory Technicians Pharmacists Physiotherapist Cleaners Sample size: 445 Measurement scale: Dichotomous scale |
| El-Ghitany et al., 2022 [67] |
Egypt January to June 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses Pharmacist Other Sample size: 2919 Measurement scale: Dichotomous scale |
| El-Sokkary et al., 2021 [46] |
Egypt January 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Dentists Pharmacists Others Sample size: 308 Measurement scale: Likert scale |
| Fares et al., 2021 [47] |
Egypt December 2020 to January 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses Pharmacists Dentists Physiotherapists Sample size: 385 Measurement scale: Likert scale |
| George et al., 2023 [68] |
South Africa August to October 2022 |
Study design: A mixed-method study Population target: Nurses Physicians Allied Health Professionals Dentists/Dental Hygienists Paramedics Pharmacists Sample size: 7763 Measurement scale: Dichotomous scale |
| Guangul et al., 2021 [69] |
Ethiopia |
Study design: A quantitative cross-sectional study Population target: Health Officer/Clinical officer Medical Laboratory Technicians Nurses Pharmacists Physicians Other Sample size: 668 Measurement scale: Dichotomous scale |
| Ibrahim et al., 2023 [70] |
Somalia February to March 2022 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Radiologists Medical Laboratory Technicians Sample size: 1476 Measurement scale: Dichotomous scale |
| Iwu et al., 2022 [71] |
Nigeria September to October 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Pharmacists Sample size: 347 Measurement scale: Dichotomous scale |
| Kanyike et al., 2021 [72] |
Uganda March 2021 |
Study design: A quantitative cross-sectional study Population target: Medical students Sample size: 600 Measurement scale: Dichotomous scale |
| Mohammed et al., 2021 [73] |
Ethiopia March to July 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Anaesthetic Technicians Pharmacists Radiologists Sample size: 614 Measurement scale: Dichotomous scale |
| Mohammed et al., 2023 [74] |
Ghana |
Study design: A quantitative cross-sectional study Population target: Physicians Allied Health Professionals Auxiliary Employees Sample size: 424 Measurement scale: Dichotomous scale |
| Moucheraud et al., 2022 [75] |
Malawi March to May 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Medical Assistants Nurses HIV Diagnostic Assistants Health Surveillance Assistants Patient Supporter Data Clerks Sample size: 400 Measurement scale: Dichotomous scale |
| Mudenda et al., 2022 [76] |
Zambia February to April 2021 |
Study design: A quantitative cross-sectional study Population target: Pharmacy students Sample size: 326 Measurement scale: Dichotomous scale |
| Ngasa et al., 2021 [77] |
Cameroon April to June 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Medical Students Nurses Medical Laboratory Technicians Public Health Specialist Pharmacists Sample size: 371 Measurement scale: Dichotomous scale |
| Niguse et al., 2023 [78] |
Ethiopia October to November 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Radiologists Public Health Specialist Pharmacists Sample size: 390 Measurement scale: Dichotomous scale |
| Nnaemeka et al., 2022 [79] |
Nigeria September 2021 & March 2022 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Pharmacists Medical Laboratory Technicians Radiologists Administrative Staff Physiotherapists Sample size: 1268 Measurement scale: Dichotomous scale |
| Nzaji et al., 2020 [80] |
The Democratic Republic of Congo March to April 2020 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses Other Sample size: 613 Measurement scale: Dichotomous scale |
| Oriji et al., 2021 [81] |
Nigeria April 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses Pharmacists Medical Laboratory Technicians Non-clinical officers Sample size: 182 Measurement scale: Likert scale |
| Orok et al., 2022 [25] |
Nigeria May to June 2021 |
Study design: A quantitative cross-sectional study Population target: Medical students Sample size: 233 Measurement scale: Likert scale |
| Ouni et al., 2023 [82] |
Uganda |
Study design: A mixed-method study Population target: Nurses & Midwives Physicians Environmental Health Specialist Medical Laboratory Technicians Sample size: 346 |
| Robinson et al., 2021 [83] |
Nigeria December 2020 to January 2021 |
Study design: A quantitative cross-sectional study Population target: Ancillary Support Staff Dental Technicians Physicians Medical Laboratory Technicians Medical Consultant Nurses & Midwives Optometrists Pharmacist Physiotherapists Primary Healthcare Worker Radiologists Sample size: 1094 Measurement scale: Likert scale |
| Saied et al., 2021 [84] |
Egypt January 2021 |
Study design: A quantitative cross-sectional study Population target: Medical students Sample size: 2133 Measurement scale: Likert scale |
| Sharaf et al., 2022 [85] |
Egypt August to October 2021 |
Study design: A quantitative cross-sectional study Population target: Dental teaching staff Sample size: 171 Measurement scale: Likert scale |
| Shehata et al., 2022 [86] |
Egypt March to May 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Sample size: 1268 Measurement scale: Dichotomous scale |
| Terefa et al., 2021 [87] |
Ethiopia June 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Pharmacists Anaesthetists Psychiatrist Dentists Public Health Specialist Other Sample size: 522 Measurement scale: Dichotomous scale |
| Tharwat et al., 2022 [88] |
Egypt August to September 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Administrative Staff Security Officers Radiologist Medical Laboratory Technicians Pharmacists Dentist Sample size: 455 Measurement scale: Likert scale |
| Toure et al., 2022 [43] |
Guinea March to August 2021 |
Study design: A mixed-method study Population target: General adult population & HCW Nurses & Midwives Medical Laboratory Technicians Physicians Sample size: 7210 (HCWs-3547) Measurement scale: Dichotomous scale |
| Voundi-Voundi et al., 2023 [89] |
Cameroon January to March 2022 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Administrative Staff Sample size: 360 |
| Watermeyer et al., 2022 [90] |
South Africa September to November 2021 |
Study design: A qualitative study Population target: CHW Sample size: 20 |
| Whitworth et al., 2022 [91] |
Multiple countries Sierra Leone DRC Uganda April to October 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Nurses & Midwives Clinical Support Staff Medical Laboratory Technicians Pharmacist Non-clinical support staff Sample size: 543 Measurement scale: Likert scale |
| Wiysonge et al., 2022 [48] |
South Africa March to May 2021 |
Study design: A quantitative cross-sectional study Population target: Admin Support Nurses Other HCWs Physicians Sample size: 395 Measurement scale: Likert scale |
| Yassin et al., 2022 [92] |
Sudan April 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Pharmacist Nurses Medical Laboratory Technicians Administrators Others Sample size: 400 Measurement scale: Dichotomous scale |
| Yendewa et al., 2022 [93] |
Sierra Leone January to March 2022 |
Study design: A quantitative cross-sectional study Population target: Physicians Medical Students Pharmacists Nurses Nursing Students Sample size: 592 Measurement scale: Likert scale |
| Yilma et al., 2022 [50] |
Ethiopia February to April 2021 |
Study design: A quantitative cross-sectional study Population target: Nurses & Midwives Physicians Medical Laboratory Technicians Pharmacists Cleaners Others Sample size: 1314 Measurement scale: Dichotomous scale |
| Zammit et al., 2022 [94] |
Tunisia January 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Dentists Pharmacists Paramedical professionals Sample size: 493 Measurement scale: Dichotomous scale |
| Zewude & Belachew, 2021 [95] |
Ethiopia June 2021 |
Study design: A quantitative cross-sectional study Population target: Physicians Health officer Administrative Staff Nurse Medical Laboratory Technician Pharmacist Others Sample size: 232 Measurement scale: Dichotomous scale |
Author Contributions
D.N., the first author, was responsible for the conceptualization and design of this research paper. He gathered data for the study, conducted data analysis, and authored the article. Supervised by Professor A.M.-W., who also gathered data for the study, conducted data analysis, and reviewed and provided constructive feedback. K.G. reviewed various drafts of the paper and provided feedback to the senior author. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Islam M.S., Siddique A.B., Akter R., Tasnim R., Sujan M.S., Ward P.R., Sikder M.T. Knowledge, Attitudes and Perceptions towards COVID-19 Vaccinations: A Cross-Sectional Community Survey in Bangladesh. BMC Public Health. 2021;21:1851. doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayenigbara I.O., Adegboro J.S., Ayenigbara G.O., Adeleke O.R., Olofintuyi O.O. The challenges to a successful COVID-19 vaccination programme in Africa. Germs. 2021;11:427–440. doi: 10.18683/germs.2021.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Massinga Loembé M., Nkengasong J.N. COVID-19 vaccine access in Africa: Global distribution, vaccine platforms, and challenges ahead. Immunity. 2021;54:1353–1362. doi: 10.1016/j.immuni.2021.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogunleye O.O., Godman B., Fadare J.O., Mudenda S., Adeoti A.O., Yinka-Ogunleye A.F., Ogundele S.O., Oyawole M.R., Schönfeldt M., Rashed W.M., et al. Coronavirus Disease 2019 (COVID-19) Pandemic across Africa: Current Status of Vaccinations and Implications for the Future. Vaccines. 2022;10:1553. doi: 10.3390/vaccines10091553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. AFRO Africa Steps Up Targeted COVID-19 Vaccination of Most at Risk People. [(accessed on 20 September 2022)]; Available online: https://www.afro.who.int/news/africa-steps-targeted-COVID-19-vaccination-most-risk-people.
- 6.Bongers A., Riggall G., Kokareva L., Chin B. Managing the challenges associated with decreasing demand for COVID-19 vaccination in Central and West Asia. BMJ Global Health. 2022;7:e010066. doi: 10.1136/bmjgh-2022-010066. [DOI] [Google Scholar]
- 7.Mutombo P.N., Fallah M.P., Munodawafa D., Kabel A., Houeto D., Goronga T., Mweemba O., Balance G., Onya H., Kamba R.S., et al. COVID-19 Vaccine Hesitancy in Africa: A Call to Action. Lancet Glob. Health. 2022;10:e320–e321. doi: 10.1016/S2214-109X(21)00563-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Afolabi A.A., Ilesanmi O.S. Dealing with Vaccine Hesitancy in Africa: The Prospective COVID-19 Vaccine Context. Pan Afr. Med. J. 2021;38 doi: 10.11604/pamj.2021.38.3.27401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. AFRO COVID-19 Vaccination in Africa Increases by Almost Three-Quarters in June 2022. [(accessed on 20 September 2022)]; Available online: https://www.afro.who.int/news/COVID-19-vaccination-africa-increases-almost-three-quarters-june-2022.
- 10.Privor-Dumm L., Excler J.-L., Gilbert S., Karim S.S.A., Hotez P.J., Thompson D., Kim J.H. Vaccine access, equity and justice: COVID-19 vaccines and vaccination. BMJ Glob. Health. 2023;8:e011881. doi: 10.1136/bmjgh-2023-011881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nchasi G., Okonji O.C., Jena R., Ahmad S., Soomro U., Kolawole B.O., Nawaz F.A., Essar M.Y., Aborode A.T. Challenges faced by African healthcare workers during the third wave of the pandemic. Health Sci. Rep. 2022;5:e893. doi: 10.1002/hsr2.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tessema G.A., Kinfu Y., Dachew B.A., Tesema A.G., Assefa Y., Alene K.A., Aregay A.F., Ayalew M.B., Bezabhe W.M., Bali A.G., et al. The COVID-19 Pandemic and Healthcare Systems in Africa: A Scoping Review of Preparedness, Impact and Response. BMJ Glob. Health. 2021;6:e007179. doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. AFRO COVID-19 Vaccination Roll-Out Stagnates in Africa. [(accessed on 5 November 2022)]; Available online: https://www.afro.who.int/news/COVID-19-vaccination-roll-out-stagnates-africa.
- 14.Galagali P.M., Kinikar A.A., Kumar V.S. Vaccine Hesitancy: Obstacles and Challenges. Curr. Pediatr. Rep. 2022;10:241–248. doi: 10.1007/s40124-022-00278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Njoga E.O., Awoyomi O.J., Onwumere-Idolor O.S., Awoyomi P.O., Ugochukwu I.C.I., Ozioko S.N. Persisting Vaccine Hesitancy in Africa: The Whys, Global Public Health Consequences and Ways-Out—COVID-19 Vaccination Acceptance Rates as Case-in-Point. Vaccines. 2022;10:1934. doi: 10.3390/vaccines10111934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baptista S., Naidoo S., Suliman S., Nepolo E., Kanoi B.N., Gitaka J., Blessing O.M., Enany S. COVID-19 vaccinology landscape in Africa. Front. Immunol. 2022;13:95516. doi: 10.3389/fimmu.2022.955168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubé E., MacDonald N.E. How Can a Global Pandemic Affect Vaccine Hesitancy? Expert Rev. Vaccines. 2020;19:899–901. doi: 10.1080/14760584.2020.1825944. [DOI] [PubMed] [Google Scholar]
- 19.Wang D., Chukwu A., Mwanyika-Sando M., Abubakari S.W., Assefa N., Madzorera I., Hemler E.C., Ismail A., Lankoande B., Mapendo F., et al. COVID-19 Vaccine Hesitancy and Its Determinants among Sub-Saharan African Adolescents. PLoS Glob. Public Health. 2022;2:e0000611. doi: 10.1371/journal.pgph.0000611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Persad G., Peek M.E., Emanuel E.J. Fairly Prioritizing Groups for Access to COVID-19 Vaccines. JAMA. 2020;324:1601. doi: 10.1001/jama.2020.18513. [DOI] [PubMed] [Google Scholar]
- 21.Pereira B., Fehl A.G., Finkelstein S.R., Jiga-Boy G.M., Caserotti M. Scarcity in COVID-19 vaccine supplies reduces perceived vaccination priority and increases vaccine hesitancy. Psychol. Mark. 2022;39:921–936. doi: 10.1002/mar.21629. [DOI] [Google Scholar]
- 22.World Health Organization. AFRO Only 1 in 4 African Health Workers Fully Vaccinated Against COVID-19. [(accessed on 20 September 2022)]; Available online: https://www.afro.who.int/news/only-1–4-african-health-workers-fully-vaccinated-against-COVID-19.
- 23.Agyekum M.W., Afrifa-Anane G.F., Kyei-Arthur F., Addo B. Acceptability of COVID-19 Vaccination among Health Care Workers in Ghana. Adv. Public Health. 2021;2021:9998176. doi: 10.1155/2021/9998176. [DOI] [Google Scholar]
- 24.Cooper S., Betsch C., Sambala E.Z., Mchiza N., Wiysonge C.S. Vaccine hesitancy—A potential threat to the achievements of vaccination programmes in Africa. Hum. Vaccines Immunother. 2018;14:2355–2357. doi: 10.1080/21645515.2018.1460987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orok E., Ndem E., Daniel E. Knowledge, attitude and perception of medical students on COVID-19 vaccines: A study carried out in a Nigerian University. Front. Public Health. 2022;10:942283. doi: 10.3389/fpubh.2022.942283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nwafor K.A., Samuel N., Basil-Eze P., Chika A.M., Irene N.J., Joel A., Oraeme S. Evaluation of Government Communication Interventions for Public Trust and Acceptance of the COVID-19 Astrazeneca Vaccine in Ebonyi State, Nigeria. Int. J. Public Health Pharm. Pharmacol. 2020;5:25–37. [Google Scholar]
- 27.Adongo C.A., Tuoyire D.A., Azuug M., Appiah A.B., Taale F., Amadu I. Decolonising vaccine production: Unpacking Ghanaians’ support for made-in-Africa vaccines. Vaccine X. 2023;14:100283. doi: 10.1016/j.jvacx.2023.100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Makoni M. Tanzania refuses COVID-19 vaccines. Lancet. 2021;397:566. doi: 10.1016/S0140-6736(21)00362-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamanis T., Carlitz R., Gonyea O., Skaff S., Kisanga N., Mollel H. Confronting ‘chaos’: A qualitative study assessing public health officials’ perceptions of the factors affecting Tanzania’s COVID-19 vaccine rollout. BMJ Open. 2023;13:e065081. doi: 10.1136/bmjopen-2022-065081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Jayyousi G.F., Sherbash M.A.M., Ali L.A.M., El-Heneidy A., Alhussaini N.W.Z., Elhassan M.E.A., Nazzal M.A. Factors Influencing Public Attitudes towards COVID-19 Vaccination: A Scoping Review Informed by the Socio-Ecological Model. Vaccines. 2021;9:548. doi: 10.3390/vaccines9060548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomson A., Vallée-Tourangeau G., Suggs L.S. Strategies to increase vaccine acceptance and uptake: From behavioral insights to context-specific, culturally-appropriate, evidence-based communications and interventions. Vaccine. 2018;36:6457–6458. doi: 10.1016/j.vaccine.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald N.E., Comeau J., Dubé È., Graham J., Greenwood M., Harmon S., McElhaney J., McMurtry M.C., Middleton A., Steenbeek A., et al. Royal society of Canada COVID-19 report: Enhancing COVID-19 vaccine acceptance in Canada. Facets. 2021;6:184–246. doi: 10.1139/facets-2021-0037. [DOI] [Google Scholar]
- 33.Mills M., Rahal C., Brazel D., Yan J., Gieysztor S. COVID-19 Vaccine Deployment: Behaviour, Ethics, Misinformation and Policy Strategies. The Royal Society & The British Academy; London, UK: 2020. [Google Scholar]
- 34.Kilanowski J.F. Breadth of the socio-ecological model. J. Agromed. 2017;22:295–297. doi: 10.1080/1059924X.2017.1358971. [DOI] [PubMed] [Google Scholar]
- 35.Rimer B.K., Glanz K. Theory at a Glance: A Guide for Health Promotion Practice. National Cancer Institute; Bethesda, MD, USA: Department of Health and Human Services, National Institutes of Health; Bethesda, MD, USA: 2005. [Google Scholar]
- 36.Ackah M., Ameyaw L., Salifu M.G., Asubonteng D.P.A., Yeboah C.O., Annor E.N., Ankapong E.a.K., Boakye H. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS ONE. 2022;17:e0268711. doi: 10.1371/journal.pone.0268711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arksey H., O’Malley L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 38.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. Prisma Extension for Scoping Reviews (PRISMA-SCR): Checklist and Explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization Classifying Health Workers. [(accessed on 23 August 2023)]; Available online: https://www.who.int/publications/m/item/classifying-health-workers.
- 40.Lisy K., Porritt K. Narrative Synthesis: Considerations and challenges. Int. J. Evid. Based Healthc. 2016;14:201. doi: 10.1097/01.XEB.0000511348.97198.8c. [DOI] [Google Scholar]
- 41.Braun V., Clarke V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 42.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Toure A.A., Traore F.A., Camara G., Magassouba A.S., Barry I., Kourouma M.L., Sylla Y., Conte N.Y., Cisse D., Dioubaté N., et al. Facilitators and Barriers to COVID-19 Vaccination among Healthcare Workers and the General Population in Guinea. BMC Infect. Dis. 2022;22:e1000097. doi: 10.1186/s12879-022-07742-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burrell N.A., DeAnne P., editors. The SAGE Encyclopedia of Communication Research Methods. Four Volume Set; SAGE Publications, Inc.; Thousand Oaks, CA, USA: 2017. [Google Scholar]
- 45.Bhandari P., Nikolopoulou K. What Is a Likert Scale? Guide & Examples. [(accessed on 1 April 2023)]. Available online: https://www.scribbr.com/methodology/likert-scale/
- 46.El-Sokkary R.H., El Seifi O.S., Hassan H.M., Mortada E.M., Hashem M.K., Gadelrab M.R., Tash R.M. Predictors of COVID-19 Vaccine Hesitancy among Egyptian Healthcare Workers: A Cross-Sectional Study. BMC Infect. Dis. 2021;21:762. doi: 10.1186/s12879-021-06392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fares S., Elmnyer M.M., Mohamed S.S., Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J. Prim. Care Community Health. 2021;12:215013272110133. doi: 10.1177/21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wiysonge C.S., Alobwede S.M., de Marie C., Katoto P., Kidzeru E.B., Lumngwena E.N., Cooper S., Goliath R., Jackson A., Shey M.S. COVID-19 Vaccine Acceptance and Hesitancy among Healthcare Workers in South Africa. Expert Rev. Vaccines. 2022;21:549–559. doi: 10.1080/14760584.2022.2023355. [DOI] [PubMed] [Google Scholar]
- 49.Adejumo O.A., Ogundele O.A., Madubuko C.R., Oluwafemi R.O., Okoye O.C., Okonkwo K.C., Owolade S.S., Junaid O.A., Lawal O.M., Enikuomehin A.C., et al. Perceptions of the COVID-19 Vaccine and Willingness to Receive Vaccination among Health Workers in Nigeria. Osong Public Health Res. Perspect. 2021;12:236. doi: 10.24171/j.phrp.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yilma D., Mohammed R., Abdela S.G., Enbiale W., Seifu F., Pareyn M., Liesenborghs L., van Griensven J., van Henten S. COVID-19 Vaccine Acceptability among Healthcare Workers in Ethiopia: Do We Practice What We Preach? Trop. Med. Int. Health. 2022;27:418–425. doi: 10.1111/tmi.13742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adane M., Ademas A., Kloos H. Knowledge, Attitudes, and Perceptions of COVID-19 Vaccine and Refusal to Receive COVID-19 Vaccine among Healthcare Workers in Northeastern Ethiopia. BMC Public Health. 2022;22:128. doi: 10.1186/s12889-021-12362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adeniyi O.V., Stead D., Singata-Madliki M., Batting J., Wright M., Jelliman E., Abrahams S., Parrish A. Acceptance of COVID-19 Vaccine among the Healthcare Workers in the Eastern Cape, South Africa: A Cross Sectional Study. Vaccines. 2021;9:666. doi: 10.3390/vaccines9060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aemro A., Amare N.S., Shetie B., Demilew B.C., Wassie M. Determinants of COVID-19 vaccine hesitancy among health care workers in Amhara region referral hospitals, Northwest Ethiopia: A cross-sectional study. Epidemiol. Infect. 2021;149:e225. doi: 10.1017/S0950268821002259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmed M.H., Kanfe S.G., Jarso M. Intention to receive vaccine against COVID-19 and associated factors among health professionals working at public hospitals in resource limited settings. PLoS ONE. 2021;16:e0254391. doi: 10.1371/journal.pone.0254391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alhassan R.K., Owusu-Agyei S., Ansah E.K., Gyapong M. COVID-19 Vaccine Uptake among Health Care Workers in Ghana: A Case for Targeted Vaccine Deployment Campaigns in the Global South. Hum. Resour. Health. 2021;19:136. doi: 10.1186/s12960-021-00657-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Allagoa D.O., Oriji P.C., Oguche O.I., Ozori S.E., Tekenah E.S., Obagah L. Acceptance of COVID-19 vaccination among doctors in the Federal Medical Centre, Yenagoa, South-South, Nigeria. IOSR J. Dent. Med. Sci. 2021;20:60–67. [Google Scholar]
- 57.Amour M.A., Mboya I.B., Ndumwa H.P., Kengia J.T., Metta E., Njiro B.J., Nyamuryekung’e K.K., Mhamilawa L.E., Shayo E.H., Ngalesoni F., et al. Determinants of COVID-19 Vaccine Uptake and Hesitancy among Healthcare Workers in Tanzania: A Mixed-Methods Study. COVID. 2023;3:777–791. doi: 10.3390/covid3050058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Amuzie C.I., Odini F., Kalu K.N., Izuka M.O., Nwamoh U.N., Emma-Ukaegbu U., Onyike G. COVID-19 vaccine hesitancy among healthcare workers and its socio-demographic determinants in Abia State, South-East Nigeria: A cross-sectional study. Pan Afr. Med. J. 2021;40 doi: 10.11604/pamj.2021.40.10.29816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Angelo A.T., Alemayehu D.S., Dachew A.M. Health Care Workers Intention to Accept COVID-19 Vaccine and Associated Factors in Southwestern Ethiopia, 2021. PLoS ONE. 2021;16:e0257109. doi: 10.1371/journal.pone.0257109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Annan J.J., Norman B.R., Mensah B., Enimil A., Kokuro C. Willingness to Accept Vaccination against SARS-COV-2: A Survey of Junior Doctors. World J. Adv. Res. Rev. 2021;9:159–166. doi: 10.30574/wjarr.2021.9.3.0092. [DOI] [Google Scholar]
- 61.Asefa L., Lemma H., Daba C., Dhengesu D., Ibrahim M. COVID-19 vaccine acceptance and associated factors among health workers in West Guji zone, Southern Ethiopia: Cross-sectional study. Front. Public Health. 2023;11:974850. doi: 10.3389/fpubh.2023.974850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aseneh J.B., Agbor V.N., Kadia B.M., Okolie E.A., Ofomata C.J., Etombi C.L., Ekaney D.S.M., Fru Y.W.J. Factors associated with COVID-19 vaccine hesitancy among healthcare workers in Cameroon and Nigeria: A web-based cross-sectional study. Int. Health. 2023. in press . [DOI] [PMC free article] [PubMed]
- 63.Ashipala D.O., Tomas N., Tenete G.C. Barriers and Facilitators Affecting the Uptake of COVID-19 Vaccines: A Qualitative Perspective of Front-line Nurses in Namibia. SAGE Open Nurs. 2023;9:237796082311584. doi: 10.1177/23779608231158419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Berhe E.T., Shama A.T., Ahmed M.Z., Gesesew H.A., Ward P., Gebremeskel T.G. Assessment of COVID-19 vaccination refusal among healthcare workers in Ethiopia. Front. Public Health. 2022;10:929754. doi: 10.3389/fpubh.2022.929754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dahie H.A., Mohamoud J.H., Adam M.A., Garba B., Dirie N.I., Nur M.A., Mohamed F.Y. COVID-19 Vaccine Coverage and Potential Drivers of Vaccine Uptake among Healthcare Workers in SOMALIA: A Cross-Sectional Study. Vaccines. 2022;10:1116. doi: 10.3390/vaccines10071116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ekwebene O.C., Obidile V.C., Azubuike P.C., Nnamani C.P., Dankano N.E., Egbuniwe M.C. COVID-19 Vaccine Knowledge and Acceptability among Healthcare Providers in Nigeria. Int. J. Trop. Dis. Health. 2021;42:51–60. doi: 10.9734/ijtdh/2021/v42i530458. [DOI] [Google Scholar]
- 67.El-Ghitany E.M., Ashour A., Omran E.F., Farghaly A.G., Hassaan M.A., Azzam N.F.A.E.-M. COVID-19 vaccine acceptance rates and predictors among the Egyptian general population and Healthcare workers, the intersectionality of age and other factors. Sci. Rep. 2022;12:19832. doi: 10.1038/s41598-022-23825-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.George G., Nota P., Strauss M., Lansdell E., Peters R., Brysiewicz P., Nadesan-Reddy N., Wassenaar D. Understanding COVID-19 Vaccine Hesitancy among Healthcare Workers in South Africa. Vaccines. 2023;11:414. doi: 10.3390/vaccines11020414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guangul B.A., Georgescu G., Osman M., Reece R., Derso Z., Bahiru A., Azeze Z.B. Healthcare Workers Attitude towards SARS-COVID-2 Vaccine, Ethiopia. Glob. J. Infect. Dis. Clin. Res. 2021;7:43–48. [Google Scholar]
- 70.Ibrahim A.M., Hamayoun M., Farid M., Al-Umra U., Shube M., Sumaili K., Shamalla L., Malik S.M.M.R. COVID-19 Vaccine Acceptance and Hesitancy in Health Care Workers in Somalia: Findings from a Fragile Country with No Previous Experience of Mass Adult Immunization. Vaccines. 2023;11:858. doi: 10.3390/vaccines11040858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Iwu C.A., Ositadinma P., Chibiko V., Madubueze U.C., Uwakwe K.A., Oluoha U.R. Prevalence and Predictors of COVID-19 Vaccine Hesitancy among Health Care Workers in Tertiary Health Care Institutions in a Developing Country: A Cross-Sectional Analytical Study. Hindawi. 2022;2022:7299092. doi: 10.1155/2022/7299092. [DOI] [Google Scholar]
- 72.Kanyike A.M., Olum R., Kajjimu J., Ojilong D., Akech G.M., Nassozi D.R., Agira D., Wamala N.K., Asiimwe A., Matovu D., et al. Acceptance of the Coronavirus Disease-2019 Vaccine among Medical Students in Uganda. Trop. Med. Health. 2021;49:37. doi: 10.1186/s41182-021-00331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mohammed R., Nguse T.M., Habte B.M., Fentie A.M., Gebretekle G.B. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PLoS ONE. 2021;16:e0261125. doi: 10.1371/journal.pone.0261125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mohammed A., Asumah M.N., Padhi B.K., Sinha A., Mohammed I., Jamil S., Boasiako O.A., Leman N., Kabir R. Predictors of SARS-CoV-2 Vaccine Uptake among Health Professionals: A Cross-Sectional Study in Ghana. Vaccines. 2023;11:190. doi: 10.3390/vaccines11010190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moucheraud C., Phiri K., Whitehead H.S., Songo J., Lungu E., Chikuse E., Phiri S., Van Oosterhout J.J., Hoffman R.M. Uptake of the COVID-19 vaccine among healthcare workers in Malawi. Int. Health. 2022;15:77–84. doi: 10.1093/inthealth/ihac007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mudenda S., Mukosha M., Hikaambo C.N., Meyer J.C., Fadare J., Kampamba M., Kalungia A.C., Munsaka S., Okoro R.N., Daka V., et al. Awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia. Malawi Med. J. 2022;34:273–280. doi: 10.4314/mmj.v34i4.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ngasa N.C., Ngasa S.N., Tchouda L.A.S., Tanisso E., Abanda C., Dingana T.N. Spirituality and other factors associated with COVID-19 Vaccine Acceptance amongst Healthcare Workers in Cameroon. Res. Sq. 2021 doi: 10.21203/rs.3.rs-712354/v1. [DOI] [Google Scholar]
- 78.Niguse S., Gebremariam S., Terefa D.R., Biset Y., Mekasha E., Meskele K. Assessment of COVID-19 vaccine take-up and its predictors among healthcare professionals in public hospitals, Addis Ababa, Ethiopia: Facility-based cross-sectional study. Hum. Vaccines Immunother. 2023;19:2171181. doi: 10.1080/21645515.2023.2171181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nnaemeka V.C., Onwe R.O., Ekwedike A.L., Oyedele O.E., Tsiterimam T.S., Ochepo O.E., Nwokoye N.N., Ike A.C. Predictors of COVID-19 Vaccine Acceptance among Healthcare Workers in Nigeria. Vaccines. 2022;10:1645. doi: 10.3390/vaccines10101645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nzaji M.K., Ngombe L.K., Mwamba G.N., Ndala D.B., Miema J.M., Lungoyo C.L., Mwimba B.L., Bene A.C., Musenga E.M. Acceptability of Vaccination against COVID-19 among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic Obs. Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Oriji P.C., Allagoa D.O., Wagio T.J., Obagah L., Tekenah E.S., Ozori S.E. Hesitancy of COVID-19 Vaccination among Health Workers (Other than Doctors) in a Tertiary Hospital in South-South, Nigeria. Asian J. Res. Infect. Dis. 2021;7:21–31. doi: 10.9734/ajrid/2021/v7i130207. [DOI] [Google Scholar]
- 82.Ouni P.D., Namulondo R., Wanume B., Okia D., Olupot P.O., Nantale R., Matovu J.K., Napyo A., Lubaale Y.A.M., Nshakira N., et al. COVID-19 vaccine hesitancy among health workers in rural Uganda: A mixed methods study. Vaccine X. 2023;13:100260. doi: 10.1016/j.jvacx.2023.100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Robinson E.D., Wilson P., Eleki B.J., Wonodi W. Knowledge, Acceptance, and Hesitancy of COVID-19 Vaccine among Health Care Workers in Nigeria. MGM J. Med. Sci. 2021;8:102. doi: 10.4103/mgmj.mgmj_4_21. [DOI] [Google Scholar]
- 84.Saied S.M., Saied E.M., Kabbash I.A., Abdo S.A. Vaccine Hesitancy: Beliefs and Barriers Associated with COVID-19 Vaccination among Egyptian Medical Students. J. Med. Virol. 2021;93:4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sharaf M., Taqa O., Mousa H., Badran A. COVID-19 Vaccine Acceptance and Perceptions among Dental Teaching Staff of a Governmental University in Egypt. J. Egypt. Public Health Assoc. 2022;97:9. doi: 10.1186/s42506-022-00104-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shehata W.M., Elshora A., Abu-Elenin M.M. Physicians’ attitudes and acceptance regarding COVID-19 vaccines: A cross-sectional study in mid Delta region of Egypt. Environ. Sci. Pollut. Res. 2021;29:15838–15848. doi: 10.1007/s11356-021-16574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Terefa D.R., Shama A.T., Feyisa B.R., Desisa A.E., Geta E., Chego M., Edosa A.T. COVID-19 Vaccine Uptake and Associated Factors Among Health Professionals in Ethiopia. Infect. Drug Resist. 2021;14:5531–5541. doi: 10.2147/IDR.S344647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tharwat S., Nassar D., Nassar M.K., Saad A., Hamdy F. Attitude towards COVID-19 vaccination among healthcare workers: A cross sectional study from Egypt. BMC Health Serv. Res. 2022;22:1357. doi: 10.1186/s12913-022-08751-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Voundi-Voundi E., Songue E., Voundi-Voundi J., Nseme E.G., Abba-Kabir H., Kamgno J. Factors associated with COVID-19 vaccine hesitancy among health personnel in Yaounde, Cameroon. Health Sci. Dis. 2023;24:23–27. [Google Scholar]
- 90.Watermeyer J., Scott M., Kapueja L., Ware L.J. To Trust or Not to Trust: An Exploratory Qualitative Study of Personal and Community Perceptions of Vaccines amongst a Group of Young Community Healthcare Workers in Soweto, South Africa. Health Policy Plan. 2022;37:1167–1176. doi: 10.1093/heapol/czac060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Whitworth H.S., Kitonsa J., Kasonia K., Tindanbil D., Kafeero P., Bangura J., Nije Y., Tetsa Teta D., Greenwood B., Kavunga-Membo H., et al. COVID-19 Vaccine Acceptability among Healthcare Facility Workers in Sierra Leone, the Democratic Republic of Congo and Uganda: A Multi-Centre Cross-Sectional Survey. Int. J. Public Health. 2022;67:1605113. doi: 10.3389/ijph.2022.1605113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yassin E.O., Faroug H.A., Ishaq Z.B., Mustafa M.M., Idris M.M., Widatallah S.E., Abd El-Raheem G.O., Suliman M.Y. COVID-19 Vaccination Acceptance among Healthcare Staff in Sudan, 2021. J. Immunol. Res. 2022;2022:3392667. doi: 10.1155/2022/3392667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yendewa S.A., Ghazzawi M., James P., Smith M., Massaquoi S.P., Babawo L.S., Deen G.F., Russell J.A., Samai M., Sahr F., et al. COVID-19 Vaccine Hesitancy among Healthcare Workers and Trainees in Freetown, Sierra Leone: A Cross-Sectional Study. Vaccines. 2022;10:757. doi: 10.3390/vaccines10050757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zammit N., Gueder A.E., Brahem A., Ayouni I., Ghammam R., Fredj S.B., Sridi C., Chouchene A., Kalboussi H., Maalel O.E., et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv. Res. 2022;22:489. doi: 10.1186/s12913-022-07803-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zewude B., Belachew A. Intention to Receive the Second Round of COVID-19 Vaccine among Healthcare Workers in Eastern Ethiopia. Infect. Drug Resist. 2021;14:3071–3082. doi: 10.2147/IDR.S326055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bai L., Zhao Y., Dong J., Liang S., Guo M., Liu X., Wang X., Huang Z., Sun X., Zhang Z., et al. Coinfection with Influenza A Virus Enhances SARS-COV-2 Infectivity. Cell Res. 2021;31:395–403. doi: 10.1038/s41422-021-00473-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Li M., Luo Y., Watson R., Zheng Y., Ren J., Tang J., Chen Y. Healthcare Workers’ (hcws) attitudes and related factors towards COVID-19 vaccination: A rapid systematic review. Postgrad. Med. J. 2021;99:520–528. doi: 10.1136/postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 98.Ghare F., Meckawy R., Moore M., Lomazzi M. Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review. Vaccines. 2023;11:311. doi: 10.3390/vaccines11020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gilmore B., Ndejjo R., Tchetchia A., de Claro V., Nyamupachitu-Mago E., Diallo A.A., Lopes C.A., Bhattacharyya S. Community engagement for COVID-19 prevention and Control: A Rapid Evidence Synthesis. BMJ Glob. Health. 2020;5:e003188. doi: 10.1136/bmjgh-2020-003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bangalee A., Bangalee V. Fake News and Fallacies: Exploring Vaccine Hesitancy in South Africa. S. Afr. Fam. Pract. 2021;63:3. doi: 10.4102/safp.v63i1.5345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zintel S., Flock C., Arbogast A.L., Forster A., von Wagner C., Sieverding M. Gender differences in the intention to get vaccinated against COVID-19: A systematic review and meta-analysis. Public Health. 2022;31:1303–1327. doi: 10.1007/s10389-021-01677-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Naidoo D., Meyer-Weitz A., Govender K. Factors Influencing the Intention and Uptake of COVID-19 Vaccines on the African Continent: A Scoping Review. Vaccines. 2023;11:873. doi: 10.3390/vaccines11040873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., Gagneur A., Dubé E. Attitudes of Healthcare Workers towards COVID-19 Vaccination: A Survey in France and French-Speaking Parts of Belgium and Canada, 2020. Eurosurveillance. 2021;26:2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tabacchi G., Costantino C., Cracchiolo M., Ferro A., Marchese V., Napoli G., Palmeri S., Raia D., Restivo V., Siddu A., et al. Information Sources and Knowledge on Vaccination in a Population from Southern Italy: The ESCULAPIO Project. Hum. Vaccines Immunother. 2016;13:339–345. doi: 10.1080/21645515.2017.1264733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kestenbaum L.A., Feemster K.A. Identifying and Addressing Vaccine Hesitancy. Pediatr. Ann. 2015;44:e71–e75. doi: 10.3928/00904481-20150410-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Talarek E., Chazan M., Winiarska P., Dembiński Ł., Sobierajski T., Banaszkiewicz A. How Attitudes towards Vaccination Change in the Face of an Outbreak. Hum. Vaccines Immunother. 2020;17:805–809. doi: 10.1080/21645515.2020.1798152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mamani-Benito O., Farfán-Solís R., Huayta-Meza M., Tito-Betancur M., Morales-García W.C., Tarqui E.E. Effect of religious fatalism and concern about new variants on the acceptance of COVID-19 vaccines. Front. Psychiatry. 2023;14:1071543. doi: 10.3389/fpsyt.2023.1071543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Peterson C.J., Lee B., Nugent K. COVID-19 vaccination hesitancy among healthcare workers—A review. Vaccines. 2022;10:948. doi: 10.3390/vaccines10060948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.