Abstract
Study Design
Retrospective cohort study.
Objectives
Investigate a composite score to evaluate the relationship between alignment proportionality and risk of distal junctional kyphosis (DJK).
Methods
84 patients with minimum 1 year follow-up were included (age = 61.1 ± 10.3 years, 64.3% women). The Cervical Score was constructed using offsets from age-adjusted normative values for sagittal vertical axis (SVA), T1 Slope (TS), and TS minus cervical lordosis (CL). Individual points were assigned based on offset with age-adjusted alignment targets and summed to generate the Cervical Score. Rates of mechanical failure (DJK revision or severe DJK [DJK> 20° and ΔDJK> 10°]) were assessed overall and based on Cervical Score. Logistical regressions assessed associations between early radiographic alignment and 1-year failure rate.
Results
Mechanical failure rate was 21.4% (N = 18), 10.7% requiring revision. By multivariate logistical regression: 3-month T1S (OR: .935), TS-CL (OR:0.882), and SVA (OR:1.015) were independent predictors of 1-year failure (all P < .05). Cervical Score ranged (−6 to 6), 37.8% of patients between −1 and 1, and 50.0% with 2 or higher. DJK patients had significantly higher Cervical Score (4.1 ± 1.3 vs .6 ± 2.2, P < .001). Patients with a score ≥3 were significantly more likely to develop a failure (71.4%) with OR of 38.55 (95%CI [7.73; 192.26]) and Nagelkerke r2 .524 (P < .001)
Conclusion
This study developed a composite alignment score predictive of mechanical failures in CD surgery. A score ≥3 at 3 months following surgery was associated with a marked increase in failure rate. The Cervical Score can be used to analyze sagittal alignment and help define realignment objectives to reduce mechanical failure.
Keywords: CD, cervical deformity, DJK, distal junctional kyphosis, sagittal alignment, mechanical failure
Introduction
Adult cervical deformity (ACD), defined as the disruption of normal cervical alignment in the sagittal and/or coronal plane is a complex pathology.1,2 ACD is associated with significant disability, 3 and the relationship between cervical sagittal alignment and patient health-related quality of life outcomes has been well established in the literature. 4
While patients can have substantial benefit from surgical treatment and realignment surgery,5,6 the surgical correction of ACD remains complex, and has been associated with a high rate of post-operative complications and revisions.7,8 Mechanical failure, more specifically distal junctional kyphosis, has been of particular concern following corrective surgery for ACD, and remains a common cause of revision surgery.8,9
In the thoracolumbar deformity literature, mechanical failures and proximal junctional kyphosis have been extensively studied, with evolving prediction and prevention strategies.10,11 Post-operative alignment and its deviation from normative targets have been identified multiple times as major risk factors for proximal junction issues.12,13 In contrast to thoracolumbar deformity corrective procedures, which are more commonly vulnerable to proximal junctional issues, surgery for ACD is more susceptible to distal junctional kyphosis (DJK), the distal equivalent to PJK. Similar to PJK, several authors have demonstrated the importance of achieving appropriate sagittal alignment in DJK prevention.14,15
Inspired by recent publications in the thoracolumbar field, 12 this study aims to establish a composite score that evaluates post-operative alignment in ACD, and assess the relationship between post-operative alignment and mechanical failure.
Methods
Patient Sample
Study data was obtained from a multi-center prospective database of ACD patients undergoing surgery. Patients were enrolled at 1 of 13 institutions across the United States between 2012 and 2015. Institutional Review Board (IRB) approval at each of the 13 participating sites was obtained prior to conducting the study (IRB No. 2014-373). Informed consent was obtained from all participating patients. Inclusion criteria for the overall database were: age >18 years and presence of ACD, defined by the presence of at least one of the following: C2–C7 sagittal Cobb angle ≥10° (cervical kyphosis), C2–C7 coronal Cobb angle ≥10° (cervical scoliosis), C2–C7 sagittal vertical axis (C2–C7 SVA) ≥4 cm, and/or chin-brow vertical angle (CBVA) ≥25°. Exclusion criteria for the overall database include the presence of active infection or malignancy, an underlying neurologic pathology (e.g., Parkinson’s disease), or post-traumatic deformity. In addition to the above inclusion criteria, the present study only included patients who completed a minimum 1-year follow-up. Those with fusions extending to the pelvis were excluded from this study.
Data Collection
This was a prospective study in which baseline patient characteristic and demographic data were collected pre-operatively. Surgical data was collected at the time of the surgical intervention. Complications, including details pertaining to revision surgery, were recorded prospectively using standardized forms.
All patients had cervical and standing 36’’ postero-anterior (PA) and lateral spine radiographs at baseline and at 3-month, 6-month, and 1-year follow-up. Radiographic evaluations were performed at a central location using validated spine software. Parameters measured included classic spino-pelvic parameters, such as pelvic incidence (PI), pelvic tilt (PT), pelvic incidence minus lumbar lordosis (PI-LL), sagittal vertical axis (SVA), and T1-pelvic angle (TPA). We also measured cervical-specific parameters, including the C2–C7 coronal Cobb angle, cervical sagittal vertical axis (cSVA), T1 slope, C2 slope, and T1 slope minus cervical lordosis (TS-CL).
Post-operative alignment was measured on 3-month post-operative radiographs. For patients who underwent revision surgery prior to the 3 month follow-up timepoint, post-operative alignment was measured on pre-revision radiographs.
Mechanical failure was defined as having a revision for mechanical failure or having a radiographic DJK. Radiographic DJK was diagnosed radiographically, using the following criteria: DJK angle greater than 20° + ΔDJK angle greater than 10 compared with pre-operative baseline imaging. 16
Cervical Score Calculation
For each patient, the difference (offset) between the post-operative alignment achieved and the age-adjusted alignment target was calculated. The age-adjusted alignment targets were calculated, based on the literature using the following formulas:17-19
• TPA: (age – 55)/3 + 20; 17
• SVA: (age – 55) *2 + 25; 17
• PT: (age – 55)/2 + 16; 17
• TS: (age – 55)/4 + 28.75; 19
• TS-CL: constant between 14.5 and 26.5°; 18
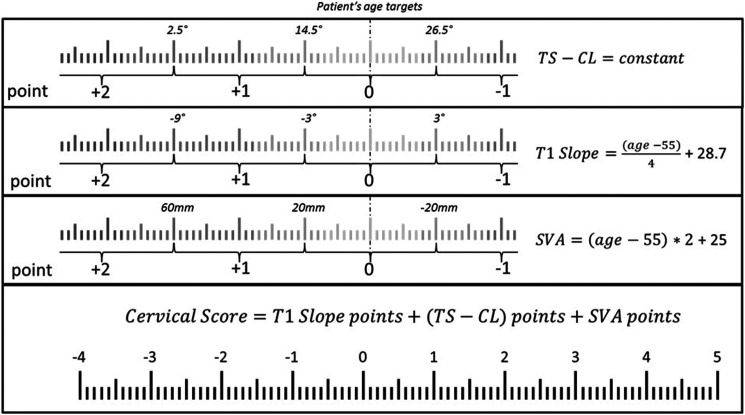
Each patient was then assigned a Cervical Score for mechanical failure, based on the offset between the post-operative alignment achieved and age-adjusted alignment targets on the T1S, TS-CL, and SVA. The details of the Cervical Score can be found in (Figure 1). Briefly, for each of the 3 radiographic parameters, a score of 0 was assigned if the alignment matched the age-adjusted target. Points were assigned based on the offset between post-operative alignment and age-adjusted targets. The total Cervical Score was then calculated by summing the points obtained for the T1S, TS-CL, and SVA.
Figure 1.
Cervical Score calculation based on offset between alignment and age-adjusted targets.
Data Analysis
Pre- to post-operative alignment was analyzed in the overall cohort using paired t-tests or Wilcoxon signed-rank tests as appropriate. Patients were divided into two groups: those who experienced mechanical failure, and those who did not. The two groups were compared regarding pre-operative alignment, post-operative alignment achieved, and the offset between post-operative alignment and age-adjusted thresholds using Mann–Whitney U test. We also analyzed the rate of mechanical failures by individual Cervical Score, and performed a cutoff analysis to assess the relative risk of failure by Cervical Score, using thresholds of 3 and 4 points. SPSS 20.0 (IBM Corp Released 2011. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp) was used for the analysis. Statistical analyses were two-sided, and P < .05 was considered statistically significant.
Results
Our database had a total of 145 patients with ACD who were eligible for 1-year follow-up; 84 patients met the specific inclusion criteria for this study. Our cohort had an average age of 61.1 years, and an average body mass index (BMI) of 28.3. A majority (64.3%) of our patients were women, and 34.5% of patients had a history of prior spine surgery. The median follow-up was 12 months.
Mechanical failure occurred in 21.4% of our cohort (n = 18), and of these patients with failure, 50% (n = 9) required revision surgery with a mean time between index surgery and revision of 145 days ±98.
Pre-operative and 3-month post-operative sagittal alignment parameters are summarized in Table 1. Our results show a moderate baseline cervical malalignment, with an average C2–C7 kyphosis of 8.2°, an average TS-CL of 38.2°, and an average C2 slope of 38.0°. At baseline, the global sagittal alignment parameters demonstrate a compensatory posterior global alignment, with an average TPA of 11.8°, and an SVA of −7.2 mm. Following surgery, there was significant improvement in the cervical parameters, based on the C2–C7 lordosis (8.2° kyphosis vs 7.5° lordosis, P < .001), C2 slope (38.0° vs 25.9°, P < .001), and TS-CL (38.2° vs 27.7°, P < .001). Relaxation of compensatory alignment mechanisms was also evident based on the TPA (11.8° vs 15.2°, P = .001), and SVA (−7.2 mm vs 16.7 mm, P < .001).
Table 1.
Pre-operative to 3-month post-operative thoracolumbar and cervical sagittal alignment for the entire cohort.
| Pre | 3 months | P-value | |||
|---|---|---|---|---|---|
| Mean | StD | Mean | StD | ||
| PT | 18.3 | 11.1 | 20.0 | 11.7 | .019 |
| TPA | 11.8 | 12.5 | 15.3 | 13.3 | <.001 |
| SVA | −7.2 | 71.4 | 16.7 | 68.4 | <.001 |
| T1 slope | 29.9 | 17.1 | 35.2 | 16.0 | <.001 |
| C2–C7 | −8.2 | 23.0 | 7.5 | 16.6 | <.001 |
| C2 slope | 38.0 | 20.2 | 25.9 | 13.4 | <.001 |
| TS-CL | 38.2 | 19.6 | 27.7 | 13.8 | <.001 |
Table 2 compares patients who experienced mechanical failure to those who did not with regard to pre-operative alignment and 3-month post-operative alignment. The two groups differ in terms of pre- and post-operative alignment. Patients who experienced mechanical failure had greater pre-operative deformity, as shown by significant differences in their baseline C2–C7 lordosis (median 17.6° kyphosis vs 14.8°, P = .045), baseline C2 slope (median 56.7° vs 29.9°, P = .001), and baseline TS-CL (median 54.4° vs 30.3°).
Table 2.
Comparison of pre-operative and post-operative sagittal alignment between patients with and without a mechanical failure.
| Not Fail (n = 66) | Fail (n = 18) | M-W | ||||||
|---|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | 25th | 50th | 75th | P -value | ||
| Pre-op | PT | 11.6 | 17.6 | 26.3 | 16.5 | 19.9 | 24.8 | .724 |
| TPA | 5.4 | 12.2 | 18.9 | 0.3 | 10.9 | 17.1 | .400 | |
| SVA | −43.2 | −11.6 | 42.2 | −107.3 | −21.3 | 3.5 | .112 | |
| T1 slope | 17.1 | 26.1 | 36.7 | 23.3 | 32.2 | 48.1 | .045 | |
| C2-C7 | −14.8 | −6.1 | 3.0 | −33.1 | −17.6 | −0.5 | .049 | |
| C2 slope | 23.3 | 29.9 | 46.9 | 32.0 | 56.7 | 65.3 | .001 | |
| TS-CL | 25.5 | 30.3 | 44.8 | 36.5 | 54.4 | 62.6 | .001 | |
| 3 months | PT | 12.5 | 18.8 | 26.9 | 15.2 | 23.0 | 27.2 | .485 |
| TPA | 7.8 | 13.6 | 21.0 | 9.0 | 16.2 | 24.7 | .735 | |
| SVA | −18.6 | 7.3 | 49.8 | −65.7 | 13.8 | 70.6 | .711 | |
| T1 slope | 23.3 | 30.4 | 37.2 | 34.5 | 47.7 | 53.7 | <.001 | |
| C2–C7 | 0.5 | 6.8 | 12.3 | −12.4 | 8.2 | 19.7 | .926 | |
| C2 slope | 15.8 | 21.4 | 27.8 | 25.2 | 42.1 | 47.5 | <.001 | |
| TS-CL | 18.9 | 23.3 | 30.8 | 28.3 | 41.1 | 48.5 | <.001 | |
Table 3 compares patients who experienced mechanical failure to those who did not with regard to offset from age-adjusted alignment targets. Patients who experienced mechanical failure were under-corrected compared to their age-adjusted targets, as shown by the T1 slope offset (median −14° vs .9°, P < .001) and the TS-CL offset (median −16.5° vs −2.8°, P < .001)
Table 3.
Comparison of the offset between post-operative sagittal alignment and age-adjusted targets between patients with and without mechanical failure.
| Not Fail (n = 66) | Fail (n = 18) | M-W | ||||||
|---|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | 25th | 50th | 75th | P -value | ||
| Offsets | PT | −6.6 | 3.3 | 10.0 | −3.6 | −0.1 | 5.2 | .586 |
| TPA | −3.7 | 5.4 | 12.4 | −2.3 | 3.2 | 8.8 | .836 | |
| SVA | −11.4 | 29.5 | 60.8 | −16.2 | 35.8 | 88.0 | .459 | |
| T1 slope | −7.5 | 0.9 | 8.0 | −21.1 | −14.0 | −3.5 | <.001 | |
| TS-CL | −10.8 | −2.8 | 4.3 | −31.5 | −16.5 | −7.2 | <.001 | |
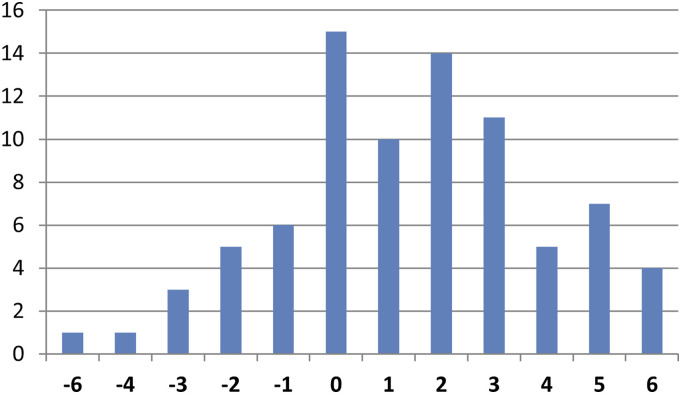
The distribution of the Cervical Score for the entire cohort is illustrated in (Figure 2). Overall, 37.8% of patients had a score between −1 and 1 (adequately corrected compared to their age-adjusted alignment targets), 12.2% of patients had a score of −2 or lower (over-corrected compared to their age-adjusted alignment targets), and 50.0% had a score of 2 or higher (under-corrected compared to their age-adjusted alignment targets). Median Cervical Scores were significantly higher among the group of patients who experienced mechanical failure (4.0 vs 1.0, P < .001).
Figure 2.
Distribution of the Cervical Score for the entire study cohort.
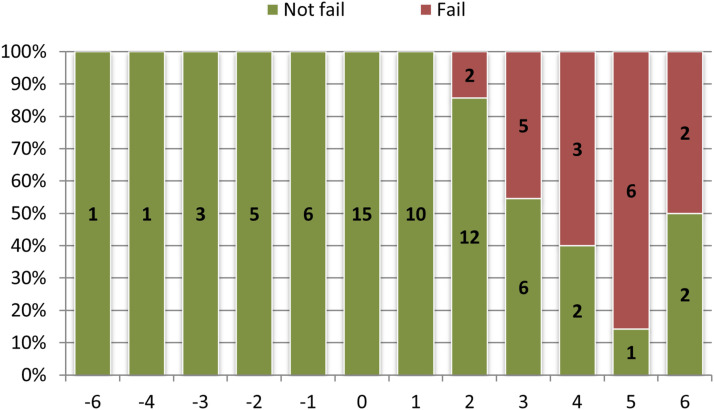
(Figure 3) illustrates the proportion of mechanical failures by individual Cervical Score. As illustrated, there were no failures for scores ≤1, and most failures occurred in patients with a Cervical Score of 3 or greater. Threshold analysis using a cutoff of 3 resulted in an OR of 38.545 (P < .001).
Figure 3.
Proportion of mechanical failure for each individual Cervical Score.
Discussion
This study focused on a cohort of ACD patients with minimum 1-year follow-up. Among our patient population, the rate of mechanical failure was 21.4%, out of which one-half underwent surgical revision. Pre-operative and post-operative cervical alignment were significantly different between patients who either did or did not develop a post-operative mechanical failure. A novel Cervical Score was developed that reflects the severity of post-operative sagittal malalignment relative to age-adjusted normative values. When applied to the 3-month post-operative imaging of ACD patients, the Cervical Score demonstrated a strong and significant association with subsequent development of mechanical failure. Patients with a Cervical Score of 3 or greater had a 35-fold greater risk of developing a mechanical issue within 1 year of surgery.
Our results show that patients who experienced mechanical failure had larger baseline deformities prior to surgical intervention. This observation has been previously noted 15 with reported thresholds of C2-C7 kyphosis greater than 12° and TS-CL greater than 36.4°. Patients presenting with the largest deformities were more likely to undergo larger corrections, increasing the risk of complications. 8 They also had greater amounts of residual deformity following surgery, when compared to their counterparts who did not experience a mechanical failure. This residual deformity can be the result of an incomplete correction, leading to increased mechanical loading at the distal junction due to gravity and a lever arm effect. 20 When combined with poor muscle quality, as previously documented in the literature, this increase in mechanical loading can lead to progressive failure. 21 This residual deformity can also be the early sign of a progressive failure. Monitoring early post-operative alignment, especially during the first several months following surgery, may allow for non-operative interventions, such as physical therapy or posture training, to help reduce the risks of needing revision surgery.
In contrast to previous reports that have assessed alignment and DJK, the present study proposes a novel Cervical Score to assess post-operative alignment. Compared to a singular radiographic parameter, this combined score allows assessment of the proportionality between parameters rather than focusing on a single aspect of alignment. 12 Parameters included in the Cervical Score have been previously associated with cervical deformity, 22 as well as with PJK 13 and health-related quality of life. 23 Other factors have been reported to be associated with junctional pathologies, including osteoporosis, age, and neurological comorbidities.15,24 While these other factors may be associated with an increased risk, surgeons have limited ability to directly affect these parameters. Thresholds used in the Cervical Score were tailored to patient age. This approach of using age-adjusted thresholds has been successfully applied to proximal junctional issues in the thoracolumbar literature. 13 The post-operative distribution of Cervical Scores revealed that most of the patients had a score between −1 and 2, and that very few patients were severely over-corrected or under-corrected (above 4 or below −4).
Our results suggest that the Cervical Score could be of use in predicting mechanical failures. In our study, a score of 3 and above was indicative of significantly higher odds of experiencing mechanical failure. Therefore, pre-operative planning should not only account for regional correction, but also the global alignment and the alignment induced by this correction. In the thoracolumbar literature, overcorrection has been linked to mechanical failure and PJK.25,26 Our results in ACD patients contrast with this finding in that undercorrection may actually play a significant role in the development of mechanical failure following cervical realignment. An increased forward sagittal alignment, combined with poor muscle and bone quality, could be dramatic due to the dynamic aspect of the cervical spine leading to more dynamic solicitation. 27 With the development of improved dynamic evaluations, 28 future studies investigating the effect of cervical fused alignment and the range of motion distal to the fusion could provide further insight.
This study is not without limitation. First and foremost, the relatively small sample size combined with a follow-up of 1-year may limit the generalization of this result. Validation of these findings based on larger sample size is warranted. Second, the large variability in terms of pre-operative deformity does not allow for more granular analysis of regional and focal alignment. Finally, the lack of dedicated patient-reported outcomes and neurological examinations limits the ability to characterize a potential association between the proposed Cervical Score and patient quality of life.
Conclusion
Mechanical failures following ACD surgery occurred in almost 1 out of 5 patients in this cohort, with 50% of them requiring a revision surgery before 1-year follow-up. Larger pre-operative malalignment combined with poor post-operative sagittal alignment were associated with mechanical failure. The proposed Cervical Score enabled quantification of the proportionality of sagittal alignment. A Cervical Score of 3 or above was associated with a marked increased risk of mechanical failure within the first year following surgery.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes (current), Nuvasive (current), K2M (current), Innovasis (past), Biomet (past), and individual donations.
ORCID iDs
Renaud Lafage https://orcid.org/0000-0002-4820-1835
Justin S Smith https://orcid.org/0000-0003-0467-5534
Han Jo Kim https://orcid.org/0000-0003-2170-3592
Virginie Lafage https://orcid.org/0000-0002-0119-7111
References
- 1.Koller H, Ames C, Mehdian H, et al. Characteristics of deformity surgery in patients with severe and rigid cervical kyphosis (CK): Results of the CSRS-Europe multi-centre study project. Eur Spine J. 2019;28(2):324-344. doi: 10.1007/s00586-018-5835-2. [DOI] [PubMed] [Google Scholar]
- 2.Kim HJ, Virk S, Elysee J, et al. The morphology of cervical deformities: A two-step cluster analysis to identify cervical deformity patterns. J Neurosurg Spine. 2020;32(3):353-359. doi: 10.3171/2019.9.SPINE19730. [DOI] [PubMed] [Google Scholar]
- 3.Smith JS, Line B, Bess S, et al. The health impact of adult cervical deformity in patients presenting for surgical treatment: Comparison to United States population norms and chronic disease states based on the euro quol-5 dimensions questionnaire. Neurosurgery. 2017;80(5):716-725. doi: 10.1093/neuros/nyx028. [DOI] [PubMed] [Google Scholar]
- 4.Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2012;71(3):662-669. doi: 10.1227/NEU.0b013e31826100c9. [DOI] [PubMed] [Google Scholar]
- 5.Segreto FA, Lafage V, Lafage R, et al. Recovery kinetics: Comparison of patients undergoing primary or revision procedures for adult cervical deformity using a novel area under the curve methodology. Neurosurgery. 2019;85(1):E40-E51. doi: 10.1093/neuros/nyy435. [DOI] [PubMed] [Google Scholar]
- 6.Ailon T, Smith JS, Shaffrey CI, et al. Outcomes of operative treatment for adult cervical deformity: A prospective multicenter assessment with 1-year follow-up. Neurosurgery. 2018;83(5):1031-1039. doi: 10.1093/neuros/nyx574. [DOI] [PubMed] [Google Scholar]
- 7.Passias PG, Oh C, Horn SR, et al. Predicting the occurrence of complications following corrective cervical deformity surgery: Analysis of a prospective multicenter database using predictive analytics. J Clin Neurosci. 2019;59(10 suppl):155-161. doi: 10.1016/j.jocn.2018.10.111. [DOI] [PubMed] [Google Scholar]
- 8.Smith JS, Buell TJ, Shaffrey CI, et al. Prospective multicenter assessment of complication rates associated with adult cervical deformity surgery in 133 patients with minimum 1-year follow-up. J Neurosurg Spine. 2020;33(5):588-600. doi: 10.3171/2020.4.SPINE20213. [DOI] [PubMed] [Google Scholar]
- 9.Passias PG, Horn SR, Oh C, et al. Predicting the occurrence of postoperative distal junctional kyphosis in cervical deformity patients. Neurosurgery. 2020;86(1):E38-E46. doi: 10.1093/neuros/nyz347. [DOI] [PubMed] [Google Scholar]
- 10.Zhao J, Chen K, Zhai X, Chen K, Li M, Lu Y. Incidence and risk factors of proximal junctional kyphosis after internal fixation for adult spinal deformity: A systematic evaluation and meta-analysis. Neurosurg Rev. 2020;44:855-866. Published online May 19. doi: 10.1007/s10143-020-01309-z. [DOI] [PubMed] [Google Scholar]
- 11.Echt M, Ranson W, Steinberger J, Yassari R, Cho SK. A systematic review of treatment strategies for the prevention of junctional complications after long-segment fusions in the osteoporotic Spine. Glob Spine J. Published online August. 2020;11:792-801. doi: 10.1177/2192568220939902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yilgor C, Sogunmez N, Boissiere L, et al. Global alignment and proportion (GAP) score. J Bone Joint Surg Am. 2017;99(19):1661-1672. doi: 10.2106/JBJS.16.01594. [DOI] [PubMed] [Google Scholar]
- 13.Lafage R, Schwab F, Glassman S, et al. Age-adjusted alignment goals have the potential to reduce PJK. Spine. 2017;42(17):1275-1282. doi: 10.1097/BRS.0000000000002146. [DOI] [PubMed] [Google Scholar]
- 14.Berjano P, Damilano M, Pejrona M, Langella F, Lamartina C. Revision surgery in distal junctional kyphosis. Eur Spine J. 2020;29(S1):86-102. doi: 10.1007/s00586-020-06304-y. [DOI] [PubMed] [Google Scholar]
- 15.Passias PG, Vasquez-Montes D, Poorman GW, et al. Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J. 2018;18(12):2187-2194. doi: 10.1016/j.spinee.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 16.Protopsaltis TS, Stekas N, Lafage R, et al. Saturday, September 29, 2018 9:00 am-10:00 am impact of adult deformity correction. Spine J. 2018;18(8):S129-S130. doi: 10.1016/j.spinee.2018.06.526. [DOI] [Google Scholar]
- 17.Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds. Spine. 2016;41(1):62-68. doi: 10.1097/BRS.0000000000001171. [DOI] [PubMed] [Google Scholar]
- 18.Staub BN, Lafage R, Kim HJ, et al. Cervical mismatch: The normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine. 2019;30(1):31-37. doi: 10.3171/2018.5.SPINE171232. [DOI] [PubMed] [Google Scholar]
- 19.Iorio J, Lafage V, Lafage R, et al. The effect of aging on cervical parameters in a normative north American population. Glob Spine J. 2018;8(7):709-715. doi: 10.1177/2192568218765400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Huec JCC, Saddiki R, Franke J, Rigal J, Aunoble S. Equilibrium of the human body and the gravity line: The basics. Eur Spine J. 2011;20(S5):558-563. doi: 10.1007/s00586-011-1939-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Passias PG, Segreto FA, Horn SR, et al. Fatty infiltration of the cervical extensor musculature, cervical sagittal balance, and clinical outcomes: An analysis of operative adult cervical deformity patients. J Clin Neurosci. 2020;72:134-141. doi: 10.1016/j.jocn.2019.12.044. [DOI] [PubMed] [Google Scholar]
- 22.Protopsaltis T, Terran J, Soroceanu A, et al. T1 slope minus cervical lordosis (TS-CL), the cervical answer to PI-LL, defines cervical sagittal deformity in patients undergoing thoracolumbar osteotomy. Int J spine Surg. 2018;12(3):362-370. doi: 10.14444/5042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine. 2020;45(3):184-192. doi: 10.1097/BRS.0000000000003214. [DOI] [PubMed] [Google Scholar]
- 24.Glassman SD, Coseo MP, Carreon LY. Sagittal balance is more than just alignment: Why PJK remains an unresolved problem. Scoliosis Spinal Disord. 2016;11(1):1. doi: 10.1186/s13013-016-0064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Line BG, Bess S, Lafage R, et al. Effective prevention of proximal junctional failure in adult spinal deformity surgery requires a combination of surgical implant prophylaxis and avoidance of sagittal alignment overcorrection. Spine. 2020;45(4):258-267. doi: 10.1097/BRS.0000000000003249. [DOI] [PubMed] [Google Scholar]
- 26.Lafage R, Bess S, Glassman S, et al. Virtual modeling of postoperative alignment after adult spinal deformity surgery helps predict associations between compensatory spinopelvic alignment changes, overcorrection, and proximal junctional kyphosis. Spine. 2017;42(19):E1119-E1125. doi: 10.1097/BRS.0000000000002116. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham BW, Hu N, Zorn CM, McAfee PC. Biomechanical comparison of single- and two-level cervical arthroplasty versus arthrodesis: Effect on adjacent-level spinal kinematics. Spine J. 2010;10(4):341-349. doi: 10.1016/j.spinee.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Otayek J, Bizdikian AJ, Yared F, et al. Influence of spino-pelvic and postural alignment parameters on gait kinematics. Gait Posture. 2020;76:318-326. doi: 10.1016/j.gaitpost.2019.12.029. [DOI] [PubMed] [Google Scholar]