Penile inversion vaginoplasty is the most common surgical technique for gender-affirming genital reconstruction in trans-feminine individuals.1–3 This video describes the technique in step-by-step narration of both the external vulvoplasty and internal canal dissection. As part of our multidisciplinary approach to transgender care, this operation is performed by a plastic surgeon and a urologist.
To provide additional vaginal depth, we raise peritoneal flaps with a robotically assisted laparoscopic approach.4 The first reported peritoneal flap vaginoplasty was performed by Ksido et al.5 in 1933 for patients with Mayer-Rokitansky-Küster-Hauser syndrome. Davydov and Zhvitiashvili subsequently popularized the technique.6 Based on this technique, our group published a series of 41 patients undergoing gender-affirming vaginoplasty with robotically assisted peritoneal flaps.4
PART I
Positioning and Markings
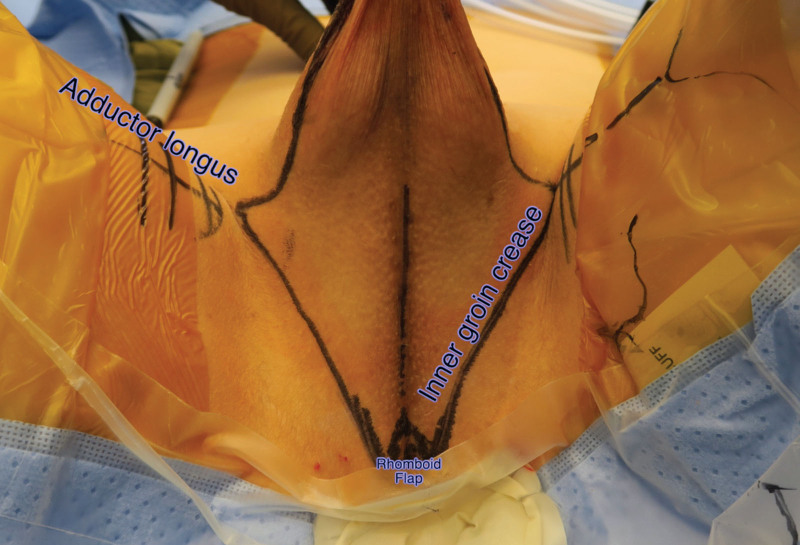
In dorsal lithotomy, the adductor tendons and inner groin creases are marked, in addition to a perineal rhomboid flap at the future vaginal introitus (approximately 2 ×1 cm) (Fig. 1). [See Video 1 (online), which demonstrates penile inversion vaginoplasty surgical technique, part I: positioning and markings, scrotal graft harvest, orchiectomy, bulbospongiosus muscle dissection, penile degloving, penile disassembly, erectile tissue removal, and vaginal canal dissection. (Audio credit: https://soundcloud.com/mattquentin.)]
Fig. 1.
Perineum landmarks: adductor tendons, inner groin creases, and rhomboid flap at the future vaginal introitus (approximately 2 × 1 cm).
Video 1. This video demonstrates penile inversion vaginoplasty surgical technique, part I: positioning and markings, scrotal graft harvest, orchiectomy, bulbospongiosus muscle dissection, penile degloving, penile disassembly, erectile tissue removal, and vaginal canal dissection. (Audio credit: https://soundcloud.com/mattquentin.).
Scrotal Graft Harvest
The scrotal skin is harvested as a graft, leaving behind the underlying dartos fascia, and is thinned on the back table, ensuring that all hair follicles are removed, as it will be subsequently used for vaginal canal lining. The remaining scrotal skin that is not excised will later be used for construction of the labia majora.
Orchiectomy
The testes are delivered by opening the tunica vaginalis. The spermatic cord is then skeletonized by dissecting the adventitia and tunica vaginalis down to the external inguinal ring. The spermatic cord is ligated with 0-silk suture. The stump of the cord should retract into the inguinal canal to prevent visible bulging.
Bulbospongiosus Muscle Dissection
The perineal dissection is carried through Colles fascia, exposing the bulbospongiosus muscles, which are excised, exposing the bulbar urethra.
Penile Degloving
A circumferential incision on the penile skin is made 2 cm proximal to the corona of the glans, leaving a cuff of prepuce. The penile skin is dissected free in the loose areolar plane between dartos and Buck’s fascia. The penis is pulled through the circumscribing incision and dissection is carried out dorsally while being mindful to preserve the neurovascular bundle. The prepuce is divided at the ventral midline and a urethrectomy is performed, amputating the urethra at the level of the adductor longus.
Penile Disassembly
A distal corporotomy is made on the ventral shaft of the penis bilaterally and a Yankauer suction tip is inserted down to the ischium and used to guide the ventral corporotomy toward the base of the corpora.
Erectile Tissue Removal
Mosquito clamps are placed on the edge of the tunica albuginea to provide tension, and a Molt periosteal elevator is used to remove all spongy erectile tissue off of the tunica albuginea. The septum is removed with electrocautery. The corporotomy is closed with a 4-0 polydioxanone (PDS; Ethicon, Inc., Somerville, N.J.) running stitch.
Vaginal Canal Dissection (Perineal/External)
Epinephrine is injected to hydrodissect between the bulbar urethra and bulbospongiosus muscle. For optimal exposure, the bulbar urethra is grasped and elevated as the dissection advances toward the pelvis. This perineal dissection will then meet the robotic surgeon’s intraabdominal pelvic dissection at the pelvic floor.
PART II
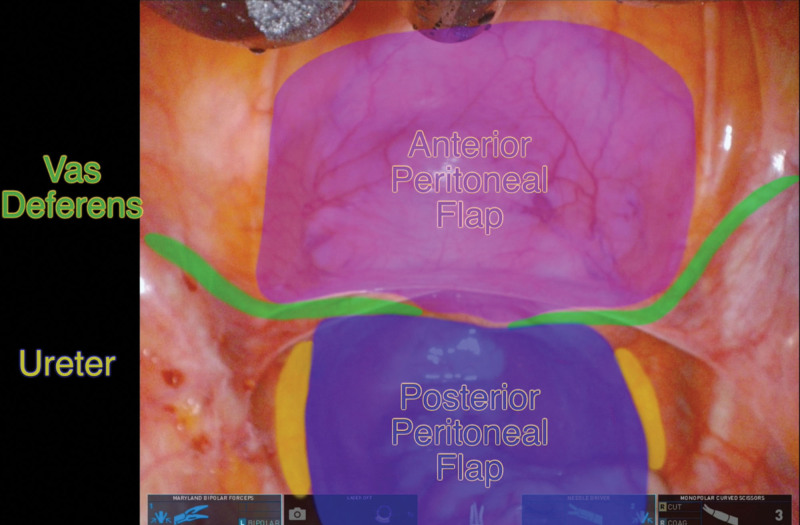
The anterior and posterior peritoneal flaps to be raised robotically are divided by the vas deferens. The ureters mark the lateral borders of the posterior peritoneal flap while the sacral promontory marks the superior border (Fig. 2). [See Video 2 (online), which demonstrates penile inversion vaginoplasty surgical technique, part II: peritoneal flap elevation, clitoroplasty, urethroplasty, penile inversion, peritoneal flap inset, and vaginal packing. (Audio credit: https://soundcloud.com/mattquentin.)] The dimensions of the anterior and posterior peritoneal flaps should match. After creation of the peritoneal flaps, dissection is advanced within the Denonvilliers fascia toward the pelvic floor, in a plane between the prostate and the rectum. At this point, the perineal surgeon can break through the pelvic floor, guided by the robotic view. The canal is widened to fit a 35-mm vaginal dilator.
Fig. 2.
Laparoscopic view of anatomical landmarks that delineate the anterior and posterior peritoneal flaps to be raised robotically.
Video 2. This video demonstrates penile inversion vaginoplasty surgical technique, part II: peritoneal flap elevation, clitoroplasty, urethroplasty, penile inversion, peritoneal flap inset, and vaginal packing. (Audio credit: https://soundcloud.com/mattquentin.).
Clitoroplasty
The central portion of the glans is excised, and the lateral wings are deepithelialized, creating a 2 × 1-cm flap, which is coned using 3-0 Vicryl (Ethicon, Inc., Somerville, N.J.) stitches to form the clitoris. The dorsal tunica is folded and the apex fixed to the suprapubic region.
Urethroplasty
The bulbar urethra is split on its ventral surface shy of the decussation of the corpora cavernosa, and the edges of the urethra are trimmed. The posterior urethral meatus is everted using 3-0 Vicryl stitches.
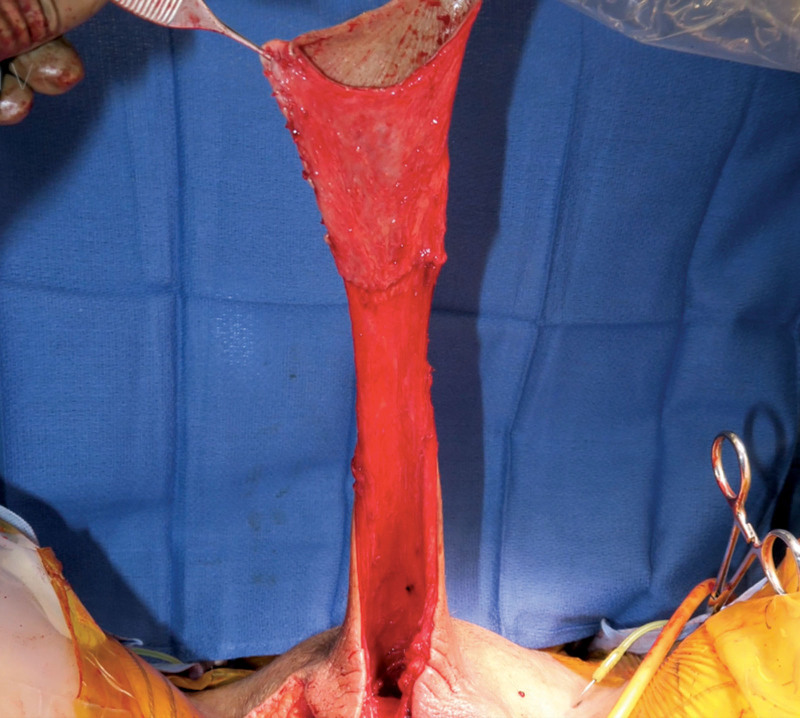
Penile Inversion
The full-thickness scrotal skin graft previously harvested is tubularized over a dilator and sutured to the cuff of penile skin, forming a skin tube that is inverted and then delivered to the robotic surgeon (Fig. 3).
Fig. 3.
Creation of skin tube by suturing of the full-thickness scrotal skin graft to the cuff of penile skin; note the suture line between the two.
Peritoneal Flap Inset
The anterior and posterior peritoneal flaps are then inset by the robotic surgeon to the penile/scrotal skin tube using absorbable barbed suture. The dilator is used to gauge for adequate vaginal depth and width. The lateral edges of the peritoneal flaps are closed with absorbable barbed suture. The apex of the vaginal canal is closed with a three-point stitch at the midline and then run laterally.
Vaginal Packing
The vaginal canal is packed with antibiotic-soaked Kerlix dressing (Cardinal Health, Dublin, Ohio) under direct laparoscopic visualization, confirming that the packing reaches the apex.
PART III
Rhomboid Flap Inset
A rhomboid perineal flap is inset to the posterior floor of the canal with interrupted 3-0 Vicryl. The penile skin that will become the posterior vaginal wall is then incised to the point that it insets into the rhomboid flap to avoid a ski-slope deformity. [See Video 3 (online), which demonstrates penile inversion vaginoplasty surgical technique, part III: rhomboid flap inset, labiaplasty (labia minora), labiaplasty (labia majora), dressings, and postoperative care. (Audio credit: https://soundcloud.com/mattquentin.)]
Video 3. This video demonstrates penile inversion vaginoplasty surgical technique, part III: rhomboid flap inset, labiaplasty (labia minora), labiaplasty (labia majora), dressings, and postoperative care. (Audio credit: https://soundcloud.com/mattquentin.).
Labiaplasty (Labia Minora)
A midline incision on the penile skin is made over the clitoris and the urethral meatus. At this point, the urinary catheter can be delivered. The preputial skin is sutured to the penile skin with a 4-0 chromic running suture. To define the labia minora, 3-0 Vicryl horizontal mattress quilting sutures are placed between the base of the preputial skin medially and the natural sulcus in the penile skin laterally. The clitoral hood is further defined with 3-0 Vicryl horizontal mattress quilting sutures.
Labiaplasty (Labia Majora)
The apex of each scrotal flap is pulled inferiorly and medially. It is important to not pull and inset these flaps laterally, as this will efface the labia. The apex of each scrotal flap is inset to the corners of the rhomboid flap with 3-0 Vicryl. The lateral edges of the scrotal flap are then tailor-tacked closed to the groin, and any skin excess of the labia majora should be trimmed medially, not laterally. The labia majora are left full to account for fat atrophy over time (Fig. 4). The lateral edges of the labia majora are then closed with 3-0 Vicryl and absorbable barbed suture, and the medial edges are closed with 3-0 Vicryl and running 4-0 chromic suture.
Fig. 4.
Postoperative appearance at 9 months.
Dressings
A negative-pressure incisional vacuum-assisted closure device is placed on the vulva, followed by an external compression dressing.
Postoperative Care
An external compression dressing, vaginal packing, Foley catheter, and antibiotics are continued until postoperative day 5. The Foley catheter and vaginal packing are removed on postoperative day 5, and the patient is taught to dilate and is discharged to home.
Although experience and cost are potential limitations of this technique, peritoneal flaps increase vaginal depth and minimize donor-site morbidity associated with extragenital skin grafting and pedicle intestinal segments.7,8 Peritoneal flaps are particularly useful in patients with limited penile and scrotal skin and in revision cases.
Footnotes
Related digital media are available in the full-text version of the article on www.PRSJournal.com.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Horbach SE, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: A systematic review of surgical techniques. J Sex Med. 2015;12:1499–1512. [DOI] [PubMed] [Google Scholar]
- 2.Hadj-Moussa M, Ohl DA, Kuzon WM, Jr. Feminizing genital gender-confirmation surgery. Sex Med Rev. 2018;6:457–468.e2. [DOI] [PubMed] [Google Scholar]
- 3.Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr Urol Rep. 2018;19:36. [DOI] [PubMed] [Google Scholar]
- 4.Jacoby A, Maliha S, Granieri MA, et al. Robotic Davydov peritoneal flap vaginoplasty for augmentation of vaginal depth in feminizing vaginoplasty. J Urol. 2019;201:1171–1176. [DOI] [PubMed] [Google Scholar]
- 5.Davydov SN. Colpopoeisis from the peritoneum of the uterorectal space. Akush Ginekol (Mosk.). 1969;45:55–57. [PubMed] [Google Scholar]
- 6.Davydov SN, Zhvitiashvili OD. Formation of vagina (colpopoiesis) from peritoneum of Douglas pouch. Acta Chir Plast. 1974;16:35–41. [PubMed] [Google Scholar]
- 7.Hage JJ, Karim RB, Asscheman H, Bloemena E, Cuesta MA. Unfavorable long-term results of rectosigmoid neocolpopoiesis. Plast Reconstr Surg. 1995;95:842–848; discussion 849–850. [PubMed] [Google Scholar]
- 8.Dreher PC, Edwards D, Hager S, et al. Complications of the neovagina in male-to-female transgender surgery: A systematic review and meta-analysis with discussion of management. Clin Anat. 2018;31:191–199. [DOI] [PubMed] [Google Scholar]