To the Editor,
We read the article by Dahl and Pripp [2] with great interest. In this well-designed study, the authors conducted a systematic review and meta-analysis and concluded that cemented prostheses were associated with a higher risk of death within 48 hours after surgery compared with uncemented prostheses. We would like to point out some methodological flaws to further refine this important study.
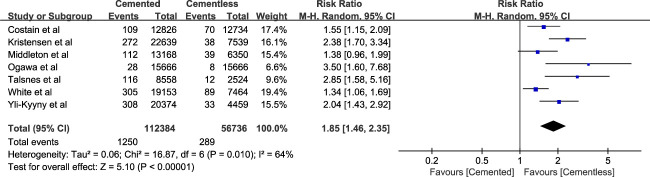
The authors noted in their study that they only searched within two databases (MEDLINE and Embase). We believe that this is not sufficient, and insufficient searches are likely to miss many potentially eligible papers. Therefore, we expanded the database search to Web of Science, Google Scholar, Scopus, and PsycINFO following our own search strategy. To our surprise, two eligible large national registry studies were omitted [4, 7]. Therefore, we combined these two papers with the original five studies [1, 6, 9-11], and the new meta-analysis outcome generally confirmed the conclusions made by the authors (Fig. 1), although the effect sizes differed somewhat.
Fig. 1.
Our reanalyzed forest plot for any mortality within 48 hours after surgery between the cemented and cementless implants.
Additionally, we would like to highlight some methodological shortcomings of this meta-analysis. First, we believe as a matter of principle that all meta-analyses should be pre-registered (in a database like PROSPERO, https://www.crd.york.ac.uk/prospero/); this is important for the same reason that prospective registration of randomized trials is [5]. Second, in the Methods section of the paper, the authors used the Newcastle-Ottawa Scale for assessing study quality. This scale has, at best, unknown validity, and we believe—and others have suggested [8]—that it attributes points for study quality to study design elements that are not necessarily associated with high-quality research. We agree with the analysis by Andreas Stang [8] that using the Newcastle-Ottawa Scale in systematic reviews and meta-analyses may result in a misleading appraisal of the quality of the included studies. We suggest using a modified version of the Downs and Black tool to assess the methodological quality of retrospective studies [3]. Finally, the authors did not suggest whether the recommendations they offer were based on evidence that was sufficiently high-quality to be trustworthy. An important principle of meta-analysis is that not all source studies from which data may arise are similarly well designed and convincing, and a good meta-analysis makes its recommendations in light of that fact. Given the problems with the Newcastle-Ottawa Sale and the other issues we raised, we are unsure whether the evidence in the meta-analysis by Dahl and Pripp [2] meets this standard.
While we are grateful to Dahl and Pripp [2] for contributing research that can guide clinical decision-making, high-quality studies with large sample sizes are still needed to determine whether the risk of death within 48 hours of hip hemiarthroplasty differs between patients treated with cemented and cementless implants
Footnotes
(RE: Dahl OE, Pripp AH. Does the risk of death within 48 hours of hip hemiarthroplasty differ between patients treated with cemented and cementless implants? A meta-analysis of large, national registries. Clin Orthop Relat Res. 2022;480:343-350.)
The institution of one or more of the authors has received, during the study period, funding from Key R&D Program of Gansu Province (21YF5FA154).
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The opinions expressed are those of the writer, and do not reflect the opinion or policy of CORR® or The Association of Bone and Joint Surgeons®.
Contributor Information
Pengfei Shi, Email: shi2919soap@126.com.
Shenghu Zhou, Email: zhou281920xpo2@126.com.
References
- 1.Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop. 2011;82:275-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dahl OE, Pripp AH. Does the risk of death within 48 hours of hip hemiarthroplasty differ between patients treated with cemented and cementless implants? A meta-analysis of large, national registries. Clin Orthop Relat Res. 2022;480:343-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kristensen TB, Dybvik E, Kristoffersen M, et al. Cemented or uncemented hemiarthroplasty for femoral neck fracture? Data from the Norwegian Hip Fracture Register. Clin Orthop Relat Res. 2020;478:90-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leopold SS, Swiontkowski M, Haddad F. Editorial: JBJS, The Bone & Joint Journal, and Clinical Orthopaedics and Related Research require prospective registration of randomized clinical trials-why is this important? Clin Orthop Relat Res. 2017;475:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Middleton RG, Uzoigwe CE, Young PS, Smith R, Gosal HS, Holt G. Peri-operative mortality after hemiarthroplasty for fracture of the hip: does cement make a difference? Bone Joint J. 2014;96-B:1185-1191. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa T, Yoshii T, Okawa A, Fushimi K, Jinno T. Association between cemented vs cementless hemiarthroplasty and short-term change of in-hospital mortality in elderly patients with femoral neck fracture: a propensity-score matching analysis in a multicenter database. Clin Interv Aging. 2021;16:1151-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [DOI] [PubMed] [Google Scholar]
- 9.Talsnes O, Vinje T, Gjertsen JE, et al. Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis: a register study of 11,210 patients. Int Orthop. 2013;37:1135-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White SM, Moppett IK, Griffiths R. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65 535 patients in a national dataset. Anaesthesia. 2014;69:224-230. [DOI] [PubMed] [Google Scholar]
- 11.Yli-Kyyny T, Sund R, Heinanen M, Venesmaa P, Kroger H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop. 2014;85:49-53. [DOI] [PMC free article] [PubMed] [Google Scholar]