Abstract
Social Anxiety Disorder is highly prevalent among children and leads to poor long-term outcomes if left untreated. Theoretical models of anxiety differ in whether children with Social Anxiety Disorder experience objective social skills deficits, negative self-interpretation biases, or some combination of the two. This pilot study evaluated evidence in support of the “deficit” and “bias” models. Approval was obtained from the ethics committee of a large private university in Cambridge, MA, USA, and data collection was completed in 2015. We recruited 68 parent-child dyads for a study in which anxious children (with Social Anxiety Disorder) and non-anxious children underwent a child-adapted version of the Trier Social Stress Test. Children were aged 8–14, 67.6% male, and self-identified as 54.4% White, 7.4% Black, 4.4% Latinx, 13.2% Asian, 14.7% multiethnic, and 5.9% “other” or no response. Performance ratings were obtained from children, their parents, and external observers. We found evidence of both specific social skills deficits and self-appraisal biases in anxious children. Anxious children struggled with signs of physical discomfort but not with actual speech content. Although children were generally able to accurately evaluate their social performance, older anxious children were most self-critical. Parents were similarly accurate in appraisals of their children’s social performance. Anxious children responded favorably to positive feedback with improved self-evaluations of performance and decreased anxiety. Findings suggest that a comprehensive “integrated” theoretical model of Social Anxiety Disorder should include both skills deficits and self-appraisal biases.
Keywords: social anxiety disorder, anxiety, Trier Social Stress Test, child psychopathology, cognitive biases, parent-child dyads
Introduction
Social Anxiety Disorder (SAD) is one of the most prevalent psychological disorders among children, with an estimated lifetime prevalence rate of 12.1% (Ruscio et al., 2008). SAD is characterized by an intense fear of embarrassment, humiliation, and negative evaluation, and avoidance of social situations in which these might occur (e.g., public speaking) (Guha, 2014). Unlike many other anxiety and mood disorders, SAD’s onset is at a relatively early age with diagnosis as early as age 8 and a mean age of onset of 15.5 years-old (Kashdan & Herbert, 2001). In children, SAD is associated with social isolation, academic impairment and truancy, and the development of comorbid depression and substance abuse (Beidel et al., 1999). The disorder seriously undermines children’s social and emotional development, and typically follows a chronic course if left untreated (Kessler et al., 2005). This can further lead to low quality of life into adulthood, including comorbid depression and alcoholism, and functional impairment in work, education, and relationships (Weeks et al., 2008).
Adult theoretical models of SAD are among the best-established, with Clark & Wells (1995) and Rapee & Heimberg (1997) positing that dysfunctional beliefs/assumptions lead to negative interpretation biases of social situations and the continued maintenance of anxiety (Clark & Wells, 1995; Rapee & Heimberg, 1997). Such anxiety maintenance models have provided a strong theoretical foundation informing evidence-based interventions. Additionally, it has been theorized that positive social interactions increase confidence and a sense of self-efficacy in individuals with SAD, whereas negative interactions decrease them (Beck et al., 2005; Haemmerlie & Montgomery, 1982). Research has examined the applicability of adult theoretical models to childhood SAD (Hodson et al., 2008). While recent meta-analyses show moderate mean effect sizes of youth anxiety treatment (Weisz et al., 2017; Weisz et al., 2019), some have argued that the effectiveness of youth interventions lag far behind that of their adult counterparts (Halldorsson & Creswell, 2017).
Social Skills Deficits or Self-Appraisal Biases
Two bodies of theory and research suggest a connection between childhood SAD and social skills deficits and biases in self-evaluation. A recent review summarized the strength of the current evidence for dysfunctional beliefs/assumptions and performance deficits (among other factors) in both clinical and nonclinical populations (Halldorsson & Creswell, 2017). A proposed “deficit model” holds that poor social skills lead to ineffective and discouraging interpersonal interactions, which then cause and maintain significant anxiety and distress (Inderbitzen-Nolan et al., 2007; Turner et al., 1994). An alternative “bias model” holds that individuals with SAD devote attentional resources to negative threat cues and exhibit a hypercritical cognitive style in evaluating their own performance in social interactions (Beck et al., 2005; Rapee & Heimberg, 1997). This can lead to negative expectations for and subsequent avoidance of future social interactions, which further decreases opportunities to develop social skills, maintaining and further exacerbating social anxiety (Wallace & Alden, 1997). An “integrated model” would allow for the presence of both underlying deficits and biases (Hopko et al., 2001; Spence et al., 1999). Indeed, an etiological model of SAD suggests evidence of both skills deficits and negative interpretation biases (Spence & Rapee, 2016).
Few studies to-date have assessed objective social skills deficits in children with SAD, and the findings are mixed (Schmitz et al., 2010; Schmitz et al., 2011). Additionally, in the few studies that have examined parent appraisals, findings suggest that parents of socially anxious children evaluate their children as less socially skilled than parents of non-anxious children, but it is unknown whether these appraisals are accurate (Ginsburg et al., 1998; Kortlander et al., 1997; Spence et al., 1999). Some direct observation studies of non-clinical cohorts have found that external observers rate socially anxious children’s performance worse than age-matched non-anxious controls on social interaction tasks (including conversational role plays and reading aloud) (Beidel et al., 1999; Norton & Hope, 2001). Other studies have found that children with SAD performed no worse than non-anxious controls on social interaction tasks when rated by external observers, but that self-ratings of performance were significantly lower for children with SAD than for non-anxious controls (Cartwright-Hatton et al., 2005; Krämer et al., 2011; Tuschen-Caffier et al., 2011). Perhaps children with SAD lack positive self-serving biases consistently found in the general population (Taylor & Brown, 1988; Zell et al., 2020).
Relevant Demographic Characteristics
Previous research has shown that in youths with SAD, adolescents are distinct from younger children in that they present with higher rates of suicidal ideation and excessive self-focused attention in social situations (Albano et al., 1995; Francis et al., 1992). Adolescence is commonly considered a key developmental stage for identity formation and social skills development, demarcated in part by preoccupations with peer acceptance and body image (Petersen & Leffert, 1995). This suggests that age effects may warrant special research attention due to socio-cognitive maturation and particular vulnerability during adolescence to cognitive distortions and pessimism about one’s performance in social situations (Elkind & Bowen, 1979; Westenberg et al., 2004). Previous research has also shown potential gender differences in SAD with higher prevalence, risk of psychological maladjustment, and worse social functioning and impairment in girls (Ginsburg et al., 1998). Although this has not previously been tested, literature suggests that boys may respond more positively to ability praise and girls to effort praise (Blumenthal et al., 2011; Koestner et al., 1989).
Study Objectives
Examining whether children with SAD and parent perceptions of performance are accurate or negatively biased could have significant treatment implications. If socially anxious children exhibit skills deficits and are accurate in their negative self-assessments, then social skills training might be appropriate (Miers et al., 2009). In fact, therapy designed to make their self-assessments more positive rather than addressing underlying skills deficits could serve as a real disservice to these children. On the other hand, if socially anxious children’s self-perceptions and parents’ perceptions are in fact negative cognitive distortions, a cognitively focused intervention approach might be appropriate. In this case, social skills training would be an unnecessary use of intervention time, and might be potentially harmful, implying that the therapist agrees with negatively biased appraisal of the child and parent.
Taken together, previous studies have added relevant evidence but findings are mixed, have been underexplored in clinical populations, and few have utilized objective skills tasks (Halldorsson & Creswell, 2017). We aimed to build on the background literature examining whether the “deficit model”, “bias model”, or perhaps some combination of the two in an “integrated model” accurately encapsulates the experiences of socially anxious children. The present study was designed to complement the aforementioned prior studies in this important area of research (Cartwright-Hatton et al., 2003; Cartwright-Hatton et al., 2005; Inderbitzen-Nolan et al., 2007; Krämer et al., 2011; Miers et al., 2009).
Unique to our pilot study, we collected evaluations from multiple relevant subjective and objective reporters: anxious children with SAD and their parents, evaluations from non-anxious children and their parents, and external observer evaluations. We focused on whether socially anxious children, compared to their non-anxious peers, (a) perform worse on a public speaking task; (b) rate themselves worse on the task; (c) respond to positive evaluative feedback with more change toward positive self-ratings of performance; (d) experience greater reductions in anxiety after receiving positive external feedback; and, (e) have parents with lower expectations for their child’s social skills. As the literature to-date is mixed, this study was framed to address specific research questions (a) - (e) rather than directional hypotheses; a number of different findings could have hypothesis-generating value for the field, with implications for the treatment of childhood SAD. In addition, we conducted exploratory analyses assessing age and sex as moderators of children’s self-perceptions of speech performance.
Method
Sample
68 parent-child dyads participated in the pilot study. 34 of the child participants had a SAD diagnosis, and 34 were non-anxious healthy controls. Exclusion criteria for the SAD group included current comorbid non-anxiety psychological disorder(s), and current psychotropic medication use. The age range of children was 8 – 14 years (M = 11.08, SD = 1.98); 22 were male. 54.4% self-identified as White, 7.4% Black, 4.4% Hispanic/Latino, 13.2% Asian, 14.7% multiethnic, 1.5% self-identified as “other”, and 4.4% did not provide ethnicity information. Participants were recruited through community organizations (e.g., afterschool programs), local schools, hospitals, and online advertisements (e.g., Craigslist, parenting listservs). Two sets of flyers were distributed, one targeting parents of socially anxious children, and the second advertising a generic study on child development. Approval was obtained from the ethics committee of a large private university in the United States (IRB No. 24143), and data collection was completed in 2015 in Cambridge, MA.
Procedure
During the lab visit, informed assent was obtained by the child participant and consent from the parent participant. An advanced clinical psychology doctoral student then administered the SAD module of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions (Albano & Silverman, 1996) (ADIS-IV-C/P) to the child and parent separately to determine SAD status. The child version of the ADIS-5 for DSM-5 has not yet been released but diagnostic criteria for SAD remain unchanged between the DSM-IV and DSM-5. The parent completed a set of baseline questionnaires, which included parenting questionnaires and measures of their own anxiety and their child’s psychological symptoms. Members of the research team administering parent questionnaires were blind to child’s status in either the SAD or control group, and questionnaire responses were not reviewed until after study completion. The child also completed a set of baseline questionnaires, which included self-report measures of anxiety and psychological symptoms. Next, the child engaged in a public speaking task. We used a child-adapted version of the Trier Social Stress Test (TSST), shortened in duration and with child-relevant speech topics (Kirschbaum et al., 1993). A strength of the TSST is that it is a well-established and widely used standardized social stress task; meta-analytic findings suggest that the TSST is the most appropriate and useful protocol to reliably elicit social-evaluative fears in a controlled research environment (Birkett, 2011; Dickerson & Kemeny, 2004). Validity data are reported in the Results section below. The child and parent were given five minutes to prepare a 5-minute speech on one of five topics (family, favorite vacation, hobbies, school, or sports). Next, the child gave a 5-minute practice speech to one of three “committee members” they were told would be judging their speech. Finally, the child gave a 5-minute speech in front of the committee, who were undergraduate lab assistants, maintaining neutral affect and taking notes on the child’s performance during the speech. If the participant stopped talking before time was up (i.e., a 10-second pause), committee members gave the child standard prompts such as “you still have some time left, please continue,” and “try to tell us something more about (topic)”. The speeches were videotaped for observational coding. After the child’s speech, the committee left the room to deliberate and returned to give the child positive feedback on speech performance. Positive feedback was realistic and tailored to individual strengths of the speech content or delivery. Child and parent participants completed measures before committee feedback (study measurement model, Table 1).
Table 1.
Study measurement model
| Baseline | Post-Speech | Post-Feedback |
|---|---|---|
| CHILD | ||
| ADIS-IV-Child | POP-Child SUDS | POP-Child SUDS |
| PARENT | ||
| ADIS-IV-Parent | POP-Parent | |
| EXTERNAL OBSERVER | ||
| POP-External Observer | ||
Note. ADIS-IV is the Anxiety Disorders Interview Schedule for DSM-IV. POP is the Perception of Performance Questionnaire. SUDS are Subjective Units of Distress Scale ratings.
Measures
Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions (ADIS-IV-C/P).
The ADIS-IV-C/P (Albano & Silverman, 1996) is a semi-structured diagnostic interview designed to assess anxiety and related disorders; it has shown good to excellent inter-rater reliability and test-retest reliability (Silverman et al., 2001).
Perception of Performance Questionnaire-Child (POP-Child).
The child’s brief speech evaluation questionnaire consists of two items rated on an 11-point Likert scale. Item #1: “How do you think you did on the speech?” 0 = really badly, 10 = really good. Item #2: “How much do you think the committee liked your speech?” 0 = not at all, 10 = very much. The child completed the questionnaire on two occasions, once immediately after the speech and again after receiving feedback from the committee. Internal consistency was α = 0.92 for the Perception of Performance Questionnaire-Child total score post-speech, and 0.86 at post-feedback. The POP-Child was administered to a subset of study participants as this measure was added to study procedures after data collection was underway.
Perception of Performance Questionnaire-Parent (POP-Parent).
Immediately after the speech, the parent completed a brief speech evaluation questionnaire consisting of two items rated on an 11-point Likert scale. Item #1: “How do you think your child performed on the speech?” 0 = very badly, 10 = very well. Item #2: “How much do you think the committee liked your child’s speech?” 0 = not at all, 10 = very much. Internal consistency of the Perception of Performance Questionnaire-Parent total score was α = 0.80 for our sample. The POP-Parent was administered to a subset of study participants as this measure was added to study procedures after data collection was underway.
Subjective Units of Distress Scale (SUDS).
SUDS ratings are a well-validated and commonly used measure of anxiety levels during research- and treatment-related exposure tasks for youths (Benjamin et al., 2010; Kiyimba & O’Reilly, 2020; McCabe, 2015). SUDS ratings were administered at 11 timepoints (including post-speech and post-committee feedback) to measure change in anxiety levels throughout the study session. The scale ranges from “0-not at all anxious” to “8-very, very much anxious” and a “feelings thermometer” was displayed as a visual aid for the ratings scale (Kendall et al., 2005).
Observational Coding.
A main coder rated all videotaped speeches, and a reliability coder rated half of the videotaped speeches. Coders were blind to psychopathology status (i.e., whether the child was socially anxious or in the healthy control group). Evaluations on global speech performance were rated on the Perception of Performance Questionnaire-External Observer (POP-External Observer). Item #1: “How do you think the child performed on the speech?” 0 = very badly, 10 = very well. Item #2: “How much do you think the committee liked the child’s speech?” 0 = not at all, 10 = very much. Internal consistency of the Perception of Performance Questionnaire-External Observer total score (α = 0.99) was high for our sample.
Social skills are conceptualized in the background literature as social or interpersonal behaviors exhibited to complete a social task (e.g., communication, visible displays of anxiety) (Hebert-Myers et al., 2006; Inderbitzen-Nolan et al., 2007; Klein et al., 2021; McDaniel et al., 2017; Spence & Rapee, 2016). Objective assessments of social skills are rated based on behavioral assessments of performance in social interactions such as the Social Performance Rating Scale (SPRS) which has been shown to exhibit convergent, divergent, and criterion validity (Fydrich et al., 1998). Specific social skills were rated on a modified version of the SPRS (Fydrich et al., 1998). The SPRS is an observational coding system on specific social skills designed for ratings of conversations between two people, and has shown excellent interrater reliability for assessing both individuals with social phobia and healthy controls (Fydrich et al., 1998). For the purposes of our study, we retained the original skills categories of eye contact, vocal quality (e.g., vocal inflections/nuances, appropriate volume), discomfort, and speech flow (e.g., speech content) and made slight modifications to coding manual descriptions so that the content was more appropriate for a child speech (modified version of SPRS, Appendix 1).
Interrater Reliability of External Ratings of Speech Performance
Interrater reliability on the SPRS was calculated via intra-class correlations (ICCs) (Hallgren, 2012) between 2 coders on a random sample of 35 videos (51% of participants). ICCs showed good to excellent interrater reliability (Cicchetti, 1994), ranging from 0.669 (discomfort) to 0.829 (speech flow) on speech microcodes. Global ratings of speech performance on the POP-External Observer showed ICCs of 0.835 for how well the child did on the speech, and 0.872 for how well the committee liked the speech, respectively.
Analytic Plan
Descriptive statistics are reported for means, standard deviations, ranges of, and correlations among, key study variables. A power calculation was conducted with program G*Power (Erdfelder et al., 1996). We conducted one-way ANOVAs to determine whether there were significant group differences between (a) anxious and non-anxious children and (b) parents of anxious and non-anxious children on their perceptions of speech performance. Additionally, we conducted one-way ANOVAs of difference scores (self-rating - observer rating) for children and parents to adjust for objective ratings of performance. Paired sample t-tests were used to evaluate changes in children’s self-perceptions of performance and anxiety levels pre- and post-committee feedback. Due to small sample size constraints and limited power, we were unable to conduct multivariable analyses although we did confirm that potential confounders such as age and sex were balanced between groups. We used linear regression to conduct exploratory analyses assessing age and sex as moderators of children’s self-perceptions of speech performance. All analyses were conducted in IBM SPSS Statistics 25.0.
Results
The Trier Social Stress task has previously been demonstrated to reliably elicit social-evaluative fears, and this was supported in our study. Across the full sample, child self-reported anxiety (i.e., SUDS ratings) increased by 2.76 from baseline to post-speech task, t(67) = 7.45, p < .01. This validity data suggests that the social evaluative task achieved its intended goals. Table 2 contains the means, standard deviations, ranges of, and correlations among, key study variables. Correlations between key variables are shown in Table 3. A power analysis suggested that a sample size of 52 would be sufficient to detect large effect sizes with a power of 0.8.
Table 2.
Means, standard deviations, and ranges of key study variables.
| Pre-Feedback POP | Post-Feedback POP | Parent POP | External Observer POP | Pre-Feedback Anxiety Rating | Post-Feedback Anxiety Rating | |
|---|---|---|---|---|---|---|
|
| ||||||
| Full Sample | ||||||
| M | 10.24 | 15.41 | 14.76 | 12.99 | 4.45 | 1.79 |
| (SD) | (4.71) | (4.92) | (3.66) | (3.23) | (2.67) | (1.89) |
| Range | 0 – 20 | 0 – 20 | 4 – 20 | 4 – 20 | 0 – 8 | 0 – 8 |
| N | N = 41 | N = 41 | N = 41 | N = 68 | N = 68 | N = 68 |
|
| ||||||
| SAD | ||||||
| M | 9.81 | 15.04 | 14.46 | 12.63 | 4.82 | 2.09 |
| (SD) | (5.62) | (5.68) | (4.04) | (3.41) | (2.58) | (2.15) |
| Range | 0 – 20 | 0 – 20 | 4 – 20 | 4 – 18.5 | 0 – 8 | 0 – 8 |
| N | N = 24 | N = 24 | N = 24 | N = 34 | N = 34 | N = 34 |
|
| ||||||
| Non-Anxious Control | ||||||
| M | 10.85 | 15.94 | 15.18 | 13.35 | 4.07 | 1.50 |
| (SD) | (3.07) | (3.68) | (3.11) | (3.05) | (2.75) | (1.56) |
| Range | 6 – 18 | 7 – 20 | 6 – 19 | 7.5 – 20 | 0 – 8 | 0 – 6 |
| N | N = 17 | N = 17 | N = 17 | N = 34 | N = 34 | N = 34 |
Table 3.
Correlations among key study variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Pre-Feedback POP | - | |||||
| 2. Post-Feedback POP | 0.68 ** | - | ||||
| 3. Parent POP | 0.04 | 0.23 | - | |||
| 4. External Observer POP | 0.26 | 0.39 * | 0.50 ** | - | ||
| 5. Pre-Feedback Anxiety Rating | −0.45 ** | −0.20 | 0.24 | −0.07 | - | |
| 6. Post-Feedback Anxiety Rating | −0.50 ** | −0.54 ** | −0.11 | −0.19 | 0.57 ** | - |
indicates p < .05
indicates p < .01
Child Evaluations of Speech Performance
Pre-feedback.
A one-way ANOVA showed no significant group differences for socially anxious children compared to non-anxious peers on global self-ratings of speech performance, F(1,39) = 0.48, p = .49. Similarly, a one-way ANOVA of difference scores (self-rating - observer rating) showed no significant group differences between socially anxious children and non-anxious peers in self-ratings of speech performance, F(1,39) = 0.00, p =.99.
Post-feedback.
Paired sample t-tests showed a significant increase in global self-ratings of speech performance after positive committee feedback for SAD children (t(23) = −5.40, p < .001) and their non-anxious peers (t(16) = −9.21, p < .001) (Figure 1). One-way ANOVA of difference scores showed no significant group differences between SAD children and non-anxious peers in self-ratings of speech performance from pre- to post-feedback, F(1, 39) = 0.01, p = .91. Paired sample t-tests showed a significant decrease in children’s self-ratings of anxiety after positive committee feedback for SAD children (t(33) = 7.43, p < .001) and non-anxious peers (t(33) = 6.37, p < .001) (Figure 2). One-way ANOVA of difference scores pre- and post-feedback showed no significant group differences between SAD children and non-anxious peers in self-ratings of anxiety from pre- to post-feedback, F(1, 66) = 0.09, p = .77.
Figure 1.
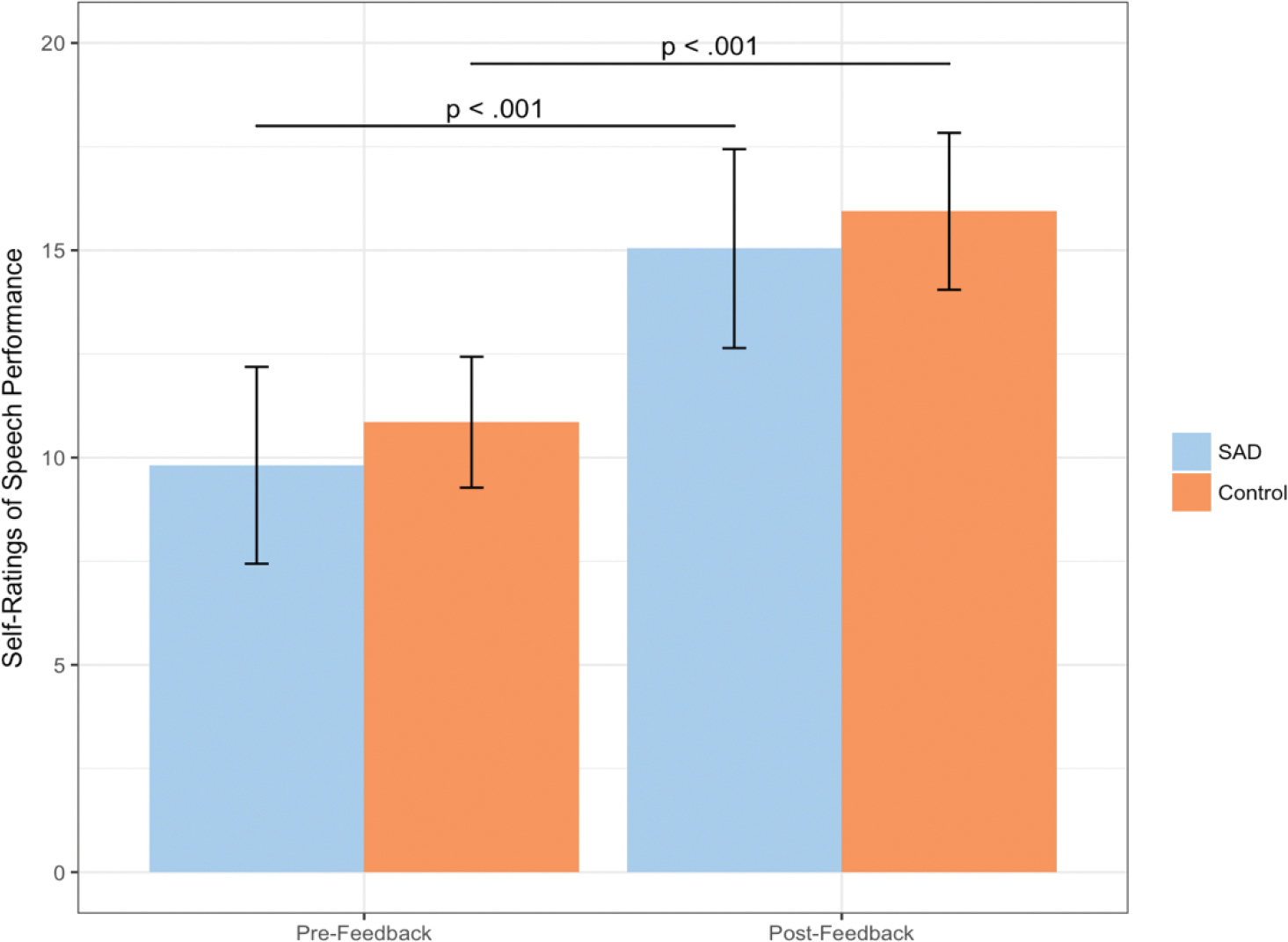
Mean child self-ratings of speech performance on the Perception of Performance-Total Scores
Figure 2.
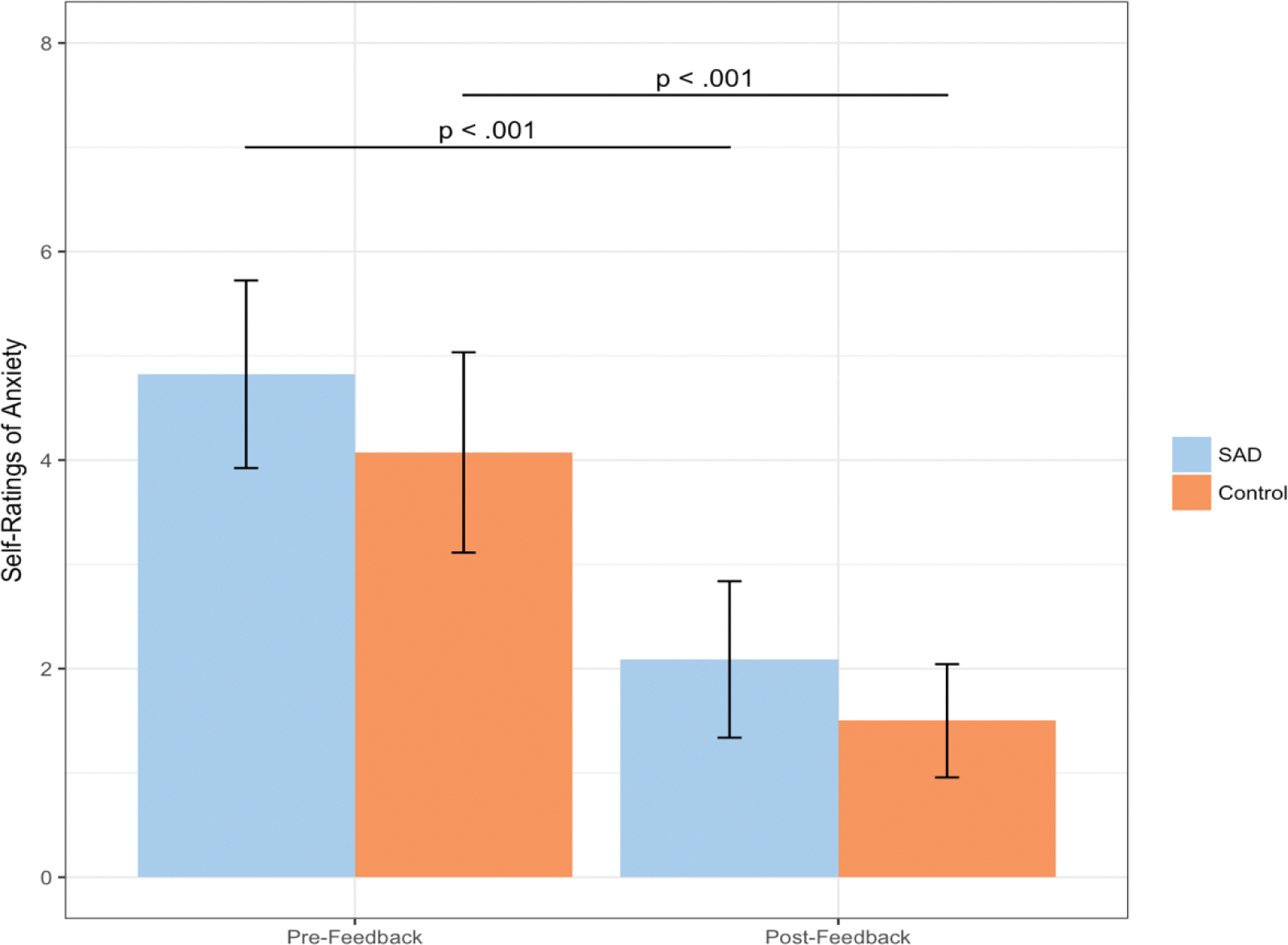
Mean child self-ratings of anxiety on the Subjective Units of Distress Scale
Age as Potential Moderator.
A multiple regression analysis showed that a diagnosis of SAD was not a significant predictor of global self-ratings of speech performance pre-feedback on the Perception of Performance Questionnaire-Child nor was child’s age. However, there was a significant group (SAD vs. healthy controls) x age interaction effect on self-ratings of speech performance pre-feedback (β = −0.49, t(37)= −2.25, p = .03, η2 = .09) and post-feedback (β = −0.48, t(37)= −2.09, p = .04, η2 = .09). Main effects were not significant given that this was a cross-over interaction. Increasing age predicted lower self-ratings only in the SAD group at both pre- and post-feedback with an inflection point during pre-adolescence whereas self-ratings remained consistent regardless of age in the control group (Figure 3).
Figure 3.
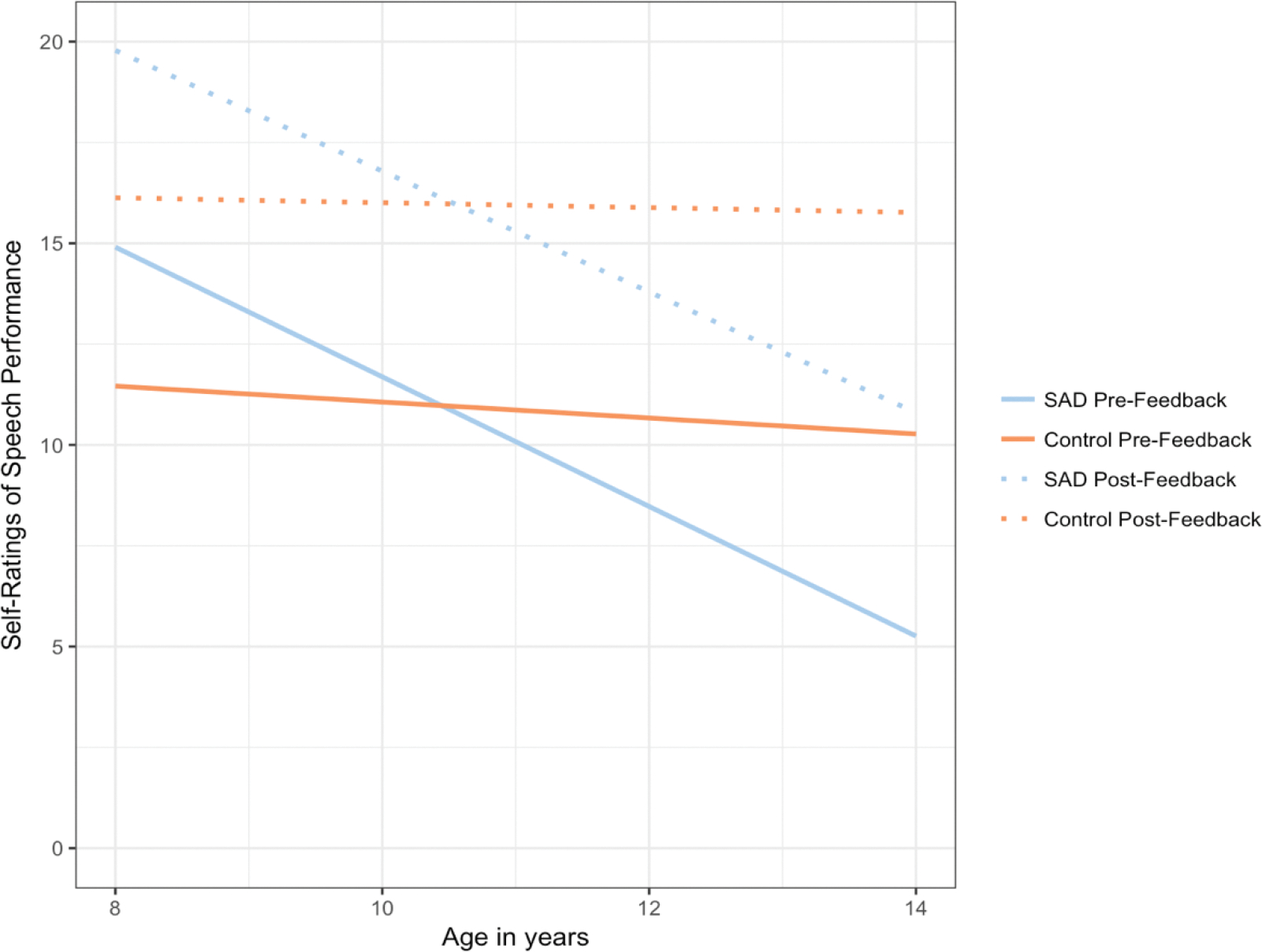
Interaction effect of child age x group (socially anxious children vs. healthy controls) such that increasing age predicted lower self-evaluations of speech performance only in the SAD group at both pre- and post-feedback
Sex as Potential Moderator.
A multiple regression analysis showed that a diagnosis of SAD was not a significant predictor of global self-ratings of speech performance on the Perception of Performance Questionnaire-Child pre- or post-feedback, nor was child sex. However, post-feedback, the group (SAD vs. healthy control group) x sex interaction trended toward significance, β= −.62, t(37)= −1.90, p = .07, η2 = .09. Main effects were not significant given that this was a cross-over interaction. After receiving positive feedback from committee members, boys in the SAD group rated their speech performance higher than boys in the control group, whereas girls in the SAD group rated their speech performance worse than girls in the control group.
Parent Evaluations of Child Performance
A one-way ANOVA showed no significant group differences between parents of socially anxious children and parents of non-anxious children in global ratings of their children’s speech performance on the Perception of Performance Questionnaire-Parent, F(1,39) = 0.38, p = .54. Similarly, a one-way ANOVA of difference scores (self-rating - external observer) showed no significant group differences in parents’ ratings of their children’s speeches, F(1,39) = 0.08, p = .78.
External Observer Ratings of Speech Performance
A one-way ANOVA showed no significant group differences on external observer ratings of children with SAD compared to non-anxious peers on global ratings of child speech performance, F(1,66) = 0.84, p = .36. One-way ANCOVAs controlling for child age showed no significant group differences on external observer ratings of eye contact (F(1,66) = 0.79, p = .38) or speech flow/content (F(1,66) = 0.73, p = .40) in socially anxious children compared to healthy control children during their speeches. One-way ANOVAs showed a significant group difference on external observer ratings of physical comfort level (F(1,66) = 5.15, p = .03, η2 = .07) and a marginal group difference on vocal quality (F(1,66) = 3.58, p = .06, η2 = .05) in socially anxious children compared to healthy control children during their speeches; non-anxious children were given higher ratings on physical comfort level and vocal quality (Figure 4).
Figure 4.
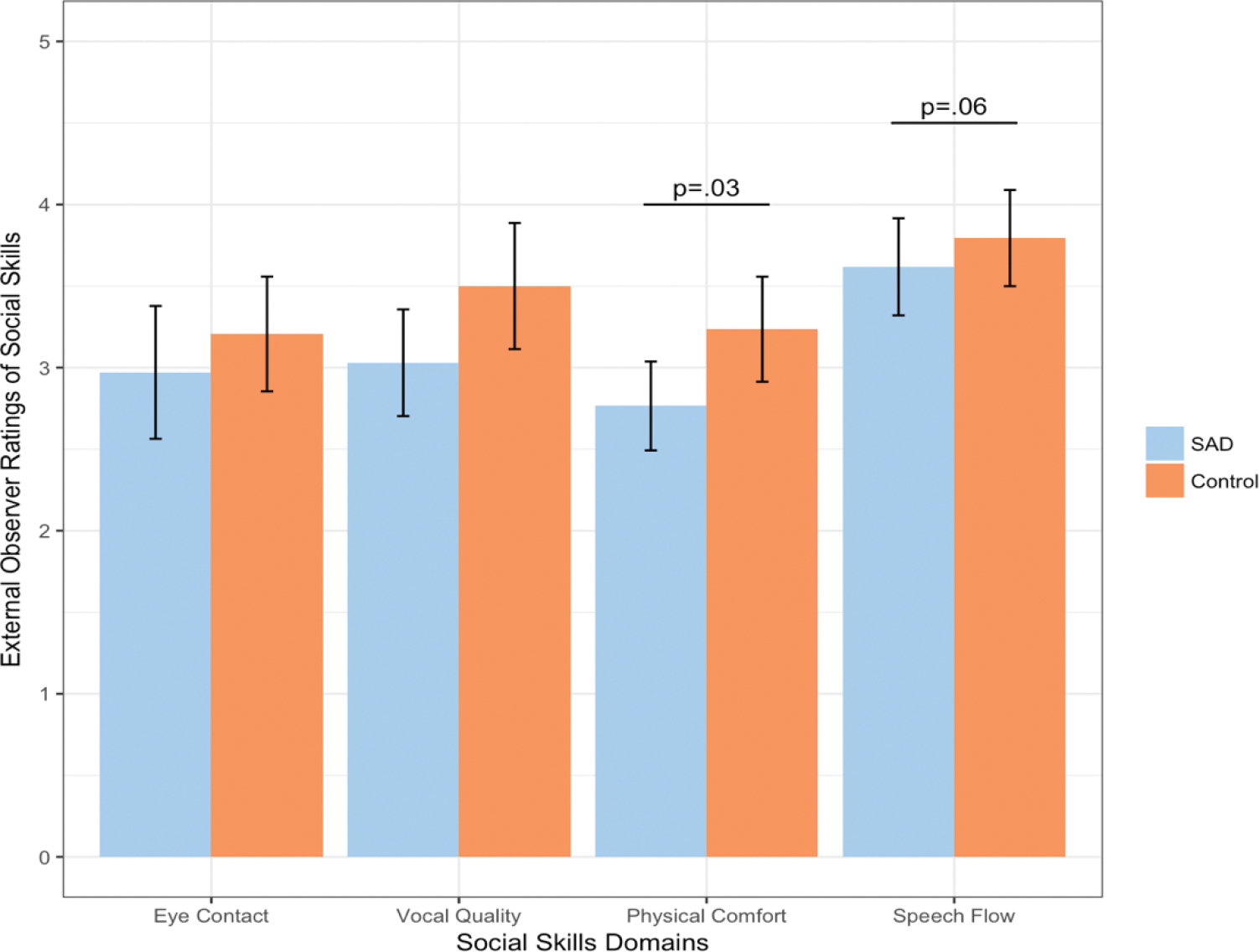
External observer mean ratings of child speech performance for the social skills domains of eye contact, vocal quality, physical comfort, and speech flow/content for children with Social Anxiety Disorder compared to healthy controls
Discussion
Some researchers have proposed a “deficit model” in which social skills deficits serve as an underlying causal and maintaining factor of SAD, others a “bias model” in which socially anxious individuals exhibit negative cognitive biases and a hypercritical cognitive style in evaluating their own performance in social situations which serve as an underlying causal and maintaining factor of SAD, and still others a “integrated model” combining elements of both (Halldorsson & Creswell, 2017; Rapee & Heimberg, 1997; Spence et al., 1999).
An important question for psychotherapy for children with SAD is whether the disorder primarily involves a skills deficit or an appraisal bias involving underestimates of skill. The current pilot study contributes to the literature on this growing topic (Cartwright-Hatton et al., 2003; Cartwright-Hatton et al., 2005; Inderbitzen-Nolan et al., 2007; Krämer et al., 2011; Miers et al., 2009); we utilized a well-established behavioral paradigm and collected data from multiple relevant reporters including children, parents, and external observers. Research that sheds light on this question has implications for appropriate intervention such as whether the main focus of psychotherapy should be on skills-building or cognitive restructuring. Answering this question could help us improve existing therapeutic interventions for socially anxious youths, as although Cognitive Behavioral Therapy (CBT) is the gold standard method of treatment for anxious youths, up to 50% still exhibit symptoms after treatment (Ginsburg et al., 1998).
We found that socially anxious youths and their age-matched non-anxious peers generate similar global ratings of speech performance by external observers, but a more granular level of analysis revealed group differences: specific skills deficits among socially anxious children in vocal quality and physical comfort level. Interestingly, the quality of speech content was rated similarly for socially anxious youths and their non-anxious peers. This pattern of findings suggests that socially anxious youths may not need help with what to say but rather how to say it. This is consistent with previous research that suggests social skills deficits in anxious youths may be specific to external signs of anxiety (i.e., “looking nervous”) (Cartwright-Hatton et al., 2003; Cartwright-Hatton et al., 2005). Appropriate targets for skills-based interventions might involve, for example, incorporating vocal inflections into speech and adjusting body language to minimize signs of physical discomfort. Perhaps promisingly, we also found that socially anxious children rated themselves more favorably on social performance after receiving positive external feedback that coincided with a corresponding decrease in anxiety, and in a manner that was consistent with the response of non-anxious peers. This may possibly suggest that positive feedback can be internalized by anxious and non-anxious children similarly, and that it may alter negative self-evaluations. Although these improvements in self-evaluation and anxiety were observed within the timeframe of pre- and post-feedback, another possibility should be noted—i.e., that simple exposure to the feared stimulus itself (i.e., giving the speech) was the primary driver of such changes.
Overall, we found that socially anxious youths were not unrealistically critical of their own speech performance or their perceptions of how well their speech was received by an external committee. Children with SAD were generally able to accurately evaluate their own performance and skills on a social-evaluative task involving public speaking. Parents of socially anxious children were similarly accurate in their appraisals of their child’s speech performance which suggests that they are not hypercritical of their child’s social skills. Of note, when we explored age and sex as potential moderators, we found differential impact on self-appraisal biases only in the subgroup of children with SAD. We found age effects such that older children/young adolescents who were socially anxious were most self-critical of their own performance, and significantly more so than their age-equivalent non-anxious peers. This is consistent with previous research suggesting that adolescence is a key developmental period for self-consciousness, self-awareness, and social-evaluative fears – i.e., “adolescent egocentrism” characterized by the belief that one is the object of everyone’s attention (Elkind & Bowen, 1979; Westenberg et al., 2004). Clark and Wells’s (1995) cognitive model of SAD posits that socially anxious individuals exhibit excessive self-focused attention, and that self-focused attention increases access to negative thoughts and feelings, leading individuals to generate and internalize a negatively distorted impression of themselves. Thus, the cognitive restructuring component of CBT may be especially relevant for anxious adolescents and less so for younger children. We also found that although self-ratings of performance did not differ between boys and girls, boys with SAD were more likely to internalize positive feedback with respect to speech content or delivery; this suggests that self-criticism is more likely to persist in girls even in the face of external feedback to the contrary. Although this has not previously been tested, literature suggests that boys may respond more positively to ability praise (which was the focus of positive feedback in our study) and girls to effort praise (Koestner et al., 1989).
To frame our findings based on the cognitive triad in CBT – i.e., the relationship among thoughts, feelings, and behaviors: (a) thoughts: Anxious children were generally able to accurately appraise their social performance, except for the vulnerable developmental period of adolescence characterized by hypercritical self-evaluations; (b) feelings: Anxiety levels were elevated for anxious children during the course of exposure, and declined post-exposure and after receiving positive social feedback; and, (c) behaviors: Social skills deficits observed were specific to physical manifestations of anxiety (i.e., vocal quality, physical comfort).
Our study has certain methodological limitations. First, although the focus of our experimental task on public speaking was appropriate because this is the most commonly endorsed feared among socially anxious children, our ability to generalize findings to other social situations is limited (Van West et al., 2008). Second, we did not evaluate older adolescents (>14 years of age) in our study, and older youths may experience even more pronounced age effects of self-criticism and self-appraisal biases (Sumter et al., 2010; Westenberg et al., 2007). Third, although the non-anxious group did not endorse SAD symptoms or report previous or current mental health diagnoses, it is possible that additional psychopathology may have been uncovered with a full diagnostic interview. Fourth, our relatively small sample size limited: statistical power to detect an effect; the conduct of multivariable analyses to examine potential confounders; and, the testing of demographic variables as potential moderators. While a power analysis suggested that a sample size of 52 would be sufficient to detect large effect sizes, some of our analyses involved missing data, and the analyses that were conducted yielded small to moderate effect sizes. We acknowledge that the number of tests conducted and use of unadjusted p-values increase the risk of Type 1 error and false positives. Thus, we intend the findings from our pilot study to be interpreted as preliminary and hypothesis-generating in nature. Fifth, we utilized a standardized laboratory social stressor task to elicit social evaluative fears, and this may limit generalizability to naturalistic social situations such as interactions with peer groups. Sixth, due to the short-term nature of our study timeframe, it remains unclear whether our results would be sustainable over time. Finally, we acknowledge that additional factors may contribute to the maintenance of anxiety that are beyond the scope of the current study (e.g., genetic predisposition, cultural/contextual variables, peer influences). Similarly, relative impact of maintenance factors may differ between and among individuals with heterogeneous presentations of anxiety.
Future Directions
Further research on social skills deficits and cognitive distortions in children and adolescents with SAD and study replication in a larger cohort is warranted. One focus of this work should involve examining differences in SAD symptomatology across development, including potentially changing presentations from early childhood through adolescence, given increases in social-evaluative concerns with age, even within typical development. A second focus of this work should involve examining gender differences in self-evaluations of social performance and internalizing of positive feedback. Our exploratory analyses suggest that theoretical models for SAD may need to be modified based on developmental stage and gender. A third focus of future research should be treatment selection. CBT protocols may be most beneficial when targeted to specific age groups based on utility of cognitive vs. behavioral principles. To the extent that self-appraisals of social performance are accurate, exposure may be explored as a beneficial standalone treatment in younger children. Given a pronounced increase in self-criticism and negative self-appraisal biases in adolescence, cognitive restructuring may be an especially important treatment focus. A fourth useful focus for future research is evaluation of social skills deficits and self-appraisal biases in a range of naturalistic settings for commonly endorsed fear situations—e.g., talking to new people, peer interactions, talking to adults, and starting or joining a conversation (examples from van West et al., 2008)—in order to explore whether deficits or bias are differentially likely in different contexts. Finally, future research should include immediate, short-term (weeks-long timeframe), and longer-term timepoints (months-long timeframe) to evaluate whether effects are maintained over time.
Summary
We recruited 68 parent-child dyads for a child-adapted Trier Social Stress Test. Our pilot study uniquely incorporated comprehensive perspectives from anxious and non-anxious parent-child dyads and neutral observers to provide further support for an “integrated” theoretical model for childhood SAD that incorporates both the “deficit model” (underlying social skills deficits) and the “bias model” (underlying self-appraisal biases). Future research should continue to incorporate the use of independent evaluators of children’s social competence in order to tease apart the role of objective skills deficits vs. subjective interpretation biases in the onset and maintenance of SAD. Our findings also suggest that a finer grained level of analysis is warranted. We found specific skills deficits in anxious children’s speech delivery (vocal quality and physical discomfort) but not in speech content. In addition, we found that older anxious children were most self-critical and that boys were more likely to respond favorably to positive feedback. Future studies should focus on strategies for precise assessment of the specific deficits for specific individuals in order to permit better personalizing of interventions.
Highlights.
This parent-child dyadic study utilized a behavioral paradigm – the Trier Social Stress Test – to examine social skills deficits and self-appraisal biases in anxious children from the perspective of multiple reporters (child, parent, and external observer).
We found evidence of both specific social skills deficits and self-appraisal biases in anxious children.
Parents of anxious children were not hypercritical or inaccurate in appraisal of their children’s social skills.
Our study supports a comprehensive “integrated” theoretical model of anxiety.
Funding:
Dr. Nancy Lau is funded as an Implementation Science Scholar through the National Heart, Lung, and Blood Institute of the National Institutes of Health (Grant number: 5K12 HL137940-02).
Appendix 1. Behavioral anchors for the Social Performance Rating Scale (SPRS) (as adapted from the SPRS; Fydrich et al, 1998)
1. GAZE
Very Poor: Participant completely avoids looking at the audience or stares continually and intently at audience member directly in front of him/her in an uncomfortable manner (i.e., no eye contact or stares down audience member). Gaze pattern is very disruptive to performance.
Poor: Participant frequently avoids looking at the audience (or stares intently at audience member directly in front of him/her) for majority of time. Gaze pattern is disruptive to performance.
Fair: Participant avoids eye contact or tends to look too much (staring intently) at specific audience member. Gaze pattern is mildly disruptive to performance.
Good: Participant shifts focus during pauses, but occasionally avoids eye contact or stares at audience members.
Very Good: Participant keeps eye contact during the speech, does not stare; shifts focus during pauses.
2. VOCAL QUALITY
Very Poor: (a) Participant speaks in a flat, monotonous voice; or (b) speaks at a low volume or mumbles; or (c) speaks overly loudly, or has intrusive tone (harsh or unpleasant voice quality).
Poor: (a) Participant demonstrates minimal vocal inflections/nuances, enthusiasm, or interest in verbal expression; or (b) volume somewhat low and speech somewhat unclear; or (c) speaks a little bit too loudly, or tone is somewhat intrusive, unpleasant, or sarcastic.
Fair: (a) Participant shows some inflections/nuances in verbal expression but at most times sounds unenthusiastic or uninterested; and (b) speaks in appropriate volume; has clear voice quality; and (c) does not have an intrusive or sarcastic tone.
Good: (a) Participant shows moderate inflections/nuances and but inconsistent enthusiasm or interest. Could also be too òver the top’ (seems fake or forced); and (b) speaks in appropriate volume; has clear voice quality and (c) does not have an intrusive, unpleasant, or sarcastic tone.
Very Good: Participant is emphatic and enthusiastic in verbal expression; and (b) speaks in appropriate volume; has clear voice quality and (c) does not have an intrusive, unpleasant, or sarcastic tone.
3. DISCOMFORT
Very High: Complete rigidity of arms, legs or whole body. Constant leg movements or fidgeting with hands, hair or clothing. Extremely stiff face or constant facial tics. Frequent nervous throat clearing, swallowing, or stuttering. Frequent inappropriate giggling or laughing. Look of extreme discomfort and desire to flee situation.
High: Rigidity or fidgeting for majority of time. Difficulty staying still is somewhat disruptive to conversation. Stiff face or frequent facial tics. Some nervous throat clearing or swallowing. Some inappropriate giggling or laughing. Participant shows signs of discomfort by frequently looking around.
Moderate: No rigidity. Slight movement of legs, fidgeting, throat clearing, or swallowing. Participant shows only brief periods of discomfort.
Low: No rigidity, nervous throat clearing, or swallowing. Minimal fidgeting that is not disruptive to performance. No notable signs of discomfort. At times may appear relaxed and at ease (smiling or gesturing).
Very Low: Relaxed body posture and natural body movement. Participant laughs and smiles at appropriate times. S/he shows effective gesturing (to be distinguished from fidgeting). Participant does not appear at all uncomfortable and is at ease in situation.
4. SPEECH FLOW
Very Poor: Participant frequently trails off, making few attempts to continue the speech. Participant does not respond appropriately to audience’s prompts, (does not acknowledge prompts and/or does not react to prompts). Even when prompted by the audience, participant cannot maintain the speech.
Poor: Participant tries to initiate and continue the speech but is only successful about half the time. The speech does not flow smoothly – participant trails off, participant does not follow up information on topics in a fluid manner or provide relevant examples. Participant sometimes repeats the same factual information during the speech (repeats himself/herself). Participant occasionally responds appropriately to audience’s prompts, (does not acknowledge prompts and/or does not react to prompts).
Fair: For the most part, the participant is able to continue the speech with little to no help/prompts from the audience, although the speech is still somewhat awkward and stalls at times, with participant occasionally trailing off. Participant provides little follow up information on topics or provide relevant examples. Participant responds appropriately to audience’s prompts.
Good: Participant is able to maintain the speech with no help/prompting from the audience. The speech flows smoothly with few awkward pauses. Participant rarely trails off. The participant readily shares information and examples. Shows interest in engaging the audience, and follows up appropriately on participant’s own remarks. No obvious deficits.
Very Good: Participant easily maintains the speech with minimal pauses and smooth transitions, often following up on previous information provided by making appropriate follow-up remarks and offering additional information on a related topic. Participant introduces new topics fluidly and speaks fluently.
Footnotes
Declarations
Conflicts of interest/Competing interests: The authors have no conflicts of interest to disclose.
Ethics approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Committee on the Use of Human Subjects of Harvard University (IRB No. 24143).
Consent to participate: Informed assent was obtained from child participants and consent was obtain from the parents.
Availability of data and material:
Our data cannot legally or ethically be released as our participants include minors, and they and their parents did not provide consent for data sharing.
References
- Albano A, & Silverman W (1996). The Anxiety Disorders Interview Schedule for Children for DSM-IV: Clinician manual (child and parent versions). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Albano AM, Marten PA, Holt CS, Heimberg RG, & Barlow DH (1995). Cognitive-behavioral group treatment for social phobia in adolescents: A preliminary study. Journal of Nervous and Mental Disease. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G, & Greenberg RL (2005). Anxiety disorders and phobias: A cognitive perspective. Basic Books. [Google Scholar]
- Beidel DC, Turner SM, & Morris TL (1999, Jun). Psychopathology of childhood social phobia. J Am Acad Child Adolesc Psychiatry, 38(6), 643–650. 10.1097/00004583-199906000-00010 [DOI] [PubMed] [Google Scholar]
- Benjamin CL, O’Neil KA, Crawley SA, Beidas RS, Coles M, & Kendall PC (2010, Jul). Patterns and predictors of subjective units of distress in anxious youth. Behav Cogn Psychother, 38(4), 497–504. 10.1017/S1352465810000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkett MA (2011, Oct 19). The Trier Social Stress Test protocol for inducing psychological stress. J Vis Exp(56). 10.3791/3238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Babson KA, Gahr JL, Trainor CD, & Frala JL (2011, Jul). Elevated social anxiety among early maturing girls. Dev Psychol, 47(4), 1133–1140. 10.1037/a0024008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Hodges L, & Porter J (2003, Jul). Social anxiety in childhood: the relationship with self and observer rated social skills. J Child Psychol Psychiatry, 44(5), 737–742. 10.1111/1469-7610.00159 [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Tschernitz N, & Gomersall H (2005). Social anxiety in children: social skills deficit, or cognitive distortion? Behaviour research and therapy, 43(1), 131–141. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological assessment, 6(4), 284. [Google Scholar]
- Clark DM, & Wells A (1995). A cognitive model of social phobia. Social phobia: Diagnosis, assessment, and treatment, 41(68), 00022–00023. [Google Scholar]
- Dickerson SS, & Kemeny ME (2004, May). Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull, 130(3), 355–391. 10.1037/0033-2909.130.3.355 [DOI] [PubMed] [Google Scholar]
- Elkind D, & Bowen R (1979). Imaginary audience behavior in children and adolescents. Developmental psychology, 15(1), 38. [Google Scholar]
- Erdfelder E, Faul F, & Buchner A (1996). GPOWER: A general power analysis program. Behavior research methods, instruments, & computers, 28(1), 1–11. [Google Scholar]
- Francis G, Last CG, & Strauss CC (1992). Avoidant disorder and social phobia in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 31(6), 1086–1089. [DOI] [PubMed] [Google Scholar]
- Fydrich T, Chambless DL, Perry KJ, Buergener F, & Beazley MB (1998, Oct). Behavioral assessment of social performance: a rating system for social phobia. Behav Res Ther, 36(10), 995–1010. 10.1016/s0005-7967(98)00069-2 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, La Greca AM, & Silverman WK (1998, Jun). Social anxiety in children with anxiety disorders: relation with social and emotional functioning. J Abnorm Child Psychol, 26(3), 175–185. 10.1023/a:1022668101048 [DOI] [PubMed] [Google Scholar]
- Guha M (2014). Diagnostic and statistical manual of mental disorders: DSM-5. Reference Reviews. [Google Scholar]
- Haemmerlie FM, & Montgomery RL (1982). Self-perception theory and unobtrusively biased interactions: A treatment for heterosocial anxiety. Journal of Counseling Psychology, 29(4), 362. [Google Scholar]
- Halldorsson B, & Creswell C (2017, Dec). Social anxiety in pre-adolescent children: What do we know about maintenance? Behav Res Ther, 99, 19–36. 10.1016/j.brat.2017.08.013 [DOI] [PubMed] [Google Scholar]
- Hallgren KA (2012). Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor Quant Methods Psychol, 8(1), 23–34. 10.20982/tqmp.08.1.p023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert-Myers H, Guttentag CL, Swank PR, Smith KE, & Landry SH (2006). The importance of language, social, and behavioral skills across early and later childhood as predictors of social competence with peers. Applied Developmental Science, 10(4), 174–187. [Google Scholar]
- Hodson KJ, McManus FV, Clark DM, & Doll H (2008). Can Clark and Wells’(1995) cognitive model of social phobia be applied to young people? Behavioural and Cognitive Psychotherapy, 36(4), 449. [Google Scholar]
- Hopko DR, McNeil DW, Zvolensky MJ, & Eifert GH (2001). The relation between anxiety and skill in performance-based anxiety disorders: A behavioral formulation of social phobia. Behavior therapy, 32(1), 185–207. [Google Scholar]
- Inderbitzen-Nolan HM, Anderson ER, & Johnson HS (2007). Subjective versus objective behavioral ratings following two analogue tasks: A comparison of socially phobic and non-anxious adolescents. Journal of Anxiety Disorders, 21(1), 76–90. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, & Herbert JD (2001, Mar). Social anxiety disorder in childhood and adolescence: current status and future directions. Clin Child Fam Psychol Rev, 4(1), 37–61. 10.1023/a:1009576610507 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Robin JA, Hedtke KA, Suveg C, Flannery-Schroeder E, & Gosch E (2005). Considering CBT with anxious youth? Think exposures. Cognitive and Behavioral Practice, 12(1), 136–148. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005, Jun). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry, 62(6), 617–627. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, & Hellhammer DH (1993). The ‘Trier Social Stress Test’--a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28(1–2), 76–81. 10.1159/000119004 [DOI] [PubMed] [Google Scholar]
- Kiyimba N, & O’Reilly M (2020). The clinical use of Subjective Units of Distress scales (SUDs) in child mental health assessments: a thematic evaluation. Journal of Mental Health, 29(4), 418–423. [DOI] [PubMed] [Google Scholar]
- Klein AM, Liber JM, van Lang ND, Reichart C, Nauta M, van Widenfelt BM, & Utens EM (2021). The Role of Social Skills in Predicting Treatment-Recovery in Children with a Social Anxiety Disorder. Research on child and adolescent psychopathology, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koestner R, Zuckerman M, & Koestner J (1989). Attributional focus of praise and children’s intrinsic motivation: The moderating role of gender. Personality and social psychology bulletin, 15(1), 61–72. [Google Scholar]
- Kortlander E, Kendall PC, & Panichelli-Mindel SM (1997). Maternal expectations and attributions about coping in anxious children. Journal of Anxiety Disorders, 11(3), 297–315. [DOI] [PubMed] [Google Scholar]
- Krämer M, Schmitz J, Heinrichs N, & Tuschen-Caffier B (2011). Self-evaluation, social and cognitive performance in children with social phobia. Journal of Experimental Psychopathology, 2(4), 586–600. [Google Scholar]
- McCabe RE (2015). Subjective units of distress scale. J Phobias: Psychol Irrational Fear, 18, 361. [Google Scholar]
- McDaniel SC, Bruhn AL, & Troughton L (2017). A brief social skills intervention to reduce challenging classroom behavior. Journal of Behavioral Education, 26(1), 53–74. [Google Scholar]
- Miers AC, Blote AW, Bokhorst CL, & Michiel Westenberg P (2009, Dec). Negative self-evaluations and the relation to performance level in socially anxious children and adolescents. Behav Res Ther, 47(12), 1043–1049. 10.1016/j.brat.2009.07.017 [DOI] [PubMed] [Google Scholar]
- Norton PJ, & Hope DA (2001). Kernels of truth or distorted perceptions: Self and observer ratings of social anxiety and performance. Behavior therapy, 32(4), 765–786. [Record #1969 is using a reference type undefined in this output style.] [Google Scholar]
- Rapee RM, & Heimberg RG (1997). A cognitive-behavioral model of anxiety in social phobia. Behaviour research and therapy, 35(8), 741–756. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, & Kessler RC (2008). Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychological medicine, 38(1), 15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz J, Kramer M, Blechert J, & Tuschen-Caffier B (2010, Oct). Post-event processing in children with social phobia. J Abnorm Child Psychol, 38(7), 911–919. 10.1007/s10802-010-9421-2 [DOI] [PubMed] [Google Scholar]
- Schmitz J, Kramer M, & Tuschen-Caffier B (2011, Nov). Negative post-event processing and decreased self-appraisals of performance following social stress in childhood social anxiety: an experimental study. Behav Res Ther, 49(11), 789–795. 10.1016/j.brat.2011.09.001 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, & Pina AA (2001, Aug). Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry, 40(8), 937–944. 10.1097/00004583-200108000-00016 [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan C, & Brechman-Toussaint M (1999, May). Social skills, social outcomes, and cognitive features of childhood social phobia. J Abnorm Psychol, 108(2), 211–221. 10.1037//0021-843x.108.2.211 [DOI] [PubMed] [Google Scholar]
- Spence SH, & Rapee RM (2016, Nov). The etiology of social anxiety disorder: An evidence-based model. Behav Res Ther, 86, 50–67. 10.1016/j.brat.2016.06.007 [DOI] [PubMed] [Google Scholar]
- Sumter S, Bokhorst C, Miers A, Van Pelt J, & Westenberg P (2010). Age and puberty differences in stress responses during a public speaking task: do adolescents grow more sensitive to social evaluation? Psychoneuroendocrinology, 35(10), 1510–1516. [DOI] [PubMed] [Google Scholar]
- Taylor SE, & Brown JD (1988, Mar). Illusion and well-being: a social psychological perspective on mental health. Psychol Bull, 103(2), 193–210. https://www.ncbi.nlm.nih.gov/pubmed/3283814 [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Cooley MR, Woody SR, & Messer SC (1994, May). A multicomponent behavioral treatment for social phobia: social effectiveness therapy. Behav Res Ther, 32(4), 381–390. 10.1016/0005-7967(94)90001-9 [DOI] [PubMed] [Google Scholar]
- Tuschen-Caffier B, Kühl S, & Bender C (2011). Cognitive-evaluative features of childhood social anxiety in a performance task. Journal of behavior therapy and experimental psychiatry, 42(2), 233–239. [DOI] [PubMed] [Google Scholar]
- Van West D, Claes S, Sulon J, & Deboutte D (2008). Hypothalamic-pituitary-adrenal reactivity in prepubertal children with social phobia. Journal of affective disorders, 111(2–3), 281–290. [DOI] [PubMed] [Google Scholar]
- Wallace ST, & Alden LE (1997). Social phobia and positive social events: The price of success. Journal of Abnormal Psychology, 106(3), 416. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Rodebaugh TL, & Norton PJ (2008). Exploring the relationship between fear of positive evaluation and social anxiety. Journal of Anxiety Disorders, 22(3), 386–400. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, Jensen-Doss A, Hawley KM, Krumholz Marchette LS, & Chu BC (2017). What five decades of research tells us about the effects of youth psychological therapy: a multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Vaughn-Coaxum RA, Ugueto AM, Eckshtain D, & Corteselli KA (2019, Mar). Are Psychotherapies for Young People Growing Stronger? Tracking Trends Over Time for Youth Anxiety, Depression, Attention-Deficit/Hyperactivity Disorder, and Conduct Problems. Perspect Psychol Sci, 14(2), 216–237. 10.1177/1745691618805436 [DOI] [PubMed] [Google Scholar]
- Westenberg PM, Drewes MJ, Goedhart AW, Siebelink BM, & Treffers PD (2004, Mar). A developmental analysis of self-reported fears in late childhood through mid-adolescence: social-evaluative fears on the rise? J Child Psychol Psychiatry, 45(3), 481–495. 10.1111/j.1469-7610.2004.00239.x [DOI] [PubMed] [Google Scholar]
- Westenberg PM, Gullone E, Bokhorst CL, Heyne DA, & King NJ (2007). Social evaluation fear in childhood and adolescence: Normative developmental course and continuity of individual differences. British Journal of Developmental Psychology, 25(3), 471–483. [Google Scholar]
- Zell E, Strickhouser JE, Sedikides C, & Alicke MD (2020, Feb). The better-than-average effect in comparative self-evaluation: A comprehensive review and meta-analysis. Psychol Bull, 146(2), 118–149. 10.1037/bul0000218 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Our data cannot legally or ethically be released as our participants include minors, and they and their parents did not provide consent for data sharing.


