Abstract
Nurses are at a high risk for short sleep duration and poor sleep quality due to irregular work schedules and high occupational stress. Considering the effect of nurses’ sleep on the safety and health of themselves and their patients, it is important to promote healthy sleep for nurses. We sought to synthesize the published experimental and quasi-experimental studies that address interventions to improve sleep in nurses. A systematic search was conducted for studies published in English up until May 15, 2023, using the databases PubMed, CINAHL, Academic Search Ultimate, and PsycINFO. In total, 38 articles were included, covering 22 experimental and 16 quasi-experimental studies with sample sizes ranging from 9 to 207. Studies were assessed using the Cochrane Risk of Bias tool and considered as low to medium quality. Thirty-six of the 38 studies reported positive findings for at least one sleep outcome. Intervention types included aroma therapy, dietary supplements, cognitive behavioral therapy, light therapy, mind-body therapy, sleep education, exercise, napping, shift schedule modification, and multicomponent intervention, all of which showed moderate effectiveness in promoting sleep outcomes of nurses. Comparing and contrasting studies on specific interventions for improving sleep in nurses is sparse and often equivocal. With the variations of research methodology and outcome measures, it is difficult to make a conclusion about each intervention’s effectiveness on specific sleep outcomes. Additional high-quality research, including randomized controlled trials, is needed to evaluate strategies for improving sleep in this unique, safety-sensitive occupational group.
Keywords: sleep promotion, sleep intervention, nurses, systematic review
Introduction
In order to provide around-the-clock patient care, many nurses are assigned to shift work. As a result, nurses are at a great risk for decreased sleep quantity and quality (Rosa et al., 2019; Sun et al., 2019). More recently, the prevalence of poor sleep among nurses increased due to high stress related to the COVID-19 pandemic (Salari et al., 2020). Night shift nurses who sleep during the day often report shortened and disturbed sleep, thereby accumulating a significant amount of sleep debt, which contributes to long-term exhaustion (Cheng & Cheng, 2017; Zhang et al., 2019).
Shift work can reduce sleep quantity and quality and may affect the overall well-being of nurses and other healthcare professionals (Books et al., 2017; Ganesan et al., 2019). Maladaptation to shift work may lead to the development of Shift Work Sleep Disorder, a circadian rhythm disorder (Pallesen et al., 2021) caused by the misalignment between internal circadian rhythms and the work/sleep schedule (Wickwire et al., 2017). Insufficient sleep adversely affects many nurses and often results in fatigue at work, decreased quality of life, and adverse physical and mental health outcomes such as musculoskeletal injuries and depression (Chaiard et al., 2019; Owens et al., 2017; Zhang et al., 2017). Fatigue, often resulting from short and poor sleep as experienced by nurses, tends to reduce the ability to concentrate and make correct judgements, leading to the possibility of errors and injuries (Scott et al., 2014) and drowsy driving and motor vehicle crashes (Imes et al., 2023; Smith et al., 2021). To avoid these negative outcomes, promoting strategies for improved sleep for nurses would likely enhance patient safety. Sleep promotion, either by individual nurse behavior or by workplace policies and activities, can benefit employees, patients, and their institutions.
Nurses are a unique occupational group, predominantly comprised of women, many of whom hold primary responsibilities for child, family, and/or elder care at home. In 2019, the Census Bureau reported that there are more than three million nurses in the U.S., and over 85% of them are women (United States Census Bureau, 2019). There have been several review articles targeting sleep promotion in the general workforce, predominantly focused on men (Albakri et al., 2021; Redeker et al., 2019; Soprovich et al., 2020), yet those recommendations may not be suitable for nurses who are primarily women with different responsibilities and shift schedules. Considering the long and irregular work hours, overnight shifts, physical and psychological work demands, and limited time available for sleep, nurses face multiple obstacles in obtaining sufficient and quality sleep (Redeker et al., 2019). More efforts to promote sleep of nurses are needed to ensure a healthy workforce and high quality of patient care (Caruso & Hitchcock, 2010; Rogers, 2008).
Sleep promotion strategies aimed at the general workforce include sleep disorders screening/evaluation and treatment, and pharmacological and non-pharmacological strategies including educational, environmental, behavioral, supportive, and multicomponent treatments (Albakri et al., 2021; Redeker et al., 2019). However, there is sparse evidence regarding current evidence to promote sleep in the nursing population. Therefore, the objective of this systematic review is to synthesize published literature that addresses the effectiveness of interventions to improve sleep in nurses.
Methods
Search Strategy and Data Extraction
A systematic literature search in PubMed, CINAHL, Academic Search Ultimate, and PsycINFO was performed on May 15, 2023. The publication time frame was not limited in order to capture all relevant literature. The search keywords included three broad categories (sleep, nurse, and intervention), each with a defined broad subset of keywords, as documented in Supplementary Table 1.
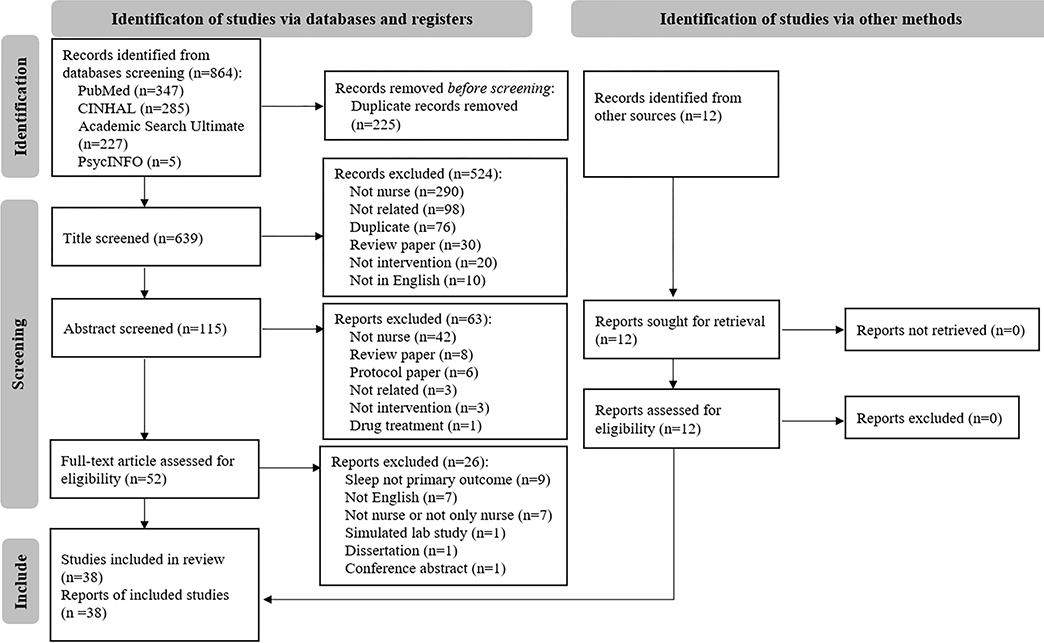
The first author (YZ) screened manuscript titles and abstracts. Full-text articles were screened independently by two authors (YZ and Y-JL), discrepancies were discussed, and consensus was reached. Figure 1 illustrates the PRISMA flow diagram (Page et al., 2021).
Figure 1. Flow diagram of the literature search.
Adapted from Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D, et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Journal of Clinical Epidemiology, 134, 178–189.
Eligibility Criteria
The inclusion criteria were: (1) types of study: experimental or quasi-experimental; (2) types of participants: nurses only; (3) types of outcomes: sleep as a primary outcome. Sleep was defined broadly, including duration, latency, deprivation, insufficiency, maintenance, quality, disturbances, disorders, problems, insomnia, and sleepiness; and (4) full text in English language. This review excluded: (1) studies that tested an intervention with healthcare/shift workers including nurses as only part of the sample; (2) studies that tested an intervention (e.g., nutrition, exercise) measuring sleep as a secondary outcome; and (3) observational studies, protocol papers, and reviews and meta-analyses. We used reviews and meta-analyses to ensure we captured all relevant studies. When a paper did not mention sleep as a primary or secondary outcome yet described sleep-related data, our study team discussed the focus of the intervention to ascertain whether the paper should be included or excluded.
Assessment of Methodological Quality
Risk of bias was graded using the Cochrane Risk of Bias tool (Higgins et al., 2011) for randomized controlled trials (RCTs). This tool covers seven items to evaluate the risk of bias, including: Random sequence generation, allocation concealment (describing the method used to conceal the allocation sequence in sufficient detail), blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias (Higgins et al., 2011). Each item was graded as “(+) low risk of bias,” “(−) high risk of bias,” or “(?) unclear risk of bias,” based on the definitions and samples provided in the tool. The overall assessment of risk of bias was graded as “(+) low risk of bias” when there were four or more items receiving low ratings; or as “(−) high risk of bias” when there were three or fewer items receiving low ratings.
Data Synthesis
Data synthesis began by summarizing study results in tables. Studies were grouped first by the study design, then by the intervention types. Intervention types were generated based on common sleep interventions identified from previous reviews (Albakri et al., 2021; Capezuti et al., 2018; Redeker et al., 2019). Each type was discussed within the study team for inclusion as a major category in this review.
The first author (YZ) began analysis by systematically reviewing each manuscript at least twice on the abstract, methods, results, and discussion, and completed Table 1, covering major study characteristics. Each manuscript was then re-analyzed independently by a co-author (HL, LB, Y-JL, or JFD) on each domain in Table 1 for information accuracy. Discrepancies were checked by a third co-author and discussed until consensus was reached. Table 2, quality appraisal, followed the same synthesis process as Table 1.
Table 1.
Characteristics of Experimental and Quasi-experimental Studies Examining Sleep Interventions in Nurses
| Source Country | Population Subjects (N) Women (%) | Mean Age (yr) | Intervention Duration (Follow-up) | Intervention | Control | Main Sleep-related Outcomes | Additional Outcomes | Conclusion on Main Sleep-related Outcomes (Comparison with control) |
|---|---|---|---|---|---|---|---|---|
| Experimental | ||||||||
| Aroma Therapy | ||||||||
| Chang, 2017 Taiwan | Nurses on monthly rotating nights shifts 50 100% |
29 | 4 wks (weekly follow up) | An aroma therapy massage with music (25 min massage +35 min rest), once a week for 4 wks | Lay down with music (60 min rest), once a week for 4 wks | PSQI total and subscale scores | Take-home sleep detector, Ezsleep | There were no differences in PSQI total score, but a significant improvement in sleep quality at post-intervention in the intervention group compared to the control group. There were significant improvements in PSQI total score, subjective sleep quality, sleep disturbance, and daytime dysfunction in the intervention group compared to baseline. |
| Hsu, 2021 Taiwan | ER and ICU nurses 103 92.7% |
31 | 4 wks (4 wk & 8-wk follow up) | 50-min lavender essential oil massage with music, once a week for 4 wks | None | PSQI-Chinese total score | Actigraphy, HRV, OBI-Chinese | There were no differences between the intervention and control group on PSQI total score at post-intervention and 8-wk follow up. For the intervention group, the self-reported PSQI score revealed an improvement at post-intervention and 8-wk follow-up compared to baseline. |
| Nasiri, 2021 Iran | Nurses on rotating shifts 80 88.8% |
29 | 2 hrs in a typical night shift | Wear a fabric (surgical) mask with a drop of rosemary essential for 5–10 mins followed by 10–15 mins removal, repeatedly for 2 hours | Wear a fabric mask with a drop of distilled water for 5–10 mins followed by 10–15 mins removal, repeatedly for 2 hours | KSS, ESS | None | Compared to the control group, intervention group had significantly decreased sleepiness and increased alertness at post-intervention. |
| Dietary Supplements | ||||||||
| Baradari, 2018 Iran | ICU nurses 53 92.5% |
31 | 1 mon | 220 mg zinc sulfate capsules every 72 hours for 1 month | Placebo every 72 hours for 1 month | PSQI total score and subscale scores | Serum zinc level | There were significantly improved PSQI total scores and subjective sleep quality scores at the post-intervention in the intervention group compared to the control group. |
| Mousavi, 2020 Iran | Nurses with significant fatigue 105 88% |
35 | 4 wks | 100 mg CoQ10 capsule twice daily | Placebo twice daily | PSQI total score | Fatigue score on Nurse’s Fatigue Scale | There was significantly improved PSQI total score in the intervention group compared to the baseline and the control group. |
| Zhang, 2020 China | Nurses on a rotating three-shift schedule 38 100% |
29 | 1 mon | 10 g Shimian granules twice daily for 1 month, plus sleep hygiene education | Placebo twice daily for 1 month, plus sleep hygiene education | ISI one day before initial treatment and 1 day after last treatment | PVT, HADS, HADS-A, and HADS-D one day before initial treatment and 1 day after last treatment, salivary melatonin and proinflammatory cytokine at bedtime every 7 days | There were significant decreases in insomnia severity at post-intervention in the intervention group compared to the control group. |
| Cognitive Behavioral Therapy | ||||||||
| Dahlgren, 2022 Sweden | Nurses with less than 12 months’ work experience 207 88% |
27 | 4 wks (6-mon follow-up) | Three 2.5hr group-based proactive recovery program sessions based on CBT and motivational interviewing techniques | Waitlist control – usual care and then receive the intervention after follow-up | ISI, KSQ | SMBQ, WIPL, Somatic Symptom Scale-8, PSS, DBAS-10 | There were no significant differences in ISI or KSQ between the two groups at post-intervention and follow-up. |
| Zhou, 2022 China | Nurses with chronic insomnia 118 98% |
30 | 6 wks | e-aid CBT-I | None | PSQI, ISI | GAD-7, PHQ-9 | There were significant improvements in sleep quality and insomnia severity in the intervention group compared to the control group and baseline. |
| Light Therapy | ||||||||
| Tanaka, 2011 Japan | Nurses working rapid day-night rotating shifts 61 100% |
30 | 1 mon | 10-min morning bright light exposure using bright light device in the workplace before 7:30am for all day-shift workdays | Crossover control – usual care then receives the intervention after one week washout period | KSS, night sleep by 0–10 VAS | CIS, RT, and number of lapses by PVT, frequency of perceived adverse events and near misses | There were significant improvements on sleepiness and night sleep for day-shift days in intervention periods compared to control periods. |
| Huang, 2013 Taiwan | Nurses with high ISI score, working three-shift rotation 92 100% |
30 | At least 10 days during 2 wks | Exposure to bright light for ≥ 30 mins during the first half of the evening/night shift and wearing dark sunglasses after shift | No exposure to bright light, but wearing dark sunglasses after shift | ISI | HADS | The ISI score was significantly improved in the intervention group compared to the control group and the baseline. |
| Rahman, 2013 Canada | 12-hr day or night shift nurses 9 56% |
31 | 8-wk randomized crossover design | Wearing glasses fitted with short-wavelength filters during night shifts | Receiving standard indoor light during night shifts | PSG, sleep diary | Saliva melatonin assays, subjective and objective alertness (self-report scale and PDA), CES-D, ESS | There were significant increases in TST and SE and decreases in WASO in the intervention group compared to the control group for nighttime sleep, but no significant differences between groups for daytime sleep. |
| Griepentrog, 2018 U.S. | Night shift ICU nurses 43 71% |
29 | One night shift, cross-over | 10-hr exposure to high illuminance white light | 10-hr exposure to standard ambient fluorescent lighting | SSS | Number of lapses and errors on PVT, PVT median response time, salivary melatonin concentration | There was a significant reduction of SSS score at the end of the night shift in the intervention group compared to the control group. |
| Bjorvatn, 2021 Norway | Nurses working at least three consecutive night shifts 35 80% |
35 | Three consecutive night shifts, counter-balanced randomized cross-over | Sit in front of a bright light box for 30 mins at each night shift, the timing of light exposure was delayed by one hour at each following night shift | Sit in front of a red dim light box for 30 mins at each night shift, the timing of light exposure was delayed by one hour at each following night shift | ATS, KSS | PVT, mood and energy, caffeine intake | Heavy eyelids significantly reduced during the night shifts in the experimental condition compared to the placebo condition. No differences in sleepiness between the two conditions during or after the night shifts. |
| Cyr, 2023 Canada | Nurses during COVID working rapid rotating schedules with consecutive night shifts 57 84% |
31 | 20 days | Evening light exposure, with suggestions on staying up 1 hr later on the night before first night shift, sleep using a provided 3D eye mask, wear dark sunglasses in the morning, optionally nap in the late afternoon, and expose to 40-min bright light at home before night shifts. | Chrononutrition control, with suggestions on the timing and content of meals and snacks | KSS, Sleep Quality Scale, sleep and wake time | Fatigue, work-related errors, mood | There were significant improvements in sleepiness and fatigue, but only minor changes in sleep duration, in the intervention group compared to the baseline. There were no differences between the intervention and control group in any sleep outcomes. |
| Mind Body Therapy | ||||||||
| Fang, 2015 China | Nurses 105 100% |
35 | 6 mons | Coached group yoga sessions, 50–60 min per session, more than 2 sessions per week | None | PSQI total score and subscale scores | QMWS | There were significantly improved PSQI total score, subjective sleep quality, sleep duration and sleep efficiency score, and less sleep disturbances, less use of sleep medication and less daytime dysfunction in the intervention group compared to the control group. |
| Nourian, 2021 Iran | COVID first-line nurses 41 87.7% |
36 | 7 wks | Online MSBR program delivered through Whats App Messenger including meditation audio, yoga video readings about the nature of mindfulness and audio or video of speeches related to mind exercises | None | PSQI total score and subscale scores | None | There were significantly improved subjective sleep quality and sleep latency scores in the intervention group compared to the control group and the baseline. There was also significantly improved sleep efficiency in the intervention group compared to the baseline. |
| Çelik, 2023 Turkey | Nurses during COVID pandemic 90 87% |
29 | 4 wks | 40-min laugher yoga evening sessions twice each week including deep breathing exercises, warm-up exercises, childish games, and laugher exercises. | Usual care (offered the intervention after post-test) | PSQI | CD-RISC | There was significantly improved PSQI total score in the intervention group compared to the control group and the baseline. |
| Sleep Education | ||||||||
| Yazdi, 2017 Iran | Shift work nurses with clinical insomnia 100 100% |
30 | 1 mon | 2-hr training and a brochure about sleep hygiene practices | A brochure about sleep hygiene practices | ISI, ESS, PSQI total score and subscale scores | None | There was significantly improved ISI, ESS, and PSQI, bedtime at night, sleep latency, frequency of unwanted napping during the day, and subjective sleep quality, sleep duration, sleep efficiency, and sleep disturbances at one-month post-intervention in the intervention group compared to the control group. |
| Exercise | ||||||||
| Niu, 2021 Taiwan | Shift work nurses with baseline PSQI>5 60 100% |
26 | 8 wks (4-wk, 8-wk, and 12-wk data collection) | Moderate-intensity aerobic exercise program including indoor treadmill walking and jogging under a rehab instructor’s supervision for 8 wks with 60 min per session and 5 times per week | Usual activity without regular exercise | Actigraphy TST, SL, WASO, SE | None | The intervention group showed improved TST and SE at 4-wk and 8-wk compared to baseline. The improvement in TST continued until 12-wk. There were significantly improved SL and WASO at 4-wk in the intervention group compared to the control group. |
| Multicomponent Intervention | ||||||||
| Yoon, 2002 Korea | Rotating night-shift nurses with backward rotation 12 100% |
Range 23–27 | 2 days of 4-day night shifts |
Mel Group: 6 mg melatonin before daytime sleep with morning sunlight permitted Mel-S Group: 6 mg melatonin before daytime sleep with sunglasses worn to attenuate morning sunlight |
Placebo before daytime sleep with morning sunlight permitted | TST, SL, SE, SPT by sleep log | VAS for nocturnal alertness, DS-CPT, POMS | There were significant increases in sleep period and total sleep time by melatonin treatment (Mel and Mel-S) compared to placebo, but no differences in sleep period and total sleep time between Mel and Mel-S, and no differences in SL and SE among the three groups. |
| Booker, 2022 Australia | Nurses on regular rotating or permanent night shifts 149 96% |
35 | Education duration is not specified, 4 one-on-one coaching sessions over 8 weeks | Sleep and shift work education, plus coaching sessions with individualized strategies on home-based activities such as napping and scheduled sleep, light exposure during work, caffeine consumption, sleep hygiene practice and melatonin (clustered randomization) | Low glycemic index diet education, plus home-based activities such as food diary and taking low glycemic index foods | SWD, SHI, ISI, FOSQ-10 | Ward-based sick leave, ASTNQ, MEQ, PHQ-9, GAD-7 | There were no significant differences in sleep outcomes between the intervention and control group. There were significantly improved ISI and FOSQ-10 scores in the intervention group compared to baseline, but no differences in SWD and SHI. |
| Hausswirth, 2022 France | Nursing staff during COVID pandemic 45 78% |
44 | 4 wks | Rebalance© Impulse, a light stimulation and mindfulness training device, 30 min per session, 2–3 sessions per week for a total of 10 sessions | None | Actigraphy, sleep diary, perceived sleep quality, SSQ, FIRST | BP, HR, HRV, blood cortisol and alpha-amylase concentration | SSQ, perceived sleep quality, sleep efficiency, and fragmentation index significantly improved in the intervention group compared to the control group. |
| Source Country | Population Subjects (N) Women (%) | Mean Age (yr) | Intervention Duration (Follow-up) | Intervention | Control | Outcomes related to Sleep | Additional Outcomes | Main Conclusion (Comparison with control) |
| Quasi-experimental | ||||||||
| Aroma Therapy | ||||||||
| Seo, 2017 Korea | Nurses on three-shift working 60 No report of women% |
>30 (72%) ≤30 (28%) |
2 wks | Dropping aroma oil to pillows every day before going to bed | No description | Self-report sleep quality | Self-report fatigue | There were significant differences in overall sleep quality at post-intervention in the intervention group compared to the control group. These differences were also observed on insufficient sleep, difficulty in falling asleep, difficulty in lying awake, sleep satisfaction, and difficulty in maintaining sleep. |
| Dietary Supplement | ||||||||
| Franco, 2012 Spain | Nursing staff having at least one night shift per week 17 100% |
41 | 2 wks | Ingest 330 mL alcohol-free beer (containing the hop, humulus lupulus L.) daily with supper | Control week not receiving the alcohol-free beer with supper (within subjects) | Actigraphy TIB, TST, SL, SE, total activity pulses during sleep | Work stress, STAI | There were significant decreases in Actigraphy sleep latency and total activity pulses during sleep after the intervention, but no significant differences in total sleep time and sleep efficiency. |
| Cognitive Behavioral Therapy | ||||||||
| Carter, 2013 U.S. | Hospice nurses 9 89% |
54 | Twice, at wk 2 and wk 4 (wk 3 and wk 5 data collection) | Two 1-hr group education intervention sessions about CBT-I | No control | PSQI | CES-D | There were no significant changes at post-intervention. |
| Lee, 2014 U.S. | Night shift nurses 21 95% |
46 | 4 wks (8-wk follow-up) | 4-wk active control intervention including a sleep diary and weekly readings from a booklet about shift work and sleep; and 4-wk SETS-SW intervention including a sleep diary and a home-based cognitive behavioral therapy | No control | PSQI, GSDS, 7 days of wrist actigraphy | CES-D, SSI | There are significant improvements on subjective PSQI and GSDS scores after the SETS-SW intervention. Subscale scores of sleep quality, onset latency, and daytime sleepiness were significantly improved after the intervention, but no significant change in objective sleep parameters assessed by actigraphy. |
| Omeogu, 2020 U.S. | Day shift nurses 13 100% |
52 | 6 wks (both 3-wk and 6-wk data collection) | CBT-I Coach app on cellphone | No control | ISI | None | There was significant decrease on ISI score at 3 week and the trend sustained at 6 week, with 24% attrition rate. |
| Light Therapy | ||||||||
| Boivin, 2012 Canada | 8-hr night shift nurses 17 59% |
42 | An average of 12 night shifts over an average of 19 days | Intermittent exposure to full-spectrum bright light during the first 6h of each night shift and wearing shaded goggles during the 2 h following the end of the night shift including the commute home plus remaining in bed for 8h | Usual habitual light environment at work and wearing clear UV-excluding goggles for the morning commute home | TST, SO, SE by Nightcap device or portable PSG | Core body temperature, melatonin markers, saliva melatonin levels | There was significant more TST (~30 mins) for daytime sleep after night shifts in the intervention group compared to the control group, but no significant differences in SO and SE. |
| Jensen, 2016 Denmark | Evening/night shift ICU nursing staff 113 No report of women% |
42/43 | 10 days with at least two evening/night shifts in a row and 2 dayshifts/days off in a row | Designated dynamic light at work | Ordinary institutional light at work | Actigraphy SE & WASO, subjective sleep quality from sleep diary | Saliva melatonin levels, subjective well-being and health | There were no significant differences in Actigraphy SE and WASO, but better self-reported sleep quality after night shifts at post-intervention between the intervention and control groups. Actigraphy showed the control group had 16% more awakenings than the intervention group. |
| Aarts, 2020 Netherlands | Rapid rotating night shift nurses 23 87% |
30 | Three consecutive night shifts (a total of 7-days data collection) | Wearing a light therapy glass with integrated LEDs for 4*15 min during 3 night shifts, for 30 min within 2 h after awakening, and wearing the orange-tinted blue-blocking goggles during the morning commute home | Wearing a placebo glass during 3 night shifts and for 30 min within 2 h after awakening, and wearing the orange-tinted blue-blocking goggles during the morning commute home | KSS, DSS, Actigraphy BT, GUT, TIB, TST, SL, SE, FI, and subjective GSQS | Person-bound light exposure, perceived effectiveness | There was no significant difference in sleepiness, but significantly lower sleepiness on commute home after the first night shift, significantly better sleep on the second recovery day, and significantly better subjective sleep quality after the first night shift in the intervention group compared to the control group. |
| Hoshi, 2022 Japan | Rotating and regular night shift nurses 17 100% |
35 | 2 wks | Dark room lightening with 110 lx on the desk at the nurse station (within subjects) | Well-lit condition with 410 lx on the desk and ceiling lights | Qguri-Shirakawa-Azumi Sleep Inventory; sleepiness | Fatigue, malpractice/incidents/accidents | There was no significant difference of sleep quality, but increased drowsiness or lethargy on certain shifts in dark conditions compared to well-lit conditions. |
| Mind Body Therapy | ||||||||
| Liu, 2021 China | COVID first-line nurses 140 93.6% |
32 | 4 wks | Nurses were provided the DBRT information guide, MP3 audio recording, demonstration video, and self-training record and required to complete the DBRT at 8pm daily. | No control | PSQI-Chinese total score and subscale scores | SAS-Chinese, SDS-Chinese | There were significantly improved PSQI total score, subjective sleep quality, sleep duration and sleep efficiency score, less sleep disturbances, less daytime dysfunction compared to the baseline. |
| Parajuli, 2021 India | Nursing staff 33 100% |
41 | 4 wks | Group yoga for 45 min/day, 5 days/week | No control | PSQI total score | PSS | There was significantly improved PSQI score compared to the baseline. |
| Sleep Education | ||||||||
| Morimoto, 2016 Japan | Nurses 25 88% |
40 | 2 wks | SHT: Two 90-min sleep education workshops on sleep hygiene education and relaxation techniques | Two 90-min sleep education workshops only | PSQI-Japanese total score and subscale scores, ESS-Japanese, | PHQ-Japanese, MBI-Japanese, SF-8 Health Survey-Japanese | There were significantly improved PSQI total score and daytime dysfunction score at post-intervention in the intervention group compared to the control group. Participants with sleep problems in the intervention group showed significant improvements in sleep latency, sleep disturbance, and sleepiness scores than those in the control group. |
| Nap | ||||||||
| Zion, 2019 Israel | Nurses working irregular rotating shifts including night shifts 110 100% |
39 | 4 nights | Two nights with a scheduled 30-min nap at 4am | Two nights without a scheduled nap (within subjects) |
KSS | DSST, LCT, MCTQShift | Lower sleepiness was observed at 5am, 6am and 7am on nights with a nap compared to nights without a nap. |
| Shift Schedule Intervention | ||||||||
| Kubo, 2022 Japan | Nurses in a cardiac surgery unit working three-shift schedule with backward rotation 30 No report of women% |
28 | 2 mons | Shift-work schedule change to add one day off after every two consecutive night shifts | Non-randomized crossover control – usual care then receives the intervention afterwards | TST, SL, SE, WASO by sleep mattress sensors, total sleep hours, mean sleep duration, number of sleep opportunities by sleep log, sleep quality, and sleepiness | PVT, CRP, MQ, REQ, KPDS, UWES, fatigue, stress, quality of care, satisfaction with days off, work satisfaction | There were significant improvements in total sleep hours and number of sleep opportunities by sleep log, self-reported sleep quality and sleepiness in the intervention group compared to the control group, but no significant differences in mean sleep duration by sleep log and objective sleep parameters from mattress sensors. |
| Multicomponent Intervention | ||||||||
| Scott, 2010 U.S. | Nurses 62 97% |
38 | 1-hr education with continuous institutional changes (4-wk and 12-wk follow-up) | 1-hr fatigue countermeasure education together with institutional changes including increasing unit staffing, providing completely relieved breaks and meal periods, and use of strategic naps during breaks with a sleep recliner and 20-min timer | No control | PSQI, ESS, total sleep duration, workday sleep duration, nonwork day sleep duration, night shift sleep duration | Drowsiness and sleep episodes at work, drowsy driving and motor vehicle crashes, errors and near errors, | There were significant increases in total sleep duration, workday sleep duration, nonwork day sleep duration, night shift sleep duration at 4-wk and 12-wk follow-up. There was a significant improvement in PSQI total score at 12-wk follow-up, but no significant changes in ESS score. |
| Zhang, 2023 China | Frontline nurses during COVID 52 96% |
31 | 4 wks | Holistic sleep improvement strategies including scientific human resource management, comfortable sleep environment establishment, self-relaxation, and self-adjustment training and humanistic care | No control | PSQI-Chinese total score and subscale scores | None | There were significantly improved PSQI total score and subjective sleep quality, sleep efficiency, and sleep disturbance scores compared to the baseline. |
Notes. PSQI = Pittsburg Sleep Quality Index, ER = Emergency, ICU = Intensive Care Unit, HRV = Heart Rate Variability, OBI = Occupational Burnout Inventory, KSS = Karolinska Sleepiness Scale, ESS = Epworth Sleepiness Scale, VSH = Verran Snyder Halpern Scale, PVT = Psychomotor Vigilance Task, ISI = Insomnia Severity Index, HADS = Hospital Anxiety and Depression Scale, HADS-A = Hospital Anxiety and Depression Scale-Anxiety, HADS-D = Hospital Anxiety and Depression Scale-Depression, KSQ = Karolinska Sleep Questionnaire, SMBQ = Shirom-Melamed Burn-out Questionnaire, WIPL = Work Interference with Personal Life Index, PSS = Perceived Stress Scale, DBAS = Dysfunctional Beliefs and Attitudes about Sleep, VAS = Visual Analog Scale, CIS = the Checklist Individual Strength questionnaire, RT = response time, PSG = Polysomnography, PDA = Personal Digital Assistant, CES-D = Center for Epidemiologic Studies Depression, TST = Total Sleep Time, SE = Sleep Efficiency, WASO = Wake After Sleep Onset, SSS = Stanford Sleepiness Scale, ATS = Accumulated Time with Sleepiness Scale, DSS = Driver Sleepiness Scale, BT = Bed Time, GUT = Get-up Time, TIB = Time in Bed, TST = Total Sleep Time, SL = Sleep Latency, FI = Fragmentation Index, GSQS = Groningen Sleep Quality Scale, MSBR = Mindfulness-Based Stress Reduction, BP = Blood Pressure; HR = Heart Rate; SSQ = Spiegel Sleep Quality Questionnaire, FIRST = Ford Insomnia Response to Stress Test; CD-RISC = Connor-Davidson Resilience Scale, SPT = sleep period time, DS-CPT = Degraded-Stimulus Continuous Performance Test, POMS = Profile of Mood States, SWD = Shift Work Disorder, SHI = Sleep Hygiene Index, MEQ = Morningness-Eveningness Questionnaire, FOSQ = Functional Outcomes of Sleep Questionnaire, GAD = General Anxiety Disorder, QMWS = Questionnaire on Medical Worker’s Stress, CBT-I = Cognitive Behavioral Therapy for Insomnia, STAI = State Trait Anxiety Inventory, GSDS = General Sleep Disturbance Scale, SSI = Standard Shiftwork Index, SETS-SW = Sleep Enhancement Training System for Shift Workers, SO = Sleep Onset, DBRT = Diaphragmatic Breathing Relaxation Training, SAS = Self-Rating Anxiety Scale, SDS = Self-Rating Depression Scale, SHT = Self-help therapy, PHQ = Patient Health Questionnaire, MBI = Maslach Burnout Inventory, SF = Short Form, LDL = Low-density Lipoprotein, HDL = High-density Lipoprotein, DSST = Digit Symbol Substitution Task, LCT = Letter Cancellation Task, MTCQShift = Munich ChronoType Questionnaire for Shiftwork, CRP = Salivary C-reactive Protein, MQ = Maastricht Questionnaire, REQ = Recovery Experience Questionnaire, KPDS = Kessler Psychological Distress Scale, UWES = Utrecht Work Engagement Scale, wk = week.
Table 2.
Risk of Bias in Randomized Controlled Trials
| Source | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective outcome reporting | Other bias | Overall Risk of bias |
|---|---|---|---|---|---|---|---|---|
| Chang, 2017 | + | + | − | − | + | + | ? | + |
| Hsu, 2021 | + | + | + | − | + | + | ? | + |
| Nasiri, 2021 | − | ? | − | − | + | + | ? | − |
| Baradari, 2018 | + | ? | + | − | + | + | ? | + |
| Mousavi, 2020 | + | ? | + | + | + | + | ? | + |
| Zhang, 2020 | + | ? | + | − | + | + | ? | + |
| Dahlgren, 2022 | − | − | − | − | + | + | − | − |
| Zhou, 2022 | + | ? | − | − | + | + | − | − |
| Tanaka, 2011 | + | − | − | − | + | + | − | − |
| Huang, 2013 | + | ? | − | − | + | + | − | − |
| Rahman, 2013 | − | − | − | − | + | + | − | − |
| Griepentrog, 2018 | − | − | − | − | + | + | − | − |
| Bjorvatn, 2021 | − | − | + | − | + | + | ? | − |
| Cyr, 2023 | − | ? | + | − | + | + | + | + |
| Fang, 2015 | + | ? | − | − | + | + | − | − |
| Nourian, 2021 | − | − | − | − | + | + | − | − |
| Çelik, 2023 | + | ? | − | − | + | + | − | − |
| Yazdi, 2017 | − | − | − | − | + | + | − | − |
| Niu, 2021 | + | + | + | − | + | + | ? | + |
| Yoon, 2002 | − | ? | + | − | + | + | − | − |
| Booker, 2022 | − | ? | + | − | + | + | − | − |
| Hausswirth, 2022 | − | − | − | − | + | + | − | − |
+ = low risk of bias; − = high risk of bias; ? = unclear risk of bias
Results
General Characteristics of Included Studies
In total, 38 articles met the inclusion criteria and were included; 22 (58%) were experimental and 16 were quasi-experimental studies. The earliest published study was in 2002. The sample sizes ranged from 9 to 207. These studies took place in various countries, including the United States, Canada, Iran, Denmark, Israel, Norway, Turkey, Spain, Netherlands, Sweden, France, Australia, China, India, Japan, Korea, Taiwan. Table 1 describes the study characteristics.
Study Sample Characteristics
In total, the 38 articles involved 2,395 participants, with a majority being female (on average 91%, range 56–100%) and a mean age ranging from 26 to 54 years. Participants included nurses working night shifts, evening/night shifts, rotating shifts, and day shifts, yet 15 studies did not specify the work shifts. Although most studies included healthy participants, seven studies included nurses with baseline sleep/fatigue/health complaints (Hausswirth et al., 2022; Huang et al., 2013; Morimoto et al., 2016; Mousavi et al., 2020; Niu et al., 2021; Yazdi et al., 2017; Zhou et al., 2022).
Quality Appraisal
Table 2 summarizes the biases and qualities of the RCTs. Overall, seven out of 22 RCTs were graded as low risk of bias (good quality) (Baradari et al., 2018; Chang et al., 2017; Cyr et al., 2023; Hsu et al., 2021; Mousavi et al., 2020; Niu et al., 2021; Zhang et al., 2020), and the rest were graded as high risk of bias. Dropout rates of the RCTs were moderate, with 10 RCTs reporting dropout rates of <10%, and twelve RCTs reporting dropout rates from 12.5% to 77% (Aarts et al., 2020; Bjorvatn et al., 2021; Booker et al., 2022; Carter et al., 2013; Dahlgren et al., 2022; Fang & Li, 2015; Hoshi et al., 2022; Lee et al., 2014; Morimoto et al., 2016; Omeogu et al., 2020; Scott et al., 2010b; Zhang et al., 2020). All others were quasi-experimental studies and considered high risk of bias.
Intervention Components
Intervention types included aroma therapy, dietary supplements, cognitive behavioral therapy, light therapy, mind-body therapy, sleep education, exercise, napping, shift schedule modification, and multicomponent intervention. Intervention durations varied, with some being carried out for 1 or 3 or 4 nights and others for as long as 6 months. Outcome evaluations took place immediately following the intervention, while eight studies also reported follow-ups at intervals ranging from 2 weeks to 6 months (see Table 1).
Outcome Measures
All of the studies except three (Booker et al., 2022; Cyr et al., 2023; Mousavi et al., 2020) used sleep as a primary outcome. Although these three studies did not measure sleep as a primary outcome, because the intervention in each of these studies addressed fatigue/sleep, the study team deemed them relevant and included them in this review. Main sleep-related outcomes were assessed with subjective measures such as Pittsburgh Sleep Quality Index (PSQI) and other scales (see Table 1); and/or objective measures generated from actigraphy, Nightcap, or polysomnography (PSG). About 40% of the studies (15/38) used the PSQI total score and/or subscale scores (See Table 1). Ten studies used an objective measure of sleep-related outcomes (Aarts et al., 2020; Boivin et al., 2012; Chang et al., 2017; Franco et al., 2012; Hausswirth et al., 2022; Hsu et al., 2021; Jensen et al., 2016; Niu et al., 2021; Rahman et al., 2013). Secondary outcomes of these interventions consisted of various objective measures and health outcomes (see Table 1).
Effectiveness of Interventions (Table 1)
Aroma Therapy
Three RCTs and one quasi-experimental study reported positive changes in certain sleep outcomes from aroma therapy. These studies tested different essential oils such as lavender or rosemary or mixed oils; different administering methods such as inhaling through a mask, uniform or pillow, or massaging; and different durations of one-time administration ranging from 5–10 mins to 2 hours or to the entire sleep episode.
One RCT reported that compared to distilled water, nurses who inhaled rosemary essential oil reported significantly decreased sleepiness and increased alertness on the night shift (Nasiri & Boroomand, 2021). A quasi-experimental study reported improved self-reported sleep quality and reduced fatigue among nurses working three shift rotations after aromatic inhalation through pillows during sleep (Seo & Park, 2017).
Two studies (Chang et al., 2017; Hsu et al., 2021) applying aroma therapy massage reported significant improvements in PSQI scores post-intervention compared to baseline, but no significant post-intervention differences between the intervention and control groups. Thus, it is uncertain whether it was the massage or aroma therapy that produced improved sleep quality.
Dietary Supplements
Three RCTs and one quasi-experimental study have shown positive effects on certain sleep outcomes from Zinc sulfate, CoQ10, Shimian granules, and non-alcoholic beer containing humulus lumpulus L.
In a double-blind RCT of intensive care unit (ICU) nurses, Zinc supplements were associated with improvements in total PSQI score and subjective sleep quality compared to placebo (Baradari et al., 2018). Similarly, Zhang and colleagues reported a significant decrease in insomnia severity index (ISI) scores in nurses on a rotating three-shift schedule after taking 10 g Shimian granules twice daily for one month compared to placebo (Zhang et al., 2020). Moursavi and colleagues reported a significant increase in PSQI total score in nurses after taking 100 mg CoQ10 twice daily for 4 weeks compared to placebo (Mousavi et al., 2020). A quasi-experimental study suggested significant improvement in sleep latency (the time it takes to fall asleep after getting into bed) and total activity pulses as assessed using actigraphy after nursing staff ingesting 330 mL alcohol-free beer daily for two weeks (Franco et al., 2012).
Cognitive Behavioral Therapy (CBT)
CBT for Insomnia (CBT-I) involves guiding participants through a series of changes in sleep-related behaviors to eliminate poor sleep habits, address conditioned arousal, and reduce sleep-related worries. One of two RCT studies reported significant improvement in subjective sleep quality and insomnia severity as assessed by the PSQI and ISI among nurses with chronic insomnia after receiving a 6-week e-aid CBT-I program compared to usual care (Zhou et al., 2022). Two of three quasi-experimental studies showed improvement in nurses’ subjective sleep quality and insomnia severity assessed by the PSQI and ISI when using cognitive behavioral components delivered either in-person or via mobile app (Lee et al., 2014; Omeogu et al., 2020).
However, Dahlgren et al. did not find significant differences in subjectively assessed insomnia severity or sleep quality after nurses received three 2.5-hour CBT-based proactive recovery program sessions (Dahlgren et al., 2022). Carter et al. did not find significant changes in subjective sleep quality assessed by the PSQI after group CBT-I education in nine hospice nurses (Carter et al., 2013). The small sample size (n = 9) in this latter study should be considered when interpreting the findings.
Light Therapy
Bright-light exposure is an intervention used to promote alertness during night work and improve daytime sleep by shifting the timing of the circadian system (Sun et al., 2019). Six RCTs and four quasi-experimental studies reported that light therapy has promise in improving nurses’ sleep, although there was inconsistency between the studies in certain sleep outcomes. These studies included different ways of delivering the light exposure, such as enhancing the workplace light environment, having participants wear light goggles, or having them sit in front of a light box; and the light exposures were sometimes coupled with having participants wear light-blocking goggles during commute home.
Huang and colleagues reported improved ISI scores of nurses after exposure to bright light for ≥ 30 mins during the first half of the evening/night shift combined with wearing dark sunglasses after shift (Huang et al., 2013). Similarly, Boivin et al. reported significantly more total sleep time but no differences in sleep onset latency (SOL) or sleep efficiency assessed through Nightcap device/portable PSG between the intervention and control groups (Boivin et al., 2012). Jensen et al. reported better self-rated sleep quality but no difference in actigraphy-assessed sleep efficiency or wake after sleep onset (WASO) between the intervention and control groups (Jensen et al., 2016). There were similar improved sleep outcomes from another two studies (Griepentrog et al., 2018; Hoshi et al., 2022).
Besides interventions with work environmental light exposure, one study reported that nurses who wore glasses fitted with short-wavelength filters during night shifts had significant increases in PSG-assessed total sleep time and sleep efficiency and decreases in WASO (Rahman et al., 2013). Similarly, another study reported nurses who wore light therapy glasses for 4*15 mins during night shifts and then 30 mins within 2 hours after awakening had improvements in Karolinska Sleepiness Scale (KSS) scores (sleepiness) on their commute home after the first night shift (Aarts et al., 2020).
Mind-Body Therapy
Mind-body therapy is a group of techniques that promote interaction of mind and body function to induce relaxation. Three RCTs and two quasi-experimental studies showed mind-body therapy improved the sleep of nurses. These studies tested different mind-body therapies including yoga, mindfulness-based stress reduction (MBSR), diaphragmatic breathing relaxation training (DBRT); different delivery formats such as in-person or online; and different durations of intervention ranging from 4 weeks to 6 months.
Two RCT and one quasi-experimental study reported that nurses had improved subjective sleep quality, as indicated by PSQI scores, following a 6-month (Fang & Li, 2015) or 4-week yoga program (Çelik & Yarali, 2023; Parajuli et al., 2021). Nourian et al. reported significantly improved subjective sleep quality and sleep latency scores after MSBR intervention compared to usual care (Nourian et al., 2021). Liu et al. reported that DBRT significantly improved nurses’ PSQI scores (Liu et al., 2021).
Sleep Education
One RCT and one quasi-experimental study showed that a sleep education program improved the sleep of nurses. These studies generally incorporated sleep hygiene education/training, with different lengths of the programs ranging from 2 hours to one day.
A sleep hygiene training showed positive effects on sleep quality, insomnia severity, and daytime sleepiness assessed by the PSQI, ISI, and Epworth Sleepiness Scale (ESS) in nurses with clinical insomnia (Yazdi et al., 2017). Another study reported a significant improvement in the PSQI total score and daytime dysfunction between the intervention and control groups (Morimoto et al., 2016).
Exercise
One RCT reported better sleep of nurses after an 8-week aerobic exercise program. Niu and colleagues reported improved SOL and WASO, as assessed using actigraphy, after implementing an 8-week moderate-intensity aerobic exercise program compared to those without regular exercise (Niu et al., 2021).
Napping
One quasi-experimental study showed reduced sleepiness in nurses after a nap. Zion et al. found significantly lower KSS sleepiness scores during 8-hour night shifts at 5am, 6am, and 7am on nights with a scheduled 30-min nap at 4am compared to those without a scheduled nap (Zion & Shochat, 2019).
Shift Schedule Modification
One quasi-experimental study reported improvements in sleep after a shift schedule modification. Kubo and colleagues found that nurses have significant improvements in self-reported total sleep time, sleep quality, and sleepiness when adding one day off after every two consecutive night shifts (Kubo et al., 2022).
Multicomponent Intervention
Three RCTs and two quasi-experimental studies reported improved sleep outcomes in nurses after a multicomponent intervention, for example, melatonin intake and light exposure, education and institutional/environmental changes, or mindfulness training and light stimulation.
Hausswirth et al. found that a 4-week light stimulation and mindfulness training program significantly improved sleep quality, sleep efficiency, and fragmentation index as assessed by actigraphy in the intervention compared to control group (Hausswirth et al., 2022). Booker et al. found no significant differences in sleep outcomes between intervention and control groups, but significant improvements in insomnia severity and functional outcomes of sleep quality as assessed by ISI and FOSQ-10 compared to the baseline among nurses receiving a shift work and sleep education plus coaching sessions with individualized strategies on behavior changes (Booker et al., 2022).
One quasi-experimental study reported that a 1-hour fatigue education intervention coupled with institutional changes such as increasing staffing, providing completely relieved breaks and meal periods, and use of strategic naps during breaks significantly improved nurses’ sleep quality as assessed by PSQI and sleep duration at 4-week and/or 12-wk follow-up (Scott et al., 2010b). Similarly, another study reported significantly improved sleep quality as assessed by PSQI in nurses after implementing holistic sleep improvement strategies including institutional and environmental changes and self-relaxation training (Zhang et al., 2023).
Discussion
To our knowledge, this is the first systematic review to summarize experimental and quasi-experimental studies involving interventions designed to improve the sleep of nurses. Overall, this systematic review contributes important information related to effective sleep promotion programs for nursing, a high-risk occupation for sleep problems.
Although 36 out of the 38 studies reported one or more positive findings regarding the sleep of nurses (e.g., sleep quality, insomnia severity), due to multiple limitations and variations in the research methodology and outcome measures, it is difficult to make a conclusion about each intervention’s effectiveness on specific sleep outcomes. Two studies that found no significant effect of the interventions both used cognitive behavioral therapy. These interventions were conducted with nurses working in different shift types, durations, and rotating patterns; they varied in design and intervention type, duration, frequency and outcome measures; and the interventions were delivered in different formats. Querstret and colleagues conducted a scoping review of sleep-related/fatigue-management interventions for nurses and midwives and similarly reported that the literature is fragmented and lacks cohesion (Querstret et al., 2020). In general, we found that each intervention type showed some promise in improving nurses’ sleep. Among these, light therapy was most widely tested and all showed positive findings in decreasing sleepiness and/or improving sleep quality in nurses. Taking into account the design rigor and quality, dietary supplement was rated more as low risk of bias due to the ease of designing a single- or double-blind placebo-controlled trial. Among the 38 studies, light therapy, napping, and shift schedule modification are interventions designed specifically for shift workers, while other interventions have been used previously to improve sleep in the general population. Six were conducted with COVID-19 frontline nurses, demonstrating light therapy, mind-body therapy, and multicomponent interventions were effective in improving the sleep of nurses during the pandemic.
Effectiveness of Interventions
Aroma therapy improved subjective sleep quality in nurses as reported in four reviewed studies. This is consistent with a meta-analysis on aroma therapy interventions for improvement of sleep quality in the general population (Hwang & Shin, 2015). That meta-analysis revealed that the use of aroma therapy was effective in improving sleep quality and that inhalation aroma therapy was more effective than massage therapy in both healthy and unhealthy participants (Hwang & Shin, 2015). Specific guidelines for the use of aroma therapy targeted to nurses is needed. Limitations to aroma therapy include the requirement of personal effort (especially through massage), materials, and time. Research examining aroma therapy in promoting sleep has several limitations. Besides small sample sizes, the studies included here also varied by aroma oil type, administering method, and duration, limiting our ability to draw definitive conclusions about the effectiveness of aroma therapy for sleep in nurses.
Dietary supplements (e.g., Zinc, CoQ10, Shimian granules) were each found to have a positive effect on subjective sleep quality of nurses in four reviewed studies. Supplements belong to nutrients or dietary intake, suggesting a link between diet and sleep. A recent narrative review of the effect of diet on sleep suggested that high carbohydrate diets and foods containing tryptophan, melatonin, and phytonutrients were linked to improvements in sleep outcomes such as insomnia in the general population (Binks et al., 2020). Although dietary supplements have shown positive effects on certain subjective sleep outcomes such as improved sleep quality and reduced insomnia severity in nurses, the mechanisms explaining the effects are not well understood. Due to an underwhelming amount of research in nurses, and these limited studies that assessed different supplements, different frequencies, and durations, we cannot be conclusive regarding effectiveness of any specific supplement on improving nurses’ sleep.
CBT-I has been demonstrated to be the most effective treatment for chronic insomnia in the general population and could hold promise to improve the sleep of nurses as reported in three out of five reviewed studies. A systematic review and meta-analysis of CBT-I for chronic insomnia found improvements in SOL, WASO, total sleep time, and sleep efficiency at post-treatment, with clinically meaningful effect sizes (Trauer et al., 2015). Another systematic review suggested that CBT-I was effective for treating insomnia when compared with medications such as benzodiazepine and non-benzodiazepine hypnotic drugs, and its effects may be more durable than medications (Mitchell et al., 2012). Considering nurses’ demanding work schedules, CBT aimed at improving sleep may be an option. However, most previous CBT-I was not targeted towards night shift workers attempting to sleep during the day, so it is unclear whether it will be effective in nurses working irregular shifts. Moreover, there are many forms of CBT-I delivery, with some requiring regular in-person or virtual meetings over many weeks, and this form of delivery may be difficult for nurses who work at night or on rotating shifts to attend. Self-paced, app-based CBT-I may be a better fit for nurses and should be explored further.
Light therapy has previously been implemented in workplaces as a strategy to reduce nighttime sleepiness and improve daytime sleep by shifting the timing of the circadian system to better match the work-sleep schedule. There were overall positive effects reported on at least one sleep outcome for all types and durations of light exposures, including both subjective and objective sleep outcomes as reported in ten reviewed studies. This is consistent with a meta-analysis on light therapy for sleep problems (van Maanen et al., 2016) and another meta-analysis on light therapy for sleepiness and circadian phase shift in shift workers (Lam & Chung, 2021). Another systematic review on light therapy for shift workers included two comparable studies, one that reported a reduction of on-shift sleepiness from bright light therapy during the night, while the other did not find a significant difference in on-shift sleepiness (Slanger et al., 2016). Because certain sleep outcomes such as sleepiness and sleep efficiency showed inconclusive results in our review of studies in nurses, more rigorously designed future studies should be carried out to investigate the impact of light therapy on the sleep and sleepiness of nurses. The Working Time Society and the International Committee on Occupational Health recommend bright light use during the first three night shifts on slowly rotating (shift changes less than once a week) night shift schedules (Lowden et al., 2019). Yet, there remain questions about the best light intensity and duration for producing changes in sleepiness and/or improvements in sleep that are clinically relevant. While light therapy is promising, the feasibility of light therapy may be limited by the lack of control over workplace lighting by individual nurses and by the nature of work duties for many nurses.
Mind-body therapies have shown effectiveness in improving subjective and objective sleep of nurses as reported in five reviewed studies. This is confirmed by two recent systematic reviews of studies carried out in the general population. For example, Neuendorf and colleagues reported that mind-body therapies have a positive effect on sleep quality (Neuendorf et al., 2015). Wang and colleagues reported in a meta-analysis that mind-body therapies (e.g., meditation, Tai Chi, qigong, yoga) resulted in significant improvement in sleep quality and reduction in insomnia severity, but had no significant effect on sleep duration (Wang et al., 2019). Mind-body therapies also emphasize the importance of self-care, leading to a holistic approach to health and well-being (Hilcove et al., 2020). Limitations to adoption of mind-body therapies in shift working nurses include costs and fees for lessons and locating and accessing trained yoga practitioners. The studies in nurses used different types of mind-body therapies, different frequencies, and varied durations, limiting the ability to make a firm recommendation on any specific therapy.
Sleep education showed effectiveness in improving subjective sleep quality of nurses as reported in two reviewed studies. A recent systematic review suggested that sleep education along with support for individualized strategies to promote sleep were effective for improving the quality of sleep in general (Soprovich et al., 2020). However, it is worth noting that one sleep education study included in this review had a dropout rate of 77% (Morimoto et al., 2016), suggesting the importance of practice reinforcement after the education program. Sleep education programs provided by the workplace, whether via training sessions, brochures, or other methods, may encourage healthy sleep hygiene practice in nurses and thereby potentially improve their sleep duration and quality.
Exercise to improve the sleep of nurses was reported in one reviewed study. Although this study showed promise on nurses’ sleep, more studies are needed to confirm this effect. A systematic review of RCTs suggested that chronic resistance exercise improves many aspects of sleep and has the greatest benefit for improving sleep quality in the general population (Kovacevic et al., 2018). Therefore, exercise could be a potential intervention for improving sleep in nurses. Because nurses are predominantly women working long and irregular shifts, it is important to design and test feasible exercise programs that can be easily implemented and sustained in the workforce.
Implementing naps at work in nurses as a strategy to reduce on-shift sleepiness was reported in one reviewed study. A previous systematic review on the effects of napping in night shift workers revealed that night shift napping led to decreased sleepiness and improved sleep-related performance, despite short periods of sleep inertia (grogginess and poor performance) immediately following the naps (Ruggiero & Redeker, 2014). In our review, only one study assessed the effectiveness of a nap on the sleepiness of nurses. Furthermore, the study did not specifically examine the impact of the at-work nap on the sleep quantity and/or quality of the nurses after work. Nap effectiveness in reducing sleepiness also depends on when and how long nurses take naps during the shift. Implementation of a nap at work requires administrative support, sufficient staffing, availability of appropriate space for napping, a culture that accepts workplace naps, and organizational policies that allow napping (Scott et al., 2010a). Feasibility and barriers to implementation need to be assessed before such a strategy can be successfully incorporated into practice.
Shift schedule modification showed positive effects in improving the sleep of nurses as reported in one reviewed study. There are many different dimensions of shift schedules, including shift duration/length, shift starting and ending time, number of consecutive shifts, and number of hours and days off between shifts, leading to many ways in which schedules can be modified. Considering the complexity of shift schedules in different organizations, it is important to tailor the shift schedule modification according to the organizational needs and feasibilities.
The combination of different interventions showed promise in improving the sleep of nurses as reported in five reviewed studies. Multicomponent interventions have been designed for the prevention and treatment of sleep problems in other populations, which all show promise in improving sleep outcomes (Epstein et al., 2012; Wilfling et al., 2021). Therefore, individualized and holistic approaches should be considered in future directions for sleep interventions in this occupational group (Alfonsi et al., 2021). Given that individual factors may affect the person’s ability to cope with shift work and sleep problems, individualized interventions that use different components could be tailored to the nurse’s work schedule, preferences, time availability, and other factors.
Limitations
This review has several limitations. First, the review was limited to English language studies. The relatively small number of included studies for each intervention type, together with the variability in treatment regimen, frequency, and duration, and variability in sleep-related outcome measures, limit the conclusions that can be drawn. Second, for 15 studies it was unclear whether the nurse participants worked regular or irregular shifts. Moreover, for interventions such as aroma therapy, dietary supplements, cognitive behavioral therapy, mind-body therapy, sleep education, and exercise, it was unclear whether the interventions incorporated components to mitigate the impact of shift work on sleep. Third, given the limitations in the research methodology (e.g., small sample sizes, loss to follow up, difficulties in blinding participants, weak designs) and quality of many of these studies, it is difficult to compare the effectiveness of each intervention. Lastly, although sleep is an important self-care domain, it is greatly impacted by work factors. It is important to identify to what extent each of these interventions may be implemented by the workplace or affected by the workplace contexts or policies. Future research needs to address the influence of shift work and other workplace factors on the outcomes of sleep interventions for nurses.
Conclusions and Implications for Practice
Of all the research on interventions to improve sleep, relatively few studies have been targeted towards nurse participants. Literature on each intervention type for improvement of sleep in nurses is limited and there are contradictory outcomes regarding the effectiveness of the intervention. Generally, light therapy, napping, and shift schedule modification are interventions designed for shift workers, among which, light therapy was most widely tested and showed promising findings in improving sleep of nurses. Most of the included studies used self-reported sleep, which may not be as reliable as objective measures. Additional research with high quality and consistent interventions (in particular, selection of participants, frequency and duration of treatment, and appropriate objective and subjective assessments of sleep outcomes) are needed to compare between intervention types and to verify and compare their effectiveness. However, we hope that findings from this review will inform and guide future research, including choice of interventions, and reliability and validity of outcomes measures (e.g., promoting use of objective measures). We hope that this encourages the design and implementation of evidence-based interventions to promote the sleep of nurses, which may in turn improve their work performance, productivity, and overall health.
Workplace context such as shift work is important to consider in relation to sleep promotion programs in the nursing workforce. Some of the interventions require administrative support (e.g., schedule changes), environmental changes in the workplace (e.g., light therapy), or availability of space on the unit (e.g., napping). Feasibility, facilitators, and barriers to implementation need to be assessed by both end-users and managers before workplace programs can be successfully implemented and sustained. The design and implementation of such programs should also consider nurses’ long and irregular work schedules, non-work responsibilities, as well as their individual needs and interests. For example, the convenient location, schedule, duration, and frequency of an intervention program should be planned to accommodate nurses’ working schedules. Participatory process engages workers to take actions to improve their own health (Baum et al., 2006). Therefore, workplaces should consider implementing participatory processes to improve nurses’ sleep. This in turn may have a transformative effect on the success of workplace sleep promotion programs.
Supplementary Material
Acknowledgement
The authors acknowledge two senior librarians, Sara Marks and Amanda Rust, who provided valuable help in the literature search process.
Funding sources
YZ, HML, LKB, and JFD are supported by a grant from the U.S. National Institutes of Health (R01 AG044416). LKB is supported in part by the U.S. National Institute for Occupational Safety and Health (R01 OH011773-01). The funder played no role in the study design and analysis, manuscript preparation, or decision to publish the report.
Footnotes
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
No Patient or Public Contribution
Because this is a systematic review of published literature, there was no involvement in the study from patients, service users, caregivers, or members of the public.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- Aarts MPJ, Hartmeyer SL, Morsink K, Kort HSM, & de Kort YAW (2020). Can special light glasses reduce sleepiness and improve sleep of nightshift workers? A placebo-controlled explorative field study. Clocks & Sleep, 2(2), 225–245. 10.3390/clockssleep2020018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albakri U, Drotos E, & Meertens R (2021). Sleep health promotion interventions and their effectiveness: An umbrella review. International Journal of Environmental Ressearch and Public Health, 18(11). 10.3390/ijerph18115533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfonsi V, Scarpelli S, Gorgoni M, Pazzaglia M, Giannini AM, & De Gennaro L (2021). Sleep-related problems in night shift nurses: Towards an individualized interventional practice. Frontiers in Human Neuroscience, 15, 644570. 10.3389/fnhum.2021.644570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baradari AG, Alipour A, Mahdavi A, Sharifi H, Nouraei SM, & Zeydi AE (2018). The effect of zinc supplementation on sleep quality of ICU nurses: A double blinded randomized controlled trial. Workplace Health & Safety, 66(4), 191–200. 10.1177/2165079917734880 [DOI] [PubMed] [Google Scholar]
- Baum F, MacDougall C, & Smith D (2006). Participatory action research. Journal of Epidemiology and Community Health, 60(10), 854–857. 10.1136/jech.2004.028662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binks H, G EV, Gupta C, Irwin C, & Khalesi S (2020). Effects of diet on sleep: A narrative review. Nutrients, 12(4). 10.3390/nu12040936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorvatn B, Pallesen S, Waage S, Thun E, & Blytt KM (2021). The effects of bright light treatment on subjective and objective sleepiness during three consecutive night shifts among hospital nurses - A counter-balanced placebo-controlled crossover study. Scandinavian Journal of Work, Environment & Health, 47(2), 145–153. 10.5271/sjweh.3930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boivin DB, Boudreau P, James FO, & Kin NM (2012). Photic resetting in night-shift work: Impact on nurses’ sleep. Chronobiology International, 29(5), 619–628. 10.3109/07420528.2012.675257 [DOI] [PubMed] [Google Scholar]
- Booker LA, Sletten TL, Barnes M, Alvaro P, Collins A, Chai-Coetzer CL, McMahon M, Lockley SW, Rajaratnam SMW, & Howard ME (2022). The effectiveness of an individualized sleep and shift work education and coaching program to manage shift work disorder in nurses: A randomized controlled trial. Journal of Clinical Sleep Medicine, 18(4), 1035–1045. 10.5664/jcsm.9782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Books C, Coody LC, Kauffman R, & Abraham S (2017). Night shift work and its health effects on nurses. Health Care Manager, 36(4), 347–353. 10.1097/hcm.0000000000000177 [DOI] [PubMed] [Google Scholar]
- Capezuti E, Zadeh RS, Woody N, Basara A, & Krieger AC (2018). An integrative review of nonpharmacological interventions to improve sleep among adults with advanced serious illness. Journal of Palliative Medicine, 21(5), 700–717. 10.1089/jpm.2017.0152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PA, Dyer KA, & Mikan SQ (2013). Sleep disturbance, chronic stress, and depression in hospice nurses: Testing the feasibility of an intervention. Clinical Journal of Oncology Nursing, 17, E368–E373. 10.1188/13.ONF.E368-E373 [DOI] [PubMed] [Google Scholar]
- Caruso CC, & Hitchcock EM (2010). Strategies for nurses to prevent sleep-related injuries and errors. Rehabilitation Nursing, 35(5), 192–197. [DOI] [PubMed] [Google Scholar]
- Çelik A, & Yarali S (2023). The effect of laughter yoga on the psychological resilience and sleep quality of nurses during the pandemic: A randomized controlled trial. Alternative Therapies in Health and Medicine, 29(5), 146–152. [PubMed] [Google Scholar]
- Chaiard J, Deeluea J, Suksatit B, Songkham W, Inta N, & Stone TE (2019). Sleep disturbances and related factors among nurses. Nursing & Health Sciences, 21(4), 470–478. 10.1111/nhs.12626 [DOI] [PubMed] [Google Scholar]
- Chang YY, Lin CL, & Chang LY (2017). The effects of aromatherapy massage on sleep quality of nurses on monthly rotating night shifts. Evidence-based Complementary & Alternative Medicine, 2017, 1–8. 10.1155/2017/3861273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng WJ, & Cheng Y (2017). Night shift and rotating shift in association with sleep problems, burnout and minor mental disorder in male and female employees. Occupational and Environmental Medicine, 74(7), 483–488. 10.1136/oemed-2016-103898 [DOI] [PubMed] [Google Scholar]
- Cyr M, Artenie DZ, Al Bikaii A, Lee V, Raz A, & Olson JA (2023). An evening light intervention reduces fatigue and errors during night shifts: A randomized controlled trial. Sleep Health. 10.1016/j.sleh.2023.02.004 [DOI] [PubMed] [Google Scholar]
- Dahlgren A, Tucker P, Epstein M, Gustavsson P, & Soderstrom M (2022). Randomised control trial of a proactive intervention supporting recovery in relation to stress and irregular work hours: Effects on sleep, burn-out, fatigue and somatic symptoms. Occupational and Environmental Medicine, 79(7), 460–468. 10.1136/oemed-2021-107789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein DR, Sidani S, Bootzin RR, & Belyea MJ (2012). Dismantling multicomponent behavioral treatment for insomnia in older adults: A randomized controlled trial. Journal of Sleep and Sleep Disorders Research, 35(6), 797–805. 10.5665/sleep.1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang R, & Li X (2015). A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. Journal of Clinical Nursing, 24(23–24), 3374–3379. 10.1111/jocn.12983 [DOI] [PubMed] [Google Scholar]
- Franco L, Sánchez C, Bravo R, Rodríguez AB, Barriga C, Romero E, & Cubero J (2012). The sedative effect of non-alcoholic beer in healthy female nurses. PloS One, 7(7), 1–6. 10.1371/journal.pone.0037290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan S, Magee M, Stone JE, Mulhall MD, Collins A, Howard ME, Lockley SW, Rajaratnam SMW, & Sletten TL (2019). The impact of shift work on sleep, alertness and performance in healthcare workers. Scientific Report, 9(1), 4635. 10.1038/s41598-019-40914-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griepentrog JE, Labiner HE, Gunn SR, & Rosengart MR (2018). Bright environmental light improves the sleepiness of nightshift ICU nurses. Critical Care, 22(1), 295. 10.1186/s13054-018-2233-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausswirth C, Nesi X, Dubois A, Duforez F, Rougier Y, & Slattery K (2022). Four weeks of a neuro-meditation program improves sleep quality and reduces hypertension in nursing staff during the COVID-19 pandemic: A parallel randomized controlled trial. Frontiers in Psychology, 13, 854474. 10.3389/fpsyg.2022.854474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović j., Schulz KF, Weeks L, & Sterne JA (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilcove K, Marceau C, Thekdi P, Larkey L, Brewer MA, & Jones K (2020). Holistic nursing in practice: Mindfulness-based yoga as an intervention to manage stress and burnout. Journal of Holistic Nursing, 0898010120921587. [DOI] [PubMed] [Google Scholar]
- Hoshi H, Iwasa H, Goto A, & Yasumura S (2022). Effects of working environments with minimum night lighting on night-shift nurses’ fatigue and sleep, and patient safety. British Medical Journal Open Quality, 11(1). 10.1136/bmjoq-2021-001638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu H-C, Lin M-H, Lee H-F, Wu C-Y, Chou C-T, & Lin S-F (2021). Effects of aromatherapy with essential oil massage on the sleep quality of critical care nurses: A randomized controlled trial. Complementary Therapies in Clinical Practice, 43, 101358. 10.1016/j.ctcp.2021.101358 [DOI] [PubMed] [Google Scholar]
- Huang LB, Tsai MC, Chen CY, & Hsu SC (2013). The effectiveness of light/dark exposure to treat insomnia in female nurses undertaking shift work during the evening/night shift. Journal of Clinical Sleep Medicine, 9(7), 641–646. 10.5664/jcsm.2824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang E, & Shin S (2015). The effects of aromatherapy on sleep improvement: A systematic literature review and meta-analysis. Journal of Alternative and Complementary Medicine, 21(2), 61–68. 10.1089/acm.2014.0113 [DOI] [PubMed] [Google Scholar]
- Imes CC, Barthel NJ, Chasens ER, Dunbar-Jacob J, Engberg SJ, Feeley CA, Fennimore LA, Godzik CM, Klem ML, Luyster FS, Ren D, & Baniak L (2023). Shift work organization on nurse injuries: A scoping review. International Journal Of Nursing Studies, 138, 104395. 10.1016/j.ijnurstu.2022.104395 [DOI] [PubMed] [Google Scholar]
- Jensen HI, Markvart J, Holst R, Thomsen TD, Larsen JW, Eg DM, & Nielsen LS (2016). Shift work and quality of sleep: Effect of working in designed dynamic light. International Archives of Occupational and Environmental Health, 89(1), 49–61. 10.1007/s00420-015-1051-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacevic A, Mavros Y, Heisz JJ, & Fiatarone Singh MA (2018). The effect of resistance exercise on sleep: A systematic review of randomized controlled trials. Sleep Medicine Reviews, 39, 52–68. 10.1016/j.smrv.2017.07.002 [DOI] [PubMed] [Google Scholar]
- Kubo T, Matsumoto S, Izawa S, Ikeda H, Nishimura Y, Kawakami S, Tamaki M, & Masuda S (2022). Shift-work schedule intervention for extending restart breaks after consecutive night shifts: A non-randomized controlled cross-over study. International Journal of Environmental Research and Public Health, 19(22). 10.3390/ijerph192215042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam C, & Chung M-H (2021). Dose–response effects of light therapy on sleepiness and circadian phase shift in shift workers: A meta-analysis and moderator analysis. Scientific Reports, 11(1). 10.1038/s41598-021-89321-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KA, Gay CL, & Alsten CR (2014). Home-based behavioral sleep training for shift workers: A pilot study. Behavioral Sleep Medicine, 12(6), 455–468. 10.1080/15402002.2013.825840 [DOI] [PubMed] [Google Scholar]
- Liu Y, Jiang T-T, Shi T-Y, Liu Y-N, Liu X-M, Xu G-J, Li F-L, Wang Y-L, & Wu X-Y (2021). The effectiveness of diaphragmatic breathing relaxation training for improving sleep quality among nursing staff during the COVID-19 outbreak: A before and after study. Sleep Medicine, 78, 8–14. 10.1016/j.sleep.2020.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowden A, Ozturk G, Reynolds A, & Bjorvatn B (2019). Working Time Society consensus statements: Evidence based interventions using light to improve circadian adaptation to working hours. Industrial Health, 57(2), 213. https://umasslowell.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=edsghw&AN=edsgcl.642580726&site=eds-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell MD, Gehrman P, Perlis M, & Umscheid CA (2012). Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review. Biomedical Chromatography Family Practice, 13, 40. 10.1186/1471-2296-13-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morimoto H, Tanaka H, Ohkubo R, Mimura M, Ooe N, Ichikawa A, & Yukitoshi H (2016). Self-help therapy for sleep problems in hospital nurses in Japan: A controlled pilot study. Sleep and Biological Rhythms, 14, 177–185. 10.1007/s41105-015-0037-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavi S, Mohammadi V, & Foroughi Z (2020). Effect of coenzyme Q10 supplementation on work-related fatigue in nurses: A double-blind, randomized placebo-controlled study. Fatigue: Biomedicine, Health & Behavior, 8(1), 1–10. 10.1080/21641846.2019.1704374 [DOI] [Google Scholar]
- Nasiri A, & Boroomand MM (2021). The effect of rosemary essential oil inhalation on sleepiness and alertness of shift-working nurses: A randomized, controlled field trial. Complementary Therapies in Clinical Practice, 43, 101326. 10.1016/j.ctcp.2021.101326 [DOI] [PubMed] [Google Scholar]
- Neuendorf R, Wahbeh H, Chamine I, Yu J, Hutchison K, & Oken BS (2015). The effects of mind-body interventions on sleep quality: A systematic review. Evidence-Based Complementary and Alternative Medicine, 2015, 902708. 10.1155/2015/902708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu S-F, Lin C-J, Chen P-Y, Fan Y-C, Huang H-C, & Chiu H-Y (2021). Immediate and lasting effects of aerobic exercise on the actigraphic sleep parameters of female nurses: A randomized controlled trial. Research in Nursing & Health, 44(3), 449–457. 10.1002/nur.22126 [DOI] [PubMed] [Google Scholar]
- Nourian M, Nikfarid L, Khavari AM, Barati M, & Allahgholipour AR (2021). The impact of an online mindfulness-based stress reduction program on sleep quality of nurses working in COVID-19 care units: A clinical trial. Holistic Nursing Practice, 35(5), 257–263. 10.1007/s10389-020-01313-z [DOI] [PubMed] [Google Scholar]
- Omeogu C, Shofer F, Gehrman P, & Green-McKenzie J (2020). Efficacy of a mobile behavioral intervention for workers with insomnia. Journal of Occupational and Environmental Medicine, 62(3), 246–250. 10.1093/sleep/zsx143 [DOI] [PubMed] [Google Scholar]
- Owens B, Allen W, & Moultrie D (2017). The impact of shift work on nurses’ quality of sleep. Official Journal of the Association of Black Nursing Faculty in Higher Education, 28(3), 59–63. [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC,…Moher D (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Journal of Clinical Epidemiology, 134, 178–189. 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- Pallesen S, Bjorvatn B, Waage S, Harris A, & Sagoe D (2021). Prevalence of shift work disorder: A systematic review and meta-analysis. Frontiers in Psychology, 12, 638252. 10.3389/fpsyg.2021.638252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parajuli N, Pradhan B, & Jat M (2021). Effect of four weeks of integrated yoga intervention on perceived stress and sleep quality among female nursing professionals working at a tertiary care hospital: A pilot study. Industrial Psychiatry Journal, 30(1), 136–140. 10.4103/ipj.ipj_11_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Querstret D, O’Brien K, Skene DJ, & Maben J (2020). Improving fatigue risk management in healthcare: A systematic scoping review of sleep-related/fatigue-management interventions for nurses and midwives. International Journal of Nursing Studies, 106. 10.1016/j.ijnurstu.2019.103513 [DOI] [PubMed] [Google Scholar]
- Rahman SA, Shapiro CM, Wang F, Ainlay H, Kazmi S, Brown TJ, & Casper RF (2013). Effects of filtering visual short wavelengths during nocturnal shiftwork on sleep and performance. Chronobiology International, 30(8), 951–962. 10.3109/07420528.2013.789894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redeker NS, Caruso CC, Hashmi SD, Mullington JM, Grandner M, & Morgenthaler TI (2019). Workplace interventions to promote sleep health and an alert, healthy workforce. Journal of Clinical Sleep Medicine, 15(4), 649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers AE (2008). The effects of fatigue and sleepiness on nurse performance and patient safety. In Hughes RG (Ed.), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Rosa D, Terzoni S, Dellafiore F, & Destrebecq A (2019). Systematic review of shift work and nurses’ health. Occupational Medicine, 69(4), 237–243. 10.1093/occmed/kqz063 [DOI] [PubMed] [Google Scholar]
- Ruggiero JS, & Redeker NS (2014). Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: A systematic review. Biological Research for Nursing, 16(2), 134–142. 10.1177/1099800413476571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, Daneshkhah A, Khaledi-Paveh B, & Hosseinian-Far M (2020). The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: A systematic review and meta-analysis. Globalization and Health, 16(1). 10.1186/s12992-020-00620-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott LD, Arslanian-Engoren C, & Engoren MC (2014). Association of sleep and fatigue with decision regret among critical care nurses. American Journal of Critical Care, 23(1), 13–23. 10.4037/ajcc2014191 [DOI] [PubMed] [Google Scholar]
- Scott LD, Hofmeister N, Rogness N, & Rogers AE (2010a). Implementing a fatigue countermeasures program for nurses: A focus group analysis. Journal of Nursing Administration, 40(5), 233–240. 10.1097/NNA.0b013e3181da4078 [DOI] [PubMed] [Google Scholar]
- Scott LD, Hofmeister N, Rogness N, & Rogers AE (2010b). An interventional approach for patient and nurse safety: A fatigue countermeasures feasibility study. Nursing Research, 59(4), 250–258. 10.1097/NNR.0b013e3181de9116 [DOI] [PubMed] [Google Scholar]
- Seo MS, & Park D (2017). The effect of inhaling aromas on the quality of sleep and fatigue of shift working nurses. Journal of Engineering and Applied Sciences, 12(14), 3612–3615. 10.36478/jeasci.2017.3612.3615 [DOI] [Google Scholar]
- Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, Ortega RAR, Costa G, Driscoll TR, Foster RG, Fristchi L, Sallinen M, Liira J, & Erren TC (2016). Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. The Cochrane Database of Systematic Reviews, 2016(8), Cd010641. 10.1002/14651858.CD010641.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, McDonald AD, & Sasangohar F (2021). The impact of commutes, work schedules, and sleep on near-crashes during nurses’ post shift-work commutes: A naturalistic driving study. IISE Transactions on Occupational Ergonomics and Human Factors, 9(1), 13–22. 10.1080/24725838.2021.1945708 [DOI] [PubMed] [Google Scholar]
- Soprovich AL, Seaton CL, Bottorff JL, Duncan MJ, Caperchione CM, Oliffe JL, … Johnson ST (2020). A systematic review of workplace behavioral interventions to promote sleep health in men. Sleep Health, 6(3), 418–430. 10.1016/j.sleh.2020.04.008 [DOI] [PubMed] [Google Scholar]
- Stimpfel AW, Fatehi F, & Kovner C (2020). Nurses’ sleep, work hours, and patient care quality, and safety. Sleep Health, 6(3), 314–320. 10.1016/j.sleh.2019.11.001 [DOI] [PubMed] [Google Scholar]
- Sun Q, Ji X, Zhou W, & Liu J (2019). Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. Journal of Nursing Management, 27(1), 10–18. 10.1111/jonm.12656 [DOI] [PubMed] [Google Scholar]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, & Cunnington D (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191–204. 10.7326/m14-2841 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2019). Your Health Care is in Women’s Hands. Retrieved March 7, 2023 from https://www.census.gov/library/stories/2019/08/your-health-care-in-womens-hands.html [Google Scholar]
- van Maanen A, Meijer AM, van der Heijden KB, & Oort FJ (2016). The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Medicine Reviews, 29, 52–62. 10.1016/j.smrv.2015.08.009 [DOI] [PubMed] [Google Scholar]
- Wang X, Li P, Pan C, Dai L, Wu Y, & Deng Y (2019). The effect of mind-body therapies on insomnia: A systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2019, 9359807. 10.1155/2019/9359807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickwire EM, Geiger-Brown J, Scharf SM, & Drake CL (2017). Shift work and shift work sleep disorder: Clinical and organizational perspectives. Chest, 151(5), 1156–1172. 10.1016/j.chest.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfling D, Hylla J, Berg A, Meyer G, Köpke S, Halek M, Möhler R, Dichter MN (2021). Characteristics of multicomponent, nonpharmacological interventions to reduce or avoid sleep disturbances in nursing home residents: A systematic review. Internaltional Psychogeriatrics, 33(3), 245–273. 10.1017/s1041610220000733 [DOI] [PubMed] [Google Scholar]
- Yazdi Z, Jalilolghadr S, & Tootoonchian F (2017). Effects of a sleep hygiene education program on sleep problems in female nurses on shift work. Journal of Sleep Sciences, 2(1–2), 28–33. [Google Scholar]
- Zhang L, Zhang R, Shen Y, Qiao S, Hui Z, & Chen J (2020). Shimian granules improve sleep, mood and performance of shift nurses in association changes in melatonin and cytokine biomarkers: A randomized, double-blind, placebo-controlled pilot study. Chronobiology International, 37(4), 592–605. 10.1080/07420528.2020.1730880 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Duffy JF, & de Castillero ER (2017). Do sleep disturbances mediate the association between work-family conflict and depressive symptoms among nurses? A cross-sectional study. Journal of Psychiatric and Mental Health Nursing, 24(8), 620–628. 10.1111/jpm.12409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, El Ghaziri M, Dugan AG, & Castro ME (2019). Work and health correlates of sleep quantity and quality among correctional nurses. Journal of Forensic Nursing, 15(1), 42–51. 10.1097/jfn.0000000000000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Tang M, & Zhou Y (2023). Holistic sleep improvement strategies for frontline nurses served during a public health emergency (COVID-19) in Wuhan, China: A quasi-experimental study. Nursing Open, 10(3), 1471–1481. 10.1002/nop2.1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou K, Kong J, Wan Y, Zhang X, Liu X, Qu B, Wang B, & Xue R (2022). Positive impacts of e-aid cognitive behavioural therapy on the sleep quality and mood of nurses on site during the COVID-19 pandemic. Sleep & Breathing, 26(4), 1947–1951. 10.1007/s11325-021-02547-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zion N, & Shochat T (2019). Let them sleep: The effects of a scheduled nap during the night shift on sleepiness and cognition in hospital nurses. Journal of Advanced Nursing, 75(11), 2603–2615. 10.1111/jan.14031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.