Abstract
Introduction
We describe an outbreak of Serratia marcescens (S. marcescens) infection in the neonatal intensive care unit at Women's Hospital in Sinaloa, Mexico.
Methods
In April 2021, an outbreak of S. marcescens infection was identified. A case was identified as any patient who tested positive for S. marcescens and showed signs of an infectious process.
Results
S. marcescens was isolated from the blood cultures of 15 neonates with clinical signs of neonatal sepsis. Statistical analysis showed that all neonates had an invasive medical device. The problem was controlled after hospital hygiene and sanitation measures were strengthened.
Conclusion
The study provides evidence of an outbreak of nosocomial bacteremia due to the cross-transmission of S. marcescens. The findings highlight the need for hospitals to implement strict hygiene measures, especially regarding hand washing, to prevent future outbreaks.
1. Introduction
Serratia marcescens (S. marcescens) is an aerobic, Gram-negative bacillus of the Enterobacteriaceae family with multiple virulence factors, including several enzymes and the ability to form biofilms; this bacterium is found in the normal microbiota of the human gut. Epidemic outbreaks of S. marcescens have been reported with mechanical ventilators and disinfectants such as chlorhexidine [1, 2], soaps, stethoscope [3], incubator [4] parenteral solutions [5, 6], infant shampoo [7], and hands as possible sources of transmission. Based on the abovementioned, this pathogen has been classified as an opportunistic pathogen in hospitalized patients causing nosocomial outbreaks [8].
Several risk factors have been identified in outbreaks of S. marcescens, such as prematurity [9], in severely immunocompromised or critically ill patients of all ages [10], especially in intensive care units (ICUs) and in neonatal intensive care units (NICUs) [11], causing healthcare-associated infections (HAIs) due to this germ [12, 13]. In the United States, Serratia species are responsible for 1.4% of nosocomial bacteremias. In Mexico, it is estimated that 450,000 cases of nosocomial infections occur annually, causing 32 deaths per 100,000 inhabitants per year (whose annual cost of care is nearly 1.5 billion) [14].
S. marcescens can cause asymptomatic or symptomatic infections with a wide range of clinical manifestations [15]. Among the symptoms are keratitis, conjunctivitis, urinary tract infections, pneumonia, surgical wound infections, sepsis, meningitis, and bloodstream infections [11, 16, 17]. It is the third most common pathogen causing epidemic outbreaks [18].
In recent decades, this microorganism has become more critical as it is responsible for outbreaks that are difficult to control with multidrug-resistant strains, especially in NICUs [11, 19]. The high survival capacity of the microorganism in the hands of healthcare workers [20], prolonged stay, use of invasive medical devices, and previous administration of antibiotics during pregnancy are described as risk factors for its acquisition.
In Mexico, antimicrobial resistance [21] and virulence profiles [22] have been evaluated in S. marcescens isolates from different regions of the country. Similarly, outbreaks of nosocomial bacteremia and colonization by S. marcescens have been reported in an intensive care unit (ICU) [23] and the neonatal intensive care unit (NICU) [24]. In Sinaloa, no evidence addresses this type of problem. Hence, the description of the outbreak of Serratia marcescens is of great relevance to seeking alternatives that help prevent and manage infections caused by this type of pathogens, especially in the intrahospital setting.
The purpose of presenting a case series of an epidemic outbreak caused by S. marcescens with its clinical and epidemiological characteristics is to improve patient-centered care and avoid new healthcare-associated infections or early and timely detection to prevent or reduce morbidity and mortality.
2. Materials and Methods
An outbreak of 15 cases of neonatal S. marcescens infection from April to May 2021 and records before the 2020 outbreak were analyzed. The cases were identified in the neonatal unit of the Women's Hospital in Sinaloa, located in northwestern Mexico. The hospital has a capacity of 32 census beds and an average birth rate of 500 newborns per month. All newborns with a positive blood culture for S. marcescens, with or without clinical symptoms, were included as confirmed cases during the abovementioned period. An outbreak was defined as two or more cases of healthcare-associated infections (HAIs) acquired by patients, healthcare workers, and/or visitors to the hospital unit [25, 26]. S. marcescens was isolated from blood cultures processed by the Women's Hospital staff.
In addition, a follow-up was performed until May 2022, during which the medical records of all suspected cases of infection were analyzed. In addition, possible sources of S. marcescens contamination were identified, and environmental cultures were collected from neonatal areas, equipment, supplies, water, soap, antiseptics, milk, and staff hands. The present study was approved by the Ethics Committee of the Women's Hospital (no. 202206-12).
3. Results
In 2020 (before the outbreak), there were 6,548 births at the Women's Hospital of Sinaloa, with no reported cases of S. marcescens. In 2021, 4,698 newborns were born, of which 15 had nosocomial S. marcescens infection, with an incidence of 0.0031 per 1000 newborns. Out of the fifteen neonates who were infected with S. marcescens, nine were taken to the NICU, five were taken to intermediate care, and one was placed in the ward with their mother. It is important to note that all the neonates were from the neonatal transitional zone.
The first neonate (primary index case) was born on April 10, 2021, and was admitted to the NICU with a diagnosis of transient tachypnea of the newborn (TTRN). The neonate displayed clinical manifestations within 4 hours of life, which included symptoms such as vomiting, tachypnea, and an abrupt onset of shock. The neonate's culture was positive for S. marcescens 48 hours after birth, and cases began to appear after that, which was considered an epidemic outbreak. Figure 1 shows the epidemiologic course of the affected neonates.
Figure 1.
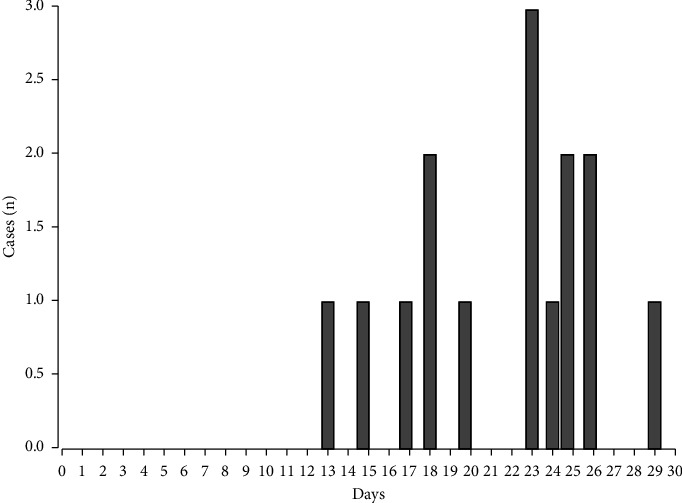
Epidemiologic curve of the S. marcescens outbreak in the neonatal intensive care unit of the Women's Hospital in Sinaloa, Mexico.
The 15 infected neonates were born to Mexican mothers, of whom 20% (n = 3/15) were adolescents and 80% (n = 12/15) were adults, with ages ranging from 15 to 39 years and a mean age of 24.6 years. All the mothers had at least one risk factor for neonatal sepsis, the most common being maternal infection (27% (n = 4/15)), hypertension (27% (n = 4/15)), and diabetes (20% (n = 3/15)). The mean number of antenatal visits was 5.8.
The distribution of the neonatal delivery route was as follows: 47% (n = 7/15) vaginal and 53.3% (n = 8/15) abdominal. Forty-seven percent (n = 7/15) of the neonates were preterm (equal to or less than 36 weeks' gestation (WG)) and 53% (n = 8/15) were term (37 to 42 WG), with a minimum of 32 WG, a maximum of 40, and a mean of 36.9 WG. 13% (n = 2/15) weighed less than 2500 g, and 87% (n = 13/15) weighed more than 2500 g with a minimum of 1500 g, a maximum of 3500 g, and a mean of 2912 g. Of the 15 neonates, 93% (n = 14/15) were born with adequate weight for their gestational age and 7% (n = 1/15) with high weight for gestational age. Of the neonates, 73.3% (n = 11/15) were identified as male and 26.6% (n = 4/15) as female. The mean length of hospital stays before S. marcescensisolation ranged from 4 to 30 hours after birth. The mean length of hospital stay was 19 days (minimum 5 and maximum 40) (Table 1).
Table 1.
Clinical characteristics of the S. marcescens outbreak cases in the neonatal intensive care unit of the Women's Hospital in Sinaloa, Mexico.
| Nos. | Gender | Admission age (hours) | Admitting diagnosis | Pregnancy status (w) | Admission weight (g) | Hospital days before S. marcescens isolation | Procedures before the symptoms | Previous antibiotics therapy | Symptoms | Antibiotics therapy | Final diagnosis | Hospital days until discharge | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 4 | TTN | Term (39) | 2870 | 2 | CPAP, nasal tips, peripheral catheter, parenteral solutions | Not | Respiratory distress, vomiting, abdominal distension, jaundice, hepatosplenomegaly, fever, pallor, skin color changes, thrombocytopenia, and ventricular hemorrhage | Yes | Sepsis respiratory | 5 | Death |
|
| |||||||||||||
| 2 | F | 24 | TTN/SDR | Term (40) | 2900 | 1 | CPAP, intubation, mechanical ventilation, umbilical catheter | Not | Respiratory distress, jaundice, fever, thrombocytopenia | Yes | Sepsis respiratory | 18 | Health improvement |
|
| |||||||||||||
| 3 | M | 11 | TTN/ARDS/respiratory depression | Preterm (36) | 3250 | 1 | NIPPV, intubation, umbilical catheter, mechanical ventilation, parenteral solutions | Not | Respiratory distress, abdominal distension, jaundice, hepatosplenomegaly, fever, pallor, skin color changes, hypoactivity | Yes | Sepsis respiratory | 21 | Health improvement |
|
| |||||||||||||
| 4 | F | 24 | APGAR low score/neonatal asphyxia | Term (39) | 3200 | 1 | NIPPV, peripheral catheter, parenteral solutions | Not | Respiratory distress, jaundice, fever, pallor, thrombocytopenia | Yes | Sepsis respiratory | 20 | Health improvement |
|
| |||||||||||||
| 5 | M | 6 | Sepsis risk by poor prenatal control | Term (39) | 3150 | 2 | Peripheral catheter, parenteral solutions | Yes | Respiratory distress, vomiting, abdominal distension, fever, thrombocytopenia | Yes | Sepsis respiratory | 21 | Health improvement |
|
| |||||||||||||
| 6 | M | 24 | TTRN/ARDS | Preterm (32) | 1600 | 1 | CPAP, intubation, umbilical catheter, and parenteral solutions | Not | Respiratory distress, jaundice, fever, pallor, thrombocytopenia, and lung hemorrhage | Yes | Sepsis respiratory | 30 | Health improvement |
| 7 | M | 27 | TTRN/ARDS | Term (39) | 2930 | 3 | CPAP, nasal tips, umbilical catheter, and parenteral solutions | Not | Respiratory distress, abdominal distension, skin color change, hypoactivity, thrombocytopenia, digestive hemorrhage | Yes | Sepsis respiratory | 14 | Health improvement |
|
| |||||||||||||
| 8 | M | 24 | TTN/ARDS/sepsis risk by maternal cervicovaginitis | Preterm (36) | 2470 | 4 | NIPPV, CPAP, intubation, umbilical catheter, parenteral solution, orogastric tube | Yes | Respiratory distress, jaundice, fever, pallor, skin color change, hypoactivity, digestive-ventricular hemorrhages | Yes | Sepsis respiratory | 40 | Transferred∗ to another hospital |
|
| |||||||||||||
| 9 | M | 18 | TTN/ARDS/neonatal asphyxia/perinatal asphyxia/MAS | Term (39) | 3400 | 8 | NIPPV, intubation, umbilical catheter, and parenteral solutions | Not | Jaundice, fever, skin color change, thrombocytopenia | Yes | Sepsis respiratory | 27 | Health improvement |
|
| |||||||||||||
| 10 | F | 6 | TTN/ARDS | Preterm (35) | 2700 | 1 | NIPPV, CPAP, umbilical catheter, and parenteral solutions | Not | Respiratory distress, abdominal distension, jaundice, hepatosplenomegaly, fever, skin color change, hypoactivity, thrombocytopenia, digestive hemorrhage | Yes | Sepsis respiratory | 15 | Health improvement |
|
| |||||||||||||
| 11 | M | 36 | TTN/ARDS | Term (37) | 2620 | 5 | CPAP, nasal tips, umbilical catheter, peripheral catheter, and parenteral solutions | Not | Vomit, jaundice, hepatosplenomegaly, hypoactivity, thrombocytopenia | Yes | Sepsis respiratory | 16 | Health improvement |
| 12 | M | 48 | TTN/ARDS | Term (38) | 3320 | 3 | CPAP, nasal tips, umbilical catheter, and parenteral solutions | Not | Jaundice, fever, pallor, skin color change, thrombocytopenia | Yes | Sepsis respiratory | 15 | Health improvement |
|
| |||||||||||||
| 13 | M | 20 | TTN/ARDS | Preterm (36) | 3500 | 1 | CPAP, umbilical catheter, and parenteral solutions | Yes | Respiratory distress, abdominal distension, jaundice, hepatosplenomegaly, fever, pallor, skin color change, hypoactivity, hemorrhages | Yes | Sepsis respiratory | 17 | Health improvement |
|
| |||||||||||||
| 14 | M | 11 | TTN/ARDS/neonatal asphyxia | Preterm (36) | 2910 | 1 | NIPPV, CPAP, intubation, mechanical ventilation, umbilical catheter, and parenteral solutions | Not | Skin color changes, hypoactivity, and thrombocytopenia | Yes | Sepsis respiratory | 13 | Health improvement |
|
| |||||||||||||
| 15 | F | 31 | Neonatal jaundice/early-onset neonatal sepsis | Preterm (35) | 2930 | 1 | No procedures | Not | No symptoms | Yes | Colonization | 11 | Health improvement |
Nos.: numbers, TTN: transient tachypnea of the newborn, ARDS: acute respiratory distress syndrome, MAS: meconium aspiration syndrome, w: weeks, NIPPV: intermittent positive pressure ventilation, and CPAP: continuous positive airway pressure. ∗: the patient was transferred for requiring procedures that the hospital did not have, and the patient left the hospital infection-free.
93% (n = 14/15) of the neonates had an invasive medical device before infection, such as vascular access; 66% (n = 10/15) had an umbilical catheter, 26.6% (n = 4/15) had a peripheral catheter, only one neonate had no prior vascular access or another type of device, and 20% (n = 3/15) received previous antibiotic treatment, as shown in Table 1. Regarding feeding, 93% (n = 14/15) received mixed feeding (combination of breast milk and formula). Twenty percent (n = 3/15) of the neonates received prior antibiotic treatment.
The type of infection observed was neonatal sepsis in 93% (n = 14/15), with respiratory changes predominating in 66% (n = 10/15), jaundice was present in 80% (n = 12/15) of the neonates, 47% (n = 7/15) had gastrointestinal manifestations, thrombocytopenia was present in 80% (n = 12/15), fever and dysthermia were present in 73.3% (n = 11/15), and earthy skin with color changes was observed mainly in 60% (n = 9/15), as shown in Table 1. Regarding biochemical parameters, procalcitonin was elevated in 86.6% (n = 13/15) of the neonates and C-reactive protein (CRP) in 80% (n = 12/15) (Supplementary Table 1). Only the index case died on the fifth day of life and hospitalization, resulting in a case fatality rate of 7%. The S. marcescens strain was susceptible to most antimicrobials, and the neonates received mainly ampicillin, amikacin, cefotaxime, and some also meropenem, among others.
In addition, cultures were obtained from potential fomites (medical equipment, areas, supplies, and personnel) (Supplementary Table 2). The follow-up of the outbreak continued for one year, and the results of cultures collected from neonates admitted to the NICU during this time were monitored, with both preoutbreak and outbreak cultures being negative for S. marcescens.
4. Discussion
Therefore, S. marcescens is widely distributed in the environment and is particularly associated with hospital-acquired infections and hospital-associated outbreaks. More than 200 hospital outbreaks caused by S. marcescens have been reported in the medical literature since 1950 [27]. Outbreaks have affected pediatric [19] and adult populations, immunocompromised hosts, and intensive care units (ICUs) [28]. In this study, an outbreak of S. marcescens was identified in 15 neonates at the Women's Hospital of Sinaloa, only one of whom died.
According to Canadian studies, the incidence of Serratia infections is estimated at 10.8 per 100,000 persons per year, with a hospital incidence rate of 0.4 per 1,000 hospitalized patients [13]. On the other hand, a multicenter study of premature infants in 774 hospitals in the United States showed an increased incidence of invasive Serratia, corresponding to approximately 2.3 Serratia infections per 1,000 premature infants [29]. Both studies showed a higher incidence than that found in our work. Most infants were transferred on average at about 20 hours of age, which may seem like a long time; however, the specificity of sepsis symptoms in the first 24 hours has low specificity, resulting in long transfer times to the ICU [30]. On the other hand, time to care for neonates with sepsis is very important; it has been estimated that the likelihood of neonatal mortality can increase by up to 1.5% for every hour of delay in transferring these patients to the ICU [31]. More effective tools are needed to identify neonatal sepsis as early as possible and provide the best treatment.
Regarding Mexico, a study conducted in a NICU at the Children's Hospital of Mexico between May 2005 and July 2006 reported an outbreak of S. marcescens. In this outbreak, only one case of S. marcescens was identified in neonates between May 2005 and May 2006, corresponding to 0.08 cases/14 admissions/month; after placing the first case, these increased to 7/14 admissions/month. No cases were identified in the month of follow-up after the outbreak [32]. The data from this outbreak are consistent with those reported in our study since the outbreak was stopped thanks to control measures.
In this work, 80% of the cases corresponded to males and 20% to females, which is similar to what has been reported in another outbreak [2], but at the same time, different from what has been reported by other researchers [15, 24], probably because when the outbreak occurs, it can affect both males and females equally. On the other hand, most of the cases corresponded to neonates born at term with a birth weight of more than 2,500 grams, which contrasts with what has been reported by other authors who identify low birth weight and prematurity as risk factors for morbidity and mortality due to this type of pathogen [19].
Regarding sepsis, the predominant manifestations in this study were generalized changes, jaundice, respiratory distress, and thrombocytopenia. These data are consistent with those reported by Voeltz et al., who, in a systematic review of 27 studies of S. marcescens outbreaks in neonatal and pediatric intensive care units, identified symptoms similar to those in our study [19].
In addition, most of the neonates in this study were exposed to a device placed in the airway, which is a significant risk factor for S. marcescens infection, which is consistent with the literature that medical devices are a risk factor for contamination and transmission of these pathogens [5]. However, despite multiple cultures in the environment and on devices, supplies, equipment, and materials, S. marcescens was not detected in the cultures. In addition, only 20% had received prior antibiotic treatment, which is in contrast to what other studies have reported, as this is a risk factor for the development of nosocomial infections due to early exposure to such drugs with consequent high antimicrobial resistance [33].
The evidence from our study shows that the outbreak had a horizontal transmission mechanism as the same bacterial strain was isolated in all cases. The index patient rapidly evolved with predominantly respiratory and gastrointestinal symptoms and severe sepsis. Contrary to what has been reported in the literature, where prolonged hospital stay is a significant risk factor, in this case series, the hospital stay before the onset of infection was very short, less than 30 hours.
It is now recognized that nosocomial outbreaks can result from poor hygienic practices and contamination of materials within a hospital, facilitating infection transmission and affecting many patients. In the present report, an outbreak of neonatal S. marcescens infection was identified in 15 cases, one of which died (case fatality rate of 7%). According to different reports, the case fatality rate of S. marcescens infection varies widely, ranging from 8% to 69% [34–37], although the trend is high in most reports. In this study, however, a low mortality rate was reported, possibly because of rapid detection and because S. marcescens was susceptible to a wide range of antibiotics, which helped to eradicate infections.
This study had the limitation that bacterial genotyping studies were not performed because blood culture samples were discarded. In addition, the lack of fecal analysis of the exposed neonates and the index patient, who had early gastrointestinal and respiratory data until the development of severe sepsis, might have revealed the origin of the infection via the gastrointestinal route and its subsequent dissemination via the hematogenous route. Although S. marcescens tends to colonize the human gastrointestinal tract, preventive measures should be promoted and implemented, with emphasis on those involving direct contact with the patient, by performing hand disinfection activities, using new gloves, clean medical equipment, and exclusive clothing such as gowns for the care of each neonate.
5. Conclusion
The epidemiologic analysis of this study provides evidence of an outbreak of nosocomial bacteremia that started in the transitional area and spread from there to different areas (NICU, intermediate care, and wards), probably caused by cross-transmission of S. marcescens by personnel or an invasive medical device, since the source of transmission could not be identified. On the other hand, it is essential to emphasize that different intervention strategies to contain outbreaks should focus on basic daily activities such as proper hand washing, use of clean medical equipment, and disinfection of other areas within a hospital to significantly reduce prolonged stays, morbidity, and mortality from these diseases, as well as the costs generated by neonatal sepsis.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval
The study was approved by the Ethics Committee of the Women's Hospital, Secretariat of Health (no. 202206-12).
Disclosure
This submission has not been published previously and is not simultaneously being considered for publication elsewhere.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Martha Guel-Gomez, Edna Mendívil-Zavala, Amparo Plata-Guzmán, Jesus J. Martinez-Garcia, Angela Ochoa-Espinoza, Paola Crespo-Palazuelos, Jesús Bracamontes-Murillo, and Angel León-Ramírez were involved in patient care, contributed to data interpretation, and revised the article critically for important intellectual content. Uriel A. Angulo-Zamudio, Nidia Leon-Sicairos, Hector Flores-Villaseñor, Jorge Angulo-Rocha, Juan C. Rodriguez-Ceceña, and Adrian Canizalez-Roman provided background research, performed data curation, wrote the original draft, and revised the article critically for important intellectual content. Martha Guel-Gomez, Uriel A. Angulo-Zamudio, Nidia Leon-Sicairos, Juan C. Rodriguez-Ceceña, and Adrian Canizalez-Roman were involved in the conception of the manuscript, acquired and interpreted results, and drafted the manuscript. All the authors approved the final submitted manuscript.
Supplementary Materials
Supplementary Table 1: laboratory parameters of neonates infected with S. marcescens. Laboratory parameters such as leukocytes, platelets, procalcitonin, and C-reactive protein (CRP) in newborn infants who have been infected with the pathogen. Supplementary Table 2: screening for S. marcescens in samples collected from various areas of the Women's Hospital. Samples for bacterial culture were collected from floors and walls, air conditioners, oxygen and air intakes, furniture, medical equipment (cribs, incubators, and ventilators), water, milk, supplies, catheters, soap, computer equipment, and staff hands.
References
- 1.Hervé B., Chomali M., Gutiérrez C., et al. Brote de infección nosocomial por Serratia marcescens asociado a contaminación intrínseca de clorhexidina acuosa. Revista chilena de infectología . 2015;32(5):517–522. doi: 10.4067/s0716-10182015000600004. [DOI] [PubMed] [Google Scholar]
- 2.de Frutos M., López-Urrutia L., Domínguez-Gil M., et al. Serratia marcescens outbreak due to contaminated 2% aqueous chlorhexidine. Enfermedades Infecciosas Y Microbiología Clínica . 2017;35(10):624–629. doi: 10.1016/j.eimc.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Millán-Lou M. I., López C., Bueno J., et al. Successful control of Serratia marcescens outbreak in a neonatal unit of a tertiary-care hospital in Spain. Enfermedades Infecciosas y Microbiología Clínica . 2022;40(5):248–254. doi: 10.1016/j.eimc.2021.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Morillo Á., González V., Aguayo J., et al. A six-month Serratia marcescens outbreak in a neonatal intensive care unit. Enfermedades Infecciosas Y Microbiología Clínica . 2016;34(10):645–651. doi: 10.1016/j.eimc.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Hejazi A., Falkiner F. R. Serratia marcescens. Journal of Medical Microbiology . 1997;46(11):903–912. doi: 10.1099/00222615-46-11-903. [DOI] [PubMed] [Google Scholar]
- 6.Chiang P. C., Wu T. L., Kuo A. J., et al. Outbreak of Serratia marcescens postsurgical bloodstream infection due to contaminated intravenous pain control fluids. International Journal of Infectious Diseases . 2013;17(9):e718–e722. doi: 10.1016/j.ijid.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Madani T. A., Alsaedi S., James L., et al. Serratia marcescens-contaminated baby shampoo causing an outbreak among newborns at King Abdulaziz University Hospital, Jeddah, Saudi Arabia. Journal of Hospital Infection . 2011;78(1):16–19. doi: 10.1016/j.jhin.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 8.Elistratova A. A., Matrosova L. E., Khilyas I. V., et al. Serratia marcescensduf1471-containing protein SrfN is needed for adaptation to acid and oxidative stresses. mSphere . 2022;7(6) doi: 10.1128/msphere.00212-22.e0021222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cano-González S. B., Romero-Vázquez A., Santamaría-Muñoz R. Factores de riesgo asociados a sepsis por Serratia marcescens en una unidad de cuidados intensivos neonatales. J Salud en Tabasco . 2004;10(2):214–220. [Google Scholar]
- 10.Serrano C., Juliet C., Fernández A., Leiva V., Fernández J. Serratia marcescens: descripción de un brote de infección intrahospitalaria. J Revista chilena de infectología . 2002;19(4):262–266. [Google Scholar]
- 11.Cristina M. L., Sartini M., Spagnolo A. M. Serratia marcescens infections in neonatal intensive care units (NICUs) International Journal of Environmental Research and Public Health . 2019;16(4):p. 610. doi: 10.3390/ijerph16040610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engel H. J., Collignon P. J., Whiting P. T., Kennedy K. J. Serratia sp. bacteremia in Canberra, Australia: a population-based study over 10 years. European Journal of Clinical Microbiology & Infectious Diseases . 2009;28(7):821–824. doi: 10.1007/s10096-009-0707-7. [DOI] [PubMed] [Google Scholar]
- 13.Laupland K. B., Parkins M. D., Gregson D. B., Church D. L., Ross T., Pitout J. D. Population-based laboratory surveillance for Serratia species isolates in a large Canadian health region. European Journal of Clinical Microbiology & Infectious Diseases . 2008;27(2):89–95. doi: 10.1007/s10096-007-0400-7. [DOI] [PubMed] [Google Scholar]
- 14.Salgado M. R. Frecuencia de infecciones asociadas a la atención de la salud en los principales sistemas de información de México. J Boletín Conamed . 2018;17 [Google Scholar]
- 15.Soria C., Nieto N., Villacís J. E., Lainez S., Cartelle M. Brote por Serratia marcescens en una Unidad de Cuidados Intensivos Neonatales: guayaquil-Ecuador. Revista chilena de infectología . 2016;33(6):703–705. doi: 10.4067/s0716-10182016000600016. [DOI] [PubMed] [Google Scholar]
- 16.Acar J. F. Serratia marcescens infections. Infection Control . 1986;7(5):273–280. doi: 10.1017/s0195941700064201. [DOI] [PubMed] [Google Scholar]
- 17.Dessì A., Puddu M., Testa M., Marcialis M. A., Pintus M. C., Fanos V. Serratia marcescens infections and outbreaks in neonatal intensive care units. Journal of Chemotherapy . 2009;21(5):493–499. doi: 10.1179/joc.2009.21.5.493. [DOI] [PubMed] [Google Scholar]
- 18.Gastmeier P., Loui A., Stamm-Balderjahn S., et al. Outbreaks in neonatal intensive care units-they are not like others. American Journal of Infection Control . 2007;35(3):172–176. doi: 10.1016/j.ajic.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Voelz A., Müller A., Gillen J., et al. Outbreaks of Serratia marcescens in neonatal and pediatric intensive care units: clinical aspects, risk factors and management. International Journal of Hygiene and Environmental Health . 2010;213(2):79–87. doi: 10.1016/j.ijheh.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Milisavljevic V., Wu F., Larson E., et al. Molecular epidemiology of Serratia marcescens outbreaks in two neonatal intensive care units. Infection Control and Hospital Epidemiology . 2004;25(9):719–722. doi: 10.1086/502466. [DOI] [PubMed] [Google Scholar]
- 21.González G. M., de J Treviño-Rangel R., Campos C. L., et al. Surveillance of antimicrobial resistance in Serratia marcescens in Mexico. New Microbiologica . 2020;43(1):34–37. [PubMed] [Google Scholar]
- 22.González G. M., Andrade A., Villanueva-Lozano H., et al. Comparative analysis of virulence profiles of Serratia marcescens isolated from diverse clinical origins in Mexican patients. Surgical Infections . 2020;21(7):608–612. doi: 10.1089/sur.2020.029. [DOI] [PubMed] [Google Scholar]
- 23.Volkow P., Ponce de S., Sifuentes J., Calva J. J., Ruiz G. Epidemia de bacteremias primarias por una cepa endémica de SERRATIA marcescens en una unidad de terapia intensiva. Salud Pública de México . 1993;35(5):440–447. [PubMed] [Google Scholar]
- 24.Romano–Mazzotti L. M.-P., Pérez–Robles V., Santos–Preciado J., Alcántar–Curiel D., Alpuche–Aranda C. Brote de bacteriemia nosocomial y colonización por Serratia marcescens en una Unidad de Cuidado Intensivo Neonatal. Boletín médico del Hospital Infantil de México . 2007;64 [Google Scholar]
- 25.Steinhaus E. Serratia marcescens Bizio as an insect pathogen. Hilgardia . 1959;28(14):351–380. doi: 10.3733/hilg.v28n14p351. [DOI] [Google Scholar]
- 26.Haque K. N. Definitions of bloodstream infection in the newborn. Pediatric Critical Care Medicine . 2005;6:S45–S49. doi: 10.1097/01.pcc.0000161946.73305.0a. [DOI] [PubMed] [Google Scholar]
- 27.Mahlen S. D. Serratia infections: from military experiments to current practice. Clinical Microbiology Reviews . 2011;24(4):755–791. doi: 10.1128/cmr.00017-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Boer M. G., Brunsveld-Reinders A. H., Salomons E. M., et al. Multifactorial origin of high incidence of Serratia marcescens in a cardio-thoracic ICU: analysis of risk factors and epidemiological characteristics. Journal of Infection . 2008;56(6):446–453. doi: 10.1016/j.jinf.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 29.Coggins S. A., Edwards E. M., Flannery D. D., Gerber J. S., Horbar J. D., Puopolo K. M. Serratia infection epidemiology among very preterm infants in the neonatal intensive care unit. The Pediatric Infectious Disease Journal . 2023;42(2):152–158. doi: 10.1097/inf.0000000000003736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vincent J. L., Opal S. M., Marshall J. C., Tracey K. J. Sepsis definitions: time for change. The Lancet . 2013;381(9868):774–775. doi: 10.1016/s0140-6736(12)61815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cardoso L. T., Grion C. M., Matsuo T., et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Critical Care . 2011;15(1):p. R28. doi: 10.1186/cc9975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Romano-Mazzotti L., Murguía-Peniche T., Pérez-Robles V. M., Santos-Preciado J. I., Alcántar-Curiel D., Alpuche-Aranda C. M. Brote de bacteriemia nosocomial y colonización por Serratia marcescens en una Unidad de Cuidado Intensivo Neonatal. J Boletín médico del Hospital Infantil de México . 2007;64(1):9–17. [Google Scholar]
- 33.Weissman S. J., Hansen N. I., Zaterka-Baxter K., Higgins R. D., Stoll B. J. Emergence of antibiotic resistance-associatedclones among Escherichia coli recovered from newborns with early-onset sepsis and meningitis in the United States, 2008–2009: table 1. Journal of the Pediatric Infectious Diseases Society . 2016;5(3):269–276. doi: 10.1093/jpids/piv013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miranda-Novales M., Gordillo-Pérez M., Solórzano-Santos F., Leaños-Miranda B., Villasís-Keever M. A., Villegas-Silva R. Brote por Serratia marcescens en una unidad de cuidados intensivos neonatales (UCIN). Estudio de casos y controles. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion . 1998;50(1):13–18. [PubMed] [Google Scholar]
- 35.Yu W., Lin C., Wang D. Serratia marcescens bacteremia: clinical features and antimicrobial susceptibilities of the isolates. J Journal of Microbiology, Immunology . 1998;31(3):171–179. [PubMed] [Google Scholar]
- 36.Uduman S. A., Farrukh A. S., Nath K. N., et al. An outbreak of Serratia marcescens infection in a special-care baby unit of a community hospital in United Arab Emirates: the importance of the air conditioner duct as a nosocomial reservoir. Journal of Hospital Infection . 2002;52(3):175–180. doi: 10.1053/jhin.2002.1308. [DOI] [PubMed] [Google Scholar]
- 37.Kim S. B., Jeon Y. D., Kim J. H., et al. Risk factors for mortality in patients with Serratia marcescens bacteremia. Yonsei Medical Journal . 2015;56(2):348–354. doi: 10.3349/ymj.2015.56.2.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: laboratory parameters of neonates infected with S. marcescens. Laboratory parameters such as leukocytes, platelets, procalcitonin, and C-reactive protein (CRP) in newborn infants who have been infected with the pathogen. Supplementary Table 2: screening for S. marcescens in samples collected from various areas of the Women's Hospital. Samples for bacterial culture were collected from floors and walls, air conditioners, oxygen and air intakes, furniture, medical equipment (cribs, incubators, and ventilators), water, milk, supplies, catheters, soap, computer equipment, and staff hands.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.


