ABSTRACT
Background
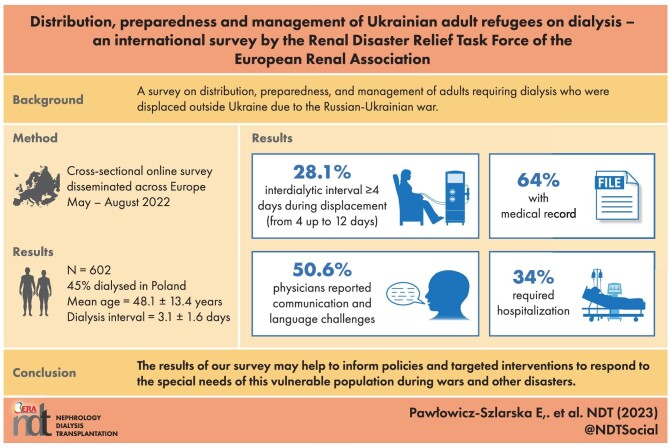
Due to the Russian–Ukrainian war, some of the about 10 000 adults requiring dialysis in Ukraine fled their country to continue dialysis abroad. To better understand the needs of conflict-affected dialysis patients, the Renal Disaster Relief Task Force of the European Renal Association conducted a survey on distribution, preparedness and management of adults requiring dialysis who were displaced due to the war.
Methods
A cross-sectional online survey was sent via National Nephrology Societies across Europe and disseminated to their dialysis centers. Fresenius Medical Care shared a set of aggregated data.
Results
Data were received on 602 patients dialyzed in 24 countries. Most patients were dialyzed in Poland (45.0%), followed by Slovakia (18.1%), Czech Republic (7.8%) and Romania (6.3%). The interval between last dialysis and the first in the reporting center was 3.1 ± 1.6 days, but was ≥4 days in 28.1% of patients. Mean age was 48.1 ± 13.4 years, 43.5% were females. Medical records were carried by 63.9% of patients, 63.3% carried a list of medications, 60.4% carried the medications themselves and 44.0% carried their dialysis prescription, with 26.1% carrying all of these items and 16.1% carrying none. Upon presentation outside Ukraine, 33.9% of patients needed hospitalization. Dialysis therapy was not continued in the reporting center by 28.2% of patients until the end of the observation period.
Conclusions
We received information about approximately 6% of Ukrainian dialysis patients, who had fled their country by the end of August 2022. A substantial proportion were temporarily underdialyzed, carried incomplete medical information and needed hospitalization. The results of our survey may help to inform policies and targeted interventions to respond to the special needs of this vulnerable population during wars and other disasters in the future.
Keywords: conflicts, dialysis, disasters, refugees, wars
Graphical Abstract
Graphical Abstract.
KEY LEARNING POINTS.
What is already known about this subject?
During armed conflicts dialysis patients may experience limitations or interruptions to therapy leading to severe life-threatening complications due to medical and logistical challenges.
Before the Russian–Ukrainian war, there were approximately 10 000 adults receiving long-term dialysis in Ukraine.
Some of these patients fled their place of residence and looked for opportunities to continue dialysis elsewhere in Ukraine or abroad. The number of such patients and their condition after displacement were thus far unknown.
What this study adds?
By the end of August 2022, we received information about approximately 6% of Ukrainian dialysis patients who fled their country since the start of the Russian–Ukrainian conflict, with the majority receiving dialysis in a country neighboring Ukraine.
Preparedness for displacement varied and was incomplete in most patients.
Almost 30% of displaced patients remained without dialysis for 4 days or longer.
Clinical status upon arrival to the host countries often necessitated hospitalization.
What impact this may have on practice or policy?
Monitoring the movement and condition of dialysis patients during armed conflicts and the present results may help inform policies that allow for prompt and targeted interventions to respond to the special needs of this vulnerable population during wars and other emergencies around the globe.
INTRODUCTION
On 24 February 2022 Russia initiated an invasion of Ukraine [1]. As of 24 September 2022, the number of Ukrainians who fled the country was estimated to be almost 7.5 million [2]. Additionally, several millions of Ukrainians migrated internally, mostly to the western part of Ukraine [3].
The impact of conflicts on health is overwhelming [4]. Direct effects include gunshot injuries and trauma-related morbidity and mortality. Assessment of indirect effects is challenging, as they remain underestimated and under-recorded. They include the impact of conflict on infectious diseases, non-communicable diseases, morbidity due to reduced healthcare access, and interruption of antenatal, pediatric and maternal services and of mental healthcare. In recent years, there has been a growing awareness of the burden of chronic diseases in conflicts [4].
There are several reports on the situation of patients with kidney diseases during natural disasters [5, 6], but less is known about the influence of military conflicts on this vulnerable population. The impact of wars on patients with kidney diseases was recently summarized in a consensus statement from the Renal Disaster Relief Task Force (RDRTF) of the European Renal Association (ERA) [7]. Patients on maintenance hemodialysis (HD) are at risk of prolonged underdialysis due to damaged healthcare infrastructure, suboptimal availability of water and energy supplies, shortage of dialysis personnel, transportation difficulties or the need to flee. Consequently, especially non-adherence to fluid and dietary restrictions may lead to serious, life-threatening complications. Patients on peritoneal dialysis (PD) may face logistical problems in obtaining dialysis solutions on time, and are at high risk of complications, such as peritoneal dialysis-related peritonitis or exit-site infections due to unhygienic circumstances. Patients after kidney transplantation may suffer from interruptions of maintenance immunosuppressive treatment and are at risk of serious infections due to their immunosuppressed state [7].
The possibility of leaving affected zones may be impacted by many factors including severity of disability, and economic, personal, emotional and cultural determinants [7].
As of 1 January 2021, there were 11 181 patients (268 per million population) on kidney replacement therapy (KRT) in Ukraine, including 6017 on HD, 2700 on hemodiafiltration, 931 on PD and 1533 with kidney transplants [8]. The exact number of Ukrainian KRT patients who were internally displaced, mostly to western parts of Ukraine, or who fled to neighboring countries is currently unknown. In accordance with the European Union protection act [9] neighboring country governments and healthcare systems provided support, including full reimbursement of healthcare costs and procedural assistance outside Ukraine. In addition, international kidney care organizations (ERA, the American Society of Nephrology, the International Society of Nephrology and the European Kidney Health Alliance) supported by the World Health Organization joined together in these relief efforts, including supply of dialysis equipment to Ukraine, organization of fundraisers, assistance for kidney patients remaining in Ukraine and to those displaced outside the country, as well as various support actions for Ukrainian nephrologists [10].
Due to scarce epidemiological data on refugees suffering from kidney failure, the RDRTF of the ERA conducted an international survey on distribution, preparedness and management of adults requiring dialysis outside Ukraine since the beginning of the war. The results may lead to a better understanding of the needs of patients with kidney failure affected by a conflict and may support improvement in preparedness procedures and equitable and evidence-based allocation of resources for this vulnerable population in ongoing and future conflicts.
MATERIALS AND METHODS
Data source
Survey data
A web-based survey hosted on the Survey Monkey application was distributed across Europe and adjacent countries that are located in the geographic area covered by the ERA (list of the countries is provided in Supplementary data, Table S1). The first e-mail invitation was sent to Presidents of National Societies of Nephrology on 16 May 2022 along with a request to disseminate the survey to a lead physician of each dialysis unit within their countries. The invitation was repeated after 5 weeks. The survey requested data about adult (≥18 years old) dialysis patients displaced from Ukraine, who received dialysis in public or private dialysis centers. Data collection was anonymized making identification of individual patients impossible. Details of the survey are provided in Supplementary data, File S1.
Aggregated data
Due to internal privacy procedures, all dialysis units from Fresenius Medical Care (FMC) shared a set of aggregated data without direct center participation. Results from all FMC European, the Middle East and Africa (EMEA) region units were provided by the FMC representatives.
Data collection
Data were collected between May 2022 and August 2022. The survey comprised questions on dialysis therapy before and at the time of war both in Ukraine and in the other countries, patients’ preparedness for displacement outside Ukraine, hospitalizations outside Ukraine, coronavirus disease 2019 (COVID-19) history, language barrier–related issues and psychological support received by the patients, demographic features (age, sex, education level) and medical history (cause of kidney failure). Questions about dialysis therapy concerned dialysis modality, time since start of dialysis, vascular access type, viral status and pharmacological treatment (erythropoiesis-stimulating agents, intravenous iron, vitamin D analogues, cinacalcet and phosphate binders).
Possible interruptions of treatment in Ukraine since the start of war (i.e. decreased frequency of dialysis sessions) were also addressed. Data about countries where patients were dialyzed after leaving their regular units in Ukraine were reported as well as data about kidney transplantation waitlist status in Ukraine and in the host country.
Additionally, for the cohort of patients dialyzed in Poland, the country hosting most Ukrainian dialysis patients, clinical and laboratory data at the time of admission to the center were gathered. Blood pressure and interdialytic body weight gain on admission to the reporting center as well as the first reported laboratory parameters were collected. Data about war-related or journey-related injuries were also gathered.
Aggregated data sent by FMC comprised gender, mean age, duration of KRT, viral status, vascular access type, COVID-19 testing and pharmacotherapy at the receiving center. The survey response rate for Polish dialysis units was 85%. For FMC EMEA units it was 100% (related to the aggregated nature of the received data).
The survey database was checked for double entries but no such cases were found.
All percentages sum up to 100%, although the total number of responses included in the percentage calculations was different for each question due to different number of non-responses and because some questions were covered only by the point-by-point survey and not by the FMC data. For some questions, ‘No data’ was an answer option—for those questions these responses were included up to 100%. The list of non-responses per particular question is presented in Supplementary data, Table S2.
Study oversight
The study was designed by the RDRTF of ERA. The study protocol and the survey were reviewed and approved by the ERA Scientific Advisory Board. The questionnaire was submitted to the Ethics Committee of the Medical University of Silesia in Katowice, Poland and need for ethics review was waived. Detailed authors’ contributions are provided at the end of this article.
RESULTS
Data on 602 patients who were dialyzed abroad in 24 countries after leaving Ukraine are reported. The distribution of patients per country is provided in Table 1. Most patients were dialyzed in Poland (45.0%), followed by Slovakia (18.1%), Czech Republic (7.8%), Romania (6.3%), Germany (4.7%) and Hungary (3.5%) (survey and aggregated FMC data together).
Table 1:
Number of dialysis patients displaced outside Ukraine and dialyzed abroad.
| Number of patients | |||
|---|---|---|---|
| Country | Survey data | Aggregated data | Total |
| Poland | 161 | 110 | 271 |
| Slovakia | 2 | 107 | 109 |
| Czech Republic | 19 | 28 | 47 |
| Romania | 9 | 29 | 38 |
| Germany | 28 | 0 | 28 |
| Hungary | 6 | 15 | 21 |
| Russia | 0 | 12 | 12 |
| Switzerland | 11 | 0 | 11 |
| Lithuania | 9 | 0 | 9 |
| Georgia | 5 | 0 | 5 |
| Latvia | 5 | 0 | 5 |
| Denmark | 4 | 0 | 4 |
| Belgium | 3 | 0 | 3 |
| Israel | 3 | 0 | 3 |
| Netherlands | 2 | 0 | 2 |
| Croatia | 1 | 0 | 1 |
| Finland | 1 | 0 | 1 |
| Luxembourg | 1 | 0 | 1 |
| Slovenia | 1 | 0 | 1 |
| Italy, Estonia, France, Portugal, Spain | Italy—14 | 11a | 30 |
| Estonia—5 | |||
| France—0 | |||
| Portugal—0 | |||
| Spain—0 | |||
aDue to the internal privacy policy, FMC gave the total number of patients for these five countries.
The location of dialysis units in Ukraine where patients were dialyzed before the displacement is provided in Fig. 1. Besides Kyiv, most patients left centers located in the south-east of Ukraine (survey data only).
Figure 1:
Location of dialysis units in Ukraine, where patients were dialyzed before the displacement and number of these patients.
At least one dialysis session/visit in one or more dialysis centers between the home institution in Ukraine and the reporting center had occurred in 34.6% of patients. The largest group of patients had these transit dialysis sessions in Poland (41.3%), Ukraine (25%, mostly in Lviv) or Slovenia (7.5%). All patients treated ad interim in Slovenia were finally dialyzed in Italy (survey data only).
Mean patient age was 48.1 ± 13.4 years, and 43.5% were females. Regarding education levels in the study group, 14.6% of patients had a university degree, 8.9% had vocational education, 18.9% secondary education and 3.2% primary education (data about education were captured only from 45.6% of migrants). Before leaving Ukraine, 98% had been on HD, 1.2% on continuous ambulatory PD and 0.8% on automated PD. Therapeutic shift from PD to HD after displacement occurred in two patients. Mean dialysis vintage was 57.7 ± 66.6 months (mean ± SD). Data on dialysis vascular access type (HD patients) and viral status (all patients) are provided in Table 2 (survey and aggregated data). The majority (89%) of HD patients had an arteriovenous fistula. Hepatitis B (HBs) antigen positivity was noted in 7.3% and anti-HBc antibodies in 27.3% of all patients.
Table 2:
Clinical data with regard to vascular access type (HD patients) and viral status (HD and PD patients) in the study group.
| % of patients | |
|---|---|
| Vascular access type | |
| Arteriovenous fistula | 89 |
| Arteriovenous graft | 2.0 |
| Tunneled catheter | 5.1 |
| Non-tunneled catheter | 3.9 |
| Viral status | |
| HBs antigen positive | 7.3 |
| Anti-HCV antibodies | 16.1 |
| Anti-HIV antibodies | 0.6 |
| Anti-HBc antibodies | 27.3 |
HBs antigen, antigen of the hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HBc antigen, hepatitis B virus protein (core antigen).
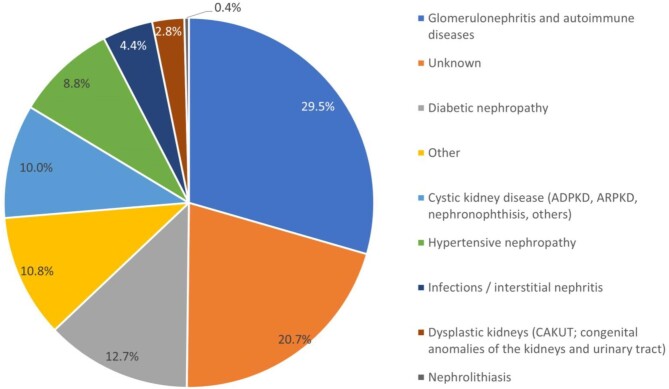
Primary causes of kidney failure are presented in Fig. 2 (survey data only). The most common causes of kidney disease were glomerulonephritis and autoimmune diseases (29.5%). In 20.7% the cause was unknown.
Figure 2:
Primary causes of kidney failure in the study group (survey data only). ADPKD, autosomal dominant polycystic kidney disease; ARPKD, autosomal recessive polycystic kidney disease; CAKUT, congenital anomalies of the kidney and urinary tract.
Under war conditions in Ukraine, HD session frequency was reduced in 23.5% of those patients who finally migrated. Mean time between last dialysis session and the first session in the reporting center was 3.1 ± 1.6 days. In 28.1% of patients this time interval ranged from 4 (16.8%) up to 12 days (survey data only).
Over one-quarter (28.2%) of patients had not continued dialysis therapy in the reporting center by the closure date of the survey (31 August). Mean number of HD visits was 11.6 ± 11.2; median 8, range 1–50; only three PD patients left the reporting centers, but the duration of stay was not provided. Of those not continuing in the reporting center, 4.1% had died and 94.6% left for another country or another city in the same country. Of the patients who left, 28.6% intended to return to Ukraine (survey data only).
Patient preparedness for displacement is outlined in Table 3. Overall, 26.1% of the patients presented in the host dialysis unit with their medical history, medication list, medications and dialysis prescriptions, whereas 16.1% presented with none of these (survey data only).
Table 3:
Possession of particular determinants of preparedness for displacement with regard to medical safety (survey data only).
| Preparedness determinant | % of patients |
|---|---|
| Medical records | 63.9 |
| List of medications | 63.3 |
| Medications themselves | 60.4 |
| Dialysis prescription | 44.0 |
After leaving Ukraine, 33.9% of patients were hospitalized upon presentation at the reporting center. The most common causes of hospitalizations are presented in Table 4.
Table 4:
Causes of hospitalizations outside Ukraine among displaced dialysis patients.
| Cause of hospitalization | Number of patients | % of patients |
|---|---|---|
| Anemia | 16 | 18.6 |
| COVID-19 pneumonia | 4 | 4.7 |
| Non-COVID-19 pneumonia | 4 | 4.7 |
| Fluid overload | 4 | 4.7 |
| Need for tunneled catheter implantation | 4 | 4.7 |
| Heart failure | 3 | 3.5 |
| Peripheral artery occlusive disease | 3 | 3.5 |
| Need AVF surgery | 3 | 3.5 |
| Acute cholecystitis | 2 | 2.3 |
| Above knee amputation | 2 | 2.3 |
| Myeloma | 2 | 2.3 |
| Endocarditis | 2 | 2.3 |
| Arterial hypertension | 2 | 2.3 |
| Dialysis peritonitis | 2 | 2.3 |
| Arrythmia | 2 | 2.3 |
| AVF thrombosis | 2 | 2.3 |
| GI hemorrhage | 2 | 2.3 |
| Ileus | 2 | 2.3 |
AVF, arteriovenous fistula; GI, gastrointestinal.
In the reporting dialysis units, 53.6% of patients received erythropoiesis-stimulating agents, 39.4% intravenous iron supplementation, 37.5% phosphate binders, 22.2% vitamin D analogues and 3.5% cinacalcet (survey and aggregated data). However, data on pharmacotherapy received in Ukraine before the displacement was insufficiently available to allow reliable information to be reported.
Twenty-nine patients (11.5%) had been waitlisted for kidney transplantation in Ukraine. Of these, 15 were also waitlisted for transplantation in their host country. In addition, 33 patients who had not been listed for transplantation in Ukraine started the listing process under the care of the reporting center (survey data only).
Of the 90.5% of patients tested for active severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the reporting center, 2.1% were positive (survey and aggregated data). At the time of presentation to the reporting center, 32.1% of patients had not been vaccinated, 8% had received three doses, 29.3% two doses and 1.6% one dose. Twenty-six patients (10.6%) were vaccinated while being cared for at the reporting dialysis center (survey data only).
Fifty-four percent of patients travelled to the destination country accompanied by at least one other person, mostly family members or, rarely, other people also requiring dialysis (survey data only).
Communication and language challenges were reported by 50.6% of responding physicians. Translation was not required in 30.4% of cases, in 26.4% a coworker was able to translate, in 17.2% patient's family members helped in translation, while 16.4% of responding physicians used telephone/internet translation services. In 9.6% of cases an interpreter, provided by hospital or dialysis unit, was physically available on site (survey data only).
A total of 43 patients (17.2%) received psychological support while being cared for in the reporting dialysis center. This service was provided by the dialysis unit itself for 29 patients and outside the center for 14 patients (survey data only).
Clinical data of the Polish cohort (survey data only)
Data about volume status, blood pressure and laboratory parameters at admission to the hosting dialysis units were collected only in Poland (N = 161). Since their last dialysis, 36.9% of patients had gained more than 3 kg of body weight, and 28.5% between 2 and 3 kg. Thirteen patients (8%) presented with a blood pressure ≥180/100 mmHg, an additional eight patients (5%) had systolic values above 180 mmHg, with diastolic values below 100 mmHg.
Detailed data on laboratory parameters are provided in Table 5. A substantial number of patients were admitted with marked anemia or hyperkalemia.
Table 5:
Laboratory parameters at admission to the hosting dialysis units collected in Poland.
| Percentage | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | N | Mean | SD | Median | Min-max | Range | % (N) |
| Hemoglobin (g/dL) | 126 | 9.5 | 1.8 | 9.15 | 5–14 | <7.0 | 7.9 (10) |
| 7.0–7.9 | 7.9 (10) | ||||||
| 8.0–8.9 | 25.4 (32) | ||||||
| 9.0–9.9 | 23.8 (30) | ||||||
| 10.0–11.5 | 19 (24) | ||||||
| >11.5 | 15.9 (20) | ||||||
| WBC count (×103/µL) | 118 | 6.6 | 2.4 | 6.3 | 2.7–16.3 | ||
| Platelet count (×103/µL) | 119 | 209.7 | 67.4 | 203 | 86–542 | ||
| Potassium (mmol/L) | 120 | 5.4 | 0.8 | 5.3 | 3.0–7.9 | <3.5 | 0.8 (1) |
| 3.5–5.0 | 30.8 (37) | ||||||
| 5.1–6.0 | 45.8 (55) | ||||||
| 6.1–7.0 | 20.8 (25) | ||||||
| >7.0 | 1.7 (2) | ||||||
| Sodium (mmol/L) | 113 | 138.7 | 2.7 | 139 | 132–145 | ||
| Calcium (mmol/L) | 98 | 2.2 | 0.3 | 2.2 | 1.6–3.1 | ||
| Phosphorus (mmol/L) | 93 | 3.6 | 2.3 | 2.4 | 0.9–10.1 | ||
| Creatinine (µmol/L) | 74 | 897.7 | 262.2 | 900.8 | 450.8–1522.2 | ||
| BUN (mg/dL) | 97 | 75.2 | 29.3 | 72.4 | 28–197 | ||
BUN, blood urea nitrogen; SD, standard deviation; WBC, white blood cells.
War-related injury (right shin hematoma) was reported in only one patient.
DISCUSSION
The Russian invasion of Ukraine forced some patients treated by dialysis to migrate to other places in Ukraine or abroad. The RDRTF established by the ERA coordinated comprehensive support for kidney patients in Ukraine. The whole spectrum of its mission and activities to date has been described elsewhere [11]. In this study we present results of an international survey conducted by the ERA Task Force which analyzed the distribution, preparedness and management of adult Ukrainian dialysis patients who migrated outside Ukraine since the Russian invasion.
Our survey documented that around 6% of all patients dialyzed in Ukraine migrated outside the country. This number may be underestimated because of incomplete distribution and/or response rates of the questionnaire, migration to non-included countries and patients who died before being captured in the survey. On the other hand, data response rates in Poland and within the FMC network were high, suggesting that we captured a large proportion of the total number of displaced patients. However, complete data on migration within Ukraine, mostly to the western part, or of mortality among Ukrainian dialysis patients is not available. Some data on relocation has been described elsewhere, including patients dialyzed in FMC centers in Chernihiv and Kharkiv who were moved to centers in Lviv and Cherkasy [12].
The proportion of dialysis patients who left the country was lower than one might have expected and a lot lower compared with migration of the general population [602 of 9648 (∼6%) vs 7.5 million of 43.8 million (∼17%)], likely reflecting enhanced vulnerability and limited mobility for various reasons of dialysis patients.
The mean age of dialysis patients fleeing Ukraine to foreign countries was 48.1 ± 13.4 years, which is markedly lower than the mean age in Europe of 62.1 years [13]. Precise data on the age of dialysis patients in Ukraine before the war is not available, but is on the mean age of all KRT patients together (on dialysis and with a kidney transplant), which was 53.4 years, and therefore at baseline was lower than the corresponding age in other European countries [14]. As the mean age of those who migrated was lower than the mean before the war, it is possible that mostly younger and less vulnerable dialysis patients were able to migrate outside Ukraine. This finding is in line with a report on Syrian hemodialysis refugees in Turkey by Gursu et al. [15].
Consistent with this is the observation that the proportion of patients with kidney failure from diabetic nephropathy (often associated with multiple comorbidities) among the displaced population was lower than that in the total Ukrainian dialysis population (12.7% vs 15.7%) [14].
It may follow, that if younger and less vulnerable dialysis patients left the country, the general health condition of the remaining cohort was worse and more demanding at a time when resources were suboptimal. This should be taken into account in preparation of crisis management plans, and the need for different emergency preparedness strategies to minimize risk of life-threatening complications both in those remaining in the conflict zones and those fleeing war-affected regions [16–19].
As expected, the majority of patients migrated to the neighboring countries, i.e. to Poland and Slovakia. Only about one-fourth of patients decided to subsequently leave the reporting dialysis center and to move to another city or country. These results may suggest that about three-fourths of the patients had directly migrated to a previously predetermined center of their choice, or that they were satisfied with the location where they arrived.
An important clinical finding is that during the migration almost 30% of patients remained without dialysis for 4 days or longer. This highlights the necessity for close cooperation between dialysis centers in the conflict area and in neighboring countries, and development of transit dialysis options and facilitation of transportation to minimize delays in accessing therapy [20].
The main clinical challenges on presentation were hyperkaliemia, fluid overload and severe anemia which could mainly be attributed to longer intervals between dialysis sessions. Severe anemia and fluid overload were among the main reasons for hospitalization upon arrival in the host center. Low hemoglobin concentrations were likely associated with fluid overload and missed ESA administration or lack of its availability before migration.
The proportion of displaced patients treated with ESA, active vitamin D and phosphate binders was rather low compared with the average European dialysis population [21, 22]. Possible reasons for this may be that the dialysis refugees from Ukraine were younger than average dialysis patients in Europe, and therefore had fewer comorbidities. Given that all patients from Ukraine received full healthcare coverage by the host healthcare system, guaranteeing standard therapy, including for kidney failure and listing for kidney transplantation if appropriate, following the international clinical and ethics guidance [23], it is unlikely that these therapies were withheld from the migrant patients.
A key challenge to optimal treatment was the lack of complete medical records in most patients, with an absence of all documentation in almost one in five patients. These findings support the importance of developing strategies of preparedness in the dialysis community. Another major problem was the language barrier, underlining the need to identify ahead of time translation resources for languages spoken by an anticipated refugee patients [20]. Contrary to our finding of the importance of a language barrier, cultural rather than linguistic differences were identified as a barrier for optimal care in the prior international survey of the nephrology community on KRT for refugees [24]. Cultural diversity in that study was however greater than ours, and migrants had had the opportunity to live in the host country for a long time, and therefore language barriers may have diminished over time.
To the best of our knowledge, this is the first report describing the clinical characteristics, distribution, preparedness and management of adult Ukrainian refugees on dialysis and one of the few systematic analyses of displaced dialysis patients during an active conflict.
The study does however have some limitations. Not all centers invited to participate responded. In addition, clinical and laboratory characteristics of these patients were requested only from dialysis centers in Poland. Finally, 51.8% of patients were treated in the FMC centers and only aggregated data were obtainable due to internal privacy regulations. Despite these limitations, a major strength of this study is that it is one of few reports providing important information on migrant dialysis patients during conflicts and emergencies.
In summary, war always has a serious impact on the civilian population, especially those suffering from chronic diseases [25]. People with kidney disease are especially vulnerable given the complexity and technicality of kidney care [26]. Many European and other countries organized humanitarian aid for Ukraine. The ERA participated in this process after establishing the RDRTF. One of the many activities of this group [11] was conducting the present international survey. The results of this study will be helpful in understanding the scale of migration of dialysis patients outside Ukraine, their clinical characteristics, as well as medical and social needs, and may be relevant for patients in similar conflicts occurring elsewhere, and to support global recognition of this small but highly vulnerable group of patients. In addition, these data may be useful for Ukrainian nephrology community and authorities as they plan support for the patients who remained in Ukraine, who migrated within the country and for those migrants who intend to return to Ukraine [11, 12].
CONCLUSIONS
After the Russian invasion of Ukraine, a relatively small proportion of Ukrainian dialysis patients appears to have fled their country and the majority of them chose a country neighboring Ukraine as the place for dialysis.
Preparedness for displacement varied and was incomplete in most patients.
During their transfer almost 30% of the patients remained without dialysis for 4 days or longer. Clinical status upon arrival necessitated hospitalization in one in three patients.
Full reimbursement of treatment enabled the receiving centers to support patients conforming to standard of care, including waitlisting for transplantation, if appropriate.
Almost one-third of patients not continuing treatment in the host country intended to return to Ukraine; however, return of these patients should be only encouraged when safety and treatment possibilities are guaranteed in their native country.
Results from our survey may inform evidence-based policies and interventions to prepare for and respond to the special needs of vulnerable kidney failure populations during armed conflicts and other emergencies.
Supplementary Material
ACKNOWLEDGEMENTS
Members of the Renal Disaster Relief Task Force of the European Renal Association: Serhan Tuğlular—Chair; Kai-Uwe Eckardt; Daniel Gallego; Dimitri Ivanov; Anna Klis; Yelena Loboda; Valerie Luyckx; Edita Noruišiene; Ionut Nistor; Ewa Pawłowicz-Szlarska; Rukshana Shroff; Andrej Škoberne; Stefano Stuard; Mehmet Sukru Sever; Raymond Vanholder; and Andrzej Wiecek. The authors would like to express their deep gratitude to all dialysis centers employees for participating in the survey. European Kidney Health Alliance is the recipient of support by the European Union in the context of the Annual Work Program 2022 on prevention of non-communicable diseases of EU4Health, topic ID EU4H-2022-PJ02, project # 101101220 PREVENTCKD.
Contributor Information
Ewa Pawłowicz-Szlarska, Department of Nephrology, Hypertension and Kidney Transplantation, Medical University of Łódź, Łódź, Poland.
Raymond Vanholder, Nephrology Section, Department of Internal Medicine and Pediatrics, Ghent University Hospital, Ghent, Belgium; European Kidney Health Alliance, Brussels, Belgium.
Mehmet S Sever, Department of Nephrology, Istanbul School of Medicine, Istanbul University, Istanbul, Turkey.
Serhan Tuğlular, Department of Nephrology, School of Medicine, Marmara University, Istanbul, Turkey.
Valerie Luyckx, Renal Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA; Department of Paediatrics and Child Health, University of Cape Town, Cape Africa, South Africa; Department of Public and Global Health, Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Zurich, Switzerland.
Kai-Uwe Eckardt, Department of Nephrology and Medical Intensive Care, Charité-Universitätsmedizin Berlin, Berlin, Germany.
Daniel Gallego, European Kidney Health Alliance, Brussels, Belgium; European Kidney Patient Federation, Wien, Austria.
Dmytro Ivanov, Department of Nephrology and RRT, Bogomolets National Medical University, Kyiv, Ukraine.
Ionut Nistor, Department of Internal Medicine, Nephrology and Geriatrics, Grigore T. Popa University of Medicine and Pharmacy, Iasi, Romania; Department of Nephrology, Dr C. I. Parhon University Hospital, Iasi, Romania.
Rukshana Shroff, Renal Unit, UCL Great Ormond Street Hospital and Institute of Child Health, London, UK.
Andrej Škoberne, Department of Nephrology, Division of Internal Medicine, University Medical Centre Ljubljana, Ljubljana, Slovenia; Medical Faculty, University of Ljubljana, Ljubljana, Slovenia.
Stefano Stuard, Global Medical Office, Fresenius Medical Care, Bad Homburg, Germany.
Ryszard Gellert, Department of Nephrology and Internal Medicine, Centre for Postgraduate Medical Education, Warsaw, Poland.
Edita Noruišiene, European Kidney Health Alliance, Brussels, Belgium; European Dialysis and Transplant Nurses Association – European Renal Care Association, Hergiswil, Switzerland.
Mohamed Sekkarie, Nephrology and Hypertension Associates, Bluefield, WV, USA.
Andrzej Wiecek, Department of Nephrology, Transplantation and Internal Medicine, Medical University of Silesia, Katowice, Poland.
the Renal Disaster Relief Task Force of the ERA:
Serhan Tuglular, Kai-Uwe Eckardt, Daniel Gallego, Dimitri Ivanov, Anna Klis, Yelena Loboda, Valerie Luyckx, Edita Noruišiene, Ionut Nistor, Ewa Pawłowicz-Szlarska, Rukshana Shroff, Andrej Skoberne, Stefano Stuard, Mehmet Sukru Sever, Raymond Vanholder, and Andrzej Więcek
AUTHORS’ CONTRIBUTIONS
E.P.-S., R.V., M.S.S., S.T., V.L., K-U.E and A.W. were responsible for the study concept and design. E.P.-S., I.N., A.S., S.S., R.G., E.N. and A.W. were responsible for the acquisition of data. E.P.-S., R.V., M.S.S. and A.W. were responsible for the analysis and interpretation of data. E.P.-S. and A.W. were responsible for drafting of the manuscript. R.V., M.S.S., S.T., V.L., K-U.E., D.G., D.I., I.N., R.S., A.S., S.S., R.G., E.N. and M.S. provided critical revision of the manuscript for important intellectual content. All authors approved the final version of the manuscript.
FUNDING
No funds, grants, or other financial support was received for conducting this study.
DATA AVAILABILITY STATEMENT
The data underlying this article will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no competing interests. The results presented in this article have not been published previously in whole or part, except in abstract format.
REFERENCES
- 1. United Nations Regional Information Center for Western Europe official website. Available from: https://unric.org/en/the-un-and-the-war-in-ukraine-key-information/ (4 January 2023, date last accessed). [Google Scholar]
- 2. United Nations High Commissioner for Refugees official website. Available from: https://data.unhcr.org/en/situations/ukraine (24 September 2022, date last accessed). [Google Scholar]
- 3. UN Office for the Coordination of Humanitarian Affairs official website. Available from: https://reliefweb.int/report/ukraine/ukraine-internal-displacement-report-general-population-survey-round-3-17-april-2022 (15 December 2022, date last accessed). [Google Scholar]
- 4. Garry S, Checchi F. Armed conflict and public health: into the 21st century. J Public Health 2020;42:e287–98. 10.1093/pubmed/fdz095. [DOI] [PubMed] [Google Scholar]
- 5. Kutner NG, Muntner P, Huang Yet al. . Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int 2009;76:60–766. 10.1038/ki.2009.268. [DOI] [PubMed] [Google Scholar]
- 6. Sever MS, Erek E, Vanholder Ret al. . Features of chronic hemodialysis practice after the Marmara earthquake. J Am Soc Nephrol 2004;15:1071–6. 10.1097/01.ASN.0000119145.40232.67. [DOI] [PubMed] [Google Scholar]
- 7. Sever MS, Vanholder R, Luyckx Vet al. . Armed conflicts and kidney patients: a consensus statement from the Renal Disaster Relief Task Force of the ERA. Nephrol Dial Transplant 2022;38:56–65. 10.1093/ndt/gfac247. [DOI] [PubMed] [Google Scholar]
- 8. Kolesnyk M, Driianska V, Liksunova Let al. . State Institution ‘Institute of Nephrology of the National Academy of Medical Sciences of Ukraine’: 20 years afterward. Ukr J Nephr Dial 2021;4:3–9. [Google Scholar]
- 9. Council Implementing Decision (EU) 2022/382 of 4 March 2022 establishing the existence of a mass influx of displaced persons from Ukraine within the meaning of Article 5 of Directive 2001/55/EC, and having the effect of introducing temporary protection. Available from: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex:32022D0382 (26 February 2023, date last accessed). [Google Scholar]
- 10. Stepanova N, Kolesnyk M, Mithanib Zet al. . Lifesaving care for patients with kidney failure during the war in Ukraine. Clin J Am Soc Nephrol 2022;17:1079–81. 10.2215/CJN.04720422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tuglular S, Luyckx V, Vanholder Ret al. . Lessons learnt during the war in Ukraine: a report from the Renal Disaster Relief Task force of ERA. Nephrol Dial Transplant 2023;gfad053. 10.1093/ndt/gfad053. [DOI] [PubMed] [Google Scholar]
- 12. Novakivskyy V, Shurduk R, Grin Iet al. . War in Ukraine and dialysis treatment: human suffering and organizational challenges. Clin Kidney J 2023;16:676–83. 10.1093/ckj/sfad003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. ERA Registry: ERA Registry Annual Report 2020 . Amsterdam, The Netherlands: Amsterdam UMC, Location AMC, Department of Medical Informatics, 2022. [Google Scholar]
- 14. ERA Registry: ERA Registry Annual Report 2019 . Amsterdam, The Netherlands: Amsterdam UMC, Location AMC, Department of Medical Informatics, 2022. [Google Scholar]
- 15. Gursu M, Arici M, Ates Ket al. . Hemodialysis experience of a large group of Syrian refugees in Turkey: all patients deserve effective treatment. Kidney Blood Press Res 2019;44:43–51. 10.1159/000498832. [DOI] [PubMed] [Google Scholar]
- 16. Murakami N, Siktel HB, Lucido Det al. . Disaster preparedness and awareness of patients on hemodialysis after Hurricane Sandy. Clin J Am Soc Nephrol 2015;10:1389–96. 10.2215/CJN.10181014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kopp JB, Ball LK, Cohen Aet al. . Kidney patient care in disasters: emergency planning for patients and dialysis facilities. Clin J Am Soc Nephrol 2007;2:825–38. 10.2215/CJN.01220307. [DOI] [PubMed] [Google Scholar]
- 18. Dent L, Finne K, Lurie N. Progress in emergency preparedness for dialysis care 10 years after Hurricane Katrina. Am J Kidney Dis 2015;66:742–4. 10.1053/j.ajkd.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 19. Morsch G, Chacko S, Randolph R. Disaster medicine: disaster preparedness planning. FP Essent 2019;487:23–6. [PubMed] [Google Scholar]
- 20. Van Biesen W, Vanholder R, Ernandez Tet al. . Caring for migrants and refugees with end-stage kidney disease in Europe. Am J Kidney Dis 2018;71:701–9. [DOI] [PubMed] [Google Scholar]
- 21. Fuller DS, Robinson BM, Locatelli Fet al. . Patterns of erythropoiesis-stimulating agent use in European hemodialysis patients: the Dialysis Outcomes and Practice Patterns study. Nephron 2018;140:24–30. 10.1159/000490202. [DOI] [PubMed] [Google Scholar]
- 22. Fernández-Martín JL, Carrero JJ, Benedik Met al. . COSMOS: the dialysis scenario of CKD-MBD in Europe. Nephrol Dial Transplant 2013;28:1922–35. 10.1093/ndt/gfs418. [DOI] [PubMed] [Google Scholar]
- 23. Martin DE, Fadhil RAS, Więcek A. Ethical aspects of kidney donation and transplantation for migrants. Semin Nephrol 2022;42:151271. 10.1016/j.semnephrol.2022.07.005. [DOI] [PubMed] [Google Scholar]
- 24. Van Biesen W, Vanholder R, Vanderhaegen Bet al. . Renal replacement therapy for refugees with end-stage kidney disease: an international survey of the nephrological community. Kidney Int Suppl 2016;6:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vanholder R, Gallego D, Sever MS. Wars and kidney patients: a statement by the European Kidney Health Alliance related to the Russian-Ukrainian conflict. J Nephrol 2022;35:377–80. 10.1007/s40620-022-01301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vanholder R, De Weggheleire A, Ivanov Det al. . Continuing kidney care in conflicts. Nat Rev Nephrol 2022;18:479–80. 10.1038/s41581-022-00588-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.