Abstract
Background
Many high-dose groups demonstrate increased leukaemia risks, with risk greatest following childhood exposure; risks at low/moderate doses are less clear.
Methods
We conducted a pooled analysis of the major radiation-associated leukaemias (acute myeloid leukaemia (AML) with/without the inclusion of myelodysplastic syndrome (MDS), chronic myeloid leukaemia (CML), acute lymphoblastic leukaemia (ALL)) in ten childhood-exposed groups, including Japanese atomic bomb survivors, four therapeutically irradiated and five diagnostically exposed cohorts, a mixture of incidence and mortality data. Relative/absolute risk Poisson regression models were fitted.
Results
Of 365 cases/deaths of leukaemias excluding chronic lymphocytic leukaemia, there were 272 AML/CML/ALL among 310,905 persons (7,641,362 person-years), with mean active bone marrow (ABM) dose of 0.11 Gy (range 0–5.95). We estimated significant (P < 0.005) linear excess relative risks/Gy (ERR/Gy) for: AML (n = 140) = 1.48 (95% CI 0.59–2.85), CML (n = 61) = 1.77 (95% CI 0.38–4.50), and ALL (n = 71) = 6.65 (95% CI 2.79–14.83). There is upward curvature in the dose response for ALL and AML over the full dose range, although at lower doses (<0.5 Gy) curvature for ALL is downwards.
Discussion
We found increased ERR/Gy for all major types of radiation-associated leukaemia after childhood exposure to ABM doses that were predominantly (for 99%) <1 Gy, and consistent with our prior analysis focusing on <100 mGy.
Subject terms: Acute lymphocytic leukaemia, Acute myeloid leukaemia, Chronic myeloid leukaemia
Introduction
Leukaemia is the malignancy most strongly associated with ionising radiation exposure, with increased risks observed at moderate-to-high doses for myeloid subtypes and to a lesser extent for acute lymphoblastic leukaemia (ALL) [1]. Radiation-associated risks are highest for leukaemia following exposures in childhood and begin to increase earlier after exposure than other cancers [1, 2]. In contrast, most major types of lymphoma, including chronic lymphocytic leukaemia (CLL), essentially the same disease as small lymphocytic lymphoma (SLL) [3], are at best weakly associated with radiation exposure [1, 4].
The rarity of leukaemia, and small numbers of subtypes in any single cohort, has precluded quantification of stable estimates in the low-to-moderate dose range (e.g., <0.5 Gy). In a recent pooled analysis of nine cohorts of children and adolescents aged less than 21 years at exposure, we reported significantly elevated dose–response trends for acute myeloid leukaemia (AML), AML plus myelodysplastic syndrome (MDS), and ALL at mean cumulative low doses (<100 mGy) to active bone marrow (ABM), with little evidence of inter-cohort heterogeneity or departure from linearity [5].
Data from the nine cohorts we previously studied [5], plus one additional cohort [6, 7], provide an opportunity to extend the assessment of dose response and provide risk estimates for low-to-moderate radiation exposures that are more precise than those derived from individual studies. The current analysis focused on the shape of the radiation dose–response curve, which the previous analysis with doses <100 mGy did not have power to do [5], and the effects of age at, and time since, exposure, while taking into account any evidence of inter-cohort heterogeneity. As before, we have focused on risks of the major types of radiation-associated leukaemia (therefore excluding CLL/SLL). We previously analysed risks of CLL/SLL, lymphoma and multiple myeloma in a subset of nine of these cohorts using the entire dose range [8].
Materials and methods
Cohort definition, incidence/mortality ascertainment
We examined all available cohort studies, with five or more leukaemias or myeloid malignancies receiving whole-body-averaged cumulative radiation doses to the ABM > 0.005 Gy while under the age of 21 years. We excluded any studies of patients being treated for malignant disease, in which chemotherapy is potentially a strong confounder, and also any studies of non-malignant disease that involved chemotherapy. We required that the cohorts had whole-body-averaged cumulative ABM dose estimates for each individual, and we reviewed the quality and completeness of the dosimetry. We identified eligible cohorts from the most recent comprehensive summaries by international committees [1, 2, 9] combined with literature reviews [10, 11] and PubMed literature searches done on May 29, 2018 to identify cohort studies published before June 30, 2014. Ten cohorts met the eligibility criteria, including nine [12–21] that were included in our previous publication [5] plus the patients who underwent radiotherapy in Israel for treatment of tinea capitis [6, 7]. Details of the 10 cohorts can be found in Appendix A (Table A1). A number of eligible cohort studies have appeared since the above literature searches were conducted, most of them studies of leukaemia in relation to computed tomography (CT) exposure [22–26].
Cohorts excluded were those in which subjects mostly received radiation exposures from internally deposited radionuclides, dosimetry was inadequately described, and those with very small numbers of leukaemia or myeloid malignancies. Studies that employed a case–control design were also excluded, because of difficulty in combining risks with those from cohorts (see Appendix A for more detail about exclusions). Apart from the Japanese atomic bomb survivors’ Life Span Study (LSS) [17], the datasets comprise medically exposed groups: five for therapeutic reasons (three haemangioma cohorts [13–16], Israeli tinea capitis [6, 7] and Rochester enlarged thymus [18, 19]), and four for diagnostic reasons (two tuberculosis [TB] monitored cohorts [12, 27], US patients monitored for scoliosis [20] and the United Kingdom–National Cancer Institute paediatric computed tomography (UK-NCI CT) cohort [21]). Follow-up started generally at the beginning or the end of the initial period of radiation exposure for most medically irradiated groups, and continued until the earliest of date of leukaemia diagnosis, date of death, loss to follow-up or the end of the study (which varies by cohort (Appendix B Table B1, Fig. B1)). Follow-up of cohorts began at the date of admission to one of the participating treatment institutions [12], the date of establishment of the relevant mortality registers [18–20, 27] or national cancer registries [14–16], or the Japanese national census establishing the LSS cohort [17]. Further details about subject identification and on follow-up in the individual cohorts are given in Appendix A Table A1.
Radiation dosimetry
Whole-body-averaged cumulative ABM doses were calculated for each subject in the cohorts according to methods described previously [5] and summarised in Appendix A. For many of the cohorts, this was the only available measure of dose—in particular, compartmental ABM doses were unavailable, which is especially pertinent for the heterogeneous exposures experienced in the therapeutic cohorts. ABM doses were expressed as absorbed doses (in gray, Gy) with each radiation component weighted by relative biological effectiveness (RBE) values, which for sparsely ionising radiations (e.g., X-rays) are equal to unweighted absorbed doses, but for the LSS cohort take account of the (generally small) neutron component of exposure by weighting by a factor of 10. No other adjustment for RBE was made, for example, in relation to the lower energy X-rays used in diagnostic exposures. Overall, the pooled analysis generally used the most recently calculated set of doses described in these studies, although for the Israeli tinea capitis data, modifications were applied to derive whole-body-averaged ABM doses from the skull ABM doses that were used until recently [7].
Outcome classification
The methods/sources of case identification were study specific. These include (I) tumour/cancer registries [6, 14–16, 28]; (II) medically validated self-reported information [13]; and (III) national vital statistics registries [12, 18–20, 27]. Further details of disease ascertainment and follow-up methods for each cohort are given in Appendix A. As these studies span several decades and include incidence and mortality data, we carefully reviewed the lympho-haematopoietic malignancy outcome data and developed International Classification of Diseases (ICD) and International Classification of Diseases for Oncology (ICD-O) coding to harmonise outcomes across studies and over calendar time (exposure and follow-up periods spanned 1916–2016 (Appendix B Table B1)), as described in Appendix A. We defined the following outcomes of interest, the main strongly radiation-associated leukaemia outcomes [1], specifically:
acute myeloid leukaemia (AML);
AML and myelodysplastic syndrome (MDS);
chronic myeloid leukaemia (CML);
acute lymphoblastic leukaemia (ALL);
acute leukaemia;
all myeloid malignant neoplasms (including AML, CML, other myeloproliferative cancers and MDS);
leukaemia excluding CLL, unclassified as AML/CML/ALL;
leukaemia excluding CLL.
Deaths were coded to the ICD revisions 6 through 10, and incident outcomes were generally coded to the ICD-O revisions 2 or 3 (see Appendix A Tables A3 and A4 for detailed ICD/ICD-O coding) [29]. CLL was excluded because it is now classified as a form of non-Hodgkin lymphoma (SLL), and there is little evidence that it is radiation-associated [1, 4, 8]. There were 18 cases of myelodysplastic syndrome (MDS). These were too few to reliably analyse by themselves, so analyses were conducted in which these cases were combined (or not) with AML.
Covariates
A unified set of covariates was employed, which could be considered as either confounders or effect modifiers, specifically sex, age at entry, age first exposed, age last exposed, age attained, year of birth, years since first exposure, years since last exposure, lagged mean ABM dose accumulated in moving windows by time since exposure and age at exposure.
Statistical analysis
We estimated the excess relative risk (ERR) per Gy of mean cumulative ABM dose (ERR/Gy) and excess absolute risk (EAR) per person-year Gy (PY Gy) for each outcome for pre-defined dose categories (see Appendix A Table A5 for the categories we evaluated) using the unexposed group (0 Gy) as the reference category; EAR was assessed by fitting generalised additive models (GAM) [30]. We also assessed the fit of a continuous dose–response model, and in order to assess possible non-linearity in dose-effect, compared the fit of linear and linear-exponential (and occasionally linear-quadratic) models. We also assessed whether the ERR varied with time since exposure or age at exposure. All models were stratified by cohort, sex, attained age and calendar time. Additional sensitivity analysis was conducted for the LSS stratifying by city (Hiroshima/Nagasaki), and also stratifying by city and membership of the Adult Health Study (AHS) within the LSS (since members of the AHS would have undergone active surveillance for cancer and cancer precursor outcomes), but as these made little difference they are not reported further. Additional statistical details are given in Appendix C. The models were fitted by Poisson maximum likelihood [31] using Epicure [32]. Confidence intervals (CI) were derived from the profile likelihood [31]; when this did not converge, Wald-based CI were employed [33]. In general, all confidence intervals are 95% (type I error = 0.05), and a two-sided P value of P = 0.05 is deemed statistically significant. No adjustment was made for multiple comparisons.
In the five therapeutic cohorts, doses would be expected to be particularly high in some ABM compartments, and would generally have been given over a fairly short timescale. These localised high doses are much higher than in the LSS or in any of the four diagnostically exposed groups; the distribution of dose is most homogeneous in the LSS. For this reason, and because of the generally lower ages at exposure in the therapeutic groups, for certain analyses, we analysed the therapeutically exposed, diagnostically exposed and LSS separately. We assessed adequacy of the assumed Poissonian distribution of the data by fitting quasi-likelihood models [31] using R [34].
No blinding was performed, but all outcomes were determined independently of exposure status.
We estimated the power of a one-sided test of trend (with type I error rate (=α) of 5%) using the methodology described in the paper of Little et al. [35]. Statistical power was 100% for AML, and 99% for ALL. Power was about 86% for CML. If the assumed risk coefficient were to be halved in all datasets apart from the LSS little changed, in particular for the three endpoints with power >80% (AML, ALL, CML) the same held. If the LSS data were excluded and risk coefficients were halved power for AML fell to 49%, for ALL fell to 50%, and for CML fell to 26%.
Results
Table 1 demonstrates that in the pooled analysis of ten cohorts there was a total of 310,905 persons accumulating 7,641,362 person-years of follow-up; this represents an additional 48,332 persons and 2,486,898 person-years compared to our earlier pooled analyses of low-dose exposures, which used only nine of the present cohorts [5]. Of the pooled cohort, 154,647 (49.7%) were male, 156,036 (50.2%) were female, with a small number (222, 0.1%, all in the UK-NCI CT cohort) of unknown sex. The mean individual whole-body-averaged cumulative ABM dose was 0.11 Gy, although there was considerable spread of individual cumulative doses (range, 0–5.95 Gy); the highest mean dose was observed in the Israeli tinea capitis cohort, 0.29 Gy, and the lowest mean dose was in the US scoliosis cohort, 0.008 Gy (Appendix A Table A2, Appendix B Table B1). Among the exposed (those with doses >0 Gy), the mean age at first exposure was 8.0 years, and the mean years since last exposure was 22.4 years (Appendix B Table B1). There was a total of 272 leukaemia cases/deaths of types that are associated with radiation exposure, of which 140 were AML, 61 CML and 71 ALL (Table 1). There was a total of 365 leukaemias excluding CLL, the additional 93 cases/deaths being due to leukaemias that could not be assigned a major specified category; we consider this rather heterogeneous group of leukaemias excluding CLL, unclassified as AML/CML/ALL, only briefly. There was some evidence of overdispersion for all endpoints, with variance approximately twice that predicted by a Poisson model.
Table 1.
Numbers of persons, person-years of follow-up and cases/deaths for key leukaemia categories.
| Class | Category | Person-years | Persons first at riska | Myeloid malignant neoplasms | AML | AML + MDS | CML | ALL | Acute leukaemia | Leukaemia excluding CLL, unclassified as AML/CML/ALL | Leukaemia excluding CLL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 7,641,362 | 310,905 | 274 | 140 | 158 | 61 | 71 | 243 | 93 | 365 | |
| Sex | Male | 3,332,630 | 154,647 | 146 | 73 | 83 | 34 | 36 | 123 | 53 | 196 |
| Female | 4,306,530 | 156,036 | 128 | 67 | 75 | 27 | 34 | 119 | 40 | 168 | |
| Unknown | 2204 | 222 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | |
| Entry year | <1920 | 56 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1920–1929 | 37,505 | 576 | 2 | 1 | 1 | 1 | 0 | 3 | 2 | 4 | |
| 1930–1939 | 170,704 | 4115 | 11 | 1 | 1 | 3 | 0 | 1 | 10 | 14 | |
| 1940–1949 | 170,857 | 4638 | 3 | 0 | 0 | 2 | 1 | 2 | 12 | 15 | |
| 1950–1959 | 5,077,780 | 118,126 | 205 | 117 | 124 | 47 | 43 | 184 | 55 | 262 | |
| 1960–1969 | 300,211 | 6372 | 4 | 2 | 3 | 1 | 0 | 2 | 4 | 7 | |
| 1970–1979 | 263,511 | 9307 | 5 | 2 | 4 | 0 | 1 | 7 | 6 | 9 | |
| 1980–1989 | 50,382 | 2701 | 1 | 1 | 1 | 0 | 2 | 3 | 0 | 3 | |
| 1990–1999 | 1,056,900 | 84,058 | 32 | 10 | 17 | 6 | 16 | 26 | 2 | 34 | |
| ≥2000 | 513,463 | 81,010 | 11 | 6 | 7 | 1 | 8 | 15 | 2 | 17 | |
| Age at entry (years)a | 0–4 | 1,427,710 | 56,366 | 34 | 17 | 23 | 6 | 17 | 42 | 12 | 52 |
| 5–9 | 1,905,370 | 60,555 | 64 | 34 | 38 | 11 | 25 | 63 | 14 | 84 | |
| 10–14 | 1,519,830 | 58,714 | 58 | 28 | 33 | 17 | 9 | 45 | 14 | 68 | |
| 15–19 | 1,177,090 | 62,903 | 52 | 29 | 30 | 12 | 5 | 36 | 10 | 56 | |
| 20–29 | 1,343,570 | 61,245 | 51 | 29 | 30 | 12 | 14 | 49 | 19 | 74 | |
| 30–39 | 191,916 | 6497 | 5 | 2 | 2 | 1 | 1 | 6 | 10 | 14 | |
| 40–49 | 51,260 | 2357 | 6 | 1 | 2 | 1 | 0 | 2 | 8 | 10 | |
| ≥50 | 24,614 | 2268 | 4 | 0 | 0 | 1 | 0 | 0 | 6 | 7 | |
| Years since first exposurea | <0 or NA | 1,667,610 | 50,335 | 68 | 27 | 31 | 16 | 10 | 44 | 41 | 94 |
| 0–0.99 | 23,335 | 19,912 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | |
| 1–1.99 | 25,243 | 2208 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 2–4.99 | 568,364 | 167,316 | 10 | 5 | 7 | 2 | 10 | 19 | 6 | 23 | |
| 5–9.99 | 1,052,290 | 56,331 | 29 | 14 | 15 | 8 | 19 | 36 | 5 | 46 | |
| 10–14.99 | 745,666 | 7630 | 24 | 9 | 13 | 4 | 9 | 21 | 7 | 29 | |
| 15–19.99 | 529,238 | 2890 | 14 | 9 | 10 | 3 | 5 | 15 | 3 | 20 | |
| 20–29.99 | 865,351 | 2537 | 21 | 12 | 12 | 8 | 6 | 23 | 6 | 32 | |
| ≥30 | 2,164,270 | 1746 | 107 | 63 | 69 | 20 | 12 | 84 | 25 | 120 | |
| Attained age (years)a | 0–4.99 | 124,753 | 56,366 | 1 | 1 | 1 | 0 | 4 | 6 | 1 | 6 |
| 5–9.99 | 411,538 | 60,555 | 5 | 4 | 5 | 0 | 13 | 20 | 5 | 22 | |
| 10–14.99 | 623,591 | 58,714 | 12 | 5 | 6 | 5 | 11 | 18 | 2 | 23 | |
| 15–19.99 | 778,480 | 62,903 | 23 | 10 | 12 | 5 | 5 | 20 | 7 | 27 | |
| 20–29.99 | 1,731,430 | 61,245 | 36 | 19 | 23 | 9 | 12 | 39 | 12 | 52 | |
| 30–39.99 | 1,281,480 | 6497 | 28 | 14 | 14 | 9 | 6 | 20 | 7 | 36 | |
| 40–49.99 | 1,152,100 | 2357 | 42 | 21 | 22 | 12 | 6 | 33 | 12 | 51 | |
| ≥50 | 1,537,990 | 2268 | 127 | 66 | 75 | 21 | 14 | 87 | 47 | 148 | |
| Mean cumulative active bone marrow dose (Gy) | 0 | 2,832,010 | 93,729 | 106 | 51 | 55 | 26 | 13 | 76 | 53 | 143 |
| 0–0.004 | 964,831 | 65,125 | 24 | 10 | 10 | 6 | 1 | 14 | 5 | 22 | |
| 0.005–0.099 | 628,876 | 50,911 | 14 | 5 | 7 | 5 | 6 | 13 | 5 | 21 | |
| 0.010–0.019 | 669,905 | 48,357 | 11 | 6 | 8 | 1 | 15 | 22 | 3 | 25 | |
| 0.020–0.049 | 534,468 | 21,414 | 24 | 15 | 19 | 3 | 8 | 24 | 3 | 29 | |
| 0.050–0.099 | 425,622 | 10,015 | 16 | 12 | 12 | 2 | 4 | 19 | 4 | 22 | |
| 0.100–0.149 | 244,034 | 4946 | 12 | 5 | 5 | 3 | 2 | 9 | 5 | 15 | |
| 0.150–0.199 | 127,858 | 2761 | 9 | 6 | 8 | 0 | 1 | 8 | 2 | 9 | |
| 0.200–0.299 | 191,887 | 3918 | 3 | 0 | 0 | 3 | 1 | 2 | 2 | 6 | |
| 0.300–0.499 | 347,124 | 4788 | 9 | 3 | 4 | 2 | 4 | 7 | 2 | 11 | |
| 0.500–0.749 | 365,219 | 2206 | 16 | 8 | 10 | 3 | 5 | 14 | 3 | 19 | |
| 0.750–0.999 | 186,260 | 1211 | 8 | 4 | 4 | 2 | 2 | 10 | 4 | 12 | |
| 1.000–1.499 | 74,472 | 754 | 6 | 5 | 5 | 1 | 3 | 9 | 1 | 10 | |
| 1.500–1.999 | 29,564 | 326 | 8 | 6 | 7 | 0 | 0 | 6 | 1 | 7 | |
| 2.000–2.499 | 8232 | 178 | 4 | 2 | 2 | 2 | 0 | 2 | 0 | 4 | |
| 2.500–2.999 | 5708 | 158 | 2 | 1 | 1 | 1 | 4 | 5 | 0 | 6 | |
| 3.000–4.999 | 5241 | 107 | 2 | 1 | 1 | 1 | 2 | 3 | 0 | 4 | |
| 5.000–7.499 | 53 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
AML acute myeloid leukaemia, CML chronic myeloid leukaemia, ALL acute lymphoblastic leukaemia.
aThe number of persons represents those first entering follow-up in the given categories (of attained age, time since first exposure etc.).
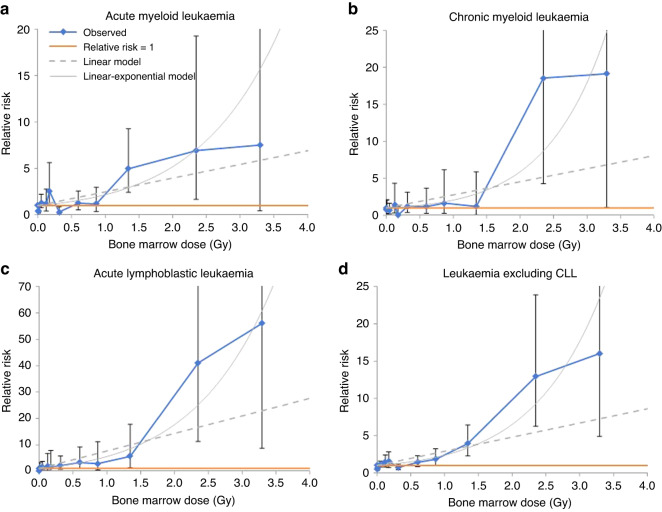
We estimated raised linear ERR/Gy for: AML, 1.48 (95% CI 0.59–2.85, P-trend < 0.0001); CML, 1.77 (95% CI 0.38–4.50, P-trend = 0.0029); ALL, 6.65 (95% CI 2.79–14.83, P-trend < 0.0001) (Table 2). The dose–response trends are shown graphically in Fig. 1 and in Appendix B Fig. B2. There was no discernible global inter-cohort heterogeneity in ERR/Gy for these three endpoints (Table 2), although there were some indications of heterogeneity when contrasting each particular cohort against all other cohorts, in particular, in comparing the LSS against the combined nine medically exposed cohorts (Appendix B Table B2).
Table 2.
Excess relative risk and excess absolute risk models with ERR/Gy and EAR/Gy estimates (and 95% CI).
| Excess relative risk models | ||||
|---|---|---|---|---|
| Endpoint | ERR /Gy ( + 95% CI)a | Cases/deaths | P valuea | P value for inter-cohort heterogeneity |
| Acute myeloid leukaemia | 1.48 (0.59, 2.85) | 140 | <0.0001 | 0.1437 |
| Chronic myeloid leukaemia | 1.77 (0.38, 4.50) | 61 | 0.0029 | 0.9072 |
| Acute lymphoblastic leukaemia | 6.65 (2.79, 14.83) | 71 | <0.0001 | 0.9171 |
| Excess absolute risk models | ||||
| Endpoint | EAR/104 PY.Gy ( + 95% CI)a | Cases/deaths | P valuea | P value for inter-cohort heterogeneity |
| Acute myeloid leukaemiab | 0.215c (0.090, 0.373) | 140 | 0.0002c | 0.0017c |
| Chronic myeloid leukaemiad | 0.125c (0.043, 0.238) | 61 | 0.0008c | 0.8090c |
| Acute lymphoblastic leukaemiae | 0.242c (0.128, 0.384) | 71 | <0.0001c | 0.2315c |
aAll P values and confidence intervals are based on the profile likelihood.
bBaseline model adjusted for cohort, sex, with continuous terms for ln[age], ln[age]2, ln[age]3, [calendar year of follow-up], [calendar year of follow-up]2.
cIndications of non-convergence.
dBaseline model adjusted for cohort, sex, with continuous terms for ln[age], [calendar year of follow-up], [calendar year of follow-up]2, [calendar year of follow-up]3, [calendar year of follow-up]4, [calendar year of follow-up]5, [calendar year of follow-up]6.
eBaseline model adjusted for cohort, sex, with continuous terms for ln[age], [calendar year of follow-up], [calendar year of follow-up]2.
A linear relative risk model is based on a semi-parametric background module stratified by cohort, sex, age and year of follow-up (using intervals of age and year of follow-up defined by person-year table, as in Appendix A Table A1). All confidence intervals are based on the profile likelihood.
Fig. 1. Relative risk (and 95% CI) by mean whole-body-averaged cumulative active bone marrow dose by leukaemia subtype.
a Acute myeloid leukaemia (AML), b chronic myeloid leukaemia (CML), c acute lymphoblastic leukaemia (ALL) and d leukaemia excluding CLL. Solid red line gives relative risk = 1, dashed grey line the fitted linear relative risk model, with ERR/Gy taken from Table 2 and Appendix B Table B2, solid grey line the linear-exponential model, taken from Table 3 and Appendix B Table B4. Dose boundaries used for categories are 0, 0.005, 0.02, 0.10, 0.15, 0.20, 0.50, 0.75, 1.00, 2.00, 3.00 Gy.
Table 3 and Appendix B Table B3 present ERR/Gy estimates for broader disease groupings and restricted cumulative ABM dose ranges and shows that all the groupings have significantly raised linear ERR/Gy estimates for the unrestricted dose range. For AML, AML + MDS, ALL, acute leukaemia and myeloid malignant neoplasms, reduction of the dose range to ≤1 Gy or ≤500 mGy results in decrease of ERR/Gy, in many cases with loss of significance (P > 0.05), but further reduction of the dose range resulted in an increase in ERR/Gy, which in all cases became again statistically significant (P < 0.05) for dose ≤200 mGy. However, for CML the reverse trend is apparent, with ERR/Gy tending to decrease as the dose range is restricted and becoming negative for doses ≤200 mGy, although the negative ERR/Gy are not statistically significant.
Table 3.
Dose response (linear ERR/Gy estimates) for selected leukaemia endpoints in relation to dose range used for fitting.
| Dose range | ERR/Gy ( + 95% CI) | Cases/deaths | P value | ERR/Gy ( + 95% CI) | Cases/deaths | P value |
|---|---|---|---|---|---|---|
| Acute myeloid leukaemia +myelodysplastic syndrome | Acute myeloid leukaemia | |||||
| Unrestricted | 1.430 (0.586, 2.725) | 158 | <0.0001 | 1.475 (0.591, 2.847) | 140 | <0.0001 |
| ≤1 Gy | −0.015 (−0.677, 1.103) | 142 | 0.9748 | −0.033 (−0.706, 1.139) | 125 | 0.9436 |
| ≤500 mGy | −0.566 (−1.943, 2.295) | 128 | 0.6143 | −1.440 (−2.580, 0.794) | 113 | 0.1590 |
| ≤300 mGy | 5.049 (−0.887, 15.62) | 124 | 0.1134 | 2.125 (−2.582, 10.76) | 110 | 0.4591 |
| ≤200 mGy | 15.40 (4.949, 33.04) | 124 | 0.0005 | 10.43 (1.845, 25.13) | 110 | 0.0100 |
| ≤100 mGy | 20.91 (4.080, 49.21) | 111 | 0.0081 | 15.56 (0.921, 40.61) | 99 | 0.0333 |
| Chronic myeloid leukaemia | Acute lymphoblastic leukaemia | |||||
| Unrestricted | 1.769 (0.384, 4.504) | 61 | 0.0029 | 6.654 (2.792, 14.83) | 71 | <0.0001 |
| ≤1 Gy | 0.346 (−0.776, 2.889) | 56 | 0.6596 | 2.934 (0.209, 9.310) | 62 | 0.0270 |
| ≤500 mGy | 0.074 (−3.156, 5.149) | 51 | 0.9643 | 4.219 (−0.600, 16.52) | 55 | 0.1141 |
| ≤300 mGy | 0.945 (−2.864, 10.30) | 49 | 0.7368 | 11.70 (−1.385, 51.91) | 51 | 0.1075 |
| ≤200 mGy | −3.614 (−8.839a, 6.602) | 46 | 0.3666 | 22.99 (1.027, 89.71) | 50 | 0.0330 |
| ≤100 mGy | −6.422 (−17.98a, 13.57) | 43 | 0.3939 | 46.60 (3.526, >100) | 47 | 0.0227 |
aWald-based CI.
Table 4 and Appendix B Table B4 show the results of fitting linear-exponential models and reinforces these findings of apparent departures from linearity, suggesting that there are weak indications of upwards curvature in the dose–response over the full dose range for AML (P = 0.06), AML + MDS (P = 0.06) and CML (P = 0.05), with rather more pronounced upward curvature for ALL (P = 0.0298), myeloid neoplasms (P = 0.0068), acute leukaemia (P = 0.0020) and myeloid neoplasms+ALL (P = 0.0002). However, if the dose range is restricted to ≤1 Gy or ≤500 mGy the curvature reverses direction for ALL, myeloid neoplasms and myeloid neoplasms+ALL, markedly so for ALL and myeloid neoplasms+ALL, with some indications of statistical significance, particularly for ≤500 mGy (P < 0.05). Appendix B Table B5 suggests that fitting slightly more complex models with separate linear terms for certain high-power subcohorts (LSS, Israeli tinea capitis, UK-NCI CT) does not much change this picture. If we consider dose–response curvature among the group of LSS plus the four diagnostically exposed cohorts at least for ALL there remains some evidence of upward curvature (P = 0.0949) (Appendix B Table B6 and Fig. B3). There are some indications of upward curvature for AML + MDS (P = 0.0794), or AML (P = 0.0992), and downward curvature for CML (P = 0.0966) for the combined five therapeutic cohorts (Appendix B Table B7 and Fig. B3). If a linear-quadratic model is fitted there are stronger indications of departures from linearity for AML (P = 0.0136), with a significant quadratic coefficient and non-significant linear coefficient (results not shown).
Table 4.
Curvature in dose response for selected leukaemia endpoints in relation to dose range used for fitting.
| Dose range | Cases/deaths | Linear ERR/Gy ( + 95% CI) | Exponential ERR/Gy ( + 95% CI) | P valuea | Cases/deaths | Linear ERR/Gy ( + 95% CI) | Exponential ERR/Gy ( + 95% CI) | P valuea |
|---|---|---|---|---|---|---|---|---|
| Acute myeloid leukaemia +myelodysplastic syndrome | Acute myeloid leukaemia | |||||||
| Unrestricted | 158 | 0.614 (0.139, 1.883) | 0.593 (−0.026, 1.127) | 0.0592 | 140 | 0.651 (0.147, 1.972) | 0.584 (−0.026, 1.113) | 0.0594 |
| ≤1 Gy | 142 | −0.006b (−1.508c, 1.495c) | 1.094b (<−100c, >100c) | 0.8963b | 125 | −0.007b (−1.102c, 1.089c) | 1.805b (<−100c, >100c) | 0.9244b |
| ≤500 mGy | 128 | −0.079b (−2.737c, 2.579c) | 3.855b (−75.37c, 83.08c) | 0.4527b | 113 | −0.778b (−4.736c, 3.179c) | 1.461b (−10.49c, 13.41c) | 0.2794b |
| Chronic myeloid leukaemia | Acute lymphoblastic leukaemia | |||||||
| Unrestricted | 61 | 0.459 (0.022, 2.626) | 0.837 (−0.013, 1.745) | 0.0532 | 71 | 2.488 (0.501, 8.583) | 0.604 (0.064, 1.126) | 0.0298 |
| ≤1 Gy | 56 | 0.183 (−2.926c, 3.292c) | 0.924 (−20.15c, 21.99c) | 0.9092 | 62 | 19.82 (0.713, 98.95) | −3.238 (−13.99, 1.377) | 0.1321 |
| ≤500 mGy | 51 | 0.129b (−14.68c, 14.94c) | −1.799b (<−100c, >100c) | 0.9643b | 55 | 71.62 (4.984, >100) | −8.935 (−42.56, −0.963) | 0.0350 |
aP value of improvement in fit of linear-exponential vs linear model.
bIndications of non-convergence.
cWald-based CI.
A linear-exponential model is used to assess departures from linearity. All CI are profile-likelihood based unless otherwise stated.
Table 2 also shows the results of fitting GAMs to ascertain EARs by endpoint. In general, EARs were in the range 0.13–0.24 per 104 PY Gy. In contrast to the ERR estimates, there was statistically significant (P < 0.002) inter-cohort heterogeneity in EAR for AML, but not for CML and ALL (P > 0.2). However, problems with convergence complicate interpretation of these findings (Table 2).
For some endpoints, ERR/Gy in the LSS, US scoliosis and UK-NCI-CT cohorts tended to be higher than those in other cohorts, whereas risks were highest for all three endpoints when the Israeli tinea capitis cohort was omitted from the analysis (see Appendix B Table B2). The only cohorts with generally good power (>75%) were the LSS and Israeli tinea capitis cohorts for AML/ALL and also the Stockholm haemangioma cohort for AML, although the LSS and Israeli tinea capitis cohorts for CML and also the Canadian TB cohort for ALL had moderate power (Appendix B Table B8).
Table 5 demonstrates that the highly significant discrepancy between the higher ERR/Gy estimates in the LSS compared to the combined other nine cohorts (Appendix B Table B2) was largely due to the five therapeutically irradiated groups, mainly driven by the generally low ERR/Gy values for the Israeli tinea capitis cohort. By comparison, Table 5 shows that while the risks in the combined four diagnostically exposed cohorts (Massachusetts + Canadian TB, US Scoliosis, UK-NCI CT) were lower than those in the LSS, the differences were only statistically significant for ALL (P = 0.0237). There is little evidence of heterogeneity for any endpoint within the therapeutic and diagnostic studies considered separately (Appendix B Table B9). It is notable that incidence risks are generally statistically significant, in contrast to the generally non-significant risks in the mortality data (Appendix B Table B10). However, there are few indications of significant differences between the risks in incidence and mortality data (Appendix B Table B10).
Table 5.
Assessment of heterogeneity in excess relative risk per Gy (and 95% CI) obtained by fitting linear relative risk model, allowing for separate risk for diagnostically exposed cohorts, therapeutically exposed cohorts, and Japanese atomic bomb survivor Life Span Study (LSS)a.
| Endpoint | Diagnostically exposed datasets | Therapeutically exposed datasets | LSS | P value for heterogeneity between 3 groups/P value for heterogeneity between diagnostically exposed and LSS/P value for heterogeneity between therapeutically exposed and LSS/P value for heterogeneity between diagnostically exposed and therapeutically exposed | |||
|---|---|---|---|---|---|---|---|
| ERR/Gy (95% CI) | Cases/deaths | ERR/Gy (95% CI) | Cases/deaths | ERR/Gy (95% CI) | Cases | ||
| Acute myeloid leukaemia (AML) | −0.387 (−1.999b, 12.44) | 28 | 0.348 (−0.611b, 1.444) | 58 | 4.318 (1.812, 8.892) | 54 | 0.0059/0.1947/0.0021/0.5740 |
| Chronic myeloid leukaemia (CML) | 1.767 (−5.930b, 16.28) | 20 | −0.133c (−1.254b, 0.723) | 19 | 7.966 (2.568, 22.00) | 22 | 0.0008c/0.3053/0.0002c/0.5328 |
| Acute lymphoblastic leukaemia (ALL) | −0.386 (−3.920b, 20.57) | 31 | −0.168 (−0.503b, 1.994) | 18 | 43.92 (12.81, >100) | 22 | <0.0001/0.0237/ < 0.0001/0.8376 |
| Leukaemia excluding CLL, unclassified as AML/CML/ALL | −0.376 (−2.159b, 1.974) | 52 | 0.376 (−1.072b, 2.754) | 34 | 6.093 (0.347, 32.13) | 7 | 0.0836/0.0288/0.0936/0.3200 |
aThe four diagnostically exposed cohorts were the Massachusetts + Canadian TB fluoroscopy, US scoliosis, UK-NCI CT, and the five therapeutically exposed cohorts were the French, Göteborg+Stockholm haemangioma, Israeli tinea capitis and Rochester thymus irradiated. Analyses were stratified by cohort, sex, age and year of follow-up (using intervals of age and year of follow-up defined by person-year table, as in Appendix A Table A1). Unless otherwise stated, all confidence intervals were based on the profile likelihood.
bWald-based CI.
cIndications of non-convergence.
Appendix B Fig. B3 illustrates the difference in dose response between the LSS combined with the diagnostically exposed groups in contrast to the therapeutically exposed groups for all three endpoints. Appendix B Table B6 shows that for the LSS and four diagnostically exposed cohorts combined there are highly significant excess risks for a linear ERR/Gy model for AML = 3.907 (95% CI 1.625, 7.985), CML = 6.211 (95% CI 2.166, 14.890), and ALL = 23.450 (95% CI 8.635, 72.280) (P-trend < 0.0001 in all cases); it is clear that these ERR/Gy estimates are dominated by the LSS estimates (Table 5). Appendix B Table B7 demonstrates that for the combined five therapeutically exposed cohorts the linear ERR/Gy estimates do not differ significantly from the null for any of the four endpoints. There are highly significant differences between the slopes of the dose responses obtained from the LSS plus diagnostically exposed cohorts and from the therapeutically exposed cohorts for AML (P = 0.0034), CML (P = 0.0003) and ALL (P < 0.0001).
Table 6 shows that in the LSS combined with the four diagnostically exposed groups there were significant reductions of ERR/Gy with increasing age at exposure for AML (P = 0.0267), driven by the LSS (Appendix B Table B11), and while for CML and ALL there were indications of such reductions with increasing age at exposure these were not statistically significant (P > 0.4). For the five therapeutically exposed groups, there were no suggestions of variation of risk by age at exposure (P > 0.5), which remained the case when all cohorts were analysed together (Table 6). Table 6 demonstrates that in the LSS combined with the four diagnostically exposed groups there were reductions in ERR/Gy with increasing time since exposure, which were statistically significant for ALL (P = 0.0062), and at marginal levels of significance for AML (P = 0.0787) and CML (P = 0.0856); however, these are very much driven by the LSS (Appendix B Table B11). The ERR/Gy estimates for the period 2–5 years after exposure were notably raised for all three endpoints, and significantly so for ALL. For the five therapeutically exposed groups there were no indications of variation of risk by time since exposure (P > 0.5) (Table 6). When all cohorts are analysed together there was significant heterogeneity of ERR/Gy by time since exposure for CML (P = 0.0108) and ALL (P = 0.0017), and at borderline levels of significance for AML (P = 0.0513).
Table 6.
Variation of excess relative risk per Gy or per Gy2 (and 95% CI) by age at exposure and time since exposure fitted to Japanese atomic bomb survivors plus diagnostically exposed cohorts and therapeutically exposed cohortsa.
| ERR/Gy | P value, heterogeneity | ERR/Gy2 | P value, heterogeneity | ERR/Gy | P value, heterogeneity | |
|---|---|---|---|---|---|---|
| Age at exposure (years) | ||||||
| Age at exposure (y) | LSS + diagnostic cohorts | Therapeutic cohorts | All cohorts | |||
| Acute myeloid leukaemia | ||||||
| 0–4.99 | 14.50 (4.558, 39.06) | 0.0267 | 0.524b (−0.470c, 1.518c) | 0.9429b | 2.035 (0.638, 4.571) | 0.6724 |
| 5–9.99 | 4.972 (0.316, 18.79) | 0.527b (−1.406c, 2.461c) | 1.734 (0.142, 4.913) | |||
| 10–14.99 | 3.769 (0.504, 11.22) | 0.238b (−3.852c, 4.327c) | 1.133 (−0.175, 4.146) | |||
| ≥15 | 0.496 (−1.265, 3.614) | −0.199b (−48.08c, 47.68c) | 0.370 (−1.218c, 3.113) | |||
| Chronic myeloid leukaemia | ||||||
| 0–4.99 | 9.691 (1.388, 39.31) | 0.5431 | −0.028b (−0.220c, 0.164c) | 0.9991b | 1.289 (−0.136, 5.069) | 0.9167 |
| 5–9.99 | 12.39 (2.262, 43.49) | −0.038b (−2.035c, 1.976) | 1.802 (0.043, 6.991) | |||
| 10–14.99 | 4.527 (−4.584, 22.83) | −0.026b (−6.487c, 6.435c) | 3.585 (−3.029c, 15.51) | |||
| ≥15 | 2.538 (−2.699, 11.95) | −0.060b (−72.54c, 72.42c) | 2.290 (−2.575c, 10.84) | |||
| Acute lymphoblastic leukaemia | ||||||
| 0–4.99 | 40.24 (8.583, >100) | 0.4519 | −0.028b (−0.066c, 1.513) | 0.9993b | 4.546 (0.802, 14.58) | 0.7322 |
| 5–9.99 | 55.52 (9.779, >100) | −0.031b (−1.968c, 6.594) | 6.773 (0.956, 23.76) | |||
| 10–14.99 | 12.28 (1.478, 56.39) | −0.089b (−4.568c, 14.65) | 5.679 (0.720, 20.84) | |||
| ≥15 | 16.59 (3.782, 71.33) | −0.261b (−52.82c, 52.30c) | 11.68 (2.837, 40.88) | |||
| Years since exposure | ||||||
| Years since exposure | LSS + diagnostic cohorts | Therapeutic cohorts | All cohorts | |||
| Acute myeloid leukaemia | ||||||
| 2–4.99 | 77.53 (−96.25c, >100) | 0.0787 | −0.074 (−1.613c, 30.39) | 0.9905 | 10.98 (−18.09c, >100) | 0.0513 |
| 5–9.99 | 13.99 (2.196, 61.37) | −0.080 (−0.510c, 29.24) | 9.687 (1.740, 35.55) | |||
| 10–14.99 | 14.29 (1.793, 67.23) | 0.011 (−2.682c, 20.82) | 7.875 (1.093, 29.30) | |||
| ≥15 | 2.320 (0.589, 5.695) | 0.532 (0.003, 1.681) | 0.916 (0.204, 2.085) | |||
| Chronic myeloid leukaemia | ||||||
| 2–4.99 | 98.16 (<−100c, >100) | 0.0856 | −0.038b (−11.07c, 10.99c) | 0.9928b | −0.283b (−16.66c, 16.10c) | 0.0108b |
| 5–9.99 | 28.88 (6.531, >100) | −0.032b (−2.973c, 2.908c) | 9.021b (−6.956c, 25.00c) | |||
| 10–14.99 | 3.331 (−9.238c, 38.75) | 0.024b (−5.382c, 5.430c) | 3.532b (−6.283c, 13.35c) | |||
| ≥15 | 2.857 (0.130, 9.988) | −0.028b (−0.173c, 0.117c) | 0.725b (−0.917c, 2.367c) | |||
| Acute lymphoblastic leukaemia | ||||||
| 2–4.99 | >100 (18.00, >100) | 0.0062 | −0.040b (−2.787c, 2.707c) | 0.9993b | −0.282 (−3.899c, 3.335c) | 0.0017 |
| 5–9.99 | >100 (27.15, >100) | −0.039b (−5.082c, 5.004c) | 29.88 (10.84, 66.12c) | |||
| 10–14.99 | >100 (25.15, >100) | −0.066b (−5.809c, 36.65) | 27.73 (−11.73c, 67.19c) | |||
| ≥15 | 4.130 (0.216, 18.80) | −0.027b (−0.277c, 0.223c) | 1.407 (−0.136, 5.062) | |||
aThe four diagnostically exposed cohorts were the Massachusetts + Canadian TB fluoroscopy, US scoliosis, UK-NCI CT, and the five therapeutically exposed cohorts were the French, Göteborg+Stockholm haemangioma, Israeli tinea capitis and Rochester thymus irradiated. Semi-parametric relative risk models (as given by expressions (C4) and (C5)) (Appendix C) were fitted, stratifying by cohort, sex, age and year of follow-up (using intervals of age and year of follow-up defined by person-year table, as in Appendix A Table A1).
bIndications of lack of convergence.
cWald-based confidence limit.
Discussion
Although there have been previous pooling analyses of leukaemia (e.g., Little et al. [36], Leuraud et al. [37]), this and the companion paper assessing risk for mean cumulative ABM doses <100 mGy [5] are the first to focus exclusively on leukaemia risks following radiation exposure in childhood. The present analysis, without restriction of ABM dose and with addition of one more cohort, adds 61 AML, 25 CML and 31 ALL cases/deaths to the 79, 36 and 40 of these types, respectively, considered in the <100 mGy analysis [5] (Table 1). The analysis is based on a long period of follow-up (with 56.3% person-years of follow-up ≥10 years after first exposure, and 28.3% person-years of follow-up ≥30 years after first exposure (Table 1)) and a large number of leukaemia cases/deaths in those exposed as children and adolescents. In this pooled analysis, all of the substantial studies of leukaemia after low and moderate dose exposure in childhood published at the time of the literature search are included. We observed significantly increasing risk with dose for AML, CML and ALL, with some indication of upward curvature in the dose response over the full dose range for all three endpoints (Table 4), and no significant heterogeneity in radiation-associated ERR between the cohorts, although there is significant heterogeneity in EAR for AML (Table 2). Our findings are entirely consistent with those from the previous pooled analysis of cohorts with cumulative ABM doses <100 mGy [5]. Table 3 and Appendix B Table B3 demonstrate that decreasing the dose range to ≤1 Gy or ≤500 mGy results in decreases of ERR/Gy for AML, AML + MDS, ALL, CML, acute leukaemia and myeloid malignant neoplasms, but with increasing restriction of dose below 500 mGy the ERR/Gy becomes larger for most endpoints, although for CML the effect of restriction of dose range tends to reduce the ERR/Gy, which becomes negative at doses ≤200 mGy. Consistent with this, Table 4, Appendix B Table B4 and Appendix B Table B5 suggest that there is upward curvature for many endpoints over the full dose range, albeit only marginally statistically significant for some endpoints (AML, AML + MDS, CML), and at least for ALL the curvature reverses direction with increasing restriction of dose. Our previous study with dose restricted to ≤100 mGy found little evidence of curvilinearity for any endpoint [5].
Although the significantly raised ERR/Gy estimates for AML, CML and ALL in the LSS are influential in the pooled results, the LSS and diagnostically exposed cohorts produce compatible estimates, with the exception of ALL (Table 5). While the limited statistical power for some (but not all (Appendix B Table B8)) of the therapeutic cohorts may have contributed to the mostly null results in the combined therapeutic cohorts, cell sterilisation in ABM compartments receiving high doses may be a better explanation, as discussed in detail below. One factor that may contribute to the heterogeneity in risk between the LSS and other cohorts is the lack of the first 5.1 years of follow-up in the LSS. There were strong indications in the late-1940s that there was a radiation-associated excess risk of leukaemia in the Japanese atomic bomb survivors [38]. This is likely to be particularly important for ALL given the significant reduction in ERR with increasing years since exposure (Table 6).
It has become clear that leukaemia is one of the most radiosensitive malignancies, with radiation-associated excesses seen in a number of exposed populations, and that excess relative risks per unit dose are much higher for those exposed in early life [1, 11, 39]. However, the shape of the dose response is unclear. In the LSS there were suggestions of upward curvature for AML, but not for ALL and CML, for which a linear dose response was indicated [17]. In the results reported here for the LSS combined with the four diagnostically exposed cohorts, there is weak evidence for upward curvature for ALL, but little departure from linearity in the dose responses for AML or CML (Appendix B Table B6). In a pooled analysis of childhood cancer survivors, there were weak and borderline significant increases in all leukaemia and AML risk with dose, although trends with dose were much stronger among those not receiving chemotherapy [40].
The small number of MDS in our study does not allow us to separately analyse this endpoint. Iwanaga et al. [41] and Matsuo et al. [42] found increased risk of MDS among the Japanese atomic bomb survivors. There has been notable controversy about inclusion (or not) of MDS in studies assessing the relationship of radiation from paediatric CT scans and subsequent risk of leukaemia [21, 26, 43]. The similarity of the dose response for AML and AML + MDS in our analysis (Tables 3 and 4 and Appendix B Table B5) weakly suggests that MDS is about as radiogenic as AML, but the small number of MDS cases in relation to the much larger number of AMLs (18 vs 140) implies that little weight can be assigned to this observation; the lack of expert haematopathology review of the MDS cases in our pooled cohorts precluded us from more detailed assessment.
Leukaemia is a rare but generally highly fatal complication of cancer treatment [44], and has been observed in some patient populations exposed to radiotherapy (RT) (that did not receive chemotherapy). There has been a number of studies of leukaemia after treatment for childhood cancer, in many of which there was chemotherapy, details of which are given in Table 7. Radiation risks in these studies were generally null (Table 7), possibly a consequence of the very high compartmental bone marrow doses, which in some compartments are well into the range at which cell sterilisation would be expected; however, the swamping effect of certain specific types of concomitant primary chemotherapy risks, which are generally markedly elevated, may also be a factor. It is notable that in RT-treated groups in which there is no or little primary chemotherapy, there is pronounced radiation-associated excess leukaemia risk [40]. The leukaemia risks in these studies of RT for cancer treatment are generally lower than, but statistically consistent with, those estimated here (Table 7).
Table 7.
Leukaemia relative risks in other groups exposed to ionising radiation in childhood and adulthood.
| Cohort | Endpoint | RR at 1 Gy ( + 95% CI) |
|---|---|---|
| Childhood exposure—present study and other childhood exposed at low-dose rate | ||
| Present study | AML | 4.91 (2.63, 8.99) |
| CML | 7.21 (3.17, 15.89) | |
| ALL | 24.45 (9.64, 73.28) | |
| UK background radiation [45] | AML | 41 (0, 211) |
| All leukaemia | 91 (21, 171) | |
| Swiss background radiation [46] | All leukaemia | 37 (0, 78) |
| French background radiation [49] | Acute leukaemia | 1 (0, 11) |
| French background radiation [50] | ALL | 0 (0, 9) |
| AML | 0 (0, 17) | |
| Finnish background radiation [51] | ALL | 0 (0, 91) |
| AML | 0 (0, 151) | |
| Chernobyl exposure age <6 [52] | All leukaemia | 33.4 (9.78, 85.0) |
| Childhood exposure—high-dose rate | ||
| LESG childhood cancer [53, 54] | All leukaemia | 1.00 (0.97, 1.09) |
| UK childhood cancer [54, 55] | All leukaemia | 1.24 (1.01, 2.28) |
| Euro2K childhood cancer [56] | All leukaemia | 1.31 (0.68, 1.94) |
| SFOP childhood cancer [57] | All leukaemia | 0.99 (0.93, 1.04) |
| Pooled childhood cancer [40] | All leukaemia without chemotherapy | 2.55 (1.14, 15.3) |
| All leukaemia with chemotherapy | 1.02 (0.99, 1.09) | |
| All-age exposure low-dose rate | ||
| Indian background radiation [58] | Leukaemia excluding CLL | 6.84 (ND, 345.3) |
| Chinese background radiation [59] | All leukaemia | 11.68 ( < 0, ∞) |
| Techa River [60] | Chronic myeloid leukaemia | 4.1 (1.5, 19) |
| Leukaemia excluding CLL | 1.51 (1.17, 2.5) | |
| Acute/subacute leukaemia | 2.8 (1.4, 6.9) | |
| Taiwan 60Co [61] | Leukaemia excluding CLL | 2.8 (1.4a, 3.8a) |
| All-age exposure high-dose rate | ||
| LSS + IRSCC + UK Spondylitis [36] | AML | 4.60b |
| CML | 3.26b | |
| Adult low-dose-rate exposure | ||
| INWORKS [37] | AML | 2.29 (0.18a, 5.28a) |
| CML | 11.45 (5.48a, 20.65a) | |
| ALL | 6.80 (NA, 32.57a) | |
| Mayak [62] | AML | 14.23 (5.25a, 49.45a) |
| CML | 2.39 (0.78a, 8.32a) | |
| Chornobyl clean-up [63] | Leukaemia excluding CLL | 6.0 (0.0a, 58a) |
| Chornobyl clean-up [64] | Leukaemia excluding CLL | 3.21 (1.05, 8.61) |
| Chornobyl clean-up [65] | Leukaemia excluding CLL | 1.44 (0.00a, 3.56a) |
LESG Late Effects Study Group, SFOP Société Française d’Oncologie Pédiatrique, IRSCC International Radiation Study of Cervical Cancer patients, INWORKS International Nuclear Workers Study.
a90% CI.
bAdjusted to age at exposure 25 years, 25 years since exposure; quadratic-exponential relative risk model RR shown at 1 Gy.
It is notable that leukaemia risks in some of the low-dose/low-dose-rate studies, in particular the UK [45] and Swiss [46] background radiation studies of childhood exposures, are higher than those estimated here (Table 7). The curvature in the dose response for the endpoints we evaluated, and the way the curvature changes direction depending on the dose range assessed (Table 4 and Appendix B Table B4) should be considered in comparing our findings with those at much lower levels of dose in the UK [45] and Swiss [46] background radiation studies; a linear dose response was observed, as might be expected since these are low-dose-rate exposures. Curvature was not seen in the low-dose range in our previous analysis ( ≤ 100 mGy) [5].
We observed pronounced and statistically significant (P < 0.05) reduction in relative risk with increasing age at exposure for AML, and weak indications of such reductions for CML and ALL, in the diagnostically exposed groups combined with the LSS (Table 6). There were no obvious variations in relative risks with increasing age at exposure for the therapeutically exposed groups (Table 6). Likewise, there were significant reductions in relative risk with increasing time since exposure for ALL, and at marginal levels of significance for AML and CML, in the diagnostically exposed groups combined with the LSS (although mostly driven by the LSS (Appendix B Table B11)), and suggestions of an excess risk 2–5 years after exposure, particularly for ALL. However, there were no time-since-exposure variations for the therapeutically exposed groups (Table 6). In a parallel analysis of the low-dose part of the radiation exposure range (<100 mGy) of this pooling study there were similar (but non-significant) age-at-exposure and time-since-exposure trends [5]. We are not aware of other studies of childhood exposure to low-to-moderate doses that evaluated risks for age at exposure and time since exposure. However, these age-at-exposure and time-since-exposure trends are consistent with the variations observed in a number of other exposed groups, in particular in a pooled analysis of all-age LSS incidence data and data from two medically exposed groups [36], also in later analysis of LSS incidence and mortality data with adjustment for dose error using Bayesian Markov Chain Monte Carlo and regression-calibration methods [47, 48].
The 93 cases/deaths of leukaemias excluding CLL, but not classified as AML/CML/ALL, produce an ERR/Gy estimate that is non-significantly positive, 0.60 (95% CI −0.76, 2.40, P = 0.27) (results not shown) but smaller than the estimates for AML, CML and ALL (Table 2). Of potential relevance are the small number (7) of cases from the LSS and the relatively large proportion (56%) of cases/deaths from the diagnostic cohorts, for which ERR/Gy estimates are generally low (Table 5). It is notable that most of these cases/deaths (81/93) occur among those with entry year before 1960 (Table 1); the majority (61/93) occur among those diagnosed before 1990, are over the age of 35 years at diagnosis (64/93), and there is a slight preponderance of deaths (52/93) (results not shown). The fact that so many of these cases/deaths are at age >35 years, and that there are only weak indications of a dose response suggest that it is possible that some of these are really CLL/SLL.
Strengths of the pooled analysis study reported here are the prospective designs used in all component cohorts, advanced dosimetry assessment for the period when the studies were carried out, long follow-up, harmonisation of endpoints, the large number of cases or deaths exposed at low and moderate doses, and assessment of possible temporal (in particular time-since-exposure and age-at-exposure) modifications. For the first time we have made extensive efforts to model the dose-response for the entire pooled analysis dataset with unrestricted doses and for several groupings of restricted dose categories, together with dose-response modelling for certain cohort subsets.
A major weakness of the study is lack of detailed information for all cohorts on several aspects of dose, including distribution of dose over time and by bone marrow compartment, and the dose rate of delivery. Consideration must be given to the within-individual heterogeneity in bone marrow dose that is present in all cohorts apart from the LSS. Therefore, a mean whole-body-averaged ABM dose of, say, 1 Gy for an individual could, in some of the medically exposed cohorts imply appreciably higher doses in certain bone marrow compartments, and as discussed above, localised ABM doses are high in most of the therapeutic cohorts. This would only matter if there were appreciable non-linearity in the leukaemia dose response, in particular, if doses were sufficiently high that cell sterilisation could be significant, which as discussed above is particularly likely in the five therapeutically exposed groups. For example, of interest are the low ERR/Gy estimates for the Israeli tinea capitis cohort, which had the highest mean whole-body-averaged ABM dose (0.29 Gy), but received mainly by the skull ABM. Among groups exposed to high-dose medical procedures there is additional evidence that this might occur for leukaemia [36]. Thus, although detailed assessment of the reported and available dosimetry was systematically undertaken by co-authors with expertise (DB and CL), the cumulative dose measure used must be considered in the light of absence of key dose information. The dosimetry is also not uniform between the component cohorts, as we discuss in Appendix A.
Another weakness is that many cohorts extend follow-up over many years, with the consequence that disease coding may not be uniform even within a single study. Varying follow-up periods for different studies exacerbates this problem. There are substantial geographic, ethnic, and socioeconomic differences between the cohorts, as well as the reason for radiation exposure (atomic bomb exposure, diagnostic medical, therapeutic medical), and in the underlying medical conditions of the subjects. However, the relative risk models we used were stratified by cohort (and so by country, underlying medical conditions, exposure type), and by calendar period and attained age, thus accounting for differences in baseline rates between countries, or over time, or both. An additional shortcoming is the indication of heterogeneity of risk between the cohorts, in particular between the LSS and the five therapeutically irradiated cohorts (Table 5). Follow-up for some of the cohorts (e.g., Rochester thymus, Canadian TB) began long after exposure, because the appropriate mechanisms of follow-up were not in place until that point (e.g., Canadian linkage to national mortality follow-up did not begin until 1950, Rochester thymus study linkage to national US mortality follow-up did not start until 1979 with creation of the National Death Index (NDI)). Inevitably this limits the information in the years soon after exposure for these studies, although it would not obviously result in bias. The number of cases for certain endpoints (e.g., MDS, CML, ALL) is limited, particularly in combination with certain subgroups (LSS, therapeutically exposed, diagnostically exposed). As with the previous analysis [5] we judged that it was important to give results for certain heterogeneous groups of disease (e.g., myeloid neoplasms, acute leukaemia) that have been commonly used in the past, although these are possibly not so useful aetiologically as the main endpoints (AML, CML, ALL) that we concentrate on. The overlap in endpoints must be taken into account in interpreting the results.
The mixture of mortality and incidence data complicates interpretation, but as we consider principally relative risk models, one would not expect ERR/Gy to differ appreciably in mortality compared with incidence. From Appendix B Table B10, ERR/Gy estimates from the combined six cohorts for which incidence data are available are significantly raised for all three endpoints, but none of the estimates from the combined four cohorts for which mortality data are available differs significantly from the null or from the estimates using incidence data; however, the numbers of deaths included in the mortality analyses were small, particularly so for ALL (n = 5). Follow-up in the various groups did not start at the same time after radiation exposure. For example, for mortality in the Rochester thymus cohort, follow-up did not begin until 1979, over 20 years after exposure, and so well past the peak period for ALL onset 5–10 years after exposure. Missed leukaemia deaths in this cohort might result in an underestimation of ERR/Gy, particularly for ALL. Although there are significant heterogeneities between the LSS, diagnostically and therapeutically irradiated groups, particularly for ALL (Table 5), these differences should be interpreted cautiously since they were based on groupings that were largely determined during the analysis and not pre-specified, although there was a general expectation that the higher dose cohorts might exhibit a distinct pattern of risks. Based on detailed analysis of the subgroups, we found that the LSS results had a considerable influence on the overall pooled analysis results, particularly for ALL. However, it should be borne in mind that global tests of heterogeneity for the ERR/Gy estimates from all ten cohorts do not show evidence of heterogeneity (Table 2).
In summary, we have documented radiation-associated excess leukaemia risks at low and moderate whole-body-averaged cumulative ABM doses for AML, CML and ALL. There is a marked and significant (or marginally significant) reduction of risk with increasing time after exposure, and indications of risk appearing within the period 2–5 years after exposure. For the full dose range, there is evidence of upward curvature in the dose response for ALL, acute leukaemia and myeloid malignant neoplasms (Table 4 and Appendix B Table B4), and weaker indications of such curvature also for AML (with or without MDS) and CML; there are also suggestions of upward curvature for ALL in the LSS+diagnostic group (Appendix B Table B6) and for AML in the therapeutic group (Appendix B Table B7). However, with increasing restriction of the dose range, downward curvature becomes apparent for ALL. Further follow-up of these and other groups using current systems of coding of lympho-haematopoietic neoplasms, possibly combined with the establishment of a uniform and up-to-date re-evaluation of dosimetry, is strongly recommended.
Supplementary information
Author contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Mark Little with assistance from Jeremy Miller and David Campbell. The first draft of the manuscript was written by Mark Little and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Division of Cancer Epidemiology and Genetics. The Radiation Effects Research Foundation (RERF), Hiroshima and Nagasaki, Japan is a public interest foundation funded by the Japanese Ministry of Health, Labour and Welfare (MHLW) and the US Department of Energy (DOE). The research was also funded in part through DOE award DE-HS0000031 to the National Academy of Sciences. Dr Zablotska’s work was supported by the National Cancer Institute of the National Institutes of Health under the R01CA197422 award. This publication was supported by RERF Research Protocol A1-16. The views of the authors do not necessarily reflect those of the two governments.
Data availability
The data are available from the first author upon request.
Code availability
All Epicure [32] and R [34] code used can be obtained from the principal author upon request.
Competing interests
Richard Wakeford is a member of the Technical Working Party of the UK Compensation Scheme for Radiation-Linked Diseases (http://www.csrld.org.uk), for which he is paid a consultancy fee. The Technical Working Party is unaware of the contents of this article, which are entirely independent of any views held by other members of the Technical Working Party. The remaining authors declare no competing interests.
Ethics approval and consent to participate
This study cohort has been declared exempt from requiring ethical approval by the NCI Special Studies Institution Review Board because we used preexisting approved data. Because of the size and age of these cohorts, and the fact that they were retrospectively assembled in many cases, individual informed consent could not have been obtained for most studies. However, in all cases, the exemption was granted by the relevant ethical review boards.
Consent for publication
There is no individual person’s data contained in the paper, so this is not relevant.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Mark P. Little, Richard Wakeford, Lydia B. Zablotska, Michael Jacob Adams, Amy Berrington de González, Martha S. Linet.
Deceased: Marie Lundell.
Supplementary information
The online version contains supplementary material available at 10.1038/s41416-023-02387-8.
References
- 1.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) UNSCEAR 2006 Report. Volume I. Annex A. Epidemiological studies of radiation and cancer. Vol E.08.IX.6. New York: United Nations; 2008. pp. 13–322. [Google Scholar]
- 2.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Volume II. Annex B: Effects of radiation exposure of children. UNSCEAR 2013 Report. Vol E.14.IX.2. New York: United Nations; 2013; p. 1–269.
- 3.Lymphoma Research Foundation (LRF). Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma https://lymphoma.org/understanding-lymphoma/aboutlymphoma/cll/. Accessed 5/2023 (2023).
- 4.Harbron RW, Pasqual E. Ionising radiation as a risk factor for lymphoma: a review. J Radiol Prot. 2020;40:R151–R185. doi: 10.1088/1361-6498/abbe37. [DOI] [PubMed] [Google Scholar]
- 5.Little MP, Wakeford R, Borrego D, French B, Zablotska LB, Adams MJ, et al. Leukaemia and myeloid malignancy among people exposed to low doses (<100 mSv) of ionising radiation during childhood: a pooled analysis of nine historical cohort studies. Lancet Haematol. 2018;5:e346–e358. doi: 10.1016/S2352-3026(18)30092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadetzki S, Chetrit A, Lubina A, Stovall M, Novikov I. Risk of thyroid cancer after childhood exposure to ionizing radiation for tinea capitis. J Clin Endocrinol Metab. 2006;91:4798–804. doi: 10.1210/jc.2006-0743. [DOI] [PubMed] [Google Scholar]
- 7.Ron E, Modan B, Boice JD., Jr Mortality after radiotherapy for ringworm of the scalp. Am J Epidemiol. 1988;127:713–25. doi: 10.1093/oxfordjournals.aje.a114852. [DOI] [PubMed] [Google Scholar]
- 8.Little MP, Wakeford R, Zablotska LB, Borrego D, Griffin KT, Allodji RS, et al. Lymphoma and multiple myeloma in cohorts of persons exposed to ionising radiation at a young age. Leukemia. 2021;35:2906–16. doi: 10.1038/s41375-021-01284-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) UNSCEAR 2019 Report. Annex A. Evaluation of selected health effects and inference of risk due to radiation exposure. Vol E.20.IX.5. New York: United Nations; 2020. pp. 21–192. [Google Scholar]
- 10.Little MP. Leukaemia following childhood radiation exposure in the Japanese atomic bomb survivors and in medically exposed groups. Radiat Prot Dosim. 2008;132:156–65. doi: 10.1093/rpd/ncn264. [DOI] [PubMed] [Google Scholar]
- 11.Wakeford R. The risk of childhood leukaemia following exposure to ionising radiation-a review. J Radiol Prot. 2013;33:1–25. doi: 10.1088/0952-4746/33/1/1. [DOI] [PubMed] [Google Scholar]
- 12.Davis FG, Boice JD, Jr., Hrubec Z, Monson RR. Cancer mortality in a radiation-exposed cohort of Massachusetts tuberculosis patients. Cancer Res. 1989;49:6130–6. [PubMed] [Google Scholar]
- 13.Dondon MG, de Vathaire F, Shamsaldin A, Doyon F, Diallo I, Ligot L, et al. Cancer mortality after radiotherapy for a skin hemangioma during childhood. Radiother Oncol. 2004;72:87–93. doi: 10.1016/j.radonc.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Lindberg S, Karlsson P, Arvidsson B, Holmberg E, Lundberg LM, Wallgren A. Cancer incidence after radiotherapy for skin haemangioma during infancy. Acta Oncol. 1995;34:735–40. doi: 10.3109/02841869509127180. [DOI] [PubMed] [Google Scholar]
- 15.Lundell M, Holm L-E. Mortality from leukemia after irradiation in infancy for skin hemangioma. Radiat Res. 1996;145:595–601. doi: 10.2307/3579278. [DOI] [PubMed] [Google Scholar]
- 16.Lundell M, Mattsson A, Karlsson P, Holmberg E, Gustafsson A, Holm L-E. Breast cancer risk after radiotherapy in infancy: a pooled analysis of two Swedish cohorts of 17,202 infants. Radiat Res. 1999;151:626–32. doi: 10.2307/3580039. [DOI] [PubMed] [Google Scholar]
- 17.Hsu W-L, Preston DL, Soda M, Sugiyama H, Funamoto S, Kodama K, et al. The incidence of leukemia, lymphoma and multiple myeloma among atomic bomb survivors: 1950-2001. Radiat Res. 2013;179:361–82. doi: 10.1667/RR2892.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams MJ, Dozier A, Shore RE, Lipshultz SE, Schwartz RG, Constine LS, et al. Breast cancer risk 55+ years after irradiation for an enlarged thymus and its implications for early childhood medical irradiation today. Cancer Epidemiol Biomark Prev. 2010;19:48–58. doi: 10.1158/1055-9965.EPI-09-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams MJ, Shore RE, Dozier A, Lipshultz SE, Schwartz RG, Constine LS, et al. Thyroid cancer risk 40+ years after irradiation for an enlarged thymus: an update of the Hempelmann cohort. Radiat Res. 2010;174:753–62. doi: 10.1667/RR2181.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174:83–90. doi: 10.1667/RR2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foucault A, Ancelet S, Dreuil S, Caër-Lorho S, Ducou Le Pointe H, Brisse H, et al. Childhood cancer risks estimates following CT scans: an update of the French CT cohort study. Eur Radiol. 2022;32:5491–8. doi: 10.1007/s00330-022-08602-z. [DOI] [PubMed] [Google Scholar]
- 23.Krille L, Dreger S, Schindel R, Albrecht T, Asmussen M, Barkhausen J, et al. Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys. 2015;54:1–12. doi: 10.1007/s00411-014-0580-3. [DOI] [PubMed] [Google Scholar]
- 24.Journy N, Rehel JL, Ducou Le Pointe H, Lee C, Brisse H, Chateil JF, et al. Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer. 2015;112:185–93. doi: 10.1038/bjc.2014.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nikkilä A, Raitanen J, Lohi O, Auvinen A. Radiation exposure from computerized tomography and risk of childhood leukemia: Finnish register-based case-control study of childhood leukemia (FRECCLE) Haematologica. 2018;103:1873–80. doi: 10.3324/haematol.2018.187716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meulepas JM, Ronckers CM, Smets A, Nievelstein RAJ, Gradowska P, Lee C, et al. Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst. 2019;111:256–63. doi: 10.1093/jnci/djy104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zablotska LB, Little MP, Cornett RJ. Potential increased risk of ischemic heart disease mortality with significant dose fractionation in the Canadian fluoroscopy cohort study. Am J Epidemiol. 2014;179:120–31. doi: 10.1093/aje/kwt244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadetzki S, Flint-Richter P, Ben-Tal T, Nass D. Radiation-induced meningioma: a descriptive study of 253 cases. J Neurosurg. 2002;97:1078–82. doi: 10.3171/jns.2002.97.5.1078. [DOI] [PubMed] [Google Scholar]
- 29.Jaffe ES, Harris NL, Stein H, Vardiman JW. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press; 2001. World Health Organization classification of tumours; pp. 1–352. [Google Scholar]
- 30.Hastie TJ, Tibshirani RJ. Generalized additive models. Boca Raton, FL: Chapman & Hall/CRC; 1990. p. i-xv+1-335. [Google Scholar]
- 31.McCullagh P, Nelder JA. Generalized linear models. 2nd edition. Boca Raton, FL: Chapman and Hall/CRC; 1989. pp. 1–526. [Google Scholar]
- 32.Risk Sciences International. Epicure version 2.0.1.0. 55 Metcalfe, K1P 6L5. Canada: Risk Sciences International; 2015.
- 33.Cox DR, Hinkley DV. Theoretical Statistics. London: Chapman and Hall; 1974. pp. 1–511. [Google Scholar]
- 34.R: A language and environment for statistical computing.https://www.r-project.org. Version 4.3.1. Vienna, Austria: R Foundation for Statistical Computing; 2023.
- 35.Little MP, Wakeford R, Lubin JH, Kendall GM. The statistical power of epidemiological studies analyzing the relationship between exposure to ionizing radiation and cancer, with special reference to childhood leukemia and natural background radiation. Radiat Res. 2010;174:387–402. doi: 10.1667/RR2110.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Little MP, Weiss HA, Boice JD, Jr., Darby SC, Day NE, Muirhead CR. Risks of leukemia in Japanese atomic bomb survivors, in women treated for cervical cancer, and in patients treated for ankylosing spondylitis. Radiat Res. 1999;152:280–92. doi: 10.2307/3580328. [DOI] [PubMed] [Google Scholar]
- 37.Leuraud K, Richardson DB, Cardis E, Daniels RD, Gillies M, O'Hagan JA, et al. Ionising radiation and risk of death from leukaemia and lymphoma in radiation-monitored workers (INWORKS): an international cohort study. Lancet Haematol. 2015;2:e276–e281. doi: 10.1016/S2352-3026(15)00094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Folley JH, Borges W, Yamawaki T. Incidence of leukemia in survivors of the atomic bomb in Hiroshima and Nagasaki, Japan. Am J Med. 1952;13:311–21. doi: 10.1016/0002-9343(52)90285-4. [DOI] [PubMed] [Google Scholar]
- 39.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. National Research Council (NRC). Health risks from exposure to low levels of ionizing radiation: BEIR VII - Phase 2. Washington, DC, USA: National Academy Press; 2006. p. 1–406. [PubMed]
- 40.Allodji RS, Tucker MA, Hawkins MM, Le Deley MC, Veres C, Weathers R, et al. Role of radiotherapy and chemotherapy in the risk of leukemia after childhood cancer: an international pooled analysis. Int J Cancer. 2021;148:2079–89. doi: 10.1002/ijc.33361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iwanaga M, Hsu WL, Soda M, Takasaki Y, Tawara M, Joh T, et al. Risk of myelodysplastic syndromes in people exposed to ionizing radiation: a retrospective cohort study of Nagasaki atomic bomb survivors. J Clin Oncol. 2011;29:428–34. doi: 10.1200/JCO.2010.31.3080. [DOI] [PubMed] [Google Scholar]
- 42.Matsuo M, Iwanaga M, Kondo H, Soda M, Jo T, Horio K, et al. Clinical features and prognosis of patients with myelodysplastic syndromes who were exposed to atomic bomb radiation in Nagasaki. Cancer Sci. 2016;107:1484–91. doi: 10.1111/cas.13025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Council on Radiation Protection and Measurements (NCRP). Report No. 171. Uncertainties in the estimation of radiation risks and probability of disease causation. 7910 Woodmont Avenue, Suite 400/Bethesda, MD 20814-3095. USA: National Council on Radiation Protection and Measurements (NCRP);2012. p. 1–418.
- 44.Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, et al. NIH Publication Number 05-5302. Bethesda, MD: National Cancer Institute; 2006. New malignancies among cancer survivors: SEER cancer registries, 1973-2000; pp. 1–492. [Google Scholar]
- 45.Kendall GM, Little MP, Wakeford R, Bunch KJ, Miles JCH, Vincent TJ, et al. A record-based case-control study of natural background radiation and the incidence of childhood leukaemia and other cancers in Great Britain during 1980-2006. Leukemia. 2013;27:3–9. doi: 10.1038/leu.2012.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Spycher BD, Lupatsch JE, Zwahlen M, Röösli M, Niggli F, Grotzer MA, et al. Background ionizing radiation and the risk of childhood cancer: a census-based nationwide cohort study. Environ Health Perspect. 2015;123:622–8. doi: 10.1289/ehp.1408548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Little MP, Hoel DG, Molitor J, Boice JD, Jr., Wakeford R, Muirhead CR. New models for evaluation of radiation-induced lifetime cancer risk and its uncertainty employed in the UNSCEAR 2006 report. Radiat Res. 2008;169:660–76. doi: 10.1667/RR1091.1. [DOI] [PubMed] [Google Scholar]
- 48.Little MP, Pawel D, Misumi M, Hamada N, Cullings HM, Wakeford R, et al. Lifetime mortality risk from cancer and circulatory disease predicted from the Japanese atomic bomb survivor Life Span Study data taking account of dose measurement error. Radiat Res. 2020;194:259–76. doi: 10.1667/RR15571.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Demoury C, Marquant F, Ielsch G, Goujon S, Debayle C, Faure L, et al. Residential exposure to natural background radiation and risk of childhood acute leukemia in France, 1990-2009. Environ Health Perspect. 2017;125:714–20. doi: 10.1289/EHP296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berlivet J, Hémon D, Cléro E, Ielsch G, Laurier D, Faure L, et al. Residential exposure to natural background radiation at birth and risk of childhood acute leukemia in France, 1990-2009. J Environ Radioact. 2021;233:106613. doi: 10.1016/j.jenvrad.2021.106613. [DOI] [PubMed] [Google Scholar]
- 51.Nikkilä A, Erme S, Arvela H, Holmgren O, Raitanen J, Lohi O, et al. Background radiation and childhood leukemia: a nationwide register-based case-control study. Int J Cancer. 2016;139:1975–82. doi: 10.1002/ijc.30264. [DOI] [PubMed] [Google Scholar]
- 52.Davis S, Day RW, Kopecky KJ, Mahoney MC, McCarthy PL, Michalek AM, et al. Childhood leukaemia in Belarus, Russia, and Ukraine following the Chernobyl power station accident: results from an international collaborative population-based case-control study. Int J Epidemiol. 2006;35:386–96. doi: 10.1093/ije/dyi220. [DOI] [PubMed] [Google Scholar]
- 53.Tucker MA, Meadows AT, Boice JD, Jr., Stovall M, Oberlin O, Stone BJ, et al. Leukemia after therapy with alkylating agents for childhood cancer. J Natl Cancer Inst. 1987;78:459–64. doi: 10.1093/jnci/78.3.459. [DOI] [PubMed] [Google Scholar]
- 54.Little MP. Comparison of the risks of cancer incidence and mortality following radiation therapy for benign and malignant disease with the cancer risks observed in the Japanese A-bomb survivors. Int J Radiat Biol. 2001;77:431–64. doi: 10.1080/09553000010022634. [DOI] [PubMed] [Google Scholar]
- 55.Hawkins MM, Wilson LM, Stovall MA, Marsden HB, Potok MHN, Kingston JE, et al. Epipodophyllotoxins, alkylating agents, and radiation and risk of secondary leukaemia after childhood cancer. BMJ. 1992;304:951–8. doi: 10.1136/bmj.304.6832.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haddy N, Le Deley MC, Samand A, Diallo I, Guérin S, Guibout C, et al. Role of radiotherapy and chemotherapy in the risk of secondary leukaemia after a solid tumour in childhood. Eur J Cancer. 2006;42:2757–64. doi: 10.1016/j.ejca.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 57.Allard A, Haddy N, Le Deley MC, Rubino C, Lassalle M, Samsaldin A, et al. Role of radiation dose in the risk of secondary leukemia after a solid tumor in childhood treated between 1980 and 1999. Int J Radiat Oncol Biol Phys. 2010;78:1474–82. doi: 10.1016/j.ijrobp.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 58.Nair RR, Rajan B, Akiba S, Jayalekshmi P, Nair MK, Gangadharan P, et al. Background radiation and cancer incidence in Kerala, India-Karanagappally cohort study. Health Phys. 2009;96:55–66. doi: 10.1097/01.HP.0000327646.54923.11. [DOI] [PubMed] [Google Scholar]
- 59.Tao Z, Akiba S, Zha Y, Sun Q, Zou J, Li J, et al. Cancer and non-cancer mortality among Inhabitants in the high background radiation area of Yangjiang, China (1979-1998) Health Phys. 2012;102:173–81. doi: 10.1097/HP.0b013e31822c7f1e. [DOI] [PubMed] [Google Scholar]
- 60.Krestinina LY, Davis FG, Schonfeld S, Preston DL, Degteva M, Epifanova S, et al. Leukaemia incidence in the Techa River Cohort: 1953-2007. Br J Cancer. 2013;109:2886–93. doi: 10.1038/bjc.2013.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsieh W-H, Lin I-F, Ho J-C, Chang PW. 30 years follow-up and increased risks of breast cancer and leukaemia after long-term low-dose-rate radiation exposure. Br J Cancer. 2017;117:1883–7. doi: 10.1038/bjc.2017.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kuznetsova IS, Labutina EV, Hunter N. Radiation risks of leukemia, lymphoma and multiple myeloma incidence in the Mayak cohort: 1948-2004. PLoS ONE. 2016;11:e0162710. doi: 10.1371/journal.pone.0162710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kesminiene A, Evrard AS, Ivanov VK, Malakhova IV, Kurtinaitis J, Stengrevics A, et al. Risk of hematological malignancies among Chernobyl liquidators. Radiat Res. 2008;170:721–35. doi: 10.1667/RR1231.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zablotska LB, Bazyka D, Lubin JH, Gudzenko N, Little MP, Hatch M, et al. Radiation and the risk of chronic lymphocytic and other leukemias among Chornobyl cleanup workers. Environ Health Perspect. 2013;121:59–65. doi: 10.1289/ehp.1204996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ivanov VK, Tsyb AF, Khait SE, Kashcheev VV, Chekin SY, Maksioutov MA, et al. Leukemia incidence in the Russian cohort of Chernobyl emergency workers. Radiat Environ Biophys. 2012;51:143–9. doi: 10.1007/s00411-011-0400-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available from the first author upon request.
All Epicure [32] and R [34] code used can be obtained from the principal author upon request.