Abstract
Background/Aims
Limited bystander assistance and delayed emergency medical service arrival reduce the chances of survival in cardiac arrest victims. Early basic life support through trained first responders (FR) and automatic external defibrillation both improve the outcome. Well-organized FR networks have shown promise, but guidance on effective implementation is lacking. This study evaluates two FR networks, in Belgium and in Switzerland, to identify main advancements in the development of such systems.
Method
Direct comparison is made of the barriers and facilitators in the development of both FR systems from 2006 up until December 2022, and summarized within a roadmap.
Results
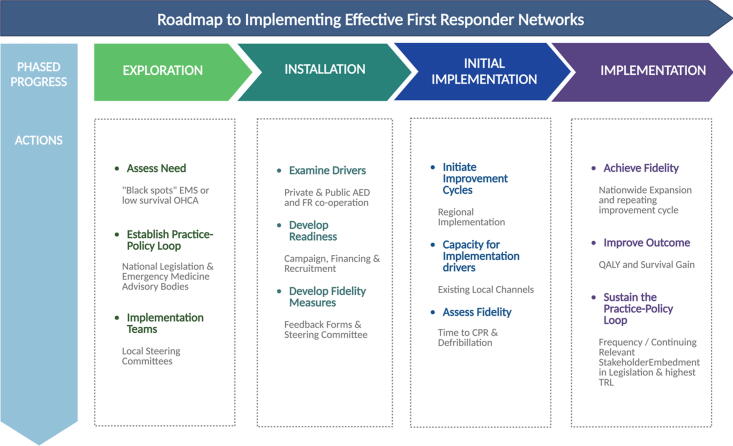
The Roadmap comprises four integral steps: exploration, installation, initiation, and implementation. Exploration involves understanding the national legislation, engaging with advisory bodies, and establishing local steering committees. The installation phase focuses on FR recruitment, engaging specific professional groups such as firemen, registering public Automated External Defibrillators (AEDs), and requesting feedback. The initiation step includes implementing improvement cycles and fidelity measures. Finally, implementation expands the network, leading to increased survival rates and the integration of these practices into legislation. A significant focus is placed on FR's psychological wellbeing. Moreover, the roadmap highlights the use of efficient geo-mapping to simplify optimal AED placement and automatically assign FRs to tasks.
Conclusion
The importance of FR networks for early resuscitation is increasingly recognized and various systems are being developed. Key developmental strategies of the EVapp and Ticino Cuore app system may serve as a roadmap for other systems and implementations within Europe and beyond.
Keywords: First responders, Mobile phone application, Europe, Challenges, Roadmap
Introduction
Community-based first responder systems
Sudden out-of-hospital cardiac arrest (OHCA) is the third leading cause of death in Europe.1 In Europe, the overall incidence of OHCA, where cardiopulmonary resuscitation (CPR) is attempted, was 56 (range 21–91) per 100 000 population per year.2 Important determinants of survival in OHCA are early CPR as part of basic life support (BLS) and rapid defibrillation to restore spontaneous circulation.3, 4, 5 Delayed arrival time of the emergency medical services (EMS) has been associated with poor survival.6, 7 Two different meta-analyses have both confirmed increased survival with similar or increased favourable neurological outcome if early defibrillation was performed, either by bystanders or citizen first responders (FR), in comparison to the standard EMS response (OR 1.45 (CI: 1.21–1.74) and 1.73 (CI: 1.36, 2.18)).8, 9 International guidance supports the implementation of systems that dispatch citizens as FR to suspected OHCA.10, 11, 12
Emergency medical system in Belgium and Switzerland
The ‘EMS landscape’ and setting in which both the Belgian13 and Swiss FR systems have been developed are largely comparable (Table 1). Aside from geographical differences, main structural difference entails a higher ‘FR basic’ or volunteer population in Ticino, which is linked to the nationally adapted availability and legislation.
Table 1.
Overview of demographic, geographic, and EMS landscape. OHCA, out-of-hospital cardiac arrest; N/A, not-available; BLS, basic-life support provided by paramedic; ALS, advanced life support provided by specialised physician and trained emergency nurse; AED, automatic external defibrillator.
| Parameter | Belgium | Switzerland |
|---|---|---|
| Population | 11.6 million (Hoogstraten: 21,386 inhabitants, Province Antwerp 506,922 inhabitants), 4.8%) | 8.5 million (Canton Ticino 353,343 inhabitants, 4.1%) |
| Population Density | 377 inhabitants per km2 | 219 inhabitants per km2 |
| Geographical setting | Largely rural and flat | Mountains, valleys, and lakes |
| Emergency services | Federal, Regional dispatching centre | Federal, Regional dispatching centre |
| Average EMS response time (BLS) | 10 minutes | 8 minutes |
| Average MUG/ SMUR response time (ALS) | 16.7 minutes (median 12 minutes) | 10 minutes |
| AED registration | Required by law | Required by law |
| Lay-responders AED use | Authorised | Authorised |
| National number of AED | Over 10 000 devices | N/A |
Emergency volunteer application (EVapp)
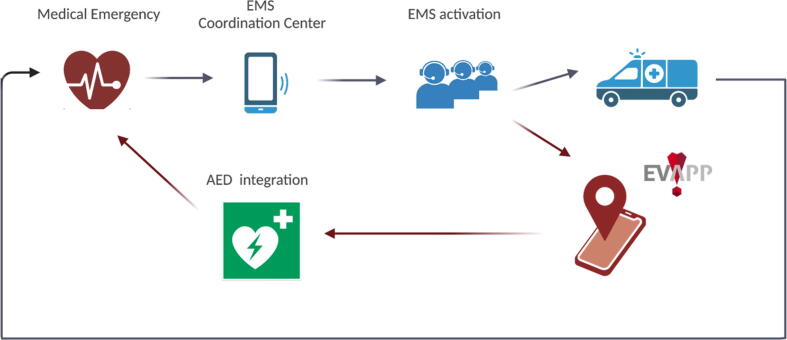
In Belgium, a community-based emergency FR network has been established to respond to OHCA using the EVapp smartphone application.14 EVapp mobilizes FR to perform CPR and uses publicly available defibrillators (PAD) in response to suspected OHCA before the arrival of EMS (Fig. 1).
Fig. 1.
Schematic representation of the Emergency Volunteer Application system (EVapp). EMS, Emergency Volunteer Services; AED, Automatic External Defibrillator. Created with BioRender.com.
When the 112-dispatch centre receives an emergency call, EVapp FR are activated in parallel with the standard EMS. The system compares the position of the incoming emergency call to the geographical position of all FR and the location of AEDs. The FR within 1 km first receive a warning alert which they can accept or decline. Subsequently, the radius is increased up to 1.5 km. The first two FR accepting the alert are send directly to the victim. The following two are sent to the victim via the closest AED. The fifth FR is sent directly to the victim. If too few FR are found with active geolocation, a short text message or SMS-alert is send to FR that have a registered home or working address within 1.5 km. The distance to the nearest AED is calculated in walking distance, programmed within the system. Instructions on how to reach non-24/7 accessible AEDs are available.
Ticino Cuore mobile APP
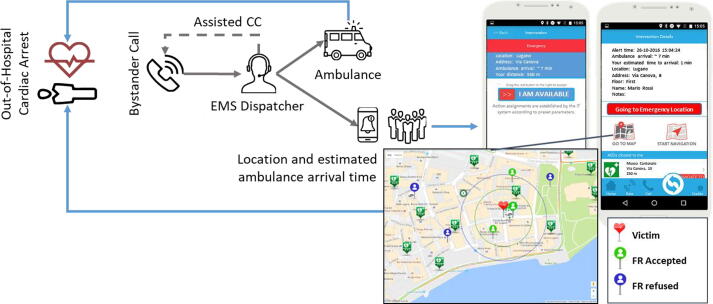
In 2005 a non-profit organization – Fondazione Ticino Cuore (FTC) – has been created with the mission to educate the population about OHCA, and to counsel local EMS to improve delivery and efficiency of the CPR and AEDs. Over the years, FTC has undertaken a number of key initiatives including training of lay persons in BLS and use of AED, implementation of the “culture” of FR, increasing the number of AEDs and increasing the focus on early revascularization. The Ticino Cuore mobile app is an application citizens can download onto their mobile device from the Apple App Store or Google Play for free (Fig. 2).15 The mobile application automatically calculates the estimated time of arrival of the FR (walking distance) compared to the EMS and only notifies those who may arrive before the EMS. Notifications are possible through push-notifications and SMS. Nearby registered AEDs are flagged on the map to facilitate their access to FR involved in the mission.
Fig. 2.
Schematic representation of the Ticino Cuore mobile Application system. EMS, Emergency Medical Services; CC, central coordinator; FR, first responder. Adapted from Caputo et al. (2017) (1).
Methodology
This paper was created to give an overview of the development of two FR systems EVapp (Belgium) and Ticino Cuore app (Switzerland) in a European setting. A direct comparison is made of the barriers and facilitators in the development of both systems. Experience-based data and national documentation is used from 2006 up until December 2022. The results have been summarized, according to the process of active implementation frameworks,16 to propose a roadmap for effective FR network. The roadmap integrates experiences from Belgium and Switzerland.
Results
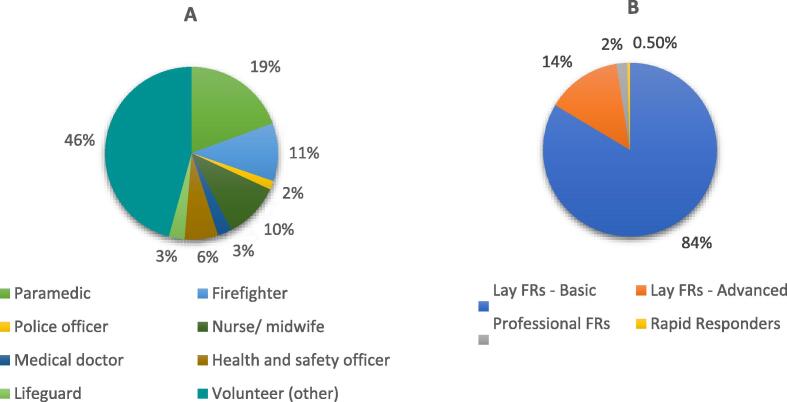
The Emergency Volunteer Application (EVapp) system has been implemented in Hoogstraten (0.2% (21,386/ 11,600,000) of Belgian population) in 2017. The Ticino Cuore app has been implemented in Canton Ticino (4.1% (353,343/8,500,000) of Swiss population). A two-by-two comparison is made based on analysis of internal registered data of both systems (Table 2, Fig. 3). In the EVapp system, all FR have a dedicated role, based on their location and allocated by the system. In contrast, the Ticino system limits the number of FR activated and uses location-based calculations to exclude those likely to arrive after the EMS, preventing FR from becoming fatigued due to futile activations. Ticino Cuore has a decade longer experience and broader geographical area, reflected in a higher amount of registered FR. The dynamics of both strategies are reflected in the overall response rate.
Table 2.
Comparison between both systems EVapp and Ticino Cuore App. AED, automatic external defibrillator; FR, First Responder; SMS, standard short message.
| System | EVapp | Ticino Cuore App |
|---|---|---|
| 1. Initiation of the system | ||
| Year of Implementation | 2017 | 2014 |
| Location of Implementation | Hoogstraten, Belgium | Canton Ticino, Switzerland |
| 2. AEDs and type of Volunteers | ||
| Number of AEDs (December 2022) |
22 | 1592 |
| Number of FR (December 2022) |
340 | 5931 |
| Number of FR on the total population (in %) | 1.6% | 1.7% |
| Ratio AED to FRs | 1:2 | 1:3 |
| AEDs privately owned | 45% | 64% |
| Types of FR |
|
|
| 3. System specifics | ||
| Equipment | 2 lay responders are navigated to the closest AED, additional nearby AEDs shown on a map. | AED navigation not included; nearby AEDs shown on a map. |
| Volunteer Activation | All nearby volunteers are activated. | All volunteers nearby are activated, only those with a transportation time less than the EMS arrival time are then activated. |
| Closure of responder call | When 5 volunteers have accepted using geolocation, or indefinite number in case of SMS activation. | Maximum of 6 volunteers, 1 for each professional or lay advanced/rapid FR and 3 for lay basic FR. |
| Response Rate | Ranging from 55 to 75% | Ranging from 70 to 80%. |
| Notification System | Notification through mobile push-notification based on geolocation or SMS (work and home address). | Notification through a mobile push notification. |
1. Statbel, het Belgische statistiekbureau | Statbel [Internet]. [cited 2023 May 1]. Available from: https://statbel.fgov.be/nl.
15. Caputo ML, Muschietti S, Burkart R, Benvenuti C, Conte G, Regoli F, et al. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: A comparison with SMS-based system notification. Resuscitation 2017;114:73–8. https://doi.org/10.1016/J.RESUSCITATION.2017.03.003.
Fig. 3.
Overview of the first responders background in the EVapp system (A), and Ticino Cuore app (B). FR, first responder.
Legal framework
In Belgium, the EMS response to emergency calls made to the 112-dispatch centre is regulated by the Law of 8 July 1964. According to this law, the dispatcher can only call on the services of a doctor, an ambulance service, a Mobile Emergency and Resuscitation Services (SMUR/MUG) or hospital. A separate article of the law provides for the possibility of also including “other interveners”, insofar as this is arranged via a royal decree. The other intervener is not necessarily a practitioner of a healthcare profession, such that, for example, individuals who have completed CPR training could get involved. A royal decree has yet to be implemented to establish the qualifications, training, availability, territorial distribution, equipment, and operation of such interveners. To initiate the pilot project of EVapp in Hoogstraten, various advisory bodies such as the Provincial Commissions for Urgent Medical Assistance, the National Council for Urgent Medical Assistance, and the 112-dispatch centre were consulted to determine the requirements for EVapp FR. Additionally, the EVapp system had to comply with the rights of volunteers outlined in the Belgian Law of July 3, 2005. EVapp FR are considered volunteers under this law and are protected from liability, provided that EVapp is organized by a non-profit association. Pursuant to this law, the organization is liable for any accidental damage caused by the FR and is required to have insurance coverage to mitigate the risks associated with volunteering. EVapp has opted for comprehensive coverage including civil liability for physical or material damage incurred during mobilization towards the victim or AED and during resuscitation, as well as additional accident insurance.
In Ticino, every citizen who becomes FR is required to read and accept the regulation on the conditions of use of the mobile app. Moreover, the user undertakes not to disclose sensitive information, not to cause damage to property and persons, assuming any responsibility.
Privacy
Within both applications, the following data may be collected and linked to the user 1) location, 2) contact information, and 3) identifiers. In Belgium, the collection and transfer of personal data of an OHCA victim by the 112-dispatch center to the EVapp server and onto the EVapp FR is regarded as processing of health data and is subject to strict legal policies prioritizing citizens' privacy. These policies in principle require the duty to inform the victim, recognition of the supervision of the Privacy Commission, and adherence to strict general principles and mandatory contractual arrangements. A customized protocol agreement defines the cooperation, data exchange and protection policies, and situations in which the network should be activated, between EVapp, 112 dispatch centers, and the (see further).
In Ticino, the user agrees not to disclose sensitive information or cause harm to property or individuals, while also assuming responsibility. From a legal point of view, FR network respects national laws on data protection and privacy (Law n.163.100 of March 9th, 1987). In both systems, the location of the alert is only disclosed after a FR accepts the mission.
Campaign and financing
In Belgium, the EVapp system maximizes community resources by utilizing available AED and BLS trained individuals.14 Recruitment is done mainly through interactions with professional and non-governmental organizations. The network’s current costs are covered by local authorities or governments. To give an example, the city annually allocates approximately 7000 euros for the operation and maintenance of the EVapp system. This investment encompasses various facets of the system, including technical infrastructure, volunteer management and insurance, real-time AED mapping available 24/7, integration with EMS, and overhead expenses. This represents a strategic expenditure, maintaining the functionality and effectiveness of the emergency response tool.
In Ticino, the development and maintenance of the FR network, including mobile app management, is part of the mission statement of Ticino Cuore Foundation, funded mostly by private donors and Cantonal contributions.
Practice-policy connections
The development of the EVapp network greatly benefited from the development of a local steering committee. The committee consists of political and official representation of the city, and technical partners (software provider, (regional) EMS and ambulance center). In addition, representation from the general practitioners and paramedical professions, fire brigade zone, local health-related non-governmental organisations, welfare advisory councils, local school organisations may offer added value. The steering committee meets at least twice a year and is accountable of the local embedment of the project. Within this steering committee, the interventions are discussed, to identify points for improvement. A firm privacy policy is in place to allow data sharing within the committee.
In Ticino, the establishment of a FR network was the main goal of the non-profit organization, Fondazione Ticino Cuore. Entrusted by the local EMS, the organization was given the mandate to manage the OHCA registry and to implement critical strategies aimed at enhancing public awareness of cardiac arrest and encouraging community participation in resuscitation efforts.
Recruitment of the first responders
Healthcare professionals and certified laypeople with 3 hours of BLS training in the last 5 years can join the EVapp network after verifying their certificate through the EVapp website. EVapp does not provide additional training but instead promotes existing high-quality training offered by organizations in the region. Promotional material was provided to the city during the pilot project to support recruitment of FR, and multiple channels were used to launch the project. Regular social events are held to emphasize the importance of the FR community network and demonstrate the operation of the EVapp system.
Since 2002, the Fondazione Ticino Cuore has implemented strategic initiatives to strengthen bystander resuscitation attempts and FR networks in Swiss Canton Ticino. These initiatives include resuscitation training for laypeople and students, improving telephone guidance from emergency dispatch centers, introducing SMS and mobile app-based FR recruitment systems, and improving public AED territorial coverage. Lay citizens and professional FRs were recruited via various channels, including websites, social media, and health centers. BLS certification is required to join the FR community and receive OHCA notifications through the app. By December 31, 2022, 18.4% of the resident population had completed a BLS-D course that complies with the recommendations of the European Resuscitation Council.17
Currently, both systems have surpassed the minimum requirement of including at least 1% of the total population as FR as well as a favorable AED to FR ratio (Table 2). The 1% threshold confirms that coverage is sufficient to dispatch volunteers to OHCA.14
Aftercare
The EVapp system provides different forms of aftercare, including hot and cold debriefings and feedback forms (cfr. Supplementary Materials I-II). Feedback forms are automatically sent within 24 hours and are used to gather information about the intervention and the need for further aftercare. In case a person needs special assistance after the intervention to process the traumatic event, EVapp guideS the FR to the local 'Centre for General Welfare' (CAW) or to regular professional assistance.
In Ticino, FRs are asked to complete a web-based questionnaire covering aspects such as the intervention, perceived intervention times, challenges encountered, treatment attempted, collaboration with EMS personnel, interaction with EMS dispatcher, and willingness to continue participation in the FR network. The Ticino Cuore Foundation celebrates the “Knight of the Heart” award annually to recognize individuals who have responded promptly to sudden cardiac arrest events and saved lives through CPR. The ceremony, held in a beautiful theatre, aims to promote community involvement in cardiac arrest management and strengthen the idea that a system can save lives. Over 600 people have been recognized so far. Since 2019, psychological support is also offered free of charge to FRs who may require it following a resuscitation.
Inclusion of AED
During the pilot implementation of the EVapp system, experience showed that the governmental registration of available AEDs was incomplete and contained errors. It was attempted to maximally increase the availability of AED (by, for example, providing an outdoor mounting box), which is preferred over investments into new devices. Through increased awareness, guidance, follow-up and collaboration with the local governments and private partners, the EVapp AED database remains up to date. The EVapp system guides placement of AEDs based on the factors of maximal radius of coverage of 1500 meters, minimal AED overlay and 24/7 public availability and is therefore a readily integrable and workable strategy. At the end of the pilot project, 22 AEDs and 340 FR were available, corresponding to 0.2 AED and 3.2 FR per square kilometre, thus allowing to meet the EVapp coverage criteria.
Fondazione Ticino Cuore owns and registers all AEDs in Canton Ticino, and lends them to individuals, corporations, and institutions. AED details such as coordinates, location, and availability are recorded. OHCA events are categorized into urban and rural areas based on population and population density. Canton Ticino has 6 urban and 125 rural municipalities. AEDs provide 23% coverage for all OHCA events and 15% coverage for public OHCA events. Coverage is higher in urban areas than in rural areas.18 The current version of the application prioritizes the FRs to deliver CPR rather than the AED retrieval; however, each FR may discretionally choose to retrieve an AED.19
Roadmap to implementing effective FR system
To effectively build a community network of FR, a roadmap was created based on experience from Belgium and Switzerland, considering the process of active implementation frameworks.16 Key strategies for implementation consist of 4 main steps (Fig. 4). Exploration involves assessing existing “black spots” in fast EMS response, consultations with national legislation- and advisory bodies and preparing installation via local steering committees. Effective installation requires involvement of local drivers (recruitment of FR, involvement of specific professional groups (e.g. police officers), registration of PAD), developing readiness by financing and campaigning, and developing fidelity measures. In initial implementation, these steps are repeated, leading to further improvement, increased capacity and validation of the system via fidelity measures (using e.g. previously developed feedback forms). After implementation at sufficient scale, the improved outcome (i.e. increased survival to hospital discharge, or gain in quality adjusted life years20 can be more reliably calculated, advancing to the next technology readiness level.21 The system is then sufficiently mature for vast embedment in policy or legislation. It is crucial to perform analysis before and after each improvement cycle.
Fig. 4.
Roadmap for FR networks. AED, automatic External Defibrillator; CPR, Cardiopulmonary Resuscitation; EMS, Emergency Medical Services; OHCA, out-of-hospital cardiac arrest; TRL, Technology Readiness Level;. QALY, quality-adjusted life years. Created with BioRender.com. Figure based on Blanchard et al. (2017) (2). Caputo et al. (2017) (15).
Discussion
The proposed roadmap for establishing FR networks includes four steps: exploration (understanding national legislation and forming committees), installation (recruiting FRs, involving professional groups, and registering AEDs), initiation (implementing improvement cycles and fidelity measures), and implementation (network expansion and legislative integration). The psychological wellbeing of FR must be prioritized. The incidence of significant prolonged. Geo-mapping for optimal AED placement and FR task allocation is highly recommended.
In 2022, main challenges are AED accessibility, meaning AED proximity to the OHCA, bystanders’ awareness and willingness to use nearby AEDs.28 Different strategies have been evaluated for the most optimal AED placement. American Heart Association and ERC guidelines recommended AED placement in locations with a “relatively high likelihood of witnessed cardiac arrest” or “in public places with a high density and movement of citizens, where cardiac arrests are usually witnessed”, respectively.22, 23, 24 Studies have demonstrated that OHCA are distributed in clusters, which remain relatively stable over the years, rendering these locations suitable candidates for the placement of AEDs, predictive of future OHCAs.25, 26, 27 However, most OHCA have appeared to occur randomly in areas with low population density, such as residential locations.1, 25 A recent study from the Netherlands recommended a density of ≥2 AEDS and ≥10 FR per square kilometre to achieve bystander defibrillation in ≤6 minutes in residential areas.28 Rather than actual GPS-based location and guidance, a text message alert based on static data of the volunteers was used (home and work addresses). Optimisation models have increased AED coverage with relative gains of up to 50–95%, relocating AED based on historical OHCA, 24/7 availability, adjacent AED proximity and predetermining the roundtrip distance individuals may travel within a predetermined time.24, 29 Both EVapp and the Ticino Cuore app localise FR based on their actual GPS-based coordinates and guides them to the AED and victim via their preferred navigation app. In Ticino, the vast majority (85%) of FRs reached the OHCA victim by car or by bicycle.19 Extensive travel guidance and the fact that responders may feasibly travel faster than walking speed, eventually by other travel modalities, or via (unmapped) short-cuts30 may account for the acceptance of prolonged distances. Ticino Cuore app prioritizes the FRs to deliver CPR rather than the AED retrieval; however, each FR may discretionally choose to retrieve an AED.
Previous research has shown that CPR experience increases the likelihood of providing care after an alert.31, 32.The incidence of significant prolonged adverse effects on FRs is likely to be low,32, 33, 34, 35, 36 yet, FR have highlighted the psychologically challenging situations and the importance of well-being. Debriefing by the EMS personnel should indeed be available to bystanders following a resuscitation attempt,37 as it was frequently employed as a coping strategy.31
Several limitations are considered in this paper. Firstly, the study's scope is concentrated on European settings, limiting the global applicability of the findings. Secondly, the primary source of data used in developing the roadmap stems from experiential insights, which can be further confirmed using systematic empirical research from other FR networks. Finally, although the roadmap proposed in this study has undergone rigorous stress testing over more than 5 years, it is limited to the two included FR networks. Further research is required to validate the roadmap in different global contexts.
Conclusions
The importance of FR networks is increasingly recognized, and various systems are being developed. Experiences and key strategies of EVapp in Belgium and the Ticino Cuore app in Switzerland may serve as a roadmap for other systems’ implementations within Europe and beyond.
Compliance with ethical standards
The Emergency Volunteer Application (EVapp) project was accepted as a test project in 2016 by the National Council of Emergency Medical Care in Belgium (NRDGH), within the Federal government of Belgium. A first test project was started in March 2017 in the city of Hoogstraten. The design of the application was in coherence with the Belgian Privacy Commission and due to National Council approval, including an ethics section, did not require ethical committee approval on local institution level.
In Swiss Canton Ticino a network was developed without a specific Ethics approval. Ticino Cuore Foundation as non-profit organization was commissioned for creation of the local first responders network by the Local EMS Service and Hospital Institutions (including an ethical section). Moreover, the creation and management of a first responder network did not require specific authorization under applicable laws.
Author contribution
Data analysis planning and methodology: Esther Moens, Eva Degraeuwe, Thomas Tackaert, Robin Arys, Steven Vercammen, Maria Luce Caputo, Cresta Ruggero. Analysis and results interpretation: Esther Moens, Eva Degraeuwe, Steven Vercammen, Maria Luce Caputo. Writing—original draft preparation: Esther Moens, Eva Degraeuwe, Maria Luce Caputo. Writing—review and editing: Esther Moens, Eva Degraeuwe, Caputo Maria Luce, Cresta Ruggero, Robin Arys, Nina Van Moorter, Angelo Auricchio, Claudio Benvenuti, Robin Arys, Thomas Tackaert, Steven Vercammen.
CRediT authorship contribution statement
Esther Moens: Methodology, Writing – original draft, Writing – review & editing. Eva Degraeuwe: Methodology, Writing – original draft, Writing – review & editing. Luce Caputo Maria: Methodology, Writing – original draft, Writing – review & editing. Ruggero Cresta: Methodology, Writing – review & editing. Robin Arys: Methodology, Writing – review & editing. Nina Van Moorter: Writing – review & editing. Thomas Tackaert: Methodology, Writing – review & editing. Claudio Benvenuti: Writing – review & editing. Angelo Auricchio: Writing – review & editing. Steven Vercammen: Methodology, Writing – review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Due to the content of this manuscript, all authors are directly or indirectly associated with the first responder networks, EVapp and Ticino Cuore respectively.
Acknowledgements
The authors wish to acknowledge the support of the steering group of EVapp in Belgium for innovating and supporting the implementation of the EVapp lay responder system. We would like to thank all the first responders for their contribution to the EVapp Network.
Ticino Cuore wishes to thank all first responders and Emergency Medical Services (EMS) staff for their contribution.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100469.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Gräsner J., Lefering R., Koster R.W., Masterson S., Böttiger B.W., Herlitz J., et al. EuReCa one 27 Nations, one Europe, one registry. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Gräsner J.T., Wnent J., Herlitz J., Perkins G.D., Lefering R., Tjelmeland I., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/J.RESUSCITATION.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 3.Valenzuela T.D., Roe D.J., Nichol G., Clark L.L., Spaite D.W., Hardman R.G. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 4.Hasselqvist-Ax I., Riva G., Herlitz J., Rosenqvist M., Hollenberg J., Nordberg P., et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 5.Mauri R., Burkart R., Benvenuti C., Caputo M.L., Moccetti T., Del Bufalo A., et al. Better management of out-of-hospital cardiac arrest increases survival rate and improves neurological outcome in the Swiss Canton Ticino. Europace. 2016;18:398–404. doi: 10.1093/EUROPACE/EUV218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pell J.P., Sirel J.M., Marsden A.K., Ford I., Cobbe S.M. Effect of reducing ambulance response times on deaths from out of hospital cardiac arrest: Cohort study. Br Med J. 2001;322:1385–1388. doi: 10.1136/bmj.322.7299.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Keeffe C., Nicholl J., Turner J., Goodacre S. Role of ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emerg Med J. 2011;28:703–706. doi: 10.1136/emj.2009.086363. [DOI] [PubMed] [Google Scholar]
- 8.Scquizzato T., Belloni O., Semeraro F., Greif R., Metelmann C., Landoni G., et al. Dispatching citizens as first responders to out-of-hospital cardiac arrests: a systematic review and meta-analysis. Eur J Emerg Med. 2022;29:163–172. doi: 10.1097/MEJ.0000000000000915. [DOI] [PubMed] [Google Scholar]
- 9.Holmberg M.J., Vognsen M., Andersen M.S., Donnino M.W., Andersen L.W. Bystander automated external defibrillator use and clinical outcomes after out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2017;120:77–87. doi: 10.1016/j.resuscitation.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Semeraro F., Greif R., Böttiger B.W., Burkart R., Cimpoesu D., Georgiou M., et al. European resuscitation council guidelines 2021: systems saving lives. Resuscitation. 2021;161:80–97. doi: 10.1016/J.RESUSCITATION.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Greif R., Bhanji F., Bigham B.L., Bray J., Breckwoldt J., Cheng A., et al. Education, implementation, and teams: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A188–A239. doi: 10.1016/J.RESUSCITATION.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Berg K.M., Cheng A., Panchal A.R., Topjian A.A., Aziz K., Bhanji F., et al. Part 7: Systems of care: 2020 American Heart association guidelines for cardiopulmonary resuscitation and emergency CARDIOVASCULAR care. Circulation. 2020;142:S580–S604. doi: 10.1161/CIR.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 13.Van Brabandt H., Gerkens S., Fairon N., Dubois C., Van Der Auwera M., Vansimpsen C., et al. Static automated external defibrillators for opportunistic use by bystanders: health technology assessment. Belgian Heal Care Knowl Centr. 2017:81. [Google Scholar]
- 14.Vercammen S., Moens E. Cost-effectiveness of a novel smartphone application to mobilize first responders after witnessed OHCA in Belgium. Cost Eff Resour Alloc. 2020;18:1–11. doi: 10.1186/S12962-020-00248-2/TABLES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caputo M.L., Muschietti S., Burkart R., Benvenuti C., Conte G., Regoli F., et al. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: A comparison with SMS-based system notification. Resuscitation. 2017;114:73–78. doi: 10.1016/J.RESUSCITATION.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Blanchard C., Livet M., Ward C., Sorge L., Sorensen T.D., McClurg M.R. The active implementation frameworks: A roadmap for advancing implementation of comprehensive medication management in primary care. Res Soc Adm Pharm. 2017;13:922–929. doi: 10.1016/J.SAPHARM.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Home - Fondazione Ticino Cuore n.d. https://www.ticinocuore.ch/it (accessed March 20, 2023).
- 18.Tierney N.J., Reinhold H.J., Mira A., Weiser M., Burkart R., Benvenuti C., et al. Novel relocation methods for automatic external defibrillator improve out-of-hospital cardiac arrest coverage under limited resources. Resuscitation. 2018;125:83–89. doi: 10.1016/J.RESUSCITATION.2018.01.055. [DOI] [PubMed] [Google Scholar]
- 19.Auricchio A., Gianquintieri L., Burkart R., Benvenuti C., Muschietti S., Peluso S., et al. Real-life time and distance covered by lay first responders alerted by means of smartphone-application: Implications for early initiation of cardiopulmonary resuscitation and access to automatic external defibrillators. Resuscitation. 2019;141:182–187. doi: 10.1016/j.resuscitation.2019.05.023. [DOI] [PubMed] [Google Scholar]
- 20.Bush J.W., Fanshel S., Chen M.M. Analysis of a tuberculin testing program using a health status index. Socioecon Plann Sci. 1972;6:49–68. doi: 10.1016/0038-0121(72)90006-7. [DOI] [Google Scholar]
- 21.Altunok T., Cakmak T. A technology readiness levels (TRLs) calculator software for systems engineering and technology management tool. Adv Eng Softw. 2010;41:769–778. doi: 10.1016/J.ADVENGSOFT.2009.12.018. [DOI] [Google Scholar]
- 22.Kronick S.L., Kurz M.C., Lin S., Edelson D.P., Berg R.A., Billi J.E., et al. Part 4: systems of care and continuous quality improvement. Circulation. 2015;132:S397–S413. doi: 10.1161/CIR.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 23.Perkins G.D., Handley A.J., Koster R.W., Castren M.S.M., Olasveengen T., et al. European Resuscitation Council guidelines for resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 24.Sun C.L.F., Karlsson L., Morrison L.J., Brooks S.C., Folke F., Chan T.C.Y. Effect of optimized versus guidelines-based automated external defibrillator placement on out-of-hospital cardiac arrest coverage: An in silico trial. J Am Heart Assoc. 2020;9:e016701. doi: 10.1161/JAHA.120.016701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aeby D., Staeger P., Dami F. How to improve automated external defibrillator placement for out-of-hospital cardiac arrests: A case study. PLoS One. 2021;16 doi: 10.1371/JOURNAL.PONE.0250591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sasson C., Keirns C.C., Smith D., Sayre M., Macy M., Meurer W., et al. Small area variations in out-of-hospital cardiac arrest: Does the neighborhood matter? Ann Intern Med. 2010;153:19. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lerner E.B., Fairbanks R.J., Shah M.N. Identification of out-of-hospital cardiac arrest clusters using a geographic information system. Acad Emerg Med. 2005;12:81–84. doi: 10.1197/J.AEM.2004.08.044. [DOI] [PubMed] [Google Scholar]
- 28.Stieglis R., Zijlstra J.A., Riedijk F., Smeekes M., van der Worp W.E., Koster R.W. AED and text message responders density in residential areas for rapid response in out-of-hospital cardiac arrest. Resuscitation. 2020;150:170–177. doi: 10.1016/J.RESUSCITATION.2020.01.031. [DOI] [PubMed] [Google Scholar]
- 29.Sun C.L.F., Karlsson L., Torp-Pedersen C., Morrison L.J., Brooks S.C., Folke F., et al. In silico trial of optimized versus actual public defibrillator locations. J Am Coll Cardiol. 2019;74:1557–1567. doi: 10.1016/J.JACC.2019.06.075. [DOI] [PubMed] [Google Scholar]
- 30.Smith C.M., Lall R., Spaight R., Fothergill R.T., Brown T., Perkins G.D. Calculating real-world travel routes instead of straight-line distance in the community response to out-of-hospital cardiac arrest. Resusc Plus. 2021;8:100176. doi: 10.1016/J.RESPLU.2021.100176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matsuyama T., Scapigliati A., Pellis T., Greif R., Iwami T. Willingness to perform bystander cardiopulmonary resuscitation: A scoping review. Resusc Plus. 2020;4:100043. doi: 10.1016/J.RESPLU.2020.100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haskins B., Nehme Z., Dicker B., Wilson M.H., Ray M., Bernard S., et al. A binational survey of smartphone activated volunteer responders for out-of-hospital cardiac arrest: Availability, interventions, and post-traumatic stress. Resuscitation. 2021;169:67–75. doi: 10.1016/J.RESUSCITATION.2021.10.030. [DOI] [PubMed] [Google Scholar]
- 33.Zijlstra J.A., Beesems S.G., De Haan R.J., Koster R.W. Psychological impact on dispatched local lay rescuers performing bystander cardiopulmonary resuscitation. Resuscitation. 2015;92:115–121. doi: 10.1016/J.RESUSCITATION.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 34.Peberdy M.A., Van O.L., Groh W.J., Hedges J., Terndrup T.E., Pirrallo R.G., et al. Adverse events associated with lay emergency response programs: The public access defibrillation trial experience. Resuscitation. 2006;70:59–65. doi: 10.1016/J.RESUSCITATION.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 35.Riegel B., Mosesso V.N., Birnbaum A., Bosken L., Evans L.M., Feeny D., et al. Stress reactions and perceived difficulties of lay responders to a medical emergency. Resuscitation. 2006;70:98–106. doi: 10.1016/J.RESUSCITATION.2005.10.029. [DOI] [PubMed] [Google Scholar]
- 36.Axelsson Å., Herlitz J., Ekström L., Holmberg S. Bystander-initiated cardiopulmonary resuscitation out-of-hospital. A first description of the bystanders and their experiences. Resuscitation. 1996;33:3–11. doi: 10.1016/S0300-9572(96)00993-8. [DOI] [PubMed] [Google Scholar]
- 37.Axelsson Å., Herlitz J., Karlsson T., Lindqvist J., Reid Graves J., Ekström L., et al. Factors surrounding cardiopulmonary resuscitation influencing bystanders’ psychological reactions. Resuscitation. 1998;37:13–20. doi: 10.1016/S0300-9572(98)00027-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.