Abstract
Study design
Technical note.
Purpose
To provide a technical description of the placement of Gardner-Wells tongs and the performance of awake cranio-cervical traction to reduce AO type C injuries of the sub-axial cervical spine with Gardner-Wells tongs.
Methods
In this technical note, the authors present the indications, the contraindications, the pull-out of the pins, a detailed description of the technique for its proper placement, traction reduction technique, reduction maneuvers, complications and post-reduction care.
Results
Awake reduction of AO type C injuries of the sub-axial cervical spine can be successfully performed using Gardner-Wells tongs.
Conclusions
There is sufficient evidence to recommend the use of cranio-cervical traction in these vertebral injuries; however, we lack a detailed technical note to guide its proper placement.
Keywords: Gardner-Wells tongs, Closed reduction, Sub-axial cervical, Fracture, Dislocation
Introduction
Spinal cord injuries of the sub-axial cervical spine are clinical entities with fatal or devastating outcomes for the patient; of those who survive, up to 87 % are expected to present tetraplegia. Therefore, immediate and adequate medical attention has a directly proportional impact on a more favorable prognosis [1].
Since the first description by Crutchfield in 1933, cranio-cervical traction has been part of the treatment of fractures and/or dislocations of the sub-axial cervical spine in many hospitals around the world [2]. In order to carry it out, different devices [tweezers] or their modifications have been used [[2], [3], [4], [5], [6]]. Their proper use allows reduction, neurological decompression, temporary stabilization and immediate alignment with the patient awake.
In 1973, Gardner published his own design and recommendations [3]; this design was initially made of steel. Today we have tweezers made of polymers and titanium pins compatible with the magnetic resonator [7]. (Fig. 1).
Fig. 1.

Polycarbonate tong and titanium pins, compatible with the magnetic resonator.
In our clinic, we use Gardner-Wells tongs since they are easy to place and handle.
We describe the indications, contraindications, resistance to untethering, placement technique, reduction technique with traction, closed reduction maneuvers, complications, and post-reduction care.
Indications
Sub-axial cervical fracture-dislocation [8].
Unilateral or bilateral pure facet dislocations [9].
Cervical spondyloptosis [10].
Contraindications
-
1.
Skull fracture [11].
-
2.
Lesions of more than two weeks [12].
-
3.
Post-traumatic disc herniation (relative contraindication*) [13,14].
-
4.
Patient unable to communicate clinical changes verbally.
*According to Onishi et al., the presence of post-traumatic disc herniation is not an absolute contraindication in facet dislocations, since neurological deterioration after reduction is a highly unlikely event. Vieira et al. also reinforce this statement by finding only 1 % probability of neurological deterioration.
Pull-off
According to Krag et al., pin pull-off determined in cadavers is 137 ± 34 pounds (610 ± 151 N) when the tongs are placed according to the manufacturer's recommendations [15].
On the other hand, Blumberg et al. point out that there is a statistically significant difference in the pull-off depending on the material of the pins (steel versus titanium alloy). It was demonstrated in cadavers that steel pins fail on average at a load of 225 pounds (range 160–250 pounds), while titanium alloy pins fail on average at a load of 75 pounds (range 60–100 pounds). In the case of steel pins, failure is due to skull fracture; and in the case of titanium alloy pins, failure is due to bending of the tip of the pin [16].
Lerman et al. [17] emphasize the difference in pull-off when new, little used (<12 uses) or heavily used (>36 uses) steel pins are utilized in a cadaveric model, modifying the bone-pin interface with a fiberglass-filled acetal copolymer to simulate the bone-pin interface on a fresh cadaver. He found statistically significant differences (p < 0.05) for the new tongs [233 ± 49 pounds] compared with the rarely used and the heavily used ones (185 ± 40 pounds and 109 ± 10 pounds, respectively).
Placement technique
Prior to its placement, we must have the written consent of the patient and their family in order for the procedure to be performed. A central venous access for medication use, for example, the use of amines in order to maintain average arterial pressure and perfusion of the spinal cord of at least 90 mmHg is also necessary.
Trichotomy and antisepsis should be performed in the pin placement area as suggested in the Fig. 2 (pink area).
Fig. 2.
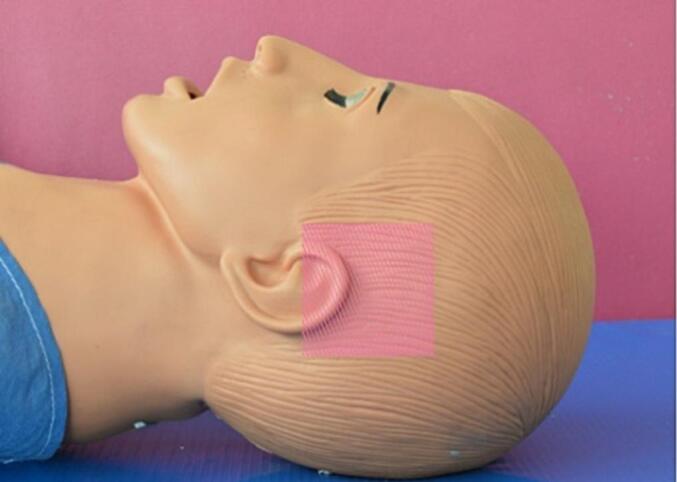
Pin placement area suggested is marked in pink. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
The scalp block or local infiltration plus the use of intravenous muscle relaxants ensures better patient cooperation, prevents the hemodynamic response to the pressure exerted by the pins, decreases anxiety, and relaxes neck muscles in order to get a traction with better chances of success. Scalp block is recommended instead of local infiltration as the anesthetic effect is longer. It has been studied in patients undergoing craniotomy that during the application of the pins and the incision there is an increase in the systemic arterial pressure, intracranial pressure and tachycardia [18]. One of the main advantages of performing a scalp block is that most of the nerves that innervate the scalp are superficial terminal sensory branches and, therefore, the risk of nerve damage is lower than that of the deeper motor nerves [18].
Anesthetic doses in Table 1.
Table 1.
Medications and doses for scalp block or local infiltration for an adult patient weighing 70 kg [19].
| Medication | Dose |
|---|---|
| Scalp block | |
| Lidocaine 1 % without epinephrine | 50–200 mg (5–20 ml) |
| Bupivacaine 0.25–0.5 % | 12.5–100 mg (5–20 ml) |
| Ropivacaine 0.2–0.5 % | 10–100 mg (5–20 ml) |
| Local infiltration | |
| Lidocaine 1 % | Maximum dose 300 mg |
| Bupivacaine 0.25–0.5 % | Maximum dose 175 mg |
| Ropivacaine 0.5–0.5 % | Maximum dose 200 mg |
| Muscle relaxants [20] | |
| Midazolam | 2.5 mg initial bolus. Increments of 0.5–1 mg until the desired degree of sedation are obtained. |
| Diazepam | 2 mg in similar increments until the desired degree of sedation is obtained. |
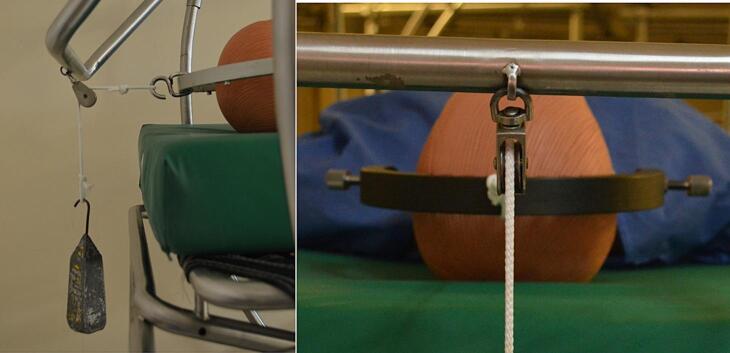
A pulley system should preferably be integrated into the patient's bed. The spot to anchor the pins is 1 cm above the pinna, at the level of the external auditory canal (Fig. 3).
Fig. 3.
A and B, dummy with tongs in place and traction with pulley and weight. In our clinic, we use circoelectric beds that have integrated pulleys to place the traction system; C, detail of the pin placement is observed: 1 cm above the upper edge of the pinna and at the level of the external auditory canal.
Preferably, the physician in charge should hold the tongs at the indicated level, while an assistant rotates the pins simultaneously and symmetrically until only the external table of the temporal bone has been perforated, observing the indicator stem protrude 1 mm; thus, ensuring proper pressure of 139 pounds, enough to perforate the external table of the temporal bone (Fig. 4).
Fig. 4.
A. Pin without load (there is no stem protrusion); B. Loaded pin (stem protrudes 1 mm).
Once in place, you must make sure the traction does not show any point of contact along its entire length since this may affect its proper functioning. The tongs must remain parallel to the horizontal plane so as to keep a physiological alignment of the spine (Fig. 5).
Fig. 5.
A, pulley traction detail: there should be no obstacles preventing adequate weight loading; B, top view of tongs in place: should be parallel to the horizontal plane.
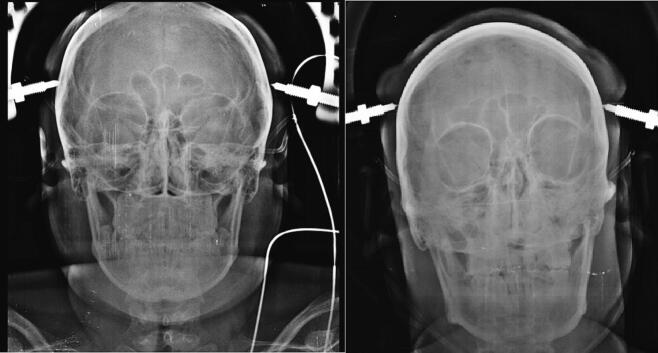
AP and lateral skull radiographs should be taken in order to confirm proper positioning and repositioning if necessary (Fig. 6, Fig. 7, Fig. 8).
Fig. 6.
Correct placement: A, symmetrical height and both pins only penetrated the external table of the temporal bone, B, placement at the level of the external auditory canal.
Fig. 7.
A. The left pin did not penetrate the outer part; B. In this case, no pin penetrated the external table and its placement is asymmetric in the coronal plane.
Fig. 8.
A, AP radiograph of the skull showing that the right pin violates the internal table of the temporal bone. B and C, simple CT scan of the skull in coronal and axial views of patient A, who required immediate repositioning and conservative handling of the temporal bone injury; he did not show neurological deterioration nor neuroinfection due to this event. The CSF fistula closed spontaneously without complications.
Reduction technique with traction
It is performed with the patient awake, sedated, conscious and capable of reporting clinical changes during traction. This has the advantage of having an immediate assessment of clinical changes to conduct the procedure safely, unlike performing it on a patient under general anesthesia; as a disadvantage, we can mention the patient's anxiety and muscle resistance, which make the reduction difficult.
As essential, we can list: the continuous monitoring of vital signs, the clinical examination (sensory and motor level according to ASIA) and radiographic evaluation, having to take controls in lateral view every 20 min during the traction process to detect the changes that help reduce the weight or immediate suspension of traction (Table 2).
Table 2.
Criteria for reducing weight or suspending traction immediately.
| Changes in vital signs monitor | Bradycardia, hypotension, cardiac rhythm disturbances (supraventricular tachycardia, longer duration of RR and QT intervals and QRS complex) [21]. |
| Clinical changes | Neurological level progression according to the ASIA scale (neurological deterioration). |
| Radiographic changes | Interbody spacer > 5 mm. |
The initial weight for traction, increase, maximum weights, criteria for suspending traction, time of sustained traction, and weight after reduction vary among different authors [11,12,[22], [23], [24], [25], [26], [27], [28], [29]]. Below are the parameters used at the Spine Clinic of the Ministry of Health in Mexico City “Dr. Manuel Dufoo Olvera” (Table 3).
Table 3.
Parameters used for craniocervical traction.
| Starting weight | 5 kg + 2.5 kg per level below C1. |
| Increased weight | 2.5 kg every 20 min. |
| Maximum weight | 50 % patient weight for 1 h traction |
| Criteria for suspending traction | Satisfactory reduction, maximum weight for 1 h without reduction, neurological deterioration or overdistraction of interbody space >5 mm, bradycardia, hypotension, supraventricular tachycardia, longer duration of RR and QT intervals and QRS complex. |
| Weight after reduction | 5 kg. |
Closed reduction maneuvers
Closed reduction maneuvers are recommended in cases where maximum weight and time traction do not decline; they should be performed only if the facets are distracted or in a tip-to-tip position [30]. An assistant is needed to hold the patient's body against traction.
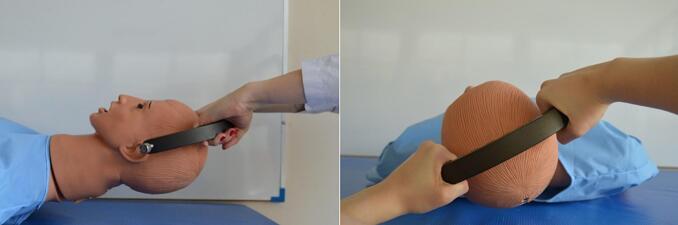
Unilateral dislocation: while traction is maintained (it can be done with flexion), the head is rotated 30° to 40° towards the dislocated side, it should be done only if there is no resistance; otherwise, the facet may be fractured and cause neurological deterioration. On a successful maneuver, a pop may be felt or heard (Fig. 9).
Fig. 9.
A. Flexion is recommended while maintaining traction to facilitate reduction. B. Simultaneously rotate the head 30° to 40° towards the dislocated side.
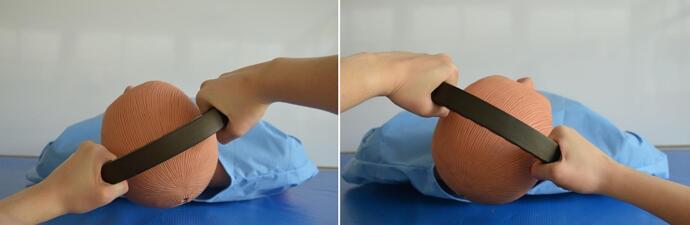
Bilateral dislocation: while maintaining traction (this can be done with flexion), the head is rotated 30° to 45° to one side, gently returned to midline, and rotation continues 30° to 45° to the other side and back to midline (Fig. 10).
Fig. 10.
Maintaining axial traction and flexion, the head is turned to one side 30° to 45° and then to the other side.
Once reduced, it should be kept in extension and a pillow placed under the shoulders to maintain the reduction and leave 5 kg traction on the tongs.
Complications
The complications associated with the placement of Gardner-Wells tongs reported in literature are very varied and relatively frequent; among these, we find the following:
Loosening of the pins, up to 19 % of the cases. It is a tendency of the surgeon to apply less force than recommended by the manufacturer, probably due to the fear of perforating the inner table of the skull [31].
On the other hand, there is the perforation of the inner table of the skull, these cases report having been treated with antibiotics for up to 30 days; some patients do not show any neurological symptoms even in the long term and others show acute neurological deficit, and central nervous system infections [32].
Another reported complication is a cerebral abscess (0.4–0.7 %), this usually occurs as a consequence of a superficial infection that extends through the pin. The most frequently isolated etiological agent is Staphylococcus aureus, which usually requires a craniotomy and the evacuation of the abscess as well as intravenous antibiotic administration for several weeks [33].
We can also find local infections, sixth cranial nerve palsy, pin slip (18.8 %), asymmetric placement (12.5 %), cellulitis of the scalp (6.3 %), superficial temporal artery laceration [34].
Conclusions
Awake craniocervical traction with Gardner-Wells tongs for closed reduction of fracture-dislocation of the sub-axial cervical spine under safety measures, control and adequate preparation results in a useful procedure with successful results, especially in hospitals with limited access to reduction open immediately. This work aims to serve as a guide for the correct placement of the tongs and closed reduction of these vertebral injuries, since we lack a detailed technical note in this regard.
Declaration of competing interest
The authors declare that there are no conflicts of interest related to the material included in this paper.
References
- 1.Quarrington R.D., Jones C.F., Tcherveniakov P., Clark J.M., Sandler S.J.I., Lee, et al. Traumatic subaxial cervical facet subluxation and dislocation: epidemiology, radiographic analyses, and risk factors for spinal cord injury. Spine J. Off. J. N. Am. Spine Soc. 2018;18(3):387–398. doi: 10.1016/j.spinee.2017.07.175. [DOI] [PubMed] [Google Scholar]
- 2.Crutchfield W.G. Skeletal traction in treatment of injuries to the cervical spine. JAMA. 1954;155(1):29–32. doi: 10.1001/jama.1954.03690190035010. [DOI] [PubMed] [Google Scholar]
- 3.Gardner W.J. The principle of spring-loaded points for cervical traction. Technical note. J. Neurosurgery. 1973;39(4):543–544. doi: 10.3171/jns.1973.39.4.0543. [DOI] [PubMed] [Google Scholar]
- 4.Parney I.F., Allen P.B., Petruk K.C., Howard H. Hepburn and the development of skull tongs for cervical spine traction. Neurosurgery. 2000;47(6):1430–1433. [PubMed] [Google Scholar]
- 5.Crutchfield W.G. Redesigned crutchfield skull tongs. Technical note describing the combined “squeeze” and “hook” principle. J. Neurosurg. 1966;25(6):656–657. doi: 10.3171/jns.1966.25.6.0656. [DOI] [PubMed] [Google Scholar]
- 6.Odebode T.O., Agaja S.B. Odebode-Agaja adult cervical traction device. Trop. Doct. 2011;41(1):21–22. doi: 10.1258/td.2010.100277. [DOI] [PubMed] [Google Scholar]
- 7.Blumberg K.D., Catalano J.B., Cotler J.M., Balderston R.A. The pullout strength of titanium alloy MRI-compatible and stainless steel MRI-incompatible Gardner-Wells tongs. Spine. 1993;18(13):1895–1896. doi: 10.1097/00007632-199310000-00029. [DOI] [PubMed] [Google Scholar]
- 8.Khelifa A., Berchiche L., Aichaoui F., Lagha N., Asfirane N., Morsli A. Traumatic cervical spine spondyloptosis: a systematic review. J. Craniovertebral Junction Spine. 2022;13(1):9–16. doi: 10.4103/jcvjs.jcvjs_132_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sousa A., Rodrigues C., Marques M., Amorim-Barbosa T., Rodrigues-Pinto R. Awake cranial traction and isolated anterior cervical discectomy and fusion in the treatment of traumatic subaxial cervical facet joint dislocations: analysis of a cohort of 70 patients and predictors of surgical failure. Int. J. Spine Surg. 2022;16(2):256–263. doi: 10.14444/8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padwal A., Shukla D., Bhat D.I., Somanna S., Devi B.I. Post-traumatic cervical spondyloptosis: a rare entity with multiple management options. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australasia. 2016;28:61–66. doi: 10.1016/j.jocn.2015.05.074. [DOI] [PubMed] [Google Scholar]
- 11.Darsaut T.E., Ashforth R., Bhargava R., Broad R., Emery D., Kortbeek F., et al. A pilot study of magnetic resonance imaging-guided closed reduction of cervical spine fractures. Spine. 2006;31(18):2085–2090. doi: 10.1097/01.brs.0000232166.63025.68. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor P.A., McCormack O., Noël J., McCormack D., O’Byrne J. Anterior displacement correlates with neurological impairment in cervical facet dislocations. Int. Orthop. 2003;27(3):190–193. doi: 10.1007/s00264-003-0449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Onishi F.J., Daniel J.W., Joaquim A.F., Evangelista A.C., de Freitas Bertolini E., Dantas F.R., et al. The impact of traumatic herniated discs in cervical facets dislocations treatments: systematic review and meta-analysis. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Section Cervical Spine Res. Soc. 2022;31(10):2664–2674. doi: 10.1007/s00586-022-07290-z. [DOI] [PubMed] [Google Scholar]
- 14.Botelho R.V., de Freitas Bertolini E., Barcelos A.C.E.S., Walter Daniel J., Fernandes Joaquim A., Dantas F.L.R., et al. The surgical treatment of subaxial acute cervical spine facet dislocations in adults: a systematic review and meta-analysis. Neurosurg. Rev. 2022;45(4):2659–2669. doi: 10.1007/s10143-022-01808-1. [DOI] [PubMed] [Google Scholar]
- 15.Krag M.H., Byrt W., Pope M. Pull-off strength of Gardner-Wells tongs from cadaveric crania. Spine. 1989;14(3):247–250. doi: 10.1097/00007632-198903000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Blumberg K.D., Catalano J.B., Cotler J.M., Balderston R.A. The pullout strength of titanium alloy MRI-compatible and stainless steel MRI-incompatible Gardner-Wells tongs. Spine. 1993;18(13):1895–1896. doi: 10.1097/00007632-199310000-00029. [DOI] [PubMed] [Google Scholar]
- 17.Lerman J.A., Haynes R.J., Koeneman E.J., Koeneman J.B., Wong W.B. A biomechanical comparison of Gardner-Wells tongs and halo device used for cervical spine traction. Spine. 1994;19(21):2403–2406. doi: 10.1097/00007632-199411000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Osborn I., Sebeo J. “Scalp block” during craniotomy: a classic technique revisited. J. Neurosurg. Anesthesiol. 2010;22(3):187–194. doi: 10.1097/ANA.0b013e3181d48846. [DOI] [PubMed] [Google Scholar]
- 19.Thiele Eryn L., Nemergut Edward C. 9th ed. Churchill Livingstone; Philadelphia: 2020. Miller’s Anesthesia. (Anesthesia & Analgesia). Book: [Google Scholar]
- 20.Reves J.G., Glass P., Lubarsky D.A. In: Miller’s Anesthesia. 7th ed. Miller R.D., Eriksson L.I., Fleischer L.A., et al., editors. Churchill Livingstone; Philadelphia: 2010. Intravenous anesthetics; pp. 719–768. Book: [Google Scholar]
- 21.Biering-Sørensen F., Biering-Sørensen T., Liu N., Malmqvist L., Wecht J.M., Krassioukov A. Alterations in cardiac autonomic control in spinal cord injury. Auton. Neurosci. Basic Clin. 2018;209:4–18. doi: 10.1016/j.autneu.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Storey R.N., Singhal R., Inglis T., Kieser D., Schouten R. Urgent closed reduction of the dislocated cervical spine in New Zealand. ANZ J. Surg. 2018;88(1–2):56–61. doi: 10.1111/ans.14231. [DOI] [PubMed] [Google Scholar]
- 23.López Ozcar Felipe García. Tratamiento de la luxación cervical mediante reducción cerrada segmento inferior (C-3 a C-7) (Uso del halo cefálico y tenazas de tracción) Medigraphics. 2007;3(3) Ortho-tips. [Google Scholar]
- 24.Eranki V., Koul K., Mendz G., Dillon D. Traumatic facet joint dislocation in Western Australia. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Section Cervical Spine Res. Soc. 2016;25(4):1109–1116. doi: 10.1007/s00586-014-3627-x. [DOI] [PubMed] [Google Scholar]
- 25.Newton D., England M., Doll H., Gardner B.P. The case for early treatment of dislocations of the cervical spine with cord involvement sustained playing rugby. J. Bone Joint Surg. 2011;93(12):1646–1652. doi: 10.1302/0301-620X.93B12.27048. British volume. [DOI] [PubMed] [Google Scholar]
- 26.Yu Z.S., Yue J.J., Wei F., Liu Z.J., Chen Z.Q., Dang G.T. Treatment of cervical dislocation with locked facets. Chin Med J (Engl) 2007;120(3):216–218. [PubMed] [Google Scholar]
- 27.Reindl R., Ouellet J., Harvey E.J., Berry G., Arlet V. Anterior reduction for cervical spine dislocation. Spine. 2006;31(6):648–652. doi: 10.1097/01.brs.0000202811.03476.a0. [DOI] [PubMed] [Google Scholar]
- 28.Greg Anderson D., Voets C., Ropiak R., Betcher J., Silber J.S., Daffner S., Cotler J.M., Vaccaro A.R. Analysis of patient variables affecting neurologic outcome after traumatic cervical facet dislocation. Spine J. Off. J. N. Am. Spine Soc. 2004;4(5):506–512. doi: 10.1016/j.spinee.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Papadopoulos S.M., Selden N.R., Quint D.J., Patel N., Gillespie B., Grube S. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J. Trauma. 2002;52(2):323–332. doi: 10.1097/00005373-200202000-00019. [DOI] [PubMed] [Google Scholar]
- 30.Cotler H.B., Miller L.S., DeLucia F.A., Cotler J.M., Davne S.H. Closed reduction of cervical spine dislocations. Clin. Orthop. Relat. Res. 1987;214:185–199. [PubMed] [Google Scholar]
- 31.Lerman J.A., Dickman C.A., Haynes R.J. Penetration of cranial inner table with Gardner-Wells tongs. J. Spinal Disord. 2001;14(3):211–213. doi: 10.1097/00002517-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Feldman R.A., Khayyat G.F. Perforation of the skull by a Gardner-Wells tong. Case report. J. Neurosurg. 1976;44(1):119–120. doi: 10.3171/jns.1976.44.1.0119. [DOI] [PubMed] [Google Scholar]
- 33.Gelalis I.D., Christoforou G., Motsis E., Arnaoutoglou C., Xenakis T. Brain abscess and generalized seizure caused by halo pin intracranial penetration: case report and review of the literature. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 2009;2(Suppl. 2):172–175. doi: 10.1007/s00586-008-0759-x. 2009; 18 Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saleh H., Yohe N., Razi A., Saleh A. Efficacy and complications of the use of Gardner-Wells Tongs: a systematic review. J. Spine Surg. 2018;4(1):123–129. doi: 10.21037/jss.2018.03.03. Hong Kong. [DOI] [PMC free article] [PubMed] [Google Scholar]