Abstract
Background
There is a lack of data assessing the influence of respiratory therapist (RT) education on clinical outcomes. The primary objective of this study was to evaluate the impact of RTs holding advanced degrees or completing adult critical care competencies on discharge outcomes of patients with COVID-19 pneumonia.
Study Design and Methods
This retrospective, cross-sectional study included adults with confirmed COVID-19 admitted to the hospital for at least three days between March-May 2020. The academic degree held by each RT was considered advanced (baccalaureate or higher) or associate degree. Discharge outcomes were considered good, compromised, or poor when subjects’ hospital discharge was directly to home, long-term care facility/rehabilitation center, or hospice/died, respectively. A time-to-event multi-state regression model was used to determine the impact of RT academic degree and adult critical care competencies on discharge outcomes using α=0.05.
Results
A total of 260 subjects (median age 59 y; 166 males) received clinical care from 132 RTs. RT median professional experience was six y (IQR 3-11), 70.8% had an advanced degree, and 70.8% completed adult critical care competencies. The time-to-event multi-state regression model showed that patients with >85% exposure to RTs with advanced degrees transitioned 3.72 times more frequently to good outcomes than RTs without advanced degrees (p=.001). Similarly, patients with >85% exposure to RTs with adult critical care competencies transitioned 5.10 times more frequently to good outcomes than RTs without adult critical care competencies (p<.001).
Conclusion
Patients with COVID-19 pneumonia who received greater than 85% of their care by RTs who earned advanced degrees or completed adult critical care competencies had improved discharge outcomes. This preliminary work suggests that advancing education for the respiratory therapist workforce may improve the discharge quality of patients with acute respiratory failure and should be further explored.
Keywords: Respiratory therapist, baccalaureate degree, COVID-19, competencies, mortality, discharge outcome
Introduction
The coronavirus disease 2019 (COVID-19) pandemic stressed our healthcare system.1,2 During the pandemic’s initial phase, approximately 25-30% of patients developed acute respiratory distress syndrome (ARDS), requiring invasive mechanical ventilation (MV) and admission to the intensive care unit (ICU).3–5 ARDS carries a high mortality and morbidity rate with no definitive treatment.6 Lung protective MV, prone positioning, and the promotion of ventilator synchrony through sedation and paralytic agents improve ARDS outcomes, primarily by preventing further iatrogenic lung injury.7,8
Respiratory therapists (RTs) specialize in cardiopulmonary care and form a surveillance system to detect subtle changes in respiratory status.9,10 Most states in the United States require RTs to pass a credentialing exam to verify their ability to fulfill this specialized role. The National Board for Respiratory Care, which confers credentials, requires candidates to be graduates of an accredited education program. The accreditation standards for entry-level RT education programs require a minimum of an associate degree.11 In 2016, the American Association for Respiratory Care (AARC) revised a position statement to require new entry-level programs to award the baccalaureate degree.12 The Commission on Accreditation for Respiratory Care (CoARC) accreditation standards followed and specified a baccalaureate degree for new entry-level programs in 2018.13 Later, the AARC targeted 2030 as the date for an entry-level baccalaureate requirement citing the need for increased critical thinking skills, higher success rates of baccalaureate graduates on credentialing exams, and preferences from RT managers.13,14 However, beginning in January 2022, the CoARC reversed its earlier decision to require a baccalaureate degree for new entry-level programs to avoid the exacerbation of a workforce shortage. The CoARC also cited the lack of empirical evidence supporting advanced education for professional practice.15
The nursing profession explored how advanced education enhanced their professional practice through two decades of research across multiple care settings. Consistently positive results emerged when a greater percentage of nurses with baccalaureate degrees or higher provided care.16–23 To date, there is a lack of studies that suggests RTs with baccalaureate-level degrees affect patient results. The COVID-19 pandemic provided a natural experiment for evaluating how the academic degrees of RTs influenced discharge outcomes. Therefore, this study addressed whether RTs with advanced degrees affected the discharge outcomes and length of stay for patients with COVID-19 pneumonia requiring MV. A secondary aim addressed the role of RT adult acute critical care competencies on the same outcomes.
Study Design and Methods
Study Design, Setting and Subjects
This retrospective, cross-sectional study was conducted among subjects who received care in March-May 2020 at a Midwestern academic medical center that used RT-driven protocols. The local institutional review board approved the study protocol (ORA#20063001). Adult subjects with a confirmed or suspected COVID-19 diagnosis, admitted to the hospital for at least three days and received MV, were included. Pregnant subjects were excluded to eliminate the impact of pregnancy-related complications.
Measures
Subjects’ demographic data was obtained from the electronic medical record (EMR), including age, sex, primary race, and body mass index (BMI). We measured race because early findings found a higher incidence of COVID-19 in marginalized communities.24 Indicators for illness severity included comorbidities, sequential organ failure assessment (SOFA) score and PaO2/FiO2 at MV initiation. Protocolized RT interventions included prone sessions, plateau pressure (Pplat) >30 cm H2O, and spontaneous breathing trials (SBTs). We recorded the academic degree of the RT who assessed the patient immediately prior to the first prone session and who recorded Pplats >30 cm H2O and SBTs. Lastly, the time (hours) from intubation to the first prone session and the subsequent number of prone sessions were recorded. The institutional protocol specified proning anytime the PaO2/FiO2 fell below 150. The proning team consisted of 4-5 members, including nurses, nursing assistants, occupational therapists, physical therapists, and RTs. Frequencies of Pplat greater than 30 cmH2O were recorded. Additional data included lengths of ventilator, ICU and hospital stays, and hospital discharge dispositions. Descriptive data from personnel files were extracted for each RT name in the EMR associated with a patient ventilator assessment. Data included the highest academic degree (baccalaureate degree or higher vs. associate degree), years of RT experience, Adult Critical Care Specialist (ACCS) credential, and completion of adult critical care competencies. Adult critical care competency testing addressed an ARDS scenario and included patient assessment, acid-base analysis, chest radiograph interpretation, ventilator management, and ventilator waveform interpretation. Competency testing occurred during employee orientation and annually thereafter, requiring employees to achieve a competency score ≥75% to provide critical care. However, to facilitate staffing during the pandemic’s surge, the department waived this competency requirement for temporary RT staff and graduate-degree RT students (within one semester of graduating). The institution targeted a staffing ratio of six intubated patients per RT.
Study Outcomes
Study endpoints were the impact of RT advanced degrees and adult critical care competencies on the subject’s discharge status and lengths of stay. Discharge outcomes were considered good, compromised, or poor when subjects’ hospital discharge was directly to home, long-term care facility/rehabilitation center, or hospice/died, respectively. Length of stays were the durations (days) of MV, ICU, and hospital stays.
Statistical Analysis
Descriptive statistics for categorical variables were reported as frequencies and continuous variables as means and standard deviations or as medians and interquartile ranges (IQRs). The differences between the groups were evaluated using the 2-tailed t-test, Mann-Whitney test or Kruskal Wallis test, for quantitative variables and the chi-square test or Fisher exact test for categorical variables and tested at α=.05.
Multi-state Models
Model 1 was a time-to-event, four-state regression model assessing the impact of RT and patient covariates on three hospital discharge outcomes.25–27 The model’s states were the baseline (intubated), good, compromised, and poor states allowing for three possible transitions from the baseline to either of these three discharge states. Model 2 was a time-to-event, three-state regression model evaluating the impact of RT and patient covariates on ventilator and ICU outcomes. Model 2’s states were baseline (intubated) and binary transition states of either good (alive) or poor (died or hospice discharge). A sensitivity analysis was used to establish the optimal threshold for the two primary covariates used in both models; RT academic degree and adult critical care competencies. For both RT covariates, a subject-level variable was assigned a 1 to subjects who had more than 85% exposure time to RTs with advanced degrees or those who completed adult critical care competencies; 0 to other subjects. The exposure time >85% was selected because it yielded the highest effect size for the advanced degree. Subject covariates (SOFA, hypertension, BMI, and age) were included based on bivariate analyses and prior research. Missing SOFA data points were inputed using the SOFA score median. BMI and age were used as continuous covariates, and hypertension as a nominal variable. The multi-state model integrated covariates through Cox proportional hazards regression using R’s mstate package, version 4.0.3.28,29 Other analyses were conducted using SPSS, version 26.0.
Results
This study included 260 subjects with a median age of 59 y (IQR 49-68) (Table 1). Of these, the median BMI was 31.4 (IQR 27-38), 166 (63.8%) were males, and the primary race was African American for 98 (37.7%) subjects. The median SOFA score was 4 (IQR 3-5), and median PaO2/FiO2 was 235 (IQR 191-305). RTs proned 197 (75.8%) subjects, with the medians for prone sessions being 2 (IQR 1-4) and time to first prone session 10 hours (IQR 5-44). RTs recorded SBTs in 158 (61%) subjects for a median of 1 (IQR 0-3). Of 260 subjects, we found good discharge outcomes for 36 (13.8%), compromised for 118 (45.4%), and poor for 106 (40.8%) subjects. There were no differences in age, gender, BMI, or primary race among discharge statuses. Hypertension was more prominent in the compromised and poor groups (p=.021), and PaO2/FiO2 was lower in those with poor outcomes (p=.003). The poor group had a significantly higher SOFA score (p=0.043), received more frequent prone sessions (p<.001), and less frequent SBTs (p<.001). The compromised group spent more days on the ventilator, in the ICU, and the hospital as compared to the good and poor groups (p<.001).
Table 1. Subject Characteristics between Hospital Discharge Outcomes.
|
Overall
(n=260) |
Good
(n=36) |
Compromised (n=118) |
Poor
(n=106) |
p | |
|---|---|---|---|---|---|
| Age (y), median (IQR) | 59 (49-68) | 54 (44-66) | 57 (47-66) | 62 (52-71) | .018* |
| Male, n (%) | 166 (63.8) | 24 (66.7) | 75 (64.1) | 67 (57.8) | .94 |
| BMI (kg/m2), median (IQR) | 31.4 (27-38) | 32.3 (29-38) | 31 (27-38) | 31.4 (27-40) | .83 |
| Primary race category, n (%) | .37 | ||||
| African American | 98 (37.7) | 15 (41.7) | 43 (36.4) | 40 (37.7) | |
| Other | 86 (33.1) | 15 (41.7) | 39 (33.1) | 32 (30.2) | |
| White | 51 (19.6) | 3 (8.3) | 26 (22) | 22 (20.8) | |
| Missing/Refusal | 18 (6.9) | 2 (5.6) | 5 (4.2) | 11 (10.4) | |
| Asian | 6 (2.3) | 1 (2.8) | 4 (3.4) | 1 (0.94) | |
| American Indian | 1 (0.4) | 0 | 1 (0.85) | 0 | |
| Comorbidities, n (%) | |||||
| Hypertension | 180 (69.2) | 22 (61.1) | 92 (77.9) | 66 (69.2) | .021 |
| Diabetes mellitus | 141 (54.2) | 16 (44.4) | 70 (59.3) | 55 (51.9) | .24 |
| Chronic kidney disease | 76 (29.2) | 8 (22.2) | 38 (32.2) | 30 (28.3) | .50 |
| Asthma | 42 (16.2) | 4 (11.1) | 21 (16.8) | 17 (16.0) | .63 |
| Heart failure | 28 (10.8) | 1 (2.7) | 15(12.8) | 12 (11.3) | .24 |
| COPD | 17 (6.5) | 4 (11.1) | 5 (4.2) | 8 (7.5) | .30 |
| Cancer | 11 (4.2) | 2 (5.5) | 5 (4.2) | 4 (3.8) | .90 |
| Critical Illness indicators | |||||
| SOFA, median (IQR) | 4 (3-5) | 3 (3-5) | 4 (3-5) | 4 (3-6) | 0.043** |
| PaO2/FiO2 ratio after MV initiation, median (IQR) | 235 (191-305) | 262 (209-352) | 259 (195-324) | 212 (186-262) | .003† |
| Clinical Interventions | |||||
| Prone sessions, median (IQR) | 2 (1-4) | 1 (1-3) | 2 (2-4) | 3 (1-5) | <.001† |
| Time to prone from intubation (h), median (IQR) | 10 (5-44) | 20 (8-46) | 9 (4-33) | 10 (4-46) | 0.424 |
| Number of SBTs, median (IQR) | 1 (0-3) | 1 (0-2) | 2 (1-4) | 0 (0-1) | <.001 |
| Ventilator days, median (IQR) | 13 (17-20) | 6 (3-12) | 16 (10-25) | 10.35 (6-18) | <.001 |
| ICU LOS (days), median (IQR) | 16 (8-26) | 8.5 (5-17) | 21 (15-33) | 11 (5-20) | <.001‡ |
| Hospital LOS (days), median (IQR) | 22.5 (12-33) | 16 (12-15) | 30 (24-37) | 13 (6-21) | <.001‡ |
Abbreviations: IQR, interquartile range; BMI, body mass index (COPD, chronic pulmonary obstructive disease; SOFA, sequential organ failure assessment; PaO2, partial pressure of arterial oxygen; FiO2, fraction of oxygen in inspired air; MV, mechanical ventilation; SBT, spontaneous breathing trial; ICU, intensive care unit; LOS, length of stay
*Adjusted p-value non-significant between the groups
** Adjusted p-value significant between good and poor group
† Adjusted p-value significant between good and poor, and compromised and poor group
‡ Adjusted p-value significant between good and compromised, and compromised and poor group
The 260 subjects admitted during the study period received care from 132 RTs (46 permanent RTs, 81 temporary RTs, and five graduate-level student RTs), had a total of 29,961 RT encounters, and averaged 115 RT encounters per subject (Table 2). Median RT experience was six y (IQR 3-11), with 45.8% holding master’s degrees, 28.1% associate degrees, 24% bachelor’s degrees, 0.9% Ph.D. degrees, and 1.1% RT students. Furthermore, 70.8% of RTs completed adult critical care competencies, and 52% held the ACCS credential. RT experience was similar across all discharge outcomes. However, a between-subjects evaluation showed that subjects with good outcomes encountered fewer RTs with advanced degrees and more RTs with adult critical care competencies and ACCS certification (Table 2). There was a significant association between RTs with adult critical care competencies and ACCS certification (p<.001).
Table 2. Respiratory Therapist Characteristics between Subjects’ Hospital Discharge Outcomes.
| Overall (n=260) |
Good
(n=36) |
Compromised
(n=118) |
Poor
(n=106) |
p | |
|---|---|---|---|---|---|
| Total RT encounters, n | 29961 | 2341 | 16733 | 10887 | |
| RT encounters/subject, n | 115 | 65 | 141 | 103 | |
| RT experience, years, median (IQR) | 6 (3-11) | 6 (3-10) | 6 (3-11) | 6 (3-11) | .243 |
| RT advanced degree, n (%) | 21201 (70.8) | 1600 (68.3) | 11893 (71.1) | 7708 (70.8) | .025 |
| RT adult critical care competency completion, n (%) | 21209 (70.8) | 1783 (76.2) | 11665 (69.7) | 7761 (71.3) | <.001 |
| RT encounters (advanced degree and RT competency), n (%) | 14124 (47) | 1146 (49) | 7814 (46.7) | 5164 (47.4) | .092 |
| ACCS certification, n (%) | 15581 (52) | 1305 (55.7) | 8462 (50.6) | 5814 (53.4) | <.001 |
| RT protocol interventions | |||||
| Received prone therapy, n (%) | 197 (75.8) | 19 (53) | 90 (76.3) | 88 (83) | |
| RT with advanced degree provided respiratory care immediately before prone initiated, n (%) | 138 (70.1) | 15 (78.9) | 68 (75.6) | 55 (62.5) | 0.106 |
| RT with critical care competency provided respiratory care immediately before prone initiated, n (%) | 149 (75.6) | 18 (94.7) | 64 (71.1) | 67 (76.1) | 0.093 |
| Plateau pressure recorded, n | 7771 | 522 | 3937 | 3312 | |
| Plateau pressure > 30 cm H2O, n (%) | 1730 (22.3) | 57 (10.9) | 608 (15.4) | 1065 (32.2) | <0.001 |
| RT with advanced degree recorded plateau pressure > 30 cm H2O, n (%) | 1169 (67.6) | 50 (87.7) | 409 (67.3) | 710 (66.7) | 0.004 |
| RT with critical care competency recorded plateau pressure > 30 cm H2O, n (%) | 1197 (69.2) | 43 (75.4) | 435 (71.5) | 719 (67.5) | 0.133 |
| Spontaneous breathing trial (SBT) recorded, n | 459 | 47 | 340 | 72 | |
| RT with advanced degree recorded SBT, n (%) | 289 (63) | 24 (51.1) | 213 (62.6) | 52 (72.2) | 0.063 |
| RT with critical care competency recorded SBT, n (%) | 357 (78) | 44 (93.6) | 260 (76.5) | 53 (73.6) | 0.019 |
Abbreviations: RT, respiratory therapist; IQR, interquartile range; ACCS, adult critical care specialist
Regarding proning, no significant differences emerged across study groups related to RT education attributes of RTs providing respiratory care immediately prior to proning. However, when survivors (good and compromised outcomes) were compared with those who died, care immediately prior to proning from an RT with an advanced degree favoured survival, p=.038. Compared to those with compromised or poor outcomes, subjects with good outcomes received care more frequently from an RT with critical care competencies, p=.041. The frequency of Pplat values >30 cm H2O increased among compromised and poor groups as compared to the good group (p<.001). When comparing discharge outcomes, RTs with advanced degrees recorded Pplat >30 cm H2O more frequently in the good discharge group (p=.004). Adult critical care competencies had no impact on the recorded Pplat (p=.133). RTs recorded a total of 459 SBTs among all subjects, of which RTs with advanced degrees recorded 289 (63%) and RTs with critical care competencies recorded 357 (78%) SBTs. When assessing SBT performance between the quality of discharge outcomes, RT degree had no impact (p=.063). However, RTs with critical care competencies performed SBTs more frequently in the good outcome group (p=.019).
Table 3 shows how different thresholds of each subject’s exposure to RTs with advanced degrees and adult critical care competencies yielded a good discharge status. A >75% subject exposure to RTs with advanced degrees had no significant impact on good discharge status compared to less exposure (p=.12). However, subjects with >80% exposure to RTs with advanced degrees transitioned 2.47 times more frequently to a good discharge status (p=.005). At 85% exposure, the transition frequency was 3.72 times higher (p< .001). Similarly, increased subject exposure (>80%) to RTs with adult critical care competencies yielded significantly higher transition rates to good discharge outcomes.
Table 3. Transition Rate Ratios for Good Discharge Outcome and Hospital Days by Different Levels of Respiratory Therapist Exposure within a Subject.
| Hospital Days | ||
| Within Subject RT exposure threshold | Transition Rate Ratio (95% CI) | p value |
| Advanced Degree | ||
| > 95% | 3.02 (1.08-8.39) | .034 |
| > 90% | 3.51 (1.49-8.25) | <.001 |
| > 85% | 3.72 (1.75-7.90) | <.001 |
| > 80% | 2.47 (1.34-5.62) | .005 |
| > 75% | 1.77 (0.85-3.69) | .12 |
| Adult Critical Care Competency | ||
| > 95% | 9.66 (4.47-20.91) | <.001 |
| > 90% | 5.36 (2.58-11.16) | <.001 |
| > 85% | 5.10 (2.54-10.24) | <.001 |
| > 80% | 3.32 (1.70-6.68) | <.001 |
| > 75% | 1.90 (0.95-3.82) | .071 |
Abbreviations: RT, respiratory therapist; CI, confidence interval
Study Outcomes
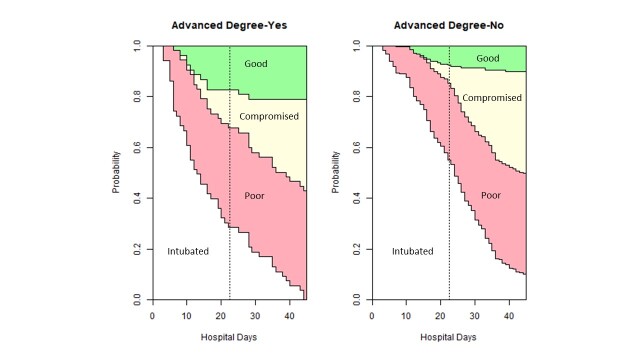
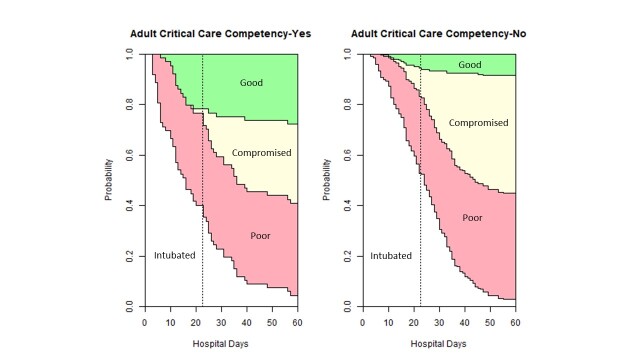
The time-to-event multi-state model (Model 1) demonstrates the impact of RT education, RT competencies and patient characteristics on discharge outcomes (Table 4). When evaluating hospital stay, each subject with >85% exposure to RTs with advanced degrees transitioned 3.72 (95% CI 1.75-7.91) times more frequently to the good outcomes as compared to those with less exposure (p=.001). Figure 1a shows that among subjects with >85% advanced degree RT exposure at hospital day 22 (median value), the probability of transitioning to a good outcome was 18% as compared to 8.1% with less exposure. Similarly, subjects with >85% exposure to RTs with adult critical care competencies transitioned 5.10 (95% CI 2.54-10.24) times more frequently to the good outcome compared to those who did not (p<.001). Figure 1b highlights how subjects with >85% exposure to RTs with adult critical care competencies at hospital day 22, the probability of transitioning to a good outcome was 23% as compared to 6% with less exposure. The SOFA score had a mild impact on the hospital discharge outcomes leading to a 1.12 transition rate towards death, p=.046. However, subjects with hypertension transitioned less frequently to the good outcome (p=.018) and nearly half as frequently to the poor outcome (p<.001). Furthermore, subjects with higher BMI transitioned more frequently to the compromised (p=.004) and poor (p=.005) states. Persons with advanced age transitioned 1.03 times more frequently to the poor state (p=.021). An >80% RT exposure threshold showed consistent findings with weaker magnitude, see Supplementary Data, Table 1.
Table 4. Model 1: Three Transition Rate Ratios for Respiratory Therapists’ Impact on Hospital Discharge Outcomes.
| Hospital Days | ||||
| Outcomes | Yes (n) | No (n) | Transition Rate Ratio (95% CI) |
p |
| > 85% subject exposure to RTs with advanced degree | ||||
| Good | 11 | 25 | 3.72 (1.75-7.91) | .001 |
| Compromised | 18 | 100 | 1.40 (0.82-2.37) | .214 |
| Poor | 21 | 85 | 1.39 (0.86-2.25) | .183 |
| > 85% subject exposure to RTs with adult critical care competencies | ||||
| Good | 18 | 18 | 5.10 (2.54-10.24) | <.001 |
| Compromised | 24 | 94 | 1.24 (0.76-2.03) | .393 |
| Poor | 20 | 86 | 1.15 (0.70-1.88) | .587 |
| SOFA | Median (IQR) | |||
| Good | 4 (3-4) | 0.85 | .284 | |
| Compromised | 4 (3.25-4) | 0.96 | .552 | |
| Poor | 4 (4-5) | 1.123 | .046 | |
| Hypertension | ||||
| Good | 22 | 14 | 0.41 (0.19-0.85) | .018 |
| Compromised | 92 | 26 | 0.77 (0.47-1.22) | .272 |
| Poor | 66 | 40 | 0.46 (0.30-0.69) | <.001 |
| BMI | Median (IQR) | |||
| Good | 32.3 (29-38) | 1.03 (0.98-1.07) | .226 | |
| Compromised | 31 (27-38) | 1.03 (1.01-1.05) | .004 | |
| Poor | 31.4 (27-40) | 1.03 (1.01-1.05) | .005 | |
| Age | Median (IQR) | |||
| Good | 54 (44-66) | 1.00 (0.97-1.02) | .861 | |
| Compromised | 57 (47-66) | 1.01 (0.99-1.02) | .275 | |
| Poor | 62 (57-21) | 1.03 (1.01-1.04) | .021 | |
Abbreviations: RT, respiratory therapist; CI, confidence interval; BMI, body mass index; IQR, interquartile range; SOFA, sequential organ function assessment
Figure 1a. Discharge outcomes based on advanced degree and hospital stay.
Figure 1b. Discharge outcomes based on adult critical care competency and hospital stay.
Results from Model 2 appear in Table 5. When evaluating ventilator days, subjects with >85% advanced degree RT exposure transitioned 1.72 (95% CI 1.21-2.45) times more frequently to good discharge outcomes (p=.002). Similarly, subjects with >85% exposure to RTs with adult critical care competencies transitioned 1.94 (95% CI 1.36-2.75) times more frequently to good outcomes (p<.001) and 2.60 (95% CI 1.46-4.63) times to poor outcomes (p=.001). Subjects with higher BMI (p=.002) and advanced age (p=.04) transitioned more frequently to the poor outcome.
Table 5. Model 2: Two Transition Rate Ratios for Respiratory Therapist’s Impact on Ventilator and ICU Discharge Outcomes.
| Ventilator Days | ICU Days | |||||||
| Outcomes | Yes (n) | No (n) | Transition Rate Ratio (95% CI) |
p | Yes (n) | No (n) | Transition Rate Ratio (95% CI) |
p |
| >85% subject exposure to RTs with advanced degree | ||||||||
| Good | 43 | 155 | 1.72 (1.21-2.45) | .002 | 46 | 181 | 1.90 (1.35-2.68) | <.001 |
| Poor | 13 | 49 | 1.54 (0.82-2.87) | .18 | 6 | 27 | 1.22 (0.49-3.03) | .67 |
| >85% subject exposure to RTs with adult critical care competencies | ||||||||
| Good | 46 | 152 | 1.94 (1.36-2.75) | <.001 | 58 | 169 | 1.78 (1.30-2.46) | <.001 |
| Poor | 17 | 45 | 2.60 (1.46-4.63) | .001 | 6 | 27 | 1.31 (0.53-3.27) | .55 |
| Hypertension | ||||||||
| Good | 143 | 55 | 0.98 (0.71-1.37) | .92 | 158 | 69 | 0.64 (0.47-0.85) | .003 |
| Poor | 37 | 25 | 0.42 (0.24-0.71) | .001 | 22 | 11 | 0.56 (0.26-1.20) | .14 |
| BMI | Median (IQR) | Median (IQR) | ||||||
| Good | 30.86 (27-37) | 0.98 (0.96-1.00) | .10 | 31.3 (27.1-37.80) | 1.02 (1.01-1.04) | .002 | ||
| Poor | 33.9 (28-42) | 1.04 (1.02-1.07) | .002 | 32.1 (28.4-40.9) | 1.04 (1.00-1.08) | .042 | ||
| Age | Median (IQR) | Median (IQR) | ||||||
| Good | 58 (49-67) | 1.00 (0.98-1.01) | .363 | 58 (48-68) | 1.01 (0.99-1.02) | .08 | ||
| Poor | 61 (53-71) | 1.02 (1.00-1.05) | .044 | 61 (54-68) | 1.04 (1.01-1.07) | .014 | ||
| SOFA | Median (IQR) | Median (IQR) | ||||||
| Good | 4 (3-4) | 1.05 (0.94-1.17) | .421 | 4(3-5) | 1.09 (0.99-1.19) | .06 | ||
| Poor | 4 (3-5) | 1.02 (1.02-1.42) | .025 | 4 (4-4) | 0.97 (0.76-1.24) | .812 | ||
Abbreviations: RT, respiratory therapist; CI, confidence interval; BMI, body mass index; IQR, interquartile range; SOFA, sequential organ function assessment
When assessing ICU days, subjects with >85% advanced degree RT care and >85% adult critical care competencies exposures transitioned more frequently to good discharge outcomes, 1.90 (95% CI 1.35-2.68) times (p<.001) and 1.78 (95% CI 1.30-2.46) times (p<.001), respectively. Subjects with advanced age and higher BMI were significantly more likely to transition to the poor state.
Discussion
This is the first study to explore the impact of either advanced RT academic degrees or critical care competencies on patient outcomes. Findings show that RTs were heavily involved in providing care to patients with COVID-19 pneumonia receiving MV, averaging 115 assessments per patient. Furthermore, the findings revealed that patients with greater than 85% exposure to RTs with either advanced degrees or critical care competencies were more likely to be discharged home.
Mortality rates of 30-50% occurred when patients with COVID-19 pneumonia required MV,30–32 which matches this study’s 40.8% hospital mortality rate. Higher mortality is associated with advanced age, obesity, and poor oxygenation.31 Additionally, ARDS clinical outcomes depend on the timely application of guideline-based ventilator management and prone positioning.7,8,32,33 A study evaluating ARDS management in patients with COVID-19 reported that only 50.4% of patients received ARDS guideline-based clinical management, though RT characteristics were absent.34 In the United States, RTs serve as the surveillance system for identifying the need, adjustments, and ongoing monitoring for lung-protective strategies, prone positioning, and others. Thus, exploring the relationship RT characteristics have on clinical outcomes is essential.
The nursing profession studied how educational characteristics affected patient outcomes and found that a 10% increase in nurses with baccalaureate degrees reduced 30-day mortality by 4%-8%.19–22 A greater impact of advanced nursing education on mortality odds occurred in postsurgical patients with dementia highlighting how the problem-solving and synthesis skills of more highly educated nurses benefit vulnerable patients who cannot communicate.23 Further, longitudinal changes in patient safety and quality care measures made over a decade showed that increases in the percentages of nurses by 10% reduced the odds of unfavourable safety and quality ratings between 7% and 17%.34 A Canadian study found patients with acute illnesses had lower rates of 30-day patient mortality when cared for by nurses with a baccalaureate degree [OR 0.81 (95% CI 0.68-0.96)].16 Another Canadian study explored mortality outcomes from adults with medical illnesses and reported that a 10% increase in the proportion of nurses with baccalaureate degrees resulted in a 9% reduction in mortality.17 In critical care settings, each 10% increase in the number of nurses with baccalaureate degrees lowered the risk of mortality by 2% in adults receiving MV.35 Given RTs’ surveillance responsibilities for a complex therapy like MV, the impact of care received from RTs with advanced degrees on mortality in the current study is unsurprising. Regarding the respiratory therapy profession, the stacked probability figure (Figure 1) suggests that RT advanced education aided discharge to home in fewer days. Although it is difficult to identify how a single profession affects a patient’s outcome, this study explored the association between RT education and specific RT protocol interventions such as proning, Pplat management, and SBT. A positive survival outcome was associated with receiving care from an RT with an advanced degree immediately prior to the first proning session. Between subjects, our data revealed that RTs with advanced degrees were more likely to record Pplat >30 cm H2O. This unexpected finding may be attributed to the study methodology. We pulled Pplat values from the patient’s chart but did not individually audit whether a high value was recorded and immediately followed by a ventilator change to align with the institution’s lung protective protocol. A closer audit process is needed to confirm future results. Academic degrees did not affect the overall SBT frequency among discharge outcomes. The retrospective nature of the analysis makes definitive conclusions difficult.
Patient mortality is an important metric; however, health status on discharge also matters. A recent study exploring outcomes from inpatient cardiac arrest found a 10% increase in nursing staff with baccalaureate degrees led to increased odds of surviving with good cerebral performance [OR 1.24 (95% CI 1.08-1.42)]. When only survival outcome was explored, nurse education was not significant.36 The current study similarly addressed the quality of the discharge status. Our study showed that when >85% of care was provided by RTs with a baccalaureate degree or higher, the transition to home was almost 4 times the rate compared to less care provided by RTs with an advanced degree. Some may argue that work experience is an adequate substitute for advanced education. Several studies in the nursing literature refute that argument.19,21,22 In the current study, work experience was not associated with improved patient outcomes.
The nursing profession recognizes education and certifications as part of the Magnet program.37 Specific to Magnet’s scientific discovery value, the impact of a baccalaureate degree on evidence-based practice was studied, and nurses with baccalaureate degrees had greater desires, ability, and frequency of using evidence-based practices.38 Nurses are the first line of surveillance for detecting healthcare complications because of their proximity to the patient and contact time.39 Similarly, RTs play an important surveillance role for patients requiring MV and also need evidence-based practice structures. Like Magnet, the AARC has recognition for respiratory care excellence in acute care hospitals through the Apex Award. Amongst the award’s criteria, the RT department must conduct annual competencies for all RTs, and at least half of the RT staff must have a bachelor’s degree.40 The current study was conducted at a facility holding the Apex designation and may support the positive impact of education and competencies on patient outcomes. However, further investigation is needed since only one Apex department was studied.
In 1992, the Evidence-Based Medicine Working Group published an article that emphasized the use of evidence-based clinical practice to improve patient outcomes.41 Competency-based education has been used since in both pre-professional education and ongoing clinical education to teach evidence-based clinical practices.42,43 A study that evaluated the impact of competency education among nurse practitioners and physician assistants showed significant improvement in acquiring new knowledge and skills.44 Another study explored the impact of competency-based education on resident physicians’ learning related to MV and reported an increase from baseline 31% to 96% in residents’ ventilator management confidence.45 Critical care competencies in the current study also appeared to impact discharge outcomes. Patients requiring proning had better discharge outcomes when the RT who provided their respiratory care immediately prior to the proning session had completed critical care competencies. Further, competencies were associated with performing more SBTs, but not the management of Pplat. The stacked probability Figure 1b from the current study shows how completing competencies impacted the positive discharge status in fewer hospital days. Model 1 demonstrated that both advanced degrees and competencies facilitated a quality discharge to home when measured independently, with competencies having a slightly higher impact. Further, Model 2 showed that high exposure to RTs with competencies increased the frequency of alive discharges by twice when considering ventilator and ICU days.
Findings from this study provide the first empirical evidence that both RTs with baccalaureate or higher education and clinical competencies may improve the outcomes of patients with COVID-19 pneumonia. If >85% of the care being delivered by therapists with advanced degrees were supported in future studies, it could have implications for department hiring practices and entry-level education. Presently, 44% of RTs in the United States have a baccalaureate degree or higher, and only 13.2% of the total number of graduates of entry-level respiratory care programs earned baccalaureate degrees in 2020.46 For respiratory care departments to hire enough RTs with a minimum of a baccalaureate degree, more entry-level baccalaureate programs are needed. Accreditation agencies will need further studies substantiating these findings before changing the entry-level respiratory care degree standards.
The major limitation of this retrospective study is that it does not prove causality. However, the study findings are useful in generating hypotheses for future research to investigate the impact of RT education on patient outcomes. This single-center study was conducted in a clinical department with many (70.8%) RTs with advanced degrees. As a result of a staffing shortage during the surge of the COVID-19 pandemic, the department hired several temporary RTs and students (within one semester of graduating with a master’s degree) who received a short orientation before providing care to critically ill patients. This center utilized a lung protective ventilation protocol which may not be present in all respiratory care departments. Also, due to a shortage of sedatives, RTs were limited in keeping tidal volume in the lung protective range; therefore, exhaled tidal volume data was not addressed in this manuscript. Adherence to PEEP/FiO2 tables was not recorded, thus limiting the ability to further understand the mechanism of RT-driven improved outcomes. Some errors may have occurred with manually inputed SOFA scores. Furthermore, we did not collect patient-level data on the use of inhaled vasodilators which may have also impacted findings. Additionally, we did not collect data on the RT experience in managing ARDS patients, RT to ventilator ratio, and nursing or physician or pharmacist characteristics, which may have influenced the results. As stated earlier, the impact of a single discipline on patient outcomes is not easily discerned.
Conclusion
Respiratory therapist education was associated with improved discharge outcomes for patients with COVID-19 pneumonia. Specifically, the subjects’ discharge quality improved when they received >85% of care from RTs with an advanced degree or who completed annual adult critical care competencies. These preliminary findings suggest that the RT workforce may need advanced education and competency training to provide high-quality, evidence-based care. However, researchers should design robust studies across multiple centers to assess causality and corroborate these findings.
Competing interests
The authors have no conflicts of interest to declare.
Contributors
RK and EB are responsible for all content of the manuscript. RK and EB conceived the idea. RK, AG and EB implemented the study. RK, EB and RM conducted data analysis and interpreted the data. RK, EB, AG and RM drafted the manuscript, all authors reviewed the manuscript for important intellectual content and approved the final manuscript.
Ethical statement
The study protocol was approved by the local institutional review board (ORA#20063001). For analysis, we used datasets which were properly anonymized.
AI statement
The authors confirm no generative AI or AI-assisted technology was used to generate content.
Supplementary Material
Supplementary Table. Multi-state Model Output using > 80% Subject exposure to Respiratory Therapist
Acknowledgments
Acknowledgements
We sincerely thank our colleagues at the Rush University Medical Center for their clinical services. We thank Maliha Syed and Aashna Modi for assisting with data collection. We also thank J. Brady Scott for reviewing this manuscript.
Funding Statement
This work was supported by the Vision Grant from the American Association for Respiratory Care. The sponsor was not involved in study design, data collection/analysis or manuscript preparation and final submission. All authors had the final decision to submit the manuscript.
References
- Critical Supply Shortages - The need for ventilators and personal protective equipment during the Covid-19 pandemic. Ranney Megan L., Griffeth Valerie, Jha Ashish K. Apr 30;2020 New England Journal of Medicine. 382(18):e41. doi: 10.1056/nejmp2006141. doi: 10.1056/nejmp2006141. [DOI] [PubMed] [Google Scholar]
- Health workforce surge capacity during the COVID-19 pandemic and other global respiratory disease outbreaks: A systematic review of health system requirements and responses. Gupta Neeru, Balcom Sarah A., Gulliver Adrienne, Witherspoon Richelle L. Mar;2021 The International Journal of Health Planning and Management. 36(Suppl 1):26–41. doi: 10.1002/hpm.3137. doi: 10.1002/hpm.3137. [DOI] [Google Scholar]
- Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study [published correction appears in Lancet Respir Med. 2020 Apr;8(4):e26] Yang Xiaobo, Yu Yuan, Xu Jiqian, Shu Huaqing, Xia Jia'an, Liu Hong, Wu Yongran, Zhang Lu, Yu Zhui, Fang Minghao, Yu Ting, Wang Yaxin, Pan Shangwen, Zou Xiaojing, Yuan Shiying, Shang You. May;2020 The Lancet Respiratory Medicine. 8(5):475–481. doi: 10.1016/s2213-2600(20)30079-5. doi: 10.1016/s2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China [published correction appears in JAMA Intern Med. 2020 Jul 1;180(7):1031] Wu Chaomin, Chen Xiaoyan, Cai Yanping, Xia Jia’an, Zhou Xing, Xu Sha, Huang Hanping, Zhang Li, Zhou Xia, Du Chunling, Zhang Yuye, Song Juan, Wang Sijiao, Chao Yencheng, Yang Zeyong, Xu Jie, Zhou Xin, Chen Dechang, Xiong Weining, Xu Lei, Zhou Feng, Jiang Jinjun, Bai Chunxue, Zheng Junhua, Song Yuanlin. Jul 1;2020 JAMA Internal Medicine. 180(7):934. doi: 10.1001/jamainternmed.2020.0994. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Characteristics and outcomes of 21 critically Ill patients with COVID-19 in Washington State. Arentz Matt, Yim Eric, Klaff Lindy, Lokhandwala Sharukh, Riedo Francis X., Chong Maria, Lee Melissa. Apr 28;2020 JAMA. 323(16):1612–1614. doi: 10.1001/jama.2020.4326. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Past and present ARDS mortality rates: A systematic review. Máca Jan, Jor Ondřej, Holub Michal, Sklienka Peter, Burša Filip, Burda Michal, Janout Vladimír, Ševčík Pavel. 2017Respiratory Care. 62(1):113–122. doi: 10.4187/respcare.04716. doi: 10.4187/respcare.04716. [DOI] [PubMed] [Google Scholar]
- Prone positioning in severe acute respiratory distress syndrome. Guérin Claude, Reignier Jean, Richard Jean-Christophe, Beuret Pascal, Gacouin Arnaud, Boulain Thierry, Mercier Emmanuelle, Badet Michel, Mercat Alain, Baudin Olivier, Clavel Marc, Chatellier Delphine, Jaber Samir, Rosselli Sylvène, Mancebo Jordi, Sirodot Michel, Hilbert Gilles, Bengler Christian, Richecoeur Jack, Gainnier Marc, Bayle Frédérique, Bourdin Gael, Leray Véronique, Girard Raphaele, Baboi Loredana, Ayzac Louis. Jun 6;2013 New England Journal of Medicine. 368(23):2159–2168. doi: 10.1056/nejmoa1214103. doi: 10.1056/nejmoa1214103. [DOI] [PubMed] [Google Scholar]
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. Acute Respiratory Distress Syndrome Network. Brower R G, Matthay M A, et al. May 4;2000 New England Journal of Medicine. 342(18):1301–1308. doi: 10.1056/nejm200005043421801. doi: 10.1056/nejm200005043421801. [DOI] [PubMed] [Google Scholar]
- Creating a vision for respiratory care in 2015 and beyond. Kacmarek Robert M., Durbin Charles G., Barnes Thomas A., Kageler Woody V., Walton John R., O'Neil Edward H. Mar;2009 Respiratory Care. 54(3):375–389. PMID: 19245732. [PubMed] [Google Scholar]
- Mechanical ventilation competencies of the respiratory therapist in 2015 and Beyond. Kacmarek Robert M. May 25;2013 Respiratory Care. 58(6):1087–1096. doi: 10.4187/respcare.02546. doi: 10.4187/respcare.02546. [DOI] [PubMed] [Google Scholar]
- CoARC Accreditation Standards for Entry into Respiratory Care Professional Practice. [2023-7-28]. https://coarc.com/wp-content/uploads/2023/05/CoARC-Entry-Standards-1.1.2022-updated-3.23-clean.pdf
- AARC Respiratory Therapist Education: Position Statement. [2022-7-18]. https://www.aarc.org/wp-content/uploads/2017/03/statement-of-respiratory-therapist-education.pdf
- CoARC Communication to our Communities of Interest: Response to AARC Position Statement on Respiratory Therapist Education (Revised December 1, 2017). [2022-7-18]. https://coarc.com/wp-content/uploads/2020/12/CoARC-Communication-Min-Degree-Reguirements-1-28-16-rev-12-1-17_1-compressed.pdf
- AARC Entry Requirements to Respiratory Therapy Practice: 2030 and Thereafter. Position Statement. [2022-7-18]. https://www.aarc.org/wp-content/uploads/2019/09/statement-entry-requirements-to-respiratory-therapy-practice-2030-and-therafter.pdf
- CoARC Communication to our Communities of Interest. [2022-7-18]. https://coarc.com/wp-content/uploads/2021/11/CoARC-Communication-Standard-1.01-11-3-21.pdf
- The impact of hospital nursing characteristics on 30-day mortality. Estabrooks Carole A., Midodzi William K., Cummings Greta G., Ricker Kathryn L., Giovannetti Phyllis. Mar;2005 Nursing Research. 54(2):74–84. doi: 10.1097/00006199-200503000-00002. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Impact of hospital nursing care on 30-day mortality for acute medical patients. Tourangeau Ann E., Doran Diane M., McGillis Hall Linda, O'Brien Pallas Linda, Pringle Dorothy, Tu Jack V., Cranley Lisa A. Jan;2007 Journal of Advanced Nursing. 57(1):32–44. doi: 10.1111/j.1365-2648.2006.04084.x. doi: 10.1111/j.1365-2648.2006.04084.x. [DOI] [PubMed] [Google Scholar]
- The relationship between inpatient cardiac surgery mortality and nurse numbers and educational level: analysis of administrative data. Van den Heede Koen, Lesaffre Emmanuel, Diya Luwis, Vleugels Arthur, Clarke Sean P., Aiken Linda H., Sermeus Walter. Jun;2009 International journal of nursing studies. 46(6):796–803. doi: 10.1016/j.ijnurstu.2008.12.018. doi: 10.1016/j.ijnurstu.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Educational levels of hospital nurses and surgical patient mortality. Aiken L. H., Clarke S.P., Cheung R.B., Sloane D.M., Silber J.H. Sep 24;2003 JAMA: The Journal of the American Medical Association. 290(12):1617–1623. doi: 10.1001/jama.290.12.1617. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Aiken Linda H., Cimiotti Jeannie P., Sloane Douglas M., Smith Herbert L., Flynn Linda, Neff Donna F. Dec;2011 Medical care. 49(12):1047–1053. doi: 10.1097/mlr.0b013e3182330b6e. doi: 10.1097/mlr.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurse specialty certification, inpatient mortality, and failure to rescue. Kendall-Gallagher Deborah, Aiken Linda H., Sloane Douglas M., Cimiotti Jeannie P. Apr 1;2011 Journal of Nursing Scholarship. 43(2):188–194. doi: 10.1111/j.1547-5069.2011.01391.x. doi: 10.1111/j.1547-5069.2011.01391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An increase in the number of nurses with baccalaureate degrees is linked to lower rates of postsurgery mortality. Kutney-Lee Ann, Sloane Douglas M., Aiken Linda H. Mar;2013 Health Affairs. 32(3):579–586. doi: 10.1377/hlthaff.2012.0504. doi: 10.1377/hlthaff.2012.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lower Postsurgical Mortality for Individuals with Dementia with Better-Educated Hospital Workforce. White Elizabeth M., Smith Jessica G., Trotta Rebecca L., McHugh Matthew D. Mar 20;2018 Journal of the American Geriatrics Society. 66(6):1137–1143. doi: 10.1111/jgs.15355. doi: 10.1111/jgs.15355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. Mude William, Oguoma Victor M, Nyanhanda Tafadzwa, Mwanri Lillian, Njue Carolyne. Jun 26;2021 Journal of Global Health. 11:05015. doi: 10.7189/jogh.11.05015. doi: 10.7189/jogh.11.05015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Multi-state models for event history analysis. Andersen Per Kragh, Keiding Niels. Apr;2002 Statistical Methods in Medical Research. 11(2):91–115. doi: 10.1191/0962280202sm276ra. doi: 10.1191/0962280202sm276ra. [DOI] [PubMed] [Google Scholar]
- Multi-state models for the analysis of time-to-event data. Meira-Machado Luís, de Uña-Álvarez Jacobo, Cadarso-Suárez Carmen, Andersen Per K. 2009Statistical methods in medical research. 18(2):195–222. doi: 10.1177/0962280208092301. doi: 10.1177/0962280208092301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Multi-state models: a review. Hougaard Philip. 1999Lifetime Data Analysis. 5(3):239–264. doi: 10.1023/a:1009672031531. doi: 10.1023/a:1009672031531. [DOI] [PubMed] [Google Scholar]
- mstate: An R Package for the analysis of competing risks and multi-state models. Wreede Liesbeth C. de, Fiocco Marta, Putter Hein. 2011Journal of Statistical Software. 38(7):1–30. doi: 10.18637/jss.v038.i07. doi: 10.18637/jss.v038.i07. [DOI] [Google Scholar]
- Beyersmann Jan, Allignol Arthur, Schumacher Martin. Competing risks and multistate models with R. Springer New York; [DOI] [Google Scholar]
- Mortality associated with early changes in ARDS severity in COVID–19 patients – Insights from the PRoVENT–COVID study. Schuijt Michiel T.U., Martin-Loeches Ignacio, Schultz Marcus J., Paulus Frederique, Neto Ary Serpa, van Akkeren J.P., Algera A.G., Algoe C.K., van Amstel R.B., Baur O.L., van de Berg P., van den Berg A.E., Bergmans D.C.J.J., van den Bersselaar D.I., Bertens F.A., Bindels A.J.G.H., de Boer M.M., den Boer S., Boers L.S., Bogerd M., Bos L.D.J., Botta M., Breel J.S., de Bruin H., de Bruin S., Bruna C.L., Buiteman-Kruizinga L.A., Cremer O., Determann R.M., Dieperink W., Dongelmans D.A., Franke H.S., Aldridge M.S. Galek, de Graaff M.J., Hagens L.A., Haringman J.J., Heijnen N.F.L., Hiel S., van der Heide S.T., van der Heiden P.L.J., Hoeijmakers L.L., Hol L., Hollmann M.W., Hoogendoorn M.E., Horn J., van der Horst R., Ie E.L.K., Ivanov D., Juffermans N.P., Kho E., de Klerk E.S., Koopman A.W.M., Koopmans M., Kucukcelebi S., Kuiper M.A., de Lange D.W., van Mourik N., Martin-Loeches I., Nijbroek S.G., Onrust M., Oostdijk E.A.N., Paulus F., Pennartz C.J., Pillay J., Pisani L., Purmer I.M., Rettig T.C.D., Roozeman J.P., Schuijt M.T.U., Schultz M.J., Neto A. Serpa, Sleeswijk M.E., Smit M.R., Spronk P.E., Stilma W., Strang A.C., Tsonas A.M., Tuinman P.R., Valk C.M.A., Veen F.L., Vlaar A.P.J., Veldhuis L.I., van Velzen P., van der Ven W.H., van Vliet P., van der Voort P., van der Wier H.H., van Welie L., Wesselink H.J.F.T., van Wijk B., Winters T., Wong W.Y., van Zanten A.R.H. Oct;2021 Journal of Critical Care. 65:237–245. doi: 10.1016/j.jcrc.2021.06.016. doi: 10.1016/j.jcrc.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators Oct 29;2020 Intensive Care Medicine. 47(1):60–73. doi: 10.1007/s00134-020-06294-x. doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prone Position in COVID-19 and -COVID-19 Acute Respiratory Distress Syndrome: An International Multicenter Observational Comparative Study*. Camporota Luigi, Sanderson Barnaby, Chiumello Davide, Terzi Nicolas, Argaud Laurent, Rimmelé Thomas, Metuor Romain, Verstraete Aude, Cour Martin, Bohé Julien, Piriou Vincent, Beuret Pascal, Guérin Claude. 2022Critical Care Medicine. 50(4):633–643. doi: 10.1097/ccm.0000000000005354. doi: 10.1097/ccm.0000000000005354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lung protective ventilation strategy for the acute respiratory distress syndrome. Petrucci Nicola, Iacovelli Walter. Jul 18;2007 Cochrane Database of Systematic Reviews. (3):CD003844. doi: 10.1002/14651858.cd003844.pub3. doi: 10.1002/14651858.cd003844.pub3. [DOI] [PubMed]
- Hospital Variation in Management and Outcomes of Acute Respiratory Distress Syndrome Due to COVID-19. Johnson Shelsey W., Garcia Michael A., Sisson Emily K. Q., Sheldrick Christopher R., Kumar Vishakha K., Boman Karen, Bolesta Scott, Bansal Vikas, Lal Amos, Domecq J. P., Melamed Roman R., Christie Amy B., Husain Abdurrahman, Yus Santiago, Gajic Ognjen, Kashyap Rahul, Walkey Allan J., from the Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group Feb;2022 Critical Care Explorations. 10(2):e0638. doi: 10.1097/cce.0000000000000638. doi: 10.1097/cce.0000000000000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Impact of critical care nursing on 30-day mortality of mechanically ventilated older adults. Kelly Deena M., Kutney-Lee Ann, McHugh Matthew D., Sloane Douglas M., Aiken Linda H. May;2014 Critical Care Medicine. 42(5):1089–1095. doi: 10.1097/ccm.0000000000000127. doi: 10.1097/ccm.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- In hospitals with more nurses who have baccalaureate degrees, better outcomes for patients after cardiac arrest. Harrison Jordan M., Aiken Linda H., Sloane Douglas M., Brooks Carthon J. Margo, Merchant Raina M., Berg Robert A., McHugh Matthew D., for the American Heart Association’s Get With the Guidelines–Resuscitation Investigators Jul;2019 Health Affairs. 38(7):1087–1094. doi: 10.1377/hlthaff.2018.05064. doi: 10.1377/hlthaff.2018.05064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Original Research: How Magnet Hospital Status Affects Nurses, Patients, and Organizations: A Systematic Review. Rodríguez-García Ma Carmen, Márquez-Hernández Verónica V., Belmonte-García Teresa, Gutiérrez-Puertas Lorena, Granados-Gámez Genoveva. Jul;2020 AJN, American Journal of Nursing. 120(7):28–38. doi: 10.1097/01.naj.0000681648.48249.16. doi: 10.1097/01.naj.0000681648.48249.16. [DOI] [PubMed] [Google Scholar]
- Empowering nurses with evidence-based practice environments: surveying Magnet®, Pathway to Excellence®, and non-magnet facilities in one healthcare system. Wilson Marian, Sleutel Martha, Newcomb Patricia, Behan Deborah, Walsh Judith, Wells Jo Nell, Baldwin Kathleen M. Jan 16;2015 Worldviews on Evidence-Based Nursing. 12(1):12–21. doi: 10.1111/wvn.12077. doi: 10.1111/wvn.12077. [DOI] [PubMed] [Google Scholar]
- Lower Medicare mortality among a set of hospitals known for good nursing care. Aiken Linda H., Smith Herbert L., Lake Eileen T. Aug;1994 Medical Care. 32(8):771–787. doi: 10.1097/00005650-199408000-00002. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- American Association for Respiratory Care Apex Recognition Award. [2022-8-1]. https://www.aarc.org/resources/programs-projects/apex-recognition-award/
- Evidence-based medicine. A new approach to teaching the practice of medicine. Evidence-Based Medicine Working Group Nov 4;1992 JAMA. 268(17):2420–2425. doi: 10.1001/jama.1992.03490170092032. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]
- CPD of the future: a partnership between quality improvement and competency-based education. Sargeant Joan, Wong Brian M, Campbell Craig M. 2018Medical Education. 52(1):125–135. doi: 10.1111/medu.13407. doi: 10.1111/medu.13407. [DOI] [PubMed] [Google Scholar]
- Competency-based medical education: theory to practice. Frank Jason R., Snell Linda S., Cate Olle Ten, Holmboe Eric S., Carraccio Carol, Swing Susan R., Harris Peter, Glasgow Nicholas J., Campbell Craig, Dath Deepak, Harden Ronald M., Iobst William, Long Donlin M., Mungroo Rani, Richardson Denyse L., Sherbino Jonathan, Silver Ivan, Taber Sarah, Talbot Martin, Harris Kenneth A. Jul 27;2010 Medical Teacher. 32(8):638–645. doi: 10.3109/0142159x.2010.501190. doi: 10.3109/0142159x.2010.501190. [DOI] [PubMed] [Google Scholar]
- Measuring the effect of a competency-based education conference for PAs and NPs. Laghezza Matthew, Clapper Timothy C., Christos Paul J., Sharma Rahul, Naik Neel. Sep;2019 JAAPA. 32(9):44–47. doi: 10.1097/01.jaa.0000578772.39180.0c. doi: 10.1097/01.jaa.0000578772.39180.0c. [DOI] [PubMed] [Google Scholar]
- Impact of a respiratory ICU rotation on resident knowledge and confidence in managing mechanical ventilation. Hayashi Fátima Kiyoko, Ayres Pedro Paulo Marino Rodrigues, Morais Anna Miethke, Laércio de Araújo Sousa Mayson, Valente Barbas Carmen Sílvia, Leite Vieira Costa Eduardo, Caruso Pedro, Carvalho Ferreira Juliana. 2020Jornal Brasileiro De Pneumologia. 46(5):e20190108. doi: 10.36416/1806-3756/e20190108. doi: 10.36416/1806-3756/e20190108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CoARC 2021 Report on Accreditation in Respiratory Care Education. [2022-7-8]. https://coarc.com/wp-content/uploads/2022/05/2021-CoARC-Report-on-Accreditation-Master-Copy-5.9.22.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table. Multi-state Model Output using > 80% Subject exposure to Respiratory Therapist