Abstract
Homeless shelter residents and staff may be at higher risk of SARS-CoV-2 infection. However, SARS-CoV-2 infection estimates in this population have been reliant on cross-sectional or outbreak investigation data. We conducted routine surveillance and outbreak testing in 23 homeless shelters in King County, Washington, to estimate the occurrence of laboratory-confirmed SARS-CoV-2 infection and risk factors during 1 January 2020–31 May 2021. Symptom surveys and nasal swabs were collected for SARS-CoV-2 testing by RT-PCR for residents aged ≥3 months and staff. We collected 12,915 specimens from 2,930 unique participants. We identified 4.74 (95% CI 4.00–5.58) SARS-CoV-2 infections per 100 individuals (residents: 4.96, 95% CI 4.12–5.91; staff: 3.86, 95% CI 2.43–5.79). Most infections were asymptomatic at the time of detection (74%) and detected during routine surveillance (73%). Outbreak testing yielded higher test positivity than routine surveillance (2.7% versus 0.9%). Among those infected, residents were less likely to report symptoms than staff. Participants who were vaccinated against seasonal influenza and were current smokers had lower odds of having an infection detected. Active surveillance that includes SARS-CoV-2 testing of all persons is essential in ascertaining the true burden of SARS-CoV-2 infections among residents and staff of congregate settings.
Keywords: cross-sectional study, homeless shelter, infection risk factors, molecular testing, SARS-CoV-2 incidence, Surveillance
Background
The coronavirus disease 2019 (COVID-19) pandemic has posed unprecedented challenges to the more than 580,000 people experiencing homelessness (PEH) estimated in the United States on a single night in 2020 [1]. These challenges exacerbated systemic inequities that adversely impact existing health conditions, access to health care, and work and living conditions, potentiating a disproportionate risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and its subsequent clinical manifestations among PEH. [2]. Difficulty with social distancing and the high prevalence of chronic diseases led to early concern that PEH in shelters would be at greater risk of COVID-19 complications [3, 4]. Homeless service providers may also face greater risk of exposure to SARS-CoV-2 as a result of working in a congregate living setting [5]. Because of this concern, many communities worked together with homeless service providers to put protective measures in place for residents [6].
However, implementation of consistently available SARS-CoV-2 testing in shelters has been challenging [7]. Most studies have relied on cross-sectional data or been centred on single outbreak investigations in specific geographies, limiting their generalisability [5, 8–10]. Robust testing data are vital to mitigating viral transmission through early identification and isolation of cases [11].
King County, Washington, has one of the largest populations of PEH in the United States (11,751 people on a single night in 2020) [12]. We previously described early characteristics of SARS-CoV-2 in King County shelters and detected a 2% test positivity rate [9]. Important questions remain as to whether certain individual- or shelter-level characteristics are associated with higher risk of infection among shelter residents and staff. In this study, we aimed to characterise the burden of disease among a diverse shelter population using data collected from active surveillance. We captured temporal trends and estimated the incidence and associated risk factors of SARS-CoV-2 infection among shelter residents and staff.
Methods
Study design overview and population
We conducted an active community-based surveillance study of SARS-CoV-2 cases in shelters across Seattle, King County, from 1 January 2020–31 May 2021. This was a sub-study of a multiyear, cluster randomised trial (CRT) of onsite testing and treatment for influenza at nine shelters that took place from 10/1/19 to 5/31/21 (registration number: NCT04141917) [13]. From 1 January 2020–31 March 2020, eligibility for participation was as follows: residents aged ≥3 months, those at a shelter study site, and those having cough alone or ≥ 2 new or worsening acute respiratory illness (ARI) symptoms with onset in the past 7 days. Once a month, eligibility was extended to residents aged ≥3 months regardless of symptoms. In response to the identification of SARS-CoV-2 community transmission in Washington state on 24 February 2020 [14], the first year of the influenza trial intervention was paused on 1 April 2020 and eligibility was expanded to include all shelter staff and residents aged ≥3 months, regardless of symptoms (Supplementary Figure S1). Participants eligible for COVID-19 testing did not have to be eligible for the influenza test-and-treat intervention during the study period, but they could elect to take part during surveillance months when the intervention was available for those who met additional criteria [15].
Study setting and sampling strategy
Participants were recruited 3 to 6 days per week by research staff at selected shelters using two mechanisms: routine surveillance and outbreak testing events. These mechanisms have been previously described [9]; in brief, routine surveillance involved self-selected participation at staffed kiosks in shelters during standardised days and times. COVID-19 outbreak testing was initiated on 30 March 2020 (and conducted intermittently thereafter) in collaboration with Public Health–Seattle & King County (PHSKC) with single-day intensive testing for all available residents and staff at shelters where ≥1 SARS-CoV-2 infections were recently detected. Individual participants were not followed longitudinally, but eligible individuals may have multiple encounters throughout the study period as routine testing was used as a study recruitment tool and proactive public health strategy. Study participation was limited to once weekly, unless new or worsening ARI symptoms developed, in which case an individual could re-enrol within 7 days. Participants were recruited from 23 shelters in total over the study period; routine surveillance and outbreak testing were conducted at 15 shelters, while outbreak-only testing was conducted at the other 8 shelters. Routine surveillance was conducted concurrently at 9 shelters at any given time over the study period; six of these shelters relocated staff and residents to new facilities to enable improved adherence to COVID-19 infection and prevention control measures, resulting in 15 shelters in total where routine surveillance occurred. Research activities were immediately initiated following these relocations (Supplementary Table S1).
Measures
The primary outcome was the incidence of reverse transcription polymerase chain reaction (RT-PCR)-confirmed SARS-CoV-2 infection, 1 January 2020–31 May 2021. All inconclusive testing results were classified as SARS-CoV-2 infections per PHSKC and Washington Department of Health guidelines [16]. Incidence is customarily defined as either the proportion of a population at risk that develops the outcome of interest over a specified time period (cumulative incidence) or the count of incidence cases divided by the aggregate amount of at-risk experience (incidence rate). This study describes incident infections detected through repeated cross-sectional testing in an open population of individuals who experienced homelessness or worked at a shelter at some point during the study period but were not necessarily at risk for its entirety; we were not able to capture individual time at risk.
Survey data were collected electronically on a tablet at the time of nasal swab collection from residents and staff. Data included participant sex, date of birth (DOB), race, ethnicity (Hispanic or Latino versus non-Hispanic or Latino), self-reported current season receipt of an influenza vaccine, underlying medical conditions, status as shelter staff versus resident, highest education level obtained, health insurance status, employment status, and self-reported receipt of any COVID-19 vaccine doses. Smoking status included any current use of tobacco products, e-cigarettes, or vape pens. Underlying conditions included asthma, blood disorders, cancer, chronic obstructive pulmonary disease or emphysema, chronic bronchitis, immunosuppression, liver disease, heart disease, diabetes, neurologic conditions, or aspirin therapy. All survey data characteristics presented in this analysis were collected from both residents and staff, with the exception of sleeping arrangements and duration of homelessness. Sleeping arrangements were reported only by shelter residents and categorised as communal, open-plan cubicles, or private rooms / shared family rooms. Communal included sleeping in a congregate space with bunk beds, bed mats, or rooms shared with more than one family. Enrolments per unique participant were defined as the number of survey responses collected from the same participant over the study period. All variables were determined by self-report.
Participant encounters with one or more new or worsening ARI symptoms with onset in the past 7 days were defined as symptomatic, and those without any new or worsening symptoms in the past 7 days were defined as asymptomatic. This phrasing aimed to specifically distinguish acute symptoms indicative of respiratory viral infection in a population with high rates of chronic illness [17]. Participants with ARI symptoms also had symptom duration data collected in response to the question, ‘When did the symptoms you mentioned at the beginning of this survey become new or worsening?’ Influenza-like illness (ILI) was defined as having a fever and either cough or sore throat. COVID-19–like illness (CLI) was defined as fever and cough or fever and increased difficulty breathing.
Specimen collection
Mid-turbinate nasal swabs were obtained using a sterile nylon flocked nasal swab (Copan Diagnostics) by a member of the research staff until 6 March 2020, after which participants self-collected a mid-turbinate nasal swab while observed by study staff. Due to supply shortages, anterior nares swabs replaced the use of mid-turbinate swabs from July 2020 through October 2020. See the Supplementary Material for specimen testing details.
Statistical analysis
The primary unit of analysis was unique participants, with corresponding individual-level characteristics taken from their last survey response. Participant encounters from unique individuals were dropped in this analysis following a positive or inconclusive test result; no persistent-positive test results or repeat infections were included in the analysis (n = 543; Supplementary Figure S2).
The incidence of SARS-CoV-2 infection was expressed as cases per 100 unique participants at risk and described by age group, sex, race, ethnicity, and shelter type. The overall incidence of SARS-CoV-2 infection was calculated by dividing the total number of confirmed cases across all shelters by the total number of unique participants tested over the study period with 95% confidence intervals (CIs).
Temporal trends of SARS-CoV-2 test positivity were also reported by epidemiologic week, a standardised method of counting weeks to allow for data comparison year after year [18]. For the specific purpose of calculating and depicting temporal trends of SARS-CoV-2 test positivity, we included all tests collected as the unit of analysis, regardless of participants’ frequency of testing.
Participant-level characteristics were summarised by using frequencies, percentages, and interquartile ranges. We used a chi-square test for independence for categorical variables (or Fisher’s exact test when cells had less than 10 observations) and a t-test for continuous variables of individual-level participant characteristics and SARS-CoV-2 infection, separately among shelter residents and shelter staff. To estimate corresponding adjusted associations with SARS-CoV-2 infection among staff and residents separately (Table 5) and symptomatic COVID-19 among all infected participants (Table 6), respectively, we used generalised linear mixed models (GLMMs), treating shelter as a random effect. Variables were selected for the models presented in Tables 5 and 6 using a causal diagram approach. Risk factors included in the final multivariable models were checked for multicollinearity and convergence issues due to excessive missingness (e.g., ‘duration of homelessness’ which was not asked of shelter staff). Descriptive statistics for test-level variables (Table 3) are presented but were not considered for inclusion in the multivariable models as we were primarily interested in fixed individual-level exposures.
Table 5.
Results of logistic regression analyses, unadjusted and adjusted, for factors associated with SARS-CoV-2 infection among residents and among staff, regardless of symptom profile, 1 January 2020–31 May 2021
| Resident (N = 2,360) | Staff (N = 570) | |||
|---|---|---|---|---|
| Variable | Unadjusted OR a (95% CI) | Multivariable aOR b (95% CI) | Unadjusted OR (95% CI) | Multivariable aOR (95% CI) |
| Age group | ||||
| <5 y | 1.33 (0.60–2.64) | 0.73 (0.27–1.98) | – | – |
| 5–11 y | 1.76 (0.89–3.23) | 1.21 (0.52–2.84) | – | – |
| 12–17 y | 1.46 (0.55–3.26) | 0.68 (0.19–2.51) | – | – |
| 18–49 y | Reference | Reference | ||
| 50–64 y | 1.41 (0.88–2.22) | 1.25 (0.66–2.38) | 1.03 (0.29–2.82) | 0.71 (0.16–3.16) |
| ≥65 y | 2.03 (0.98–3.88) | 1.68 (0.69–4.13) | 0.00 – Inf. | 0.00 – Inf. |
| Race | ||||
| American Indian and Alaskan Native | 1.15 (0.34–3.04) | 1.46 (0.46–4.61) | 0.00 – Inf. | 0.00 – Inf. |
| Asian | 0.00 – Inf. | 0.00 – Inf. | 1.00 (0.05–6.04) | 0.00 – Inf. |
| Black/African American | 1.83 (1.15–2.99) | 1.68 (0.98–2.86) | 3.11 (1.10–9.44) | 2.42 (0.68–8.59) |
| Multiracial | 1.17 (0.51–2.44) | 1.24 (0.54–2.85) | 2.24 (0.12–13.96) | 1.47 (0.14–15.22) |
| Native Hawaiian and Other Pacific Islander | 0.41 (0.07–1.40) | 0.24 (0.03–1.88) | 18.80 (4.27–77.35) | 22.37 (3.48–143.80) |
| White | Reference | Reference | ||
| Smoker (ref. No) | ||||
| Yes | 0.53 (0.36–0.79) | 0.34 (0.20–0.59) | 1.06 (0.34–2.74) | 0.52 (0.15–1.87) |
| Received seasonal influenza vaccine for corresponding influenza season (ref. No) | ||||
| Yes | 0.72 (0.48–1.07) | 0.54 (0.33–0.90) | 0.71 (0.28–1.70) | 0.98 (0.32–3.02) |
Unadjusted odds ratio (OR) between specified factor and SARS-CoV-2 infection using logistic regression; statistically significant results are bolded.
Adjusted odds ratio (aOR) for the association between the specified factor and SARS-CoV-2 infection using mixed effects logistic regression controlling for all other factors in the table, plus frequency of enrolment for each unique participant, and adjusting for correlation within each shelter (via inclusion of a random intercept). Resident model random intercept had a variance of 1.25 (SD, 1.12); staff model random intercept had a variance of 1.70 (SD, 1.30).
Table 6.
Factors associated with symptomatic COVID-19 (n = 36) among all unique participants with a SARS-CoV-2 infection detected (N = 139)
| Variable | Unadjusted OR (95% CI) a | Multivariable aOR (95% CI) b |
|---|---|---|
| Age group | ||
| <5 y | 0.66 (0.09–3.05) | 0.41 (0.04–4.24) |
| 5–11 y | 0.69 (0.14–2.58) | 0.79 (0.16–3.92) |
| 12–17 y | 0.00 – Inf. | 0.00 – Inf. |
| 18–49 y | Reference | Reference |
| 50–64 y | 0.86 (0.34–2.09) | 0.94 (0.30–2.94) |
| ≥65 y | 0.51 (0.07–2.24) | 0.65 (0.11–3.94) |
| Underlying medical condition (≥1) a | ||
| No | Reference | Reference |
| Yes | 1.62 (0.68–3.76) | 2.21 (0.79–6.19) |
| Received seasonal influenza vaccine for corresponding influenza season | ||
| No | Reference | Reference |
| Yes | 0.74 (0.32–1.66) | 0.62 (0.25–1.59) |
| Participant type | ||
| Staff | Reference | Reference |
| Resident | 0.34 (0.13–0.90) | 0.30 (0.10–0.97) |
Unadjusted odds ratio (OR) between specified factor and symptomatic COVID-19 (asymptomatic infection as reference group); statistically significant results have been bolded.
Adjusted odds ratio (aOR) for the association between specified factor and symptomatic SARS-CoV-2 infection using mixed effects logistic regression controlling for all other factors in the table, plus frequency of enrolment for each unique participant, and adjusting for correlation within each shelter (via inclusion of a random intercept).
Table 3.
Shelter-level characteristics by SARS-CoV-2 RT-PCR test result based on all participant encounters, 1 January 2020–31 May 2021 (N = 12,915)
| Residents | Staff | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive (n = 117, %) a |
Negative (n = 9,729, %) |
Total (N = 9,846) |
P-value | Positive (n = 22, %) |
Negative (n = 3,047, %) |
Total (N = 3,069) |
P-value | |
| Testing event | <0.01 | <0.01 | ||||||
| Routine | 87 (1.0%) | 8646 (99.0%) | 8733 (88.7%) | 14 (0.5%) | 2759 (99.5%) | 2773 (90.4%) | ||
| Outbreak | 30 (2.7%) | 1083 (97.3%) | 1113 (11.3%) | 8 (2.7%) | 288 (97.3%) | 296 (9.64%) | ||
| Shelter type | <0.01 | 0.16 | ||||||
| Adult female | 3 (0.7%) | 421 (99.3%) | 424 (4.31%) | 0 (0.0%) | 204 (100.0%) | 204 (6.65%) | ||
| Adult male | 33 (2.2%) | 1434 (97.8%) | 1467 (14.9%) | 4 (1.5%) | 260 (98.5%) | 264 (8.60%) | ||
| Family | 46 (1.4%) | 3337 (98.6%) | 3383 (34.4%) | 8 (0.7%) | 1179 (99.3%) | 1187 (38.7%) | ||
| Mixed adult | 32 (0.8%) | 3910 (99.2%) | 3942 (40.0%) | 8 (1.1%) | 750 (98.9%) | 758 (24.7%) | ||
| Youth | 3 (0.5%) | 627 (99.5%) | 630 (6.40%) | 2 (0.3%) | 654 (99.7%) | 656 (21.4%) | ||
| Sleeping arrangement | 0.06 | -- | ||||||
| Communal | 39 (1.3%) | 2869 (98.7%) | 2908 (29.5%) | NA | NA | NA | ||
| Cubicles | 3 (0.4%) | 791 (99.6%) | 794 (8.06%) | NA | NA | NA | ||
| Private/shared family rooms | 75 (1.2%) | 6069 (98.8%) | 6144 (62.4%) | NA | NA | NA | ||
All columns apart from ‘Total’ have calculated row percentages; ‘Total’ column percentages calculated exclude missing responses.
There was a high degree of missingness for certain variables that were added mid-study as we learned more about SARS-CoV-2 and COVID-19 (e.g., COVID-19 vaccination status and anosmia as a self-assessed symptom). However, sensitivity analyses showed this had little effect on the associated risk factors assessed through multivariable regression.
Ethics approval was obtained from the University of Washington Human Subjects Division. The CDC determined that the study was conducted consistent with applicable federal law and CDC policy (see 45 C.F.R part 46; 21 C.F.R. part 56).
Results
Participant characteristics
Overall, 12,915 nasal swab specimens were collected from 2,930 unique participants from 1 January 2020 through 31 May 2021. Of these participants, 2,360 were shelter residents (80.5%) and 570 (19.5%) were shelter staff (Table 1). Each participant was tested a median of two times (interquartile ranges (IQRs) of [4] and [5] among residents and staff, respectively) over the study period. The median age of residents and staff was 37 (range: 0–85) and 32.5 (range: 18–81 ) years, respectively. A majority of residents self-identified as male (64.3%), whereas a majority of staff self-identifying as female (58.2%). A plurality of residents self-identified as Black (39.3%), whereas the majority of staff self-identified as White (55.0%). Receipt of seasonal influenza vaccines for the corresponding influenza season was reported by 42.5% of residents and 51.1% of staff. Among residents, 45.6% (n = 611) had experienced chronic homelessness (duration ≥1 year) and 17.5% (n = 191) of residents were employed.
Table 1.
Participant characteristics by SARS-CoV-2 RT-PCR test result, by shelter staff and residents, based on last survey response a, 1 January 2020–31 May 2021 (N = 2,930)
| Residents | Staff | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive (n = 117, %) b |
Negative (n = 2,243, %) |
Total (N = 2360) |
P-value | Positive (n = 22, %) |
Negative (n = 548, %) |
Total ( N = 570) |
P-value | |
| Demographic | ||||||||
| Median age (IQR) | 41.0 (39.0) | 37.0 (31.0) | 37.0 (32.0) | 0.30 | 38.0 (14.8) | 32.0 (22.0) | 32.5 (22.0) | 0.28 |
| Age group | 0.26 | 0.99 | ||||||
| <5 y | 9 (5.2%) | 165 (94.8%) | 174 (7.37%) | NA | NA | NA | NA | |
| 5–11 y | 13 (6.7%) | 180 (93.3%) | 193 (8.18%) | NA | NA | NA | NA | |
| 12–17 y | 6 (5.7%) | 99 (94.3%) | 106 (4.49%) | NA | NA | NA | NA | |
| 18–49 y | 45 (3.9%) | 1096 (96.1%) | 1140 (48.3%) | 18 (4.0%) | 434 (96.0%) | 452 (79.3%) | ||
| 50–64 y | 33 (5.5%) | 571 (94.5%) | 604 (25.6%) | 4 (4.1%) | 94 (95.9%) | 98 (17.2%) | ||
| ≥65 y | 11 (7.7%) | 132 (92.3%) | 143 (6.06%) | 0 (0.0%) | 20 (100.0%) | 20 (3.51%) | ||
| Sex | 0.30 | 0.19 | ||||||
| Male | 79 (5.3%) | 1405 (94.7%) | 1484 (64.3%) | 6 (2.6%) | 227 (97.4%) | 233 (41.8%) | ||
| Female | 35 (4.2%) | 789 (95.8%) | 824 (35.7%) | 16 (4.9%) | 309 (95.1%) | 325 (58.2%) | ||
| Race | 0.02 | <0.01 | ||||||
| American Indian and Alaskan Native | 4 (4.4%) | 87 (95.6%) | 91 (4.68%) | 0 (0.0%) | 7 (100.0%) | 7 (1.34%) | ||
| Asian | 0 (0.0%) | 59 (100.0%) | 59 (3.03%) | 1 (2.1%) | 47 (97.9%) | 48 (9.16%) | ||
| Black/African American | 52 (6.8%) | 712 (93.2%) | 764 (39.3%) | 9 (6.2%) | 136 (93.8%) | 145 (27.7%) | ||
| Multiracial | 9 (4.5%) | 193 (95.5%) | 202 (10.4%) | 1 (4.5%) | 21 (95.5%) | 22 (4.20%) | ||
| Native Hawaiian and Other Pacific Islander | 2 (1.6%) | 122 (98.4%) | 124 (6.38%) | 4 (28.6%) | 10 (71.4%) | 14 (2.67%) | ||
| White | 27 (3.8%) | 678 (96.2%) | 705 (36.2%) | 6 (2.1%) | 282 (97.9%) | 288 (55.0%) | ||
| Hispanic/Latinx ethnicity | 0.60 | 0.99 | ||||||
| No | 96 (5.0%) | 1810 (95.0%) | 1906 (82.7%) | 20 (3.9%) | 491 (96.1%) | 511 (90.3%) | ||
| Yes | 17 (4.3%) | 382 (95.7%) | 399 (17.3%) | 2 (3.6%) | 53 (96.4%) | 55 (9.72%) | ||
| Smoker | <0.01 | 0.99 | ||||||
| No | 79 (6.3%) | 1180 (93.7%) | 1259 (53.3%) | 17 (3.8%) | 429 (96.2%) | 446 (78.2%) | ||
| Yes | 38 (3.5%) | 1063 (96.5%) | 1101 (46.7%) | 5 (4.0%) | 119 (96.0%) | 124 (21.8%) | ||
| Received seasonal influenza vaccine for corresponding influenza season | 0.13 | 0.51 | ||||||
| No | 72 (5.7%) | 1197 (94.3%) | 1269 (57.5%) | 12 (4.4%) | 258 (95.6%) | 270 (48.9%) | ||
| Yes | 39 (4.2%) | 898 (95.8%) | 937 (42.5%) | 9 (3.2%) | 273 (96.8%) | 282 (51.1%) | ||
| Median no. of enrolments c (IQR) | 4.00 (10.0) | 2.00 (4.0) | 2.00 (4.0) | <0.01 | 5.50 (10.8) | 2.00 (5.0) | 2.00 (5.0) | 0.16 |
| Self-reported duration of homelessness | 0.02 | |||||||
| <6 months | 11 (2.2%) | 493 (97.8%) | 504 (37.6%) | NA | NA | NA | NA | |
| 6–12 months | 5 (2.2%) | 220 (97.8%) | 225 (16.8%) | NA | NA | NA | NA | |
| 12–24 months | 9 (6.2%) | 135 (93.8%) | 144 (10.7%) | NA | NA | NA | NA | |
| >24 months | 23 (4.9%) | 444 (95.1%) | 467 (34.9%) | NA | NA | NA | NA | |
| Highest education level | 0.99 | <0.01 | ||||||
| Less than high school | 18 (3.7%) | 472 (96.3%) | 492 (37.3%) | 1 (14.3%) | 6 (85.7%) | 7 (2.17%) | ||
| High school/GED | 16 (3.6%) | 424 (96.4%) | 439 (33.3%) | 7 (11.1%) | 56 (88.9%) | 63 (19.6%) | ||
| Some college | 12 (3.9%) | 293 (96.1%) | 305 (23.1%) | 0 (0.0%) | 81 (100.0%) | 81 (25.2%) | ||
| Bachelors or higher | 3 (3.6%) | 80 (96.4%) | 83 (6.29%) | 9 (5.3%) | 162 (94.7%) | 171 (53.1%) | ||
| Employed d | 0.56 | 0.99 | ||||||
| No | 36 (4.0%) | 867 (96.0%) | 902 (82.5%) | 1 (4.5%) | 21 (95.5%) | 22 (6.77%) | ||
| Yes | 10 (5.2%) | 181 (94.8%) | 191 (17.5%) | 16 (5.3%) | 287 (94.7%) | 303 (93.2%) | ||
| Health insurance | 0.02 | 0.99 | ||||||
| No | 2 (1.0%) | 189 (99.0%) | 191 (14.1%) | 0 (0.0%) | 10 (100.0%) | 10 (3.13%) | ||
| Yes | 50 (4.3%) | 1116 (95.7%) | 1166 (85.9%) | 17 (5.5%) | 293 (94.5%) | 310 (96.9%) | ||
Abbreviations: GED, General Educational Development; IQR, interquartile range; NA, not available.
Final survey responses were not collected on the same calendar dates within the study period and are instead representative of the last study encounter from each unique participant.
All columns apart from ‘Total’ have calculated row percentages; ‘Total’ column percentages calculated exclude missing responses.
Number of times each unique participant enrolled in the study and had a nasal specimen/survey collected.
Shelter staff included both unpaid volunteers and paid employees.
Among unique participants, 80.3% (n = 1,894, Table 2) of residents and 89.5% (n = 510) of staff were asymptomatic when specimens were collected. Among symptomatic participants (residents, n = 466; staff, n = 60), the most commonly reported symptoms were cough (51.5%), sore throat (33.5%), and fatigue (32.6%) for residents, and cough (25.0%), fatigue (25.0%), sore throat (26.7%), and headache (26.7%) for staff. Based on their last survey response, 18.6% of residents and 49.3% of staff had received ≥1 COVID-19 vaccine dose; however, only 15% of these individuals completed their final study enrolment from 31 March 2021 onwards (when vaccine eligibility expanded to include anyone living in congregate settings) [19], limiting interpretability.
Table 2.
Clinical characteristics by SARS-CoV-2 RT-PCR test result, by shelter staff and residents, based on last survey response a, 1 January 2020–31 May 2021
| Residents | Staff | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive (n = 117, %) b |
Negative (n = 2,243, %) |
Total (N = 2,360) |
P-value | Positive n = 22 (%) |
Negative (n = 548, %) |
Total ( N = 570) |
P-value | |
| Clinical and illness | ||||||||
| Underlying medical condition (≥1) c | 0.37 | 0.95 | ||||||
| No | 89 (5.2%) | 1611 (94.8%) | 1700 (72.0%) | 17 (4.0%) | 407 (96.0%) | 424 (74.4%) | ||
| Yes | 28 (4.2%) | 632 (95.8%) | 660 (28.0%) | 5 (3.4%) | 141 (96.6%) | 146 (25.6%) | ||
| COVID-like illness (CLI) d | 3 (4.2%) | 69 (95.8%) | 72 (3.05%) | 0.99 | 1 (50.0%) | 1 (50.0%) | 2 (0.351%) | 0.08 |
| Influenza-like illness (ILI) e | 3 (3.8%) | 75 (96.2%) | 78 (3.31%) | 0.99 | 2 (66.7%) | 1 (33.3%) | 3 (0.526%) | 0.11 |
| Reported symptoms | ||||||||
| None | 91 (77.8%) | 1803 (80.4%) | 1894 (80.3%) | 0.57 | 12 (54.5%) | 498 (90.9%) | 510 (89.5%) | <0.01 |
| Cough | 11 (9.40%) | 229 (10.2%) | 240 (10.2%) | 0.90 | 3 (13.6%) | 12 (2.19%) | 15 (2.63%) | 0.02 |
| Shortness of breath | 4 (3.42%) | 79 (3.52%) | 83 (3.52%) | 0.99 | 2 (9.09%) | 4 (0.73%) | 6 (1.05%) | 0.02 |
| Fever | 4 (3.42%) | 96 (4.28%) | 100 (4.24%) | 0.82 | 2 (9.09%) | 4 (0.73%) | 6 (1.05%) | 0.02 |
| Loss of taste/smell | 0 (0%) | 7 (0.31%) | 7 (0.30%) | 0.99 | 1 (4.55%) | 1 (0.18%) | 2 (0.35%) | 0.08 |
| Sore throat | 7 (5.98%) | 149 (6.64%) | 156 (6.61%) | 0.99 | 3 (13.6%) | 13 (2.37%) | 16 (2.81%) | 0.01 |
| Headache | 4 (3.42%) | 127 (5.66%) | 131 (5.55%) | 0.41 | 3 (13.6%) | 13 (2.37%) | 16 (2.81%) | 0.02 |
| Fatigue | 7 (5.98%) | 145 (6.46%) | 152 (6.44%) | 0.99 | 3 (13.6%) | 12 (2.19%) | 15 (2.63%) | 0.02 |
| Other f | 23 (19.7%) | 365 (16.3%) | 388 (16.4%) | 0.40 | 8 (36.4%) | 21 (3.83%) | 29 (5.09%) | <0.01 |
| Days from symptom onset to swab collection (n = 350) |
0.02 | 0.55 | ||||||
| ≤2 days | 8 (5.4%) | 139 (94.6%) | 147 (44.7%) | 5 (33.3%) | 10 (66.7%) | 15 (71.4%) | ||
| 3–4 days | 6 (6.8%) | 82 (93.2%) | 88 (26.7%) | 0 (0.0%) | 4 (100.0%) | 4 (19.0%) | ||
| 5–7 days | 0 (0.0%) | 94 (100.0%) | 94 (28.6%) | 0 (0.0%) | 2 (100.0%) | 2 (9.52%) | ||
| ≥1 COVID-19 vaccine dose received g (n = 334) | 0.09 | 0.50 | ||||||
| No | 15 (2.6%) | 557 (97.4%) | 572 (81.4%) | 2 (2.7%) | 72 (97.3%) | 74 (50.7%) | ||
| Yes | 0 (0.0%) | 131 (100%) | 131 (18.6%) | 0 (0.0%) | 72 (100%) | 72 (49.3%) | ||
Final survey responses were not collected on the same calendar dates within the study period and are instead representative of the last study encounter from each unique participant.
All columns apart from ‘Total’ and ‘Reported symptoms’ have calculated row percentages; ‘Total’ column percentages calculated exclude missing responses.
Asthma, blood disorders, cancer, chronic obstructive pulmonary disease or emphysema, chronic bronchitis, immunosuppression, liver disease, heart disease, diabetes, neurologic conditions, or aspirin therapy.
Fever and cough or increased difficulty breathing.
Fever and cough or fever and sore throat.
Chills, diarrhoea, ear pain or discharge, myalgia, runny nose, nausea/vomiting, rash, or sweats.
Participants were not asked to report COVID-19 vaccination intent or uptake until November 1, 2020; COVID-19 vaccination eligibility was not expanded to include homeless service staff or residents until March 31, 2021 in Washington State.
Shelter characteristics
Table 3 presents shelter characteristics by SARS-CoV-2 test result. Nearly 90% (n = 11,506) of swabs were collected during routine surveillance testing events, and a plurality were collected from shelters serving mixed gender adults (36.4%, n = 4,700 residents and staff). Among residents, most tests were collected from participants sleeping in private/shared rooms or rooms serving single family units (62.4%, n = 6,144).
Incidence of SARS-CoV-2 infection
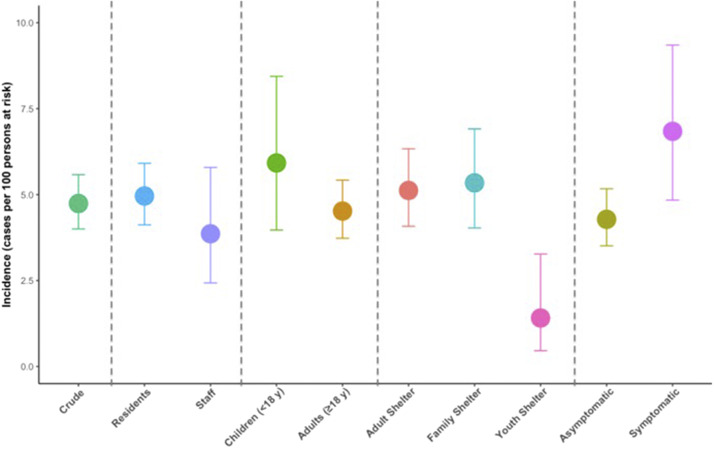
A total of 139 cases of SARS-CoV-2 infection were detected over the study period. The overall estimated incidence of infection was 4.74 (95% CI 4.00–5.58) cases per 100 individuals at risk. Among unique shelter residents, the incidence was 4.96 (95% CI 4.12–5.91) cases per 100 individuals at risk compared to 3.86 (95% CI 2.43–5.79, Table 4) among staff. Incidence was the highest among residents aged ≥65 years (7.69 cases per 100, 95% CI 3.90–13.35). Black participants had the highest observed incidence of infection compared to other racial groups (residents: 6.81, 95% CI 5.12–8.83; staff: 6.21, 95% CI 2.88–11.46). When stratifying by shelter type, incidence was lower in youth shelters (1.41, 95% CI 0.46–3.27) than in adult and family shelters. Incidence was higher among symptomatic individuals (6.84 cases per 100, 95% CI 4.84–9.35) than among asymptomatic individuals (4.28, 95% CI 3.51–5.17, Figure 1).
Table 4.
Incidence estimates for SARS-CoV-2 RT-PCR-positive test results among unique study participants. Characteristics are based on last survey response a
| Residents | Staff | |||||
|---|---|---|---|---|---|---|
| Characteristic | Positive | Total tested | Incidence (95% CI) per 100 persons at risk | Positive | Total tested | Incidence (95% CI) per 100 persons at risk |
| Overall | 117 | 2,360 | 4.96 (4.12–5.91) | 22 | 570 | 3.86 (2.43–5.79) |
| Age group | ||||||
| <5 y | 9 | 174 | 5.17 (2.39–9.59) | – | – | – |
| 5–11 y | 13 | 193 | 6.74 (3.63–11.24) | – | – | – |
| 12–17 y | 6 | 106 | 5.66 (2.11–11.91) | – | – | – |
| 18–49 y | 45 | 1,140 | 3.94 (2.89–5.25) | 18 | 452 | 3.98 (2.38–6.22) |
| 50–64 y | 33 | 604 | 5.46 (3.79–7.59) | 4 | 98 | 4.08 (1.12–10.12) |
| ≥65 y | 11 | 143 | 7.69 (3.90–13.35) | 0 | 20 | – |
| Sex | ||||||
| Female | 35 | 824 | 4.25 (2.98–5.86) | 16 | 325 | 5.92 (2.84–7.87) |
| Male | 79 | 1,484 | 5.32 (4.24–6.59) | 6 | 233 | 2.58 (0.95–5.52) |
| Race | ||||||
| American Indian and Alaskan Native | 4 | 91 | 4.40 (1.21–10.87) | 0 | 7 | – |
| Asian | 0 | 59 | – | 1 | 48 | 2.08 (0.05–11.07) |
| Black/African American | 52 | 764 | 6.81 (5.12–8.83) | 9 | 145 | 6.21 (2.88–11.46) |
| Multiracial | 9 | 202 | 4.46 (2.06–8.29) | 1 | 22 | 4.55 (0.12–22.84) |
| Native Hawaiian and Other Pacific Islander | 2 | 124 | 1.61 (0.20–5.70) | 4 | 14 | 28.57 (8.39–58.10) |
| White | 27 | 705 | 3.83 (2.54–5.52) | 6 | 288 | 2.08 (0.77–4.48) |
| Hispanic/ Latinx |
||||||
| Yes | 17 | 399 | 4.26 (2.50–6.73) | 2 | 55 | 3.63 (0.44–12.53) |
| No | 96 | 1,906 | 5.03 (4.09–6.12) | 20 | 511 | 3.91 (2.41–5.98) |
| Shelter type | ||||||
| Adult | 68 | 1,329 | 5.12 (3.99–6.44) | 12 | 235 | 5.11 (2.67–8.75) |
| Family | 46 | 851 | 5.41 (3.98–7.14) | 8 | 161 | 4.97 (2.17–9.56) |
| Youth | 3 | 180 | 1.67 (0.35–4.79 | 2 | 174 | 1.15 (0.14–4.09) |
Final survey responses were not collected on the same calendar dates within the study period and are instead representative of the last study encounter from each unique participant.
Figure 1.
Crude incidence estimates among all unique participants, plus stratifications: (a) resident versus staff; (b) children versus adults; (c) shelter type (adult, family, youth); (d) asymptomatic versus symptomatic (≥1 symptom).
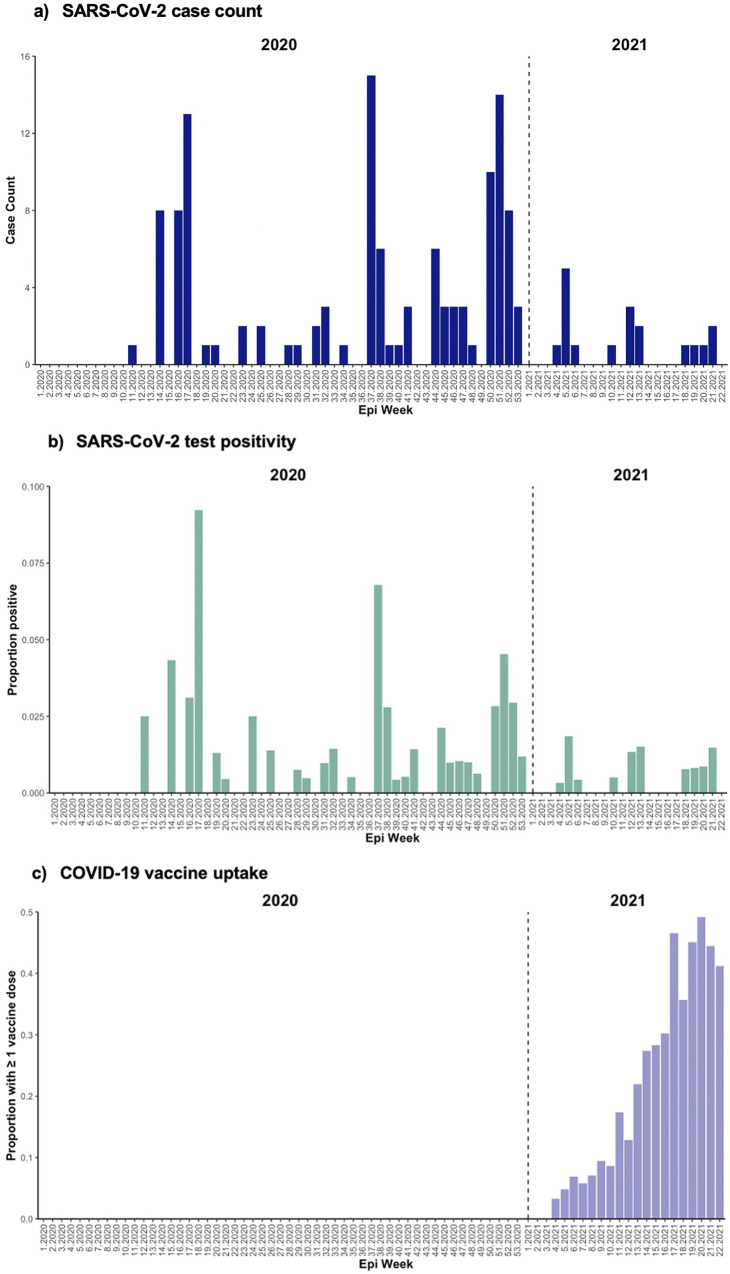
Among 2,930 persons tested, SARS-CoV-2 infections peaked in Week 37 (6 September 2020–12 September 2020) of 2020 with 15 unique participants testing positive, with additional peaks in infections observed in Week 17 (19 April 2020–25 April 2020) and Week 51 (13 December 2020–19 December 2020) of 2020 and continued detection observed through the duration of the study period (Figure 2a). Among 12,915 tests performed, SARS-CoV-2 test positivity peaked earlier at 9% in epidemiologic Week 17 of 2020 (Figure 2b). The proportion of participant encounters self-reporting at least one dose of a COVID-19 vaccine is represented in Figure 2c; we observed a consistent trend towards increased vaccine uptake from Week 4 (24 January 2021–30 January 2021) in 2021 through the end of the study period.
Figure 2. (.
a)–(c) Epidemic curves of SARS-CoV-2 case count (a; N = 139); test positivity (b; N = 139/12,915); and COVID-19 vaccine uptake (≥1 dose) (c; N = 597/12,915) by epidemiological week.
Combining data from residents and staff, most infections were asymptomatic at the time of detection (74%, 103/139, Table 2) and detected during routine surveillance (73%, 101/139, Table 3). Overall test positivity was 1.2%; however, outbreak testing yielded higher positivity (2.7%, 38/1,409 versus 0.9%, 101/11,506, Table 3).
Factors associated with SARS-CoV-2 infection
Based on unique participants’ last surveys (N = 2,930), unadjusted models show that among residents, Black race (OR = 1.83, 95% CI 1.15–2.99) was significantly associated with higher odds of SARS-CoV-2 infection, whereas residents who were current smokers had a decreased odds of infection (OR = 0.53, 95% CI 0.36–0.79). Adjusting for other model variables (Table 5), residents who smoked had 66% (aOR = 0.34, 95% CI 0.20–0.59) lower odds of SARS-CoV-2 infection than non-smokers, and residents who had received that season’s influenza vaccine had 46% (aOR = 0.54, 95% CI 0.33–0.90) lower odds of infection than those who had not received an influenza vaccine. Among staff, Native Hawaiian and Other Pacific Islander (NHPI) race was also identified with a significant association; however, the validity of this finding is undermined due to the small sample size of NHPI participants.
Individual factors associated with symptomatic COVID-19
When assessing factors associated with symptomatic COVID-19 among unique participants (n = 36) with SARS-CoV-2 infections detected (n = 139), the only variable significantly associated with symptomatic infection was staff versus resident status (Table 6). Adjusting for other variables, shelter residents had 70% (0.30, 95% CI 0.10–0.97) lower odds of reporting ≥1 new or worsening symptom within 7 days of sample collection than shelter staff.
Discussion
From 1 January 2020 through 31 May 2021, we conducted active surveillance in 23 homeless shelters in King County, Washington. We detected an incidence of 4.74 SARS-CoV-2 cases per 100 persons at risk and identified risk factors associated with infection. Most infections were detected during routine surveillance, and staff were more likely to report symptoms than residents among those infected.
Among King County’s estimated population of 2.26 million people, there were 106,347 confirmed cases reported from the start of the pandemic through 5/31/21; an incidence of 4.71 cases per 100 persons can be calculated based on these figures [20]. This striking similarity in disease burden when compared to our findings may be reflective of our study’s early focus on testing asymptomatic individuals: if only symptomatic individuals in our study received testing, as was largely the case for the greater King County community during the early months of the pandemic, the denominator of persons at risk may have been smaller but more likely to test positive. Calculated incidence as a result would have been higher in the shelters than among the general population. As of 1/4/22, PEH comprised 1.4% of COVID-19 cases in King County but only represented 0.5% of its population [21]. Additionally, 12.4% of PEH reported to PHSKC were hospitalised due to COVID-19 compared to 3.3% among King County’s general population [21]. A population-level study in Wales, UK, found that SARS-CoV-2 prevalence among PEH was lower than that among the general population [22]. However, this study and others may not account for the differential healthcare-seeking behaviour or time at risk between PEH and non-PEH, which may result in an under-detection of infections when testing is performed in a clinical setting. Despite differential testing methodologies between the general population and our study, we did observe similar temporal trends and spikes in test positivity in mid-April and late December 2020, supporting previously published evidence of genetic relationships and synergistic transmission dynamics with the broader community [20, 23].
A model of SARS-CoV-2’s potential effect among the U.S. PEH population published in late March 2020 projected that 40% of the population would be infected at pandemic’s peak due to conditions at homeless service sites and a high prevalence of medical comorbidities [24]. Comparable cross-sectional results were reported in an adult shelter in Boston, MA, USA, where an outbreak investigation yielded 36% test positivity, while one in San Francisco, CA, USA, yielded even higher test positivity (67%) [8, 25]. These estimates and results from specific outbreak testing demonstrate a substantially higher burden than that observed in this study during similar time periods, likely due to discrepant testing methodologies (e.g., data from the San Francisco and Boston studies were collected from contact tracing efforts post-outbreak), in addition to regional differences in background community prevalence. A systematic review of studies addressing COVID-19 and health-related outcomes in PEH and shelter staff estimated a pooled SARS-CoV-2 prevalence of 32% among PEH in an outbreak context compared to 2% in the absence of an acute outbreak [5]. This analysis, however, was limited by the relatively short observational periods of its studies.
A substantial proportion of SARS-CoV-2 infections in our study were asymptomatic at the time specimens were collected. Prior studies of seropositive cases in shelters found that 68–85% of all cases had no symptoms at the time of testing [9, 26–28]. An Atlanta, Georgia, USA, study of symptom evolution of PEH staying in isolation hotels after testing positive for SARS-CoV-2 found 32% of community referrals became symptomatic after testing positive [29]. Our participants were not longitudinally followed after detection, but our data add to the evidence that asymptomatic routine testing of all staff and residents is important in congregate living settings.
SARS-CoV-2-positive staff were more likely to report symptoms than residents. This has important implications. First, residents might be hesitant or unable to report symptoms [30]. Second, regardless of policies in place, staff may have worked while experiencing COVID-19 symptoms due to unavailability of paid sick leave, fear of job loss [31], or dedication to their roles as essential workers. A study of SARS-CoV-2 molecular epidemiology in shelters found evidence that most infections were the result of intra-shelter transmission while staff working across multiple facilities may have introduced the virus into some of the facilities [23]. This finding may also be an artefact of surveillance timing, given that residents were less consistently surveilled than staff, and therefore, their positive tests may have been taken well into their course of infection (i.e., persistent positives).
We found that the highest test positivity was detected in adult male shelters, all of which provided services 24 hours per day. Comparatively, the youth shelters included in this study, which had the lowest observed test positivity, closed services during the day, likely reducing social mixing in both formal and informal communal spaces. King County’s swift creation of nearly 2,000 new spaces (i.e., beds, isolation, or quarantine areas) in homeless service sites likely had a substantial impact on mitigating transmission [29, 32, 33]. Specifically, protocols enacted by PHSKC that relocated consenting SARS-CoV-2-positive shelter residents from our study sites to medically attended isolation and quarantine units likely reduced incidence. The lack of significant association between sleeping arrangements and risk of infection in our study suggests that other factors, such as intra-shelter social mixing patterns, are facilitating virus transmission, especially in facilities with non-congregate sleeping arrangements but shared hygiene and communal spaces. The provision of high-efficiency particulate air (HEPA) filters by PHSKC to shelters during the pandemic may have also reduced particulate matter exposure and subsequently impacted SARS-CoV-2 incidence in our study population [34]. However, a simulation study found that in shelters at high risk of a SARS-CoV-2 outbreak, no additional non-pharmaceutical infection control strategy is likely to prevent outbreaks [35]. This evidence supports the prioritisation of non-congregate housing options for PEH.
Our findings suggest that over a prolonged surveillance period, environmental and behavioural factors may obfuscate associations between SARS-CoV-2 infection and individual-level risk factors. The protective association observed between influenza vaccination and SARS-CoV-2 infection is consistent with the published literature [36–38], as well as the negative association between smoking and infection [39]. However these studies were subject to methodological limitations and probable confounding variables [39–42], and there is no consensus about either relationship. Furthermore, these associations were only observed among residents, limiting our ability to conclude if they are reflective of true biological mechanisms, behavioural differences, or unobserved confounding variables.
This study has several limitations. The repeated cross-sectional nature of this study in an open population where participant time at risk was not calculable likely resulted in an underestimation of the true disease burden. For these reasons, more specific measures of disease occurrence such as ‘cumulative incidence’ or ‘incidence rate’ could not be applied to this study population. Another limitation is our inability to differentiate between pre-symptomatic, asymptomatic, and convalescent cases due to the cross-sectional design of this study and limiting self-report of new or worsening from <7 days. We also did not have a complete infection history of study participants before their entry into the shelters, likely resulting in an underestimation of incident infection – especially among residents who are less consistently surveilled in this study population – given the protective effect of SARS-CoV-2 infection history [43]. Finally, data on organisational infection prevention methods instituted to mitigate transmission were not routinely collected in this study, and therefore, their impact could not be examined.
Conclusion
To our knowledge, this is one of the first studies to capture temporal trends and estimate incident SARS-CoV-2 infections among shelter populations through prolonged, active surveillance efforts. Our findings suggest that routine surveillance for SARS-CoV-2 that includes testing of all persons, regardless of symptoms, is essential for ascertaining the true burden of disease among residents and staff of congregate settings. As the COVID-19 pandemic evolves [44], additional studies are recommended to assess the cost-effectiveness of routine shelter-based SARS-CoV-2 testing and the impact of transmission mitigation efforts in low-resource, congregate living settings.
Supporting information
Rogers et al. supplementary material
Acknowledgements
We thank the shelter staff and program managers for their cooperation and collaboration throughout the participant recruitment process. A special thanks to all participants and the research assistants who assisted with data collection.
Supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268823001036.
click here to view supplementary material
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author contribution
Data curation: E.M., E.J.C., B.P., A.L., G.N., P.H., S.C., J.H.R.; Formal analysis: E.M., E.J.C., M.E.H., J.H., T.U., M.R., J.H.R.; Investigation: E.M., E.J.C., J.D., H.C., J.E., J.H., L.S., M.B., M.M.S., T.U., M.R.; Methodology: E.M., H.C., J.E., J.H., M.B., S.C., T.U., M.R.; Supervision: E.M., M.E.H., H.C., J.E., J.H., M.B., T.U., M.R.; Writing – original draft: E.M., J.E., J.H.R.; Writing – review & editing: E.M., E.J.C., J.D., M.E.H., B.P., C.W., H.C., J.E., J.H., L.S., A.L., M.B., M.M.S., G.N., P.H., S.C., T.U., M.R.; Conceptualization: E.J.C., H.C., J.E., J.H., L.S., M.B., T.U., M.R., J.H.R.; Resources: J.D., B.P., C.W., H.C., L.S., A.L., G.N., P.H., S.C.; Validation: J.D., M.M.S., S.C.; Project administration: B.P., C.W., A.L., G.N., P.H., S.C., J.H.R.; Funding acquisition: H.C.
Financial support
This work was supported by Gates Ventures and the Centers for Disease Control and Prevention (75D30120C09322).
Competing interest
Dr. Chu reported consulting with Ellume, Pfizer, the Bill & Melinda Gates Foundation, Glaxo Smith Kline, and Merck. She has received research funding from Gates Ventures and Sanofi Pasteur, and support and reagents from Ellume and Cepheid outside of the submitted work. Dr. Englund reported research support from Merck, AstraZeneca, Pfizer, and GlaxoSmithKline. She is a consultant for Meissa Vaccines, Sanofi Pasteur, and Astra Zeneca.
Disclaimers
The findings and conclusions in this report are those of the authors and do not necessarily represent the view of the U.S. Centers for Disease Control and Prevention.
References
- [1].Henry M, de Sousa T, Roddey C, Gayen S and Bednar TJ (2020). The 2020 Annual Homeless Assessment Report (AHAR) to Congress [Internet]. Available at https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf. Accessed 2 August 2022.
- [2].Hsu HE, Ashe EM, Silverstein M, Hofman M, Lange SJ, Razzaghi H, Mishuris RG, Davidoff R, Parker EM, Penman-Aguilar A, Clarke KEN, Goldman A, James TL, Jacobson K, Lasser KE, Xuan Z, Peacock G, Dowling NF, Goodman AB (2020). Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an urban safety-net medical center — Boston, Massachusetts, 2020. MMWR Morbidity and Mortality Weekly Report 69(27), 864–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Toseef MU, Armistead I, Bacon E, Hawkins E, Bender B, Podewils LJ and Hurley H (2022). Missed appointments during COVID-19: The impact of telehealth for persons experiencing homelessness with substance use disorders. Asian Journal of Psychiatry 69, 102987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tsai J and Wilson M (2020). COVID-19: A potential public health problem for homeless populations. The Lancet Public Health 5(4), e186–e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mohsenpour A, Bozorgmehr K, Rohleder S, Stratil J and Costa D (2021). SARS-Cov-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: Systematic review and meta-analysis. EClinicalMedicine 38, 101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Huggett TD, Tung EL, Cunningham M, Ghinai I, Duncan HL, McCauley ME and Detmer WM (2021). Assessment of a hotel-based protective housing program for incidence of SARS-CoV-2 infection and management of chronic illness among persons experiencing homelessness. JAMA Network Open 4(12), e2138464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Voices from the Field: COVID-19 and Recession Surveys, Interviews, and Data [Internet]. National Alliance to End Homelessness (2020). Available at https://endhomelessness.org/wp-content/uploads/2020/03/COVID-19-Survey-Final-Report.pdf.
- [8].Baggett TP, Keyes H, Sporn N and Gaeta JM (2020). Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA - Journal of the American Medical Association 323(21), 2191–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rogers JH, Link AC, McCulloch D, Brandstetter E, Newman KL, Jackson ML, Hughes JP, Englund JA, Boeckh M, Sugg N, Ilcisin M, Sibley TR, Fay K, Lee J, Han P, Truong M, Richardson M, Nickerson DA, Starita LM, Bedford T, and Chu HY (2021). Characteristics of COVID-19 in homeless shelters. Annals of Internal Medicine 174(1), 42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chang YS, Mayer S, Davis ES, Figueroa E, Leo P, Finn PW and Perkins DL (2020). Transmission dynamics of large coronavirus disease outbreak in homeless shelter, Chicago, Illinois, USA, 2020. Emerging Infectious Diseases 28(1), 76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gray D, Chau S, Huerta T and Frankish J (2011). Urban-rural migration and health and quality of life in homeless people. Journal of Social Distress and the Homeless 20(1–2), 75–93. [Google Scholar]
- [12].Winslow D, Van T, Green L, Donahue L, Jain V and Garcia TT (2020). Seattle/King County Point-in-Time Count of Individuals Experiencing Homelessness [Internet]. Seattle. Available at https://kcrha.org/wp-content/uploads/2020/07/Count-Us-In-2020-Final.pdf.
- [13].Newman KL, Rogers JH, McCulloch D, Wilcox N, Englund JA, Boeckh M, Uyeki TM, Jackson ML, Starita L, Hughes JP and Chu HY (2020). Point-of-care molecular testing and antiviral treatment of influenza in residents of homeless shelters in Seattle, WA: Study protocol for a stepped-wedge cluster-randomized controlled trial. Trials 21(1), 956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chu HY, Englund JA, Starita LM, Famulare M, Brandstetter E, Nickerson DA, Rieder MJ, Adler A, Lacombe K, Kim AE, Graham C, Logue J, Wolf CR, Heimonen J, McCulloch DJ, Han PD, Sibley TR, Lee J, Ilcisin M, Fay K, Burstein R, Martin B, Lockwood CM, Thompson M, Lutz B, Jackson M, Hughes JP, Boeckh M, Shendure J and Bedford T (2020). Early detection of Covid-19 through a citywide pandemic surveillance platform. New England Journal of Medicine 383(2), 185–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rogers JH, Casto AM, Nwanne G, Link AC, Martinez MA, Nackviseth C, Wolf CR, Hughes JP, Englund JA, Sugg N, Uyeki TM, Han PD, Pfau B, Shendure J and Chu HY (2023). Results from a test-and-treat study for influenza among residents of homeless shelters in King County, WA: A stepped-wedge cluster-randomized trial. Influenza and Other Respiratory Viruses 17, e13092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Interim COVID-19 Testing Guidance for Healthcare Providers [Internet] (2020). Available at https://doh.wa.gov/sites/default/files/legacy/Documents/1600/coronavirus//Interim-2019NovelCoronavirusQuicksheetProviders.pdf.
- [17].Fazel S, Geddes JR and Kushel M (2014). The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. The Lancet 384(9953), 1529–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Check Code: Customizing the Data Entry Process [Internet] Centers for Disease Control and Prevention (2021). Available at https://www.cdc.gov/epiinfo/user-guide/check-code/epiweekfunctions.html.
- [19].Washington Department of Health Ditching Phase Finder as Vaccine Eligibility Requirement Starting Wednesday [Internet]. KING 5 (2021). Available at https://www.king5.com/article/news/health/coronavirus/vaccine/phase-finder-phasefinder-department-of-health-vaccine-eligibility-washington-state/281-1af42352-b91f-4d6e-b1d0-a98992a23c2c. Accessed 2 August 2022.
- [20].COVID-19 Summary Dashboard [Internet]. Overall Counts and Rates by Geographic Levels (2022). Available at https://kingcounty.gov/depts/health/covid-19/data/summary-dashboard.aspx.
- [21].Homelessness and COVID-19 [Internet]. Public Health Seattle-King County (2022). Available at https://kingcounty.gov/depts/health/covid-19/data/homeless.aspx.
- [22].Thomas I and Mackie P (2020). A population level study of SARS-CoV-2 prevalence amongst people experiencing homelessness in Wales, UK. International Journal of Population Data Science [Internet] 5(4), 1695. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8757314/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Casto AM, Rogers JH, Link AC, Boeckh M, Jackson ML, Uyeki TM, Englund JA, Starita LM and Chu HY (2022). Phylogenomics of severe acute respiratory syndrome coronavirus 2 in emergency shelters for people experiencing homelessness. The Journal of Infectious Diseases 226, 217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Culhane D, Treglia D and Steif K (2020). Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality [Internet]. Available at https://endhomelessness.org/resource/estimated-emergency-and-observational-quarantine-bed-need-for-the-us-homeless-population-related-to-covid-19-exposure-by-county-projected-hospitalizations-intensive-care-units-and-mortality/.
- [25].Imbert E, Kinley PM, Scarborough A, Cawley C, Sankaran M, Cox SN, Kushel M, Stoltey J, Cohen S and Fuchs JD (2021). Coronavirus disease 2019 outbreak in a San Francisco homeless shelter. Clinical Infectious Diseases 73(2), 324–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Roederer T, Mollo B, Vincent C, Nikolay B, Llosa AE, Nesbitt R, Vanhomwegen J, Rose T, Goyard S, Anna F, Torre C, Fourrey E, Simons E, Hennequin W, Mills C and Luquero FJ (2021). Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: A cross-sectional study. The Lancet Public Health 6(4), e202–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ralli M, Morrone A, Arcangeli A and Ercoli L (2021). Asymptomatic patients as a source of transmission of COVID-19 in homeless shelters. International Journal of Infectious Diseases 103, 243–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Karb R, Samuels E, Vanjani R, Trimbur C and Napoli A (2020). Homeless shelter characteristics and prevalence of SARS-CoV-2. Western Journal of Emergency Medicine 21(5), 1048–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Montgomery MP, Paulin HN, Morris A, Cotton A, Speers A, Boyd AT, Buff AM, Mathew D, Wells A, Marchman C, Gaffga N, Morris SB and Cavanaugh SS (2021). Establishment of isolation and noncongregate hotels during COVID-19 and symptom evolution among people experiencing homelessness - Atlanta, Georgia, 2020. Journal of Public Health Management and Practice 27(3), 285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rodriguez NM, Martinez RG, Ziolkowski R, Tolliver C, Young H and Ruiz Y (2022). “COVID knocked me straight into the dirt”: Perspectives from people experiencing homelessness on the impacts of the COVID-19 pandemic. BMC Public Health [Internet] 22(1), 1327. Available at http://www.ncbi.nlm.nih.gov/pubmed/35820879%0A; http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC9275174. Accessed 2 August 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Galdeen TR and Humphrey RP (2022). Safety nets work both ways: The influence of available paid leave on employee risk taking during the COVID-19 pandemic. Workplace Health and Safety 70(5), 235–241. [DOI] [PubMed] [Google Scholar]
- [32].King County and Seattle expand COVID-19 emergency shelter and housing response [Internet]. Seattle Weekly (2020). Available at https://www.seattleweekly.com/news/king-county-and-seattle-expand-covid-19-emergency-shelter-and-housing-response/.
- [33].Perri M, Dosani N and Hwang SW (2020). COVID-19 and people experiencing homelessness: Challenges and mitigation strategies. CMAJ 192(26), E716–E719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Huang C-H, Bui T, Hwang D and Shirai J (2023). Assessing the effectiveness of portable HEPA air cleaners for reducing particulate matter exposure in King County, Washington homeless shelters during the COVID-19 pandemic: Implications for community congregate settings. medRxiv. Available at https://www.medrxiv.org/content/10.1101/2023.01.20.23284493v1. Accessed 5 March 2022. [DOI] [PubMed]
- [35].Chapman LAC, Kushel M, Cox SN, Scarborough A, Cawley C, Nguyen TQ, Rodriguez-Barraquer I, Greenhouse B, Imbert E and Lo NC (2021). Comparison of infection control strategies to reduce COVID-19 outbreaks in homeless shelters in the United States: A simulation study. BMC Medicine 19(116), doi: 10.1186/s12916-021-01965-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Conlon A, Ashur C, Washer L, Eagle KA and Hofmann Bowman MA (2021). Impact of the influenza vaccine on COVID-19 infection rates and severity. American Journal of Infection Control 49(6), 694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Huang K, Lin SW, Sheng WH and Wang CC (2021). Influenza vaccination and the risk of COVID-19 infection and severe illness in older adults in the United States. Scientific Reports 11(1), 11025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Greco M, Cucci F, Portulano P, Lazzari RA, Caldararo C, Sicuro F, Catanese C and Lobreglio G (2021). Effects of influenza vaccination on the response to BNT162b2 messenger RNA COVID-19 vaccine in healthcare workers. Journal of Clinical Medicine Research 13(12), 549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].van Westen-Lagerweij NA, Meijer E, Meeuwsen EG, Chavannes NH, Willemsen MC and Croes EA (2021). Are smokers protected against SARS-CoV-2 infection (COVID-19)? The origins of the myth. npj Primary Care Respiratory Medicine 31(1), 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Amato M, Werba JP, Frigerio B, Coggi D, Sansaro D, Ravani A, Ferrante P, Veglia F, Tremoli E and Baldassarre D (2020). Relationship between influenza vaccination coverage rate and COVID-19 outbreak: An Italian ecological study. Vaccines (Basel) 8(3), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Sultana J, Mazzaglia G, Luxi N, Cancellieri A, Capuano A, Ferrajolo C, de Waure C, Ferlazzo G and Trifirò G (2020). Potential effects of vaccinations on the prevention of COVID-19: Rationale, clinical evidence, risks, and public health considerations. Expert Review of Vaccines 19(10), 919–936. [DOI] [PubMed] [Google Scholar]
- [42].Martínez-Baz I, Trobajo-Sanmartín C, Arregui I, Navascués A, Adelantado M, Indurain J, Fresán U, Ezpeleta C and Castilla J (2020). Influenza vaccination and risk of SARS-CoV-2 infection in a cohort of health workers. Vaccines (Basel) 8(4), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Stein C, Nassereldine H, Sorenson RJ and Amlag JO (2023). Past SARS-CoV-2 infection protection against re-infection: A systematic review and meta-analysis. The Lancet 401(10379), 833–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Antia R and Halloran ME (2021). Transition to endemicity: Understanding COVID-19. Immunity 54(10), 2172–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rogers et al. supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1017/S0950268823001036.
click here to view supplementary material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.