Abstract
Background:
There is low social awareness of vaginismus despite it being a relatively common female sexual dysfunction that makes vaginal penetration painful, difficult, and/or impossible. While existing literature on vaginismus has had a clinical focus on the affected genitalia, there is a lack of research on women’s help-seeking experiences of vaginismus from their perspective.
Objectives:
This integrative review’s objective was to explore: women’s help-seeking experiences of vaginismus, and how such help-seeking experiences impact their sense of self.
Design:
Cooper’s five-step integrative review approach was followed to develop a research question, a search strategy, selection criteria, and data evaluation, analysis, and presentation.
Data Sources and Methods:
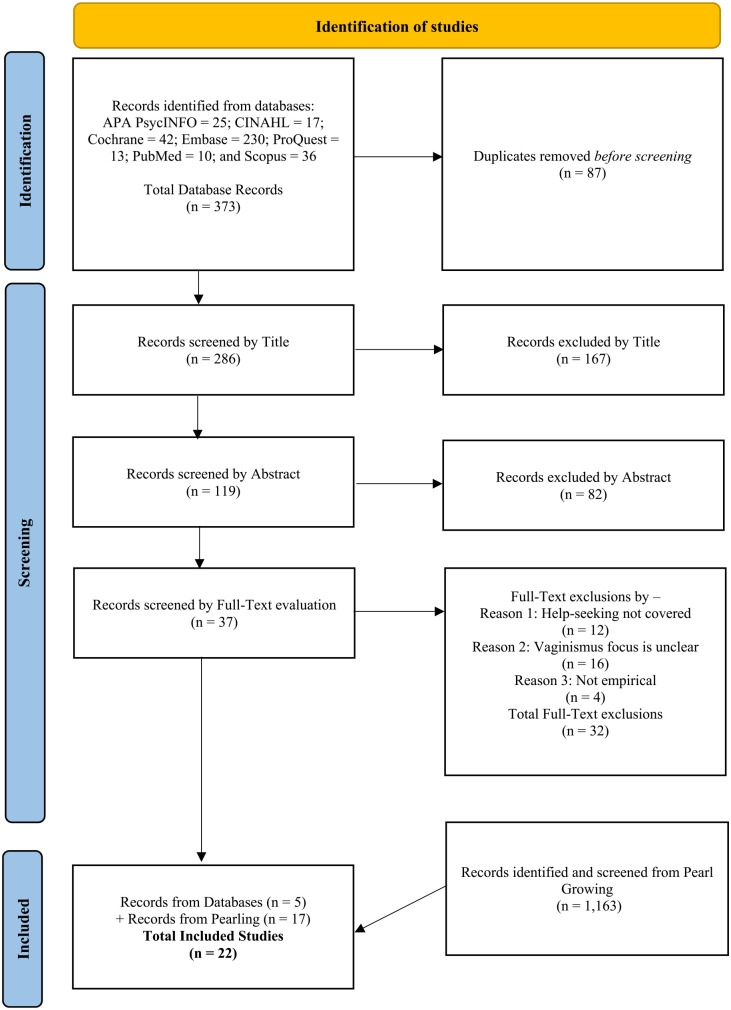
A systematic search of the literature was completed in the following seven databases in January 2023: PsycINFO, ProQuest Central, PubMed, Scopus, CINAHL, Cochrane, and Embase. Out of the 373 articles found through database searches and additional citation searching, 22 studies were included in this review for meeting the eligibility criteria of having an empirical design, being written in English, and examining women’s help-seeking experiences for vaginismus and its impact on their sense of self.
Results:
Thematic analysis was used to summarize the findings from the included studies which were informed by 1671 participants. Help-Seeking Process, Medical Management, Help-Seeking and Sense of Self, and Holistic Care Recommendations from the Findings emerged as four major themes with corresponding subthemes.
Conclusion:
This review indicates that women continue to face difficulties in seeking and receiving help for vaginismus even through the healthcare system. However, the studies did not explicitly discuss how women’s help-seeking for vaginismus impacted their sense of self. This highlights an epistemological gap on how women’s help-seeking for their vaginismus impacts their sense of self, which can affect their treatment responses. Recommendations are provided for future healthcare and research to improve health outcomes for women with vaginismus.
Keywords: vaginismus, genito-pelvic pain/penetration disorder, female sexual dysfunction, painful sex, help-seeking, treatment-seeking, sense of self
Introduction
Vaginismus
Vaginismus is characterized by the persistent involuntary closure of the vagina upon attempts at penetration of any sort whether by a penis, tampons, fingers, or speculum. 1 This can make penetration via vaginal entry painful, difficult, and/or impossible depending on the severity of vaginismus. 2 Vaginismus can be diagnosed as primary (lifelong) or secondary (acquired). 3 The current fifth edition of the Diagnostic and Statistical Manual controversially merged vaginismus and dyspareunia into genito-pelvic pain/penetration disorder (GPPPD).4,5 While some believed that this merging would improve diagnostic accuracy, others continue to argue that the scope of GPPPD is too broad and does not capture the clinical difference between dyspareunia and vaginismus.5 –7 Dyspareunia is often used as a general term that refers to painful sexual intercourse due to varied causes such as endometriosis, vulvodynia, or vaginal atrophy to name a few. 8 The term dyspareunia does not capture the specific combination of symptoms of pain, anxiety, and excessive vaginal tightness or closure upon attempts at vaginal penetration that occurs with vaginismus or the treatment for it. Also, the term vaginismus continues to be used in clinical settings to diagnose patients and in recent research.6,9,10 The authors recognize the unique experiences of vaginismus and not the dyspareunic conditions it is merged with in GPPPD. Vaginismus will therefore be used to refer to the condition throughout this article.
Due to making sexual intercourse or any type of vaginal sexual penetration difficult or unachievable, vaginismus is regarded as a female sexual dysfunction or female sexual pain disorder. Yet, vaginismus remains a specialist term that never transitioned into common usage in the same way as erectile dysfunction and premature ejaculation. 11 This contributes to the low social awareness of vaginismus throughout societies around the world. While there has been some increased interest in vaginismus, it is still a specialist term that is not known well enough in the public to be casually mentioned in social circles, movies, or television in the same way as erectile dysfunction or premature ejaculation. Vaginismus continues to be under-researched6,12 and not well known among women and even among health professionals.2,6,12
Current research on vaginismus and its prevalence
Vaginismus is reported to be a common female sexual dysfunction.13 –15 Yet, there is no consensus on the specific prevalence of vaginismus.6,14,15 A recent study from Denmark assessed the prevalence of vaginismus as affecting 0.8% of the female population. 16 However, different studies have estimated vaginismus to affect anywhere between 7% and 68% of the female population with higher reported prevalence in certain countries, such as Iran, Turkey, and Ghana.6,12,14,17,18 McEvoy et al. 6 highlight that information on prevalence of vaginismus is only based on women who attend clinics. However, due to the guilt, shame, and secrecy of vaginismus, many with the condition do not seek help and are therefore not counted. 6 This makes it difficult to estimate the general prevalence of the condition. 6 Given that this indicates that many women suffer with vaginismus, it is important to examine women’s experiences of making sense of the condition.
However, the existing literature on vaginismus has had a large clinical focus on the affected genitalia in terms of aetiology,19,20 efficacy of treatments,21 –23 and ongoing debates regarding the classification and diagnostic criteria of vaginismus.5,24 Many studies that examine fear, anxiety, or disgust in relation to vaginismus still have a clinical focus on how it affects women’s response to penetration rather than their phenomenological experiences of it from their perspective. Sánchez Bravo et al.’s 25 Spanish-written work examines how conflict between desire and sexual prohibition causes associations of sex with pain. Koops et al.’s 26 quantitative study also considers personality functioning in relation to vaginismus symptoms. In a recent systematic review by Mellado et al. 27 that included 52 studies on female pelvic pain conditions, only two qualitative studies examining the impact of vaginismus and treatment on women’s lives were identified in the literature. This indicates a lack of research on women’s subjective experiences of struggling with vaginismus from their perspective.
Help-seeking
Women with female sexual dysfunctions face barriers to seek help and access treatment. 28 In health contexts, help-seeking behaviour can be understood as people’s process, interactions and experiences to search for help to gain diagnosis, information, and treatment or relief for a presenting health issue. 29 Moreover, the healthcare system has shown to be androcentric and dismissive of women’s sexual problems when they seek help. 30 This increases the risk of women with vaginismus being misdiagnosed, given inappropriate treatment, or having their experience dismissed altogether. Not receiving help for vaginismus can have severe consequences on women’s relationships, sex life, and emotional wellbeing, which can snowball to cause mental health issues and overall poor quality of life.31,32
Sense of self
Women face challenges to seek help to gain information, diagnosis, and treatment for taboo conditions such as vaginismus, 33 which can impact their sense of self. The concept of sense of self refers to how one perceives themselves as an individual. 34 Sense of self can be understood as an umbrella term that can include self-esteem, self-awareness, and self-reflection to name a few. For clarity in expression, ‘sense of self’, ‘construction/s of self’, and ‘self’ will be used interchangeably in this article. The body, and its afflictions such as vaginismus, influence one’s sense of self.34,35 Women’s social interactions to seek help through the healthcare system and other avenues can affect their sense of self too. 35 Therefore, women’s constructions of self are unique to their individual social interactions, which renders sense of self to be a highly subjective phenomenon that is difficult to quantitively measure. Understanding how help-seeking for vaginismus impacts women’s sense of self can reveal valuable insight into women’s processes to make sense of negotiating treatment for the condition.
Objective
The experiences of women help-seeking for their vaginismus can impact their constructions of self in ways that influence how well they perceive and respond to interventions. An integrative review, which can include diverse methods of research, was therefore employed to examine such broad phenomena of experience. 36 This mixed-methods integrated review was undertaken as the first study to summarize the existing literature on how women seek help for vaginismus, and its impact on their constructions of sense of self. Using a Population, Phenomena of Interest, and Context (PICo) framework, 37 an integrative literature review was conducted to answer the following question: What are women’s experiences to seek help for their vaginismus, and how does such help-seeking impact their sense of self?
Methods
This was an integrative review using Cooper’s38,39 five-stage framework. This review followed the five stages of (1) formulating the purpose and research question(s) which has been outlined above, (2) systematic literature search and selection, (3) data evaluation, (4) data analysis, and (5) data presentation.38,39 As a mixed-methods review, it is able to integrate quantitative evidence of effectiveness and qualitative data on participants’ experiences. 40 This can offer a broader and deeper understanding of the complex issue of women’s help-seeking experiences for their vaginismus and its impact on their constructions of self. Estimating the effectiveness of an intervention from included studies is not applicable in integrative reviews which examine broader experiential phenomena.
Search strategy
Unlike systematic reviews, integrative review guidelines have not been formalized for literature searches. 41 Therefore, to support stage two of Cooper’s framework, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines42,43 were adapted to report strategies to search, screen, and select literature as suggested. 41 The literature search included seven databases: PsycINFO, ProQuest Central, PubMed, Scopus, CINAHL, Cochrane, and Embase. The eligibility criteria presented in Table 1 were devised by all authors to translate the review’s research question into searchable keywords to screen the database results step-by-step by title, abstract, and full-text. 42 The Medical Subject Heading (MeSH) terms searched on databases are also presented in Table 1. Relevant keywords, Boolean phrases, advanced search techniques of using truncated symbols, MeSH terms, and any applicable subject headings were first searched on all seven databases in English in January 2023 which produced 373 results as detailed in Table 2. There were 87 duplicates that were removed to leave 286 results which were systematically screened by title, abstract, and full-text by the first two authors. Five eligible studies were found in the search.
Table 1.
Summary of the inclusion/exclusion criteria and keywords.
| PICo parameters | Inclusion | Exclusion | Key words/steps | MeSH terms searched on applicable databases | |
|---|---|---|---|---|---|
| Population (P) | Literature which focuses on women with vaginismus | Literature which does not focus on women with vaginismus. Other dyspareunic conditions which are not vaginismus. Empirical studies on combined female sexual dysfunctions where participants with vaginismus were not separated to extract relevant data. | (Title) (vaginismus OR dyspareunia OR vaginism OR ‘genito-pelvic pain/penetration disorder’ OR GPPPD OR ‘penetration disorder’ OR ‘vaginal pain’) | Vaginismus, Dyspareunia | |
| Phenomena of interest (I) | Literature which mentions people’s help-seeking for their vaginismus and its impact on constructions of sense of self in the abstract | Literature which does not mention people’s help-seeking for their vaginismus and its impact on constructions of self in the abstract | AND (Abstract) (‘help-seeking’ OR help-seeking OR treatment OR ‘treatment-seeking’ OR treatment-seeking OR diagnosis OR information OR relief OR support) AND (Abstract) (experience OR perception OR construct* OR perceiv*) AND (Abstract) (self* OR identity) |
Help-seeking behaviour OR Information-seeking behaviour AND Self Concept OR Gender Identity |
|
| Context (Co) | Location | International | None | N/A | N/A |
| Language | English | Other languages | English | English | |
| Time | Any | None | N/A | N/A | |
| Study/literature type | Published peer-reviewed primary research including qualitative, quantitative, or mixed-method designs | Published literature which DOES NOT include qualitative, quantitative, or mixed methods of data collection and analysis | N/A | N/A | |
GPPPD: genito-pelvic pain/penetration disorder.
Table 2.
Database searches.
| PsycINFO (EBSCO) | S1 | TI vaginismus OR dyspareunia OR vaginism OR “genito-pelvic pain/penetration disorder” OR GPPPD OR “penetration disorder” OR “vaginal pain” | 306 |
| S2 | MM “Vaginismus” | 216 | |
| S3 | MM “Dyspareunia” | 253 | |
| S4 | AB “help seeking” OR help-seeking OR treatment OR “treatment seeking” OR treatment-seeking OR diagnosis OR information OR relief OR support | 1,647,840 | |
| S5 | MM “Help Seeking Behavior” OR MM “Health Care Seeking Behavior” | 9519 | |
| S6 | MM “Health Care Seeking Behavior” OR MM “Professional Referral” OR MM “Self-Referral” | 7147 | |
| S7 | MM “Information Seeking” OR MM “Questioning” | 6056 | |
| S8 | AB experience OR perception OR construct* OR perceiv* | 1,197,401 | |
| S9 | MM “Self-Perception” OR MM “Belonging” OR MM “Body Image” OR MM “Interoception” OR MM “Perceived Control” OR MM “Self-Acceptance” OR MM “Self-Deception” OR MM “Self-Efficacy” OR MM “Self-Knowledge” OR MM “Self-Reference” OR MM “Self-Reflection” | 52,927 | |
| S10 | AB self* OR identity | 711,408 | |
| S11 | MM “Self-Concept” OR MM “Academic Self Concept” OR MM “Athletic Identity” OR MM “Entitlement (Psychological)” OR MM “Impostor Phenomenon” OR MM “Professional Identity” OR MM “Self-Compassion” OR MM “Self-Confidence” OR MM “Self-Congruence” OR MM “Self-Esteem” OR MM “Self-Forgiveness” OR MM “Self-Regard” OR MM “Self-Worth” OR MM “Sense of Coherence” | 67,184 | |
| S12 | MM “Gender Identity” OR MM “Cisgender” OR MM “Gender Nonbinary” OR MM “Gender Nonconforming” OR MM “LGBTQ” OR MM “Transsexualism” | 12,815 | |
| S13 | S1 OR S2 OR S3 | 458 | |
| S14 | S4 OR S5 OR S6 OR S7 | 1,653,656 | |
| S15 | S8 OR S9 | 1,225,192 | |
| S16 | S10 OR S11 OR S12 | 731,000 | |
| S17 | S13 AND S14 AND S15 AND S16 | 25 | |
| S18 | S13 AND S14 AND S15 AND S16 Narrow by Language: English | 25 | |
| CINAHL | S1 | (MM “Vaginismus”) | 72 |
| S2 | (MM “Dyspareunia”) | 509 | |
| S3 | TI vaginismus OR dyspareunia OR vaginism OR “genito-pelvic pain/penetration disorder” OR GPPPD OR “penetration disorder” OR “vaginal pain” | 366 | |
| S4 | AB “help seeking” OR help-seeking OR treatment OR “treatment seeking” OR treatment-seeking OR diagnosis OR information OR relief OR support | 1,741,128 | |
| S5 | (MM “Help Seeking Behaviour”) | 4270 | |
| S6 | (MM “Information Seeking Behaviour”) | 2777 | |
| S7 | AB experience OR perception OR construct* OR perceiv* | 607,652 | |
| S8 | AB self* OR identity | 328,534 | |
| S9 | (MM “Self Concept +”) | 31,731 | |
| S10 | (MM “Gender Identity +”) | 4806 | |
| S11 | S1 OR S2 OR S3 | 639 | |
| S12 | S4 OR S5 OR S6 | 1,743,692 | |
| S13 | S8 OR S9 OR S10 | 343,943 | |
| S14 | S11 AND S12 AND S7 AND S13 | 17 | |
| Cochrane | #1 | MeSH descriptor: [Vaginismus] explode all trees | 13 |
| #2 | MeSH descriptor: [Dyspareunia] explode all trees | 233 | |
| #3 | (vaginismus OR dyspareunia OR vaginism OR “genito-pelvic pain/penetration disorder” OR “penetration disorder” OR gpppd OR “vaginal pain”): ti (Word variations have been searched) | 7667 | |
| #4 | MeSH descriptor: [Help-Seeking Behaviour] explode all trees | 47 | |
| #5 | MeSH descriptor: [Information-Seeking Behaviour] explode all trees | 54 | |
| #6 | (“Help seeking” OR help-seeking OR treatment OR treatment-seeking OR “treatment seeking” OR diagnosis OR information OR relief OR support): ab (Word variations have been searched) | 928,439 | |
| #7 | (experience OR perception OR construct* OR perceiv*): ab (Word variations have been searched) | 142,266 | |
| #8 | (self* OR identity): ab (Word variations have been searched) | 134,527 | |
| #9 | MeSH descriptor: [Gender Identity] explode all trees | 279 | |
| #10 | MeSH descriptor: [Self Concept] explode all trees | 7704 | |
| #11 | #1 OR #2 OR #3 | 7804 | |
| #12 | #4 OR #5 OR #6 | 928,448 | |
| #13 | #8 OR #9 OR #10 | 136,810 | |
| #14 | #11 AND #12 AND #7 AND #13 | 42 | |
| Embase | 1 | vaginismus.mp. or exp *vaginism/ | 982 |
| 2 | Limit 1 to English language | 809 | |
| 3 | dyspareunia.mp. or exp *dyspareunia/ | 14,203 | |
| 4 | Limit 3 to English language | 13,122 | |
| 5 | vaginism.mp. or exp *vaginism/ | 1245 | |
| 6 | Limit 5 to English language | 1064 | |
| 7 | “genito-pelvic pain/penetration disorder”.mp. | 72 | |
| 8 | Limit 7 to English language | 70 | |
| 9 | GPPPD.mp. | 22 | |
| 10 | Limit 9 to English language | 21 | |
| 11 | “penetration disorder”.mp. | 116 | |
| 12 | Limit 11 to English language | 113 | |
| 13 | “vaginal pain”.mp. or exp *vagina pain/ | 577 | |
| 14 | Limit 13 to English language | 557 | |
| 15 | 2 or 4 or 6 or 8 or 10 or 12 or 14 | 14,163 | |
| 16 | exp *help seeking behaviour/ | 3840 | |
| 17 | Limit 16 to English language | 3771 | |
| 18 | information seeking.mp. or exp *information seeking/ | 6953 | |
| 19 | Limit 18 to English language | 6791 | |
| 20 | “treatment seeking”.mp. | 8036 | |
| 21 | Limit 20 to English language | 7971 | |
| 22 | treatment-seeking.mp. | 8036 | |
| 23 | Limit 22 to English language | 7971 | |
| 24 | “help seeking”.mp. | 20,704 | |
| 25 | Limit 24 to English language | 20,305 | |
| 26 | “help-seeking”.mp. | 20,704 | |
| 27 | Limit 26 to English language | 20,305 | |
| 28 | treatment.mp. | 8,585,885 | |
| 29 | Limit 28 to English language | 7,508,193 | |
| 30 | diagnosis.mp. or exp *diagnosis/ | 7,555,104 | |
| 31 | Limit 30 to English language | 6,208,544 | |
| 32 | exp *information/ or information.mp. | 2,985,312 | |
| 33 | Limit 32 to English language | 2,793,728 | |
| 34 | relief.mp. | 157,636 | |
| 35 | Limit 34 to English language | 143,496 | |
| 36 | support.mp. | 1,692,333 | |
| 37 | Limit 36 to English language | 1,624,428 | |
| 38 | 17 or 19 or 21 or 23 or 25 or 27 or 29 or 31 or 33 or 35 or 37 | 14,829,902 | |
| 39 | experience.mp. or exp *experience/ | 1,256,428 | |
| 40 | Limit 39 to English language | 1,121,815 | |
| 41 | perception.mp. or exp *perception/ | 513,729 | |
| 42 | Limit 41 to English language | 483,311 | |
| 43 | perceiv*.mp. | 355,489 | |
| 44 | Limit 43 to English language | 345,823 | |
| 45 | construct*.mp. | 803,148 | |
| 46 | Limit 45 to English language | 752,192 | |
| 47 | 40 or 42 or 44 or 46 | 2,484,754 | |
| 48 | self.mp. or exp *self concept/ | 1,325,403 | |
| 49 | Limit 48 to English language | 1,259,422 | |
| 50 | exp *gender identity/ or exp *identity/ or identity.mp. | 208,392 | |
| 51 | Limit 50 to English language | 199,104 | |
| 52 | 49 or 51 | 1,425,375 | |
| 53 | 15 and 38 and 47 and 52 | 230 | |
| ProQuest | S1 | (MJMESH.EXACT.EXPLODE(“Vaginismus: C.12.100.250.919”) OR MJMESH.EXACT.EXPLODE(“Vaginismus: C.12.050.351.500.894.870”) OR MJMESH.EXACT.EXPLODE(“Vaginismus: C.12.100.875.871”) OR MJMESH.EXACT.EXPLODE(“Vaginismus: C.12.100.250.894.870”) OR MJMESH.EXACT.EXPLODE(“Vaginismus: F.03.835.900”) OR MJMESH.EXACT.EXPLODE(“Vaginismus: C.12.050.351.500.919”)) OR (MJMESH.EXACT.EXPLODE(“Dyspareunia: F.03.835.199”) OR MJMESH.EXACT.EXPLODE(“Dyspareunia: C.12.100.875.242”) OR MJMESH.EXACT.EXPLODE(“Dyspareunia: C.12.100.250.110”) OR MJMESH.EXACT.EXPLODE(“Dyspareunia: C.12.100.500.100”) OR MJMESH.EXACT.EXPLODE(“Dyspareunia: C.12.200.294.100”) OR MJMESH.EXACT.EXPLODE(“Dyspareunia: C.12.050.351.500.110”)) OR ti(vaginismus OR dyspareunia OR vaginism OR “genito-pelvic pain/penetration disorder” OR GPPPD OR “penetration disorder” OR “vaginal pain”) (Limit to peer reviewed applied) | 356 |
| S2 | ab(“help seeking” OR help-seeking OR treatment OR “treatment seeking” OR treatment-seeking OR diagnosis OR information OR relief OR support) OR MJMESH.EXACT.EXPLODE(“Help-Seeking Behaviour”) OR (MJMESH.EXACT.EXPLODE(“Information Seeking Behaviour: L.01.143.458”) OR MJMESH.EXACT.EXPLODE(“Information Seeking Behaviour: F.01.145.209.372”) OR MJMESH.EXACT.EXPLODE(“Information Seeking Behaviour: F.01.145.535”)) OR MAINSUBJECT.EXACT(“Health behaviour”) OR MAINSUBJECT.EXACT(“Information seeking behaviour”) (Limit to peer-reviewed applied) | 4,299,298 | |
| S3 | ab(experience OR perception OR construct* OR perceiv*) OR MAINSUBJECT.EXACT(“Social construction”) (Limit to peer-reviewed applied) | 1,842,495 | |
| S4 | ab(self* OR identity) OR (MJMESH.EXACT.EXPLODE(“Gender Identity: F.01.752.747.385.200”) OR MJMESH.EXACT.EXPLODE(“Gender Identity: F.01.393.446.250”) OR MJMESH.EXACT.EXPLODE(“Gender Identity: F.01.752.747.722.200”) OR MJMESH.EXACT.EXPLODE(“Gender Identity: F.02.739.794.793.200”)) OR MJMESH.EXACT.EXPLODE(“Self Concept”) OR (MAINSUBJECT.EXACT(“Self control”) OR MAINSUBJECT.EXACT(“Self image”) OR MAINSUBJECT.EXACT(“Self representation”) OR MAINSUBJECT.EXACT(“Self esteem”) OR MAINSUBJECT.EXACT(“Self expression”)) OR MAINSUBJECT.EXACT(“Self awareness”) OR MAINSUBJECT.EXACT(“Otherness”) OR MAINSUBJECT.EXACT(“Gender identity”) (Limit to peer-reviewed applied) | 934,690 | |
| S5 | S1 AND S2 AND S3 AND S4 (Limit to peer-reviewed applied) | 13 | |
| PubMed | #1 | “vaginismus”[MeSH Terms] | 13 |
| #2 | “dyspareunia”[MeSH Terms] | 235 | |
| #3 | (vaginismus(Title) OR dyspareunia(Title) OR vaginism(Title) OR “genito-pelvic pain/penetration disorder”[Title] OR GPPPD[Title] OR “penetration disorder”[Title] OR “vaginal pain”[Title]) | 157 | |
| #4 | (#1 OR #2 OR #3) | 340 | |
| #5 | (“help seeking”(Abstract) OR help-seeking(Abstract) OR treatment(Abstract) OR “treatment seeking”(Abstract) OR treatment-seeking(Abstract) OR diagnosis(Abstract) OR information(Abstract) OR relief(Abstract) OR support(Abstract) | 2,215,641 | |
| #6 | “help seeking behaviour”[MeSH Terms] | 370 | |
| #7 | “information seeking behaviour”[MeSH Terms] | 1081 | |
| #8 | (#5 OR #6 OR #7) | 2,215,843 | |
| #9 | (experience(Abstract) OR perception(Abstract) OR construct*(Abstract) OR perceiv*(Abstract) | 497,710 | |
| #10 | (self*[Abstract] OR identity(Abstract)) | 333,093 | |
| #11 | self concept[MeSH Terms] | 16,898 | |
| #12 | “gender identity”[MeSH Terms] | 2627 | |
| #13 | (#10 OR #11 OR #12) | 339,862 | |
| #14 | (#4 AND #8 AND #9 AND #13) | 10 | |
| Scopus | (TITLE ( vaginismus OR dyspareunia OR vaginism OR “genito-pelvic pain/penetration disorder” OR “penetration disorder” OR gpppd OR “vaginal pain”) AND TITLE-ABS-KEY (“Help seeking” OR help-seeking OR treatment OR treatment-seeking OR “treatment seeking” OR diagnosis OR information OR relief OR support) AND TITLE-ABS-KEY (experience OR perception OR construct* OR perceiv*) AND TITLE-ABS-KEY (self* OR identity)) AND ( LIMIT-TO ( LANGUAGE, “English”)) | 36 |
In line with stage 2 of conducting an integrative review, it is recommended to use two or more search strategies to retrieve more relevant literature and reduce bias. 41 Research has found that citation searching can uncover over half the studies relevant for a review 44 and therefore be more comprehensive in identifying the relevant literature than database searches. 45 Following this, an additional strategy of bi-directional citation searching (also known as pearl growing) was undertaken on the five studies by examining their reference list, and using Google Scholar to find and screen literature that it was ‘cited by’. 46 This uncovered 17 more eligible studies. Altogether, 22 studies were identified as eligible and included in the review.47 –68 See Figure 1 for a summary of the article selection process. Following PRISMA guidelines, all authors were involved in selecting the studies for inclusion. The authors discussed, and sometimes debated, which studies to include until consensus was reached.
Figure 1.
PRISMA flow chart outlining the article selection process.
Quality assessment
As part of the data evaluation of stage three outlined by Cooper, the Mixed-Methods Appraisal Tool (MMAT) by Hong et al. 69 was used to assess the methodological quality of the diverse study types of the 22 included articles. The MMAT uses five criteria to assess the quality of quantitative, qualitative, and mixed-method designs which enables the standardization of the quality assessment of diverse studies. 69 While Hong et al’.s 69 publication of the MMAT discouraged calculating a score for quality assessment, Hong et al. 70 later recognized that it is problematic for reporting results. Hong et al. 70 then suggested to score studies according to the number of MMAT quality criteria it meets out of 100%. Therefore, studies that meet: no criteria = 0%, 1 criterion = 20%, 2 criteria = 40%, 3 criteria = 60%, 4 criteria = 80%, and 5 criteria = 100%. 70 A higher MMAT score indicates higher methodological quality. 70 The first author initially assessed the included studies with the MMAT and then the second and third authors reviewed it and any disagreements were discussed until resolved with the results presented in Table 3. While 13 studies scored 80%–100%, three studies scored 60%. Due to scoring 40% or less, the remaining six studies were of lower methodological quality. Lower methodological quality can indicate a lack of rigour and an increased risk of bias for review findings. However, no studies were excluded based on their quality assessment by the MMAT to avoid missing any new findings in an under-researched area.
Table 3.
MMAT quality assessment of the included studies.
| Study | Study design | Methodological quality criteria | Responses | |||
|---|---|---|---|---|---|---|
| Yes | No | Unclear | Comments | |||
| Achour et al. 47 | Mixed methods | Is there an adequate rationale for using a mixed-methods design to address the research question? | X | |||
| Are the different components of the study effectively integrated to answer the research question? | X | |||||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | X | |||||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | X | |||||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | X | It is unclear whether the nonresponse bias was low for the quantitative component | ||||
| Akhavan-Taghavi et al. 48 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | Since it was 115 consecutive clinical records, it is assumed that the nonresponse bias is low | ||||
| Is the statistical analysis appropriate to answer the research question? | X | This is not explained. | ||||
| Bhatt et al. 49 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | There is no research question or aim clearly presented | ||
| Are the qualitative data collection methods adequate to address the research question? | X | There is no research question or aim clearly presented | ||||
| Are the findings adequately derived from the data? | X | |||||
| Is the interpretation of results sufficiently substantiated by data? | X | |||||
| Is there coherence between qualitative data sources, collection, analysis, and interpretation? | X | |||||
| Drenth et al. 50 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | |||||
| Is the statistical analysis appropriate to answer the research question? | X | |||||
| Engman et al. 51 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | |||||
| Is the statistical analysis appropriate to answer the research question? | X | |||||
| Fageeh 52 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | |||
| Are the qualitative data collection methods adequate to address the research question? | X | |||||
| Are the findings adequately derived from the data? | X | |||||
| Is the interpretation of results sufficiently substantiated by data? | X | The Discussion section is not linked to the presented data | ||||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | X | There is lack of coherence because the interpretation in the Discussion is not linked to the data sources | ||||
| Fejza et al. 53 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | |||
| Are the qualitative data collection methods adequate to address the research question? | X | There is no clear methods section to explain or justify data collection | ||||
| Are the findings adequately derived from the data? | X | There is lack of coherence because the interpretation in the Discussion is not linked to the data sources | ||||
| Is the interpretation of results sufficiently substantiated by data? | X | There is no Discussion or any other clear section to interpret the Results | ||||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | X | There is no clearly marked Results or Discussion section to cohere the data, collection, analysis and interpretation | ||||
| Kurban et al. 54 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | |||||
| Is the statistical analysis appropriate to answer the research question? | X | |||||
| Macey et al. 55 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | |||
| Are the qualitative data collection methods adequate to address the research question? | X | |||||
| Are the findings adequately derived from the data? | X | |||||
| Is the interpretation of results sufficiently substantiated by data? | X | |||||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | X | |||||
| Muammar et al. 56 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | The information on nonrespondents has not been provided to assess the risk of bias | ||||
| Is the statistical analysis appropriate to answer the research question? | X | Sample size not justified | ||||
| Ogden and Ward 57 | Mixed methods | Is there an adequate rationale for using a mixed-methods design to address the research question? | X | |||
| Are the different components of the study effectively integrated to answer the research question? | X | |||||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | X | |||||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | X | |||||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | X | |||||
| O’Sullivan 58 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | There is no research question or aim clearly presented. This may be due to the age of the research | ||
| Are the qualitative data collection methods adequate to address the research question? | X | There is no research question or aim clearly presented. This may be due to the age of the research | ||||
| Are the findings adequately derived from the data? | X | |||||
| Is the interpretation of results sufficiently substantiated by data? | X | |||||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | X | |||||
| Ramli et al. 59 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | |||
| Are the qualitative data collection methods adequate to address the research question? | X | No justification provided for the chosen number of participants | ||||
| Are the findings adequately derived from the data? | X | Only the first paragraph of the discussion was derived from the data | ||||
| Is the interpretation of results sufficiently substantiated by data? | X | Data presented as cases is not sufficiently analysed nor interpreted in the Discussion | ||||
| Is there coherence between qualitative data sources, collection, analysis and interpretation? | X | The way that the data were collected and analysed is not clear and therefore does not clearly cohere with the interpretation of findings | ||||
| Reissing 60 | Quantitative descriptive | Is the sampling strategy relevant to address the research question? | X | |||
| Is the sample representative of the target population? | X | |||||
| Are the measurements appropriate? | X | |||||
| Is the risk of nonresponse bias low? | X | |||||
| Is the statistical analysis appropriate to answer the research question? | X | The statistical analysis used is neither clearly stated nor justified | ||||
| Scholl 61 | Quantitative non-randomized | Are the participants representative of the target population? | X | |||
| Are measurements appropriate regarding both the outcome and intervention (or exposure)? | X | |||||
| Are there complete outcome data? | X | |||||
| Are the confounders accounted for in the design and analysis? | X | |||||
| During the study period, is the intervention administered (or exposure occurred) as intended? | X | |||||
| Stelko 62 | Qualitative | Is the qualitative approach appropriate to answer the research question? | X | |||
| Are the qualitative data collection methods adequate to address the research question? | X | |||||
| Are the findings adequately derived from the data? | X | |||||
| Is the interpretation of results sufficiently substantiated by data? | X | |||||
| Is there coherence between qualitative data sources, collection, analysis, and interpretation? | X | |||||
| Svedhem et al. 63 | Qualitative | Appropriate approach to answer research question | X | |||
| Adequate data collection methods | X | |||||
| Findings are adequately derived from data | X | |||||
| Interpretations of results substantiated by data | X | |||||
| Coherence between qualitative data sources, collection, analysis, and interpretation | X | |||||
| Thorpe et al. 64 | Qualitative | Appropriate approach to answer research question | X | |||
| Adequate data collection methods | X | |||||
| Findings are adequately derived from data | X | |||||
| Interpretations of results substantiated by data | X | |||||
| Coherence between qualitative data sources, collection, analysis, and interpretation | X | |||||
| Tulla et al. 65 | Qualitative | Appropriate approach to answer research question | X | |||
| Adequate data collection methods | X | |||||
| Findings are adequately derived from data | X | |||||
| Interpretations of results substantiated by data | X | The discussion is largely speculative rather than based on the findings | ||||
| Coherence between qualitative data sources, collection, analysis, and interpretation | X | Several points in the discussion are not based on the findings from the case study | ||||
| Ward and Ogden 66 | Mixed methods | Is there an adequate rationale for using a mixed-methods design to address the research question? | X | The study states that quantitative and qualitative methods are used. But there is no explicit statement that mixed methods are used to justify its rationale | ||
| Are the different components of the study effectively integrated to answer the research question? | X | |||||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | X | |||||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | X | |||||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | X | |||||
| Zgueb et al. 67 | Mixed methods | Is there an adequate rationale for using a mixed-methods design to address the research question? | X | No mention of using mixed methods. No explicit rationale provided for the use of mixed methods | ||
| Are the different components of the study effectively integrated to answer the research question? | X | The quantitative assessment was not adequately covered or integrated | ||||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | X | The quantitative assessment was not adequately integrated to be interpreted | ||||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | X | Any divergences and inconsistencies are not mentioned or explained | ||||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | X | The statistical analysis used is not justified | ||||
| Zulfikaroglu 68 | Mixed methods | Is there an adequate rationale for using a mixed-methods design to address the research question? | X | No mention of using mixed methods. No explicit rationale is provided for the use of mixed methods | ||
| Are the different components of the study effectively integrated to answer the research question? | X | |||||
| Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | X | |||||
| Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | X | |||||
| Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | X | |||||
Data analysis
While commonly used to summarize qualitative research, thematic analysis can also be used to synthesize diverse quantitative, qualitative, and mixed-method studies for analysis,71,72 including in integrated reviews. 73 Since quantitative and qualitative data can address the same research phenomena, these different types of data can be transformed into the same format to be organized and analysed. 74 Therefore, to follow stage four of data analysis in Cooper’s framework, Dwyer 73 recommends to use Braun and Clarke’s 75 six-phase approach of thematic analysis in integrative reviews. This review uses Braun and Clarke’s73,75 thematic approach to extract, organize, and analyse the findings from the included studies.
First, familiarization with the qualitative and quantitative data occurred by reading the Results, Discussion, and Conclusion sections of the included studies several times and noting initial ideas for coding. 75 Quantitative studies were ‘qualitized’, as Sandelowski et al. 74 call it, by repeatedly reading and taking notes on the descriptive and inferential statistics and summarized quantitative results articulated in the findings. Second, initial codes from the data were generated. 75 Third, themes were searched using Quirkos, a computer-assisted qualitative data analysis software (CAQDAS), as an organizational tool to extract data to answer the research question and visually sort codes into themes. 75 For the fourth and fifth phase, the themes were reviewed and refined with appropriate subthemes. 75 A narrative report of the themes is presented below for the sixth phase. 75 According to Toronto, 38 statistical synthesis methods such as meta-analysis are not included in integrative reviews.
Results
Sample
Out of the 22 included studies, seven studies had quantitative study designs, 10 were qualitative studies, and five used mixed-method designs. The 22 studies included 1671 women’s help-seeking experiences for vaginismus. The sample varied to include women who either currently or formerly had vaginismus, and those who had primary and secondary vaginismus. These women interacted with a range of health professionals and tried various treatments. The participants ranged from 18 to 71 years of age in 21 of the 22 studies. The remaining study by Stelko 62 did not disclose participants’ ages. The sample represented women from Saudi Arabia, Iran, Tunisia, Turkey, India, Netherlands, Sweden, Australia, the United States, the United Kingdom, and Malaysia. Only four included studies by Ward and Ogden, 66 Ogden and Ward, 57 Svedhem et al., 63 and Thorpe et al. 64 mentioned participants’ sexual orientation. Stelko 62 discussed heterosexuality at length but the sexual orientation of participants was not stated. No studies indicated gender diversity. The characteristics of the included studies, including methods used, are summarized in Table 4.
Table 4.
Characteristics of the included studies in the integrative review.
| No. | Authors/year | Condition | Country/city | Theoretical approach | Sample size | Study design | Methods | Analytical approach |
|---|---|---|---|---|---|---|---|---|
| 1. | Achour et al. 47 | Vaginismus and pregnancy | Tunisia | Not stated | 20 | Mixed methods € | Interviews with standardized questionnaire and STAI | Descriptive analysis |
| 2. | Akhavan-Taghavi et al. 48 | Vaginismus | Tehran, Iran | Not stated | 115 | Quantitative | Data from clinical records extracted using a standard questionnaire | Descriptive analysis |
| 3. | Bhatt et al. 49 | Vaginismus | Gujarat, India | Not stated | 25 | Qualitative | Retrospective study | Not stated |
| 4. | Drenth et al. 50 | Vaginismus | Groningen, the Netherlands | Not stated | 49 | Quantitative | Retrospective study | Descriptive statistics |
| 5. | Engman et al. 51 | Primary or Secondary, and Partial or Total Vaginismus | Linköping, Sweden | Not stated | 44 | Quantitative | Questionnaire and therapy records | Pre- and post-intervention comparisons (Pearson Chi-squared test and Wilcoxon’s rank sum test) |
| 6. | Fageeh 52 | Vaginismus | Jeddah, Saudi Arabia | Not stated | 15 | Qualitative | Interviews | Descriptive analysis |
| 7. | Fejza et al. 53 | Vaginismus | Not stated (assumed to be Kosovo Ω ) | Not stated | 3 | Qualitative | Case series | Not stated |
| 8. | Kurban et al. 54 | Primary vaginismus | Ankara, Turkey | Not stated | 482 | Quantitative | Questionnaire | Descriptive statistics |
| 9. | Macey et al. 55 | Lifelong or acquired vaginismus | Online and Nottingham, East Midlands, the United Kingdom µ | Not stated | 13 | Qualitative | Interviews | Thematic analysis |
| 10. | Muammar et al. 56 | Vaginismus | Saudi Arabia | Not stated | 100 | Quantitative | Retrospective descriptive study | Pre- and post-intervention comparisons (Chi-squared tests) |
| 11. | Ogden and Ward 57 | Former or current vaginismus | The United Kingdom, Australia, and United States | Not stated | 89 | Mixed methods | Surveys with free responses | Quantitative descriptive statistics and thematic analysis ¥ |
| 12. | O’Sullivan 58 | Vaginismus | Ireland | Not stated | 23 | Qualitative | Observational study | Qualitative categories and descriptive statistics ¥ |
| 13. | Ramli et al. 59 | Vaginismus | Malaysia | Not stated | 3 | Qualitative | Case series | Not stated |
| 14. | Reissing 60 | Lifelong or acquired vaginismus | Online | N/A | 168 | Quantitative | Surveys | Between lifelong- and acquired-vaginismus group comparisons (Chi-squared tests) |
| 15. | Scholl 61 | Vaginismus | New York, United States µ | Not stated | 24 | Quantitative | Non-randomized study £ | Non-parametric two-tailed Mann-Whitney test |
| 16. | Stelko 62 | Primary vaginismus | Online – United States, European countries, and Israel | Not stated | 12 | Qualitative | In-depth interviews | Not stated |
| 17. | Svedhem et al. 63 | Vaginismus | Sweden | Grounded theory | 8 | Qualitative | Semi-structured interviews | Interpretative phenomenological analysis (IPA) |
| 18. | Thorpe et al. 64 | Vaginismus | Southern United States | Not stated | 1 β | Qualitative | Semi-structured interviews | Constructivist grounded theory |
| 19. | Tulla et al. 65 | Vaginismus | New York, United States µ | Not stated | 1 | Qualitative | Case study | Not stated |
| 20. | Ward and Ogden 66 | Former or current vaginismus | The United Kingdom, Australia, and United States | N/A | 89 ± | Mixed methods | Surveys with free responses | Descriptive statistics, between former- and current-vaginismus groups comparisons (two-tailed t-tests), and discourse analysis |
| 21. | Zgueb et al. 67 | Vaginismus | Not stated (assumed to be Tunisia Ω ) | N/A | 4 | Mixed methods | Case series | N/A |
| 22. | Zulfikaroglu 68 | Vaginismus | Ankara, Turkey | N/A | 472 | Mixed methods | Cross-sectional methodology, interview questionnaire, and gynaecological examination | Descriptive analysis |
IPA: interpretative phenomenological analysis.
Paper did not explicitly state mixed methods – this was assumed from the manuscript.
Assumed city/country as this information was not provided.
City/country was inferred from given information.
Paper did not explicitly state analytical methods – this was assumed from the manuscript.
Paper did not explicitly state it was a non-randomized study – this was assumed from the manuscript.
Ogden and Ward 57 and Ward and Ogden 66 used the same 89 participants in their studies which were only counted once in the sample total.
This study included 25 participants with various sexual pain issues. Only the data from one participant with vaginismus were extracted for this review.
Thematic analysis results
Four major themes emerged: Help-seeking process, Medical management, Help-seeking and sense of self, and Holistic care recommendations from the included studies. The major themes and relevant subthemes are detailed below as part of stage five outlined by Cooper 39 for the presentation of the integrative review findings. References are presented next to the key findings.
Theme 1: Help-seeking process
All the included studies described women’s experiences of seeking help for vaginismus in some way. Their experiences reflected both internal and external factors that influenced their treatment journeys. This included women’s Motivations to seek help and varied experiences with Health Professionals.
Motivations
Women with vaginismus were largely motivated by heterosexual and heteronormative expectations of womanhood to seek help. Women’s motivations included wanting to conceive a child, fears of not being able to have a long-term relationship or losing their partner, and wanting to achieve penis-in-vagina (PIV) sex.47,49 –51,53,54,56,58 –60,63,65,67 Women who were specifically motivated to treat their vaginismus to conceive a child were found to achieve treatment success faster than those who were only motivated to achieve PIV sex.50,61 However, it was also found that some women with vaginismus, who had not yet achieved PIV sex with treatment, used artificial or self-insemination strategies for conception.47,50,59,60,63,65,67 Self-insemination strategies included ‘splash pregnancy’ wherein there is no PIV penetration and instead ejaculation at the vaginal opening propels the sperm to the ovaries. 59
Only some women with vaginismus were motivated to seek help for other reasons, such as being able to insert tampons and to have examinations without anxiety or fear.51,60,63 For many women, previous, or anticipated, bad experiences with the healthcare system demotivated them from seeking help for their vaginismus.47,55,57,61 Often, women had to negotiate their personal reservations and the social taboo of discussing sexual matters before they could feel motivated to begin to seek help.47,53,55,58,59,62,64 Consequently, it frequently took women 1–3+ years to begin seeking help,48 –50,53,54 and up to 5–10 years in some cases.52,59
Health professionals
Women consulted a range of health professionals for their vaginismus. They found it helpful when health professionals were knowledgeable, emotionally supportive, and listened non-judgementally.49,57,64 Health professionals were unhelpful when they lacked understanding, did not appreciate or appropriately respond to women’s concerns pertaining to their vaginismus, or gave generic verbal advice such as telling women to ‘relax’.47,48,55,56,62,64 If women perceived having negative experiences with health professionals who did not take them seriously or made inappropriate comments, they stopped help-seeking for vaginismus and sometimes took years to seek help again.47,50,55
Women valued health professionals who had the specialist expertise to offer specific advice on treatments. In the countries of the United Kingdom, Australia, and the United States, women with vaginismus were most likely to first consult general practitioners to seek help and treatment.55,57,60 In the studies based in Tunisia, Iran, Saudi Arabia, and Turkey, specialist health professionals were more often consulted by women for vaginismus.47,48,56,67,68
Theme 2: Medical management
All the reviewed studies explored women’s different experiences to gain Diagnosis and/or undertake treatment Interventions. Some women indicated that there were difficulties in gaining a diagnosis of vaginismus. However, others also described how interventions were helpful.
Diagnosis
The studies indicated that women often consulted several sources, which could take years, to finally receive a diagnosis of vaginismus.47,50,53,55,57,60 Many women either had difficulty or were unable to complete physical examination which informed their diagnosis.47,55,58,59,65,67 Some women had received a prior diagnosis of provoked vestibulodynia, generalized vulvodynia, or a narrowed or thickened hymen.48,54,56,60,68 Many women sought help specifically for infertility and were diagnosed with vaginismus.47,49,58,59,61 The partners of some women with vaginismus were also diagnosed with male sexual dysfunctions.48,49,52,58,59,66,68
Interventions
Women attempted various interventions, often over several years. Common conventional and conservative treatments, which did not include invasive procedures, that women tried were vaginal trainers, pelvic floor exercises such as Kegels, relaxation, sensate focus exercises, sex education, various psychotherapies, cognitive behavioural therapy (CBT), and exposure therapy.49,51 –56,58 –60,62 Interventions had to address myths that women believed such as having a narrow vagina, pain and bleeding after having sex for the first time, and vaginal rupture with sex.49,54,59,66 Women’s partners often, but not always, participated in treatment such as therapy, physical touch exercises, or lending their fingers for vaginal insertion and desensitization with varying results.53,55,57,65,67
Women had varied responses to using vaginal trainers. While many women found vaginal trainers helpful,49,55,62,65 others needed more instructions to appropriately use trainers, 55 or required complementary treatments such as lubricant, 62 topical anaesthetic, 52 or escitalopram. 56 Women found it harder to progress through conservative treatment when they had more severe vaginismus.52,54 A few of these women used medical aids to facilitate conservative treatment (such as Botox injections).52,56 Some women were reported to have received hymenotomy which often did not treat symptoms.48,53,54,68 A few women insisted on, and received, a hymenotomy despite health professionals advising them that it was not necessary. 53
The authors of the studies based in Turkey, Saudi Arabia, Kosovo, and Tunisia described the societal culture as religious and viewing vaginismus as taboo.53,56,67,68 In these studies, women were reported as consulting faith healers or traditional non-academic medicine for their vaginismus.53,56,67,68 Moreover, treatment was adapted to suit the cultural context in more conservative countries.53,62,67 For example, religious figure heads were involved in CBT interventions to reframe the patient’s thinking, 67 or women made their own vaginal trainers in countries where they were not allowed to buy clinical vaginal trainers due to religious reasons. 62 Also, in more culturally conservative countries, such as the studies based in Tunisia, Iran, Kosovo, and Turkey, women referred to not receiving education from their family, hiding their vaginismus from relatives, or feeling pressure from family to conceive a child when they got married.47,48,53,54,67
Theme 3: Help-seeking and sense of self
There was a lack of explicit discussion of how women’s help-seeking for vaginismus shaped their constructions of self. Hence, this theme describes the limited findings from three included studies which report on women’s experiences of self in the context of living with their vaginismus. 75 Engman et al. 51 briefly discussed a correlation between women with vaginismus who completed CBT and a reported higher sense of self-worth as women and human beings. However, Engman et al. 51 also noted that they were uncertain whether the reported increase in self-worth was a result of CBT treatment because no such study exists to confirm this correlation. Ogden and Ward 57 explored how experiencing vaginismus influences women’s self-perception. Stelko 62 considers women’s experiences of vaginismus in relation to heteronormativity. While Engman et al. 51 and Ogden and Ward 57 more directly reported on the self, Stelko 62 implicitly discussed the self in relation to women’s perceptions of heteronormativity. However, these three studies did not explicitly consider how the process of help-seeking, specifically interactions with the healthcare system and other avenues to gain information, diagnosis, and treatment, impacts women’s constructions of self.
Theme 4: Holistic care recommendations from the included studies
The recommendations from nineteen included studies were centred around improving women’s healthcare experiences. Women and health professionals having congruent expectations towards the medical management of vaginismus may determine productive help-seeking experiences.47,49,52,55,57,61 Incongruent beliefs between patients and health professionals may foreshadow negative and varied help-seeking experiences for women with vaginismus.47,57 Therefore, health professionals should strive to have “a mutual understanding” with their patients regarding experiences of vaginismus and “expectations about therapeutic interventions” (p. 29). 57
Women may not initiate a discussion about vaginismus due to the stigma associated with sexual health.47,53,63 Those with vaginismus indicated that they would prefer health professionals to initiate discussions regarding their sexual health rather than bring up sexual concerns themselves due to it making them feel uncomfortable.47,50,53,63 Health professionals who are often the initial contact for vaginismus should be trained in sexual health to better treat women with the condition.54,56,65 There should be a multidisciplinary health professional team to support the varied treatment needs of women with vaginismus.47,56,59,60,65 Also, the approach to treat vaginismus should be adapted to suit the cultural context of the patients.47,53,55,56,67,68 In predominantly Muslim countries, given the closeness and/or importance of the family, treatment should educate family members to better support women with vaginismus.48,67,68
Discussion
This review found that while women with vaginismus have varied experiences of seeking help, there are also commonalities. Common unhelpful actions of health professionals were to not appropriately respond to women’s raised concerns or provide generic verbal advice which fostered negative help-seeking experiences for women. Such unhelpful actions cannot be assumed as a sign of uncaring health professionals. Rather, the review’s findings suggest that health professionals, including doctors, are lacking knowledge to support those with vaginismus and recognize symptoms of the condition. This aligns with Pacik’s 3 contention that vaginismus is not sufficiently taught in medical schools or discussed in medical meetings. In fact, in a study by Auwad and Hagi, 76 73% of Arab gynaecologists, 47% of British Society of Urogynaecology (BSUG) gynaecologists, and 23% of the American Urogynaecologic Society (AUGS) gynaecologists reported themselves as being unsatisfied with their training in female sexual dysfunction. Therefore, it is important that all health professionals, especially health professionals who tend to be the first port of healthcare, are trained in future to be better versed in female sexual dysfunctions. This may help to minimize the number of referrals that those with vaginismus need to gain a diagnosis.
Women with vaginismus appeared to be predominantly motivated to seek help to meet the heterosexual and heteronormative expectations for women. Put differently, women with vaginismus seemed driven to seek help by a desire to achieve PIV sexual intercourse, which is also known as the ‘coital imperative’.77,78 In the studies based in Tunisia, India, Kosovo, Saudi Arabia, Malaysia, and Turkey, women’s coital imperative was often primarily driven by societal expectations to become a mother.47,49,53,56,59,68 While women in the studies focused in the Netherlands, Sweden, the United States, and European countries were motivated to seek help for vaginismus to become mothers, many were also driven by a need to sexually satisfy their partners.50,51,60,62,63 Such desires to become a mother and sexually please male partners through PIV sex are part of the embodied expectations held towards heterosexual women. 79
The studies did not directly discuss how women’s help-seeking for vaginismus impacted their sense of self. Nonetheless, information gathered within this review suggests that women’s help-seeking for vaginismus shaped their perceived sense of self with respect to conforming or deviating from heteronormative femininity. The ideals of heteronormative femininity dictate that ‘a good woman’ is: receptive to the penis for the coital imperative; a man’s partner; and a mother. 80 Since women with vaginismus may not be able to achieve the aforementioned, they often feel like their ‘self-image of femininity’ has been jeopardized and have trouble ‘believing in themselves as women’ (p. 12). 33 This can drive women to not believe in themselves, which can exacerbate their struggles to find help or follow treatment.
Strategies should be developed and employed by health professionals to ‘redo’ heteronormative femininity by normalizing non-penetrative sex.81,82 This can strengthen women’s sense of self to believe in themselves as capable women to persevere even when their treatment-seeking journey is trying. However, the heterosexual and heteronormative motivations of those with vaginismus in the included studies cannot be generalized to all people with the condition. These findings may be skewed by the generally heterosexual orientation of participants in the studies. For instance, those with diverse sexual and gender identities often do not subscribe to heteronormative femininity, or relate to the embodied expectations held towards heterosexual women.
Given that the locations of the included studies were based in some religious and other non-religious countries, key cultural differences between women’s help-seeking experiences for vaginismus were highlighted. The prevalence of vaginismus in religious countries has been reported to be higher.6,17,67,83,84 In religious societies where women are very close to family, trusted religious figures and family members may need to be involved in treatment to foster the appropriate support and positive interactions to help strengthen women’s sense of self to overcome vaginismus.48,67,68 Moreover, Stelko 62 referred to how women in her study had to make vaginal trainers due to not being able to buy it in certain countries due to religious reasons. Conventional vaginismus treatments focused on vaginal insertion and physical touch may be taboo in the religious cultures of certain countries. 67 Therefore, conventional treatment approaches for vaginismus and professional practice should be adapted to suit women’s cultural context to foster positive help-seeking experiences for them.21,67
Six out of the seven studies based in the multicultural Western countries of Australia, the United States, and the United Kingdom did not articulate that attempts were made to recruit participants from diverse ethnic backgrounds.55,57,60,61,65,66 While Thorpe et al. 64 focused on Black women, the data from one participant in their study which was extracted into this integrated review were not enough to inform results on ethnically diverse women’s experiences of vaginismus and its impact on their constructions of self. It cannot be assumed that all the participants from the other six studies identified as White. However, future research on this topic should strive to include participants from diverse non-White backgrounds, especially in multicultural Western countries. This can help to generate data to improve the unique help-seeking experiences for women with vaginismus from culturally diverse backgrounds when navigating Western healthcare systems.
The fact that none of the included studies explicitly discussed how help-seeking for vaginismus impacts women’s sense of self highlights an epistemological gap in the literature. It has been overlooked that help-seeking impacts women’s strength of the therapeutic alliance and constructions of sense of self in ways that can have implications on their treatment journeys for vaginismus. This should be investigated in future research to improve health outcomes for those who receive a vaginismus diagnosis.
Limitations
In line with stage five of Cooper’s framework, the limitations of the integrated review are examined. The participants in the included studies were described exclusively as women. The sexual orientation of participants was missing from 18 studies. Therefore, the unique help-seeking experiences of those who do not identify as women or heterosexual could not be represented in this review. Only three studies55,57,60 focused on help-seeking in its research aim or objective which may reflect that the concept and term ‘help-seeking’ is not universally used. Six included studies that were of low methodological quality according to the MMAT could potentially have a high risk of bias, which reduces the trustworthiness of the review findings. Future studies on women’s experiences of vaginismus need to strive to better meet its methodological criteria to increase the number of quality studies in an under-researched area. Some of this review’s findings are informed by included studies that have very small sample sizes which poses a risk of participant selection bias. Fourteen included studies lacked a clearly stated theoretical approach. This presents issues for the interpretation of findings, and the potential of transferability because there is no guide to conceptualize how a study applies to broader contexts. 85 Unpublished and non-peer-reviewed literature, such as master's and doctoral theses, were excluded from the search. However, the retrieval and analysis of unpublished dissertations is time-consuming and laborious, and the benefit of including dissertations in reviews is minimal as they are unlikely to change the conclusions. 86
Conclusion
This is the first integrative review to describe mixed methods of evidence to examine women’s help-seeking experiences for their vaginismus and its impact on their constructions of self. The review found that women continue to face difficulties in seeking and receiving help for vaginismus. Conventional treatment approaches for vaginismus should be amended to suit women’s cultural context to improve their help-seeking outcomes. The review also identified an epistemological gap in the literature regarding how women’s help-seeking experiences for their vaginismus impact their constructions of self, which highlights it as an under-researched area. This review of evidence uncovers an important inferred correlation between women’s help-seeking for vaginismus shaping their construction of a sense of self in relation to heteronormative femininity. Future research should not be limited to heterosexual women but include the experiences of those with vaginismus who have diverse gender identities. The experiences of those from culturally and ethnically diverse backgrounds, especially in multicultural Western countries, should be examined. Research should focus on people’s help-seeking for vaginismus and its impact on their sense of self to provide insight into how it can determine their responses to treatment. Such findings can be used in the future for people with vaginismus, health professionals, and in policy to understand how to better support those with vaginismus to seek help and construct a positive sense of self to persevere with treatment regimens.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057231199383 for The experiences of women seeking help for vaginismus and its impact on their sense of self: An integrative review by Rashmi Pithavadian, Jane Chalmers and Tinashe Dune in Women’s Health
Acknowledgments
The authors thank the Western Sydney University online library for providing them access to conduct database searches and view non-open access articles to undertake this review.
Footnotes
ORCID iD: Rashmi Pithavadian  https://orcid.org/0000-0002-7499-9393
https://orcid.org/0000-0002-7499-9393
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: Ethics approval and consent was not required for this research because it did not involve human participants. Published information that is available online was used as the dataset.
Consent for publication: Not applicable
Author contribution(s): Rashmi Pithavadian: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Writing – original draft; Writing – review & editing.
Jane Chalmers: Conceptualization; Methodology; Supervision; Validation; Writing – review & editing.
Tinashe Dune: Conceptualization; Methodology; Supervision; Validation; Writing – review & editing.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Western Sydney University provided funding for the open-access article processing charges to publish this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Availability of data and materials: Database searches have been provided as a table for replication of search results. Any further information pertaining to data will be available upon reasonable request from the corresponding author’s email address (R.Pithavadian@westernsydney.edu.au).
References
- 1. ter Kuile MM, Weijenborg PTM. A woman who never could have coitus: treatment of lifelong vaginismus. In: Paarlberg KM, Van de Wiel HBM. (eds) Bio-psycho-social obstetrics and gynecology: a competency-oriented approach. Cham: Springer International Publishing, 2017, pp. 297–309. [Google Scholar]
- 2. Pacik PT, Babb CR, Polio A, et al. Case series: redefining severe grade 5 vaginismus. Sex Med 2019; 7(4): 489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pacik PT. Understanding and treating vaginismus: a multimodal approach. Obstet Gynecol Surv 2015; 70: 314–316. [Google Scholar]
- 4. Azim KA, Happel-Parkins A, Moses A, et al. Exploring relationships between Genito-Pelvic Pain/Penetration Disorder, sex guilt, and Religiosity Among College Women in the US. J Sex Med 2021; 18(4): 770–782. [DOI] [PubMed] [Google Scholar]
- 5. Reissing ED, Borg C, Spoelstra SK, et al. ‘Throwing the baby out with the bathwater’: the demise of Vaginismus in favor of Genito-Pelvic Pain/Penetration Disorder. Arch Sex Behav 2014; 43(7): 1209–1213. [DOI] [PubMed] [Google Scholar]
- 6. McEvoy M, McElvaney R, Glover R. Understanding vaginismus: a biopsychosocial perspective. Sex Relatsh Ther. Epub ahead of print 5 December 2021. DOI: 10.1080/14681994.2021.2007233. [DOI] [Google Scholar]
- 7. Conforti C. Genito-Pelvic Pain/Penetration Disorder (GPPPD): an overview of current terminology, etiology, and treatment. Univ Ottawa J Med 2017; 7: 48. [Google Scholar]
- 8. Seehusen DA, Baird DC, Bode DV. Dyspareunia in women. Am Fam Physician 2014; 90: 465–470. [PubMed] [Google Scholar]
- 9. Ramanathan V, Gautham K, Ramasubramaniam UM. Common pitfalls in the management of vaginismus in couples with subfertility in India. J Psychosex Health 2022; 4: 133–137. [Google Scholar]
- 10. Zulfikaroglu E, Yaman S. Obstetric outcomes of 297 women treated for vaginismus. Eur J Obstet Gynecol Reprod Biol 2022; 276: 134–138. [DOI] [PubMed] [Google Scholar]
- 11. Cryle P, Moore A. Vaginismus. In: Cryle P, Moore A. (eds) Frigidity: an intellectual history. London: Palgrave Macmillan, 2011, pp. 67–99. [Google Scholar]
- 12. Laskowska A, Gronowski P. Vaginismus: an overview. J Sex Med 2022; 19: S228–S229. [Google Scholar]
- 13. Velayati A, Jahanian Sadatmahalleh S, Ziaei S, et al. Can botox offer help women with vaginismus? A systematic review and meta-analysis. Int J Sex Health 2019; 31: 233–243. [Google Scholar]
- 14. Velayati A, Jahanian Sadatmahalleh S, Ziaei S, et al. The role of personal factors in quality of life among Iranian women with vaginismus: a path analysis. Health Qual Life Outcomes 2021; 19: 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harish T, Muliyala K, Murthy P. Successful management of vaginismus: an eclectic approach. Indian J Psychiatry 2011; 53: 154–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Andresen JB, Graugaard C, Andersson M, et al. Sexual inactivity and dysfunction in Denmark: a Project SEXUS study. Arch Sex Behav 2022; 51(8): 3669–3688. [DOI] [PubMed] [Google Scholar]
- 17. Amidu N, Owiredu WK, Woode E, et al. Incidence of sexual dysfunction: a prospective survey in Ghanaian females. Reprod Biol Endocrinol 2010; 8: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Oksuz E, Malhan S. Prevalence and risk factors for female sexual dysfunction in Turkish women. J Urology 2006; 175: 654–658. [DOI] [PubMed] [Google Scholar]
- 19. Jeng C-J. The pathophysiology and etiology of vaginismus. Taiwan J Obstet Gynecol 2004; 43: 10–15. [Google Scholar]
- 20. Shafik A, El-Sibai O. Study of the pelvic floor muscles in vaginismus: a concept of pathogenesis. Eur J Obstet Gynecol Reprod Biol 2002; 105: 67–70. [DOI] [PubMed] [Google Scholar]
- 21. Lahaie MA, Boyer SC, Amsel R, et al. Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment. Womens Health 2010; 6(5): 705–719. [DOI] [PubMed] [Google Scholar]
- 22. Pacik PT, Geletta S. Vaginismus treatment: clinical trials follow up 241 patients. Sex Med 2017; 5(2): e114–e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al-Sughayir MA. Vaginismus treatment. Hypnotherapy versus behavior therapy. Neurosciences 2005; 10: 163–167. [PubMed] [Google Scholar]
- 24. Binik YM. Will vaginismus remain a ‘lifelong’ baby? Response to Reissing et al. (2014). Arch Sex Behav 2014; 43(7): 1215–1217. [DOI] [PubMed] [Google Scholar]
- 25. Bravo CS, Meléndez JC, Ayala NPC, et al. Perfiles e indicadores psicológicos relacionados con la dispareunia y el vaginismo: Estudio cualitativo, Segunda Parte. Salud Mental 2010; 33: 437–449. [Google Scholar]
- 26. Koops TU, Wiessner C, Ehrenthal JC, et al. Assessing psychodynamic conflicts and level of personality functioning in women diagnosed with vaginismus and dyspareunia. Front Psychol 2021; 12: 687369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mellado BH, Pilger TL, Poli-Neto OB, et al. Current usage of qualitative research in female pelvic pain: a systematic review. Arch Gynecol Obstet 2019; 300(3): 495–501. [DOI] [PubMed] [Google Scholar]
- 28. Donaldson RL, Meana M. Early dyspareunia experience in young women: confusion, consequences, and help-seeking barriers. J Sex Med 2011; 8(3): 814–823. [DOI] [PubMed] [Google Scholar]
- 29. Rickwood D, Thomas K. Conceptual measurement framework for help-seeking for mental health problems. Psychol Res Behav Manag 2012; 5: 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shallcross R, Dickson JM, Nunns D, et al. Women’s experiences of vulvodynia: an interpretative phenomenological analysis of the journey toward diagnosis. Arch Sex Behav 2019; 48(3): 961–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Witzeman K, Flores OA, Renzelli-Cain RI, et al. Patient-physician interactions regarding dyspareunia with endometriosis: Online survey results. J Pain Res 2020; 13: 1579–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zarski AC, Berking M, Ebert DD. Efficacy of Internet-based guided treatment for genito-pelvic pain/penetration disorder: rationale, treatment protocol, and design of a randomized controlled trial. Front Psychiatry 2018; 8: 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Theve-Gibbons S. Women and chronic pelvic pain: stigma, invisibility, and sexuality. J Sect Women’s Health 2000; 24: 7–12. [Google Scholar]
- 34. Chrisler JC, Johnston-Robledo I. Woman’s embodied self: feminist perspectives on identity and image. Washington, DC: American Psychological Association (APA), 2018. [Google Scholar]
- 35. Ferrè ER, Lopez C, Haggard P. Anchoring the self to the body: vestibular contribution to the sense of self. Psychol Sci 2014; 25(11): 2106–2108. [DOI] [PubMed] [Google Scholar]
- 36. Melillo KD. Formulating review question. In: Toronto CE, Remington R. (eds) A step-by-step guide to conducting an integrative review. Cham: Springer International Publishing, 2020, pp. 11–20. [Google Scholar]
- 37. Munn Z, Stern C, Aromataris E, et al. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 2018; 18: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Toronto CE. Overview of the integrative review. In: Toronto CE, Remington R. (eds) A step-by-step guide to conducting an integrative review. Cham: Springer International Publishing, 2020, pp. 1–9. [Google Scholar]
- 39. Cooper HM. Scientific guidelines for conducting integrative research reviews. Rev Educ Res 1982; 52: 291–302. [Google Scholar]
- 40. Lizarondo L, Stern C, Carrier J, et al. Chapter 8: mixed methods systematic reviews. In: Aromataris E, Munn Z. (eds) JBI manual for evidence synthesis. Adelaide, SA, Australia: Joanna Briggs Institute; (JBI), 2020. [Google Scholar]
- 41. Lawless J, Foster MJ. Searching systematically and comprehensively. In: Toronto CE, Remington R. (eds) A step-by-step guide to conducting an integrative review. Cham: Springer International Publishing, 2020, pp. 21–44. [Google Scholar]
- 42. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 350: g7647. [DOI] [PubMed] [Google Scholar]
- 44. Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005; 331: 1064–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Badampudi D, Wohlin C, Petersen K. Experiences from using snowballing and database searches in systematic literature studies. In: Proceedings of the 19th international conference on evaluation and assessment in software engineering, Nanjing, China, 27–29 April 2015, p. 17. New York: Association for Computing Machinery (ACM). [Google Scholar]
- 46. Schlosser RW, Wendt O, Bhavnani S, et al. Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: the application of traditional and comprehensive Pearl Growing. Int J Lang Commun Disord 2006; 41(5): 567–582. [DOI] [PubMed] [Google Scholar]
- 47. Achour R, Koch M, Zgueb Y, et al. Vaginismus and pregnancy: epidemiological profile and management difficulties. Psychol Res Behav Manag 2019; 12: 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Akhavan-Taghavi MH, Asghari-Moghaddam MA, Froutan SK, et al. Vaginismus in Iran: a single center report of 7 years experience. Nephrourol Mon 2015; 7(6): e30077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bhatt JK, Patel VS, Patel AR. A study of vaginismus in patients presenting with infertility. Int J Reprod Contracept Obstet Gynecol 2017; 6: 5508–5511. [Google Scholar]
- 50. Drenth JJ, Andriessen S, Heringa MP, et al. Connections between primary vaginismus and procreation: some observations from clinical practice. J Psychosom Obstet Gynaecol 1996; 17(4): 195–201. [DOI] [PubMed] [Google Scholar]
- 51. Engman M, Wijma K, Wijma B. Long-term coital behaviour in women treated with cognitive behaviour therapy for superficial coital pain and vaginismus. Cogn Behav Ther 2010; 39(3): 193–202. [DOI] [PubMed] [Google Scholar]
- 52. Fageeh WMK. Different treatment modalities for refractory vaginismus in Western Saudi Arabia. J Sex Med 2011; 8(6): 1735–1739. [DOI] [PubMed] [Google Scholar]
- 53. Fejza H, Icka E, Fejza F. Vaginismus as a hidden problem: our case series. Int J Adv Stud Sex 2021; 3: 5–9. [Google Scholar]
- 54. Kurban D, Eserdag S, Yakut E, et al. The treatment analysis of the patients suffering from vaginismus and the correlation with the psychological issues. Int J Reprod Contracept Obstet Gynecol 2021; 10: 1328–1336. [Google Scholar]
- 55. Macey K, Gregory A, Nunns D, et al. Women’s experiences of using vaginal trainers (dilators) to treat vaginal penetration difficulties diagnosed as vaginismus: a qualitative interview study. BMC Womens Health 2015; 15: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Muammar T, McWalter P, Alkhenizan A, et al. Management of vaginal penetration phobia in Arab women: a retrospective study. Ann Saudi Med 2015; 35(2): 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ogden J, Ward E. Help-seeking behaviour in sufferers of vaginismus. Sex Marital Ther 1995; 10: 23–30. [Google Scholar]
- 58. O’Sullivan K. Observations on vaginismus in Irish women. Arch Gen Psychiatry 1979; 36(7): 824–826. [DOI] [PubMed] [Google Scholar]
- 59. Ramli M, Nora M, Roszaman R, et al. Vaginismus and subfertility: case reports on the association observed in clinical practice. Malays Fam Physician 2012; 7(1): 24–27. [PMC free article] [PubMed] [Google Scholar]
- 60. Reissing ED. Consultation and treatment history and causal attributions in an online sample of women with lifelong and acquired vaginismus. J Sex Med 2012; 9(1): 251–258. [DOI] [PubMed] [Google Scholar]
- 61. Scholl GM. Vaginismus and infertility. J Psychosom Obst Gyn 1991; 12: 45–49. [Google Scholar]
- 62. Stelko S. Practicing vaginistic femininity: doing bodies, enacting normative heterosexuality. J Comp Res Anthropol Sociol 2015; 6: 31–50. [Google Scholar]
- 63. Svedhem C, Eckert G, Wijma B. Living with genito-pelvic pain/penetration disorder in a heterosexual relationship: an interpretative phenomenological analysis of interviews with eight women. Sex Relatsh Ther 2013; 28: 336–349. [Google Scholar]
- 64. Thorpe S, Iyiewuare P, Ware S, et al. ‘Why would i talk to them about sex?’: Exploring patient-provider communication among black women experiencing sexual pain. Qual Health Res 2022; 32(10): 1527–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Tulla ME, Dunn ME, Antilus R, et al. Vaginismus and failed in vitro fertilization. Sex Relatsh Ther 2006; 21: 439–443. [Google Scholar]
- 66. Ward E, Ogden J. Experiencing vaginismus–sufferers beliefs about causes and effects. Sex Marital Ther 1994; 9: 33–45. [Google Scholar]
- 67. Zgueb Y, Ouali U, Achour R, et al. Cultural aspects of vaginismus therapy: a case series of Arab-Muslim patients. Cogn Behav Ther 2019; 12: e3. [Google Scholar]
- 68. Zulfikaroglu E. Patient’s characteristics and outcome of therapy in vaginismus: a single-center report of nine-year experience. Sex Relatsh Ther 2023; 38: 24–36. [Google Scholar]
- 69. Hong QN, Pluye P, Fàbregues S, et al. Mixed Methods Appraisal Tool (MMAT), 2018, http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf [DOI] [PubMed]
- 70. Hong QN, Pluye P, Fabrègues S, et al. Reporting the results of the MMAT (version 2018), 2020, http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/140056890/Reporting%20the%20results%20of%20the%20MMAT.pdf
- 71. Dixon-Woods M, Agarwal S, Jones D, et al. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005; 10(1): 45–53. [DOI] [PubMed] [Google Scholar]
- 72. Ryan C, Hesselgreaves H, Wu O, et al. Protocol for a systematic review and thematic synthesis of patient experiences of central venous access devices in anti-cancer treatment. Syst Rev 2018; 7: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Dwyer PA. Analysis and synthesis. In: Toronto CE, Remington R. (eds) A step-by-step guide to conducting an integrative review. Cham: Springer International Publishing, 2020, pp. 57–70. [Google Scholar]
- 74. Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006; 13(1): 29. [PMC free article] [PubMed] [Google Scholar]
- 75. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 76. Auwad WA, Hagi SK. Female sexual dysfunction: what Arab gynecologists think and know. Int Urogynecol J 2012; 23(7): 919–927. [DOI] [PubMed] [Google Scholar]
- 77. Ayling K, Ussher JM. ‘If sex hurts, am I still a woman?’ The subjective experience of vulvodynia in hetero-sexual women. Arch Sex Behav 2008; 37: 294–304. [DOI] [PubMed] [Google Scholar]
- 78. McPhillips K, Braun V, Gavey N. Defining (hetero)sex: how imperative is the ‘coital imperative’? Women Stud Int Forum 2001; 24: 229–240. [Google Scholar]
- 79. Sörensdotter R. Heteronormativity as a painful script: how women with vulvar pain (re)negotiate sexual practice. In: Rees E. (ed.) Talking bodies: interdisciplinary perspectives on embodiment, gender and identity. Cham: Springer International Publishing, 2017, pp. 163–182. [Google Scholar]
- 80. Ussher JM. Fantasies of femininity: reframing the boundaries of sex. London: Penguin Books, 1997. [Google Scholar]
- 81. Connell C. Doing, undoing, or redoing gender?: Learning from the workplace experiences of transpeople. Gender Soc 2010; 24: 31–55. [Google Scholar]
- 82. West C, Zimmerman DH. Doing gender. Gender Soc 1987; 1: 125–151. [Google Scholar]
- 83. Farnam F, Janghorbani M, Merghati-Khoei E, et al. Vaginismus and its correlates in an Iranian clinical sample. Int J Impot Res 2014; 26(6): 230–234. [DOI] [PubMed] [Google Scholar]
- 84. Ozdemir O, Simsek F, Ozkardeş S, et al. The unconsummated marriage: its frequency and clinical characteristics in a sexual dysfunction clinic. J Sex Marital Ther 2008; 34(3): 268–279. [DOI] [PubMed] [Google Scholar]
- 85. Evans BC, Coon DW, Ume E. Use of theoretical frameworks as a pragmatic guide for mixed methods studies: a methodological necessity? J Mix Methods Res 2011; 5: 276–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Vickers AJ, Smith C. Incorporating data from dissertations in systematic reviews. Int J Technol Assess Health Care 2000; 16(2): 711–713. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057231199383 for The experiences of women seeking help for vaginismus and its impact on their sense of self: An integrative review by Rashmi Pithavadian, Jane Chalmers and Tinashe Dune in Women’s Health