Abstract
We report a case of a woman presenting with acute onset of delirium following ingestion of Amanita muscaria mushrooms for anxiolytic effect. Immediate diagnosis was obtained after taking a detailed history and confirmation with online poison database images. She fully recovered with supportive treatment and was discharged 24 hours after presentation. To the best of our knowledge, this is the first case report on A muscaria mushroom poisoning in the UK.
KEYWORDS: Amanita muscaria, mushroom, poisoning
Clinical presentation
A 46-year-old woman, a Ukrainian emigrant, presented to the emergency department (ED) in the early hours of the morning in an acute confusional state. She had been found at home by her son at around 10pm acutely confused, complaining of ‘feeling cold’. She had been seen earlier in the evening by a family member and was then well in herself. On arrival to the ED, she had a temperature of 37.9°C but normal vital signs. She was extremely agitated with slurred speech and shouting. She had what appeared to be vivid visual and auditory hallucinations, in addition to involuntary twitching of her upper limbs.
On examination, Glasgow Coma Scale (GCS) was 10/15 (E2V3M5), with pupils equal and reactive to light. There were no signs of meningism. She was initially treated with IM lorazepam 2 mg, empirical IV ceftriaxone and acyclovir for presumptive central nervous system (CNS) infection.
Initial laboratory investigations revealed microcytic anaemia and mild lactic acidosis (Table 1). Her ECG showed normal sinus rhythm. Imaging studies, including chest X-ray and CT head, were normal.
Table 1.
Initial investigations
| Biochemistry | ||
| Sodium | 141 mmol/L | 136–145 |
| Potassium | 4.3 mmol/L | 3.5–5.1 |
| Urea | 10.1 mmol/L | 2.5–6.7 |
| Creatinine | 81 umol/L | 50–98 |
| C-reactive protein | 12 mg/L | 0–5 |
| Creatine kinase | 124 U/L | 29–168 |
| Total protein | 46 g/L | 64–83 |
| Albumin | 23 g/L | 35–50 |
| Alanine transferase | 14 U/L | 10–35 |
| Alkaline phosphatase | 39 U/L | 40–150 |
| Total bilirubin | 2 umol/L | 0–21 |
| Total globulins | 23 g/L | 20–39 |
| Haematology | ||
| Haemoglobin | 93 g/L | 115–165 |
| White blood count | 12.2 × 109/L | 3.7–11 |
| Platelets | 371 × 109/L | 150–450 |
| Mean cell volume | 65 fl | 80–100 |
| INR | 1.0 | |
| Toxicology | ||
| Paracetamol | <3 mg/L | >50 @12 hr |
| Salicylate | <50 mg/L | 0–300 |
| Venous blood gas on arrival | ||
| pH | 7.31 | 7.32–7.43 |
| pCO2 | 6.6 kPa | 1.16–1.32 |
| pO2 | 4.0 kPa | 3.6–5.3 |
| Ca | 1.11 mmol/L | 0.6–1.4 |
| Glucose | 7.5 mmol/L | 22.0–29.0 |
| Lactate | 3.0 mmol/L | |
| Base excess | −1.7 | |
| HCO3 | 22.5 mmol/L |
As the patient became more awake and coherent, a more detailed history was obtained with her 16-year-old daughter acting as an interpreter. Her only past medical history included iron deficiency anaemia. There was no history of recent foreign travel, excessive alcohol intake or recreational drug use. She was not on any regular medications.
She reported a daily ingestion of 0.5 g of raw red-orange mushroom on a regular basis in the evenings for the past 2 weeks. These mushrooms are considered a common herbal remedy to help with sleep or relieve stress/anxiety in her country of origin. She had purchased 20 g of dried mushrooms via a social media website. On the night before admission, she had taken ∼1 g of dried mushroom before going to bed as she had been told by her mother, who was still in Ukraine, that their hometown was being heavily shelled. 2–3 hours later, she woke up feeling drunk with extremely vivid visual and auditory hallucinations, including beliefs that she was flying and her dead grandmother was talking to her, out-of-body experiences, and finally the sense that she had died before being reborn.
Her husband subsequently brought in the mushroom, which corresponds to dried Amanita muscaria mushroom in TOXBASE®, the clinical toxicology database providing information on diagnosis and treatment of poisoning. A urine toxicology screen was sent. She was subsequently diagnosed with A muscaria mushroom poisoning and antimicrobial therapy was stopped. IV Hartmann's infusion was continued in view of hyperlactatemia. She regained full consciousness 8 hours after ingestion of the dried mushroom. She was monitored in the hospital for 24 hours before being discharged with safety netting.
Discussion
A muscaria, commonly known as fly agaric mushroom, is a type of mushroom native to the temperate regions of the Northern Hemisphere.1 Traditionally, it has been used for the control of house flies because of its ability to attract and intoxicate flies.1 The muscaria originates from the Latin word musca, ‘a fly’. It has a distinctive large red to orange-yellow cap mottled with white/yellow spots on its surface.1 These mushrooms appear an orange/brown colour after drying but the mottled spotting can still be clearly visible (Fig 1).
Fig 1.
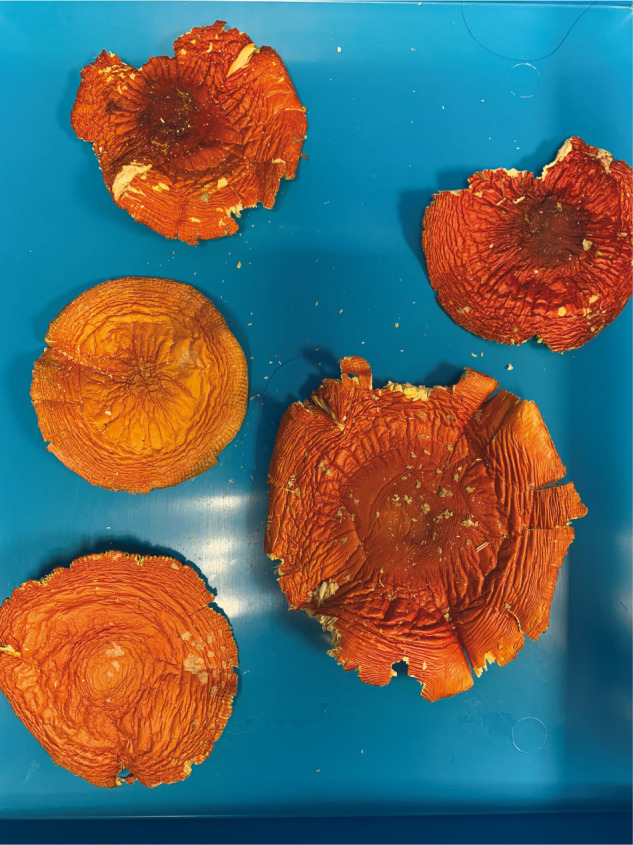
Amanita muscaria, commonly known as fly agaric mushroom.
The medicinal use of this mushroom is historically observed in Siberia, Ukraine and Eastern Europe since ancient times for treatment of anxiety, insomnia and inflammatory disorders.2 It is unlawful to trade A muscaria for human consumption in the UK as it is classified as a poisonous substance under the 1971 Misuse of Drugs Act. However, it can still be purchased illegally over the online websites and social media platforms.
A muscaria is well known for its hallucinogenic and psychoactive properties.2 The main constituents include biologically active muscimol and its precursor, ibotenic acid.1 Muscimol is generated from ibotenic acid by decarboxylation.1 Muscimol is structurally similar to gamma aminobutyric acid (GABA) whereas Ibotenic acid is closely related to glutamic acid.3 These neurotoxins are responsible for most of the CNS symptoms via their effects on GABA and glutamic acid receptors in the brain.4 Drying of mushroom may potentiate its psychoactive properties via enhanced conversion of ibotenic acid to muscimol.4
Symptoms typically occur 30 minutes to 2 hours after ingestion of the mushroom.5,6 The effects can be variable, depending on the amount of mushroom ingestion, preparation (fresh vs dried) and processing (raw vs boiled).1,7 The cardinal manifestations include CNS symptoms such as visual and/or auditory hallucinations, confusion, incoherent speech, agitation and dizziness.5 Nausea, vomiting, diarrhoea, abdominal cramps may happen soon after ingestion.6 Seizure and coma can occur, especially in children.6 Fatality, albeit rarely, has been reported in severe cases.7 The duration of symptoms varies from 8–24 hours.8 Recovery is typically complete within 24 hours.8
Supportive treatment is the key for A muscaria poisoning.7,8 Activated charcoal and gastric lavage can be considered if presentation is within 1–2 hours of ingestion.4 There is no specific antidote for A muscaria poisoning. Benzodiazepines can be used for psychoactive symptoms and seizures.5 It is important to monitor and correct fluid/electrolyte derangements. Patients should be closely monitored till signs and symptoms have completely resolved prior to discharge.
Learning points
Obtaining a comprehensive history is imperative to the diagnosis of accidental mushroom poisoning.
The predominant features of A muscaria poisoning typically involve neuropsychiatric symptoms due to its psychoactive constituents.
The rapid and correct identification of the mushroom is essential for early diagnosis, appropriate treatment and preventing unwarranted investigations.
References
- 1.Michelot D, Melendez-Howell LM. Amanita muscaria: chemistry, biology, toxicology, and ethnomycology. Mycol Res 2003;107:131–46. [DOI] [PubMed] [Google Scholar]
- 2.Feeney K. (Ed). Fly Agaric: A compendium of history, pharmacology, mythology and exploration. Ellensburg WA: Fly Agaric Press, 2020. [Google Scholar]
- 3.Johnston GA, Curtis DR, De Groat WC, et al. Central actions of ibotenic acid and muscimol. Biochem Pharmacol 1968;17:2488–9. [DOI] [PubMed] [Google Scholar]
- 4.Tsujikawa K, Mohri H, Kuwayama K, et al. Analysis of hallucinogenic constituents in Amanita mushrooms circulated in Japan. Forensic Sci Int 2006;164:172–8. [DOI] [PubMed] [Google Scholar]
- 5.Rampolli FI, Kamler P, Carnevale Carlino C, et al. The deceptive mushroom: accidental Amanita muscaria poisoning. Eur J Case Rep Intern Med 2021;8:002212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benjamin DR. Mushroom poisoning in infants and children: the Amanita pantherina/muscaria group. J Toxicol Clin Toxicol 1992;30:13–22. [DOI] [PubMed] [Google Scholar]
- 7.Meisel EM, Morgan B, Schwartz M, et al. Two cases of severe amanita muscaria poisoning including a fatality. Wilderness Environ Med 2022;33:412–6. [DOI] [PubMed] [Google Scholar]
- 8.Satora L, Pach D, Butryn B, et al. Fly agaric (Amanita muscaria) poisoning, case report and review. Toxicon 2005;45:941–3. [DOI] [PubMed] [Google Scholar]


