Abstract
Abnormal uterine bleeding is a term used to describe any irregular bleeding from the uterus that is not part of a woman's normal menstrual cycle and can happen during different life periods. Abnormal uterine bleeding can have structural etiologies (polyp, adenomyosis, leiomyoma, malignancy) or nonstructural etiologies (coagulopathy, ovulatory dysfunction, and not-classified). The post- and pre-menopausal period requires a detailed investigation to establish the etiology of the bleeding because the chances that the woman has a malignancy are plentiful in this period. The treatment plan is determined based on the underlying cause of the bleeding. The main objective of this paper was to determine the prevalence of endometrial carcinoma in different periods, focusing on the postmenopausal period. This research was a cross-sectional study and included 79 cases of abnormal uterine bleeding in different periods of women's lives. Our study found that abnormal uterine bleeding occurs more frequently during the premenopausal period (59%) and that the causes of irregular bleeding during this period were mainly benign. Our study focused on the postmenopausal period, where we found that 32.9% of irregular uterine bleeding occurs during this period, and the leading causes were malignant pathologies (83.3%), mainly endometrial adenocarcinomas. The average age was 66.7 years. During the study, it was observed that 50% of women with abnormal uterine bleeding due to malignancy were classified as overweight, 25% were obese, and 25% had normal weight. It was confirmed that obesity is a co-factor of malignancy in the postmenopausal period, and the pathophysiological mechanism is well understood now. Our study also found a high number of co-morbidities among women with abnormal uterine bleeding due to malignancy. We came to the conclusion that any abnormal uterine bleeding should be initially investigated in a multidisciplinary manner, an accurate diagnosis should be determined, and then a treatment plan should be established. The treatment strategy should be determined depending on the cause of abnormal bleeding.
Keywords: Abnormal uterine bleeding , premenopausal period , postmenopausal period , malignancy
Introduction
Abnormal uterine bleeding (AUB) is a term used to describe any irregular bleeding from the uterus that is not part of a woman's normal menstrual cycle.
This can include bleeding that is heavier or lighter, and it can happen during different life periods for a woman, including menarche, the reproductive period, perimenopause, and postmenopausal bleeding.
By PALM-COEIN classification, abnormal uterine bleeding can have structural etiologies (polyp, adenomyosis, leiomyoma, malignancy, and hyperplasia) or nonstructural etiologies (coagulopathy, ovulatory dysfunction, endometrial, iatrogenic, and not-classified) [1].
Diagnosing abnormal uterine bleeding typically involves a combination of medical history, physical examination, and diagnostic tests, including laboratory and imaging tests, as well as an endometrial biopsy [2, 3].
The specific tests depend on the patient's symptoms and medical history. The post-and pre-menopausal period requires a detailed investigation to establish the aetiology of the bleeding because in this period the chances that the woman has a malignancy are great [4].
Once a diagnosis has been made, the treatment plan is determined based on the underlying cause of the bleeding.
Aim
The main objective of this paper was to determine the prevalent cases of endometrial carcinoma in different periods, focusing on the postmenopausal period.
Materials and Methods
This investigation was a prospective cross-sectional study.
The study was conducted in patients with abnormal uterine bleeding from the uterus, of different ages, with an interval of 25-85 years, admitted to the Department of Gynaecology of a tertiary public service institution.
Sample Size
The study included 79 cases of abnormal uterine bleeding, in different periods of women's lives.
The sampling technique was consecutive. Women who underwent dilatation and curettage (D&C) for endometrial sampling with complaints of AUB were included in the study by obtaining histopathological samples.
Age, duration of abnormal uterine bleeding, and observed histopathological spectrum were recorded.
Patients with systemic disease/cause of bleeding such as low platelet count or miscarriage were excluded from the study.
Cases were stratified into reproductive, peri-menopausal, and post-menopausal age groups.
Reproductive age was considered from the age of puberty to the perimenopausal age (approximately 12 to 39 years).
Perimenopausal age was around menopause and was different for every woman (roughly 40-50 years old).
The postmenopausal age group was defined as the permanent cessation of menstruation, confirmed after 12 consecutive months of amenorrhea (median age 50 years and above).
Specimens were immediately fixed in 10% formalin, appropriately labelled for patient name, sex, age, and type of procedure/specimen, and transferred to the histopathology laboratory.
Tissue processing was performed and slides were stained with haematoxylin and eosin under strict quality assurance.
Microscopic evaluation was done by two experienced consultant histopathologists more than 5 years after the study, blinded to the study objectives.
Each specimen was independently evaluated by two consultant histopathologists.
Materials and the route followed
This study was conducted over a period of 10 months, from December 2021 to September 2022, in a public tertiary service institution using the purposive sampling method.
After adequate information about the purpose, methodology, and benefits of the study, the patient agreed to participate in the study and informed consent was obtained from them.
They were also assured of confidentiality and autonomy.
Socio-demographic data including age, educational level, and economic status were collected.
Identification of patient risk factors such as weight, height, BMI, presence of comorbidities, smoking history, and treatment received, and period of diagnosis were also analysed.
Data were entered into SPSS version 21.
Results were presented as mean±SD for age, frequencies and percentages were calculated for descriptive variables, i.e. normal menstrual pattern, hormonal imbalance pattern, endometrial polyp, chronic endometritis, atrophic endometrium, endometrial hyperplasia, and endometrial carcinoma.
Stratification of age and duration of abnormal uterine bleeding was done to control for confounding factors.
A written informed consent was obtained from all the patients, as well as the approval of the Local Ethics Committee. Anonymity and confidentiality of women's data were ensured.
Results
Out of a total of 79 cases with irregular uterine bleeding; 56.9% (45 cases) of the women were in the perimenopausal period, 32.9% were in the postmenopausal period, while 10.2% were in the reproductive period (Figure 1).
Figure 1.
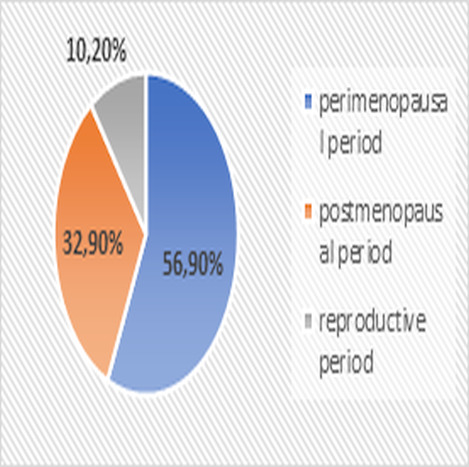
The percentage of abnormal uterine bleeding, according to the periods.
The average age of women with irregular uterine bleeding in the postmenopausal period was 62.03 years, in the perimenopausal period 47.5 years, and in the reproductive period it was 33.3 years. 46.8% of women with irregular uterine bleeding were smokers, while 53.2% were non-smokers (Table 1).
Table 1.
Socio-demographic data
|
Socio-demographic data |
Postmenopausal bleeding |
Perimenopausal bleeding |
Reproductive ages uterine bleeding |
Total |
|
The average ages of women |
62.03 years |
47.5 years |
33.3 years |
|
|
Smoking YES NO |
5 cases 21 cases |
25 cases 20 cases |
7 cases 1 case |
37 cases or 46.8% 42 cases or 53.2% Total 79 cases 100% |
|
Educational level High Secondary Lower |
6 cases 15 cases 5 cases |
18 cases 20 cases 7 cases |
3 cases 4 cases 1 case |
27 cases 34.2% 39 cases 49.4% 13 cases 16.4% Total 79 cases 100% |
|
Economic status High Middle Low |
2 cases 13 cases 11 cases |
5 cases 19 cases 21 cases |
2 cases 3 cases 3 cases |
9 cases 11.4% 35 cases 44.3% 35 cases 44.3% Total 79 cases 100% |
In 79 cases with irregular uterine bleeding in different lifestyles, exploratory curettage and histopathological analysis were performed, resulting in 67 cases (84.8%) of abnormal uterine bleeding due to benign causes such as endometrial hyperplasia simplex, endometrial polyp, endometrial atrophy, submucous fibroids, etc.
Meanwhile, 12 cases (15.2%) of abnormal uterine bleeding were due to malignant causes such as endometrial adenocarcinoma (Figure 2).
Figure 2.
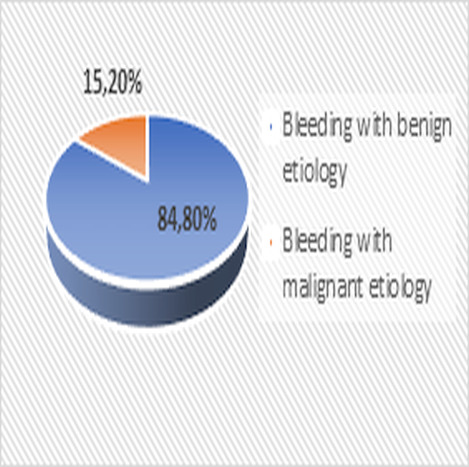
The percentage of abnormal uterine bleeding, according to the etiology
Out of a total of 12 cases with malignant pathology, 10 cases (83.3%) were women with abnormal uterine bleeding in the postmenopausal period, while 2 cases (16.7%) were women with irregular bleeding in the perimenopausal period.
All women with abnormal uterine bleeding in the reproductive period had benign causes such as endometrial polyp, ovulatory dysfunction, etc. (Figure 3).
Figure 3.
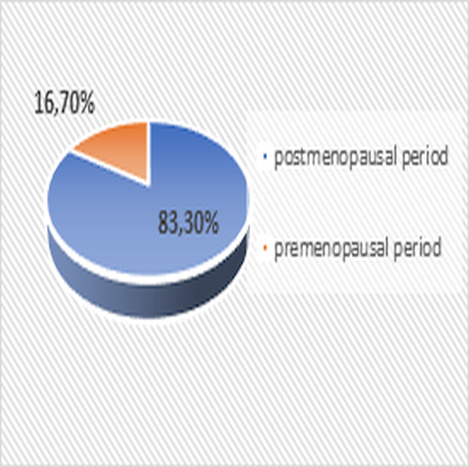
Distribution of cases with malignant pathology according to periods
The average age of women with malignant pathology was 66.7 years, while the average postmenopausal period was 17.3 years.
The average age of menopause onset was 49.4 years.
Out of 12 cases with malignant pathology, 6 cases (50%) had Class I obesity with an average BMI of 31.63kg/m2, 3 cases (25%) were overweight with an average BMI of 28.0kg/m2, and 3 cases had normal weight with an average BMI of 23.3kg/m2.
All women with abnormal uterine bleeding due to malignant causes had co-morbidities and used daily medication therapy, with the most common co-morbidities being: arterial hypertension, Class I obesity, type II diabetes mellitus, chronic anaemia, etc. (Table 2).
Table 2.
Distribution in percentages of co-morbidities
|
Co-morbidities |
Cases (percentage) |
|
Arterial Hypertension |
12/12 (100%) |
|
Class 1 Obesity |
6/12 (50%) |
|
Type 2 diabetes mellitus |
5/12 (41.6%) |
|
Anaemia chronic disease |
4/12 (33.3%) |
|
Overweight |
3/12 (25%) |
Discussions
Abnormal uterine bleeding can occur at any stage of a woman’s life, and depending on when it happens; it can have different causes and treatments.
Our study found that abnormal uterine bleeding occurs more frequently during the premenopausal period (56.9%), and the causes of irregular bleeding during this period are mainly benign, similar to the results of a study by Berndt-Johan Procopè [5].
Although less frequent, the most common cause of abnormal bleeding during the postmenopausal period is malignancy.
Due to the malignancy-related causes of irregular uterine bleeding that occur in the postmenopausal period of a woman, our study focused on this period, where we found that 32.9% of irregular uterine bleeding occurs during this period, and the main causes were malignant pathologies (83.3%), mainly endometrial adenocarcinoma.
With an average age of 66.7 years, the same results were found in a large number of studies on the malignant causes of abnormal uterine bleeding in the postmenopausal period [6, 7, 8, 9].
The diagnosis of the cause of abnormal uterine bleeding was made in our study using exploratory curettage and histopathological analysis for the postmenopausal, perimenopausal, and reproductive periods, while the adolescence period was excluded from this diagnostic plan, respecting the age-specific characteristics, as was done in many other studies [10, 11, 12, 13].
In our study, the average age of women entering menopause was 49.4 years, which was found to be similar to the average age of menopause in the world, which is between 47.5 and 51.4 years [14].
During the study, it was observed that 50% of women with abnormal uterine bleeding due to malignancy were classified as overweight, 25% were obese, and 25% had normal weight.
It was confirmed that obesity is a co-factor of malignancy in the postmenopausal period, and the pathophysiological mechanism is well understood now these findings are also described in many other studies [15, 16, 17].
Additionally, our study also found a high number of co-morbidities among women with abnormal uterine bleeding due to malignancy, such as hypertension, class I hypertension, class I obesity, type II diabetes mellitus, chronic anemia, and overweight, which is also confirmed by Yang X et al. study [18].
Conclusions
We came to the conclusion that any abnormal uterine bleeding should be initially investigated in a multidisciplinary manner, the accurate diagnosis should be determined, and then a treatment plan should be established.
The treatment strategy should be determined depending on the cause of abnormal bleeding.
In any abnormal uterine bleeding in the premenopausal period, especially in the postmenopausal period, it is cost-effective to perform an exploratory curettage and confirm the histopathological diagnosis first, and then determine the treatment strategy.
Since the role of metabolic syndrome in endometrial cancer is well known, all women in the pre and postmenopausal periods are recommended to have regular physical activity, reduce stress, maintain a normal weight, and properly manage hypertension, diabetes mellitus, anaemia, and hyperlipidaemia.
Conflict of interests
None to declare
References
- 1.Munro MG, Critchley HO, Broder MS, Fraser IS, FIGO Working. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. International Journal of Gynecology & Obstetrics. 2011;113(1):3–13. doi: 10.1016/j.ijgo.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Albers J, Hull SK, Wesley RM. Abnormal uterine bleeding. American family physician. 2004;69(8):1915–1926. [PubMed] [Google Scholar]
- 3.Van Dongen, De Kroon, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology. 2007;114(6):664–675. doi: 10.1111/j.1471-0528.2007.01326.x. [DOI] [PubMed] [Google Scholar]
- 4.Cooper NA, Barton PM, Breijer M, Caffrey O, Opmeer BC, Timmermans A, Mol BW, Khan KS, Clark TJ. Cost-effectiveness of diagnostic strategies for the management of abnormal uterine bleeding (heavy menstrual bleeding and post-menopausal bleeding): a decision analysis. Health technology assessment. 2014;18(24):1–201. doi: 10.3310/hta18240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Procopé BJ. Aetiology of postmenopausal bleeding. Acta Obstetricia et Gynecologica Scandinavica. 1971;50(4):311–313. doi: 10.3109/00016347109157330. [DOI] [PubMed] [Google Scholar]
- 6.Gredmark T, Kvint S, Havel G, Mattsson LÅ. Histopathological findings in women with postmenopausal bleeding. BJOG: An International Journal of Obstetrics &Gynaecology. 1995;102(2):133–136. doi: 10.1111/j.1471-0528.1995.tb09066.x. [DOI] [PubMed] [Google Scholar]
- 7.Astrup K, Olivarius ND. Frequency of spontaneously occurring postmenopausal bleeding in the general population. Acta Obstetrician et Gynecologica Scandinavica. 2004;83(2):203–207. doi: 10.1111/j.0001-6349.2004.00400.x. [DOI] [PubMed] [Google Scholar]
- 8.Opmeer BC, Van Doorn, Heintz AP, Burger CW, Bossuyt PM, Mol BW. Improving the existing diagnostic strategy by accounting for characteristics of the women in the diagnostic work up for postmenopausal bleeding. BJOG: An International Journal of Obstetrics & Gynaecology. 2007;114(1):51–58. doi: 10.1111/j.1471-0528.2006.01168.x. [DOI] [PubMed] [Google Scholar]
- 9.Keirse MJ. Aetiology of postmenopausal bleeding. Postgraduate medical journal. 1973;49(571):344–348. doi: 10.1136/pgmj.49.571.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Postmenopausal bleeding. 2022 Available from: https://www.ncbi.nlm.nih.gov/books/NBK562188/
- 11.Wouk N, Helton M. Abnormal uterine bleeding in premenopausal women. American family physician. 2019;99(7):435–443. [PubMed] [Google Scholar]
- 12.Kaunitz AM. Abnormal uterine bleeding in reproductive-age women. Jama. 2019;321(21):2126–2127. doi: 10.1001/jama.2019.5248. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez A, Dietrich JE. Abnormal uterine bleeding in the adolescent. Obstetrics & Gynecology. 2020;135(3):615–621. doi: 10.1097/AOG.0000000000003693. [DOI] [PubMed] [Google Scholar]
- 14.Sharman Moser, Chodick G, Bar-On S, Shalev V. Healthcare utilization and prevalence of symptoms in women with menopause: a real-world analysis. International Journal of Women's Health. 2020;12:445–454. doi: 10.2147/IJWH.S246113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacKintosh ML, Derbyshire AE, McVey RJ, Bolton J, Nickkho‐Amiry M, Higgins CL, Kamieniorz M, Pemberton PW, Kirmani BH, Ahmed B, Syed AA. The impact of obesity and bariatric surgery on circulating and tissue biomarkers of endometrial cancer risk. International journal of cancer. 2019;144(3):641–650. doi: 10.1002/ijc.31913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kokts‐Porietis RL, Elmrayed S, Brenner DR, Friedenreich CM. Obesity and mortality among endometrial cancer survivors: a systematic review and meta‐analysis. Obesity Reviews. 2021;22(12):e13337–e13337. doi: 10.1111/obr.13337. [DOI] [PubMed] [Google Scholar]
- 17.Smrz SA, Calo C, Fisher JL, Salani R. An ecological evaluation of the increasing incidence of endometrial cancer and the obesity epidemic. American Journal of Obstetrics and Gynecology. 2021;224(5):506–e1. doi: 10.1016/j.ajog.2020.10.042. [DOI] [PubMed] [Google Scholar]
- 18.Yang X, Wang J. The role of metabolic syndrome in endometrial cancer: a review. Frontiers in oncology. 2019;9:744–744. doi: 10.3389/fonc.2019.00744. [DOI] [PMC free article] [PubMed] [Google Scholar]


