Abstract
In this paper, a comparative statistical analysis of some performance indicators from the health system at SCJU Craiova and SJU Slatina is made in the period 2010-2021. Also, the correlations between the average duration of hospitalization, the bed utilization rate, the number of cases and the case complexity index for each hospital are studied. It is found that there are similarities, but also statistically significant differences between the two analyzed hospitals. Thus, it turns out that there are no significant differences between the bed utilization rate and the complexity index between the two hospitals, but there are statistically significant differences at a significance threshold of 5% between the average duration of hospitalization and the number of cases registered at the two hospitals analyzed. Moreover, the case complexity index is strongly negatively correlated with the bed utilization rate and with the number of cases in both hospitals, but positively correlated with the average duration of hospitalization at SCJU Craiova and weakly negatively correlated at SJU Slatina.
Keywords: Performance indicators , health system , comparative statistical analysis , health management
Introduction
Studying performance indicators is essential to evaluate the efficiency and quality of medical services provided by the health system. Performance indicators allow monitoring the performance and improving the quality of medical services provided by the health system, in order to ensure a high level of patient care. The study of performance indicators helps to identify problems, improve processes and services and make decisions to improve the quality of medical services. It can also help to compare the performance of the health system with other countries and to identify good practices that can be applied in one's own health system. These indicators are also useful in health management to evaluate the efficiency of managerial activities, as well as decisions and policies adopted in the health system. By studying performance indicators, the performance of managers and staff in the health system can be monitored and evaluated and they can be used to improve the performance and quality of medical services, especially in terms of efficient use of resources, cost reduction, improvement of satisfaction patients and increasing the accessibility of medical services.
The novelty of our research consists in this comparative analysis of two similar medical units, both being the top medical facilities in their areas, using statistical methods, as well as in the interpretation of the results, the identification of the causes of the differences between the indicators, but also in the proposed measures that can lead to the improvement of the medical services offered to patients.
In order to carry out a comparative statistical analysis of some performance indicators in the health system, we went through several stages. The first stage was the identification of the performance indicators used in the healthcare environment, by studying the specialized literature [1, 2, 3, 4, 5]. There are several performance indicators in the health system, in this work we will study four of them, namely: the average duration of hospitalization (DMS), the bed utilization rate (RUP), the number of cases in a calendar year (NC) and the case complexity index (ICM). The statistical study analyzes the indicators for the period 2010-2021 at two county emergency hospitals in the Oltenia region, namely SCJU Craiova and SJU Slatina.
Key performance indicators in the health system are used to measure managerial performance, but also the quality of medical services within a health organization (see, for example [1, 2, 3, 5]). Healthcare management is a complex and demanding activity that requires leadership and resource management skills, as well as a deep knowledge of healthcare systems and healthcare regulations. Effective health management can contribute to improving the health and quality of life of patients, as well as increasing the efficiency and sustainability of health systems.
Asbroek et al. [6] studied performance indicators for the Dutch health system. They used the Lalonde population health model combined with a balanced scoreboard model. The constructed model makes evident the relationship between population health and health system management and facilitates the presentation of performance information from various perspectives. There are a total of 20 indicators selected for information on health system management. The merit of linking the balanced scorecard-inspired model to public health data is that it facilitates visualization of the health system's contribution to improving population health.
In their work, the authors Barliba, Nestian and Tiță [4] proposed and validated a hospital performance management model through the prism of seven key performance indicators, using a sample of five county emergency hospitals. Among the performance indicators are the degree of occupancy of hospital beds, the average duration of hospitalization and the index of complexity of cases, which are also indicators used in our work. Finally, the article highlights some conclusions regarding the strengths and weaknesses of the model, resulting from testing the relevance of key performance indicators.
Birsan [7] makes a presentation of the criteria according to which the performance indicators of the health system in Romania should be selected. At the end, choose a set of 5 indicators, which includes the indicators used in our work, for a hospital with 274 beds, between 2015-2019 and do an empirical analysis, without using statistical methods.
Burlea-Schiopoiu and Ferhati [8] identified a set of key performance indicators in the health system with the aim of providing health managers with recommendations for evaluating, monitoring and controlling the critical factors that influence the performance of the health sector during a crisis of pandemic.
The work of Cicea and Busu [9] analyzes the main indicators that characterize the health system in Romania, in order to identify its potential strengths and weaknesses, focusing on financial indicators. Also, the evolution of the number of medical personnel per 10,000 inhabitants between 1994 and 2007 in Romania is presented. A comparison is made between the number of doctors and dentists per 10,000 inhabitants, the number of beds per 1,000 inhabitants and the average duration of hospitalization in 2007, in different countries.
A paper by Freeman [10] provides a systematic review of the empirical and theoretical writings on the use of performance indicators in the United Kingdom. The paper highlights potential issues and investigates how best to obtain, implement and use performance indicator data, presenting the results thematically.
The second stage consisted in the collection of relevant data for each performance indicator, from the two hospitals. The two stages were closely correlated, the analyzed indicators being dependent on the availability of statistical data made available by the health units studied. The third stage consisted of the data analysis carried out by means of statistical methods, such as the t-test, the F-test, the variance analysis and the correlation analysis. These statistical methods were also used to compare the differences between the data groups and to identify the relationships between the analyzed variables. The fourth stage meant the interpretation of the data, identifying the significant differences between SCJU Craiova and SJU Slatina, as well as the presentation of the results of the comparative statistical analysis.
Finally, we proposed some measures that could lead to the improvement of the operational health management at the two public units by managing the daily operations of the medical institutions, including scheduling patients, managing medical records, supplying medical equipment and supplies and improving operational processes. Effective health management can contribute to improving the health and quality of life of patients, as well as increasing the efficiency and sustainability of health systems.
The main purpose of this work is to study from a statistical point of view certain performance indicators in the health system, having SCJU Craiova and SJU Slatina as case studies. We want to do a comparative statistical study of the performance indicators between the two health units, to find out what are the differences and similarities between them, to identify the causes of the differences and to propose certain measures that can lead to the improvement of health management and, implicitly, of the performance and quality of medical services.
Research methodology
The comparative statistical analysis was made by using the results obtained between 2010-2021 at SCJU Craiova, Dolj county and SJU Slatina in Olt county. To check whether the statistical series follow a normal distribution or not, the Jarque-Bera test was used. To verify the significance of the difference between the variances, the F-test was used, and to determine whether or not the means differed statistically significantly at a chosen significance level of 5%, the t-Student test was used (see [11, 12]).
The Jarque-Bera test is a statistical test for verifying the normality hypothesis of a distribution and is based on measuring the skewness S and kurtosis K of a distribution. The tested variable is given by the following relationship
which follows a distribution law χ-square, where n is the number of degrees of freedom. The null hypothesis of the Jarque-Bera test is H0: the data are normally distributed and the alternative hypothesis is H1: the data are not normally distributed. If
, (chi-square distribution with two degrees of freedom), then, at the significance threshold α, H0 is accepted, this hypothesis being equivalent to the fact that the probability attached to the Jarque-Bera test is higher than the chosen significance threshold α=0.05.
In order to verify the equality or statistical difference between the dispersions for two volume samples n1 and n2 from different communities with the estimated dispersions s_1^2 and s_2^2 the variable F_c=(s_1^2)/(s_2^2 ) is calculated, which follows a Fisher distribution with n1-1 respectively n2-1 degrees of freedom. Thus, for a chosen significance threshold α=0.05 the null hypothesis H0: s_1^2= s_2^2 is checked, against the alternative hypothesis H1: s_1^2≠ s_2^2. In case Fc<Fcritical, which is equivalent to the fact that the probability attached to the F test is greater than the significance threshold α=0.05, then the null hypothesis is accepted, otherwise the null hypothesis is rejected and the alternative hypothesis is accepted.
Verification of the hypothesis of equality of the means of two samples from two different communities, denoted H0: m1=m2, against the alternative hypothesis H1: m_1≠m_2, is done by applying the t-Student test, depending on the equality or significant difference of the dispersions. If the dispersions do not differ significantly, we can consider that s_1^2= s_2^2, and then the variable s2 is calculated
and the random variable
which follows a t-Student distribution with n1+n2-2 degrees of freedom. If |tc|<tcritical, which is equivalent to the fact that the probability attached to the t-Student test is higher than the chosen significance threshold α=0.05, then the null hypothesis H0 is accepted, and otherwise it is rejected.
If the dispersions differ significantly, then considering s_1^2≠ s_2^2, the random variable
is calculated, which follows a t-Student distribution, with a certain number of degrees of freedom (see [12]). If |tc|<tcritical, (which is equivalent to the fact that the probability attached to the t-Student test is higher than the chosen significance threshold α=0.05) then the null hypothesis H0 is accepted and otherwise it is rejected.
The correlation matrix is a measure of the linear relationship between variables. The values in the matrix represent the correlation coefficients between pairs of variables. Correlations are measured between -1 and 1 and show the strength and direction of the relationship between two variables. A value of 1 indicates a perfect positive correlation, that is, when one variable increases, the other also increases, while a value of -1 indicates a perfect negative correlation, that is, when one variable increases, the other decreases. A value of 0 indicates an absence of correlation.
Results
The research consisted in the identification of performance indicators, data collection (Tables 1 and 2), comparative statistical analysis and interpretation of the results.
Table 1.
Performance indicators at SCJU Craiova
|
Years |
DMS |
RUP |
ICM |
NC |
|
2010 |
5.78 ± 0.22 |
78.35% ± 3.48% |
1.0741 ± 0.07 |
65289 |
|
2011 |
5.68 ± 0.34 |
76.88% ± 5.08% |
1.1267 ± 0.08 |
65191 |
|
2012 |
5.87 ± 0.18 |
75.00% ± 4.40% |
1.1618 ± 0.01 |
64995 |
|
2013 |
5.91 ± 0.15 |
75.00% ± 4.50% |
1.1587 ± 0.03 |
67913 |
|
2014 |
6.01 ± 0.20 |
73.00% ± 3.57% |
1.2015 ± 0.01 |
65717 |
|
2015 |
5.92 ± 0.18 |
71.00% ± 5.04% |
1.1967 ± 0.04 |
64654 |
|
2016 |
5.92 ± 0.19 |
69.00% ± 5.79% |
1.1779 ± 0.02 |
61793 |
|
2017 |
5.85 ± 0.18 |
61.23% ± 5.93% |
1.1958 ± 0.03 |
54478 |
|
2018 |
5.76 ± 0.13 |
60.78% ± 4.29% |
1.1907 ± 0.04 |
55345 |
|
2019 |
5.92 ± 0.08 |
60.30% ± 2.01% |
1.2826 ± 0.05 |
54183 |
|
2020 |
5.98 ± 0.18 |
37.66% ± 13.01% |
1.3154 ± 0.04 |
32191 |
|
2021 |
5.90 ± 0.32 |
37.11% ± 2.46% |
1.3483 ± 0.05 |
33009 |
Table 2.
Performance indicators at SJU Slatina
|
Years |
DMS |
RUP |
ICM |
NC |
|
2010 |
6.42 ± 0.12 |
91.23% ± 2.12% |
1.0745 ± 0.02 |
54863 |
|
2011 |
6.42 ± 0.09 |
85.00% ± 5.22% |
1.0875 ± 0.01 |
51273 |
|
2012 |
7.47 ± 0.08 |
97.27% ± 5.21% |
1.1044 ± 0.02 |
50409 |
|
2013 |
7.84 ± 0.62 |
89.50% ± 3.29% |
1.1375 ± 0.00 |
47612 |
|
2014 |
7.66 ± 0.07 |
80.52% ± 4.55% |
1.1153 ± 0.02 |
43986 |
|
2015 |
7.63 ± 0.07 |
78.44% ± 4.97% |
1.1162 ± 0.00 |
42899 |
|
2016 |
7.80 ± 0.14 |
77.26% ± 1.78% |
1.2452 ± 0.02 |
41338 |
|
2017 |
7.70 ± 0.04 |
76.53% ± 3.87% |
1.3166 ± 0.02 |
41441 |
|
2018 |
7.64 ± 0.04 |
78.10% ± 3.12% |
1.3775 ± 0.01 |
41887 |
|
2019 |
6.97 ± 0.13 |
70.10% ± 5.07% |
1.4174 ± 0.01 |
40557 |
|
2020 |
6.90 ± 0.11 |
45.70% ± 4.34% |
1.4340 ± 0.01 |
25995 |
|
2021 |
6.32 ± 0.11 |
43.20% ± 0.44% |
1.5119 ± 0.01 |
24428 |
The statistical analysis of four performance indicators from the health system from 2010-2021 was carried out by calculating some statistical indicators such as the mean, dispersion, standard deviation and coefficient of variation (Tables 3 and 4). After applying the Jarque-Bera statistical test it was found (see Tables 5 and 6) that all data series follow a normal distribution and consequently, we can apply the t-Student test to check the difference between the means for these statistical series.
Table 3.
Descriptive statistics of the performance indicators at SCJU Craiova
|
Mean |
Standard Error |
Median |
Standard Deviation |
Coefficient of variation |
Sample Variance |
Minimum |
Maximum |
|
|
DMS |
5.8750 |
0.0272 |
5.9050 |
0.0944 |
1.60% |
0.0089 |
5.6800 |
6.0100 |
|
RUP |
0.6460 |
0.0409 |
0.7 |
0.1418 |
21.95% |
0.0201 |
0.3711 |
0.7835 |
|
NC |
57063.16 |
3572.19 |
63223.5 |
12374.45 |
21.68% |
153127084.5 |
32191 |
67913 |
|
ICM |
1.2025 |
0.0225 |
1.1932 |
0.0780 |
6.48% |
0.0060 |
1.0741 |
1.3483 |
Table 4.
Descriptive statistics of the performance indicators at SCJU Slatina
|
Mean |
Standard Error |
Median |
Standard Deviation |
Coefficient of variation |
Sample Variance |
Minimum |
Maximum |
|
|
DMS |
7.2308 |
0.1697 |
7.55 |
0.5881 |
8.13% |
0.3459 |
6.32 |
7.84 |
|
RUP |
0.7610 |
0.0478 |
0.7827 |
0.1656 |
21.76% |
0.0274 |
0.432 |
0.9727 |
|
NC |
42224 |
2648.01 |
42393 |
9172.9957 |
21.72% |
84143850.9 |
24428 |
54863 |
|
ICM |
1.2448 |
0.04588 |
1.1913 |
0.1589 |
12.76% |
0.0252 |
1.0745 |
1.5119 |
Table 5.
Jarque-Bera test for indicators at SCJU Craiova
|
|
Jarque-Bera test |
Probability |
Skewness |
Kurtosis |
Conclusion |
|
DMS |
0.915739 |
0.632630 |
-0.660557 |
2.706516 |
normal distribution |
|
RUP |
2.403731 |
0.300633 |
-1.095424 |
2.912564 |
normal distribution |
|
NC |
3.229577 |
0.198933 |
-1.267256 |
3.188165 |
normal distribution |
|
ICM |
0.519290 |
0.771325 |
0.464505 |
2.581046 |
normal distribution |
Table 6.
Jarque-Bera test for indicators at SCJU Slatina
|
|
Jarque-Bera test |
Probability |
Skewness |
Kurtosis |
Conclusion |
|
DMS |
1.519818 |
0.467709 |
-0.530710 |
1.616879 |
normal distribution |
|
RUP |
1.988848 |
0.369936 |
-0.996654 |
3.066496 |
normal distribution |
|
NC |
1.262205 |
0.532005 |
-0.792933 |
2.902844 |
normal distribution |
|
ICM |
1.324404 |
0.515715 |
0.390397 |
1.572005 |
normal distribution |
The next step consisted in checking the difference in dispersions, using the F test, between the data series from SCJU Craiova and SJU Slatina, with a view to the subsequent application of the corresponding t-Student test. The results obtained were grouped in Table 7 and it is found that there are no significant differences between the variances of bed utilization rate and the number of cases in a calendar year from a statistical point of view at a significance threshold of 5%, between the two hospitals, but we have a significant difference between the variances obtained for the average duration of hospitalization and the complexity index of the cases between the two health units analyzed. These results are important, allowing us to choose the appropraite sttistical test, in order to analyze the significant differences between means.
Table 7.
Variances’ comparison of performance indicators between SCJU Craiova and SJU Slatina
|
|
Calculated value of F-test/probability associated with the F-test |
The theoretical value of the F-test |
Conclusions |
|
DMS |
Fc=38.78992525 P=3.47509E-07 |
2.81793047 |
The null hypothesis H0 is rejected. The alternative hypothesis H1 is accepted. There is a significant difference between variances. |
|
RUP |
Fc=1.363327526 P=0.308027852 |
2.81793047 |
The null hypothesis H0 is accepted. There is no significant difference between variances. |
|
NC |
Fc=1.819825012 P=0.167603519 |
2.81793047 |
The null hypothesis H0 is accepted. There is no significant difference between variances |
|
ICM |
Fc=4.145695709 P=0.013211429 |
2.81793047 |
The null hypothesis H0 is rejected. The alternative hypothesis H1 is accepted. There is a significant difference between variances. |
Thus, there is a significant difference between the average duration of hospitalization and the annual number of cases between SCJU Craiova and SJU Slatina, and there are no significant differences between the means for the bed utilization rate and the case mix index (Table 8).
Table 8.
Variances’ comparison of performance indicators between SCJU Craiova and SJU Slatina
|
|
Calculated value of t-test/probability associated with the t-test |
The theoretical value of the t-test |
Equal/Unequal Variances |
Conclusions |
|
DMS |
tc= 7.884464592 P= 4.36233E-06 |
2.17881283 |
Unequal variances |
The null hypothesis H0 is rejected. The alternative hypothesis H1 is accepted. There is a significant difference between means. |
|
RUP |
tc= 1.826723592 P= 0.081341953 |
2.073873068 |
Equal variances |
The null hypothesis H0 is accepted. There is no significant difference between means |
|
NC |
tc= 3.337166417 P= 0.00298648 |
2.073873068 |
Equal variances |
The null hypothesis H0 is rejected. The alternative hypothesis H1 is accepted. There is a significant difference between means. |
|
ICM |
tc= 0.827700768 P= 0.420014645 |
2.119905299 |
Unequal variances |
The null hypothesis H0 is accepted. There is no significant difference between means |
Average duration of hospitalization
Average duration of hospitalization is a measure of the average time patients spend in hospital during a given period of time. This measure is calculated by dividing the total number of hospital days of all patients in a given time period by the total number of hospitalized patients in the same time period.
Average duration of hospital stay is an important measure for evaluating the efficiency of hospital services and can be used to identify trends or anomalies in patients' hospital stays. A duration of stay that is too long may indicate a need to improve workflows within the hospital and provide better patient management, while a duration that is too short may indicate problems with planning or assessing patients' condition.
For the average duration of hospitalization at SCJU Craiova, an average of 5,875 days was calculated in the analyzed period. The maximum value of 6.01 was recorded in 2014, and the minimum of 5.68 was achieved in 2011. It is found that the average duration of hospitalization at SCJU Craiova in the period 2010-2021 tends towards a normal distribution according to the Jarque-Bera test with a value of 0.916 and attached probability p=0.632 (Skewness=-0.661; Kurtosis=2.706). The coefficient of variation, calculated as the ratio between the standard deviation and the average, has a value of 1.6%, which is far below the value of 35%, which leads to the conclusion of a homogeneous series for the average duration of hospitalization, the mean being very significant. Regarding the dynamics of the average duration of hospitalization, it can be seen from Figure 1 that it follows a linear trend, relatively constant, with small variations around the mean, the standard deviation having a very small value of 0.0944.
Figure 1.
Average duration of hospitalization at SCJU Craiova and SJU Slatina
Analyzing the average duration of hospitalization at SJU Slatina, an mean of 7.23 days was found in the period 2010-2021, with a maximum of 7.84 achieved in 2013 and a minimum of 6.32 recorded in 2021. According to the Jarque-Bera test with a value of 1.519 and probability attached p=0.467, the average duration of hospitalization follows a normal distribution (Skewness=-0.531; Kurtosis=1.617). The coefficient of variation has a value of 8.13%, which means that the mean is representative and the series is homogeneous. There is an increasing trend in the period 2010-2013, followed by a somewhat constant period with small variations until 2018 and a decreasing trend in the period 2018-2021.
Bed utilization rate
Hospital bed utilization rate is a measure of the degree to which beds are occupied in a given period of time. This is calculated by dividing the number of hospital days spent by all patients in a given time interval by the total number of beds available in the hospital in the same time interval. The bed utilization rate is an important measure for efficient hospital management, as it can help optimize resource utilization and identify potential problems related to overcrowding or underutilization of beds. It can also be used to assess the need to expand hospital capacity or redistribute resources within it.
Analyzing the data at SCJU Craiova, it is found that for the bed utilization rate, a mean of 0.646 was obtained, that is, 64.6% in the period 2010-2021, with a maximum value of 78.35% in 2010 and a minimum of only 37,11% in 2011, in the midst of the Coronavirus crisis. It also results that the data from the analyzed period follows a normal distribution, according to the Jarque-Bera test with a value of 2.403731 and the attached probability p=0.300633 (Skewness=-1.095424; Kurtosis=2.912564). The coefficient of variation has a value of 21.95%, which indicates a sufficiently homogeneous series, the mean being representative. Figure 2 shows a downward trend, accentuated in the last two years by the Coronavirus crisis, which imposed restrictions on hospital admissions. Regarding the bed utilization rate at SJU Slatina, a mean of 76.1% was calculated for the studied period, with a maximum value in 2012 of 97.27% and a minimum of 43.2% obtained in 2021, which is also due to the admission restrictions imposed by the Coronavirus. The statistical data follows a normal distribution, according to the Jarque-Bera test, which has a value of 1.988848 with probability p=0.369936 (Skewness=-0.996654; Kurtosis=3.066496). Regarding the coefficient of variation, it has a value of 21.76%, indicating a sufficiently homogeneous series with a representative mean. The trend is a decreasing one, similar to the one at SCJU Craiova, with an exception in 2012, when a maximum value was recorded.
Figure 2.
Bed utilization rate at SCJU Craiova and SJU Slatina
Number of Cases
The indicator representing the number of treated cases represents the total number of medical cases treated by the hospital in a calendar year. This may include inpatients, outpatient consultations, surgical procedures, imaging investigations and other types of medical care. This indicator can be used to assess the volume of medical services provided by a hospital and can be compared with other performance measures such as expenditure, efficiency and quality of medical care. In addition, this indicator can be used to identify trends or anomalies in cases treated over time, such as increases or decreases in the number of medical cases. It can also be used to assess the need for resources and help plan and allocate them within a health system.
The descriptive statistics show a mean of 57063.16 cases treated during the period studied at SCJU Craiova, with a maximum of 67913 in 2013 and a minimum value of 32191 cases in 2020, due to the restrictions imposed by the Coronavirus pandemic. The statistical series follows a normal distribution, resulting from the Jarque-Bera test with the value 3.229 with the attached probability p=0.199 (Skewness=-1.267; Kurtosis=3.188). By calculating the coefficient of variation with the value of 21.68%, it results that the series is sufficiently homogeneous and the mean is significant. It is also noted that the trend is a decreasing one, starting with 2013, amplified in the last two years analyzed by the Coronavirus crisis (see Figure 3).
Figure 3.
The number of cases treated at SCJU Craiova and SJU Slatina
Analyzing the number of cases treated in the period 2010-2021 at SJU Slatina, a mean of 42224 was found, with a maximum value of 54863 cases reached in 2010 and a minimum of only 24428 cases in 2021, observing a clear trend of their decrease over time, amplified in 2020-2021 by the restrictions on hospital treatment for other pathologies due to the Coronavirus pandemic. By applying the Jarque-Bera test with the value 1.262 with the attached probability p=0.532 (Skewness=-0.793; Kurtosis=2.903), a normal distribution of the statistical data results. The coefficient of variation has a value of 21.72%, indicating a sufficiently homogeneous series with a representative mean.
Case complexity index
The case complexity index or case mix index is a measure of the complexity and severity of the cases treated in a given set of medical or hospital services. It takes into account the severity level of patients, the type of conditions and comorbidities they are dealing with, and the medical interventions needed to treat them. The case mix index is used particularly in the health insurance industry to determine the level of funding required for health care providers. It is also used in research and analysis to assess the performance of health care systems and to identify needs and trends in patient care.
The case complexity index is calculated by dividing the total number of weighted cases by the total number of solved cases, finding a number that expresses the resources needed by the hospital in accordance with the patients treated. Weighted cases represent the "virtual" patients generated by adjusting the discharged cases according to the resources associated with each case type.
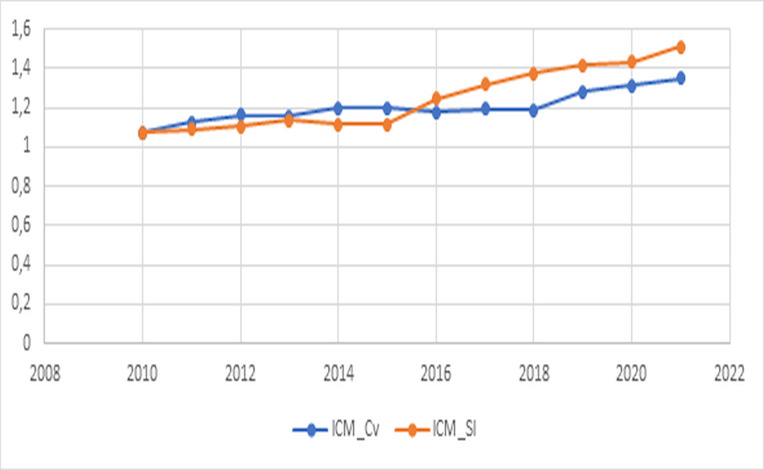
The case complexity index at SCJU Craiova has a mean of 1.202 in the analyzed period, having the maximum value of 1.3483 in 2021, while the minimum value of 1.074 was obtained in 2010, observing an increasing trend in the last four years studied (Figure 4). This trend may be associated with an increase in the complexity of cases treated in the medical unit. Also, the statistical data follows a normal distribution, a statement supported by the Jarque-Bera test with the value 0.519290 and the attached probability p=0.771 (Skewness=0.464; Kurtosis=2.581). The coefficient of variation has a value of 6.48%, which means that the series is homogeneous, the mean is representative and the standard deviation having a very small value of 0.078.
Figure 4.
Case complexity index at SCJU Craiova and SJU Slatina
For SJU Slatina, a mean of 1.2448 of the case complexity index was calculated, with a minimum of 1.0745 in 2010 and a maximum of 1.5119 in 2021, the trend being obviously an increasing one. And for this series, a normal distribution is found, by applying the Jarque-Bera test with the value 1.324404, having the attached probability p=0.516 (Skewness=0.390; Kurtosis=1.572). The coefficient of variation has a small value of 12.76%, the series is homogeneous and the mean is significant.
Correlations between indicators
The last step in our analysis was to find possible correlations between the performance indicators, for the two hospitals. For this, we computed the correlation matrices for the KPI recorded for both SCJU Craiova and SJU Slatina (Table 9 and Table 10) Only correlation coefficients greater than 0.3 were considered for a level of significance of 5%
Table 9.
Matrix of correlations between indicators at SCJU Craiova
|
|
DMS |
RUP |
NC |
ICM |
|
DMS |
1 |
|
|
|
|
RUP |
-0.33628 |
1 |
|
|
|
NC |
-0.26325 |
0.988925 |
1 |
|
|
ICM |
0.552075 |
-0.90756 |
-0.86076 |
1 |
|
|
|
|
|
|
Table 10.
Matrix of correlations between indicators at SJU Slatina
|
|
DMS |
RUP |
NC |
ICM |
|
DMS |
1 |
|
|
|
|
RUP |
0.368511 |
1 |
|
|
|
NC |
0.163168 |
0.967884 |
1 |
|
|
ICM |
-0.19729 |
-0.84972 |
-0.86227 |
1 |
Discussions
Comparative analysis of the main indicators of the health system’s performance
Comparing the average duration of hospitalization in the period 2010-2021 between SCJU Craiova and SJU Slatina, it is found that there are significant differences between means from a statistical point of view, according to the t-Student test, tc= 7.884 with the attached probability p=3.475 x 10-7, at a significance level of 5%. The mean at the SJU Slatina level is significantly higher than the one obtained at the SCJU Craiova, this is most likely explained by the pre-operative hospitalizations carried out at the SJU Slatina in order to carry out the necessary analyses.
Analyzing the rate of use of beds in the period 2010-2021 between SCJU Craiova and SJU Slatina, it is found that there are no significant differences between means from a statistical point of view, according to the t-Student test, at a significance level of 5% (tc= 1.827 with the attached probability p= 0.0813).
Comparing the number of cases treated in the period 2010-2021 at SCJU Craiova and SJU Slatina, it is found that there are significant differences between means from a statistical point of view, according to the t-Student test, tc=3.337 with the attached probability p=0.003, at a level of significance of 5%. The mean at SCJU Craiova is significantly higher than that obtained at SJU Slatina, this is due to the fact that in Craiova there are a number of 1518 continuous hospitalization beds, with a number of 31 wards (28 clinical and 3 non-clinical) and a number of 27 specialties, while in Slatina there are 1142 hospital beds.
Analyzing the complexity index of the cases treated in the period 2010-2021 between SCJU Craiova and SJU Slatina, it is found that there are no significant differences between means from a statistical point of view, according to the t-Student test, at a significance level of 5%, tc=0.828 with the attached probability p=0.420.
However, in reality, more serious and complex cases are sent from SJU Slatina to SCJU Craiova or to hospitals in Bucharest. The fact that the complexity index of the cases from SCJU Craiova has a lower value in the last analyzed years, can be explained by deficiencies in completing the observation sheets for more complex cases, in the sense of passing some lower codes.
Analysis of correlations between indicators
From the analysis of the results given in Table 9, which corresponds to the correlation matrix, it is found that there is a moderate positive correlation at SCJU Craiova, between the average duration of hospitalization and the case mix index, with a correlation coefficient of 0.552. This may suggest that this hospital with a higher case complexity index tends to have a longer average duration of stay.
There is a moderate negative correlation between the bed utilization rate and the average duration of hospitalization, with a correlation coefficient of-0.336. This result may indicate that SCJU Craiova, with a higher bed utilization rate, tends to have a shorter average duration of hospitalization. Also, the average duration of hospitalization and the number of cases in a year have a weak negative correlation, with a correlation coefficient of only-0.263.
It is found that we have a strong positive correlation between the bed utilization rate and the number of cases, with a correlation coefficient of 0.988, indicating that at SCJU Craiova, the treatment of a larger number of cases is directly related to a higher rate of bed use.
Also, there is a strong negative correlation between the case complexity index and the bed utilization rate, with a correlation coefficient of-0.908, this fact leading to the conclusion that the hospital with a higher case mix index tends to have a lower bed utilization rate. There is also a negative correlation between the number of cases and the case mix index, with a correlation coefficient of -0.861. This suggests that the hospital in Craiova with a higher case complexity index tends to treat a smaller number of cases. It is important to remember that, in general, correlation does not always imply a causal relationship between variables, but only an association between them.
Regarding the correlation analysis at SJU Slatina given in Table 10, it is found that the average duration of hospitalization has a very small negative correlation with the case mix index, having a correlation coefficient of only-0.197. Also, the average duration of hospital stay and the number of cases have a weak positive correlation, with a correlation coefficient of 0.163.
On the other hand, the bed utilization rate has a strong positive correlation with the number of cases in a year, having a correlation coefficient of 0.967. This indicates that at SJU Slatina, a higher bed utilization rate is closely related to treating a larger number of patients in a year.
The case mix index is negatively correlated with the bed utilization rate, having a correlation coefficient of -0.849. This fact leads to the conclusion that at SJU Slatina, a higher case mix index is closely related to a lower bed utilization rate. There is a negative correlation between the number of treated cases and the case complexity index, with a correlation coefficient of -0.862. This shows us that the hospital in Slatina with a higher case mix index tends to treat a smaller number of cases.
The average duration of hospitalization and the bed utilization rate have a moderate positive correlation, having a correlation coefficient of 0.368. This may suggest that at SJU Slatina, a longer average duration of hospitalization may result in a higher bed utilization rate. It is important to note that correlation coefficients only indicate a linear relationship between variables, and not direct causation. Other factors and unobserved variables may influence these relationships.
From the comparative analysis of the two correlation matrices between the performance indicators at the two hospitals, it is found that there are similarities, but also differences. Thus, at both hospitals, there are strong positive correlations between the number of cases and the bed utilization rate and high negative correlations between the complexity index of the cases and the bed utilization rate, respectively the number of cases. Also, the correlations between the average duration of hospitalization and the other three indicators are moderate, also having sign differences between the two subjects. The differences regarding the average duration of hospitalization can be explained by the fact that at SCJU Craiova the preoperative analyzes are mostly carried out in the outpatient setting.
Conclusions
It can be seen from what is presented in the paper, that the bed utilization rate and the number of treated cases had a downward evolution in both hospitals, this decrease being more accentuated during the pandemic due to the restrictions imposed on hospitalization. As regards the dynamics of the average duration of hospitalization, it registers a linear trend, relatively constant at SCJU Craiova, being significantly lower from a statistical point of view at a significance threshold of 5% compared to the average recorded at SJU Slatina. This can be explained by the fact that at SJU Slatina preoperative analyzes are carried out predominantly with hospitalized patients, and at SCJU Craiova these analyzes are mostly performed in the outpatient setting. Another interesting conclusion refers to the fact that there is no significant difference between the average case complexity indices at the two analyzed hospitals, although more complex cases are treated at SCJU Craiova, some cases also coming from SJU Slatina. This fact can be explained by some deficiency in completing the observation sheets for complex cases from SCJU Craiova, in the sense of passing some codes lower than the degree of complexity. Moreover, the case mix index is positively correlated, naturally, with the average duration of bed use at SCJU Craiova, while at SJU Slatina they are negatively correlated, resulting in the latter a certain anomaly with what is known from practice specialized.
In conclusion, we propose at SJU Slatina to decrease the average length of hospitalization by performing medical tests mostly in the outpatient setting and at SCJU Craiova, a careful completion of the observation sheets of complex cases. Thus, the comparative statistical analysis of some performance indicators in the health system proves to be an effective method to evaluate the performance of a medical institution and to identify opportunities to improve the medical services offered.
Regarding further developments, we propose to analyze several performance indicators from the health system, for several regional hospitals in Romania.
Conflict of interests
None to declare
References
- 1. Fuchs V . The Health Economy . London, UK : Harvard University Press ; 1986 . ; pp. 174 – 193 . [Google Scholar]
- 2.Leggat SG, Narine L, Lemieux-Charles L, Barnsley J. A Review of Organizational Performance Assessment in Health Care. Health Services Research Management. 1998;11(1):3–23. doi: 10.1177/095148489801100102. [DOI] [PubMed] [Google Scholar]
- 3. Parmenter D . Key performance indicators (KPI): developing, implementing, and using winning KPIs . Hoboken, New Jersey, USA : John Wiley & Sons ; 2010 . pp. 3 – 24 . [Google Scholar]
- 4.Barliba I, Nestian AS, Tiţă SM. Relevance of Key Performance Indicators in a Hospital Performance Management Model. Journal of Eastern Europe Research in Business & Economics. 2012;2012(674169)1):15–15. [Google Scholar]
- 5. Bergeron B . Performance Management in Healthcare: From Key Performance Indicators to Balanced Scorecard. Abingdon-on-Thames, UK: Taylor&Francis ; 2017 . pp. 41 – 55 . [Google Scholar]
- 6.Asbroek AHA, Arah OA, Geelhoed J, Custers T, Delnoij DM, Klazinga NS. Developing a national performance indicator framework for the Dutch health system. International Journal for Quality in Health Care. 2004;16(1):i65–i71. doi: 10.1093/intqhc/mzh020. [DOI] [PubMed] [Google Scholar]
- 7.Birsan O. Analysis of performance indicators in the health system. Romanian Statistical Review. 2020;5:217–225. [Google Scholar]
- 8.Burlea-Schiopoiu A, Ferhati K. The Managerial Implications of the Key Performance Indicators in Healthcare Sector: A Cluster Analysis. Healthcare (Basel) 2021;9(1):19–19. doi: 10.3390/healthcare9010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cicea C, Busu C. Indicators of healthcare system, an important element of SWOT systemic analysis in this area. Economia (Management Series) 2009;12(2):284–293. [Google Scholar]
- 10.Freeman T. Using performance indicators to improve health care quality in the public sector: a review of the literature. Health Services Management Research. 2002;15(2):126–137. doi: 10.1258/0951484021912897. [DOI] [PubMed] [Google Scholar]
- 11. Maddala GS . Introduction to Econometrics. Hoboken, New Jersey, USA: John Wiley & Sons; 2001 . pp. 21 – 32 . [Google Scholar]
- 12. Wooldridge J . Introductory Econometrics: A modern Approach. Nashville, Tennessee, USA: South-Western College Pub; 1999 . pp. 770 – 779 . [Google Scholar]