Abstract
Key Clinical Message
Actinomycosis is a rare cause of appendicitis with an incidence of 0.3–1 incident per year per 100,000 people. A significant preoperative diagnostic challenge exists and is usually diagnosed incidentally on histopathological examination.
Abstract
Appendicular actinomycosis, a rare, chronic granulomatous infection caused by actinomyces species, holds a significant preoperative diagnostic summons and is often diagnosed serendipitously during the regular histopathological examination. Herein, we present a case of a 36‐year‐old female who presented with features suggestive of acute appendicitis, underwent laparoscopic appendicectomy, and was diagnosed with appendicular actinomycosis from the histopathological examination.
Keywords: actinomyces, appendicitis, case report, Nepal
1. INTRODUCTION
Acute appendicitis is the most prevalent emergency medical condition in the world, characterized by an acute abdomen and necessitating prompt surgical procedures. 1 Among numerous etiological factors such as lymphoid hyperplasia, faecolith, pinworms, carcinoids, eosinophilia, and granuloma, actinomycosis continues to be a very uncommon agent for causing acute appendicitis. 1 , 2
Actinomycosis is a rare, multisystemic, chronic granulomatous disease caused by Actinomyces, a gram‐positive, filamentous, anaerobic bacteria. The commensal microbiota of the intestinal mucosa, oral cavity, and urogenital tract, known as actinomyces, frequently manifests as perforated appendicitis. 3 , 4 Preoperative diagnosis continues to be challenging considering the symptoms are nonspecific and the condition mimics other abdominal ailments such as intestinal tuberculosis, cancer, or inflammatory bowel disease. 5 , 6
On searching PubMed, with keywords (actinomycosis) AND (Nepal), actinomycosis affecting the esophagus, skin, gall bladder, and brain was reported, however, could not find the cases of appendicular actinomycosis reported from Nepal, so might be the first case to be reported from the country. Thus, this case report highlights actinomycosis of the appendix, the first case to be reported from Nepal, to aid the physician in understanding uncommon medical conditions, diagnosis, and management.
2. CASE PRESENTATION
A 36‐year‐old nonpregnant female with a known case of hypertension under medication presented to the emergency department with a complaint of acute abdominal pain, starting from the periumbilical region and shifting to the right iliac region, that was continuous, nonradiating, and not associated with nausea and vomiting. The patient also gave a history of fever, for which she self‐medicated with antipyretics, and also had a history of loss of appetite. She denied a change in bowel and bladder habits with no association with food intake. She denied any history of recent contraceptive use, previous bowel surgery, use of immunosuppressive medication, or any immunosuppressive/chronic medical condition. There was no significant personal, family, or allergic history.
On examination, her vital parameters revealed no deviation from normal findings. An abdominal examination was significant for tenderness and rebound tenderness in the McBurney point, along with positive Rovsing's signs. Routine baseline laboratory investigations were within normal limits except for an increase in the total leukocyte count (12,118 cells/mm3) and neutrophils (78%). Overall Alvarado's Score was found to be 8/10 which suggested surgical intervention. Also, ultrasonography of the abdomen and pelvis showed increased thickness and echogenicity of the ileo‐caecal valve lumen with the associated minimal hypoechoic collection as well as positive probe tenderness in the right iliac fossa. Additionally, contrast‐enhanced computed tomography of the abdomen and pelvis (Figure 1) was performed in order to further establish the diagnosis. The result revealed an enlarged appendix with a maximum diameter of 12 mm, fat strandings in the periappendiceal region, and mucosal enhancement in the terminal ileum, ileocecal valve, and nearby cecum. Acute appendicitis was identified based on the history, clinical examination, laboratory, and radiographic results. Considering the history, clinical examination, laboratory, and radiological findings, acute appendicitis was diagnosed.
FIGURE 1.
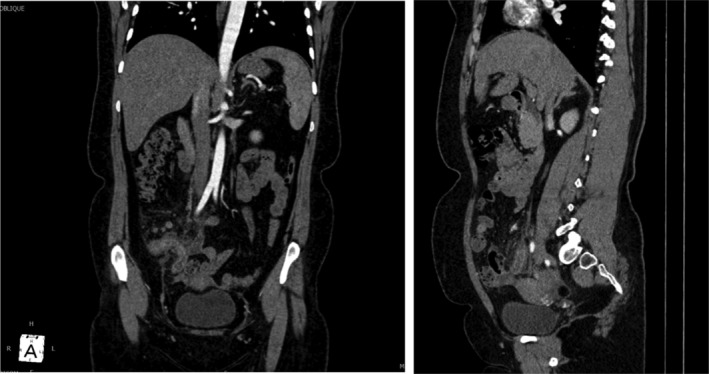
Contrast‐enhanced computed tomography of abdomen and pelvis (a‐ coronal and b‐ saggital) showing enlarged appendix with fat strandings in the periappendiceal region, and mucosal enhancement in the terminal ileum, ileocecal valve, and nearby cecum.
Following a discussion with the patient, she underwent a laparoscopic appendectomy. The intraoperative finding was an inflamed appendix adherent to the abdominal wall in contrast with the healthy base of the appendix. Following that, the specimen was sent for regular histopathological examination. Grossly (Figure 2), the appendix measured 7.0 × 2.0 cm, with the outer surface gray‐white, congested, and covered with lobulated fatty tissue. The cut section of the tip of the appendix showed an obliterated lumen, and the body showed a dilated lumen measuring 0.5 cm in diameter. Microscopic examination (Figure 3) showed a lining of columnar epithelium with a lumen containing necrotic debris, inflammatory cells, plant seed, and clusters of filamentous organisms consistent with actinomyces. Likewise, there was moderate transmural infiltration by inflammatory cells comprising neutrophils, eosinophils, and lymphocytes extending up to the periappendiceal fat. Following the diagnosis of appendicular actinomycosis, the medication was changed to a high dose of amoxicillin (1 gm thrice a day for 45 days), metronidazole (500 mg thrice a day for 7 days) along with proton pump inhibitor‐ pantoprazole (40 mg once a day on empty stomach for 45 days). The postoperative period was uneventful, and follow‐up of the patient after 7 days and 45 days remains unremarkable.
FIGURE 2.
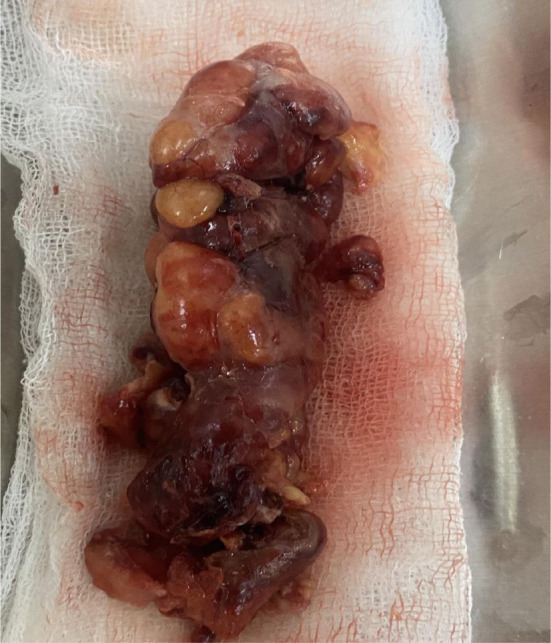
Gross images showing a gray‐white congested resected specimen of the appendix.
FIGURE 3.
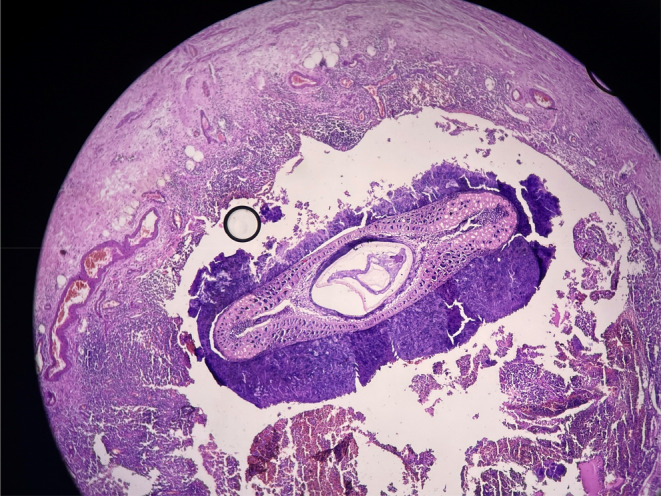
Histopathological image showing features of periappendicitis with appendicular actinomycosis and luminal plant seed.
3. DISCUSSION
Actinomycosis is a rare infectious disease caused by actinomyces species, which is a gram‐positive anaerobic bacterium. 3 , 4 Despite the clear statistical data, an incidence of 0.3–1 incident per year per 100,000 people has been estimated. 5 It occurs as a commensal in the oral cavity, gastrointestinal tract, and female genital tract, and becomes pathogenic when the mucosal barrier is breached. 3 , 4 , 7 It commonly involves the cervicofacial region (50%) followed by the abdominal region (20%). 7
Although abdominal actinomycosis commonly involves the appendix and ileocecal region, 7 it is rarely encountered. A retrospective study of 1627 appendectomy specimens showed only one case (0.06%) of actinomycosis, 1 whereas the evaluation of 3602 appendicectomy specimens in another study showed only a case of actinomycosis (0.02%). 2 There are few cases reported for actinomycosis of the appendix 5 , 6 , 7 , 8 , 9 , 10 , 11 ; however, this study seems to be the first of its kind to be reported from the country.
Factors predisposing to abdominal actinomycosis include a history of bowel surgery, bowel perforation, tumors, long‐standing intrauterine devices, foreign bodies, immunosuppression, malnutrition, and HIV infection. 9 Despite a long list of risk factors, none were appreciated in our case. Abdominal actinomycosis is common in adolescents and middle‐aged groups and approximately three times more common in males. 12 However, a case series of 22 patients with intra‐abdominal actinomycosis showed females were more affected (90%), 13 supporting the gender preference as in our case.
The cases among females are rising due to an increase in the use of intrauterine contraceptive devices inducing chronic inflammation. The reported cases of abdominal actinomycosis before 1970 showed that most cases were due to bowel perforation; however, female genital tract colonization has played a major role in the development of abdominal actinomycosis recently. 4 Unlike age and gender, there is no association of residence, social class, or ethnicity with the disease. 12
It has a varied clinical presentation, so it was described earlier as “the most misdiagnosed disease”. 12 Abdominal actinomycosis is a rare differential diagnosis of appendicitis. 7 Nonspecific symptoms such as abdominal pain (90%), fever (60%), and weight loss (60%) were the most common clinical features among actinomycosis cases localized to the abdominopelvic location. 3 Our case also presented with a fever and an acute abdomen mimicking acute appendicitis.
Laboratory values are of little help in the diagnosis. 7 Likewise, the preoperative or intraoperative diagnosis is rare as the findings are confused with acute inflammatory conditions or malignancy. 12 So, the diagnosis depends on the histologic examination. The appearance of characteristic sulfur granules or the culture of the organism gives a definitive diagnosis. 7 Although characteristic sulfur granules were not noticed in our case, the histopathological findings were consistent with actinomycosis, which helped in the diagnosis of the case.
Surgical resection is frequently required for diagnosis and management. 12 Combined surgical treatment and antibiotics are the preferred management. 7 , 12 Long‐term antibiotic treatment with penicillin controls and cures the infection after an appendectomy. 11 Likewise, in our case, amoxicillin was administered for six and a half weeks. Abdominal actinomycosis has a favorable prognosis with low mortality as it is cured in the majority of cases. 7 , 12
AUTHOR CONTRIBUTIONS
Sujan Bohara: Conceptualization; resources; writing – original draft; writing – review and editing. Manoj Khadka: Conceptualization; resources; writing – original draft; writing – review and editing. Pawan Singh Bhat: Resources; validation; writing – original draft. Prajwal Syangtang: Resources; writing – original draft. Badal Karki: Resources; writing – review and editing. Bhagawan Shrestha: Resources; writing – review and editing. Shoshan Arja Acharya: Data curation; investigation. Khusbhu Khetan: Data curation; investigation. Jyoti Rayamajhi: Supervision. Sushil Bahadur Rawal: Supervision.
FUNDING INFORMATION
All authors declare that they have not received any grants or funding for this manuscript.
CONFLICT OF INTEREST STATEMENT
All the authors declare that they have no conflicts of interest.
ETHICS STATEMENT
Not required for the publication of this manuscript.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy. A copy of the written consent is available for review by the editor in chief of this journal on request.
Bohara S, Khadka M, Bhat PS, et al. Appendicular actinomycosis: The first reported case of an uncommon finding of a common ailment from Nepal. Clin Case Rep. 2023;11:e7996. doi: 10.1002/ccr3.7996
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon request
REFERENCES
- 1. Limaiem F, Arfa N, Marsaoui L, Bouraoui S, Lahmar A, Mzabi S. Unexpected histopathological findings in appendectomy specimens: a retrospective study of 1627 cases. Indian J Surg. 2015;1(77):1285‐1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alemayehu H, Snyder CL, St. Peter SD, Ostlie DJ. Incidence and outcomes of unexpected pathology findings after appendectomy. J Pediatr Surg. 2014;49(9):1390‐1393. [DOI] [PubMed] [Google Scholar]
- 3. Bonnefond S, Catroux M, Melenotte C, et al. Clinical features of actinomycosis a retrospective, multicenter study of 28 cases of miscellaneous presentations. Medicine. 2016;95(24):e392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wagenlehner FME, Mohren B, Naber KG, Männl HFK. Abdominal actinomycosis. Clin Microbiol Infect. 2003;9(8):881‐885. [DOI] [PubMed] [Google Scholar]
- 5. Completo S, Veríssimo M, Pereira AMG, França I, Sande Lemos P. Appendicular actinomycosis: behind the curtains of appendicitis. Cureus. 2022;14:e29709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sung YN, Kim J. Appendiceal actinomycosis mimicking appendiceal tumor, appendicitis or inflammatory bowel disease. J Pathol Transl Med. 2021;55(5):349‐354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu K, Joseph D, Lai K, Kench J, Ngu MC. Abdominal actinomycosis presenting as appendicitis: two case reports and review. J Surg Case Rep. 2016;2016(5):rjw068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gómez‐Torres GA, Ortega‐Gárcia OS, Gutierrez‐López EG, et al. A rare case of subacute appendicitis, actinomycosis as the final pathology reports: a case report and literature review. Int J Surg Case Rep. 2017;36:46‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Karakuş E, Mambet E, Azılı MN, Gülhan B, Tiryaki T, Tezer H. Actinomycosis of the appendix. APSP J Case Rep. 2014;5:26. [PMC free article] [PubMed] [Google Scholar]
- 10. Lee SY, Kwon HJ, Cho JH, et al. Actinomycosis of the appendix mimicking appendiceal tumor: a case report. World J Gastroenterol. 2010;16(3):395‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yardimci VH, Yardimci AH. Is appendectomy always the adequate treatment? Clinical manifestations of isolated actinomycosis in appendix. Turk J Surg. 2021;37(4):403‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int J Surg. 2007;5:441‐448. [DOI] [PubMed] [Google Scholar]
- 13. Choi MM, Beak JH, Lee JN, Park S, Lee WS. Clinical features of abdominopelvic actinomycosis: report of twenty cases and literature review. Yonsei Med J. 2009;50(4):555‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request


