Abstract
Background:
The aim of the study was to map microvascular complications associated with diabetes mellitus from personal health records and to guide chronic disease management by revealing the economic burden of the disease.
Method:
The data of patients with diabetes who developed microvascular complications were obtained from the e-Pulse database of the Ministry of Health, with the definitions of the disease. First, the distribution of patients by province and gender was determined and then patients with multiple complications were identified. Only direct costs and their distribution on the basis of complications were determined from the database according to the cost of illness methodology from the payer’s perspective. Then, average annual per-patient costs were determined using a top-down costing approach.
Results:
Between 2016 and 2020, a total of 7 656 700 patients with diabetes were reached. The number of patients with microvascular complications between 2016 and 2020 obtained from the e-Pulse database with the above definitions was 1 406 904. Regarding the complications, a total of 66 838 people developed nephropathy, 314 706 people developed retinopathy, and 1 084 843 people developed neuropathy. The total cost of patients with microvascular complications was $1 356 663 204.31 and the average annual cost per patient was $1096.21. The average annual cost of neuropathy is $659 862 971.96, retinopathy is $356 594 282.51 and nephropathy is $465 821 696.29, with per-patient costs of $701.82, $1495.24, and $10 516.11, respectively.
Conclusion:
Diabetes mellitus, with its microvascular complications, causes significant disease and economic burden. Türkiye’s national health database system, e-Pulse, is an important database that provides patient follow-up at both individual and population levels and helps with the management of the disease and taking preventive measures before the development of the complications.
Keywords: Diabetes mellitus, economic burden of diabetes related microvascular complications, neuropathy, nephropathy, retinopathy, personal health record
Highlights
Between 2016 and 2020, a total of number of 7 656 700 patients with diabetes were reached.
The total cost of patients with microvascular complications was $1 356 663 204.31, and the average annual cost per patient was $1096.21.
The number of patients with microvascular complications is 1 406 904. In terms of patient sex distribution: 534 124 were male (38%) and 872 780 (62%) were female.
On a provincial basis, the provinces with the highest number of complications were Gaziantep, Burdur, and Manisa, and the provinces with the lowest number were Ankara, Edirne, and Artvin.
Introduction
An electronic personal health record (PHR) is an electronic application through which individuals can access, manage, and share their own health information and the health information of others for whom they are authorized in a private, secure, and confidential environment. At a minimum, PHRs allow individuals to manually enter their health information on a website, which can then be accessed over the internet as needed. Advanced, interoperable PHRs can electronically transfer a patient’s clinical data from electronic health records (EHRs) of different hospitals, pharmacies, health insurers, and other institutions so that other health-care organizations can have access to the patient. In addition to storing and accessing clinical data, many PHRs provide secure patient–clinician messaging, prescription request and renewal features, access to high-quality educational materials, and other features designed to promote patient self-management and improved communication with health-care professionals.1
The collection of Turkish citizens’ health records electronically under the umbrella of “e-Nabız/e-Pulse” has been ongoing since 2015. The statisticalization and interpretation of these data is carried out through the SINA (Statistical Causation and Analyses in Health) system. In order to interpret the information from this system and provide added value to chronic disease management, this study focuses on diabetes mellitus (DM), which is of critical importance for Türkiye.2
Diabetes mellitus is a chronic disease with an increasing prevalence worldwide. In 2021, there were 537 million people living with DM, which causes significant disease burden and economic burden. According to the International Diabetes Federation (IDF), this number is projected to increase to 643 million in 2030 and 783 million in 2045. With a dramatic increase observed in all continents, it is obvious that it will create significant pressure on the health systems of countries.3
According to IDF estimates, 9 million people with diabetes live in Türkiye and the prevalence is estimated to be 15.9%. A cost study on diabetic patients in Türkiye was conducted by the SSI (Social Security Institution) in 2010 and was estimated at 10 billion Turkish liras (TL).4 In another study published in 2014, the estimated cost of diabetes to Türkiye was estimated to be in the range of 12.5 billion TL.5 In a report published in 2017, it was estimated that type 2 diabetes mellitus (T2DM) complication costs would reach 19 billion TL.6 In addition, complications cause serious negative health problems for the patient if they are not prevented and treated. In addition, while there is minimal resource utilization in case of precautions, the progression of the disease causes very high resource utilization, prolonged hospitalization, even disability, and early death.7
Prevention of acute and chronic complications and halting the progression of chronic complications are considered among the goals of diabetes treatment. The importance of increasing health literacy and access to primary health-care services is emphasized in preventing diabetes-related complications and reducing their effects.8 In Türkiye, the rate of individuals with diabetes with low treatment compliance and continuity can reach up to 40.4%, according to the results of a study conducted in a university hospital between October 2010 and October 2011. In the report published by IQVIA, when the CORE Diabetes Model is adapted by taking into account the level of T2DM treatment compliance and continuity in Türkiye, it is calculated that 7.42% of this cost (approximately 1.26 billion TL per year) is due to complications related to low T2DM treatment compliance and continuity. This avoidable expenditure and economic loss is only one dimension of the total cost of low T2DM treatment adherence and continuity; it is only associated with preventable complications.6
In this direction, we aimed to reveal the microvascular complication map of the disease for Türkiye and to determine the current economic burden of the disease by using the Ministry of Health digital database e-nabız for microvascular complications related to DM, which is known to be an important disease and economic burden.
Methods
In order to obtain data on microvascular complications of diabetes and diabetes-related patients, different definitions were made on the basis of both type 1 DM and T2DM and complications in order to obtain accurate data through the e-Pulse electronic registration system. In this definition, ICD (International Classification of Disease) data codes and patients who were in the system but did not meet the definitions but entered the system once with the correct ICD code were excluded. Microvascular complications were defined by the following criteria (Table 1). Based on the relevant ICD codes, patients with diabetes who developed microvascular complications in 2016-2020 were extracted from the system.
Table 1.
Definitions of DM Microvascular Complications
| Microvascular complications | 1 | Nephropathy ①ICD10 Codes: E11.2 E13.2 E08.2, E09.2, E14.2 N18.x, I12, I13 OR ②Patients with kidney transplant (ICD Z94.0 or procedure P618610) OR ③Patients on chronic dialysis program (with one of the procedures P704230 P704233 530710 704260 704270) |
| 2 | Retinopathy ①ICD10 Codes: E08.3 E09.3 E11.3 E13.3 E14.3 H36 H35.0 H35.3 H35.9 OR Non-proliferative Diabetic Retinopathy Proliferative Diabetic Retinopathy ② Vitrectomy (SUT Code: P617660 or 617660 /P617640 or 617640 / P617650 or 617650 / 617640) OR Diffuse Diabetic Macular Edema ③Macular Laser/Panretinal photocoagulation (SUT Code: 617630 Laser photocoagulation) OR Diffuse Diabetic Macular Edema ④Intravitreal injection (SUT code: 617620 AND ATC codes S01LA04 or S01LA05) OR Stable Diabetic Retinopathy ⑤Intravitreal injection (SUT code: 617620 and ATC code S01BA01) |
|
| 3 | Cataract ①ICD10: E08.36, E09.36, E10.36, E11.36, E13.36 H28 H26.2 H26.4 H26.8 H26.9 OR ②Those with cataract intervention (SUT Codes: P617341/P617342/P617540 / 617341 / 617342 / 617540) |
|
| 4 | Neuropathy ①ICD10: E11.4 E14.4 G63.2 OR ②Use of pregabalin (N03AX) or duloxetine (N06AX21) or alpha-lipoic acid (A16AX01) |
Launched in 2015 by the Ministry of Health, the e-Pulse system is a digital database where the personal health records of each individual who is a citizen of the Republic of Türkiye and has General Health Insurance are stored. The system contains the data of 68 million people. With the permission of the Ministry of Health, the E-95741342-708.01-206385672 number code was used to anonymize patient personal data, and patients were reached with the relevant codes. The reason for analyzing the data between 2016 and 2020 is that the e-Pulse system has been collecting data since 2015. The data were cleaned and were ready for analysis in 6 months. Between 2016 and 2020, a total of 7 656 700 patients (7 438 764 patients with T2DM and 217 936 patients with Type 1 DM) with diabetes were reached. Between 2016 and 2020, 1 406 904 patients who were diagnosed with DM and developed microvascular complications were identified. The provinces where these patients lived, the prevalence of the disease according to province, and the prevalence of retinopathy, nephropathy, and neuropathy according to gender and province of residence were determined. Then, the economic burden of each complication according to the cost of disease method was determined from a payer perspective.
Cost of illness studies consisting of direct, indirect, and intangible costs can be presented differently according to the databases of countries and the data obtained. Moral costs are excluded from the studies since they cannot be quantified.9 In this study, only direct costs were calculated from the perspective of the reimbursing institution (SSI).
Direct cost is the money spent by individuals, insurance institutions, or the state for the care, cure, and prevention of a disease. It is the use or consumption of resources in the process of the direct treatment of a disease. Examples such as the use of time and knowledge of physicians, nurses, and medical care personnel, the use of machines and medical equipment, and the use of medicines and other consumables can be given for direct costs.9
Generally, direct costs are classified as direct medical and nondirect medical costs. This classification depends on whether the resource is used directly in treatment. Direct medical costs are the amount spent on outpatient clinic, other clinics, medical supplies, all laboratory or imaging tests, and interventions. Only direct medical costs were taken into consideration in the study.
For the calculation of direct disease costs, the method developed by Cowley et al10 on behalf of the World Bank (WB) and WHO was used. In the method, the clinical path is followed, and the number of uses of each expenditure item is multiplied by the percentage of cases using it and unit costs to reach the main total expenditure. The formulation used is as follows:
Unit cost of health services required to deliver the intervention (C)
Quantity of each type of service required for the intervention (V)
Number of people applying to the health institution for that service (n)
In the following equation, “i” denotes the service levels and “j” denotes the required services needed for the intervention. The equation assumes that there are s-types of appropriate services. If some of the services are not needed in the production of intervention j, the values of V will be 0.
 |
Direct medical costs were obtained by multiplying the type and amount of service received by the utilization rate and unit cost.10 Total costs were then converted to per-patient costs based on the total number of patients using a top-down costing approach.
Results
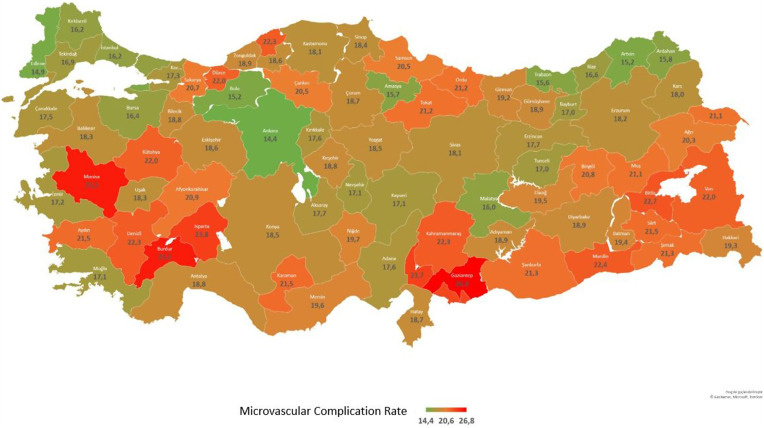
Frequency Rate of Microvascular Complications in Patients with Diabetes
The number of patients with microvascular complications between 2016 and 2020, obtained from the e-Pulse database with the above definitions, was determined as 1 406 904. About 534 124 were male (38%) and 872 780 (62%) were female. On a provincial basis, the provinces with the highest number of complications were Gaziantep, Burdur, and Manisa, and the provinces with the lowest number were Ankara, Edirne, and Artvin (Table 2, Figure 1).
Table 2.
Number of People with DM Related Microvascular Complications (Türkiye)
| Province | Male | Microvascular Complication Rate—Male | Female | Microvascular Complication Rate—Female | Microvascular Complication Number | Microvascular Complication Rate | Total Diabetes Mellitus Patients |
|---|---|---|---|---|---|---|---|
| Adana | 15 359 | 16.7 | 24 028 | 18.2 | 39 386 | 17.6 | 224 266 |
| Adıyaman | 2826 | 17.6 | 5041 | 19.7 | 7868 | 18.9 | 41 589 |
| Afyonkarahisar | 6387 | 19.0 | 12 220 | 22.0 | 18 609 | 20.9 | 89 123 |
| Ağrı | 1346 | 17.9 | 2680 | 21.8 | 4026 | 20.3 | 19 805 |
| Amasya | 2473 | 15.1 | 3925 | 16.1 | 6398 | 15.7 | 40 813 |
| Ankara | 28 065 | 13.2 | 47 462 | 15.3 | 75 529 | 14.4 | 523 944 |
| Antalya | 18 757 | 17.4 | 26 295 | 19.9 | 45 047 | 18.8 | 239 538 |
| Artvin | 1072 | 14.2 | 1532 | 15.9 | 2604 | 15.2 | 17 178 |
| Aydın | 11 371 | 20.1 | 16 977 | 22.6 | 28 346 | 21.5 | 131 762 |
| Balıkesir | 10 794 | 17.4 | 16 574 | 19.0 | 27 367 | 18.3 | 149 417 |
| Bilecik | 1590 | 17.0 | 2760 | 20.1 | 4351 | 18.8 | 23 123 |
| Bingöl | 1075 | 21.3 | 1527 | 20.5 | 2602 | 20.8 | 12 502 |
| Bitlis | 1314 | 22.4 | 2029 | 22.9 | 3343 | 22.7 | 14 731 |
| Bolu | 2235 | 15.3 | 3031 | 15.1 | 5265 | 15.2 | 34 707 |
| Burdur | 3351 | 23.9 | 4953 | 26.7 | 8303 | 25.5 | 32 560 |
| Bursa | 17 865 | 15.1 | 29 473 | 17.3 | 47 338 | 16.4 | 288 748 |
| Çanakkale | 4330 | 15.9 | 7124 | 18.6 | 11 455 | 17.5 | 65 449 |
| Çankırı | 2 212 | 18.5 | 3489 | 22.0 | 5701 | 20.5 | 27 773 |
| Çorum | 4241 | 17.0 | 7363 | 19.8 | 11 604 | 18.7 | 62 187 |
| Denizli | 11 977 | 20.8 | 18 157 | 23.5 | 30 132 | 22.3 | 134 877 |
| Diyarbakır | 4987 | 16.7 | 9756 | 20.2 | 14 744 | 18.9 | 78 189 |
| Edirne | 2932 | 14.2 | 4417 | 15.4 | 7348 | 14.9 | 49 461 |
| Elazığ | 3792 | 19.2 | 5747 | 19.7 | 9539 | 19.5 | 48 919 |
| Erzincan | 1549 | 16.8 | 2327 | 18.4 | 3875 | 17.7 | 21 864 |
| Erzurum | 3207 | 17.7 | 4720 | 18.6 | 7927 | 18.2 | 43 558 |
| Eskişehir | 6450 | 16.4 | 12 195 | 20.1 | 18 647 | 18.6 | 100 129 |
| Gaziantep | 15 548 | 24.8 | 28 664 | 28.1 | 44 215 | 26.8 | 164 682 |
| Giresun | 3809 | 17.0 | 6 862 | 20.8 | 10 672 | 19.2 | 55 490 |
| Gümüşhane | 867 | 17.9 | 1345 | 19.6 | 2212 | 18.9 | 11 712 |
| Hakkâri | 501 | 16.7 | 952 | 21.1 | 1453 | 19.3 | 7514 |
| Hatay | 10 914 | 17.3 | 15 510 | 19.9 | 26 422 | 18.7 | 140 986 |
| Isparta | 5162 | 22.8 | 7892 | 24.4 | 13 054 | 23.8 | 54 927 |
| Mersin | 14 322 | 18.2 | 21 469 | 20.7 | 35 789 | 19.6 | 182 442 |
| İstanbul | 82 124 | 15.0 | 132 777 | 17.1 | 214 900 | 16.2 | 1 325 186 |
| İzmir | 34 474 | 16.4 | 52 579 | 17.8 | 87 049 | 17.2 | 506 049 |
| Kars | 924 | 16.1 | 1531 | 19.5 | 2455 | 18.0 | 13 604 |
| Kastamonu | 4062 | 17.5 | 5592 | 18.6 | 9653 | 18.1 | 53 371 |
| Kayseri | 7723 | 15.9 | 13 101 | 17.9 | 20 825 | 17.1 | 121 524 |
| Kırklareli | 2777 | 15.4 | 4225 | 16.8 | 7002 | 16.2 | 43 270 |
| Kırşehir | 2029 | 17.4 | 3328 | 19.7 | 5357 | 18.8 | 28 489 |
| Kocaeli | 11 749 | 15.4 | 21 258 | 18.6 | 33 009 | 17.3 | 190 275 |
| Konya | 14 140 | 16.7 | 25 129 | 19.7 | 39 271 | 18.5 | 212 254 |
| Kütahya | 5855 | 19.9 | 10 438 | 23.4 | 16 294 | 22.0 | 73 947 |
| Malatya | 4215 | 14.9 | 6930 | 16.7 | 11 146 | 16.0 | 69 856 |
| Manisa | 16 308 | 24.3 | 26 357 | 26.3 | 42 665 | 25.5 | 167 396 |
| Kahramanmaraş | 6763 | 19.8 | 12 463 | 24.0 | 19 227 | 22.3 | 86 086 |
| Mardin | 2855 | 18.6 | 6082 | 24.7 | 8939 | 22.4 | 39 989 |
| Muğla | 8204 | 15.9 | 10 459 | 18.1 | 18 660 | 17.1 | 109 416 |
| Muş | 1212 | 20.0 | 2007 | 21.9 | 3219 | 21.1 | 15 254 |
| Nevşehir | 2091 | 15.6 | 3544 | 18.1 | 5634 | 17.1 | 32 900 |
| Niğde | 2314 | 17.5 | 4501 | 21.1 | 6816 | 19.7 | 34 530 |
| Ordu | 6673 | 19.0 | 12 132 | 22.7 | 18 806 | 21.2 | 88 750 |
| Rize | 2303 | 15.3 | 3382 | 17.7 | 5685 | 16.6 | 34 187 |
| Sakarya | 8090 | 19.3 | 13 159 | 21.7 | 21 249 | 20.7 | 102 510 |
| Samsun | 10 900 | 18.5 | 18 796 | 22.0 | 29 697 | 20.5 | 144 594 |
| Siirt | 1066 | 19.2 | 1902 | 23.0 | 2968 | 21.5 | 13 828 |
| Sinop | 2546 | 17.2 | 3726 | 19.2 | 6272 | 18.4 | 34 163 |
| Sivas | 4338 | 16.0 | 8286 | 19.4 | 12 626 | 18.1 | 69 765 |
| Tekirdağ | 6645 | 15.8 | 10 367 | 17.6 | 17 012 | 16.9 | 100 867 |
| Tokat | 5170 | 18.8 | 9950 | 22.8 | 15122 | 21.2 | 71 193 |
| Trabzon | 4698 | 14.8 | 7111 | 16.2 | 11 809 | 15.6 | 75 849 |
| Tunceli | 476 | 17.4 | 527 | 16.6 | 1003 | 17.0 | 5 908 |
| Şanlıurfa | 6818 | 19.0 | 11 859 | 22.8 | 18 678 | 21.3 | 87 782 |
| Uşak | 3488 | 17.8 | 5186 | 18.6 | 8674 | 18.3 | 47 483 |
| Van | 3614 | 21.3 | 5941 | 22.5 | 9555 | 22.0 | 43 406 |
| Yozgat | 3170 | 17.4 | 5464 | 19.2 | 8634 | 18.5 | 46 705 |
| Zonguldak | 5409 | 17.4 | 8928 | 20.0 | 14 338 | 18.9 | 75 678 |
| Aksaray | 2478 | 15.7 | 4630 | 18.9 | 7 108 | 17.7 | 40 253 |
| Bayburt | 417 | 15.4 | 620 | 18.3 | 1036 | 17.0 | 6099 |
| Karaman | 1905 | 19.7 | 3387 | 22.7 | 5292 | 21.5 | 24 569 |
| Kırıkkale | 2146 | 16.5 | 3678 | 18.3 | 5825 | 17.6 | 33 047 |
| Batman | 1803 | 17.7 | 3364 | 20.5 | 5167 | 19.4 | 26 585 |
| Şırnak | 1178 | 18.9 | 2410 | 22.6 | 3588 | 21.3 | 16 877 |
| Bartın | 2345 | 19.9 | 3876 | 24.0 | 6220 | 22.3 | 27 928 |
| Ardahan | 337 | 15.0 | 455 | 16.4 | 791 | 15.8 | 5015 |
| Iğdır | 759 | 18.9 | 1295 | 22.6 | 2054 | 21.1 | 9755 |
| Yalova | 1843 | 14.1 | 3046 | 16.2 | 4889 | 15.3 | 31 937 |
| Karabük | 2475 | 17.3 | 3745 | 19.6 | 6219 | 18.6 | 33 426 |
| Kilis | 1108 | 21.4 | 1867 | 24.7 | 2975 | 23.3 | 12 748 |
| Osmaniye | 4479 | 21.1 | 7690 | 25.5 | 12 169 | 23.7 | 51 394 |
| Düzce | 2946 | 19.4 | 5209 | 23.8 | 8155 | 22.0 | 37 039 |
| Unknown | 9570 | ||||||
| 534 124 | 17.0 | 872 780 | 19.4 | 1 406 904 | 18.4 | 7 656 700 |
Figure 1.
Prevalence of Microvascular Complications by Province, % (minimum–maximum 14.4%-26.8%).
The frequency rate of microvascular complications by district is presented in Figure 2. According to this detail, the Nizip district of Gaziantep had the highest frequency of microvascular complications (40.3%), while the Hamamözü district of Amasya had the lowest frequency rate (9.6%).
Figure 2.
Prevalence of Microvascular Complications by District.
In terms of complications, there were a total of 66 838 people with nephropathy, 33 065 men (49%) and 33.773 women (51%). Its weight in microvascular complications is 5%. The highest prevalence is in Ardahan, Nevşehir, Rize, and Erzincan, and the lowest in Şanlıurfa, Uşak, Aksaray, and Denizli. The proportion of the population with a glycated hemoglobin (HbA1c) value >7, which is considered uncontrolled, is 55%, 53.5%, 51.9%, and 50.1% in the provinces with the highest frequency of microvascular complications and 58.4%, 47.6%, 47.3%, and 40.4% in the provinces with the lowest frequency of complications, respectively (Table 3).
Table 3.
Patients Developing Nephropathy by Gender and Province (Türkiye)
| City | Male | Female | Total Patients |
|---|---|---|---|
| Adana | 919 | 938 | 1857 |
| Adıyaman | 153 | 157 | 310 |
| Afyonkarahisar | 344 | 352 | 696 |
| Ağrı | 83 | 85 | 167 |
| Amasya | 176 | 179 | 355 |
| Ankara | 2025 | 2068 | 4093 |
| Antalya | 1290 | 1318 | 2608 |
| Artvin | 112 | 115 | 227 |
| Aydın | 758 | 774 | 1532 |
| Balıkesir | 576 | 589 | 1165 |
| Bilecik | 74 | 75 | 149 |
| Bingöl | 68 | 70 | 138 |
| Bitlis | 56 | 57 | 114 |
| Bolu | 172 | 175 | 347 |
| Burdur | 129 | 131 | 260 |
| Bursa | 1238 | 1265 | 2503 |
| Çanakkale | 258 | 264 | 523 |
| Çankırı | 123 | 125 | 248 |
| Çorum | 314 | 320 | 634 |
| Denizli | 443 | 453 | 896 |
| Diyarbakır | 261 | 266 | 527 |
| Edirne | 175 | 178 | 353 |
| Elazığ | 146 | 149 | 295 |
| Erzincan | 148 | 151 | 299 |
| Erzurum | 221 | 225 | 446 |
| Eskişehir | 404 | 412 | 816 |
| Gaziantep | 690 | 704 | 1394 |
| Giresun | 237 | 242 | 479 |
| Gümüşhane | 58 | 59 | 118 |
| Hakkâri | 29 | 29 | 58 |
| Hatay | 732 | 747 | 1479 |
| Isparta | 217 | 221 | 438 |
| Mersin | 720 | 736 | 1456 |
| İstanbul | 5778 | 5901 | 11679 |
| İzmir | 2199 | 2246 | 4444 |
| Kars | 53 | 54 | 107 |
| Kastamonu | 271 | 277 | 547 |
| Kayseri | 609 | 622 | 1231 |
| Kırklareli | 146 | 149 | 295 |
| Kırşehir | 151 | 154 | 306 |
| Kocaeli | 845 | 863 | 1708 |
| Konya | 754 | 770 | 1524 |
| Kütahya | 334 | 341 | 675 |
| Malatya | 258 | 264 | 523 |
| Manisa | 716 | 732 | 1448 |
| Kahramanmaraş | 298 | 305 | 603 |
| Mardin | 168 | 171 | 339 |
| Muğla | 557 | 569 | 1126 |
| Muş | 57 | 58 | 116 |
| Nevşehir | 192 | 196 | 388 |
| Niğde | 123 | 125 | 248 |
| Ordu | 481 | 492 | 973 |
| Rize | 258 | 264 | 523 |
| Sakarya | 562 | 574 | 1136 |
| Samsun | 592 | 604 | 1196 |
| Siirt | 52 | 53 | 105 |
| Sinop | 151 | 154 | 306 |
| Sivas | 296 | 303 | 599 |
| Tekirdağ | 378 | 386 | 764 |
| Tokat | 314 | 320 | 634 |
| Trabzon | 430 | 439 | 869 |
| Tunceli | 25 | 25 | 50 |
| Şanlıurfa | 206 | 211 | 417 |
| Uşak | 137 | 140 | 277 |
| Van | 187 | 191 | 378 |
| Yozgat | 204 | 209 | 413 |
| Zonguldak | 428 | 437 | 865 |
| Aksaray | 121 | 123 | 244 |
| Bayburt | 28 | 28 | 56 |
| Karaman | 91 | 93 | 184 |
| Kırıkkale | 132 | 135 | 266 |
| Batman | 73 | 74 | 147 |
| Şırnak | 62 | 64 | 126 |
| Bartın | 127 | 129 | 256 |
| Ardahan | 43 | 44 | 87 |
| Iğdır | 39 | 40 | 78 |
| Yalova | 158 | 162 | 320 |
| Karabük | 170 | 173 | 343 |
| Kilis | 55 | 56 | 112 |
| Osmaniye | 237 | 242 | 479 |
| Düzce | 173 | 176 | 349 |
| Total | 33 065 | 33 773 | 66 838 |
The total number of patients who developed retinopathy was 314 706, with 146 810 (47%) males and 167 896 (53%) females. Its weight in microvascular complications is 22%. When weighing the frequency of diabetes, Gaziantep, Burdur, Manisa, and Osmaniye have the highest frequency and Ankara, Bolu, and Ardahan have the lowest frequency. The proportion of the population with HbA1c values > 7 in these provinces is 50.9% in Gaziantep, 40.9% in Burdur, 40.8% in Manisa, 46.4% in Osmaniye, 40.3% in Ankara, 43.7% in Bolu, and 55% in Ardahan (Table 4).
Table 4.
Patients with Retinopathy According to Gender and Province
| City | Male | Female | Total Patients |
|---|---|---|---|
| Adana | 4715 | 5231 | 9946 |
| Adıyaman | 636 | 894 | 1530 |
| Afyonkarahisar | 1820 | 2243 | 4063 |
| Ağrı | 235 | 344 | 579 |
| Amasya | 645 | 822 | 1467 |
| Ankara | 9160 | 10 655 | 19 815 |
| Antalya | 4548 | 3915 | 8462 |
| Artvin | 321 | 322 | 643 |
| Aydın | 3223 | 3120 | 6343 |
| Balıkesir | 3028 | 3384 | 6412 |
| Bilecik | 330 | 422 | 752 |
| Bingöl | 285 | 313 | 598 |
| Bitlis | 260 | 329 | 589 |
| Bolu | 627 | 661 | 1288 |
| Burdur | 989 | 1009 | 1998 |
| Bursa | 4643 | 5349 | 9991 |
| Çanakkale | 1232 | 1255 | 2487 |
| Çankırı | 631 | 723 | 1354 |
| Çorum | 1116 | 1461 | 2577 |
| Denizli | 3172 | 3267 | 6439 |
| Diyarbakır | 1034 | 1438 | 2472 |
| Edirne | 617 | 555 | 1172 |
| Elazığ | 937 | 1107 | 2044 |
| Erzincan | 442 | 476 | 919 |
| Erzurum | 552 | 604 | 1157 |
| Eskişehir | 1268 | 1605 | 2873 |
| Gaziantep | 3302 | 4013 | 7315 |
| Giresun | 1045 | 1209 | 2254 |
| Gümüşhane | 252 | 259 | 511 |
| Hakkâri | 110 | 140 | 250 |
| Hatay | 2703 | 2511 | 5214 |
| Isparta | 1531 | 1998 | 3529 |
| Mersin | 3680 | 3907 | 7587 |
| İstanbul | 26 377 | 29 290 | 55 667 |
| İzmir | 10 066 | 11 347 | 21 413 |
| Kars | 180 | 183 | 364 |
| Kastamonu | 1 337 | 1288 | 2625 |
| Kayseri | 2070 | 2799 | 4869 |
| Kırklareli | 730 | 647 | 1376 |
| Kırşehir | 521 | 687 | 1208 |
| Kocaeli | 3195 | 3972 | 7167 |
| Konya | 3415 | 4278 | 7693 |
| Kütahya | 1384 | 1857 | 3241 |
| Malatya | 1280 | 1520 | 2800 |
| Manisa | 5193 | 6214 | 11 407 |
| Kahramanmaraş | 1708 | 2044 | 3753 |
| Mardin | 554 | 836 | 1390 |
| Muğla | 2628 | 2014 | 4642 |
| Muş | 283 | 365 | 648 |
| Nevşehir | 526 | 704 | 1230 |
| Niğde | 561 | 711 | 1272 |
| Ordu | 1458 | 1902 | 3360 |
| Rize | 566 | 507 | 1073 |
| Sakarya | 2291 | 2700 | 4991 |
| Samsun | 2636 | 3264 | 5900 |
| Siirt | 200 | 273 | 472 |
| Sinop | 751 | 782 | 1532 |
| Sivas | 1177 | 1612 | 2790 |
| Tekirdağ | 1428 | 1495 | 2923 |
| Tokat | 1737 | 2544 | 4281 |
| Trabzon | 1315 | 1443 | 2759 |
| Tunceli | 137 | 114 | 251 |
| Şanlıurfa | 1292 | 1611 | 2904 |
| Uşak | 832 | 922 | 1754 |
| Van | 647 | 713 | 1360 |
| Yozgat | 1112 | 1390 | 2502 |
| Zonguldak | 1149 | 1407 | 2556 |
| Aksaray | 619 | 805 | 1424 |
| Bayburt | 90 | 128 | 218 |
| Karaman | 438 | 545 | 983 |
| Kırıkkale | 512 | 758 | 1270 |
| Batman | 386 | 625 | 1011 |
| Şırnak | 259 | 381 | 640 |
| Bartın | 620 | 893 | 1513 |
| Ardahan | 93 | 83 | 175 |
| Iğdır | 148 | 205 | 354 |
| Yalova | 543 | 604 | 1148 |
| Karabük | 773 | 836 | 1609 |
| Kilis | 318 | 340 | 658 |
| Osmaniye | 1105 | 1259 | 2364 |
| Düzce | 1,078 | 1459 | 2537 |
| Türkiye | 146 810 | 167 896 | 314 706 |
The total number of patients with DM-related neuropathy was 1 084 843, with 377 852 men (35%), and 706 991 women (65%) experiencing neuropathy complications. The highest rates were observed in Gaziantep (22.8%), Burdur (20.1%), and Manisa (19.3%). In these provinces, the population of patients with diabetes with HbA1c values > 7 was 50.9% in Gaziantep, 40.9% in Burdur, and 40.8% in Manisa (Table 5).
Table 5.
Patients with Neuropathy by Gender and Province
| City | Male | Female | Total Patients |
|---|---|---|---|
| Adana | 10 595 | 19 116 | 29 710 |
| Adıyaman | 2164 | 4181 | 6345 |
| Afyonkarahisar | 4529 | 10 115 | 14 645 |
| Ağrı | 1059 | 2287 | 3347 |
| Amasya | 1763 | 3087 | 4851 |
| Ankara | 17 977 | 36 654 | 54 634 |
| Antalya | 13 693 | 22 308 | 35 997 |
| Artvin | 682 | 1182 | 1864 |
| Aydın | 7961 | 13 973 | 21 933 |
| Balıkesir | 7699 | 13 330 | 21 028 |
| Bilecik | 1255 | 2359 | 3613 |
| Bingöl | 791 | 1213 | 2004 |
| Bitlis | 1045 | 1686 | 2731 |
| Bolu | 1520 | 2330 | 3849 |
| Burdur | 2458 | 4074 | 6532 |
| Bursa | 12 679 | 23 877 | 36 557 |
| Çanakkale | 3051 | 5867 | 8919 |
| Çankırı | 1563 | 2805 | 4368 |
| Çorum | 3022 | 5932 | 8954 |
| Denizli | 8961 | 15 251 | 24 211 |
| Diyarbakır | 3842 | 8231 | 12 074 |
| Edirne | 2230 | 3757 | 5986 |
| Elazığ | 2884 | 4741 | 7624 |
| Erzincan | 1027 | 1816 | 2843 |
| Erzurum | 2468 | 3998 | 6465 |
| Eskişehir | 5030 | 10 516 | 15 547 |
| Gaziantep | 12 313 | 25 164 | 37 479 |
| Giresun | 2703 | 5693 | 8398 |
| Gümüşhane | 603 | 1081 | 1684 |
| Hakkâri | 378 | 805 | 1183 |
| Hatay | 7984 | 12 952 | 20 934 |
| Isparta | 3764 | 6187 | 9950 |
| Mersin | 10 641 | 17 805 | 28 444 |
| İstanbul | 53 278 | 102 764 | 156 045 |
| İzmir | 23 670 | 41 133 | 64 800 |
| Kars | 720 | 1338 | 2058 |
| Kastamonu | 2690 | 4356 | 7046 |
| Kayseri | 5346 | 10 223 | 15 569 |
| Kırklareli | 2007 | 3546 | 5553 |
| Kırşehir | 1445 | 2646 | 4091 |
| Kocaeli | 8204 | 17 223 | 25 429 |
| Konya | 10 546 | 21 010 | 31 557 |
| Kütahya | 4304 | 8624 | 12 928 |
| Malatya | 2833 | 5421 | 8255 |
| Manisa | 11 449 | 20 834 | 32 282 |
| Kahramanmaraş | 5071 | 10 630 | 15 703 |
| Mardin | 2239 | 5263 | 7503 |
| Muğla | 5406 | 8473 | 13 878 |
| Muş | 923 | 1658 | 2581 |
| Nevşehir | 1460 | 2791 | 4251 |
| Niğde | 1702 | 3817 | 5520 |
| Ordu | 5063 | 10 213 | 15 277 |
| Rize | 1587 | 2783 | 4370 |
| Sakarya | 5568 | 10 386 | 15 954 |
| Samsun | 8204 | 15 697 | 23 901 |
| Siirt | 842 | 1646 | 2489 |
| Sinop | 1727 | 2944 | 4671 |
| Sivas | 3060 | 6685 | 9747 |
| Tekirdağ | 5077 | 8829 | 13 906 |
| Tokat | 3444 | 7703 | 11 148 |
| Trabzon | 3138 | 5505 | 8642 |
| Tunceli | 346 | 402 | 747 |
| Şanlıurfa | 5576 | 10 393 | 15 969 |
| Uşak | 2647 | 4304 | 6950 |
| Van | 2898 | 5224 | 8122 |
| Yozgat | 2021 | 4091 | 6113 |
| Zonguldak | 3986 | 7333 | 11 319 |
| Aksaray | 1825 | 3853 | 5679 |
| Bayburt | 315 | 492 | 808 |
| Karaman | 1470 | 2908 | 4378 |
| Kırıkkale | 1601 | 2930 | 4531 |
| Batman | 1420 | 2767 | 4187 |
| Şırnak | 888 | 1982 | 2870 |
| Bartın | 1733 | 3066 | 4799 |
| Ardahan | 213 | 351 | 563 |
| Iğdır | 605 | 1086 | 1691 |
| Yalova | 1214 | 2388 | 3602 |
| Karabük | 1675 | 2951 | 4625 |
| Kilis | 804 | 1557 | 2361 |
| Osmaniye | 3399 | 6515 | 9913 |
| Düzce | 1876 | 3884 | 5761 |
| Türkiye | 377 852 | 706 991 | 1 084 843 |
Cost of Microvascular Complications
For 2020, the costs of patients with microvascular complications were calculated from a reimburser perspective. The dollar exchange rate was taken as the average for 2020 ($1 = 7.006 TL). The total cost of patients with microvascular complications from the total number of DM patients is $1356 663 204.31 per year, with inpatient (41%), intervention (22%), and outpatient (16%) treatments accounting for the highest cost. The share of drugs and medical supplies in total cost is 20%. The average annual cost per patient was $1096.21 (Table 6).
Table 6.
Cost of Microvascular Complications
| Cost ($) | Share of Total Cost | Cost Per Patient ($) | |
|---|---|---|---|
| Oral antidiabetics | 85 371 151.76 | 6% | 63.04 |
| Needle tip and strip | 15 580 426.72 | 1% | 11.50 |
| Insulin | 175 525 418.71 | 13% | 129.61 |
| Outpatient | 217 860 095.57 | 16% | 160.87 |
| Inpatient | 557 367 293.61 | 41% | 472.60 |
| Intervention | 304 958 817.95 | 22% | 258.58 |
| Total | 1 356 663 204.31 | 100% | 1096.21 |
The average 1-year total cost of patients with neuropathy from microvascular complications is $659 862 971.96, with the highest cost item being inpatient treatments (36%). This was followed by drugs and medical supplies (29%) and outpatient treatments (23%). The average annual cost per patient was $701.82 (Table 7).
Table 7.
Cost of Neuropathy Complication
| Cost ($) | Share of Total Cost | Cost Per Patient ($) | |
|---|---|---|---|
| Oral antidiabetics | 67 291 122.98 | 10% | 62.35 |
| Needle tip and strip | 109 393 522.77 | 17% | 101.36 |
| Insulin | 10 613 244.00 | 2% | 9.83 |
| Outpatient | 154 895 646.33 | 23% | 143.52 |
| Inpatient | 237 418 502.64 | 36% | 252.51 |
| Intervention | 80 250 933.24 | 12% | 85.35 |
| Total | 659 862 971.96 | 100% | 701.82 |
The total cost of retinopathy from microvascular complications is $356 594 282.51, with the highest cost in inpatient treatments (40%), followed by drugs and medical supplies (26%), and intervention (20%). The total annual average cost per patient was $1495.24 (Table 8).
Table 8.
Retinopathy Complication Cost ($)
| Cost ($) | Share of Total Cost | Cost Per Patient ($) | |
|---|---|---|---|
| Oral antidiabetics | 20 535 767.64 | 6% | 78.36 |
| Needle tip and strip | 68 637 546.83 | 19% | 261.91 |
| Insulin | 5 084 155.69 | 1% | 19.40 |
| Outpatient | 50 907 939.84 | 14% | 194.26 |
| Inpatient | 141 542 315.79 | 40% | 593.50 |
| Intervention | 69 886 556.73 | 20% | 293.04 |
| Total | 356 594 282.51 | 100% | 1495.24 |
Finally, the total annual cost of patients with nephropathy is $465 821 696.29, with the largest cost item being inpatient treatment at 50% and intervention at 41%. The annual cost per patient is $10 516.11 (Table 9).
Table 9.
Cost of Nephropathy Complications ($)
| Cost ($) | Share of Total Cost | Cost Per Patient ($) | |
|---|---|---|---|
| Oral antidiabetics | 1 675 960.29 | 0,4% | 27.32 |
| Needle tip and strip | 12 165 550.85 | 3% | 198.29 |
| Insulin | 933 553.18 | 0,2% | 15.22 |
| Outpatient | 25 180 939.66 | 5% | 410.44 |
| Inpatient | 234 019 930.58 | 50% | 5283.09 |
| Intervention | 191 845 761.73 | 41% | 4331.00 |
| Total | 465 821 696.29 | 100% | 10516.11 |
Discussion
Türkiye’s population is aging and the burden of chronic diseases is increasing, forcing health-care organizations to seek innovations for the efficient and effective care of these patients. In order to make the most effective use of scarce resources allocated to health, PHRs offer important outputs. Thanks to the outputs obtained, it is possible to ensure proper treatment, prevention of complications, and control of the disease. Personal health records can be used for a variety of purposes but may have the greatest potential clinical value in chronic disease management, which requires continuity of care and long-term follow-up. In Europe, Estonia is among the leading countries with e-prescription and digital health infrastructure. National electronic patient records are kept in a system called the Estonian National Health Information System (ENHIS), which includes all disease histories of the entire population of the country and where health data is recorded. The system has facilitated the early diagnosis of diseases, and thus treatment processes have been both correctly managed and shortened.11 Another example of a country whose citizens trust its health infrastructure is Denmark. On the portal developed, citizens’ health histories are stored with an identification number. Israel started a similar health digitalization project in 1995.12 In Israel, e-prescription, telemedicine, and online access to health data have been implemented within the scope of health services organizations. Another important example is Spain. There are digital health projects in different regions of the country with their own budgets.11 The costs associated with diabetes and related conditions are rising even higher. Diabetes can be successfully managed, and associated complications can be prevented, especially if it is diagnosed and treated early.13 Significant advances and global initiatives in chronic disease management have focused on leveraging digital health solutions such as mobile apps, wearables, remote monitoring systems, EHRs and disease management platforms. Electronic health record digitally store patients’ medical histories, lab results, allergy information, drug prescriptions, and treatment plans, allowing health-care providers and patients to easily access and share them. These systems enable better and faster decisions in chronic disease management, help patients adjust treatment plans based on their current condition, and improve continuity of care.
In this study, the total cost of patients with microvascular complications was $1 356 663 204.31, and the average annual cost per patient was $1096.21. The highest complication cost belongs to patients who developed nephropathy, and the average annual cost is $10 516.11. Then retinopathy had an average annual cost per patient of $1495.24, and neuropathy had an average annual cost per patient of $701.82. Of the total costs for patients with microvascular complications, inpatient treatment at 41% and intervention at 22% accounted for the highest cost. The total annual cost of neuropathy was $659 862 971.96, and the cost of retinopathy was $356 594 282.51. On a provincial basis, the provinces with the highest complications have a large population whose HbA1c value cannot be controlled according to population weight.
The United Kingdom Prospective Diabetes Study (UKPDS) and other studies have clearly demonstrated that glycemic control is important in DM.14,15 For every 1% decrease in HbA1c levels in T2DM, DM-related mortality can be reduced by 25% and all-cause mortality by 7%. A 1% reduction in HbA1c also leads to an 18% reduction in the prevalence of myocardial infarction (AMI), a 16% reduction in the development of heart failure (congestive heart failure), a 43% reduction in lower limb amputations, a 12% reduction in the development of stroke, and a 35% risk reduction in microvascular complications. There is also a 34% risk reduction in the development of microalbuminuria with tight blood glucose control. The results of the UKPDS and some other epidemiologic studies have shown that an HbA1c level of 7% and a systolic blood pressure below 130 mmHg reduce the risk of chronic complications.14,15 For type 1 DM, a 1% decrease in HbA1c reduces the risk of retinopathy by 35%, neuropathy by 30%, and nephropathy by 24%-44%.16
In general, if there is no special condition that increases the risk of hypoglycemia in T2DM and life expectancy is long enough, it should be preferred to set the HbA1c target at ≤7.0% (53 mmol/mol) to reduce microvascular complications. In order to manage the complications that arise according to the study results and to protect patients who have not yet developed complications, the course of the disease should be well followed, the health literacy of patients should be increased, and awareness should be raised. The distribution of patients with microvascular complications on a provincial basis is known from this study, so preventive and preventive medicine services should be mobilized in accordance with the regional conditions. Follow-up of DM patients should primarily be performed by the family medicine system, and patient education should be ensured. In order to eliminate risk factors, both primary care and secondary care should take an active role, and measures to reduce risk factors (such as smoking cessation) should be developed.
Study Limitations
The number of patients with microvascular complications is expected to be much higher, according to previously published national data. The frequency of nephropathy is given as 5% of the microvascular complications in this study. This is a much lower rate when compared to the previous national reports published so far. The frequency of diabetic kidney disease is given as between 20% and 30% of the patient population with diabetes.17 Using the ICD codes alone would inevitably miss patients without ICD codes but with albuminuria or low glomerular filtration rate. Because many of the clinicians do not use these codes in their daily practice. That is why analyses were made based on data from the relevant ICD codes, as far as the available data allowed. We think that using ICD codes alone would inevitably miss many subjects who were not registered with codes.
Conclusion
In conclusion, these and similar cost-of-illness studies reveal the economic burden that society has to bear when any member of society suffers from a disease. This will provide important evidence on how much of the scarce resources allocated to health care are spent on which diseases, how to prevent these diseases, and how to ensure efficiency through proper resource allocation. It is essential to ensure the continuity of studies. Diabetes mellitus causes significant disease burden and economic burden. For the management of the disease, patients can be followed up thanks to the e-Pulse system in Türkiye. By using this important resource, disease management can be achieved with correct and appropriate interventions, and complications can be prevented.
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Ethics Committee Approval: Anonymous data usage decision approval was provided by the Ministry of Health at the date of January 5, 2023. Approval number: E-95741342-708.01-206385672.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – Ş.B., B.S.M.; Design – Ş.B., B.S.M.; Supervision – Ş.B., B.S.M.; Resources – Ş.B., B.S.M.; Materials – Ş.B., B.S.M.; Data Collection and/or Processing – Ş.B., B.S.M.; Analysis and/or Interpretation – Ş.B., B.S.M.; Literature Search – Ş.B., B.S.M.; Writing – Ş.B., B.S.M.; Critical Review – Ş.B., B.S.M.
Declaration of Interests: The authors have no conflict of interest to declare.
References
- 1. Birinci Ş. A digital opportunity for patients to manage their health: Turkey national personal health record system (the e-Nabız). Balk Med J. 2023;40(3):215 221. ( 10.4274/balkanmedj.galenos.2023.2023-2-77) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Birinci Ş. An Example of Chronic Disease Management in Türkiye: Macrovascular Complication Due to Diabetes Mellitus [PhD thesis]. Istanbul: Üsküdar Üniversitesi; 2023. [Google Scholar]
- 3. International Diabetes Federation. IDF Diabetes Atlas. International Diabetes Federation; 2021. [Google Scholar]
- 4. SSI. Social security Incopration. Istanbul: Turk Uluslararası Diyabet Liderler Zirvesi. 2013. [Google Scholar]
- 5. Malhan S, Öksüz E, Babineaux SM, Ertekin A, Palmer JP. Assessment of the direct medical costs of type 2 diabetes mellitus and its complications in Turkey. Turk J Endocrinol Metab. 2014;18(2):39 43. ( 10.4274/tjem.2441) [DOI] [Google Scholar]
- 6. IQVIA. Improving Compliance and Continuity in Type 2 Diabetes Treatment in Turkey. IQVIA Institute; 2017. [Google Scholar]
- 7. Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in Type 2 diabetes: a systematic review. Value Health. 2018;21(7):881 890. ( 10.1016/j.jval.2017.12.019) [DOI] [PubMed] [Google Scholar]
- 8. National Diabetes Consensus Group. Diabetes Diagnosis and Treatment Guidelines. Istanbul: Türkiye Diabetes Foundation; 2019. [Google Scholar]
- 9. Rascati KL. Essentials of pharmacoeconomics. J Comm Biotechnol. 2009;15(1):92 94. [Google Scholar]
- 10. Cowley P, Bodabilla L, Musgrove P, Saxenian H. Content and Financing of an Essential National Package of Health Services, Global Assessments in the Health Sector. World Health Organization; 1994:171 181. [PMC free article] [PubMed] [Google Scholar]
- 11. Dijital sağlık: Başkalarından öğrenmek. deutschland.de. Available at: https://www.deutschland.de/tr/topic/bilim/dijital-saglik-hizmetleri-baska-ulkelerden-ogrenmek. (Published January 3, 2020). [Google Scholar]
- 12. Williams J, Malden S, Heeney C, et al. Optimizing hospital electronic prescribing systems: a systematic scoping review. J Patient Saf. 2022;18(2):e547 e562. ( 10.1097/PTS.0000000000000867) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yeaw J, Halinan S, Hines D, et al. Direct medical costs for complications among children and adults with diabetes in the US commercial payer setting. Appl Health Econ Health Policy. 2014;12(2):219 230. ( 10.1007/s40258-014-0086-9) [DOI] [PubMed] [Google Scholar]
- 14. Turner RC. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus progressive requirement for multiple therapies (UKPDS 49). JAMA. 1999;281(21):2005 2012. [DOI] [PubMed] [Google Scholar]
- 15. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837 853. ( 10.1016/S0140-6736(98)07019-6) [DOI] [PubMed] [Google Scholar]
- 16. Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977 986. ( 10.1056/NEJM199309303291401) [DOI] [PubMed] [Google Scholar]
- 17. Süleymanlar G, Utaş C, Arinsoy T, et al. A population-based survey of Chronic REnal disease in Turkey–the CREDIT study. Nephrol Dial Transplant. 2011;26(6):1862 1871. ( 10.1093/ndt/gfq656) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a