Abstract
Introduction:
Cognitive Behavioral Immersion (CBI) is a novel cognitive-behavioral skills program delivered by lay coaches in the metaverse through immersive virtual reality technology.
Objectives:
The objective for this study was to run a feasibility and pilot study of CBI for individuals in recovery from a substance use disorder.
Methods:
Data from 48 participants were used and program usage was assessed. Participants were asked to complete questionnaires assessing affect, perceived online social support, and group therapy alliance throughout their participation in the program. Structured qualitative interviews were also conducted with a subset of participants (n = 11) to understand the feasibility of the novel program.
Results:
Participants experienced a significant increase in their positive affect and non-significant decrease in their negative affect during their most recently attended session. Participants also experienced a nonsignificant increase in online social support across their participation in the program. Structured qualitative interviews revealed eight primary themes, including both advantages (community, psychoeducational impact, immersion, comparability with other interventions, coping in the pandemic, and anonymity) and areas of improvement (challenges and technological usability) of the program.
Conclusion:
This study provides preliminary support for the feasibility and potential effects of CBI and its incorporation of lay coaches to lead cognitive-behavioral skills groups in the metaverse. Future research is encouraged to examine the feasibility and efficacy of this program for a broader array of clinical presentations.
Keywords: Virtual reality, Cognitive behavioral therapy, Affect, Substance use disorders, Metaverse, Cognitive behavioral immersion
Introduction
Substance use disorders (SUDs) are a prevalent health problem and among the leading causes of mortality worldwide.1–3 Cognitive-behavioral therapy (CBT) is an efficacious intervention for SUDs.4–6 CBT for SUDs is designed to break the maladaptive cycle of substance use by targeting changes in thoughts, behaviors, feelings, and physiology within each person's environment. CBT aims to teach patients how to modify inaccurate beliefs about substance use, change behaviors that trigger cravings, develop healthier lower-risk strategies to reduce negative affect (NA), and engage in alternative healthy behaviors to boost positive affect (PA).
Additionally, therapy, particularly when conducted in group settings, can provide social support, which serves as a protective factor for the development and recurrence of SUDs.7,8 Despite its efficacy, CBT remains difficult to access, leaving many individuals with SUDs without a feasible intervention option. Fortunately, two pathways to increase the accessibility of evidence-based interventions have been accumulating evidence for their utility in recent years: the use of lay therapists and the use of gaming technology.
There is accumulating empirical support for the use of peer coaches who have little to no prior training or experience in mental health care (also known as lay therapists) to deliver effective psychological interventions.9 There is also evidence showing that peer coaches can be taught to deliver effective evidence-based interventions.10,11 In turn, the use of lay individuals to provide effective evidence-based interventions can increase the accessibility of these interventions by concurrently increasing their reach and decreasing their cost.10
Technology can also be leveraged to deliver accessible treatments. Digital mental health interventions have demonstrated outcomes comparable with traditional face-to-face interventions.12 While some forms of digital CBT treatments increase access by eliminating the need for therapists altogether, findings from a recent meta-analysis suggest that the efficacy and engagement in these digital programs are improved when provided with peer support.12
Serendipitously, a new digital modality, the metaverse, allows participants to interact as avatars through internet-connected environments. This allows for the opportunity to increase social support between participants and peers, which has been identified as key in the recovery and sustained recovery from SUDs.8
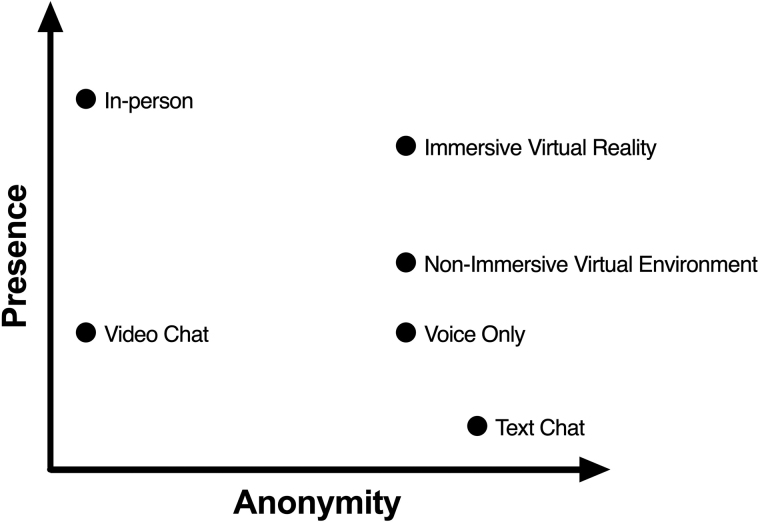
Virtual reality (VR) extends two-dimensional experiences in the metaverse by creating a truly immersive, three-dimensional social environment. VR is powerful because it facilitates a sense of presence, defined as the subjective experience of being in a place or environment when one is physically situated in another.13 Research suggests that virtual stimuli can elicit affective reactions much like real-life stimuli.13 Using VR for social interaction is unique compared with other modalities insofar as it can increase the sense of presence in an intervention (more than with a text chat, voice chat, or video chat) while also maintaining a complete sense of anonymity (more than an in-person or video chat meeting; Fig. 1).
FIG. 1.
Modalities of mental health services.
Individuals using VR to access interventions in the metaverse may feel safer to try new skills, open up with strangers and disclose vulnerabilities that may be more difficult to do in nonanonymous settings. In addition, VR allows an individual to “leave” the home environment and be transported into different environments. These novel environments can promote acquisition of cognitive-behavioral skills by changing the context of thoughts, feelings, behaviors, and physiology.
This Study
Historically, VR in the metaverse has been used to enhance gaming, and its feasibility to implement mental health interventions remains relatively unexplored. Cognitive Behavioral Immersion (CBI) is a novel approach (developed by Innerworld, Inc.) that incorporates cognitive-behavioral tools into an immersive massive multiplayer online (MMO) application called Innerworld (developed by Innerworld, Inc.).
The term “Immersion” was added to “cognitive behavioral” due to the unique property of immersive VR that allows an individual to be transported out of one's real environment into a carefully controlled virtual one that can be designed to facilitate cognitive-behavioral skill acquisition. We aimed to run a feasibility and pilot study of CBI for a sample of individuals using Innerworld who identified as being in recovery from SUDs.
To do so, we examined participants' engagement with the program, change in affect, and change in online social support during their CBI participation. We then conducted a qualitative analysis of participants' experiences with CBI.
Methods
Participants
The sample consisted of 48 individuals who self-reported being in recovery from an SUD. The modal participant was a White male, aged 30 to 39 years, with an annual average income of $50,000 to $74,999. Most participants indicated being in recovery from a primary alcohol use disorder (see Table 1 for a full list of demographic characteristics).
Table 1.
Demographic and Program Usage Variables
| Variable | n |
|---|---|
| Primary substance use disorder | |
| Alcohol | 22 |
| Cannabis | 2 |
| Narcotics | 8 |
| Stimulants | 5 |
| Tranquilizers | 2 |
| Other | 2 |
| Chose to not answer | 1 |
| More than one | 6 |
| Age, years | |
| 21–29 | 6 |
| 30–39 | 18 |
| 40–49 | 11 |
| 50–59 | 6 |
| 60–69 | 6 |
| 70+ | 1 |
| Gender | |
| Female | 8 |
| Male | 36 |
| Other | 3 |
| Chose to not answer | 1 |
| Race | |
| Asian | 3 |
| Black or African American | 4 |
| White | 38 |
| Other | 1 |
| Chose to not answer | 2 |
| Income | |
| <$20,000 | 12 |
| $20,000–$49,999 | 3 |
| $50,000–$74,999 | 17 |
| $75,000 or more | 16 |
Program and application
CBI was delivered on a gamified metaverse application called “Innerworld” (developed by Innerworld, Inc.). Innerworld acquired participants through a variety of channels, including marketing and blog posts. All Innerworld participants consented to data sharing through the terms of service and privacy policy, in addition to a pop-up prompt in the tutorial that informed participants that the Innerworld application is a research platform. If participants did not agree to this prompt, they would not be able to participate in Innerworld.
All quantitative and qualitative data were collected by Innerworld, Inc. Innerworld, Inc. designed the application to administer self-report measures, including demographic information, recovery status, mood, and social belonging. Innerworld, Inc., personnel conducted qualitative interviews with participants in the Innerworld application and then transcribed the interviews. Deidentified data were then passed to Vanderbilt University researchers for the purpose of quality improvement, as determined by Vanderbilt University's Institutional Review Board (No. 200327).
Participants connected to the application with an Oculus Quest VR headset and handheld controllers. Participants depicted themselves through customizable avatars with anonymous usernames while communicating through a microphone on the headset. Participants could observe other participants' avatars, body movements, and voices. The core game loop of Innerworld is social interaction—each time a participant enters Innerworld, there is a list of upcoming mental health events (e.g., check-in groups and topic-focused meetings) and recreational events (e.g., drawing games, chess tournaments, charades) displayed on a bulletin board.
Participant name tags were displayed alongside a leveling system that indicated the account age of participants. Innerworld provides an introductory tutorial to teach individuals how to navigate the application. In addition, it also requires individuals to answer screening questions before being able to interact with others (including information regarding informed consent about data collection, risk of being identified in the application, notice that the intervention was neither therapy nor crisis intervention, and requirement for individuals to read the community guidelines regarding courtesy to others and keeping discussions confidential).
Coaches who facilitated CBI groups participated in at least 18 hours of training on basic therapy skills, cognitive-behavioral principles and skills, and management of difficult situations. Cognitive skills taught included identifying the connections between thoughts, feelings, physiology, and behaviors; identifying and examining negative automatic thoughts; and identifying common cognitive distortions. Behavioral strategies taught included activity scheduling, behavioral monitoring, problem solving, assertion training, and assigning homework.
As is standard practice in conventional CBT, coaches set agendas for each group, but had the flexibility to adjust content to meet groups' needs. Coaches also attended ongoing hour-long weekly group consultation/supervision meetings. Coaches came from a variety of backgrounds, including undergraduate students at Vanderbilt University, retired folks, and people with other careers. None of the coaches had formal training or background in health or therapy.
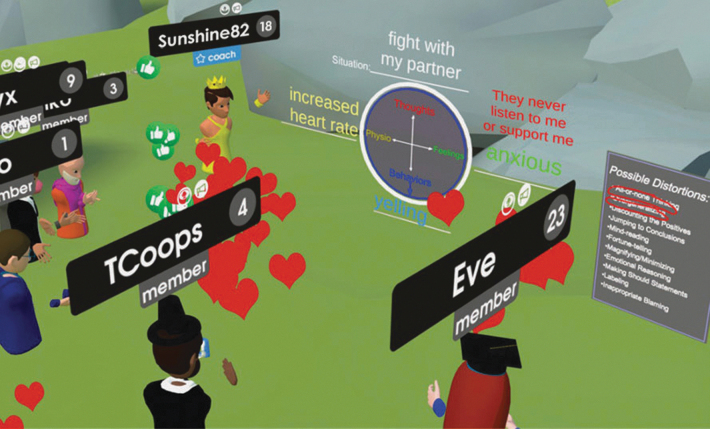
CBI sessions were held daily at different times each day. A calendar of sessions was made publicly available in the Innerworld application at all times, and participants were encouraged to attend whichever and however many sessions they would like. Coaches led as many sessions as fit into their own personal schedules, and participants need not only attend sessions offered by the same coach. Each session lasted ∼60 minutes. The CBI sessions began with a check-in during which each participant had the opportunity to share a recent challenge and success, followed by introduction and discussion of a CBT-based skill (e.g., psychoeducation, cognitive skill, behavioral skill) (see Fig. 2 for a screenshot of a CBI session).
FIG. 2.
Screenshot of a Cognitive Behavioral Immersion session with a coach teaching the cognitive-behavioral model as members react with emojis.
Measures
Net promoter score
The net promoter score14 (NPS) is a highly utilized one-item measure of participant satisfaction that assesses the likelihood a participant would recommend the program to a friend.
Each score is measured on an 11-point Likert scale. Scores of 0 to 6 indicate participants who are unlikely to recommend, or may even discourage, others from using the program (called “detractors”). A score of 7 or 8 indicates participants who are satisfied with the program, but not happy enough to recommend to others (called “passives”). A score of 9 or 10 indicates loyal and enthusiastic participants who are likely to recommend the program to others (called “promoters”). The NPS is calculated by subtracting the percentage of detractors from the percentage of promoters.
Positive and negative affect schedule
The positive and negative affect schedule (PANAS) is a 20-item self-report questionnaire that assesses PA and NA.15 Each item is rated on five-point scales. PA and NA scores were averaged across their corresponding items. Higher scores indicated greater levels of the respective affect. The PANAS has demonstrated acceptable reliability and validity.15 Participants completed the PANAS before and after each session they attended.
Online social support scale
The online social support scale (OSSS) is a 40-item scale that measures the online occurrence of the four dimensions of social support: esteem/emotional support, social companionship, informational support, and instrumental support.16 We removed the 10 items assessing instrumental support since this type of support was neither relevant nor likely due to the anonymity of the intervention. We also removed one item that did not apply to the program (“I get likes, favorites, upvotes, views, etc., online”).
Items are assessed on five-point scales. Scores were summed across items. Higher scores reflected greater online social support. The OSSS has demonstrated evidence of reliability and validity.16 Participants completed the OSSS once per month.
Qualitative interviews
Structured interviews were conducted with a subset (n = 11) of participants who volunteered to be interviewed about their experiences. A group of four volunteer Innerworld coaches, who also happened to be undergraduate students at Vanderbilt University, conducted the interviews on behalf of Innerworld, Inc. No incentive was provided. Each participant completed two interviews scheduled ∼3 weeks apart.
The first interview (Supplementary Appendix SA1) explored the participants' prior experience with VR and other behavioral interventions. This interview also explored participants' initial impressions of CBI. The second interview (Supplementary Appendix SA2) explored participants' desire to continue attending CBI, negative experiences with CBI, and comparison of CBI with other behavioral interventions and telehealth platforms.
While the interviews were based on a structured list of questions, participants were encouraged to bring up anything they desired, letting them create their own narrative of their experiences. Interviews were conducted through Zoom audio and lasted ∼20 minutes. Once completed, interviews were transcribed and identifying information removed.
Data analyses
Since participants had flexibility in the number of sessions they could attend, participants varied in the number of sessions they attended as well as the number of measures they completed. Therefore, we conducted paired-sample t-tests to examine changes on the PANAS, from pre- to postsession, during participant's most recently attended CBI session. We examined changes in both PA and NA. We then conducted paired-sample t-tests to examine changes from participants' first to most recent OSSS scores during their total time of attending VR sessions. We calculated effect sizes using Hedges' g.
The interview transcripts were analyzed using a thematic analysis, a widely used method that concisely identifies, analyzes, and reports patterns in large amounts of qualitative data.17 We conducted the thematic analysis using an inductive approach, in which the process was data driven without any attempt to fit themes into a pre-existing framework.17
Four individuals (Innerworld volunteer coaches) read through all the transcripts. Then, this team had discussion meetings in which they jointly generated relevant themes, identified theme occurrences in each interview transcript, and created clear definitions for each theme. Under each theme, the team jointly developed subthemes that emerged from the data and identified their occurrences in the data.
After this process was finished, the team met and jointly decided which themes were most relevant to and reflective of the data. This decision was influenced by the number of times a theme occurred in the data as well as their own agreement on which were most important.
Results
Engagement
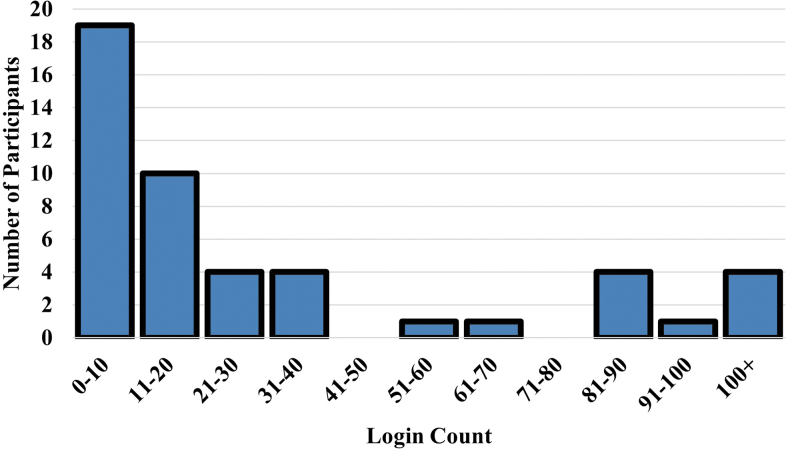
Participants spent an average of 19.34 hours (standard deviation [SD] = 43.96; range = 0.40–291.00) on the CBI platform across an average of 41.52 logins. See Figure 3 for a histogram of login counts. These logins were spread across an average of 12.54 weeks (SD = 14.31, range = 2–52). The NPS was 66.67, indicating a participant satisfaction score in the excellent range.
FIG. 3.
Histogram of login counts.
Changes in affect
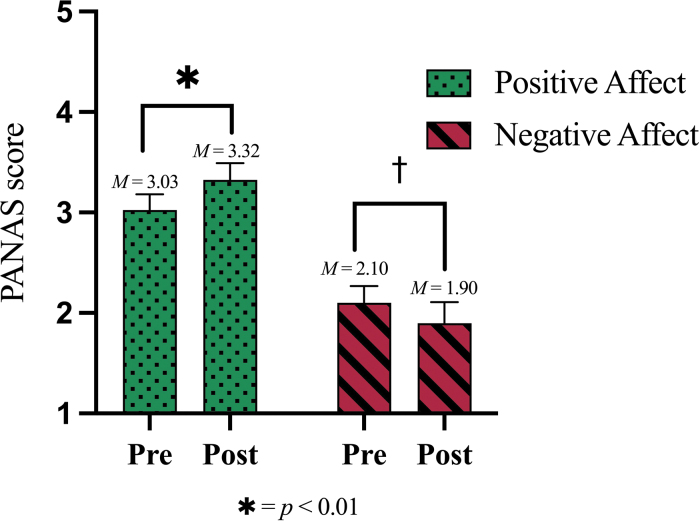
Twenty participants completed the PANAS during their most recent session. We found a significant increase in PA from pre- (M = 3.03, SD = 0.70) to postsession (M = 3.32, SD = 0.75), t(19) = 2.76, P = 0.01, g = 0.31. We did not find a significant decrease in NA from pre- (M = 2.10, SD = 0.75) to postsession (M = 1.90, SD = 0.93), t(19) = −1.77, P = 0.09, g = 0.08 (see Fig. 4 for a graphical depiction of these results). Effect sizes and mean differences for the PANAS are reported in Table 2.
FIG. 4.
Changes in affect from pre- to postsession. PANAS, positive and negative affect schedule.
Table 2.
Change in Positive and Negative Affect Schedule Total and Item Scores from Pre- to Postsession
| Valence | Emotion | M (difference) | t-value | g |
|---|---|---|---|---|
| + | Positive affect | 0.30* | 2.76 | 0.31 |
| − | Negative affect | −0.20** | −1.77 | 0.08 |
P < 0.05 and **P < 0.10.
Change in online social support
Twenty participants provided at least two OSSS ratings. We did not find a significant difference from participants' first OSSS rating (M = 106.35, SD = 24.80) to the most recent OSSS rating (M = 110.80, SD = 28.73), t(19) = 0.47, P = 0.64. g = 0.17. An exploration of the OSSS subscales did not reveal any significant differences from participants' first rating to the most recent rating (all Ps > 0.27).
Qualitative analysis
Eight major themes emerged from the qualitative interviews: technological usability, community, comparison with other behavioral interventions, psychological/psychoeducational impact, challenges, immersion, anonymity, and pandemic (Table 3).
Table 3.
First Set of Major Themes from the Qualitative Analysis
| Theme | Definition and subthemes | Frequencya | Examples |
|---|---|---|---|
| Technological usability | How the use of a VR headset and controllers impacts participants' experiences | 50; 11 | “I'm still trying to figure it all out. I'm still trying to get comfortable with the technology.” “I really like that you can join anywhere…it was two weeks ago I just got off work and I ran to the store…my husband had picked me up and I was doing a class in my car…I really like that.” |
| Community | Feeling of fellowship with others because of sharing common attitudes, interests, and goals | 53; 11 | “My mom got a diagnosis of Alzheimer's’…being able to talk about it and knowing that people have also experienced it and worked through it has been helpful, but more it's really having a place to bring it.” “That is one of the really fun things about VR…that there's this huge cultural and geographic mix of people, which I really enjoy that a lot.” |
| Comparison with other interventions or platforms | Comparisons of VR recovery sessions with any mental health intervention or telehealth platform | 41; 11 | “I love the immersion factor of it, just being in the actual app as opposed to a Zoom kind of meeting” “So, if [Innerworld] can move beyond just meetings to recreating, you know building a broader social world for myself then it can be a much bigger part of my life. Right now, it's a replacement for the group meetings I'm doing several times a week, but it could move up from that.” |
| Psychological/psychoeducational impact | The impact of VR recovery sessions on mental well-being and ability to retain tools | 33; 11 | “For the first time outside of [Innerworld], I took the cognitive behavioral model and put it up on a white board and took a thing I was dealing with and worked it through the model on my own…I was like oh that was super helpful!” “What happens for me is I always feel more motivated, more engaged, less frustrated, less anxious, less distressed.” |
| Challenges | Negative experiences and difficulties with VR recovery sessions | 32; 10 | “I'll have like some glitch tech issue stuff where I'll get locked into that spawning room.” “Like accidentally grabbing someone else's chair and moving it when I'm not even looking at it… and I'm like ‘oh I didn't want to do that’…when I was in early recovery, you know attention and things are sort of harder to direct…that [may] be problematic for people.” |
| Anonymity | Impact of being unidentifiable in recovery sessions | 21; 10 | “I literally don't need to hold back on anything…I don't even have to stay focused on the “am I actually being honest right now” - I can just let stuff out.” “Nobody makes an immediate judgment just based on age or where you come from.” |
| Immersion | Feeling of being placed in a different alternate environment | 28; 8 | “When I'm in those meetings I don't feel like I'm where I am like if I'm in a bedroom or a living room; I feel very transported.” “I do get the sense that I am in a physical space with somebody else.” |
| Pandemic | Mentioning the COVID-19 pandemic in relation to VR recovery sessions | 8; 6 | “It was nice to be able to hear that other people were having similar issues and…what worked with them…which I needed a lot, especially during this pandemic.” “I'm currently feeling the effects of this long-standing shelter in place, so the connection is welcome.” |
Frequency values are reported as the number of times mentioned (a given participant could mention a specific theme more than once); number of participants who mentioned (of n = 11 participants). Detailed descriptions of subthemes and an abundance of relevant quotes can be found in Supplementary Appendix SA3.
VR, virtual reality.
Theme 1: Technological usability
All 11 participants noted how the technological usability of VR equipment impacted their experience (50 comments). Of these comments, 8 participants mentioned difficulty navigating VR for the first time (18 comments). Five participants experienced negative physiological impacts (e.g., nausea, headaches) associated with using VR for the first time (7 comments).
Four participants reported that a desktop experience allowed them to understand what a virtual meeting looked like, while a VR experience provided a more immersive engaging experience (8 comments). Eight participants mentioned how aspects of the user interface experience, particularly those surrounding the lack of visual social cues, negatively impacted the virtual experience (11 comments). Four participants described how the accessibility of the application allowed them to attend more meetings (6 comments).
Theme 2: Community
All 11 participants experienced a feeling of fellowship, namely sharing common attitudes, interests, and goals, during sessions (53 comments). Participants described valuing the sense of community through shared experiences and emotional connections they built with others in the program (30 comments). Six participants reported valuing the online community due to the rich diversity of members in geographical location, experience, and age (23 comments).
Theme 3: Comparison with other interventions/platforms
All 11 participants compared CBI with other behavioral mental health interventions or telehealth platforms (41 comments). Nine participants reported CBI being generally different from any other platform or intervention they had previously experienced and that the virtual experience was a promising future direction as a modality for the provision of recovery groups (17 comments). Five participants described CBI as a recovery intervention that could be part of their own or someone else's recovery process from SUDs (9 comments).
The consensus among participants was that CBI could be helpful as a supplemental resource to someone's recovery journey. Six participants mentioned similarities between CBI and traditional in-person recovery meetings (6 comments). Four participants mentioned differences between CBI and telehealth platforms such as Zoom (9 comments), often highlighting how the immersive nature of VR facilitated a sense of presence with others versus video chat platforms such as Zoom that did not lead to a sense of being in the same room with other people.
Theme 4: Psychological and psychoeducational impact
Eleven participants noted the impact of CBI on their own psychological well-being (33 comments). Seven participants reported experiencing positive emotions from CBI (18 comments), while three participants reported experiencing a negative psychological impact from CBI, particularly from hearing others' struggles (3 comments). Four participants reported experiencing psychoeducational benefits, such as real-life applications of CBT-based tools (6 comments). Five participants reported being able to interact with psychoeducational tools through drawing and typing abilities offered in CBI (6 comments).
Theme 5: Challenges
Overall, 10 participants spoke about the challenges of CBI (26 comments). Eight participants reported experiencing time conflicts with obligations, such as work and other support groups (10 comments). Four participants mentioned shortcomings of the meeting structure, such as timing issues and frustrations with the initial check-in format (8 comments). Four participants mentioned technological challenges, such as general glitches and having to troubleshoot the program (5 comments). Two participants mentioned challenges specific to VR technology, such as accidentally grabbing things online (3 comments).
Theme 6: Anonymity
Ten participants noted how being completely unidentifiable positively impacted their virtual experience (21 comments). These participants mentioned how they appreciated anonymity due to the freedom of self-expression and lack of judgment that it provided.
Theme 7: Immersion
Eight participants made 28 comments regarding being placed in a different environment and its effect on their experience. Five participants reported feeling their own physical presence along with others, which facilitated an experience of virtual interaction (9 comments). Four participants described feeling like they were escaping to an alternate reality when entering CBI, which they felt was helpful (10 comments). Five participants reported the immersive environments as a source of engagement during meetings (9 comments).
Theme 8: Pandemic
Six participants mentioned the COVID-19 pandemic in relation to their experiences with virtual meetings (8 comments). Five participants reported that the pandemic had negative implications on people's lives and ability to connect socially (5 comments). Two participants described valuing the online community during the period of isolation caused by the pandemic (3 comments).
Discussion
This study was the first to examine a cognitive-behavioral skills coaching program delivered in the metaverse. Through a mixed-methods approach, this pilot study provided insight into the feasibility and potential effects of this intervention. Participants appeared to find the platform usable, spending an average of ∼20 hours in the intervention across an average of 41 logins. We observed a significant increase in PA and a nonsignificant decrease in NA across the course of participants' most recent CBI session.
More than half of the participants interviewed reported feeling a positive psychological impact from attending CBI sessions. Most participants reported feeling more relaxed and motivated after attending meetings. Data from this study suggests that CBI demonstrates feasibility and could be a viable method to promote affective regulation and social support for individuals with SUDs. This is especially important for individuals in recovery who are at greater risk for relapsing due to affective changes and social isolation.
Our results also suggest that attendance at CBI sessions was associated with a high level of perceived social support. While we did not observe significant changes in online social support from participant's first to most recent attended CBI session, we found that mean online social support scores at both time points were higher than those found in members of MMO role-playing games.18 This adds to the support for the feasibility of CBI insofar as it can provide an engaging experience that is like other popular online videogames that are used by millions of people.
A key difference between CBI and other videogames, however, is that CBI is designed to facilitate acquisition of cognitive-behavioral skills rather than simply entertain the participant. Perhaps one reason we did not find a significant increase in online social support scores was participants immediately feeling a high level of online social support during their first CBI sessions and subsequently reaching a ceiling effect with our measure. Relatedly, every interviewee reported experiencing a strong sense of community.
Almost every interviewee mentioned the ability to engage in open honest discourse while being completely unidentifiable, thus allowing for emotional connections and a deep sense of community to spontaneously grow. Participants also noted valuing the ability to form strong social connections with virtually anyone from any place. These findings suggest that involvement in CBI is associated with a positively perceived level of social support.
Individuals also reported some challenges with the platform. These included technological usability (learning how to navigate the VR platform), negative physiological side effects (nausea and headaches), timing issues of meetings, and bugs in the software. These comments provide several avenues for improvement. For example, a more robust tutorial could teach users how to turn off the “smooth locomotion” mode (which can cause nausea) and instead enable the “teleport” mode.
Limitations
First, the lack of a control group precludes drawing any causal inferences about the changes we observed. Second, the self-selected recruitment of participants may have influenced the range of qualitative experiences reported. For example, it is likely that most self-selected participants had some prior interest in learning to use VR, and it is not clear that others would share that motivation.
Third, participants also self-reported being in recovery from an SUD, and future research could benefit from a more reliable assessment of SUDs through a diagnostic interview. Relatedly, future studies exploring the impact of CBI on SUDs could include additional measures to assess SUD-specific symptoms such as cravings.
Fourth, since there was no limitation to the number of sessions attended by participants, different participants may have received different “doses” of this intervention. Future research could explore how the extent of engagement in the intervention may predict differential outcomes.
Last, a larger and more diverse sample is needed to aid with the study's generalizability. It will also be important to assess additional factors related to feasibility (e.g., acceptability, commitment to the program) and efficacy (e.g., symptoms) as well as participant factors that may predict engagement outcomes in metaverse mental health interventions (e.g., age, prior therapy experience).
Conclusions
This study showed preliminary support for the feasibility of using trained peer coaches to lead cognitive-behavioral skills groups in the metaverse. We observed changes in affect, positive levels of social support, and general psychological/psychoeducational benefits for individuals in recovery from SUDs. We have also gained insight into how to improve and advance the potential benefits of disseminating VR mental health interventions in the metaverse.
Since the conclusion of this pilot study, over 80,000 people have downloaded Innerworld, and a substantial number of these participants have endorsed clinical levels of depression or anxiety symptoms. We recommend that future studies conduct randomized controlled trials to determine whether the platform has a beneficial causal impact on a variety of clinical presentations.
Supplementary Material
Authors' Contributions
Noah Robinson contributed to conceptualization, funding acquisition, investigation, methodology, and writing. Iony D. Ezawa contributed to conceptualization, data curation, formal analysis, methodology, supervision, and writing. Steven D. Hollon contributed to conceptualization and supervision. Anjali Mahapatra, Brianna Jean-Baptiste, Austin Mallard, and Aaron Yang contributed to investigation.
Author Disclosure Statement
Noah Robinson is the CEO of Innerworld, Inc., the company that developed the Innerworld platform. No other competing financial interests exist.
Funding Information
This work was supported, in part, by a National Institute of Mental Health Training Grant (T32 MH018921) and the National Institute on Drug Abuse (R41 DA051294-01).
Supplementary Material
References
- 1. Drug Overdose Deaths in the U.S. Top 100,000 Annually. Published November 17, 2021. Available from: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm [Last accessed: January 15, 2022].
- 2. Merikangas KR, McClair VL. Epidemiology of substance use disorders. Hum Genet 2012;131(6):779–789; doi: 10.1007/s00439-012-1168-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. 2017 WHO Forum on Alcohol, Drugs and Addictive Behaviours. 2017. Available from: www.who.int/substance_abuse/activities/fadab/event/en/ [Last accessed: October 31, 2022].
- 4. Magill M, Ray LA. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. J Stud Alcohol Drugs 2009;70(4):516–527; doi: 10.15288/jsad.2009.70.516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McHugh RK, Hearon BA, Otto MW. Cognitive behavioral therapy for substance use disorders. Psychiatr Clin 2010;33(3):511–525; doi: 10.1016/j.psc.2010.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zamboni L, Centoni F, Fusina F, et al. The effectiveness of cognitive behavioral therapy techniques for the treatment of substance use disorders: A narrative review of evidence. J Nervous Mental Dis 2021;209(11):835–845. [DOI] [PubMed] [Google Scholar]
- 7. Gifford E, Humphreys K. The psychological science of addiction. Addiction 2007;102(3):352–361; doi: 10.1111/j.1360-0443.2006.01706.x [DOI] [PubMed] [Google Scholar]
- 8. Tracy K, Wallace S. Benefits of peer support groups in the treatment of addiction. Subst Abuse Rehabil 2016;7:143–154; doi: 10.2147/SAR.S81535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van Ginneken N, Tharyan P, Lewin S, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low-and middle-income countries. Cochrane Database Syst Rev 2013;11:CD009149; doi: 10.1002/14651858.CD009149.pub2 [DOI] [PubMed] [Google Scholar]
- 10. Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: Lessons from developing countries. Behav Res Therapy 2011;49(9):523–528; doi: 10.1016/j.brat.2011.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel V, Weobong B, Weiss HA, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: A randomised controlled trial. Lancet 2017;389(10065):176–185; doi: 10.1016/S0140-6736(16)31589-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karyotaki E, Efthimiou O, Miguel C, et al. Internet-based cognitive behavioral therapy for depression: A systematic review and individual patient data network meta-analysis. JAMA Psychiatry 2021;78(4):361–371; doi: 10.1001/jamapsychiatry.2020.4364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Witmer BG, Singer MJ. Measuring presence in virtual environments: A presence questionnaire. Presence Teleoperators Virtual Environ 1998;7(3):225–240; doi: 10.1162/105474698565686 [DOI] [Google Scholar]
- 14. Reichheld FF. The one number you need to grow. Harvard Business Rev 2003;81(12):46–55. [PubMed] [Google Scholar]
- 15. Watson D, Anna L, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol 1988;54(6):1063–1070. [DOI] [PubMed] [Google Scholar]
- 16. Nick EA, Cole DA, Cho SJ, et al. The Online Social Support Scale: Measure development and validation. Psychol Assess 2018;30(9):1127–1143; doi: 10.1037/pas0000558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77–101; doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 18. Cole DA, Nick EA, Pulliam KA. Are Massively Multiplayer Online Role-Playing Games healthy or not and why? Preliminary support for a Compensatory Social Interaction model. Comput Hum Behav 2020;102:57–66; doi: 10.1016/j.chb.2019.08.012 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.