Abstract
Traumatic brain injury (TBI) is a global public health problem and a leading cause of mortality, morbidity, and disability. The increasing incidence combined with the heterogeneity and complexity of TBI will inevitably place a substantial burden on health systems. These findings emphasize the importance of obtaining accurate and timely insights into healthcare consumption and costs on a multi-national scale. This study aimed to describe intramural healthcare consumption and costs across the full spectrum of TBI in Europe. The Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) core study is a prospective observational study conducted in 18 countries across Europe and in Israel. The baseline Glasgow Coma Scale (GCS) was used to differentiate patients by brain injury severity in mild (GCS 13–15), moderate (GCS 9–12), or severe (GCS ≤8) TBI. We analyzed seven main cost categories: pre-hospital care, hospital admission, surgical interventions, imaging, laboratory, blood products, and rehabilitation. Costs were estimated based on Dutch reference prices and converted to country-specific unit prices using gross domestic product (GDP)-purchasing power parity (PPP) adjustment. Mixed linear regression was used to identify between-country differences in length of stay (LOS), as a parameter of healthcare consumption. Mixed generalized linear models with gamma distribution and log link function quantified associations of patient characteristics with higher total costs. We included 4349 patients, of whom 2854 (66%) had mild, 371 (9%) had moderate, and 962 (22%) had severe TBI. Hospitalization accounted for the largest part of the intramural consumption and costs (60%). In the total study population, the mean LOS was 5.1 days at the intensive care unit (ICU) and 6.3 days at the ward. For mild, moderate, and severe TBI, mean LOS was, respectively, 1.8, 8.9, and 13.5 days at the ICU and 4.5, 10.1, and 10.3 days at the ward. Other large contributors to the total costs were rehabilitation (19%) and intracranial surgeries (8%). Total costs increased with higher age and greater trauma severity (mild; €3,800 [IQR €1,400–14,000], moderate; €37,800 [IQR €14,900–€74,200], severe; €60,400 [IQR €24,400–€112,700]). The adjusted analysis showed that female patients had lower costs than male patients (odds ratio (OR) 0.80 [CI 0.75–1.85]). Increasing TBI severity was associated with higher costs, OR 1.46 (confidence interval [CI] 1.31–1.63) and OR 1.67 [CI 1.52–1.84] for moderate and severe patients, respectively. A worse pre-morbid overall health state, increasing age and more severe systemic trauma, expressed in the Injury Severity Score (ISS), were also significantly associated with higher costs. Intramural costs of TBI are significant and are profoundly driven by hospitalization. Costs increased with trauma severity and age, and male patients incurred higher costs. Reducing LOS could be targeted with advanced care planning, in order to provide cost-effective care.
Keywords: healthcare consumption, healthcare costs, hospital costs, traumatic brain injury;
Introduction
Each year, ∼1,500,000 people with traumatic brain injury (TBI) are hospitalized in the European Union, and ∼57 000 die as a result of a TBI, translating on average into 287 hospital admissions and ∼12 deaths per 100 000 inhabitants.1,2 The population-based incidence that includes those injuries that are not treated at hospitals can even be as high as 790 per 100,000.3 The incidence of TBI may further increase in the future, mainly driven by an increasing incidence of falls within the growing elderly population in most high-income countries, and the increasing number of road traffic incidents in low-to-middle-income countries where the implementation and effectiveness of preventative measures are outpaced by the rapid increase in motorization.4–7 The increasing number of cases combined with the heterogeneity and complexity of TBI will inevitably put a substantial burden on health systems, as the consumption of specialized acute care and long-term rehabilitation or chronic care will concomitantly increase.1,8
The healthcare costs of TBI, driven by cost prices and the healthcare consumption of patients, will cause major economic and societal challenges, as estimates indicate the worldwide annual economic burden of TBI to be US $400 billion dollars, which is ∼0.5% of the gross world product.1,9–11 This is of concern, as the associated increase of costs occurs at a time when there is a global shortage in healthcare personnel, healthcare spending budgets are under pressure, and justification of healthcare expenses will become increasingly important.12–15 It is therefore essential to obtain accurate and timely insight into healthcare consumption after TBI, and the cost effectiveness of TBI treatments, to optimize future allocation of restricted healthcare budgets.16 In view of these trends, cost studies have gained more importance, as measurement of healthcare consumption and accompanied costs serves as a fundament for improvement of access to and delivery of healthcare and for identification of potential savings.1,2,8,17
Published studies report in-hospital costs of patients with TBI to range from $3,079 to $7,800 (€2,721–6,893) for mild TBI patients16,18–21 and from $2,130 to $401,808 (€1,882–355,117) for severe TBI patients.17 Hospital costs increase with higher TBI severity and are mostly driven by the length of stay at the hospital.16–21 Unfortunately, the interpretation, comparability, and generalizability of these study results are difficult and limited. Most available research on costs after TBI frequently suffers from major methodological heterogeneity and inadequate quality, and is commonly restricted to one TBI severity level. Additionally, implementation of clinical guideline recommendations and personnel costs differ across hospitals and countries, resulting in different treatment practices and cost patterns.9,10,16,22 As measurement of healthcare consumption and costs after TBI differs among countries, researchers usually assess strictly local or national expenses, which limits the understanding and possibility of comparisons on a multi-national scale. In order to address these shortcomings, this study aimed to provide a detailed overview of intramural healthcare consumption and healthcare costs arising from hospital admission and inpatient rehabilitation, across the full spectrum of TBI in Europe.
Methods
Study design and patients
The Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) core study is a prospective longitudinal non-randomized observational study, registered at clinicaltrials.gov NCT02210221, which included patients with TBI from 18 countries across Europe and in Israel between 2014 and 2017. Inclusion criteria were: (1) a clinical diagnosis of TBI, (2) a clinical indication for a computed tomographic (CT) scan, (3) presentation within 24 h of injury, and (4) informed consent obtained according to local and national policies. Patients were excluded if they had a severe pre-existing neurological disorder that would confound outcome assessments. For this particular study, patients from Israel and those <16 years of age were excluded. Ethical approval for the CENTER-TBI study was obtained from all responsible medical ethical committees, and informed consent procedures followed applicable regulations.23
Clinical data
Clinical data were prospectively collected by local research staff using electronic case report forms (eCRF). Data were de-identified using a randomly generated Global Unique Patient Identifier (GUPI) and stored on a secured database by the International Neuroinformatics Coordinating Facility (INCF) (www.incf.org) in Stockholm, Sweden. Data were extracted in January 2021 (version 3.1) and included demographic characteristics, trauma and injury information, results of neurological assessment, imaging, and patient outcomes. Using the baseline Glasgow Coma Scale (GCS) score, patients were classified into three categories of TBI severity: GCS 13–15 (mild TBI), GCS 9–12 (moderate TBI), and GCS 3–8 (severe TBI).24 The baseline GCS score is a derived variable and represents the total GCS score for baseline risk adjustment. The systemic injury severity score (ISS) was categorized into three groups: ISS ≤16 (minor injury), ISS 17–25 (major injury), and ISS >25 (critical injury).25 Pre-injury health status was classified using the American Society of Anesthesiologists (ASA) physical status classification.26 Brain injury is further described according to the Abbreviated Injury Scale (AIS) and classified as minor, moderate, serious, severe, critical, or unsurvivable.27
Healthcare consumption
Healthcare consumption data were extracted following the same procedure as with clinical data. The healthcare consumption of patients included seven main healthcare service categories: (1) pre-hospital care, including ambulance transportation and, for secondary referral patients, costs of TBI-related admission and any emergent surgical interventions in the “referring hospital,” before admission to a CENTER-TBI study hospital; (2) hospital admission, including initial assessment and care at the emergency room (ER) and length of stay (LOS) in days at the ward or ICU; (3) all surgical interventions, both intra- and extra-cranial; (4) imaging of the brain; (5) laboratory; (6) blood products; and (7) rehabilitation; including only LOS at an inpatient rehabilitation center. Healthcare consumption of outpatient rehabilitation care facilities was not included. The transitions of care forms, in which the care pathway of patients was registered, were used to extract the in-hospital LOS of patients. Inpatient rehabilitation LOS was extracted using the transitions of care forms and patient-reported outcome forms. Missing LOS at the ward, ICU, and rehabilitation were imputed using single imputation. All healthcare services registered within CENTER-TBI and included in this study are reported in Supplementary Table S1.
Healthcare costs
Because of the unavailability of country-specific unit prices for each healthcare service, Dutch reference prices were used as fundament for this study. In addition, definitions, calculations, and sources of country-specific unit prices may vary (e.g., unit prices can differ based on the inclusion/exclusion of personnel costs), which could potentially lead to an over- or underestimation of costs when such unit prices are used. For example, it was found that the reported monthly salary for a senior resident ranged from a low between €500 and €800 in Eastern Europe to a high of €7900 in Norway.28 By using a uniform price list, this study focuses on differences in healthcare consumption rather than price differences among countries.
Reference prices were extracted from the Dutch Guidelines for economic healthcare evaluations.29 Reference prices not mentioned in the Dutch Guidelines were complemented using unit prices reported by the Netherlands Healthcare Authority or by using the average national price, based on declared fees30,31 (Supplementary Table S1). First, using the Dutch national general consumer price index, all reference prices were corrected to EURO 2017, the last year of patient inclusion (Supplementary Table S2).32 Second, in order to calculate the economic burden of a patient with TBI within Europe, the Dutch reference prices were converted to country-specific unit prices by correcting the Dutch reference prices for the purchasing power parity (PPP) for the general domestic product (GDP) (Supplementary Table S3). The GDP-PPP is the standard measure when comparing differences in life standards among countries.33
Third, the total intramural healthcare costs were calculated by multiplying the number of healthcare units (e.g. length of days at ward and ICU for hospitalization costs) with the corresponding reference price, according to country of admission. See Supplemental Methods, Supplementary Tables S2 and S3 for further details about the calculations.
Statistical analysis
Data were analyzed using descriptive statistics. Baseline characteristics of patients are based on crude data and presented as absolute numbers and percentages. Continuous variables are presented as medians (interquartile range [IQR]) and means (standard deviation [SD]). Median and mean prices were rounded to hundreds. To compare continuous and categorical variables across all subgroups, the Kruskal–Wallis test and the χ2 test were applied respectively. A p value <0.05 was considered statistically significant. Healthcare consumption (i.e., LOS at ICU, ward, and rehabilitation unit) and total healthcare costs were presented for the total study population, including all severities, and according to TBI severity.
Missing data were statistically imputed based on correlations among baseline characteristics, healthcare consumption, in-hospital mortality, and Glasgow Outcome Scale Extended (GOSE) score at 6 months using the mice package in R.34 To determine between-country differences in ICU and ward LOS, a mixed linear regression model was applied, with results presented in forest plots. The country effect was included in the model as a random intercept, and case-mix adjustment was performed using variables in the International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) prognostic model: age, pupils, GCS score, hypoxia, hypotension, traumatic subarachnoid hemorrhage, epidural hemorrhage, Marshall CT classification, hemoglobin, and glucose measurements.35 Countries including fewer than five patients per severity group were excluded from this analysis.
We used a mixed general linear model (GLM) with gamma distribution and log link function to determine which baseline characteristics were associated with the total intramural healthcare costs. GLM models are recommended for use in linear regression of costs data, as they provide parametric methods of analysis in which non-normal distributions can be specified.36 A random effect for country was added to both the univariable and multi-variable models to account for between-country differences in costs. Statistical analysis were performed in STATA and R version 4.0.4.37,38
Results
Patient population
After exclusion of patients from Israel and those <16 years of age, a total of 4349 out of 4509 CENTER-TBI patients were included in this study. Patients were mostly male (67%), with a median age of 51 years (IQR 32–67). Of the total population, 27% were ≥65 years of age (Table 1). A total of 457 patients (11%), had severe systemic disease, of whom 291 (64%), were ≥65 years of age. The most common causes of TBI were falls (45%), road traffic incidents (37%), and violence (6%). Of the 4349 patients, 2854 (66%) had mild TBI, 371 (9%) had moderate TBI, and 962 (22%) had severe TBI. Pupillary reaction was abnormal in 10% of patients. Intracranial CT abnormalities were found in 55%, with traumatic subarachnoid hemorrhage (41%), contusions (31%) and acute subdural hematoma (26%) as the most common abnormalities. Total in-hospital mortality was 7%, increasing from 1% for patients with mild TBI, to 22% for those with severe TBI.
Table 1.
Baseline Characteristics of Patients According to Trauma Severity
| Patient characteristics | Trauma severity |
p value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild |
Moderate |
Severe |
Total |
||||||
| No. | (%) | No. | (%) | No. | (%) | No. | (%) | ||
| Total | 2854 | 65.6% | 371 | 8.5% | 962 | 22.1% | 4349 | 100.0% | |
| Sex | <0.001 | ||||||||
| Male | 1835 | 64.3% | 254 | 68.5% | 726 | 75.5% | 2926 | 67.3% | |
| Female | 1019 | 35.7% | 117 | 31.5% | 236 | 24.5% | 1423 | 32.7% | |
| Age | <0.001 | ||||||||
| Median [IQR], years | 53 [33-68] | 55 [35-70] | 47 [29-64] | 51 [32-67] | |||||
| 16-25 years | 449 | 15.7% | 52 | 14.0% | 197 | 20.5% | 725 | 16.7% | |
| 26-40 years | 501 | 17.6% | 64 | 17.3% | 190 | 19.8% | 783 | 18.0% | |
| 41-64 years | 1087 | 38.1% | 132 | 35.6% | 358 | 37.2% | 1648 | 37.9% | |
| ≥65 years | 817 | 28.6% | 123 | 33.2% | 217 | 22.6% | 1193 | 27.4% | |
| Medical history | <0.001 | ||||||||
| Healthy patient | 1563 | 54.8% | 181 | 48.8% | 528 | 54.9% | 2352 | 54.1% | |
| Mild systemic disease | 951 | 33.3% | 130 | 35.0% | 275 | 28.6% | 1401 | 32.2% | |
| Severe systemic disease | 310 | 10.9% | 47 | 12.7% | 97 | 10.1% | 460 | 10.6% | |
| Missing | 30 | 1.1% | 13 | 3.5% | 62 | 6.4% | 136 | 3.1% | |
| Cause of injury | <0.001 | ||||||||
| Road traffic accident | 973 | 34.1% | 139 | 37.5% | 456 | 47.4% | 1619 | 37.2% | |
| Fall | 1392 | 48.8% | 157 | 42.3% | 352 | 36.6% | 1955 | 45.0% | |
| Violence | 186 | 6.5% | 22 | 5.9% | 28 | 2.9% | 244 | 5.6% | |
| Self-harm | 15 | 0.5% | 6 | 1.6% | 23 | 2.4% | 48 | 1.1% | |
| Other | 240 | 8.4% | 36 | 9.7% | 66 | 6.9% | 362 | 8.3% | |
| Missing | 48 | 1.7% | 11 | 3.0% | 37 | 3.8% | 121 | 2.8% | |
| Brain AIS | <0.001 | ||||||||
| Minor | 773 | 27.1% | 14 | 3.8% | 8 | 0.8% | 803 | 18.5% | |
| Moderate | 470 | 16.5% | 8 | 2.2% | 18 | 1.9% | 503 | 11.6% | |
| Serious | 1081 | 37.9% | 42 | 11.3% | 29 | 3.0% | 1183 | 27.2% | |
| Severe | 371 | 13.0% | 131 | 35.3% | 179 | 18.6% | 714 | 16.4% | |
| Critical | 130 | 4.6% | 166 | 44.7% | 653 | 67.9% | 1000 | 23.0% | |
| Unsurvivable | 2 | 0.1% | 5 | 1.3% | 70 | 7.3% | 86 | 2.0% | |
| Missing | 27 | 0.9% | 5 | 1.3% | 5 | 0.5% | 60 | 1.4% | |
| ISS | <0.001 | ||||||||
| Minor (≤16) | 1973 | 69.1% | 169 | 45.6% | 667 | 69.3% | 1256 | 28.9% | |
| Major (17-25) | 506 | 17.7% | 100 | 27.0% | 223 | 23.2% | 862 | 19.8% | |
| Critically injured (>25) | 351 | 12.3% | 97 | 26.1% | 67 | 7.0% | 2167 | 49.8% | |
| Missing | 24 | 0.8% | 5 | 1.3% | 5 | 0.5% | 64 | 1.5% | |
| Baseline pupillary reaction | <0.001 | ||||||||
| Both reacting | 2655 | 93.0% | 315 | 84.9% | 618 | 64.2% | 3654 | 84.0% | |
| One reacting | 46 | 1.6% | 15 | 4.0% | 95 | 9.9% | 162 | 3.7% | |
| Non-reacting | 28 | 1.0% | 20 | 5.4% | 216 | 22.5% | 277 | 6.4% | |
| Missing | 125 | 4.4% | 21 | 5.7% | 33 | 3.4% | 256 | 5.9% | |
| CT abnormalities | |||||||||
| Any CT abnormality | <0.001 | ||||||||
| Absent | 1443 | 50.6% | 31 | 8.4% | 59 | 6.1% | 1575 | 36.2% | |
| Present | 1217 | 42.6% | 287 | 77.4% | 789 | 82.0% | 2388 | 54.9% | |
| Cisternal compression | 124 | 4.3% | 89 | 24.0% | 380 | 39.5% | 627 | 14.4% | <0.001 |
| Midline shift | 103 | 3.6% | 77 | 20.8% | 252 | 26.2% | 455 | 10.5% | <0.001 |
| Subarachnoid hemorrhage | 808 | 28.3% | 244 | 65.8% | 663 | 68.9% | 1793 | 41.2% | <0.001 |
| Epidural hematoma | 207 | 7.3% | 73 | 19.7% | 128 | 13.3% | 425 | 9.8% | <0.001 |
| Acute subdural hematoma | 472 | 16.5% | 166 | 44.7% | 442 | 45.9% | 1126 | 25.9% | <0.001 |
| Diffuse axonal injury | 166 | 5.8% | 48 | 12.9% | 212 | 22.0% | 443 | 10.2% | <0.001 |
| Contusion | 563 | 19.7% | 207 | 55.8% | 502 | 52.2% | 1336 | 30.7% | <0.001 |
| No CT scan performed | 129 | 4.5% | 35 | 9.4% | 80 | 8.3% | 261 | 6.0% | |
| In-hospital mortality | <0.001 | ||||||||
| No | 2034 | 71.3% | 327 | 88.1% | 742 | 77.1% | 3216 | 73.9% | |
| Yes | 35 | 1.2% | 40 | 10.8% | 207 | 21.5% | 310 | 7.1% | |
| Missing | 785 | 27.5% | 4 | 1.1% | 13 | 1.4% | 823 | 18.9% | |
| GOSE-6 months disability | <0.001 | ||||||||
| 1 | 89 | 3.1% | 74 | 19.9% | 273 | 28.4% | 470 | 10.8% | |
| 2-3 | 97 | 3.4% | 33 | 8.9% | 171 | 17.8% | 314 | 7.2% | |
| 4 | 83 | 2.9% | 25 | 6.7% | 57 | 5.9% | 174 | 4.0% | |
| 5 | 169 | 5.9% | 47 | 12.7% | 110 | 11.4% | 339 | 7.8% | |
| 6 | 244 | 8.5% | 36 | 9.7% | 90 | 9.4% | 383 | 8.8% | |
| 7 | 528 | 18.5% | 39 | 10.5% | 78 | 8.1% | 658 | 15.1% | |
| 8 | 1160 | 40.6% | 63 | 17.0% | 66 | 6.9% | 1325 | 30.5% | |
| Missing | 484 | 17.0% | 54 | 14.6% | 117 | 12.2% | 686 | 15.8% | |
A total of 157 patients were missing information on the baseline Glasgow Coma Scale score.
The p value assesses the null hypothesis of no differences among the mild, moderate, and severe subgroups.
IQR, interquartile range; AIS, Abbreviated Injury Score; ISS, Injury Severity Score; CT, computed tomography; GOSE, Glasgow Outcome Scale Extended.
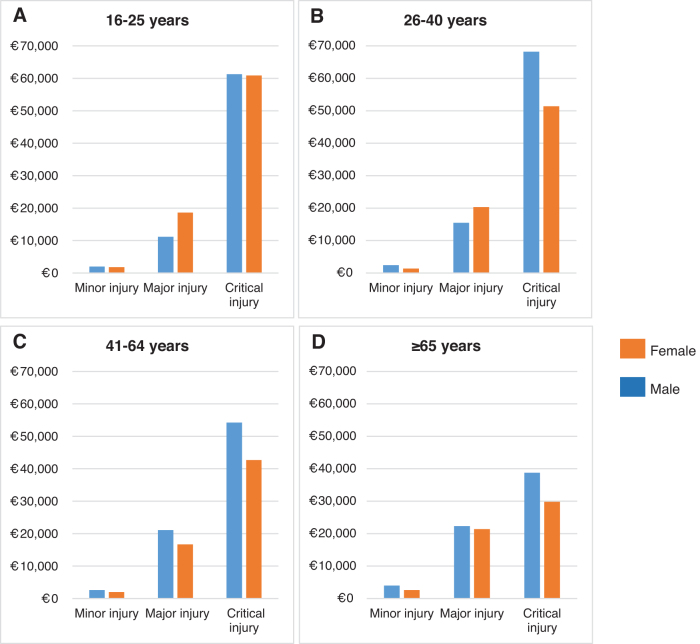
Healthcare consumption
Hospital admission (i.e. including ICU and ward admission) accounted for over half (60%) of the mean total intramural costs (mild TBI: €8,200 [55%], moderate TBI: €33,400 [61%], severe TBI: €48,500 [61%]), of which 47% were related to ICU admission and 13% were related to ward admission (Fig. 1 and Supplementary Table S4). For the total study population, the mean LOS at the ICU and ward were 5.1 and 6.3 days respectively (Table 2). For mild, moderate, and severe TBI, mean LOS was 1.8, 8.9, and 13.5 days in the ICU and 4.5, 10.1, and 10.3 days on the ward, respectively. The mean LOS for inpatient rehabilitation was 13.5 days for the total population and 5.8, 22.1, and 32.6 days, respectively, for mild, moderate, and severe TBI. Rehabilitation costs (19%; €6,400) and intracranial surgeries (8%; €2,700) were also large cost contributors (Fig. 1 and Supplementary Table S4). Costs for all categories were higher for each TBI severity level. Proportion of total costs related to ICU admission and intracranial surgery increased with TBI severity, while proportion of costs related to ward admission, pre-hospital expenses, and extracranial surgery decreased. Patients who sustained TBI as a result of self-harm had the longest ICU and ward LOS (11 and 17 days, respectively). Patients who died during admission had higher median total costs (€18.900 vs. €8,500) (Table 2).
FIG. 1.
Proportion of mean total intramural costs per cost- category according to severity of traumatic brain injury (TBI). The proportion of the total intramural costs from each cost category are plotted in a histogram for each TBI severity level separately. The exact percentage for each cost category (including pre-hospital costs, intensive care unit and ward admission costs, intra- and extracranial surgery costs, laboratory costs, imaging costs, blood products costs, and rehabilitation costs) are presented in the table below the figure. For example, of the total costs within the mild TBI category, 7% of the expenses were from pre-hospital costs.
Table 2.
Median Intramural Costs for Each Cost Category According to Baseline Characteristics
| Patient characteristics | Cost category |
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total costs |
Pre-hospital |
Intracranial |
Extracranial |
Hospitalization |
ICU (days) |
Ward (days) |
Laboratory |
Imaging |
Blood products |
Rehabilitation |
Rehabiliation (days) |
||||||||||||||||||||||
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Mean | SD | Mean | SD | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Mean | SD | ||||||||||
| Total | 9500 | 2000 | 41,300 | 700 | 600 | 1200 | 0 | 0 | 4300 | 0 | 0 | 0 | 4600 | 900 | 23,500 | 5.1 | 10.3 | 6.3 | 13.0 | 300 | 100 | 900 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 13.5 | 34.8 |
| Sex | |||||||||||||||||||||||||||||||||
| Male | 11,600 | 2500 | 48,600 | 700 | 600 | 1500 | 0 | 0 | 4400 | 0 | 0 | 0 | 6100 | 1000 | 27,400 | 5.9 | 11.3 | 6.8 | 13.7 | 300 | 100 | 1000 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 14.6 | 37.3 |
| Female | 5900 | 1600 | 27,700 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 3100 | 300 | 14,400 | 3.5 | 7.6 | 5.4 | 11.5 | 200 | 0 | 700 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 11.1 | 29.0 |
| Age | |||||||||||||||||||||||||||||||||
| 16-25 years | 7400 | 1800 | 42,700 | 700 | 600 | 3000 | 0 | 0 | 4300 | 0 | 0 | 0 | 3700 | 900 | 24,600 | 5.6 | 10.4 | 5.7 | 12.7 | 200 | 100 | 900 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 14.5 | 38.0 |
| 26-40 years | 8900 | 1800 | 46,100 | 700 | 600 | 1200 | 0 | 0 | 4400 | 0 | 0 | 0 | 4500 | 900 | 27,300 | 6.0 | 13.2 | 6.3 | 12.7 | 300 | 100 | 1000 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 14.2 | 35.8 |
| 41-64 years | 10,400 | 2100 | 44,300 | 700 | 600 | 1300 | 0 | 0 | 4300 | 0 | 0 | 0 | 5500 | 900 | 25,400 | 5.2 | 10.0 | 6.6 | 13.2 | 300 | 100 | 1000 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 13.8 | 36.8 |
| ≥65 years | 10,000 | 2400 | 34,600 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 4900 | 900 | 18,600 | 4.1 | 8.4 | 6.4 | 13.2 | 300 | 100 | 800 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 11.9 | 28.8 |
| Medical history | |||||||||||||||||||||||||||||||||
| Healthy patient | 8300 | 1800 | 40,700 | 700 | 600 | 1200 | 0 | 0 | 4300 | 0 | 0 | 0 | 4300 | 900 | 23,100 | 5.2 | 9.9 | 5.8 | 12.0 | 300 | 100 | 900 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 13.3 | 34.6 |
| Mild systemic disease | 10,300 | 2300 | 39,000 | 700 | 600 | 1200 | 0 | 0 | 3800 | 0 | 0 | 0 | 5200 | 900 | 24,000 | 5.0 | 11.0 | 6.7 | 12.7 | 300 | 100 | 900 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 900 | 13.8 | 36.0 |
| Severe systemic disease | 12,100 | 2200 | 47,700 | 700 | 700 | 1200 | 0 | 0 | 4700 | 0 | 0 | 0 | 5400 | 900 | 27,200 | 5.1 | 10.3 | 7.7 | 17.9 | 300 | 100 | 1100 | 200 | 100 | 400 | 0 | 0 | 200 | 0 | 0 | 3700 | 13.4 | 32.1 |
| Cause of injury | |||||||||||||||||||||||||||||||||
| Road traffic accident | 14,800 | 3100 | 57,900 | 700 | 700 | 3000 | 0 | 0 | 4400 | 0 | 0 | 2000 | 7900 | 1200 | 32,500 | 6.3 | 10.8 | 6.8 | 12.8 | 400 | 100 | 1100 | 200 | 100 | 400 | 0 | 0 | 200 | 0 | 0 | 7100 | 16.8 | 38.4 |
| Fall | 7100 | 1800 | 30,800 | 700 | 600 | 900 | 0 | 0 | 3000 | 0 | 0 | 0 | 3700 | 900 | 16,600 | 4.4 | 10.3 | 5.8 | 12.2 | 200 | 100 | 800 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 11.5 | 32.8 |
| Violence | 5000 | 1500 | 24,200 | 700 | 400 | 900 | 0 | 0 | 5300 | 0 | 0 | 0 | 2200 | 900 | 12,800 | 3.4 | 7.3 | 6.1 | 16.7 | 200 | 100 | 600 | 300 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 8.9 | 26.4 |
| Self-harm | 43,700 | 14,700 | 108,000 | 800 | 600 | 3300 | 0 | 0 | 8700 | 2200 | 0 | 10,100 | 31,000 | 5700 | 69,900 | 10.9 | 13.2 | 16.9 | 27.9 | 900 | 200 | 2900 | 300 | 200 | 500 | 700 | 0 | 2300 | 0 | 0 | 16,000 | 22.5 | 37.0 |
| Other | 6600 | 1800 | 33,600 | 700 | 600 | 1200 | 0 | 0 | 0 | 0 | 0 | 0 | 3600 | 900 | 18800 | 4.3 | 8.8 | 5.8 | 11.9 | 200 | 100 | 700 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 11.1 | 32.0 |
| TBI severity | |||||||||||||||||||||||||||||||||
| Mild | 3800 | 1400 | 14,100 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 1700 | 300 | 7400 | 1.8 | 5.5 | 4.5 | 9.5 | 100 | 0 | 400 | 200 | 100 | 300 | 0 | 0 | 0 | 0 | 0 | 0 | 5.8 | 21.5 |
| Moderate | 37,800 | 14,900 | 74,200 | 800 | 700 | 3300 | 4200 | 0 | 8500 | 0 | 0 | 0 | 20,600 | 8000 | 47,500 | 8.9 | 10.9 | 10.1 | 13.5 | 800 | 400 | 1600 | 400 | 200 | 500 | 0 | 0 | 500 | 0 | 0 | 13,700 | 22.1 | 41.0 |
| Severe | 60,400 | 24,400 | 112,700 | 900 | 700 | 3700 | 4800 | 0 | 10,500 | 0 | 0 | 2200 | 37,200 | 13,900 | 70,400 | 13.5 | 14.7 | 10.3 | 19.2 | 1100 | 400 | 2000 | 400 | 200 | 600 | 0 | 0 | 900 | 0 | 0 | 23,700 | 32.6 | 51.7 |
| Brain AIS | |||||||||||||||||||||||||||||||||
| Minor | 1400 | 900 | 3300 | 700 | 300 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 300 | 300 | 1400 | 0.3 | 1.7 | 1.9 | 4.6 | 0 | 0 | 100 | 100 | 100 | 200 | 0 | 0 | 0 | 0 | 0 | 0 | 1.4 | 9.8 |
| Moderate | 1800 | 1100 | 4800 | 700 | 600 | 800 | 0 | 0 | 0 | 0 | 0 | 0 | 700 | 300 | 2000 | 0.7 | 3.3 | 2.8 | 11.7 | 100 | 0 | 200 | 200 | 100 | 200 | 0 | 0 | 0 | 0 | 0 | 0 | 2.9 | 14.6 |
| Serious | 4700 | 2100 | 11,600 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 2200 | 900 | 5600 | 1.0 | 3.8 | 5.5 | 9.2 | 200 | 100 | 400 | 200 | 100 | 300 | 0 | 0 | 0 | 0 | 0 | 0 | 6.1 | 21.9 |
| Severe | 26,900 | 13,500 | 53,800 | 800 | 700 | 3000 | 0 | 0 | 4800 | 0 | 0 | 1600 | 15,100 | 8200 | 33,000 | 7.2 | 9.6 | 8.9 | 13.1 | 600 | 300 | 1200 | 300 | 200 | 500 | 0 | 0 | 200 | 0 | 0 | 10,000 | 18.1 | 37.6 |
| Critical | 70,700 | 35,100 | 119,800 | 900 | 700 | 3700 | 6800 | 3800 | 12,300 | 0 | 0 | 1900 | 42,300 | 20,200 | 75,700 | 14.8 | 14.5 | 11.2 | 19.1 | 1200 | 600 | 2200 | 500 | 300 | 700 | 100 | 0 | 900 | 5200 | 0 | 25,900 | 34.9 | 52.0 |
| Unsurvivable | 7200 | 4200 | 15,700 | 700 | 700 | 3400 | 0 | 0 | 4200 | 0 | 0 | 0 | 3300 | 2900 | 5500 | 3.4 | 11.4 | 0.8 | 3.5 | 100 | 100 | 100 | 100 | 100 | 300 | 0 | 0 | 900 | 0 | 0 | 0 | 0.5 | 3.6 |
| ISS | |||||||||||||||||||||||||||||||||
| Minor (≤16) | 2400 | 1100 | 7100 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 1000 | 300 | 3700 | 0.8 | 3.5 | 3.3 | 8.5 | 100 | 0 | 300 | 200 | 100 | 300 | 0 | 0 | 0 | 0 | 0 | 0 | 4.1 | 18.8 |
| Major (17-25) | 19,000 | 7000 | 54,700 | 800 | 700 | 2700 | 0 | 0 | 6500 | 0 | 0 | 0 | 10,500 | 3500 | 31,000 | 6.4 | 12.6 | 7.9 | 12.6 | 500 | 200 | 1100 | 300 | 100 | 500 | 0 | 0 | 0 | 0 | 0 | 8300 | 16.9 | 38.0 |
| Critically injured (>25) | 51,800 | 20,300 | 99,300 | 900 | 700 | 3700 | 3800 | 0 | 8700 | 0 | 0 | 4200 | 30,100 | 10,500 | 61,000 | 11.5 | 12.6 | 10.5 | 17.6 | 1000 | 400 | 1900 | 400 | 200 | 500 | 0 | 0 | 900 | 0 | 0 | 18,700 | 27.2 | 46.7 |
| Baseline pupillary reaction | |||||||||||||||||||||||||||||||||
| Both reacting | 7800 | 1800 | 34,400 | 700 | 600 | 1000 | 0 | 0 | 0 | 0 | 0 | 0 | 4200 | 900 | 19,300 | 4.4 | 9.5 | 6.2 | 12.8 | 300 | 100 | 800 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 12.4 | 33.4 |
| One reacting | 51,600 | 15,000 | 102,700 | 900 | 700 | 3700 | 5300 | 0 | 10,400 | 0 | 0 | 1800 | 28,800 | 6200 | 58,600 | 11.0 | 12.1 | 9.1 | 14.7 | 900 | 300 | 1900 | 400 | 200 | 500 | 0 | 0 | 900 | 0 | 0 | 22,600 | 30.0 | 49.8 |
| Non-reacting | 31,500 | 8100 | 87,800 | 900 | 700 | 3700 | 4800 | 0 | 9600 | 0 | 0 | 1600 | 18,300 | 3300 | 54,900 | 10.6 | 15.2 | 6.3 | 14.5 | 400 | 100 | 1500 | 300 | 100 | 500 | 200 | 0 | 1400 | 0 | 0 | 7500 | 18.0 | 39.9 |
| CT abnormalities | |||||||||||||||||||||||||||||||||
| Any CT abnormality | |||||||||||||||||||||||||||||||||
| Absent | 2400 | 1100 | 10,000 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 900 | 300 | 4500 | 2.3 | 9.1 | 3.7 | 11.0 | 100 | 0 | 300 | 100 | 100 | 200 | 0 | 0 | 0 | 0 | 0 | 0 | 6.7 | 26.1 |
| Present | 23,300 | 7200 | 66,600 | 800 | 700 | 3100 | 0 | 0 | 5600 | 0 | 0 | 0 | 12,800 | 3700 | 39,600 | 7.4 | 10.7 | 8.5 | 14.1 | 600 | 200 | 1300 | 300 | 200 | 500 | 0 | 0 | 300 | 0 | 0 | 10,300 | 19.1 | 39.7 |
| Cisternal compression | 47,500 | 15,900 | 106,100 | 900 | 700 | 3300 | 6800 | 3300 | 12,300 | 0 | 0 | 0 | 27,000 | 7200 | 63,300 | 11.4 | 12.2 | 9.3 | 16.2 | 800 | 300 | 1900 | 400 | 200 | 600 | 0 | 0 | 1200 | 0 | 0 | 18,700 | 28.2 | 51.6 |
| Midline shift | 42,100 | 14,900 | 93,700 | 900 | 700 | 3300 | 6800 | 3800 | 12,300 | 0 | 0 | 0 | 23,400 | 6500 | 54,900 | 10.0 | 11.4 | 9.1 | 15.3 | 800 | 300 | 1700 | 400 | 200 | 500 | 0 | 0 | 1000 | 0 | 0 | 17,600 | 27.0 | 49.3 |
| Subarachnoid heamorrhage | 30,400 | 9900 | 74,000 | 800 | 700 | 3300 | 0 | 0 | 7700 | 0 | 0 | 0 | 16,500 | 5100 | 46,300 | 8.4 | 11.0 | 9.3 | 15.5 | 700 | 300 | 1500 | 400 | 200 | 500 | 0 | 0 | 400 | 0 | 0 | 12,900 | 21.6 | 42.5 |
| Epidural hematoma | 27,800 | 10900 | 74,400 | 900 | 700 | 3000 | 4400 | 0 | 9300 | 0 | 0 | 0 | 16,000 | 5900 | 45,600 | 8.6 | 11.7 | 9.5 | 16.8 | 700 | 300 | 1500 | 400 | 300 | 500 | 0 | 0 | 300 | 0 | 0 | 9900 | 19.8 | 43.1 |
| Acute subdural hematoma | 31,400 | 9400 | 75,900 | 800 | 700 | 3100 | 3400 | 0 | 9200 | 0 | 0 | 0 | 17,000 | 4900 | 46,400 | 8.6 | 11.0 | 9.1 | 15.5 | 700 | 300 | 1500 | 400 | 200 | 500 | 0 | 0 | 500 | 0 | 0 | 13,200 | 21.8 | 42.8 |
| Diffuse axonal injury | 42,300 | 10,800 | 96,400 | 900 | 700 | 3700 | 0 | 0 | 7000 | 0 | 0 | 2200 | 24,200 | 5400 | 57,500 | 10.2 | 12.2 | 9.1 | 17.0 | 800 | 300 | 1700 | 400 | 200 | 600 | 0 | 0 | 400 | 0 | 0 | 17,500 | 26.7 | 46.8 |
| Contusion | 33,300 | 11,400 | 86,500 | 800 | 700 | 3300 | 3500 | 0 | 8700 | 0 | 0 | 0 | 20,100 | 6400 | 51,800 | 9.5 | 11.7 | 9.4 | 15.7 | 800 | 300 | 1600 | 400 | 300 | 600 | 0 | 0 | 400 | 0 | 0 | 13,800 | 23.0 | 43.7 |
| In-hospital mortality | |||||||||||||||||||||||||||||||||
| No | 8500 | 1800 | 42,000 | 700 | 600 | 1200 | 0 | 0 | 3500 | 0 | 0 | 0 | 4500 | 900 | 23,500 | 5.1 | 10.4 | 6.8 | 13.4 | 300 | 100 | 900 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 1800 | 14.6 | 36.0 |
| Yes | 18,900 | 7200 | 38,300 | 700 | 700 | 3400 | 4200 | 0 | 8700 | 0 | 0 | 0 | 8000 | 3300 | 24,300 | 5.9 | 9.2 | 0.6 | 3.1 | 200 | 100 | 600 | 300 | 100 | 400 | 0 | 0 | 1200 | 0 | 0 | 0 | - | - |
| GOSE-6 months disability | |||||||||||||||||||||||||||||||||
| 1 | 23,700 | 7900 | 52,200 | 700 | 700 | 3300 | 3800 | 0 | 8700 | 0 | 0 | 0 | 11,900 | 3300 | 34,900 | 7.5 | 14.2 | 4.3 | 11.7 | 300 | 100 | 1000 | 300 | 100 | 500 | 0 | 0 | 800 | 0 | 0 | 0 | 5.1 | 18.1 |
| 2-3 | 94,300 | 41,200 | 155,800 | 900 | 700 | 3500 | 5200 | 0 | 12,300 | 0 | 0 | 2500 | 52,700 | 21,600 | 88,600 | 16.3 | 14.3 | 17.8 | 27.5 | 1700 | 800 | 3000 | 400 | 200 | 700 | 0 | 0 | 1100 | 16,300 | 0 | 46,000 | 61.3 | 70.8 |
| 4 | 45,100 | 12,400 | 110,700 | 900 | 700 | 3400 | 0 | 0 | 7000 | 0 | 0 | 3000 | 28,800 | 7200 | 63,500 | 10.7 | 12.1 | 12.3 | 18.2 | 1000 | 400 | 2000 | 400 | 200 | 500 | 0 | 0 | 600 | 0 | 0 | 22,900 | 28.8 | 44.9 |
| 5 | 36,000 | 10,400 | 75,500 | 800 | 700 | 3400 | 0 | 0 | 6800 | 0 | 0 | 1800 | 18,300 | 5200 | 42,600 | 8.2 | 12.3 | 9.4 | 11.1 | 800 | 300 | 1500 | 300 | 200 | 500 | 0 | 0 | 300 | 0 | 0 | 17,500 | 23.2 | 35.6 |
| 6 | 17,100 | 4900 | 49,900 | 700 | 700 | 3000 | 0 | 0 | 4100 | 0 | 0 | 1900 | 8700 | 2200 | 28,100 | 5.4 | 9.0 | 7.2 | 9.6 | 400 | 200 | 1100 | 300 | 100 | 500 | 0 | 0 | 0 | 0 | 0 | 9400 | 15.9 | 30.8 |
| 7 | 5400 | 1800 | 18,900 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 2900 | 900 | 11,300 | 2.4 | 5.9 | 4.7 | 6.7 | 200 | 100 | 600 | 200 | 100 | 400 | 0 | 0 | 0 | 0 | 0 | 0 | 6.3 | 18.5 |
| 8 | 2600 | 1200 | 8700 | 700 | 600 | 900 | 0 | 0 | 0 | 0 | 0 | 0 | 1200 | 300 | 4800 | 1.4 | 4.8 | 3.3 | 8.1 | 100 | 0 | 300 | 200 | 100 | 300 | 0 | 0 | 0 | 0 | 0 | 0 | 3.3 | 15.8 |
ICU, intensive care unit; IQR, interquartile range; SD, standard deviation; TBI, traumatic brain injury; AIS, Abbreviated Injury Score; ISS, Injury Severity Score; CT, computed tomography; GOSE, Glasgow Outcome Scale Extended
Healthcare costs
Median intramural healthcare costs for mild, moderate, and severe TBI patients in Europe were, respectively, €3,800 [IQR €1,400–€14,000], €37,800 [IQR €14,900–€74,200], and €60,400 [IQR €24,400–€112,700], with males (€11,600; IQR [€2,500–€48,600]) having higher costs than females (€5,900; IQR [€1,600–€27,600]) (Table 3). A similar increase in costs was found for increasing systemic injury severity: minor injury (ISS ≥ 16) €2,400 [IQR €1,100–€7,100], major injury (ISS 17–25), €19,000 [IQR €7,000–€54,700], and critically injured (ISS >25) €51,800 [IQR €20,300–€99,200]. The costs for patients 16–25 years of age, 26–40 years of age, 41–64 years of age, and ≥65 years of age were, respectively, €7,400 [IQR €1,800–€42,700], €8,900 [IQR €1,800–€46,100], €10,400 [IQR €2,200–€44,300], and €10,000 [IQR €2,400–€34,600]. Across all severities, costs increased with age. Although elderly patients (≥ 65 years) had shorter ICU LOS and lower costs for surgical interventions, they had longer ward LOS (Supplementary Table S5). A worse pre-morbid overall health state was accompanied by higher costs in mild and moderate TBI patients, whereas costs were lower for severe TBI. Patients with CT abnormalities had higher costs than patients without CT abnormalities. Self-harm €43,700 [IQR €15,000–€107,000] and road traffic incidents €14,800 [IQR €3,100–€57,900], as causes of injury also showed high costs. Patients with mild TBI who died during hospital admission had higher median costs than survivors (€3,800 vs. €14,300). In contrast, patients surviving hospital admission after moderate (€42,000 vs. €22,800) and severe TBI (€75,800 vs. €19,400) had higher costs than patients who died during admission. Mean costs are available in Supplementary Tables S5 and S6.
Table 3.
Median Intramural Costs of Traumatic Brain Injury (TBI) According to Trauma Severity
| Patient characteristics | TBI severity |
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mild |
Moderate |
Severe |
Total |
||||||||||||||
| Median (€) | IQR | Median (€) | IQR | Median (€) | IQR | Median (€) | IQR | p value | |||||||||
| Total | 3800 | 1400 | - | 14,100 | 37,800 | 14,900 | - | 74,200 | 60,400 | 24,400 | - | 112,400 | 9500 | 2000 | - | 41,300 | <0.001 |
| Sex | |||||||||||||||||
| Male | 4400 | 1800 | - | 15,400 | 40,800 | 15,100 | - | 78,800 | 64,100 | 27,800 | - | 115,000 | 11,600 | 2500 | - | 48,600 | <0.001 |
| Female | 2900 | 1200 | - | 11,300 | 33,200 | 14,900 | - | 70,100 | 52,100 | 19,200 | - | 103,100 | 5900 | 1600 | - | 27,600 | <0.001 |
| Age | |||||||||||||||||
| 16-25 years | 2900 | 1400 | - | 8500 | 31,900 | 8700 | - | 81,000 | 71,500 | 26,600 | - | 121,300 | 7400 | 1800 | - | 42,700 | <0.001 |
| 26-40 years | 2500 | 1100 | - | 10,500 | 41,200 | 14,900 | - | 86,300 | 74,700 | 35,100 | - | 121,000 | 8900 | 1800 | - | 46,100 | <0.001 |
| 41-64 years | 4000 | 1500 | - | 14,000 | 44,500 | 20,800 | - | 75,100 | 64,700 | 31,300 | - | 114,300 | 10,400 | 2200 | - | 44,300 | <0.001 |
| ≥65 years | 5400 | 1800 | - | 20,100 | 32,900 | 14,700 | - | 60,700 | 34,500 | 10,500 | - | 72,900 | 10,000 | 2400 | - | 34,600 | <0.001 |
| Medical history | |||||||||||||||||
| Healthy patient | 3400 | 1400 | - | 11,300 | 37,800 | 14,500 | - | 78,100 | 65,700 | 28,100 | - | 114,100 | 8300 | 1800 | - | 40,700 | <0.001 |
| Mild systemic disease | 4400 | 1500 | - | 16,800 | 34,700 | 18,800 | - | 66,600 | 57,200 | 19,800 | - | 112,900 | 10,300 | 2300 | - | 39,000 | <0.001 |
| Severe systemic disease | 4900 | 1400 | - | 21,900 | 44,200 | 10,900 | - | 84,000 | 52,500 | 18,300 | - | 91,600 | 12,100 | 2200 | - | 47,500 | <0.001 |
| Cause of injury | |||||||||||||||||
| Road traffic accident | 4700 | 1800 | - | 15,900 | 44,000 | 21,100 | - | 73,100 | 69,900 | 31,600 | - | 113,800 | 14,800 | 3100 | - | 57,900 | <0.001 |
| Fall | 3400 | 1400 | - | 13,800 | 30,600 | 12,400 | - | 74,300 | 50,100 | 18,400 | - | 103,600 | 7100 | 1800 | - | 30,800 | <0.001 |
| Violence | 2500 | 1100 | - | 9500 | 30,400 | 14,900 | - | 61,400 | 77,300 | 42,100 | - | 138,700 | 5000 | 1500 | - | 24,200 | <0.001 |
| Self-harm | 19,400 | 7000 | - | 43,700 | 97,100 | 47,800 | - | 169,000 | 52,100 | 17,000 | - | 110,200 | 43,700 | 15,000 | - | 107,000 | 0.037 |
| Other | 3100 | 1100 | - | 10,500 | 24,600 | 9000 | - | 55,800 | 59,800 | 26,800 | - | 110,300 | 6600 | 1800 | - | 32,900 | <0.001 |
| Brain AIS | |||||||||||||||||
| Minor | 1400 | 900 | - | 3200 | 10,000 | 3300 | - | 16,600 | 12,600 | 3200 | - | 30,900 | 1400 | 900 | - | 3300 | <0.001 |
| Moderate | 1800 | 1100 | - | 4400 | 4500 | 2000 | - | 8300 | 28,900 | 5500 | - | 79,200 | 1800 | 1100 | - | 4800 | <0.001 |
| Serious | 4300 | 2100 | - | 10,600 | 9600 | 4100 | - | 30,100 | 15,900 | 6400 | - | 58,600 | 4700 | 2100 | - | 11,600 | <0.001 |
| Severe | 18,700 | 10,800 | - | 36,100 | 34,700 | 17,400 | - | 60,500 | 48,600 | 24,000 | - | 89,200 | 26,900 | 13,600 | - | 53,600 | <0.001 |
| Critical | 58,800 | 28,600 | - | 96,700 | 57,500 | 29,100 | - | 107,300 | 76,200 | 39,600 | - | 125,900 | 70,700 | 35,100 | - | 119,700 | <0.001 |
| Unsurvivable | 20,400 | 7700 | - | 30,500 | 4200 | 2900 | - | 5700 | 7200 | 4200 | - | 15,000 | 7200 | 4200 | - | 15,500 | 0.080 |
| ISS | |||||||||||||||||
| Minor (≤16) | 2000 | 1100 | - | 5600 | 13,900 | 7400 | - | 30,800 | 24,600 | 6900 | - | 49800 | 2400 | 1100 | - | 7100 | <0.001 |
| Major (17-25) | 10,100 | 4000 | - | 22,700 | 41,900 | 25,200 | - | 77,400 | 58,600 | 24,300 | - | 114,200 | 19,000 | 7000 | - | 54,700 | <0.001 |
| Critically injured (>25) | 29,100 | 13400 | - | 63,400 | 54,000 | 27,200 | - | 90,600 | 66,900 | 28,400 | - | 114,400 | 51,800 | 20,300 | - | 99,200 | <0.001 |
| Baseline pupillary reaction | |||||||||||||||||
| Both reacting | 3800 | 1400 | - | 13,800 | 35,200 | 14,900 | - | 72,000 | 64,600 | 31,200 | - | 113,900 | 7800 | 1800 | - | 34,400 | <0.001 |
| One reacting | 8300 | 2600 | - | 29,300 | 59,800 | 36,600 | - | 79,700 | 69,900 | 35,400 | - | 131,600 | 51,600 | 15,100 | - | 102,600 | <0.001 |
| Non-reacting | 5700 | 1000 | - | 35,700 | 45,100 | 9600 | - | 84,100 | 36,500 | 10,900 | - | 89,100 | 31,500 | 8300 | - | 87,400 | <0.001 |
| CT abnormalities | |||||||||||||||||
| Any CT abnormality | |||||||||||||||||
| Absent | 1800 | 1100 | - | 5100 | 27,200 | 7700 | - | 57,000 | 47,000 | 17,000 | - | 106,900 | 2400 | 1100 | - | 10,000 | <0.001 |
| Present | 10,400 | 3900 | - | 26,100 | 42,000 | 17,100 | - | 78,000 | 63,200 | 27,600 | - | 113,400 | 23,300 | 7200 | - | 66,600 | <0.001 |
| Cisternal compression | 31,100 | 13300 | - | 72,500 | 43,100 | 15,400 | - | 86,800 | 57,400 | 20,100 | - | 119,100 | 47,500 | 16,000 | - | 106,100 | <0.001 |
| Midline shift | 30,200 | 11900 | - | 68,200 | 39,400 | 14,700 | - | 72,100 | 52,100 | 19,900 | - | 110,500 | 42,100 | 15,000 | - | 93,600 | 0.003 |
| Subarachnoid hemorrhage | 13,500 | 5000 | - | 32,800 | 42,000 | 19,100 | - | 84,400 | 64,500 | 28,400 | - | 113.900 | 30,400 | 9900 | - | 74,000 | <0.001 |
| Epidural hematoma | 14,200 | 6500 | - | 31,700 | 37,100 | 15,800 | - | 64,100 | 73,300 | 33,300 | - | 125,200 | 27,800 | 10,900 | - | 74,400 | <0.001 |
| Acute subdural hematoma | 12,400 | 5100 | - | 34,400 | 45,100 | 19,200 | - | 88,500 | 60,200 | 24,100 | - | 115.500 | 31,400 | 9400 | - | 75,900 | <0.001 |
| Diffuse axonal injury | 9700 | 3600 | - | 21,800 | 48,800 | 27,200 | - | 93,800 | 82,600 | 48,000 | - | 119.000 | 42,300 | 11,000 | - | 96,300 | <0.001 |
| Contusion | 14,400 | 5900 | - | 34,200 | 45,200 | 21,000 | - | 86,800 | 70,700 | 32,400 | - | 123,600 | 33,300 | 11,400 | - | 86,500 | <0.001 |
| Inhospital mortality | |||||||||||||||||
| No | 3800 | 1400 | - | 13,800 | 42,000 | 16,700 | - | 78,600 | 75,800 | 38,700 | - | 126,700 | 8500 | 1800 | - | 42,000 | <0.001 |
| Yes | 14,300 | 1600 | - | 34,500 | 22,800 | 7800 | - | 32,400 | 19,400 | 8200 | - | 40,800 | 18,900 | 7200 | - | 37,900 | 0.069 |
| GOSE-6 months disability | |||||||||||||||||
| 1 | 13,600 | 2400 | - | 33,400 | 29,500 | 11,500 | - | 54,700 | 25,500 | 10,200 | - | 58,000 | 23,700 | 8000 | - | 52,200 | <0.001 |
| 2-3 | 38,000 | 11100 | - | 96,800 | 79,100 | 46,900 | - | 151,200 | 128,600 | 77,700 | - | 177,800 | 94,300 | 41,600 | - | 155,300 | <0.001 |
| 4 | 13,900 | 4000 | - | 38,400 | 56,600 | 32,200 | - | 114,300 | 110,500 | 69,000 | - | 142,300 | 45,100 | 12,400 | - | 110,600 | <0.001 |
| 5 | 12,900 | 4000 | - | 35,300 | 46,500 | 25,900 | - | 78,600 | 81,300 | 51,300 | - | 116,500 | 36,000 | 10,500 | - | 75,200 | <0.001 |
| 6 | 8600 | 3000 | - | 27,000 | 41,800 | 17,100 | - | 78,600 | 64,500 | 36,000 | - | 98,600 | 17,100 | 4900 | - | 49,700 | <0.001 |
| 7 | 3400 | 1800 | - | 11,100 | 24,000 | 13,500 | - | 58,800 | 38,700 | 21,600 | - | 78,800 | 5400 | 1800 | - | 18,900 | <0.001 |
| 8 | 2200 | 1100 | - | 6000 | 26,300 | 9400 | - | 46,000 | 32,700 | 11,600 | - | 71,200 | 2600 | 1200 | - | 8700 | <0.001 |
The p value assesses the null hypothesis of no differences among the mild, moderate, and severe subgroups.
IQR, interquartile range; AIS, Abbreviated Injury Score; ISS, Injury Severity Score; CT, computed tomography; GOSE, Glasgow Outcome Scale. Extended
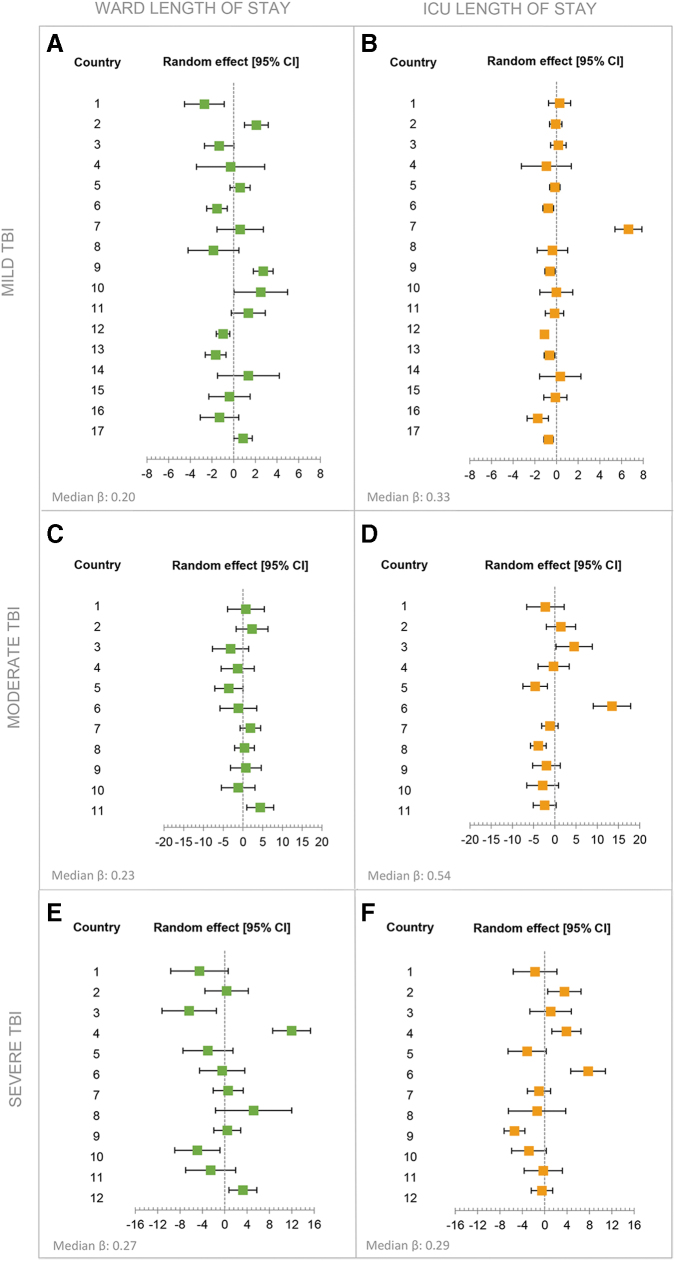
Sex differences in intramural costs
Male patients (median €11,600 [IQR €2,500–€48,600]) had higher median costs than female TBI patients (median €5,900 [IQR €1,600–€27,600]) (Table 3). Male patients incurred higher costs, across almost all age groups and injury severities (Fig. 2). Male patients showed higher costs across all seven intramural cost categories (p < 0.001). ICU LOS (mean 5.9 vs. 3.5 days) and ward LOS (mean LOS 6.8 vs. 5.4 days) were both longer for male than for female patients (p < 0.001) (Table 2). Irrespective of adjustment for several patient characteristics, costs remained higher for male patients (Table 4).
FIG. 2.
The median total intramural costs for male and female patients are plotted according to injury severity and age category. The injury severity was determined using the baseline systemic Injury Severity Score (ISS) and was categorized into three groups: ISS ≤16 (minor injury); ISS 17–25 (major injury); ISS >25 (critical injury). The four panels represent the four different age categories: (A) 16–25 years, (B) 26–40 years, (C) 41–64 years, and (D) ≥ 65 years.
Table 4.
Associations With Total Healthcare Costs Based on Generalized Linear Models
| Patient characteristics | Generalized linear model |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Multi-variate univariable |
Multi-variate multivariable |
|||||||||
| Exp[β] | 95% CI | p value | Exp[β] | 95% CI | p value | |||||
| Sex | ||||||||||
| Male | (ref) | (ref) | ||||||||
| Female | 0.72 | 0.66 | - | 0.78 | <0.001 | 0.80 | 0.75 | - | 0.85 | <0.001 |
| Age | ||||||||||
| 16-25 years | (ref) | (ref) | ||||||||
| 26-40 years | 1.04 | 0.91 | - | 1.19 | 0.547 | 1.13 | 1.02 | - | 1.24 | 0.015 |
| 41-64 years | 1.03 | 0.92 | - | 1.16 | 0.580 | 1.04 | 0.96 | - | 1.14 | 0.353 |
| ≥65 years | 0.89 | 0.79 | - | 1.01 | 0.074 | 1.13 | 1.01 | - | 1.25 | 0.026 |
| Medical history | ||||||||||
| Healthy patient | (ref) | (ref) | ||||||||
| Mild systemic disease | 0.97 | 0.89 | - | 1.07 | 0.572 | 1.06 | 0.99 | - | 1.14 | 0.105 |
| Severe systemic disease | 1.09 | 0.96 | - | 1.25 | 0.198 | 1.28 | 1.15 | - | 1.42 | <0.001 |
| Cause of injury | ||||||||||
| Road traffic accident | (ref) | (ref) | ||||||||
| Fall | 0.76 | 0.70 | - | 0.83 | <0.001 | 0.84 | 0.78 | - | 0.89 | <0.001 |
| Violence | 0.73 | 0.63 | - | 0.85 | <0.001 | 0.94 | 0.85 | - | 1.05 | 0.291 |
| Self-harm | 0.67 | 0.56 | - | 0.80 | <0.001 | 0.75 | 0.66 | - | 0.85 | <0.001 |
| Other | 1.83 | 1.26 | - | 2.68 | 0.002 | 1.09 | 0.83 | - | 1.43 | 0.536 |
| TBI severity | ||||||||||
| Mild | (ref) | (ref) | ||||||||
| Moderate | 3.52 | 3.10 | - | 3.99 | <0.001 | 1.46 | 1.31 | - | 1.63 | <0.001 |
| Severe | 4.88 | 4.48 | - | 5.32 | <0.001 | 1.67 | 1.52 | - | 1.84 | <0.001 |
| Brain AIS | ||||||||||
| Minor | (ref) | (ref) | ||||||||
| Moderate | 1.80 | 1.60 | - | 2.03 | <0.001 | 1.30 | 1.17 | - | 1.44 | <0.001 |
| Serious | 2.84 | 2.58 | - | 3.13 | <0.001 | 1.61 | 1.46 | - | 1.77 | <0.001 |
| Severe | 9.79 | 8.77 | - | 10.93 | <0.001 | 2.75 | 2.43 | - | 3.13 | <0.001 |
| Critical | 17.70 | 15.99 | - | 19.59 | <0.001 | 2.75 | 2.37 | - | 3.19 | <0.001 |
| Unsurvivable | 3.79 | 3.00 | - | 4.79 | <0.001 | 0.39 | 0.31 | - | 0.51 | <0.001 |
| ISS | ||||||||||
| Minor (≤16) | (ref) | (ref) | ||||||||
| Major (17-25) | 4.51 | 4.12 | - | 4.94 | <0.001 | 1.85 | 1.70 | - | 2.01 | <0.001 |
| Critically injured (>25) | 7.10 | 6.55 | - | 7.70 | <0.001 | 2.57 | 2.34 | - | 2.81 | <0.001 |
| Hypoxia | ||||||||||
| No | (ref) | (ref) | ||||||||
| Yes | 2.08 | 1.74 | - | 2.50 | <0.001 | 1.15 | 1.00 | - | 1.32 | 0.045 |
| Hypotension | ||||||||||
| No | (ref) | (ref) | ||||||||
| Yes | 2.32 | 1.96 | - | 2.76 | <0.001 | 1.18 | 1.03 | - | 1.35 | 0.016 |
| Hemoglobin | 0.81 | 0.80 | - | 0.82 | <0.001 | 0.91 | 0.90 | - | 0.93 | <0.001 |
| Glucose | 1.15 | 1.12 | - | 1.17 | <0.001 | 1.04 | 1.03 | - | 1.06 | <0.001 |
| Marshall CT classification | ||||||||||
| 1 | (ref) | (ref) | ||||||||
| 2 | 4.05 | 3.74 | - | 4.40 | <0.001 | 1.53 | 1.39 | - | 1.69 | <0.001 |
| 3 | 8.03 | 6.68 | - | 9.65 | <0.001 | 2.17 | 1.78 | - | 2.66 | <0.001 |
| 4 | 5.96 | 4.05 | - | 8.79 | <0.001 | 2.40 | 1.72 | - | 3.35 | <0.001 |
| 5 | 9.93 | 6.59 | - | 14.97 | <0.001 | 2.49 | 1.77 | - | 3.49 | <0.001 |
| 6 | 7.11 | 6.43 | - | 7.87 | <0.001 | 2.34 | 2.05 | - | 2.67 | <0.001 |
| CT abnormalities | ||||||||||
| Cisternal compression | 2.55 | 2.29 | - | 2.85 | <0.001 | 0.94 | 0.81 | - | 1.08 | 0.394 |
| Midline shift | 2.19 | 1.92 | - | 2.48 | <0.001 | 0.86 | 0.74 | - | 1.00 | 0.044 |
| Subarachnoid heamorrhage | 2.65 | 2.45 | - | 2.87 | <0.001 | 1.03 | 0.95 | - | 1.13 | 0.444 |
| Epidural hematoma | 1.59 | 1.39 | - | 1.82 | <0.001 | 0.98 | 0.89 | - | 1.08 | 0.654 |
| Acute subdural hematoma | 2.11 | 1.93 | - | 2.31 | <0.001 | 1.18 | 1.09 | - | 1.28 | <0.001 |
| Diffuse axonal injury | 1.92 | 1.69 | - | 2.19 | <0.001 | 0.98 | 0.90 | - | 1.06 | 0.623 |
| Contusion | 2.46 | 2.27 | - | 2.68 | <0.001 | 0.94 | 0.85 | - | 1.04 | 0.259 |
CI, confidence interval; TBI, traumatic brain injury; AIS, Abbreviated Injury Score; ISS, Injury Severity Score; CT, computed tomography.
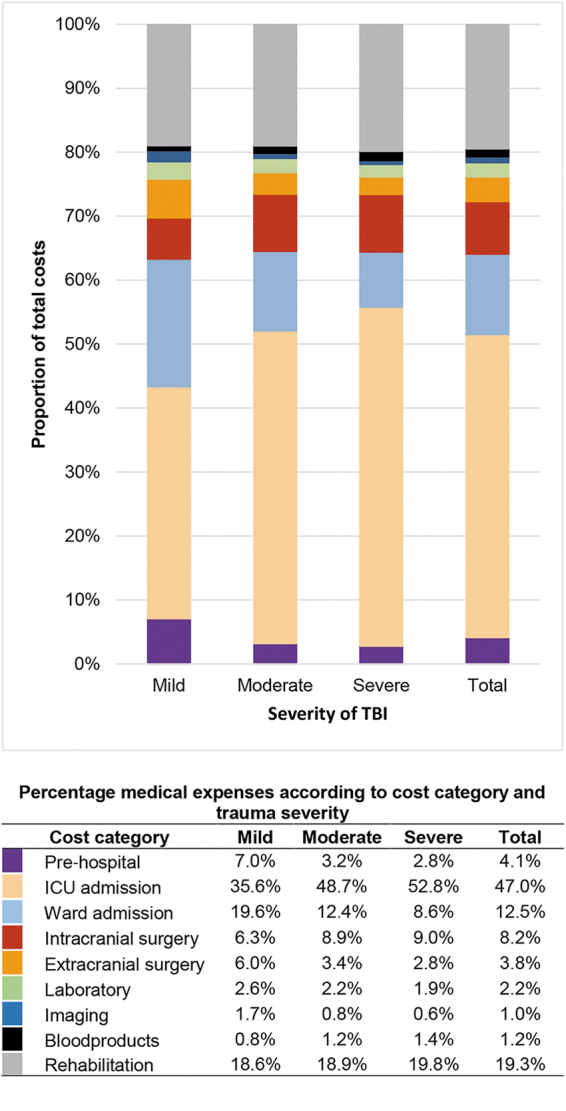
Between-country differences in healthcare consumption
Case-mix of patients varied substantially among countries. The total number of patients per country ranged from 15 to 962. France (52%), Sweden (35%), and Lithuania (33%) had a high percentage of severe TBI patients. Patients with critical injury (Injury Severity Score [ISS] = critical) were mostly found in France (67%), Italy (42%) and the United Kingdom (37%) (Supplementary Table S7). Throughout Europe, costs related to hospitalization were the largest contributor to the total intramural costs, especially in Romania (83%), Austria (76%), and France (72%) (Supplementary Fig. S1). The costs generated from intracranial surgery were the highest in Denmark (12%), Lithuania (12%), Sweden (13%), and Hungary (13%). The multi-variable linear regression model showed that across all TBI severities and adjusted for patient characteristics, some differences among countries in the LOS in the ICU and on the ward were present (Fig. 3A–3F). Most profound differences were visible in the LOS in the ICU, especially in the moderate and severe patient groups (Fig. 3D and 3F). Outliers within this analysis are most profoundly caused by the selective sampling of countries. The median β value indicates that mild, moderate, and severe TBI patients with the same baseline characteristics from a random country will have an average ICU LOS longer by 0.33 days, 0.54 days, and 0.29 days, respectively, when compared with another random country (Fig. 3A–F).
FIG. 3.
This panel shows forest plots reporting the random country effect (random intercept estimate and 95% confidence intervals) on the length of stay at the ICU and ward for mild (A–B), moderate (C–D) and severe (E–F) TBI patients. Countries including fewer than five patients per severity group were excluded from this analysis. The models included adjustment according to the International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) prognostic model. The median β reflects the between-country variation; a median β equal to 0 represents no variation, the larger the median β, the larger the variation.
Generalized linear model
Female patients showed lower total intramural costs with an OR of 0.80 [CI 0.75–0.85] times lower than male patients. Increasing TBI severity was associated with higher costs for moderate and severe patients: OR 1.46 [CI 1.31–1.63] and OR 1.67 [CI 1.52–1.84], respectively. Compared with minor brain AIS, severe and critically injured patients showed higher costs (OR 2.75 [CI 2.43–3.13] and 2.75 [CI 2.37–3.19]) (Table 4). Hypotension at admission was also associated with higher costs with an OR of 1.18 [CI 1.03–1.35]. Increasing severity of CT abnormalities, as measured by the Marshall CT score, was also associated with higher costs.
Discussion
The median intramural healthcare costs of a TBI patient in Europe were €3,800 [IQR €1,400–€14,000] for mild, €37,800 [IQR €14,900–€74,200] for moderate, and €60,400 [IQR €24,400–€112,700] for severe TBI. Costs generally increased with higher age, higher injury severity, and male gender. For all TBI severity groups and across all countries, hospitalization was the main driver for total intramural costs.
Patient population
Studies describing the global burden of TBI, estimated that mild TBI accounted for 81% of injuries, moderate TBI for 11% and severe TBI for 8% and estimated that the first-year lifetime costs per person for mild TBI was between US$3395 and US$4636 and respectively US$21379 and US$36648 for moderate and severe patients.20,39 In comparison to these studies, the CENTER-TBI population included only those patients with a CT indication and recruited mostly patients from academic medical centers, leading to a lower proportion of mild TBI patients and higher rates of severely injured patients. Severe TBI patients have longer LOS and undergo more neurosurgical interventions compared to the other severity levels of TBI, which could result in higher total intramural costs for the entire CENTER-TBI population.17,20,40–44 The exclusion of TBI patients without a CT indication combined with higher proportions of severely injured patients show that the CENTER-TBI study is not fully representative of the European TBI population.
As mentioned, the European TBI population is composed mostly of mild TBI patients, for whom CT is not always indicated, and neurosurgical interventions are required in <1%.45 Notwithstanding, stratification on injury severity in our study was based on the baseline clinical assessment wherein clinical deterioration was not accounted for. Additionally, the mild TBI population is a highly heterogeneous group, and although classified as mild, ∼50% do not reach full recovery 6 months after injury. The possibility of clinical deterioration combined with the heterogeneity of this population and possible presence of extracranial injury could explain their comparable need for inpatient rehabilitation and the observed inhospital mortality rate.46
Sex differences
We showed that male patients incurred higher total intramural costs, in almost all age and severity groups, than female patients. It is known that TBI most commonly affects younger adults, specifically men, causing substantial costs to society as a result of their death and disability.47–49 Common causes of trauma within the younger male population are road traffic incidents and interpersonal violence, mostly resulting in severe TBI and concomitant severe injury to the chest, abdomen, and extremities.50–52 Compared with patients with isolated TBI, defined as brain injury without concomitant severe extracranial injury, patients with severe extracranial injury have longer hospitalizations because of the necessity of continuing treatment for body sites other than the head.53 The presence of severe extracranial injury could lead to longer hospital LOS resulting in higher intramural costs and causing differences in costs between males and females. However, higher costs for male patients remained after adjustment for relevant confounders, including extracranial injury. Several studies have shown that in comparison to male TBI patients, female TBI patients have lower access to trauma centers and are less often admitted to the ICU. Regarding TBI guideline adherence, CT seems to be performed less often in women than in men.54–56 Within CENTER-TBI, differences in care pathways were most frequently observed in patients who sustained mild TBI, wherein women with comparable injury severity and demographic characteristics were more likely to be discharged home after presenting to the ER and were less likely to be admitted to the ICU.56 The differences in healthcare consumption and costs between males and females could therefore be explained by differences in management of TBI and suboptimal healthcare access among female TBI patients.
The elderly and TBI
We reported that an increase in age is associated with an increase in costs, which is line with previous studies showing that increasing age, severe brain injury, and extracranial injury are related to higher hospital costs.41,57 The cost pattern of the elderly did however, differ from the younger patient group, as they had shorter ICU LOS and lower costs for surgical interventions. The difference in healthcare consumption by the elderly could be explained by (1) mechanism of injury and (2) their pre-morbid health state.
In the elderly population, low energy falls are a common cause of TBI, which are most commonly adjoined by injuries to the lower extremities. Although these injuries are expected to incur higher costs, the need for critical care or emergency interventions remains low.49,58–60 Additionally, although most older patients initially had mild TBI, proportions of in-hospital mortality remained high.61 Because of vulnerability and pre-existing comorbidities, older adults are less likely to survive their TBI than are their younger counterparts, which could presumably lead to higher consumption of care during the end phase life.61,62
Between-country differences in healthcare consumption
In this study, we found some differences in LOS of TBI patients in the ICU and on the ward across countries. Although part of this difference could be explained by a different case mix of patients in each country, differences in ward and ICU LOS remained within each TBI severity level. When interpreting these differences, we should acknowledge that the design of CENTER-TBI, with enrollment of patients in three admission strata (ER, ward, and ICU) led to different recruitment procedures of TBI severities among countries (i.e. some countries enrolled only patients in the ICU stratum, meaning patients admitted directly to the ICU upon presentation). Although we performed extensive case-mix adjustment, we cannot exclude the possibility of remaining differences in the patient population. Besides differences in patient population, the observed between-country differences in healthcare consumption can still be for other reasons, such as the overall health status of the residential population, the proportion of patients with insurance, pharmaceutical costs, and personnel costs.63 Additionally, the economic development of a country determines the health spending per person.64 In general, differences in expenditure also affect the outcome of TBI patients, as lower- resource, developing countries experience significant higher mortality rates than the higher-resource countries.65 Using GDP-corrected prices, we have adjusted for this factor within this study. In addition to these economic factors, the organization of care and guidelines adaptation is an important key factor in healthcare expenditure. The difference in organization of care can result in a difference of guidelines being used; for example, it is known that some countries are more likely to perform CT scans in patients with mild TBI.54,66 Within TBI care, clinical guidelines are scarce and adherence is suboptimal, resulting in considerable between-country variation in treatment of TBI and subsequently different expenditure patterns across countries.54,67 A previous study has shown that there is considerable variation regarding ICU admission policies, especially in the mild TBI population, wherein it is unclear whether a liberal admission policy is truly benefiting the patient while costs are rising.68
Strength and limitations
The most important strength of this study is the availability of detailed data of high quality collected from several European countries. The data provide a detailed perspective for all severities of TBI, including data about different age groups with detailed clinical presentation, neuroimaging, and performed interventions. However, several limitations should be acknowledged. The CENTER-TBI study consisted mostly of trauma levels I and II hospitals, resulting in a population of relatively severely injured patients. This may not correctly represent the total TBI population in Europe, as trauma level I centers are known to have overall higher expenses resulting in higher costs.69 This, combined with the selective sampling per country, makes it overall difficult to interpret between-country differences.
Total costs were calculated using inflation- and GDP-corrected cost prices, as health financial systems are determinative of the care products` cost prices. Because of the use of inflation- and GDP-corrected prices in this study, we were able to compare the cost of TBI across countries, and focus on healthcare consumption rather than price differences. However, it should be noted that adjustment for GDP-PPP does not fully compensate for actual cost differences among countries. Second, our study did not include detailed information about the interventions in the first hospital for referred patients, despite the burden of TBI in acute care being substantial.11 With 17% of our study population consisting of secondary referrals, missing data on the total healthcare consumption in acute care setting at the referring hospital, could cause an underestimation of the total costs.
In our study, information on long-term healthcare consumption, such as outpatient rehabilitation care and outpatient clinic visits, was not available. Outpatient rehabilitation care and outpatient clinic visits are inevitably large contributors to the overall costs of TBI. After TBI, a range of problems can persist, including cognitive impairment, post-concussion symptoms, emotional difficulties, and functional limitations, requiring long-term outpatient care.46 A study conducted in the United States has shown that patients receiving inpatient rehabilitation still experience major health consequences 5 years after injury, wherein 12% were living in an institutional setting and almost 50% were readmitted to the hospital at least once.70 A study from New Zealand showed that in the first year after trauma, patients use their general practitioner in 36% of the cases, allied health in 18% of cases, and specialized services in 14% of cases, increasing respectively with TBI severity.20 In our study, we observed that inpatient rehabilitation accounted for 19% of the total costs across all TBI severities. This is most probably an underestimated contribution to the total costs, as a previous study has shown that the need for rehabilitation services is largely unmet within the TBI population.71 We should additionally acknowledge that the long-term consequences of TBI are the drivers of the indirect costs caused by loss of productivity, disability, and reduced quality of life.46 These indirect costs are contemplated to be the largest contributors to the overall costs related to TBI, indicating that the economic impact of TBI is even higher than shown in this study.
Recommendations
Intramural costs of TBI are significant, with hospital admission being the largest contributor. Costs increased with trauma severity, male patients incurred higher costs, and cost patterns of the elderly differed from those of the overall TBI population. This knowledge about healthcare expenses could be a leading step toward more cost-efficient TBI care. Hospitalization (ICU LOS in particular), incurs the highest costs and differs among countries. Improvements in resource allocation and eventual reduction of costs could be effected by the development of admission guidelines wherein only those who would truly benefit will be admitted to the ICU, combined with special attention to gender differences in assessment of patients. A leading step toward tailored and cost-effective TBI treatment, is, for example, the use of acute serum biomarkers to determine CT indication in mild TBI patients, thereby preventing unnecessary imaging.72 Additionally, discharge planning according to patient needs and preventive interventions targeting in-hospital complications are highly valuable in reducing unnecessary healthcare consumption. The long-term consequences of TBI are of substantial concern for the patient, the healthcare provider, and, eventually, society. Advanced care planning, wherein patients start early on with rehabilitation, could lead to reduction of hospitalization and better patient outcome, which will subsequently lead to a reduction of the indirect costs related to TBI. Differences in healthcare consumption between males and females should also be explored more extensively, as differences in the management of TBI could also lead to different outcomes. Conclusively, TBI patients must be considered as a distinct patient population, with targeted interventions that suit the different subgroups within TBI, in order to reduce costs.
Supplementary Material
Acknowledgments
We are grateful to all patients and investigators who participated in the CENTER-TBI study. Portions of this work were presented at the 15th International Neurotrauma Symposium, Berlin, Germany, July 17–20, 2022 and the 44th Annual North American Meeting for the Society of Medical Decision Making, October 23–26, 2022.
Contributor Information
Collaborators: CENTER-TBI Participants and Investigators
CENTER-TBI Participants and Investigators
Cecilia Åkerlund,1 Krisztina Amrein,2 Nada Andelic,3 Lasse Andreassen,4 Audny Anke,5 Anna Antoni,6 Gérard Audibert,7 Philippe Azouvi,8 Maria Luisa Azzolini,9 Ronald Bartels,10 Pál Barzó,11 Romuald Beauvais,12 Ronny Beer,13 Bo-Michael Bellander,14 Antonio Belli,15 Habib Benali,16 Maurizio Berardino,17 Luigi Beretta,9 Morten Blaabjerg,18 Peter Bragge,19 Alexandra Brazinova,20 Vibeke Brinck,21 Joanne Brooker,22 Camilla Brorsson,23 Andras Buki,24 Monika Bullinger,25 Manuel Cabeleira,26 Alessio Caccioppola,27 Emiliana Calappi,27 Maria Rosa Calvi,9 Peter Cameron,28 Guillermo Carbayo Lozano,29 Marco Carbonara,27 Simona Cavallo,17 Giorgio Chevallard,30 Arturo Chieregato,30 Giuseppe Citerio,31,32 Hans Clusmann,33 Mark Coburn,34 Jonathan Coles,35 Jamie D. Cooper,36 Marta Correia,37 Amra Čović,38 Nicola Curry,39 Endre Czeiter,24 Marek Czosnyka,26 Claire Dahyot-Fizelier,40 Paul Dark,41 Helen Dawes,42 Véronique De Keyser,43 Vincent Degos,16 Francesco Della Corte,44 Hugo den Boogert,10 Bart Depreitere,45 Đula Đilvesi,46 Abhishek Dixit,47 Emma Donoghue,22 Jens Dreier,48 Guy-Loup Dulière,49 Ari Ercole,47 Patrick Esser,42 Erzsébet Ezer,50 Martin Fabricius,51 Valery L. Feigin,52 Kelly Foks,53 Shirin Frisvold,54 Alex Furmanov,55 Pablo Gagliardo,56 Damien Galanaud,16 Dashiell Gantner,28 Guoyi Gao,57 Pradeep George,58 Alexandre Ghuysen,59 Lelde Giga,60 Ben Glocker,61 Jagoš Golubovic,46 Pedro A. Gomez,62 Johannes Gratz,63 Benjamin Gravesteijn,64 Francesca Grossi,44 Russell L. Gruen,65 Deepak Gupta,66 Juanita A. Haagsma,64 Iain Haitsma,67 Raimund Helbok,13 Eirik Helseth,68 Lindsay Horton,69 Jilske Huijben,64 Peter J. Hutchinson,70 Bram Jacobs,71 Stefan Jankowski,72 Mike Jarrett,21 Ji-yao Jiang,58 Faye Johnson,73 Kelly Jones,52 Mladen Karan,46 Angelos G. Kolias,70 Erwin Kompanje,74 Daniel Kondziella,51 Evgenios Kornaropoulos,47 Lars-Owe Koskinen,75 Noémi Kovács,76 Ana Kowark,77 Alfonso Lagares,62 Linda Lanyon,58 Steven Laureys,78 Fiona Lecky,79,80 Didier Ledoux,78 Rolf Lefering,81 Valerie Legrand,82 Aurelie Lejeune,83 Leon Levi,84 Roger Lightfoot,85 Hester Lingsma,64 Andrew I.R. Maas,43 Ana M. Castaño-León,62 Marc Maegele,86 Marek Majdan,20 Alex Manara,87 Geoffrey Manley,88 Costanza Martino,89 Hugues Maréchal,49 Julia Mattern,90 Catherine McMahon,91 Béla Melegh,92 David Menon,47 Tomas Menovsky,43 Ana Mikolic,64 Benoit Misset,78 Visakh Muraleedharan,58 Lynnette Murray,28 Ancuta Negru,93 David Nelson,1 Virginia Newcombe,47 Daan Nieboer,64 József Nyirádi,2 Otesile Olubukola,79 Matej Oresic,94 Fabrizio Ortolano,27 Aarno Palotie,95, 96, 97 Paul M. Parizel,98 Jean-François Payen,99 Natascha Perera,12 Vincent Perlbarg,16 Paolo Persona,100 Wilco Peul,101 Anna Piippo-Karjalainen,102 Matti Pirinen,95 Dana Pisica,64 Horia Ples,93 Suzanne Polinder,64 Inigo Pomposo,29 Jussi P. Posti,103 Louis Puybasset,104 Andreea Radoi,105 Arminas Ragauskas,106 Rahul Raj,102 Malinka Rambadagalla,107 Isabel Retel Helmrich,64 Jonathan Rhodes,108 Sylvia Richardson,109 Sophie Richter,47 Samuli Ripatti,95 Saulius Rocka,106 Cecilie Roe,110 Olav Roise,111,112 Jonathan Rosand,113 Jeffrey V. Rosenfeld,114 Christina Rosenlund,115 Guy Rosenthal,55 Rolf Rossaint,77 Sandra Rossi,100 Daniel Rueckert,61 Martin Rusnák,116 Juan Sahuquillo,105 Oliver Sakowitz,90,117 Renan Sanchez-Porras,117 Janos Sandor,118 Nadine Schäfer,81 Silke Schmidt,119 Herbert Schoechl,120 Guus Schoonman,121 Rico Frederik Schou,122 Elisabeth Schwendenwein,6 Charlie Sewalt,64 Ranjit D. Singh,101 Toril Skandsen,123,124 Peter Smielewski,26 Abayomi Sorinola,125 Emmanuel Stamatakis,47 Simon Stanworth,39 Robert Stevens,126 William Stewart,127 Ewout W. Steyerberg,64,128 Nino Stocchetti,129 Nina Sundström,130 Riikka Takala,131 Viktória Tamás,125 Tomas Tamosuitis,132 Mark Steven Taylor,20 Aurore Thibaut,78 Braden Te Ao,52 Olli Tenovuo,103 Alice Theadom,52 Matt Thomas,87 Dick Tibboel,133 Marjolein Timmers,74 Christos Tolias,134 Tony Trapani,28 Cristina Maria Tudora,93 Andreas Unterberg,90 Peter Vajkoczy,135 Shirley Vallance,28 Egils Valeinis,60 Zoltán Vámos,50 Mathieu van der Jagt,136 Gregory Van der Steen,43 Joukje van der Naalt,71 Jeroen T.J.M. van Dijck,101 Inge A. M. van Erp,101 Thomas A. van Essen,101 Wim Van Hecke,137 Caroline van Heugten,138 Dominique Van Praag,139 Ernest van Veen,64 Thijs Vande Vyvere,137 Roel P. J. van Wijk,101 Alessia Vargiolu,32 Emmanuel Vega,83 Kimberley Velt,64 Jan Verheyden,137 Paul M. Vespa,140 Anne Vik,123,141 Rimantas Vilcinis,132 Victor Volovici,67 Nicole von Steinbüchel,38 Daphne Voormolen,64 Petar Vulekovic,46 Kevin K.W. Wang,142 Daniel Whitehouse,47 Eveline Wiegers,64 Guy Williams,47 Lindsay Wilson,69 Stefan Winzeck,47 Stefan Wolf,143 Zhihui Yang,113 Peter Ylén,144 Alexander Younsi,90 Frederick A. Zeiler,47,145 Veronika Zelinkova,20 Agate Ziverte,60 Tommaso Zoerle27
1Department of Physiology and Pharmacology, Section of Perioperative Medicine and Intensive Care, Karolinska Institutet, Stockholm, Sweden
2János Szentágothai Research Centre, University of Pécs, Pécs, Hungary
3Division of Clinical Neuroscience, Department of Physical Medicine and Rehabilitation, Oslo University Hospital and University of Oslo, Oslo, Norway
4Department of Neurosurgery, University Hospital Northern Norway, Tromso, Norway
5Department of Physical Medicine and Rehabilitation, University Hospital Northern Norway, Tromso, Norway
6Trauma Surgery, Medical University Vienna, Vienna, Austria
7Department of Anesthesiology & Intensive Care, University Hospital Nancy, Nancy, France
8Raymond Poincare hospital, Assistance Publique –Hopitaux de Paris, Paris, France
9Department of Anesthesiology & Intensive Care, S Raffaele University Hospital, Milan, Italy
10Department of Neurosurgery, Radboud University Medical Center, Nijmegen, The Netherlands
11Department of Neurosurgery, University of Szeged, Szeged, Hungary
12International Projects Management, ARTTIC, Munchen, Germany
13Department of Neurology, Neurological Intensive Care Unit, Medical University of Innsbruck, Innsbruck, Austria
14Department of Neurosurgery & Anesthesia & intensive care medicine, Karolinska University Hospital, Stockholm, Sweden
15NIHR Surgical Reconstruction and Microbiology Research Centre, Birmingham, UK
16Anesthesie-Réanimation, Assistance Publique – Hopitaux de Paris, Paris, France
17Department of Anesthesia & ICU, AOU Città della Salute e della Scienza di Torino - Orthopedic and Trauma Center, Torino, Italy
18Department of Neurology, Odense University Hospital, Odense, Denmark
19BehaviourWorks Australia, Monash Sustainability Institute, Monash University, Victoria, Australia
20Department of Public Health, Faculty of Health Sciences and Social Work, Trnava University, Trnava, Slovakia
21Quesgen Systems Inc., Burlingame, California, USA
22Australian & New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia
23Department of Surgery and Perioperative Science, Umeå University, Umeå, Sweden
24Department of Neurosurgery, Medical School, University of Pécs, Hungary and Neurotrauma Research Group, János Szentágothai Research Centre, University of Pécs, Hungary
25Department of Medical Psychology, Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany
26Brain Physics Lab, Division of Neurosurgery, Dept of Clinical Neurosciences, University of Cambridge, Addenbrooke's Hospital, Cambridge, UK
27Neuro ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy
28ANZIC Research Centre, Monash University, Department of Epidemiology and Preventive Medicine, Melbourne, Victoria, Australia
29Department of Neurosurgery, Hospital of Cruces, Bilbao, Spain
30NeuroIntensive Care, Niguarda Hospital, Milan, Italy
31School of Medicine and Surgery, Università Milano Bicocca, Milano, Italy
32NeuroIntensive Care Unit, Department Neuroscience, IRCCS Fondazione San Gerardo dei Tintori, Monza, Italy
33Department of Neurosurgery, Medical Faculty RWTH Aachen University, Aachen, Germany
34Department of Anesthesiology and Intensive Care Medicine, University Hospital Bonn, Bonn, Germany
35Department of Anesthesia & Neurointensive Care, Cambridge University Hospital NHS Foundation Trust, Cambridge, UK
36School of Public Health & PM, Monash University and The Alfred Hospital, Melbourne, Victoria, Australia
37Radiology/MRI department, MRC Cognition and Brain Sciences Unit, Cambridge, UK
38Institute of Medical Psychology and Medical Sociology, Universitätsmedizin Göttingen, Göttingen, Germany
39Oxford University Hospitals NHS Trust, Oxford, UK
40Intensive Care Unit, CHU Poitiers, Potiers, France
41University of Manchester NIHR Biomedical Research Centre, Critical Care Directorate, Salford Royal Hospital NHS Foundation Trust, Salford, UK
42Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK
43Department of Neurosurgery, Antwerp University Hospital and University of Antwerp, Edegem, Belgium
44Department of Anesthesia & Intensive Care, Maggiore Della Carità Hospital, Novara, Italy
45Department of Neurosurgery, University Hospitals Leuven, Leuven, Belgium
46Department of Neurosurgery, Clinical centre of Vojvodina, Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
47Division of Anaesthesia, University of Cambridge, Addenbrooke's Hospital, Cambridge, UK
48Center for Stroke Research Berlin, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
49Intensive Care Unit, CHR Citadelle, Liège, Belgium
50Department of Anaesthesiology and Intensive Therapy, University of Pécs, Pécs, Hungary
51Departments of Neurology, Clinical Neurophysiology and Neuroanesthesiology, Region Hovedstaden Rigshospitalet, Copenhagen, Denmark
52National Institute for Stroke and Applied Neurosciences, Faculty of Health and Environmental Studies, Auckland University of Technology, Auckland, New Zealand
53Department of Neurology, Erasmus MC, Rotterdam, the Netherlands
54Department of Anesthesiology and Intensive care, University Hospital Northern Norway, Tromso, Norway
55Department of Neurosurgery, Hadassah-hebrew University Medical center, Jerusalem, Israel
56Fundación Instituto Valenciano de Neurorrehabilitación (FIVAN), Valencia, Spain
57Department of Neurosurgery, Shanghai Renji hospital, Shanghai Jiaotong University/school of medicine, Shanghai, China
58Karolinska Institutet, INCF International Neuroinformatics Coordinating Facility, Stockholm, Sweden
59Emergency Department, CHU, Liège, Belgium
60Neurosurgery clinic, Pauls Stradins Clinical University Hospital, Riga, Latvia
61Department of Computing, Imperial College London, London, UK
62Department of Neurosurgery, Hospital Universitario 12 de Octubre, Madrid, Spain
63Department of Anesthesia, Critical Care and Pain Medicine, Medical University of Vienna, Austria
64Department of Public Health, Erasmus Medical Center-University Medical Center, Rotterdam, The Netherlands
65College of Health and Medicine, Australian National University, Canberra, Australia
66Department of Neurosurgery, Neurosciences Centre & JPN Apex trauma centre, All India Institute of Medical Sciences, New Delhi-110029, India
67Department of Neurosurgery, Erasmus MC, Rotterdam, the Netherlands
68Department of Neurosurgery, Oslo University Hospital, Oslo, Norway
69Division of Psychology, University of Stirling, Stirling, UK
70Division of Neurosurgery, Department of Clinical Neurosciences, Addenbrooke's Hospital & University of Cambridge, Cambridge, UK
71Department of Neurology, University of Groningen, University Medical Center Groningen, Groningen, Netherlands
72Neurointensive Care, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
73Salford Royal Hospital NHS Foundation Trust Acute Research Delivery Team, Salford, UK
74Department of Intensive Care and Department of Ethics and Philosophy of Medicine, Erasmus Medical Center, Rotterdam, The Netherlands
75Department of Clinical Neuroscience, Neurosurgery, Umeå University, Umeå, Sweden
76Hungarian Brain Research Program - Grant No. KTIA_13_NAP-A-II/8, University of Pécs, Pécs, Hungary
77Department of Anaesthesiology, University Hospital of Aachen, Aachen, Germany
78Cyclotron Research Center , University of Liège, Liège, Belgium
79Centre for Urgent and Emergency Care Research (CURE), Health Services Research Section, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK
80Emergency Department, Salford Royal Hospital, Salford UK
81Institute of Research in Operative Medicine (IFOM), Witten/Herdecke University, Cologne, Germany
82VP Global Project Management CNS, ICON, Paris, France
83Department of Anesthesiology-Intensive Care, Lille University Hospital, Lille, France
84Department of Neurosurgery, Rambam Medical Center, Haifa, Israel
85Department of Anesthesiology & Intensive Care, University Hospitals Southhampton NHS Trust, Southhampton, UK
86Cologne-Merheim Medical Center (CMMC), Department of Traumatology, Orthopedic Surgery and Sportmedicine, Witten/Herdecke University, Cologne, Germany
87Intensive Care Unit, Southmead Hospital, Bristol, Bristol, UK
88Department of Neurological Surgery, University of California, San Francisco, California, USA
89Department of Anesthesia & Intensive Care,M. Bufalini Hospital, Cesena, Italy
90Department of Neurosurgery, University Hospital Heidelberg, Heidelberg, Germany
91Department of Neurosurgery, The Walton centre NHS Foundation Trust, Liverpool, UK
92Department of Medical Genetics, University of Pécs, Pécs, Hungary
93Department of Neurosurgery, Emergency County Hospital Timisoara , Timisoara, Romania
94School of Medical Sciences, Örebro University, Örebro, Sweden
95Institute for Molecular Medicine Finland, University of Helsinki, Helsinki, Finland
96Analytic and Translational Genetics Unit, Department of Medicine; Psychiatric & Neurodevelopmental Genetics Unit, Department of Psychiatry; Department of Neurology, Massachusetts General Hospital, Boston, MA, USA
97Program in Medical and Population Genetics; The Stanley Center for Psychiatric Research, The Broad Institute of MIT and Harvard, Cambridge, MA, USA
98Department of Radiology, University of Antwerp, Edegem, Belgium
99Department of Anesthesiology & Intensive Care, University Hospital of Grenoble, Grenoble, France
100Department of Anesthesia & Intensive Care, Azienda Ospedaliera Università di Padova, Padova, Italy
101Dept. of Neurosurgery, Leiden University Medical Center, Leiden, The Netherlands and Dept. of Neurosurgery, Medical Center Haaglanden, The Hague, The Netherlands
102Department of Neurosurgery, Helsinki University Central Hospital
103Division of Clinical Neurosciences, Department of Neurosurgery and Turku Brain Injury Centre, Turku University Hospital and University of Turku, Turku, Finland
104Department of Anesthesiology and Critical Care, Pitié -Salpêtrière Teaching Hospital, Assistance Publique, Hôpitaux de Paris and University Pierre et Marie Curie, Paris, France
105Neurotraumatology and Neurosurgery Research Unit (UNINN), Vall d'Hebron Research Institute, Barcelona, Spain
106Department of Neurosurgery, Kaunas University of technology and Vilnius University, Vilnius, Lithuania
107Department of Neurosurgery, Rezekne Hospital, Latvia
108Department of Anaesthesia, Critical Care & Pain Medicine NHS Lothian & University of Edinburg, Edinburgh, UK
109Director, MRC Biostatistics Unit, Cambridge Institute of Public Health, Cambridge, UK
110Department of Physical Medicine and Rehabilitation, Oslo University Hospital/University of Oslo, Oslo, Norway
111Division of Orthopedics, Oslo University Hospital, Oslo, Norway
112Institue of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, Norway
113Broad Institute, Cambridge MA Harvard Medical School, Boston MA, Massachusetts General Hospital, Boston MA, USA
114National Trauma Research Institute, The Alfred Hospital, Monash University, Melbourne, Victoria, Australia
115Department of Neurosurgery, Odense University Hospital, Odense, Denmark
116International Neurotrauma Research Organisation, Vienna, Austria
117Klinik für Neurochirurgie, Klinikum Ludwigsburg, Ludwigsburg, Germany
118Division of Biostatistics and Epidemiology, Department of Preventive Medicine, University of Debrecen, Debrecen, Hungary
119Department Health and Prevention, University Greifswald, Greifswald, Germany
120Department of Anaesthesiology and Intensive Care, AUVA Trauma Hospital, Salzburg, Austria
121Department of Neurology, Elisabeth-TweeSteden Ziekenhuis, Tilburg, the Netherlands
122Department of Neuroanesthesia and Neurointensive Care, Odense University Hospital, Odense, Denmark
123Department of Neuromedicine and Movement Science, Norwegian University of Science and Technology, NTNU, Trondheim, Norway
124Department of Physical Medicine and Rehabilitation, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
125Department of Neurosurgery, University of Pécs, Pécs, Hungary
126Division of Neuroscience Critical Care, John Hopkins University School of Medicine, Baltimore, USA
127Department of Neuropathology, Queen Elizabeth University Hospital and University of Glasgow, Glasgow, UK
128Dept. of Department of Biomedical Data Sciences, Leiden University Medical Center, Leiden, The Netherlands
129Department of Pathophysiology and Transplantation, Milan University, and Neuroscience ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Ital
130Department of Radiation Sciences, Biomedical Engineering, Umeå University, Umeå, Sweden
131Perioperative Services, Intensive Care Medicine and Pain Management, Turku University Hospital and University of Turku, Turku, Finland
132Department of Neurosurgery, Kaunas University of Health Sciences, Kaunas, Lithuania
133Intensive Care and Department of Pediatric Surgery, Erasmus Medical Center, Sophia Children's Hospital, Rotterdam, The Netherlands
134Department of Neurosurgery, Kings college London, London, UK
135Neurologie, Neurochirurgie und Psychiatrie, Charité – Universitätsmedizin Berlin, Berlin, Germany
136Department of Intensive Care Adults, Erasmus MC– University Medical Center Rotterdam, Rotterdam, the Netherlands
137icoMetrix NV, Leuven, Belgium
138Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK
139Psychology Department, Antwerp University Hospital, Edegem, Belgium
140Director of Neurocritical Care, University of California, Los Angeles, USA
141Department of Neurosurgery, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
142Department of Emergency Medicine, University of Florida, Gainesville, Florida, USA
143Department of Neurosurgery, Charité– Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany
144VTT Technical Research Centre, Tampere, Finland
145Section of Neurosurgery, Department of Surgery, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada.
Authors' Contributions
Z.L. Rana Kaplan was responsible for formal analysis, methodology, visualization, and writing – original draft. Marjolein van der Vlegel was responsible for formal analysis, methodology, and writing – original draft. Jeroen T.J.M. van Dijck was responsible for formal analysis, methodology, and writing – original draft. Dana Pisică was responsible for writing – review & editing. Nikki van Leeuwen was responsible for writing – review & editing. Hester F. Lingsma was responsible for writing – review & editing. Ewout W. Steyerberg was responsible for writing – review & editing. Juanita A. Haagsma was responsible for writing – review & editing. Marek Majdan was responsible for writing – review & editing. Suzanne Polinder was responsible for conceptualization, project administration, supervision, methodology, and writing – review & editing. All authors read and approved the final manuscript.
Ethical Approval Statement
The CENTER-TBI study (EC grant 602150) has been conducted in accordance with all relevant laws of the European Union if directly applicable or if of direct effect, and in accordance with all relevant laws of the country where the recruiting sites were located, including but not limited to, the relevant privacy and data protection laws and regulations (the “Privacy Law”), the relevant laws and regulations on the use of human materials, and all relevant guidance relating to clinical studies from time to time in force including, but not limited to, the ICH Harmonised Tripartite Guideline for Good Clinical Practice (CPMP/ICH/135/95) (ICH GCP) and the World Medical Association Declaration of Helsinki entitled “Ethical Principles for Medical Research Involving Human Subjects.” Informed consent by the patients and/or the legal representative/next of kin was obtained according to local legislation, for all patients recruited in the core data set of CENTER-TBI and documented in the eCRF. Ethical approval was obtained for each recruiting site. The list of sites, ethical committees, approval numbers, and approval dates can be found on https://www.center-tbi.eu/project/ethical-approval
Funding Information
CENTER-TBI was supported by the European Union 7th Framework program (EC Grant 602150). Additional funding was obtained from the Hannelore Kohl Stiftung (project no 2014014) (Germany), from OneMind (USA), and from Integra LifeSciences Corporation (USA).
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 2017;16(12):987–1048; doi: 10.1016/S1474-4422(17)30371-X [DOI] [PubMed] [Google Scholar]
- 2. Majdan M, Plancikova D, Brazinova A, et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health 2016;1(2):e76–e83; doi: 10.1016/S2468-2667(16)30017-2 [DOI] [PubMed] [Google Scholar]
- 3. Feigin VL, Theadom A, Barker-Collo S, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol 2013;12(1):53–64; doi: 10.1016/S1474-4422(12)70262-4 [DOI] [PubMed] [Google Scholar]
- 4. Brazinova A, Rehorcikova V, Taylor MS, et al. Epidemiology of traumatic brain injury in Europe: a living systematic review. J Neurotrauma 2021;38(10):1411–1440; doi: 10.1089/neu.2015.4126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kleiven S, Peloso PMJ, Holst HV. The epidemiology of head injuries in Sweden from 1987 to 2000. Inj Control Saf Promot 2003;10:173–180; doi: 10.1076/icsp.10.3.173.14552 [DOI] [PubMed] [Google Scholar]
- 6. Koskinen S AH. Traumatic brain injury in Finland 1991–2005: a nationwide register study of hospitalized and fatal TBI. Brain Inj 2008;22:205–214; doi: 10.1080/02699050801938975 [DOI] [PubMed] [Google Scholar]
- 7. Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol 2008;7(8):728-741; doi: 10.1016/S1474-4422(08)70164-9 [DOI] [PubMed] [Google Scholar]
- 8. Maas AI, Menon DK, Steyerberg EW, et al. Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): a prospective longitudinal observational study. Neurosurgery 2015;76(1):67–80; doi: 10.1227/NEU.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 9. Faul M, Wald MM, Rutland-Brown W, et al. Using a cost-benefit analysis to estimate outcomes of a clinical treatment guideline: testing the Brain Trauma Foundation guidelines for the treatment of severe traumatic brain injury. J Trauma 2007;63(6):1271–8; doi: 10.1097/TA.0b013e3181493080 [DOI] [PubMed] [Google Scholar]
- 10. Berg J, Tagliaferri F, Servadei F. Cost of trauma in Europe. Eur J Neurol 2005;12 (Suppl. 1):85–90; doi: 10.1111/j.1468-1331.2005.01200.x [DOI] [PubMed] [Google Scholar]
- 11. McGarry LJ, Thompson D, Millham FH, et al. Outcomes and costs of acute treatment of traumatic brain injury. J Trauma 2002;53(6):1152–1159; doi: 10.1097/00005373-200212000-00020 [DOI] [PubMed] [Google Scholar]
- 12. Lu J, Roe C, Aas E, et al. Traumatic brain injury: methodological approaches to estimate health and economic outcomes. J Neurotrauma 2013;30(23):1925–1933; doi: 10.1089/neu.2013.2891 [DOI] [PubMed] [Google Scholar]
- 13. Parlementary letter, Ministry of Health 2016. Available from: https://www.rijksoverheid.nl/documenten/kamerstuk ken/2016/01/28/kamerbrief-over-beeindiging-sluis-nivolumab-per-1-maart-2016 [Last Accessed: September 1, 2022].
- 14. Alali AS, Burton K, Fowler RA, et al. Economic evaluations in the diagnosis and management of traumatic brain injury: a systematic review and analysis of quality. Value Health 2015;18(5):721–734; doi: 10.1016/j.jval.2015.04.012 [DOI] [PubMed] [Google Scholar]
- 15. WHO. Health workforce. Available from: https://www.who.int/health-topics/health-workforce#tab=tab_1 [Last Accessed: September 1, 2022].
- 16. van Dijck J, Mostert CQB, Greeven APA, et al. Functional outcome, in-hospital healthcare consumption and in-hospital costs for hospitalised traumatic brain injury patients: a Dutch prospective multicentre study. Acta Neurochir (Wien) 2020;162(7):1607–1618; doi: 10.1007/s00701-020-04384-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Dijck J, Dijkman MD, Ophuis RH, et al. In-hospital costs after severe traumatic brain injury: a systematic review and quality assessment. PLoS One 2019;14(5):e0216743; doi: 10.1371/journal.pone.0216743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farhad K, Khan HMR, Ji AB, et al. Trends in outcomes and hospitalization costs for traumatic brain injury in adult patients in the United States. J Neurotrauma 2013;30(2):84–90; doi: 10.1089/neu.2011.2283 [DOI] [PubMed] [Google Scholar]
- 19. Marin JR, Weaver MD, Mannix RC. Burden of USA hospital charges for traumatic brain injury. Brain Inj 2017;31(1):24–31; doi: 10.1080/02699052.2016.1217351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Te Ao B, Brown P, Tobias M, et al. Cost of traumatic brain injury in New Zealand. Evidence from a population-based study 2014;83(18):1645–1652; doi: 10.1212/wnl.0000000000000933 [DOI] [PubMed] [Google Scholar]
- 21. Tuominen R, Joelsson P, Tenovuo O. Treatment costs and productivity losses caused by traumatic brain injuries. Brain Inj 2012;26:1697–1701; doi: 10.3109/02699052.2012.722256 [DOI] [PubMed] [Google Scholar]
- 22. Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res 2012;43(4):299–307; doi: 10.1016/j.jsr.2012.08.011 [DOI] [PubMed] [Google Scholar]
- 23. CENTER-TBI. Ethical Approval. 2016. Available from: https://www.center-tbi.eu/project/ethical-approval [Last Accessed: 22 June 2022].
- 24. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974;2(7872):81–84, doi: 10.1016/s0140-6736(74)91639-0 [DOI] [PubMed] [Google Scholar]
- 25. Baker SP, O'Neill B, Haddon WJR, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma: Inj Infect Crit Care 1974;14(3):187–196. [PubMed] [Google Scholar]
- 26. Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status - historical perspectives and modern developments. Anaesthesia 2019;74(3):373–379; doi: 10.1111/anae.14569 [DOI] [PubMed] [Google Scholar]
- 27. MacKenzie EJ, Shapiro S, Eastham JN. The Abbreviated Injury Scale and Injury Severity Score. Levels of inter- and intrarater reliability. Med Care 1985;23(6):823–835; doi: 10.1097/00005650-198506000-00008 [DOI] [PubMed] [Google Scholar]
- 28. European Commission. Remuneration of Researchers in the Public and Private sectors 2011. [Google Scholar]
- 29. Hakkaart-van Roijen L, van der Linden N, Bouwmans C, Kanters T, Tan SS. [Kostenhandleiding: Methodologie van kostenonderzoek en referentieprijzen voor economische evaluaties in de gezondheidszorg. Zorginstituut Nederland. 2015]. Dutch Guidelines: Methodology of cost research and reference prices for economic evaluations in health care. Dutch National Healthcare institute; 2015. [Google Scholar]
- 30. Dutch Healthcare Authority. Open data from the Dutch Healthcare Authority. 2014–2023 [Nederlandse Zorgautoriteit. Open data van de Nederlandse Zorgautoriteit.] Available from: http://www.opendisdata.nl [Last Accessed: 6 September 2019].
- 31. Dutch Healthcare Authority. Healthcare products. [Nederlandse Zorgautoriteit. Zorgproducten.] Available from: https://zorgproducten.nza.nl/Home.aspx [Last Accessed: 6 September 2019].
- 32. Statistics Netherlands. Annual change consumer price index; from 1963 [Centraal Bureau voor de Statistiek. Jaarmutatie consumentenprijsindex; vanaf 1963.] Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/70936ned/table?ts=1551859688904 [Last Accessed: 6 September 2019].
- 33. Organization for Economic Co-operation and Development (OECD). Purchasing Power Parities for GDP and related indicators. Available from: https://stats.oecd.org/Index.aspx?DataSetCode=PPPGDP [Last Accessed: 1 October 2020].
- 34. Buuren S, Groothuis-Oudshoorn C. MICE: Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45; doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 35. Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med 2008;5(8):e165; doi: 10.1371/journal.pmed.0050165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Barber JTS. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 2004;9(4):197–204; doi: 10.1258/1355819042250249 [DOI] [PubMed] [Google Scholar]
- 37. RStudio Team. RStudio: Integrated Development for R. Rstudio, PBC MA: Boston; 2020. [Google Scholar]
- 38. StataCorp. Stata Statistical Software: Release 17. TX: StataCorp LLC: College Station; 2021. [Google Scholar]
- 39. Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg 2018;1–18, doi: 10.3171/2017.10.JNS17352 [DOI] [PubMed] [Google Scholar]
- 40. Fountain DM, Kolias AG, Laing RJ, et al. The financial outcome of traumatic brain injury: a single centre study. Br J Neurosurg 2017;31(3):350–355; doi: 10.1080/02688697.2016.1244254 [DOI] [PubMed] [Google Scholar]
- 41. Morris S, Ridley S, Lecky FE, et al. Determinants of hospital costs associated with traumatic brain injury in England and Wales. Anaesthesia 2008;63(5):499–508; doi: 10.1111/j.1365-2044.2007.05432.x [DOI] [PubMed] [Google Scholar]
- 42. Ponsford JL, Spitz G, Cromarty F, et al. Costs of care after traumatic brain injury. J Neurotrauma 2013;30(17):1498–505; doi: 10.1089/neu.2012.2843 [DOI] [PubMed] [Google Scholar]
- 43. Raj R, Bendel S, Reinikainen M, et al. Costs, outcome and cost-effectiveness of neurocritical care: a multi-center observational study. Crit Care 2018;22(1):225; doi: 10.1186/s13054-018-2151-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tardif PA, Moore L, Boutin A, et al. Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: a retrospective multicenter cohort study. Injury 2017;48(1):94–100; doi: 10.1016/j.injury.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 45. Jagoda AS, Bazarian JJ, Bruns JJJr., et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med 2008;52(6):714–748; doi: 10.1016/j.annemergmed.2008.08.021 [DOI] [PubMed] [Google Scholar]
- 46. Bramlett HM, Dietrich WD. Long-term consequences of traumatic brain injury: current status of potential mechanisms of injury and neurological outcomes. J Neurotrauma 2015;32(23):1834–1848; doi: 10.1089/neu.2014.3352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Faul M XL, Wald M, Coronado V. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths, 2002–2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta; 2010. [Google Scholar]
- 48. Polinder S, Meerding WJ, Mulder S, et al. Assessing the burden of injury in six European countries. Bull World Health Organ 2007;85(1):27–34; doi: 10.2471/blt.06.030973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Polinder S, Meerding WJ, van Baar ME, et al. Cost estimation of injury-related hospital admissions in 10 European countries. J Trauma 2005;59(6):1283–1291; doi: 10.1097/01.ta.0000195998.11304.5b [DOI] [PubMed] [Google Scholar]
- 50. MRC CRASH Trial Collaborators, Perel P, Arango M, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 2008;336(7641):425–429; doi: 10.1136/bmj.39461.643438.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Heinzelmann M, Platz A, Imhof HG. Outcome after acute extradural haematoma, influence of additional injuries and neurological complications in the ICU. Injury 1996;27(5):345–349; doi: 10.1016/0020-1383(95)00223-5 [DOI] [PubMed] [Google Scholar]
- 52. Lawrence T, Helmy A, Bouamra O, et al. Traumatic brain injury in England and Wales: prospective audit of epidemiology, complications and standardised mortality. BMJ Open 2016;6(11):e012197; doi: 10.1136/bmjopen-2016-012197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Watanabe T, Kawai Y, Iwamura A, et al. Outcomes after traumatic brain injury with concomitant severe extracranial injuries. Neurol Med Chir (Tokyo) 2018;58(9):393–399; doi: 10.2176/nmc.oa.2018-0116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Cnossen MC, Scholten AC, Lingsma HF, et al. Adherence to guidelines in adult patients with traumatic brain injury: a living systematic review. J Neurotrauma 2021;38(8):1072–1085; doi: 10.1089/neu.2015.4121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gomez D, Haas B, de Mestral C, et al. Gender-associated differences in access to trauma center care: a population-based analysis. Surgery 2012;152(2):179–185; doi: 10.1016/j.surg.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 56. Mikolić A, van Klaveren D, Groeniger JO, et al. Differences between men and women in treatment and outcome after traumatic brain injury. J Neurotrauma 2021;38(2):235–251; doi: 10.1089/neu.2020.7228 [DOI] [PubMed] [Google Scholar]
- 57. Spitz G, McKenzie D, Attwood D, et al. Cost prediction following traumatic brain injury: model development and validation. J Neurol Neurosurg Psychiatry 2016;87(2):173–180; doi: 10.1136/jnnp-2014-309479 [DOI] [PubMed] [Google Scholar]
- 58. Albrecht JS, Slejko JF, Stein DM, et al. Treatment charges for traumatic brain injury among older adults at a trauma center. J Head Trauma Rehabil 2017;32(6):E45–E53; doi: 10.1097/HTR.0000000000000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Peeters W, van den Brande R, Polinder S, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien) 2015;157(10):1683–1696; doi: 10.1007/s00701-015-2512-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lecky FE, Otesile O, Marincowitz C, et al. The burden of traumatic brain injury from low-energy falls among patients from 18 countries in the CENTER-TBI registry: a comparative cohort study. PLoS Med 2021;18(9):e1003761; doi: 10.1371/journal.pmed.1003761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Coronado VG, Thomas KE, Sattin RW, et al. The CDC traumatic brain injury surveillance system: characteristics of persons aged 65 years and older hospitalized with a TBI. J Head Trauma Rehabil 2005;20(3):215–228; doi: 10.1097/00001199-200505000-00005 [DOI] [PubMed] [Google Scholar]
- 62. Wang CY, Chen YC, Chien TH, et al. Impact of comorbidities on the prognoses of trauma patients: analysis of a hospital-based trauma registry database. PLoS One 2018;13(3):e0194749; doi: 10.1371/journal.pone.0194749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA 2018;319(10):1024–1039; doi: 10.1001/jama.2018.1150 [DOI] [PubMed] [Google Scholar]
- 64. Dieleman J, Campbell M, Chapin A, et al. Evolution and patterns of global health financing 1995–2014: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. Lancet 2017;389:1953–2080; doi: 10.1016/s0140-6736(17)30874-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Georgoff P, Meghan S, Mirza K, et al. Geographic variation in outcomes from severe traumatic brain injury. World Neurosurg 2010;74(2–3):331–345; doi: 10.1016/j.wneu.2010.03.025 [DOI] [PubMed] [Google Scholar]
- 66. Haydon NB. Head injury: audit of a clinical guideline to justify head CT. J Med Imaging Radiat Oncol 2013;57(2):161–168; doi: 10.1111/1754-9485.12007 [DOI] [PubMed] [Google Scholar]
- 67. Cnossen MC, Polinder S, Andriessen TM, et al. Causes and consequences of treatment variation in moderate and severe traumatic brain injury: a multicenter study. Crit Care Med 2017;45(4):660–669; doi: 10.1097/CCM.0000000000002263 [DOI] [PubMed] [Google Scholar]
- 68. Volovici V, Ercole A, Citerio G, et al. Intensive care admission criteria for traumatic brain injury patients across Europe. J Crit Care 2019;49:158–161; doi: 10.1016/j.jcrc.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 69. Davis KL, Joshi AV, Tortella BJ, et al. The direct economic burden of blunt and penetrating trauma in a managed care population. J Trauma 2007;62(3):622–630; doi: 10.1097/TA.0b013e318031afe3 [DOI] [PubMed] [Google Scholar]
- 70. Corrigan JD, Cuthbert JP, Harrison-Felix Cet al. US Population Estimates of Health and Social Outcomes 5 Years After Rehabilitation for Traumatic Brain Injury. J Head Trauma Rehab 2014;29(6):E1–E9; doi: 10.1097/HTR.0000000000000020 [DOI] [PubMed] [Google Scholar]
- 71. Andelic N, Røe C, Tenovuo O, et al. Unmet Rehabilitation Needs after Traumatic Brain Injury across Europe: Results from the CENTER-TBI Study. J Clin Med 2021;10(5), doi: 10.3390/jcm10051035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Czeiter E, Amrein K, Gravesteijn BY, et al. Blood biomarkers on admission in acute traumatic brain injury: Relations to severity, CT findings and care path in the CENTER-TBI study. EBioMedicine 2020;56(102785, doi: 10.1016/j.ebiom.2020.102785 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.