Abstract
Introduction
Phytochemical standardization of herbal materials involves establishing consistent levels of one or more active ingredients or markers. It ensures the authenticity and quality of herbal materials, extracts, and their products. This research aimed to apply the herbal chemical marker ranking system (Herb MaRS) originally proposed for quality assurance of complex herbal products to establish markers for controlling the quality of herbal raw materials.
Methods
The assessment of compounds for suitability as markers was based on the Herb MaRS, with minor modifications as follows: for more objective scoring, evidence of biological activity of the potential marker compound(s) was determined at three levels based on the number of symptoms of the disease condition a compound can treat or alleviate: (i) one symptom (1 point), two symptoms (2 points), and 3 or more symptoms (3 points). The reported concentrations of the compounds were also scored as follows: concentration not determined (0 points), concentration ≥ 5 ppm (1 point), concentration ≥ 50 ppm (2 points) and availability of analytical standards (1 point). Finally, the compounds were scored for the availability of an analytical method (1 point). The compounds were scored from 0 to 8, where 8 indicated the most suitable chemical marker.
Results
The selected markers were as follows: aromadendrine, α-terpineol, globulol, and 1,8-cineol (in Eucalyptus globulus Labill. ); aloin, aloe emodin, acemannan (in Aloe barbadensis (L.) Burm.f. ), lupeol, lupenone, betulinic acid, betulin, and catechin (in Albizia coriaria Oliv.); mangiferin, catechin, quercetin, and gallic acid (in Mangifera indica L.); polygodial (in Warburgia ugandensis Sprague); azadirachtin, nimbin, nimbidin (in Azadirachta indica A. Juss. ); and 6,8,10-gingerols, and 6-shogaol (in Zingiber officinalis Roscoe).
Conclusions
Herb MaRS can be efficiently applied to select marker compounds for quality control of herbal materials. However, for herbs whose phytochemicals have not been sufficiently researched, it is difficult to establish evidence of activity, and there are no analytical standards and/or methods; this is the case for plants exclusively used in Africa. The markers identified should be incorporated into chromatographic fingerprints, their quantitative methods developed, and evaluated for applicability at the various stages of the production chain of herbal medicines; then, they can be included in future local plant monographs. There is also a need to build local capacity to isolate marker compounds, particularly those that are not sold by current vendors.
Keywords: Markers, Phytochemical standardization, Quality control, Herbal materials, Herbal products
Introduction
Herbal materials vary greatly in chemical composition due to several factors, including climate, cultivation and harvesting practices, as well as genetic differences among cultivars of the same species [1]. To cater to this variability, herbal raw materials must be standardized before they are used for manufacturing medicinal products. Standardization involves activities that ensure that the materials and the resultant extracts are phytoequivalent. This ensures the reproducibility of the efficacy and safety of the materials and their products [1, 2].
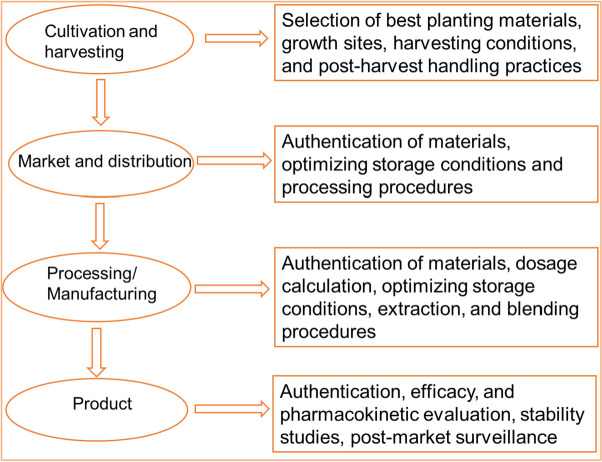
The evaluation of chemical constituents of plant material involves screening and quantification of the major phytochemical groups, the establishment of fingerprint profiles, and/or quantification of selected chemical markers. Once the phytochemical profile is established, the data are evaluated using chemometric methods such as principal component analysis and hierarchical clustering to confirm the phytochemical equivalence of the materials (Fig. 1).
Fig. 1.
A scheme for phytochemical evaluation of herbal materials
Markers may be measured in both raw materials and finished products to obtain useful information for various applications. These include the identification and selection of raw materials where concentration limits are set, identification of adulterants and toxicants, assessment of batch-to-batch uniformity of materials from different sources, control of the manufacturing process, assessment of the suitability of packaging and storage, standardization of physiological activities, and calculation of the dosage of raw materials to include in the product formula [2–4] (Fig. 2).
Fig. 2.
Applications of markers at different stages of the herbal medicine production chain
Selection of marker compounds
When choosing a marker(s) for routine quality control of herbal materials, the following factors should be considered: (i) local availability of effective and easy-to-use analytical methods such thin layer chromatography, high-performance chromatography, and spectroscopy, (ii) availability of analytical standards of acceptable quality, (iii) relevance of the compounds to therapeutic application of the herbal material, and (iv) suitability of the compound(s) as stability indicators. According to the WHO, constituents with known biological activity (related to the traditional use of the herbal material), if known and available, should preferably be selected as markers. Otherwise, compounds with recognized biological activities or characteristic constituents can be used [3]. In line with the WHO and other regulatory guidelines, researchers at the National Institute of Complementary Medicine, University of Western Sydney, proposed a Herbal Chemical Marker Ranking System (Herb MaRS) for selecting markers for quality control of complex herbal products. The Herb MaRS was aimed at providing a uniform and comprehensive guide for the selection of marker compounds for the quality control of polyherbal products. The authors validated this system using an herbal product made from seven herbs. To determine the suitability of phytochemicals as markers, the Herb MaRS ranks the compounds on a scale of 0 to 5. A compound scoring 5 is the most suitable; this is a compound with the highest pharmacological activity related to major symptoms of the disease as claimed by the manufacturer; present in relatively high concentration in the herb or finished product (at least 5 µg/mL); and bioavailable. In addition, it is mandatory to screen toxic compounds, so they are scored 5 by default [5].
In Uganda, comprehensive phytochemical standardization of herbal materials is not yet mandatory since there are no relevant monographs. As such, the products produced from them are not registered; the National Drug Authority issues a “notification” status [6, 7]. For notification, the manufacturer only presents results for general phytochemical screening. Consequently, there have been reports of poor-quality herbal medicines on the market, including adulteration with conventional medicines. The NDA draft guidelines for the regulation of herbal medicines disseminated in 2021, for comments, have recommended the quantification of markers and the establishment of chromatographic fingerprints with reference to the WHO guidelines (https://www.nda.or.ug/wp-content/uploads/2022/03/Guidelines-on-Regulation-of-Traditional-and-Local-Herbal-Medicnes-in-Uganda_Draft-2.pdf). However, since most plants have no monographs yet [8], manufacturers will not know what analytical markers and/or methods to use.
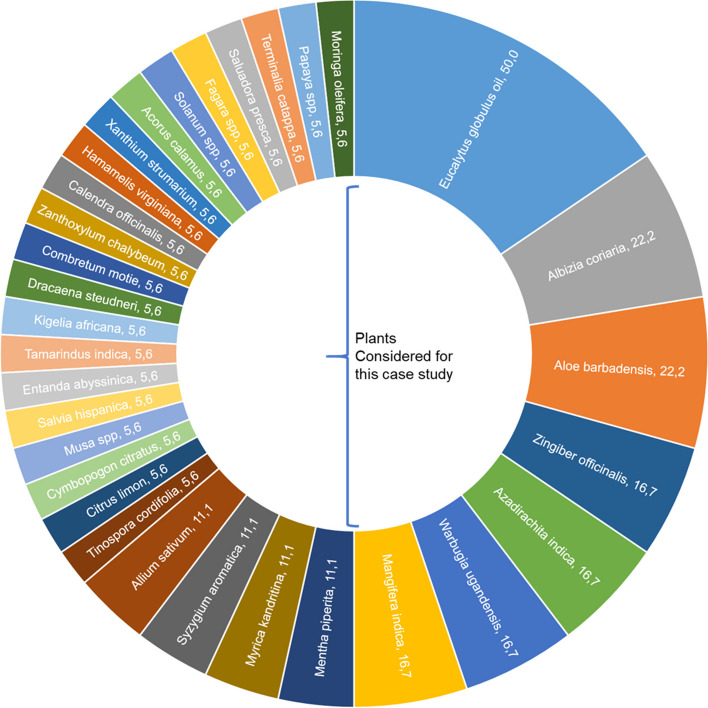
The aim of this work was to assess the applicability of the Herb MaRS to establish the quality control of herbal materials. To achieve this, a case study of the seven most commonly used plant species in the manufacture of herbal medicinal products in Uganda was conducted. According to our previous study [7], Eucalyptus globulus Labill., Aloe barbadensis (L.) Burm.f., Albizia coriaria Oliv., Mangifera indica L., Warburgia ugandensis Sprague, Azadirachta indica A. Juss. and Zingiber officinalis Roscoe were the most frequently used plants (Fig. 3).
Fig. 3.
Popularity of herbal materials in Ugandan registered herbal products. The numbers indicate the percentage of products that contain the plant as active ingredient. modified with permission from [7]
It is evident from Fig. 3 that the seven plant materials considered for this case study are as popular as the other 25 plants combined.
Methods
Identification of potential marker compounds
The suitability of analytical markers was determined based on the WHO guidelines for selecting marker substances of herbal origin for quality control of herbal medicines [3] and on the Herbal Chemical Marker Ranking System (Herb MaRS) [5]. Both the WHO guidelines and the Herb MaRS give priority to a compound whose biological activity is related to the traditional use of the plant and can be identified and quantified by the analytical methods available. Additionally, the compound chosen should be available commercially in pure form.
Establishment of active compounds and evidence of biological activity
An extensive literature search to identify the bioactive compounds and to establish evidence of their biological activity relevant to the therapeutic claims made on the product label was performed for the seven most commonly used herbal materials. Such evidence included studies reporting on the ability of the compound(s) to treat or ameliorate one or more symptoms of the disease condition as indicated by the manufacturer. According to Kaggwa et al. [7], Albizia coriaria, Mangifera indica, and Zingiber officinale are exclusively used in cough syrups; Warburgia ugandensis in cough and anti-ulcer syrups; Eucalyptus globulus in mouth washes, cough syrups and pain balms; Aloe vera in mouth washes, cough syrups, lip balms and GIT cleansing tablets; and Azadirachta indica in cough, anti-ulcer syrups and lip balms. The same study established evidence of the efficacy and safety of the plant materials for these therapeutic applications. Table 1 summarizes the diseases (or their symptoms) the products are indicated to manage.
Table 1.
Disease conditions managed by the most commonly used herbal materials in herbal manufacturing in Uganda. Table modified with permission from [7]
| No. | Plant material Source of plant Part of plant used |
Dosage form of product containing the material | Indication(s) of the products containing the material |
|---|---|---|---|
| 1 |
Eucalyptus globulus Labill. (Myrtaceae) Wild, cultivated Leaf oil |
Mouth wash | Toothache, bad odor, sensitivity, bleeding gums, (tooth) cavities, tooth decay, antibacterial, mouth sores |
| Cough syrups | Cough, common cold, catarrh, sore throat, congestion from asthma, bronchitis, whooping cough, allergic conditions- sinusitis, rhinitis, mouth sores, hiccups, relieving fever, measles symptoms | ||
| Pain balm | Pain relief | ||
| 2 |
Aloe vera Burm.f. (Asphodelaceae) Cultivated Whole leaf |
Mouth wash | Toothache, bad odor, sensitivity, bleeding gums, (tooth) cavities, tooth decay, antibacterial, |
| Aloe tablets | Cleanses GIT | ||
| cough syrup | Cough, flu, sore throat, sinusitis | ||
| Lip balm | Dry, cracked, and painful lips | ||
| 3 |
Albizia coriaria Oliv. (Fabaceae) Wild Stem bark |
(Cough) syrups |
Whooping cough, catarrh, sore throat, congestion from asthma and bronchitis, relieving fever, sinusitis |
| 4 |
Mangifera indica L. (Anacardiaceae) Wild, cultivated Stembark, leaves |
Whooping cough, catarrh, sore throat, congestion from asthma and bronchitis |
|
| 5 |
Warburgia ugandensis Sprague (Canellaceae) Wild, cultivated Stem bark, leaves |
Cough, flu, mouth sores, measles symptoms, common colds, sinusitis, rhinitis, asthma, catarrh, whooping cough, bronchial congestion, mouth sores, hiccups | |
| (antiulcer) syrups | (GIT) Ulcers | ||
| 6 |
Azadirachta indica A. Juss. (Meliaceae) Wild, cultivated Stem bark, leaves |
Cough syrup | Cough, flu, sore throat, sinusitis |
| (antiulcer) syrups | Gastric ulcers, stomach ulcers, flatulence, constipation | ||
| Lip balm | Dry, cracked, and painful lips | ||
| 7 |
Zingiber officinale Roscoe (Zingiberaceae) Cultivated Rhizome |
cough syrups | Allergic cough, smokers cough, whooping cough, productive cough, flu, lung cleaning, sore throat, sinusitis, bronchial asthma, relieving fever |
A systematic search for articles was performed using search engines such as Google and indexes including PubMed, Google Scholar, ResearchGate, and Web of Science. The search terms consisted of the chemical name, pharmacological or therapeutic activity of interest, such as “anti-inflammatory activity of 6-gingerol”, plant botanical name and bioactive compounds thereof, such as “bioactive compounds in Mangifera indica leaves”, and “mechanism of action of mangiferin”. Only full-length articles published in English were reviewed. We did not limit the search to any timeline since evidence is considered valid until disputed by new findings.
Availability of analytical methods for the potential marker compounds
In addition to evidence of biological activity of the identified compounds, information regarding quality control methods recommended by existing pharmacopoeial monographs was included, particularly the WHO monographs on selected medicinal plants [9–13], the African Pharmacopoeia, the West African Herbal Pharmacopoeia [14] and the Pharmaceutical monographs for South African plants species [15]. Additionally, the availability of assay methods for the quantification of markers in the respective plant materials was crucial. The primary focus was on high-performance liquid chromatography (HPLC) methods because they are highly sensitive, specific, versatile and readily accessible even in resource-limited countries. Where HPLC methods were not available or not suitable, such as for essential oils, high-performance thin layer chromatography (HPTLC), gas chromatography (GC) or ultraviolet/visible (UV/VIS) spectrophotometric methods, and other available methods were considered. Both HPTLC-densitometry and spectrophotometric methods are less sensitive for the quantitative determination of markers than HPLC, although they are easier to use. On the other hand, GC-based methods are as sensitive as HPLC but are selective to only compounds that are volatile, such as essential oils, while some compounds can be derivatized to make them volatile, the analysis cost is escalated by expensive derivatization reagents.
Availability of analytical reference standards for the potential marker compounds
Information on the availability of analytical standards and the prices for the smallest units was obtained, preferably from the Sigma Aldrich ® website (https://www.sigmaaldrich.com/UG/en). This was for two main reasons: (i) from our experience, Sigma Aldrich is among the most reliable suppliers of high-quality chemicals, and (ii) they willingly display the prices for various grades and quantities of the same analytical standard. If the compounds were not available from Sigma Aldrich®, a general Google search to establish other potential sources was executed. Finally, the cost of 1 mg or mL of the marker was computed with an assumption that this amount is sufficient for a single analysis to construct calibration curves. We believe that the cost of equivalent grades of standards from other vendors will differ only slightly.
Selection of the most suitable marker compounds
Using a modified Herb MaRS, compounds were given scores from 0 to 8, where 8 indicates the most suitable chemical marker. The Herb MaRS [5] does not elaborate on how the individual attributes of the compound are scored but rather gives a lumpsum mark after the overall assessment. Therefore, for more objective scoring, we modified the ranking system as follows: evidence of biological activity was divided into three levels based on the number of symptoms of the disease condition a compound can treat or alleviate: (i) one symptom (1 point), two symptoms (2 points), 3 and more symptoms, with well-elucidated mechanisms of action (3 points). We also scored the reported concentrations of the compounds in the plant material (concentration not determined (0 points), concentration ≥ 5 ppm (1 point), (concentration ≥ 50 ppm, 2 points) and availability of analytical standards (1 point); last, we scored the availability of an analytical method (1 point).
Results
Evidence of biological activity of potential chemical markers
For most plant materials, there are compounds with sufficient biological evidence relevant to the industrial application of the products in which the medicinal plant is contained. However, most of the compounds in Warburgia ugandensis have not been individually evaluated. The most important bioactive compounds are shown in Fig. 4: E. globulus (1,8-cineol (1), aromadendrin (2), globulol (3) and α-terpineol (4)), A. barbadensis; (aloin A (5), aloin B (6), aloe emodin (7), acemannan (8) and mannose 6 phosphate (9)), A. coriaria; (lupeol (10), lupenone (11), betulinic acid (12), catechin (13)), M. indica; (catechin (13), quercetin (14), mangiferin (15) and gallic acid (16)), Azadirachta indica; (azadirachtin (20), mahmoodin (21), nimbin (22), and nimbolide (23), Zingiber officinalis; (gingerols (17), shogaols (18) and zingerone (19)), Warburgia ugandensis; (bemadienolide (24), muzigadial, polygodial (25), warbuganal (26), ugandensolide (27), and muzigadial (28).
Fig. 4.
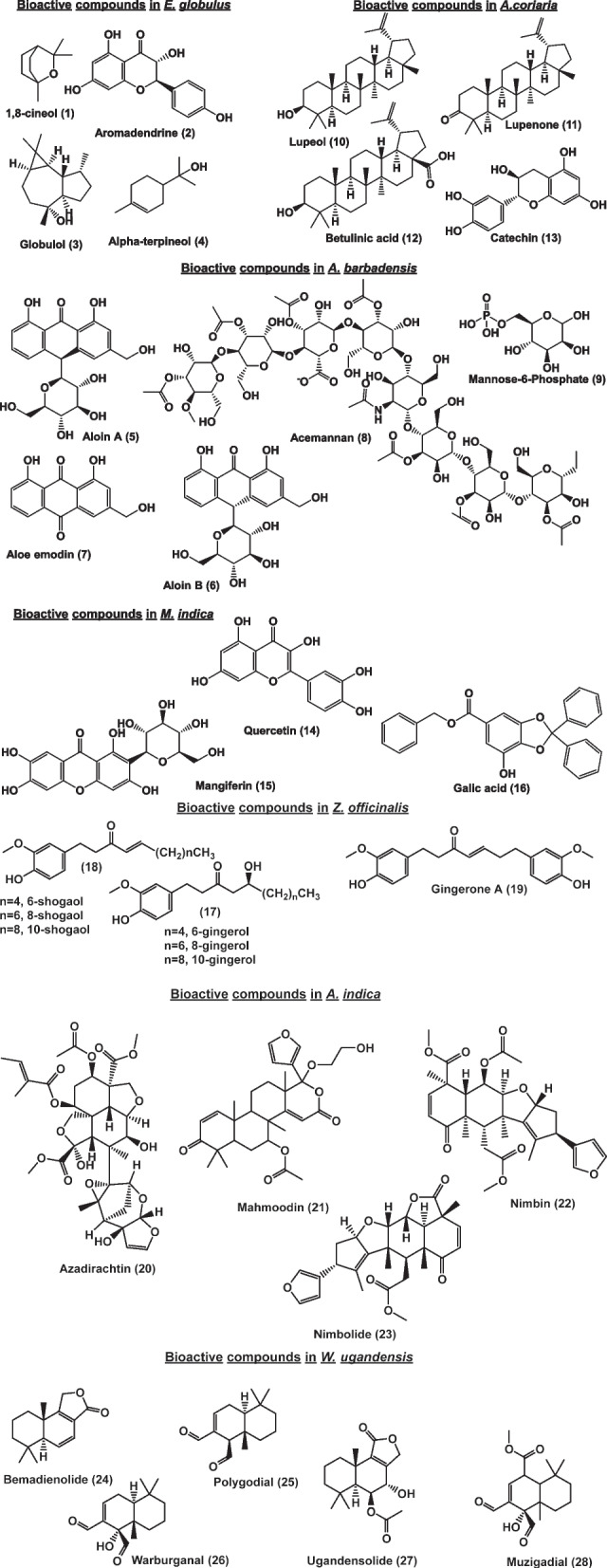
Bioactive compounds in the studied medicinal plants relevant to industrial application (the structures were generated with ChemDraw® software)
The biological activities of these compounds and their mechanisms of action are summarized in Table 2 below.
Table 2.
Evidence of biological activity of the compounds found in the plant materials
| Plant species and manufacturer therapeutic claim | Bioactive compound |
Evidence of Biological activity of bioactive compound related to traditional use of the plant | Mechanism of action |
|---|---|---|---|
|
Eucalyptus globulus pain relief, URT disorders, mouth wash, GIT disorders |
Aromadendrine (dihydrokaempferol) |
Anti-inflammatory Ani-oxidant |
Scavenging of reactive oxygen species, chelation of metal ions [16] |
| Antibacterial; against Staphylococcus aureus, Streptococcus mutans | Inhibits biofilm formation [17] | ||
| 1,8-cineol | Antibacterial-against K. pneumoniae, S. aureus, P. aeruginosa | Disruption of bacterial cell membrane & loss of intracellular materials [18] | |
| Antiasthma, anti-bronchitis, anti COPD, Anti-influenza | Downregulation of inflammation cytokines such as interleukin- 1b (IL-1b) and tumor necrosis factor-a resulting in bronchial muscle relaxant and reduction in mucus secretion [19] | ||
|
Anti-inflammatory Ani-oxidant |
Regulates nuclear factor-kappa B (NF- κB) and nuclear factor erythroid-2-related factor 2 (Nrf2) pathways [20, 21] | ||
| Analgesic/sedative | Suppression on the CNS by modulating glutamatergic & dopaminergic systems, activates transient receptor potential melastatin 8 [22, 23] | ||
| Antispasmodic and antisecretory, gastroprotective, antidiarrheal | Promotes regeneration of the gastric cells, increases gastric mucus, antioxidant anti-inflammatory effects [20] | ||
| globulol | Antibacterial-against K. pneumoniae, S. aureus, P. aeruginosa [24, 25] | ||
| α-terpineol |
Anti-inflammatory & antioxidant mainly analgesic |
Suppresses superoxide production by monocytes; inhibits release of inflammatory mediators including serotonin, histamine, bradykinin, & prostaglandins [26, 27] | |
| Antibacterial-against K. pneumoniae, S. aureus, P. aeruginosa | As 1,8-cineole | ||
| Anti-gastric ulcer | As 1,8-cineole | ||
| Aloe barbadensis cracked lips, mouth wash, URT disorders, GIT disorders |
Aloin A and B Aloe emodin |
Laxative | Inhibition of Na+/K + pump & Cl-channels increase gastric motility; stimulate secretion of mucus and chloride ions [28, 29] |
| immuno-modulatory effects | Inhibition of histamine release from mast cells -reduced production of Tumor Necrosis Factor (TNF)-α [30] | ||
|
anti-inflammatory- antioxidant |
Cyclooxygenase pathways and reducing prostaglandin E2 production [31, 32] | ||
| antibacterial activity-H pylori | Activation of phagocytic leukocytes; inhibition of the N-acetyltransferase activity of H. pylori [33, 34] | ||
| Acemannan |
Wound healing anti-inflammatory |
Activates macrophages to release fibrogenic cytokines; inhibits thromboxane A2 [35, 36] Cyclooxygenase pathways and reducing prostaglandin E2 production [30] |
|
| Mannose 6 phosphate | Wound healing | Enhances activity of fibroblasts [37, 38] | |
| Lupeol |
Anti-inflammatory- antioxidant Wound healing effect |
Lupeol reduces TNF-α, IL-1, and IL-6 cytokine production. This lowers the infiltration macrophage to damaged tissues, hence reducing inflammation. [39]. It also chelates toxins such as heavy metal ions [40] Stimulates the production, and migration of keratinocytes and fibroblasts to injured tissues, by activating the PI3K-PKB/Akt and p38/ERK/MAPK pathways [41]. |
|
|
Albizia coriaria URT disorders, |
Lupeol and lupenone |
Anti-inflammatory Analgesic |
Decreases PGE2, TNF-α, interleukin-1b production [42, 43] |
| Immunomodulating; anti allergen, anti-asthmatic, | Reduces the production eosinophils, thus interleukins-reduced fluid production in the bronchoalveolar pathway [44] | ||
| Antibacterial-against S. aureus, K. pneumoniae, P. aeruginosa [45, 46] | |||
| Anti-viral-herpes simplex [47] | Inhibits virus plaque formation [48] | ||
| Betulinic acid/betulin |
Anti-inflammatory Analgesic |
Inhibits production of nitric oxide & PG2 (cyclooxygenase-2 activity); also decreases production of pro-inflammatory cytokines including IL-1β, IL-6, IL-8, IL-12, & TNF [49, 50] | |
| Antibacterial-P. aeruginosa, S. aureus, Mycobacterium tuberculosis [51] | Enhance the rate of electron transport chain activity, which results in excess production of ROS, which damage DNA, and cause bacterial death [52]. | ||
| Anti-viral-against herpes simplex [53] | Inhibits viral plaque formation [48] | ||
| (+/-) Catechin | Anti-inflammatory | Radical scavenging; activates production of erythroid-derived factor 2 which regulates antioxidant enzymes [54] | |
| Immunomodulatory; anti-allergenic | Reduces production & infiltration of lung tissue by inflammatory cytokines such as TNF-α, IL-1β [55] | ||
| Anti-viral-against Influenza A, SARS-CoV-2 [56, 57] | Inhibits viral receptor binding [58] | ||
|
Mangifera indica URT disorders, |
Mangiferin |
Antioxidant, anti‑inflammatory, antipyretic, analgesic, |
Scavenging of ROS, chelation of toxic metal ions; downregulates phosphorylation of NF- κB pathways-reduces production of proinflammatory cells [59, 60] |
| Antiallergic, anti-asthmatic, immunomodulatory | Reduces tracheal contraction by inhibiting the nitric oxide‑cyclic GMP pathway [61]; Inhibits production of nitric oxide and PG2 (cyclooxygenase-2 activity); also decreases production of pro-inflammatory cytokines including [62] | ||
| Antibacterial-activity against S. aureus [63] | Increased antibody titers; increases cell mediated immunity. Stimulates lysozyme activity, [64] | ||
| Antiviral-against Herpes simplex [65] | Inhibits viral replication [66] | ||
| (+/-) Catechin, epicatechin |
Anti-viral, anti-inflammatory and anti-allergenic |
Activity against influenza A and B; catechins inhibit receptor binding and sialidase activities [58]. Catechins regulate the production of proinflammatory agents such as TNF-α, NF-κB, COX-2 in lung tissue. They also scavenge noxious metal ions and ROS [67, 68]. |
|
| Gallic acid | Antioxidant, anti-inflammatory | Scavenging of ROS, chelation of toxic metal ions; downregulates phosphorylation of NF- κB pathways-reduces production of proinflammatory cells [50–52] | |
| Antimicrobial- P. aeruginosa, S. aureus | Interferes with colonization by inhibiting motility & adherence; disrupts cell membrane leading to leakage of cell nutrients; inhibits dihydrofolate reductase, topoisomerase IV [69, 70] | ||
| Antiviral - Haemophilus influenza A & B | Disruption of the viral particles [71] | ||
| Quercetin |
Antioxidant, anti-inflammatory, |
Scavenging of ROS, chelation of toxic metal ions; downregulates phosphorylation of NF- κB pathways-reduces production of proinflammatory cells, inhibits cyclooxygenase & lipoxygenase enzymes [67, 72–74] | |
| Immune-modulatory; anti-allergic | Inhibits IL 8 & 6, TNF-α [75] | ||
| Antibacterial; P. aeruginosa, S. aureus, B. subtilis, M. tuberculosis, K. pneumoniae | Inhibits nucleic acid synthesis, disrupts plasma membrane, inhibits glutamine synthetase, inhibits biofilm formation [76, 77] | ||
| Antiviral - Influenza-A virus [78] | Interacts with Hemagglutinin (HA) glycoprotein to prevent entry into the host cell, thereby inhibiting viral replication. It also inhibits the M2 protein and neuraminidase (NA) glycoprotein interfering with packaging of genome segments into influenza virus particles [79]. | ||
|
Azadirachta indica URT disorders, cracked lips |
Tetranortriterpenes- Azadirachtin |
Anti-inflammatory, antipyretic, antioxidant Wound healing, Anti-gastric ulcer |
Inhibits cyclooxygenase (COX), & lipoxygenase (LOX) enzymes. Modulates transcription factors NF-κB, radical scavenging |
| Immunostimulant | Inhibits TNF-induced biological responses [80] | ||
| Antibacterial- against S. aureus & MRSA | Inhibits biofilm formation [81] | ||
| Nimbidin, Nimbin, | Antipyretic, anti-inflammatory and antioxidant [82, 83] | Suppresses production of inflammatory cytokines from neutrophils & macrophages [84] | |
| Anti-gastric ulcer | Reduces secretion of gastric acid by inhibiting histamine (H2) receptors and muscarinic receptors [85] | ||
| Immunomodulatory; anti-allergic | Inhibits macrophage migration [86] | ||
| Nimbolide | Antibacterial [87] | ||
| Mahmoodin |
Anti-inflammatory, Antibacterial [88] |
||
| Diterpens-Margolone, margolonone, margolonone |
Antibacterial-against Klebsiella, Staphylococcus & Serratia Species [88] |
||
|
Zingiber officinalis URT disorders, GIT disorders |
Gingerols 8- gingerol 10-gingerol 12-gingerol 6-gingerol Shogaols 6-shogaol |
Antioxidant activity, Anti-inflammatory, analgesic: 6-gnigerol and 6-shogaol most studied |
Scavenging of ROS, chelation of metal ions; oxygenation arachidonic acid, a substrate for cyclooxygenase enzymes, thus inhibiting production of prostaglandins; reduced activation of macrophages; inhibit nitrite oxide (NO) production [89, 90] |
| Anti-asthmatic, anti-allergen | Reduced contraction of smooth respiratory muscles by reduction in Ca2 + influx & β2 receptor activation; reduced production of proinflammatory cytokines [91] | ||
|
Antibacterial- S. aureus, Mycobacteria, Streptococcus pyogenes, Streptococcus pneumoniae, Haemophilus influenzae |
Inhibition of biofilm formation, inhibition of hydroxymethyl-7, 8- dihydro pterin pyrophosphokinase, 6-gingero > 8- gingerol > 10-gingerol > 12-gingerol [92, 93] | ||
|
Anti-gastric-ulcer activities -anti- H. pylori, 10-gingero > 8- gingerol > 6-gingerol > 6-shogaol [94] -anti-emetic- |
Inhibit 5-hydroxytryptamine to increase gastric motility and emptying [95, 96] | ||
| Zingerone (major pungent compound in ginger) |
Anti-inflammatory antioxidant activity |
Reducing ROS production; chelation of metal ions [97] | |
| Antibacterial activity | Dihydro pterin pyrophosphokinase inhibition | ||
|
Warburgia ugandensis URT disorders, |
Drimane sesquiterpenes Muzigadial, Muzigadiolide Warburganal, warburgadione, warburgadial, warburgin Ugandensidial, Ugandensolide polygodial |
Anti-inflammatory and anti-allergic – polygodial | inhibition of phospholipase A2 and neuropeptide release [98] |
| Antimicrobial-antimycobacterial (muzigadial & muzigadiolide) [99] | |||
| Antibacterial (against K. pneumoniae, P. aeruginosa, S. aureus (warburganal, ugandensidial, and polygodial) [100] |
URT Upper respiratory tract, GIT Gastrointestinal, ROS Reactive oxygen species
Availability of analytical standards and assay methods
For Eucalyptus globulus, Aloe barbadensis, Zingiber officinalis, and Azadirachta indica, monographs with well-elaborated quality control methods have been published. In addition, analytical standards for the selected compounds are available, and their assay methods have been developed. On the other hand, no monographs for Albizia coriaria, Mangifera indica, and Warburgia ugandensis exist; for W. ugandensis, there are no analytical standards or assay methods to quantify the individual compounds. The cost per mg or mL of analytical standard ranged from €0.6 to 498 for α-terpineol and azadirachtin, respectively, with an average cost of €62.5 ± 101.5. The results are summarized in Table 3.
Table 3.
Available analytical standards and assay methods for selected medicinal plant compounds
| Plant material | Identified Analytical markers | Commercial sources | Smallest commercial unit available, purity and/cost (Euros-€) | Cost per mg/mL of marker (Euros-€)) | Analytical methods for the plant material mentioned in local or WHO Pharmacopoeia |
Assay methods already developed for the compounds in same or other materials |
|---|---|---|---|---|---|---|
| Eucalyptus globulus oil | Aromadendrine (dihydrokaempferol) | Sigma‒Aldrich/Supelco |
Analytical standard-530/5 mg ≥95% HPLC grade-221/10 mg ≥ 95% LC/MS-ELSD-421/1 mg |
106.0 22.1 421 |
WHO monographs &African pharmacopoeia-identification tests for 1,8-cineole in oil & leaf materials. TLC fingerprint for leaf materials with 1,8-cineole as reference [10, 13]. |
Gas chromatography FID & MS method for quantification of oil components [25, 101] |
| α-terpineol | Sigma‒Aldrich/Supelco | Analytical standard (≥ 95%)-63.9/100 mg | 0.6 | |||
| globulol | Sigma‒Aldrich | ≥ 98.5% (sum of enantiomers, GC)- 247/100 mg | 2.5 | |||
| 1,8-cineol (eucalyptol) | Sigma‒Aldrich/Supelco | Analytical standard- 48.3/1 mL | 48.3 | |||
| Aloes -whole leaf products | Aloin A | Sigma‒Aldrich | Analytical standard- 440/10 mg | 44.0 |
WHO monographs-Thin-layer chromatography, microchemical analyses to identify anthracenes, Spectrophotometry-to determine total glycosides as aloin [10] |
HPLC-DAD/MS quantification methods for anthracenes in aloe vera samples [102] |
| Aloin B | Sigma‒Aldrich | Phyproof® Reference Substance- 605/10 mg | 60.5 | |||
| Aloe emodin | Sigma‒Aldrich |
Analytical standard 311/10 mg |
31.1 | |||
| Aloe vera gel | Acemannan | Toronto Research chemicals | Technical grade- 208.3/10 mg | 20.8 |
Chemical test for carbohydrates; Polysaccharide composition analysis by gas–liquid chromatography [10] |
Molecular Exclusion Chromatography [103] UV‒Vis Spectrophotometry [104] |
| D-Mannose 6 phosphate | Sigma‒Aldrich | ≥ 98% (HPLC) (sodium salt)- 354.0/100 mg | 3.5 | None found | ||
| Albizia coriaria stem bark | Lupeol | Sigma‒Aldrich | Analytical standard-130/10 mg | 13.0 | No monographs for Albizia coriaria stem bark materials | HPLC-DAD quantification method for triterpenoids [105, 106] |
| lupenone | Toronto Research chemicals | Analytical standard-170/2.5 mg | 68.0 | HPLC-DAD quantification method for triterpenoids in Albizia inundata [107] | ||
| Betulinic acid | Sigma‒Aldrich/Supelco |
Analytical standard 95.1/10 mg ≥ 98% (HPLC)- 70/5 mg |
9.5 14.0 |
HPLC-DAD quantification method for betulinic acid in Albizia lebbeck [108] | ||
| Catechin | Sigma‒Aldrich/Supelco | Analytical standard − 307/10 mg | 30.7 | HPLC-DAD quantification method Albizia lebbeck [109], | ||
| Mangifera indica leaf or stem bark | Mangiferin | Sigma‒Aldrich/Supelco | Analytical standard-108/10 mg | 10.8 | No monographs for Mangifera indica leaf or stem bark materials | HPLC-UV quantification method for mangiferin [110] |
| Catechin | Sigma‒Aldrich/Supelco | Analytical standard − 307/10 mg | 30.7 |
HPLC-UV quantification method for phenolic compounds [111] |
||
| Epicatechin | Not found | N/A | ||||
| Gallic acid | Sigma‒Aldrich | Phyproof® Reference Substance − 345/100 mg | 34.5 | |||
| Quercetin | Sigma‒Aldrich |
United States Pharmacopeia (USP) Reference Standard- 357/200 mg phyproof® Reference Substance- 253/20 mg ≥ 95% (HPLC)- 68.3/10 g |
1.8 12.7 6.8 |
|||
| Azadirachta indica stem bark or leaf | Azadirachtin | Sigma‒Aldrich |
Phyproof® Reference Substance- 403/5 mg ~ 95%-249/0.5 mg |
80.6 498.0 |
WHO monographs-high-performance liquid chromatography quantification of tetranortriterpenes in oil and leaf materials [11] |
HPLC-UV quantification method for Azadirachtins [114] |
| Nimbin | Toronto Research chemicals | Analytical standard-105/1 mg | 105.0 | HPLC-UV quantification method for nimbin [115] | ||
| Nimbidin | Not found | N/A | None found | |||
| Nimbolide | Sigma‒Aldrich | ≥ 98%-624/5 mg | 124.8 | HPLC-UV quantification method for nimbolide [116] | ||
| Mahmoodin | Not found | N/A | None found | |||
| Zingiber officinalis rhizome | 8-gingerol | Sigma‒Aldrich/Supelco | Analytical standard 489.0/10 mg | 48.9 |
WHO monographs-Thin-layer chromatography fingerprinting to identify gingerols and shogaols; quantitative gas chromatography and high-performance liquid chromatography analyses of ginger oils for gingerols, Shogaols [10] |
HPLC‒MS quantification methods for gingerols and related compounds [117] |
| 10-gingerol | Sigma‒Aldrich |
Analytical standard-546/10 mg ≥ 98% (HPLC)-276/5 mg phyproof® Reference Substance-472/10 mg |
54.6 55.2 47.2 |
|||
| 12-gingerol | Not found | N/A | ||||
| 6-gingerol | Sigma‒Aldrich |
Analytical standard- 448/10 mg ≥ 98% (HPLC)- 358/5 mg phyproof® Reference Substance- 472/10 mg |
44.8 71.6 47.2 |
|||
| 6-shogaol | Sigma‒Aldrich | Analytical standard-538/10 mg Phyproof® Reference Substance- 657/10 mg |
53.8 65.7 |
|||
| Zingerone | Sigma‒Aldrich | Analytical standard- 84.50/50 mg | 1.7 | None found | ||
| Warburghia ugandensis stem bark | Polygodial | Sigma‒Aldrich | ≥97% (HPLC)-216/10 mg | 21.6 | No monograph for Warburghia ugandensis stem bark | None found |
| Bemadienolide | Not available | N/A | None found | |||
| Muzigadial | Not available | N/A | None found | |||
| Warbuganal | Not available | N/A | None found | |||
| Warbugadione | Not available | N/A | None found | |||
| Warbugadial | Not available | N/A | None found | |||
| Warbugin | Not available | N/A | None found | |||
| Ugandensolide | Not available | N/A | None found | |||
| Ugandensidial | Not available | N/A | None found |
N/A Not applicable
Selection of markers
Most of the compounds scored at least 5 points out of 8 except those for Warburgia ugandensis, which scored only one point. The scores of the markers for each plant are summarized in Table 4.
Table 4.
Ranking of the biomarkers
| Plant material and manufacturer therapeutic claim | Bioactive Compound |
Evidence of Biological activity of bioactive compound | Level of evidence of biological activity related to traditional use of the material | Relative Concentration in plant or extract | Mean Concentration above (5 ppm) %ppm | Mean concentration above 50ppm Yes (1)/no (0) E |
Reference Standard available Yes (1)/no (0) F |
Analytical methods available? Yes (1)/no (0) |
Herb MaRS score |
|---|---|---|---|---|---|---|---|---|---|
| Score |
Yes-1 No-0 (A) |
1 symptom-1 2 symptoms-2 3 symptoms-3 (B) |
Yes (1) No (0) (C) |
Yes (1) No (0) (D) |
Yes (1) No (0) (E) |
Yes (1) No (0) (F) |
/8 (A + B + C + D + E + F) |
||
| Eucalyptus globulus leaf/oil | aromadendrine | 1 | 2 | 10–30% of essential oil [25] | 1 | 1 | 1 | 1 | 7 |
| α-terpineol | 1 | 3 | 0.50% of essential oil [25] | 1 | 1 | 1 | 1 | 8 | |
| Globulol | 1 | 1 | 10–11% of essential oil [25] | 1 | 1 | 1 | 1 | 6 | |
| 1,8-cineol | 1 | 3 | 97.32% of essential oil [120] | 1 | 1 | 1 | 1 | 8 | |
| Aloe barbadensis whole leaf/gel | Aloin A and B | 1 | 3 | 0.1–0.6% of leaf, 10–30% of latex [121, 122] | 1 | 1 | 1 | 1 | 8 |
| Aloe emodin | 1 | 2 | 0.09–0.29 mg/g of whole leaf [123] | 1 | 1 | 1 | 1 | 7 | |
| Acemannan | 1 | 2 | 109-135ppm of gel [103] | 1 | 1 | 1 | 1 | 8 | |
| Mannose 6 phosphate | 1 | 1 | ND | 0 | 0 | 1 | 0 | 3 | |
| Albizia coriaria stem bark | Lupeol | 1 | 3 | 1–6 mg/g of stembark [106] | 1 | 1 | 1 | 1 | 8 |
| Lupenone | 1 | 1 | 19–200 ppm of stem bark [107] | 1 | 1 | 1 | 1 | 6 | |
| Betulinic acid | 1 | 3 | 1.2–10 mg/g of stem bark [106, 108] | 1 | 1 | 1 | 1 | 8 | |
| Catechin | 1 | 3 | 0.2–12 mg/g of stem bark [109] | 1 | 1 | 1 | 1 | 8 | |
| Mangifera indica leaves/stem bark | Mangiferin | 1 | 3 | 5–20 mg/g of leaves [110] | 1 | 1 | 1 | 1 | 8 |
| Catechin | 1 | 3 | 71.4 mg/g of stem bark [111] | 1 | 1 | 1 | 1 | 8 | |
| Epicatechin | 1 | 1 | 8.07 mg/g of stem bark [111] | 1 | 1 | 0 | 1 | 5 | |
| Gallic acid | 1 | 3 | 2.08 mg/g of stem bark [111] | 1 | 1 | 1 | 1 | 8 | |
| Quercetin | 1 | 3 | 0.76 to 1.16 mg/g of leaves [124] | 1 | 1 | 1 | 1 | 8 | |
| Azadirachta indica leaves/stem bark/seeds | Azadirachtin | 1 | 3 |
3.8 to 4.8 mg/g of seeds [125] 0.1-1 mg/g of leaves [126] |
1 | 1 | 1 | 1 | 8 |
| Nimbin, | 1 | 3 | 0.018 to 0.64 mg/g of oil [115] | 1 | 1 | 1 | 1 | 8 | |
| Nimbolide | 1 | 2 | 0.9–6.7 mg/g of leaf [116] | 1 | 1 | 1 | 1 | 7 | |
| Mahmoodin | 1 | 2 | Not determined | 1 | 1 | 0 | 0 | 5 | |
| Zingiber officinalis rhizome | 12-gingerol | 1 | 2 | 0.01–0.02 mg/g of rhizome [119] | 1 | 1 | 0 | 1 | 6 |
| 10-gingerol | 1 | 2 | 0.2–0.4 mg/g of rhizome [117] | 1 | 1 | 1 | 1 | 7 | |
| 8-gingerol | 1 | 1 | 0.4–0.5 mg/g of rhizome [117] | 1 | 1 | 1 | 1 | 6 | |
| 6-gingerol | 1 | 3 | 1.1-2.0 mg/g of rhizome [117] | 1 | 1 | 1 | 1 | 8 | |
| 6-shogaol | 1 | 3 | 0.01–0.02 mg/g of rhizome [119] | 1 | 1 | 1 | 1 | 8 | |
| Zingerone | 1 | 2 | ND | 0 | 0 | 1 | 1 | 5 | |
| Warburgia ugandensis stem bark | Bemadienolide | 1 | 0 | ND | 0 | 0 | 0 | 0 | 1 |
| Muzigadial, | 1 | 1 | ND | 0 | 0 | 0 | 0 | 2 | |
| Polygodial | 1 | 2 | ND | 0 | 0 | 1 | 0 | 3 | |
| Warbuganal, | 1 | 1 | ND | 0 | 0 | 0 | 0 | 2 | |
| warbugadione, | 1 | 0 | ND | 0 | 0 | 0 | 0 | 1 | |
| warbugadial, | 1 | 0 | ND | 0 | 0 | 0 | 0 | 1 | |
| Warbugin | 1 | 0 | ND | 0 | 0 | 0 | 0 | 1 | |
| Ugandensidial, | 1 | 1 | ND | 0 | 0 | 0 | 0 | 2 | |
| Ugandensolide | 1 | 0 | ND | 0 | 0 | 0 | 0 | 1 |
Key: ND Not determined, ppm parts per million
Discussion
Standardization is a key step in the quality assurance of herbal materials and their products; it is essential to ensure reproducibility of the biological activity and quality of the product. In this study, we established a list of compounds that can be used as markers for seven of the most commonly used plant materials in Uganda. Our emphasis was on compounds that are known to be active such that their determination informs both the quality and efficacy of the materials. We hope this information will be relevant to manufacturers once the new National Drug Authority (NDA) guidelines are put in force; quantification of markers and establishment of chromatographic fingerprints will be needed (https://www.nda.or.ug/wp-content/uploads/2022/03/Guidelines-on-Regulation-of-Traditional-and-Local-Herbal-Medicnes-in-Uganda_Draft-2.pdf).
With the use of a modified herbal marker ranking system, compounds were identified that can be utilized to control the quality of herbal materials. Evidence of biological activity, availability of the analytical standard and availability of an analytical method are paramount. Thus, a compound should score at least 5 points to be suitable, that is, 3 points for biological activity and one point each for analytical standard and analytical method availability. The minimum concentrations of the markers in the plant material, if not already known, can be established by the manufacturer, and the compound assigned a qualitative (≤ 50 ppm) or quantitative (≥ 50 ppm) role depending on the concentrations in the plant material [5]. Another important factor to consider in quantitative analysis is the cost of the marker compounds. In this study, we highlight unit costs and the costs of the smallest packs for each compound. It is important to note, however, that the final acquisition costs will include vendor or agent markups and so might be significantly higher. While 1 mg or 1 mL is considered sufficient for external calibration, other forms of calibration, such as standard addition, will require higher amounts of the marker. To show the relevance of the selected markers, we list situations for which standardization of each plant material is needed.
Markers for Eucalyptus globulus oil
Eucalyptus globulus is known for the essential oils obtained from the leaves of the plant. The oil is used to manufacture products such as syrups used to manage symptoms of respiratory tract disorders (cough, common cold, catarrh, sore throat, congestion from asthma, bronchitis, allergic conditions- sinusitis, rhinitis, hiccups), fever and measles; pain balms applied topically to manage pain and inflammation; and mouth washes for conditions such as toothache, bad odor, sensitive teeth, bleeding gums, tooth cavities, tooth decay, and mouth sores [7]. Some of the most studied compounds that exhibit pharmacological activities to support the indications include aromadendrine, α-terpineol, globulol, and 1,8-cineol (Table 2; Fig. 4), with scores of 7, 8, 6, and 8, respectively. Since all the compounds are available in pure form and several quantitative methods have been established (Table 3), these compounds are all suitable as markers. Aromadendrine is the most expensive, with a unit cost of €183), while α-terpineol is the cheapest, with a unit cost of €0.6. The WHO and the African pharmacopoeia recommend the use of 1,8-cineol as a standard for both chemical reaction and TLC fingerprint identification methods [10, 13]; however, some studies have shown aromadendrine to be the major component, and perhaps a multimarker approach is more appropriate than determining only cineol [25]. These markers can be used to authenticate, determine phyto-equivalence and monitor the consistency in quality of oils obtained from different subspecies and geographical locations.
Markers for Aloe vera (Aloe barbadensis)
Aloe vera is used as the gel, latex or whole leaf extract. Whole leaf and latex products are used to treat constipation, to “cleanse” the GIT, and to treat wounds [7]. The main active ingredients are anthraquinone glycosides, notably aloin (barbaloin A and B) and aloe emodin [33] (Fig. 4). The efficacy of these compounds is well established, their analytical standards are available, and many analytical methods have been published (Tables 2 and 3). Therefore, aloin A and B scored 8 points, while aloe emodin scored 7 points. The unit cost of analytical standards for aloin A is €44.0, that of aloin B is €60.5, and that of aloe emodin is €31.1. The WHO monograph recommends chemical and TLC methods for the identification of anthracenes and spectrophotometric determination of total anthracene glycosides as barbaloin equivalents for quantitative analysis [10]. These markers can be employed in identifying aloes obtained from different geographical regions, determining the best geographical sources of aloe vera gel products [123], and standardizing aloe products marketed for the treatment of constipation [10].
Because of suspected carcinogenicity [127], some regulatory authorities have banned the inclusion of aloe (whole leaf and latex) in oral over-the-counter nutraceuticals and laxative products. For instance, the International Aloe Science Council set a limit of 10 ppm total anthraquinone glycoside concentration (as aloin), while the European Medicines agency and Food and Drug authority set the limit at 0 ppm [128, 129]. In this case, aloin and aloe emodin are negative markers and can be used to assess the quality of over-the-counter products. However, the Uganda National Drug Authority and Uganda Bureau of Standards have not published any regulations on the use of aloes.
The main components of the gel are carbohydrates such as glucomannans and sugars [103]). One of the main compounds, acemannan, scored 8 points. Its biological activity is well studied, analytical markers are available and analytical methods have been developed (Tables 2 and 3). The main sugar, mannose 6 phosphate, scored only 3 points since its bioactivity is not well studied, and there are no analytical methods; thus, its concentration in the gel has not been reported. The unit cost of acemannan is approximately €20.8. For quality assurance of Aloe vera gel, the WHO monograph recommends a chemical test for carbohydrate and polysaccharide analysis by GC/MS. A molecular exclusion chromatographic method and a UV‒Vis spectrophotometric method for polysaccharides have also been published and are more affordable.
Assay methods for acemannan can be used to select high-yielding plant varieties, the best cultivation sites, suitable agronomic practices, and harvest seasons [130, 131].
Markers for Albizia coriaria
The dried stem bark is the plant material of interest for medicinal purposes. Commercial products are used for managing symptoms of respiratory tract disorders (whooping cough, catarrh, sore throat, congestion from asthma bronchitis, fever, sinusitis) [7]. Some pharmacologically active compounds, such as triterpenoids, lupeol, lupenone, betulinic acid and betulin [132, 133] (Fig. 4), have been elucidated with scores of 8, 6, 8, and 8, respectively. These compounds possess biological activities relevant to the commercial uses of the products, are available in pure form and have been quantified in many Albizia species, although assay methods specific to A. coriaria are scarce. The unit costs range between €68 for betulinic acid and €9.5 for betulinic acid.
There are no pharmacopoeial methods or monographs for A. coriaria materials. The identified markers can be used to monitor the batch-to-batch consistency of raw materials [134, 135] and to evaluate the efficiency of extraction methods.
Markers for Mangifera indica
The pharmacologically active compounds are obtained from extracts of the stem bark and leaves of Mangifera indica. The products containing these extracts are used for the management of respiratory tract disorders (whooping cough, catarrh, sore throat, congestion from asthma and bronchitis) [7]. Several phenolic compounds have been characterized and shown to possess biological activity relevant to the medicinal use of the materials. Mangiferin, catechin, quercetin and gallic acid scored 8. The unit costs of these markers ranged from €1.8 for quercetin to €34.5 for gallic acid. While epicatechin scored 5 points, its analytical standard is not readily available.
The identified markers can be used to monitor the batch-to-batch consistency of raw materials, to select the most suitable plant cultivars to source from [111] and to control the extraction and processing methods. There are no monographs for M. indica materials [7].
Markers for Azadirachta indica
The seed oil, leaves and stem bark are used as herbal materials. Products containing these herbal materials are used to manage respiratory tract disorders (cough, flu, sore throat, sinusitis), gastrointestinal disorders (gastric ulcers, flatulence, constipation) and lip balms (dry, cracked, and painful lips) [7]. The most important compounds are the limonoid azadirachtin and the tetranortriterpenes [84] nimbin, nimbidin, nimbolide and mahmoodin (Fig. 4). Most compounds scored 7 and above and are therefore suitable markers. The unit costs of these markers range from €105 to 289 for nimbin and azadirachtin, respectively. Although nimbolide and mahmoodin scored 5 points, they lack analytical standards and assay methods. According to the WHO monographs, high-performance liquid chromatography quantification of oxidized tetranortriterpenes in oil and leaf materials can be used for quality control [11]. Assays of these markers can be applied to select habitats for cultivation of neem, determine the best harvesting season and ensure consistency of materials obtained from various sources [115, 136, 137].
Markers for Zingiber officinalis (Ginger)
Herbal material is obtained from the rhizome, and the products are used to manage symptoms of respiratory tract disorders (cough, flu, sore throat, sinusitis, bronchial asthma, and fever) [7]. Gingerols and their dehydration products, shogaols (Fig. 4), have been extensively studied [89]. The compounds possess several pharmacological activities relevant to the application of the products; their analytical standards are readily available (apart from 12-gingerol), and analytical methods have been published. Thus, all compounds scored between 6 and 8 points and are thus suitable as markers. The unit cost of the analytical standards ranges between 50 and 60 euros. The WHO monographs recommend TLC fingerprinting with gingerols and shogaols as standards and GC and HPLC assay methods [10]. Since gingerols are dehydrated to form shogaols during storage and upon exposure to heat [138], the ratio of gingerols to shogaols can be used to determine the freshness of the ginger samples and optimize storage conditions. The quantities of the markers can be applied to optimize extraction processes and to study the phyto-equivalence of gingers obtained from different sources [139].
Markers for Warburgia ugandensis
The bark of the stem is used as a drug for the treatment of respiratory tract disorders (cough, measles symptoms, common colds, sinusitis, rhinitis, asthma, catarrh, bronchial congestion, and hiccups) and gastric ulcers [7]. While many compounds have been elucidated, the most important being the drimane sesquiterpenes bemadienolide, muzigadial, polygodial, warburganal, ugandensolide, and muzigadial [99] (Fig. 4), specific bioactivity studies are rare.
Only polygodial, muzigadial muzigadiolide, warburganal, and ugandensidial have been shown to possess some antimycobacterial activity [99]. In addition to limited pharmacological evidence, most of these compounds are not available in pure form for use as analytical standards, and no assay methods have been published. Thus, the compounds scored between only 1 and 3 points and are therefore not suitable quality control markers according to the Herb MaRS. In such cases, the WHO recommends the use of other constituents, whose biological activities are known even though the relevance of such activities to the traditional use of the plant may not be well established [3]. Thus, compounds such as linoleic acid, myrcene, and linalool, which are known components of W. ugandensis [140], can be used for its quality control; such evaluation will not be relevant to pharmacological standardization of the plant materials. This lack of pharmacological data, analytical methods and standards is common to plants that are exclusively used in Africa [8].
Conclusions
This study has demonstrated the applicability of the Herb MaRS to the quality assurance of herbal materials. Markers have been identified for the phytochemical standardization of the six most common medicinal plants in Uganda. The selected markers were as follows: (aromadendrine, α-terpineol, globulol, and 1,8-cineol) (in Eucalyptus globulus Labill. ); (aloin, aloe emodin, acemannan) (in Aloe barbadensis (L.) Burm.f. ), (lupeol, lupenone, betulinic acid, betulin, and catechin) (in Albizia coriaria Oliv.); (mangiferin, catechin, quercetin, and gallic acid (in Mangifera indica L.); (azadirachtin, nimbin, nimbidin (in Azadirachta indica A.Juss. ); and (6,8,10-gingerols, and 6-shogaol (in Zingiber officinalis Roscoe). For W. ugandensis, the compounds with known biological activity were not suitable as markers because they lack analytical standards and/or analytical methods. This implies that the Herb MaRS is only applicable for plants that have been extensively researched, such that it is possible to establish evidence of efficacy and/or safety. The method is also only applicable to plants whose phytochemical ingredients have analytical standards and corresponding analytical methods.
Recommendations
Markers for the other twenty-five (25) plant materials should be established using the same approach. The identified markers should be evaluated for suitability at the various stages of the production chain of herbal medicines in Uganda, i.e., from authentication and quality control of raw materials to evaluating reproducibility in the efficacy, safety, and stability of finished products notified by the National Drug Authority. Information about marker evaluation can be included in future Ugandan medicinal plant monographs and/or product databases to guide their quality assurance. In addition to the quantification of marker compounds, the construction of fingerprint databases for various plants is encouraged. The standardized fingerprints can then be used for routine quality assessment of the plant materials.
Acknowledgements
We appreciate the guidance and mentorship of Engineer Anke Weisheit (Business and Innovation manager), Dr. Casim Umba Tolo (Center Leader) of the Pharm-Biotechnology and Traditional Medicine Centre (PHARMBIOTRAC), Mbarara University of Science and Technology.
Authors' contributions
B.K conceived the idea, and drafted the manuscript. GA, E.I.M and H.K collected and analyzed bioactivity data. H.O and H.K collected and analyzed data on availability of analytical standards and assay methods. R.W drew the chemical structures, tables and graphs. F.P.K and O.P.E supervised the work. All authors reviewed and approved the final manuscripts.
Funding
This study was funded by the World Bank through the Pharm-Biotechnology and Traditional Medicine Centre (PHARMBIOTRAC), African Center of Excellence II (ACE-II) Project. The funder contributed research money and stipends (SD) but was not involved in the planning and implementation of the study.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This work was approved by the Mbarara University of Science and Technology, Research and Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Herbal Products Association. Good agricultural and collection practices and good manufacturing practices for botanical materials. 2021.
- 2.American Herbal Products Association. Standardization of botanical products: white paper. Silver Spring: American Herbal Products Association; 2003. p. 33.
- 3.World Health Organization. WHO guidelines for selecting marker substances of herbal origin for quality control of herbal medicines. In: Edited by Preparations WECoSfP. 2016. p. 72–85.
- 4.EMA E. Guideline on specifications: test procedures and acceptance criteria for herbal substances, herbal preparations and herbal medicinal products/traditional herbal medicinal products. In: París. Obtenido de www.ema.europa. eu; 2011.
- 5.Bensoussan A, Lee S, Murray C, Bourchier S, Van Der Kooy F, Pearson JL, Liu J, Chang D, Khoo C. Choosing chemical markers for quality assurance of complex herbal medicines: development and application of the herb MaRS criteria. Clin Pharmacol Ther. 2015;97(6):628–640. doi: 10.1002/cpt.100. [DOI] [PubMed] [Google Scholar]
- 6.National Drug Authority. Drug Register. In: National Drug Authorty; 2021.
- 7.Kaggwa B, Kyeyune H, Munanura EI, Anywar G, Lutoti S, Aber J, Bagoloire LK, Weisheit A, Tolo CU, Kamba PF, et al. Safety and efficacy of medicinal plants used to manufacture herbal products with regulatory approval in uganda: a cross-sectional study. Evid Based Complement Alternat Med. 2022;2022:1304839. doi: 10.1155/2022/1304839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaggwa B, Kyeyune H, Munanura EI, Anywar G, Lutoti S, Aber J, Bagoloire LK, Weisheit A, Tolo CU, Kamba PF. Safety and efficacy of medicinal plants used to manufacture herbal products with regulatory approval in Uganda: a cross-sectional study. Evid Based Complement Alternat Med. 2022;2022:1304839. doi: 10.1155/2022/1304839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray V, Shaw D. WHO monographs on selected medicinal plants, volume 2. Health Hyg. 2000;21(3):129. [Google Scholar]
- 10.World Health Organization . WHO monographs on selected medicinal plants. Geneva: World Health Organization; 1999. [Google Scholar]
- 11.World Health Organization . WHO monographs on selected medicinal plants: volume 3. Geneve: World Health Organization; 2007. [Google Scholar]
- 12.World Health Organization . WHO monographs on selected medicinal plants: volume 4. Geneve: World Health Organization; 2009. [Google Scholar]
- 13.Inter African Committee on Medicinal. African Traditional P, Organization of African M, Scientific U, Research T. African pharmacopoeia. Nigeria: Organization of African Unity, Scientific, Technical, & Research Commission: 2 edn. Lagos; 2014. [Google Scholar]
- 14.West African Health Organization. West African Herbal Pharmacopoeia BOBO-DIOULASSO (BURKINA FASO), Vol. 1. Bobo-Dioulasso: West African Health Organization; 2013.
- 15.Scott G, Springfield EP. Pharmaceutical monographs for 60 South African plant species used as traditional medicines. South African National Biodiversity Institute (SANBI). Available at http://www.plantzafrica.com/medmonographs. Accessed 15 Feb 2023.
- 16.Amić A, Milenković D, Marković Z, Cagardová D, Pedregal JR-G, Marković JMD. Impact of the phenolic O–H vs. C-ring C–H bond cleavage on the antioxidant potency of dihydrokaempferol. New J Chem. 2021;45(18):7977–7986. [Google Scholar]
- 17.Zeng Y, Nikitkova A, Abdelsalam H, Li J, Xiao J. Activity of quercetin and kaemferol against Streptococcus mutans biofilm. Arch Oral Biol. 2019;98:9–16. doi: 10.1016/j.archoralbio.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moo C-L, Osman MA, Yang S-K, Yap W–S, Ismail S, Lim S-H-E, Chong C-M, Lai K-S. Antimicrobial activity and mode of action of 1,8-cineol against carbapenemase-producing Klebsiella pneumoniae. Sci Rep. 2021;11(1):1–13. doi: 10.1038/s41598-021-00249-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Juergens U, Engelen T, Stöber M, Racké K, Gillissen A, Vetter H. Inhibitory activity of 1,8-cineol (eucalyptol) on cytokine production in human mononuclear phagocytes in vitro. Pulm Pharmacol Ther. 2004;17:281–287. doi: 10.1016/j.pupt.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Cai Z-M, Peng J-Q, Chen Y, Tao L, Zhang Y-Y, Fu L-Y, Long Q-D, Shen X-C. 1,8-Cineole: a review of source, biological activities, and application. J Asian Nat Prod Res. 2021;23(10):938–954. doi: 10.1080/10286020.2020.1839432. [DOI] [PubMed] [Google Scholar]
- 21.Jiang Z, Guo X, Zhang K, Sekaran G, Cao B, Zhao Q, Zhang S, Kirby GM, Zhang X. The essential oils and eucalyptol from Artemisia vulgaris L. prevent acetaminophen-induced liver injury by activating Nrf2–Keap1 and enhancing APAP clearance through nontoxic metabolic pathway. Front Pharmacol. 2019;10:782. doi: 10.3389/fphar.2019.00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luedtke K, Rushton A, Wright C, Geiss B, Juergens TP, May A. Transcranial direct current stimulation for the reduction of clinical and experimentally induced pain: a systematic review and meta-analysis. Clin J Pain. 2012;28(5):452–461. doi: 10.1097/AJP.0b013e31823853e3. [DOI] [PubMed] [Google Scholar]
- 23.Takaishi M, Fujita F, Uchida K, Yamamoto S, Sawada M, Hatai C, Shimizu M, Tominaga M. 1,8-cineole, a TRPM8 agonist, is a novel natural antagonist of human TRPA1. Mol Pain. 2012;8:1744 –8069-1748-1786. doi: 10.1186/1744-8069-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bachheti R. Chemical composition and antibacterial activity of the essential oil from the leaves of Eucalyptus globulus collected from Haramaya University, Ethiopia. Der Pharma Chem. 2015;7(2):209–214. [Google Scholar]
- 25.Mulyaningsih S, Sporer F, Reichling J, Wink M. Antibacterial activity of essential oils from Eucalyptus and of selected components against multidrug-resistant bacterial pathogens. Pharm Biol. 2011;49(9):893–899. doi: 10.3109/13880209.2011.553625. [DOI] [PubMed] [Google Scholar]
- 26.Brand C, Ferrante A, Prager R, Riley T, Carson C, Finlay-Jones J, Hart P. The water-soluble components of the essential oil of Melaleuca alternifolia (tea tree oil) suppress the production of superoxide by human monocytes, but not neutrophils, activated in vitro. Inflamm Res. 2001;50(4):213–219. doi: 10.1007/s000110050746. [DOI] [PubMed] [Google Scholar]
- 27.Quintans-Júnior LJ, Oliveira MG, Santana MF, Santana MT, Guimarães AG, Siqueira JS, De Sousa DP. Almeida RN: α-Terpineol reduces nociceptive behavior in mice. Pharm Biol. 2011;49(6):583–586. doi: 10.3109/13880209.2010.529616. [DOI] [PubMed] [Google Scholar]
- 28.de Witte P. Metabolism and pharmacokinetics of anthranoids. Pharmacology. 1993;47(Suppl 1):86–97. doi: 10.1159/000139847. [DOI] [PubMed] [Google Scholar]
- 29.Ishii Y, Tanizawa H, Takino Y. Studies of Aloe. III.: mechanism of Cathartic Effect.(2) Chem Pharm Bull. 1990;38(1):197–200. doi: 10.1248/cpb.38.197. [DOI] [PubMed] [Google Scholar]
- 30.Arosio B, Gagliano N, Fusaro LMP, Parmeggiani L, Tagliabue J, Galetti P, De Castri D, Moscheni C, Annoni G. Aloe-emodin quinone pretreatment reduces acute liver injury induced by carbon tetrachloride. Pharmacol Toxicol. 2000;87(5):229–233. doi: 10.1034/j.1600-0773.2000.d01-79.x. [DOI] [PubMed] [Google Scholar]
- 31.Im S-A, Oh S-T, Song S, Kim M-R, Kim D-S, Woo S–S, Jo TH, Park YI, Lee C-K. Identification of optimal molecular size of modified Aloe polysaccharides with maximum immunomodulatory activity. Int Immunopharmacol. 2005;5(2):271–279. doi: 10.1016/j.intimp.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 32.Park M-Y, Kwon H-J, Sung M-K. Evaluation of aloin and aloe-emodin as anti-inflammatory agents in aloe by using murine macrophages. Biosci Biotechnol Biochem. 2009;73(4):828–832. doi: 10.1271/bbb.80714. [DOI] [PubMed] [Google Scholar]
- 33.Sánchez-Machado DI, López-Cervantes J, Sendón R, Sanches-Silva A. Aloe vera: ancient knowledge with new frontiers. Trends Food Sci Technol. 2017;61:94–102. [Google Scholar]
- 34.Wang HH, Chung JG, Ho CC, Wu LT, Chang SH. Aloe-emodin effects on arylamine N-acetyltransferase activity in the bacterium Helicobacter pylori. Planta Med. 1998;64(02):176–178. doi: 10.1055/s-2006-957399. [DOI] [PubMed] [Google Scholar]
- 35.Roberts DB, Travis EL. Acemannan-containing wound dressing gel reduces radiation-induced skin reactions in C3H mice. Int J Radiat Oncol Biol Phys. 1995;32(4):1047–1052. doi: 10.1016/0360-3016(94)00467-y. [DOI] [PubMed] [Google Scholar]
- 36.Karaca K, Sharma J, Nordgren R. Nitric oxide production by chicken macrophages activated by Acemannan, a complex carbohydrate extracted from Aloe vera. Int J Immunopharmacol. 1995;17(3):183–188. doi: 10.1016/0192-0561(94)00102-t. [DOI] [PubMed] [Google Scholar]
- 37.Davis RH, Donato J, Hartman GM, Haas RC. Anti-inflammatory and wound healing activity of a growth substance in Aloe vera. J Am Podiatr Med Assoc. 1994;84(2):77–81. doi: 10.7547/87507315-84-2-77. [DOI] [PubMed] [Google Scholar]
- 38.Davis RH, DiDonato JJ, Johnson R, Stewart CB. Aloe vera, hydrocortisone, and sterol influence on wound tensile strength and anti-inflammation. J Am Podiatr Med Assoc. 1994;84(12):614–621. doi: 10.7547/87507315-84-12-614. [DOI] [PubMed] [Google Scholar]
- 39.Rathinavel T, Ammashi S, Shanmugam G. Analgesic and anti-inflammatory potential of Lupeol isolated from indian traditional medicinal plant Crateva adansonii screened through in vivo and in silico approaches. J Genet Eng Biotechnol. 2021;19(1):62. doi: 10.1186/s43141-021-00167-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sunitha S, Nagaraj M, Varalakshmi P. Hepatoprotective effect of lupeol and lupeol linoleate on tissue antioxidant defense system in cadmium-induced hepatotoxicity in rats. Fitoterapia. 2001;72(5):516–523. doi: 10.1016/s0367-326x(01)00259-3. [DOI] [PubMed] [Google Scholar]
- 41.Pereira Beserra F, Xue M, Maia GLA, Leite Rozza A, Helena Pellizzon C, Jackson CJ. Lupeol, a Pentacyclic Triterpene, promotes Migration, Wound Closure, and Contractile Effect in Vitro: possible involvement of PI3K/Akt and p38/ERK/MAPK pathways. Molecules. 2018;23(11):2819. doi: 10.3390/molecules23112819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ciurlea S, Ionescu D, Redes L, Soica C. Lupeol, a pentacylcic triterpene that reduces the lesions and irritability on murine skin and is effective on in vitro tumor models. J Agroaliment Process Technol. 2010;16(4):427–432. [Google Scholar]
- 43.Thirumalaisamy R, Ameen F, Subramanian A, Selvankumar T, Alwakeel S, Govarthanan M. In vitro and in-silico anti-inflammatory activity of Lupeol isolated from Crateva adansonii and its hidden molecular mechanism. Int J Pept Res Ther. 2020;26(4):2179–2189. [Google Scholar]
- 44.Lee C, Lee JW, Seo JY, Hwang SW, Im JP, Kim JS. Lupeol inhibits LPS-induced NF-kappa B signaling in intestinal epithelial cells and macrophages, and attenuates acute and chronic murine colitis. Life Sci. 2016;146:100–108. doi: 10.1016/j.lfs.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 45.Okusa PN, Stévigny C, Névraumont M, Gelbcke M, Van Anrwerpen P, Braekman JC, Duez P. Ferulaldehyde and lupeol as direct and indirect antimicrobial compounds from Cordia gilletii (Boraginaceae) root barks. Nat Prod Commun. 2014;9(5):1934578X1400900506. [PubMed] [Google Scholar]
- 46.Ahamed B, Krishna V, Gowdru H, Rajanaika H, Kumaraswamy H, Rajshekarappa S, Dandin C, Mahadevan K. Isolation of bactericidal constituents from the stem bark extract of Grewia tiliaefolia Vahl. Res J Med Plant. 2007;1(3):72–82. [Google Scholar]
- 47.Mutai C, Keter L, Ngeny L, Jeruto P. Effects of triterpenoids on Herpes Simplex Virus Type1 (Hsv-1) in vitro. 2012;1:140. 10.4172/scientificreports.140.
- 48.Tanaka T, Ikeda T, Kaku M, Zhu X-H, Okawa M, Yokomizo K, Uyeda M, Nohara T. A new Lignan glycoside and phenylethanoid glycosides from Strobilanthes cusia B REMEK. Chem Pharm Bull. 2004;52(10):1242–1245. doi: 10.1248/cpb.52.1242. [DOI] [PubMed] [Google Scholar]
- 49.Yun Y, Han S, Park E, Yim D, Lee S, Lee C-K, Cho K, Kim K. Immunomodulatory activity of betulinic acid by producing pro-inflammatory cytokines and activation of macrophages. Arch Pharm Res. 2003;26(12):1087–1095. doi: 10.1007/BF02994763. [DOI] [PubMed] [Google Scholar]
- 50.Oyebanji BO, Saba AB, Oridupa OA. Studies on the anti-inflammatory, analgesic and antipyrexic activities of betulinic acid derived from Tetracera potatoria. Afr J Tradit Complement Altern Med. 2014;11(1):30–33. [PMC free article] [PubMed] [Google Scholar]
- 51.Sakna ST, Maghraby YR, Abdelfattah MS, et al. Phytochemical diversity and pharmacological effects of triterpenes from genus Ziziphus: a comprehensive review. Phytochem Rev. 2022 doi: 10.1007/s11101-022-09835-y. [DOI] [Google Scholar]
- 52.Oloyede HOB, Ajiboye HO, Salawu MO, Ajiboye TO. Influence of oxidative stress on the antibacterial activity of betulin, betulinic acid and ursolic acid. Microb Pathog. 2017;111:338–344. doi: 10.1016/j.micpath.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 53.Kurokawa M, Basnet P, Ohsugi M, Hozumi T, Kadota S, Namba T, Kawana T, Shiraki K. Anti-herpes Simplex Virus Activity of Moronic Acid purified fromRhus javanica in Vitro and in vivo. J Pharmacol Exp Ther. 1999;289(1):72–78. [PubMed] [Google Scholar]
- 54.Chiou Y-S, Huang Q, Ho C-T, Wang Y-J, Pan M-H. Directly interact with Keap1 and LPS is involved in the anti-inflammatory mechanisms of (-)-epicatechin-3-gallate in LPS-induced macrophages and endotoxemia. Free Radic Biol Med. 2016;94:1–16. doi: 10.1016/j.freeradbiomed.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 55.Kim JM, Kang JY, Park SK, Moon JH, Kim MJ, Lee HL, Jeong HR, Kim JC, Heo HJ. Powdered Green Tea (Matcha) attenuates the cognitive dysfunction via the regulation of systemic inflammation in chronic PM2. 5-exposed BALB/c mice. Antioxidants. 2021;10(12):1932. doi: 10.3390/antiox10121932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mishra CB, Pandey P, Sharma RD, Malik MZ, Mongre RK, Lynn AM, Prasad R, Jeon R, Prakash A. Identifying the natural polyphenol catechin as a multitargeted agent against SARS-CoV-2 for the plausible therapy of COVID-19: an integrated computational approach. Brief Bioinform. 2021;22(2):1346–1360. doi: 10.1093/bib/bbaa378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Onishi S, Mori T, Kanbara H, Habe T, Ota N, Kurebayashi Y, Suzuki T. Green tea catechins adsorbed on the murine pharyngeal mucosa reduce influenza a virus infection. J Funct Foods. 2020;68:103894. [Google Scholar]
- 58.Song J-M, Lee K-H, Seong B-L. Antiviral effect of catechins in green tea on influenza virus. Antivir Res. 2005;68(2):66–74. doi: 10.1016/j.antiviral.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 59.Pardo-Andreu GL, Sánchez-Baldoquín C, Ávila-González R, Delgado R, Naal Z, Curti C. Fe (III) improves antioxidant and cytoprotecting activities of mangiferin. Eur J Pharmacol. 2006;547(1–3):31–36. doi: 10.1016/j.ejphar.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 60.Li H, Wang Q, Ding Y, Bao C, Li W. Mangiferin ameliorates Porphyromonas gingivalis-induced experimental periodontitis by inhibiting phosphorylation of nuclear factor‐κB and Janus kinase 1–signal transducer and activator of transcription signaling pathways. J Periodontal Res. 2017;52(1):1–7. doi: 10.1111/jre.12360. [DOI] [PubMed] [Google Scholar]
- 61.Vieira AB, Coelho LP, Insuela DB, Carvalho VF, Dos Santos MH, Silva PM, Martins MA. Mangiferin prevents guinea pig tracheal contraction via activation of the nitric oxide-cyclic GMP pathway. PLoS One. 2013;8(8):e71759. doi: 10.1371/journal.pone.0071759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rivera DG, Hernández I, Merino N, Luque Y, Álvarez A, Martín Y, Amador A, Nuevas L, Delgado R. Mangifera indica L. extract (Vimang) and mangiferin reduce the airway inflammation and Th2 cytokines in murine model of allergic asthma. J Pharm Pharmacol. 2011;63(10):1336–1345. doi: 10.1111/j.2042-7158.2011.01328.x. [DOI] [PubMed] [Google Scholar]
- 63.Biswas T, Sen A, Roy R, Maji S, Maji HS. Isolation of mangiferin from flowering buds of Mangifera indica L and its evaluation of in vitro antibacterial activity. J Pharm Anal. 2015;4(3):49–56. [Google Scholar]
- 64.Sahu S, Das BK, Pradhan J, Mohapatra B, Mishra B, Sarangi N. Effect of Magnifera indica kernel as a feed additive on immunity and resistance to Aeromonas hydrophila in Labeo rohita fingerlings. Fish Shellfish Immunol. 2007;23(1):109–118. doi: 10.1016/j.fsi.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 65.Du S, Liu H, Lei T, Xie X, Wang H, He X, Tong R, Wang Y. Mangiferin: an effective therapeutic agent against several disorders. Mol Med Rep. 2018;18(6):4775–4786. doi: 10.3892/mmr.2018.9529. [DOI] [PubMed] [Google Scholar]
- 66.Zheng MS, Lu ZY. Antiviral effect of mangiferin and isomangiferin on herpes simplex virus. Chin Med J (Engl) 1990;103(2):160–165. [PubMed] [Google Scholar]
- 67.Oh WY, Ambigaipalan P, Shahidi F. Preparation of quercetin esters and their antioxidant activity. J Agric Food Chem. 2019;67(38):10653–10659. doi: 10.1021/acs.jafc.9b04154. [DOI] [PubMed] [Google Scholar]
- 68.Wang Y, Tang Y, Li Z, Hua Q, Wang L, Song X, Zou B, Ding M, Zhao J, Tang C. Joint toxicity of a multiheavy metal mixture and chemoprevention in sprague dawley rats. Int J Environ Res Public Health. 2020;17(4):1451. doi: 10.3390/ijerph17041451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kahkeshani N, Farzaei F, Fotouhi M, Alavi SS, Bahramsoltani R, Naseri R, Momtaz S, Abbasabadi Z, Rahimi R, Farzaei MH. Pharmacological effects of gallic acid in health and diseases: a mechanistic review. Iran J Basic Med Sci. 2019;22(3):225. doi: 10.22038/ijbms.2019.32806.7897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kang M-S, Oh J-S, Kang I-C, Hong S-J, Choi C-H. Inhibitory effect of methyl gallate and gallic acid on oral bacteria. J Microbiol. 2008;46(6):744–750. doi: 10.1007/s12275-008-0235-7. [DOI] [PubMed] [Google Scholar]
- 71.Lee JH, Oh M, Seok JH, Kim S, Lee DB, Bae G, Bae HI, Bae SY, Hong YM, Kwon SO, et al. Antiviral Effects of Black Raspberry (Rubus coreanus) seed and its gallic acid against Influenza Virus infection. Viruses. 2016;8(6):157. doi: 10.3390/v8060157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang Y, Li Y, Yu H, Gao C, Liu L, Xing M, Liu L, Yao P. Quercetin attenuates chronic ethanol hepatotoxicity: implication of free iron uptake and release. Food Chem Toxicol. 2014;67:131–138. doi: 10.1016/j.fct.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 73.Granado-Serrano AB, Martín MA, Bravo L, Goya L, Ramos S. Quercetin modulates Nrf2 and glutathione-related defenses in HepG2 cells: involvement of p38. Chem Biol Interact. 2012;195(2):154–164. doi: 10.1016/j.cbi.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 74.Boesch-Saadatmandi C, Loboda A, Wagner AE, Stachurska A, Jozkowicz A, Dulak J, Döring F, Wolffram S, Rimbach G. Effect of quercetin and its metabolites isorhamnetin and quercetin-3-glucuronide on inflammatory gene expression: role of miR-155. J Nutr Biochem. 2011;22(3):293–299. doi: 10.1016/j.jnutbio.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 75.Li Y, Yao J, Han C, Yang J, Chaudhry MT, Wang S, Liu H, Yin Y. Quercetin, inflammation and immunity. Nutrients. 2016;8(3):167. doi: 10.3390/nu8030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hossion AM, Zamami Y, Kandahary RK, Tsuchiya T, Ogawa W, Iwado A, Sasaki K. Quercetin diacylglycoside analogs showing dual inhibition of DNA gyrase and topoisomerase IV as novel antibacterial agents. J Med Chem. 2011;54(11):3686–3703. doi: 10.1021/jm200010x. [DOI] [PubMed] [Google Scholar]
- 77.Safwat NA, Kashef MT, Aziz RK, Amer KF, Ramadan MA. Quercetin 3-O-glucoside recovered from the wild egyptian Sahara plant, Euphorbia paralias L., inhibits glutamine synthetase and has antimycobacterial activity. Tuberculosis. 2018;108:106–113. doi: 10.1016/j.tube.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 78.Fan D, Zhou X, Zhao C, Chen H, Zhao Y, Gong X. Anti-inflammatory, antiviral and quantitative study of quercetin-3-O-β-D-glucuronide in Polygonum perfoliatum L. Fitoterapia. 2011;82(6):805–810. doi: 10.1016/j.fitote.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 79.Di Petrillo A, Orrù G, Fais A, Fantini MC. Quercetin and its derivates as antiviral potentials: a comprehensive review. Phytother Res. 2022;36(1):266–278. doi: 10.1002/ptr.7309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thoh M, Babajan B, Raghavendra PB, Sureshkumar C, Manna SK. Azadirachtin interacts with retinoic acid receptors and inhibits retinoic acid-mediated biological responses. J Biol Chem. 2011;286(6):4690–4702. doi: 10.1074/jbc.M110.169334. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81.Sarmiento WC, Maramba CC, Gonzales MLM. An in vitro study on the antibacterial effect of neem (Azadirachta indica) leaf extract on methicillin-sensitive and Methicillin-resistant Staphylococcus aureus. PIDSP J. 2011;12(1):40–45. [Google Scholar]
- 82.Bhargava K, Gupta M, Gupta G, Mitra C. Anti-inflammatory activity of saponins and ot-her natural products. Indian J Med Res. 1970;58(6):724–730. [PubMed] [Google Scholar]
- 83.Pillai N, Santhakumari G. Anti-arthritic and anti-inflammatory actions of nimbidin. Planta Med. 1981;43(09):59–63. doi: 10.1055/s-2007-971474. [DOI] [PubMed] [Google Scholar]
- 84.Hossain MA, Al-Toubi WA, Weli AM, Al-Riyami QA, Al-Sabahi JN. Identification and characterization of chemical compounds in different crude extracts from leaves of Omani neem. J Taibah Univ Sci. 2013;7(4):181–188. [Google Scholar]
- 85.Pillai N, Santhakumari G. Effect of nimbidin on gastric acid secretion. Anc Sci Life. 1985;5(2):91. [PMC free article] [PubMed] [Google Scholar]
- 86.Alam A, Haldar S, Thulasiram HV, Kumar R, Goyal M, Iqbal MS, Pal C, Dey S, Bindu S, Sarkar S. Novel anti-inflammatory activity of epoxyazadiradione against macrophage migration inhibitory factor: inhibition of tautomerase and proinflammatory activities of macrophage migration inhibitory factor. J Biol Chem. 2012;287(29):24844–24861. doi: 10.1074/jbc.M112.341321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rojanapo W, Suwanno S, Somaree R, Glinsukon T, Thebtaranonth Y. Mutagenic and antimicrobial testing activity of nimbolide and nimbic acid. J Sci Thailand. 1985;11:177–188. [Google Scholar]
- 88.Ara I, Siddiqui BS, Faizi S, Siddiqui S. Structurally novel diterpenoid constituents from the stem bark of Azadirachta indica (Meliaceae) J Chem Soc Perkin Trans 1. 1989;2:343–5. [Google Scholar]
- 89.Mustafa T, Srivastava K, Jensen K. Pharmacology of ginger, Zingiber officinale. J Drug Develop. 1993;6:25–39. [Google Scholar]
- 90.Suekawa M, Yuasa K, Isono M, Sone H, Ikeya Y, Sakakibara I, Aburada M, Hosoya E. Pharmacological studies on ginger. IV. Effect of (6)-shogaol on the arachidonic cascade. Nihon Yakurigaku Zasshi. 1986;88(4):263–269. doi: 10.1254/fpj.88.263. [DOI] [PubMed] [Google Scholar]
- 91.Aimbire F, Penna S, Rodrigues M, Rodrigues K, Lopes-Martins RAB, Sertié JAA. Effect of hydroalcoholic extract of Zingiber officinalis rhizomes on LPS-induced rat airway hyperreactivity and lung inflammation. Prostaglandins Leukot Essent Fatty Acids. 2007;77(3–4):129–138. doi: 10.1016/j.plefa.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 92.Hiserodt R, Franzblau S, Rosen R. Isolation of 6-, 8-, and 10-Gingerol from Ginger Rhizome by HPLC and preliminary evaluation of inhibition of Mycobacterium a vium and Mycobacterium t uberculosis. J Agric Food Chem. 1998;46(7):2504–2508. [Google Scholar]
- 93.Park M, Bae J, Lee DS. Antibacterial activity of [10]-gingerol and [12]‐gingerol isolated from ginger rhizome against periodontal bacteria. Phytother Res. 2008;22(11):1446–1449. doi: 10.1002/ptr.2473. [DOI] [PubMed] [Google Scholar]
- 94.Mahady GB, Pendland SL, Yun GS, Lu Z-Z, Stoia A. Ginger (Zingiber officinale Roscoe) and the gingerols inhibit the growth of Cag A + strains of Helicobacter pylori. Anticancer Res. 2003;23:3699. [PMC free article] [PubMed] [Google Scholar]
- 95.Yamahara J, Rong HQ, Iwamoto M, Kobayashi G, Matsuda H, Fujimura H. Active components of ginger exhibiting anti-serotonergic action. Phytother Res. 1989;3(2):70–71. [Google Scholar]
- 96.Huang Q, Iwamoto M, Tanaka AOKIS, Tajima N, Yamahara K, Takaishi J, Yoshida Y, Tomimatsu M, Tamai T. Anti-5-hydroxytryptamine3 effect of galanolactone, diterpenoid isolated from ginger. Chem Pharm Bull. 1991;39(2):397–399. doi: 10.1248/cpb.39.397. [DOI] [PubMed] [Google Scholar]
- 97.Aeschbach R, Löliger J, Scott B, Murcia A, Butler J, Halliwell B, Aruoma O. Antioxidant actions of thymol, carvacrol, 6-gingerol, zingerone and hydroxytyrosol. Food Chem Toxicol. 1994;32(1):31–36. doi: 10.1016/0278-6915(84)90033-4. [DOI] [PubMed] [Google Scholar]
- 98.da Cunha FM, Fröde TS, Mendes GL, Malheiros A, Cechinel Filho V, Yunes RA, Calixto JB. Additional evidence for the anti-inflammatory and anti-allergic properties of the sesquiterpene polygodial. Life Sci. 2001;70(2):159–169. doi: 10.1016/s0024-3205(01)01387-x. [DOI] [PubMed] [Google Scholar]
- 99.Wube AA, Bucar F, Gibbons S, Asres K. Sesquiterpenes from Warburgia ugandensis and their antimycobacterial activity. Phytochemistry. 2005;66(19):2309–2315. doi: 10.1016/j.phytochem.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 100.Khumalo G, Sadgrove N, Van Vuuren S, Van Wyk B-E. Antimicrobial activity of volatile and nonvolatile isolated compounds and extracts from the bark and leaves of Warburgia salutaris (Canellaceae) against skin and respiratory pathogens. South Afr J Bot. 2019;122:547–550. [Google Scholar]
- 101.Apel MA, Rodrigues RA, Soares LAL, Henriques AT. Quantification of the components in commercial essential oil of Eucalyptus globulus labill. By gas chromatography–GC-FID and GC–MS. Drug Anal Res. 2017;1(2):9–14. [Google Scholar]
- 102.Elsohly MA, Gul W, Avula B, Khan IA. Determination of the anthraquinones aloe-emodin and aloin-A by liquid chromatography with mass spectrometric and diode array detection. J AOAC Int. 2007;90(1):28–42. [PubMed] [Google Scholar]
- 103.Cuevas BA, Méndez CHH, Flores II, Solís-Pereira S, Cuevas-Glory L, Muñoz GR. Y Vargas MdLV, Cortez JT: Main Polysaccharides isolated and quantified of Aloe vera Gel in different Seasons of the year. Food Nutr Sci. 2016;7(06):447. [Google Scholar]
- 104.Metcalfe C. Quantitation of aloe vera polysaccharides by O-Acetyl and UV–Vis spectrophotometry: first action 2018.14. J AOAC Int. 2019;102(4):1091–1094. doi: 10.5740/jaoacint.18-0400. [DOI] [PubMed] [Google Scholar]
- 105.Somwong P, Theanphong O. Quantitative analysis of triterpene lupeol and anti-inflammatory potential of the extracts of traditional pain-relieving medicinal plants Derris scandens, Albizia procera, and Diospyros rhodocalyx. J Adv Pharm Technol Res. 2021;12(2):147–151. doi: 10.4103/japtr.JAPTR_13_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kaggwa B, Munanura EI, Kyeyune H, Anywar G, Okella H, Ajayi CO, Wangalwa R, Mulangwa J, Sesaazi CD, Bagoloire LK. Evaluation of catechin, lupeol, and betulinic acid as markers for the chromatographic quality control of Albizia coriaria raw materials; an experimental study. J Med Plants Res. 2023;17(5):180–200. [Google Scholar]
- 107.Andrade EM, Teixeira JS, Silva DK, Santos TBd, Korn MG, Brandão HN, Ferraz CG, Meira CS, Soares MB, Guimarães ET. Phytochemical analysis, multielement composition and biological activities of extracts and lupenone from Albizia inundata (Mart.) Barneby & JW Grimes. J Braz Chem Soc. 2020;31:1825–1837. [Google Scholar]
- 108.Tatke P, Desai S, Gabhe S. Estimation of betulinic acid in extracts and formulations containing Albizialebbeck by HPLC. World J Pharm Res. 2014;3(6):1277–1286. [Google Scholar]
- 109.Desai S, Tatke P, Gaitonde V, Gabhe S. Fast HPLC-DAD method for estimation of Catechin for standardization of extracts and antiasthmatic polyherbal formulations containing Albizia lebbeck. Indian J Pharm Educ Res. 2020;54(3):550–555. [Google Scholar]
- 110.Zhang X, Su B, Li J, Li Y, Lu D, Zhu K, Pei H, Zhao M. Analysis by RP-HPLC of mangiferin component correlation between Medicinal Loranthus and their Mango host trees. J Chromatogr Sci. 2012;52(1):1–4. doi: 10.1093/chromsci/bms196. [DOI] [PubMed] [Google Scholar]
- 111.Núñez Sellés AJ, Vélez Castro HT, Agüero-Agüero J, González-González J, Naddeo F, De Simone F, Rastrelli L. Isolation and quantitative analysis of phenolic antioxidants, free sugars, and polyols from mango (Mangifera indica L.) stem bark aqueous decoction used in Cuba as a nutritional supplement. J Agric Food Chem. 2002;50(4):762–766. doi: 10.1021/jf011064b. [DOI] [PubMed] [Google Scholar]
- 112.Gottumukkala RV, Nadimpalli N, Sukala K, Subbaraju GV. Determination of catechin and epicatechin content in chocolates by high-performance liquid chromatography. Int Sch Res Notices. 2014;2014:628196. doi: 10.1155/2014/628196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kim TJ, Kim YJ, Seo WD, Park SU, Kim JK. Improved quantification of catechin and epicatechin in red rice (Oryza sativa L.) using stable isotope dilution liquid chromatography–mass spectrometry. Appl Biol Chem. 2022;65(1):85. [Google Scholar]
- 114.Ramesh A, Balasubramanian M. Rapid preconcentration method for the determination of azadirachtin-A and -B, nimbin and salannin in neem oil samples by using graphitized carbon solid phase extraction. Analyst. 1999;124(1):19–21. doi: 10.1039/a806527f. [DOI] [PubMed] [Google Scholar]
- 115.Sidhu OP, Kumar V, Behl HM. Variability in triterpenoids (nimbin and salanin) composition of neem among different provenances of India. Ind Crops Prod. 2004;19(1):69–75. [Google Scholar]
- 116.Suttiarporn P, Choommongkol V. Microwave-assisted improved extraction and purification of Anticancer Nimbolide from Azadirachta indica (neem) Leaves. Molecules. 2020;25(12):2913. doi: 10.3390/molecules25122913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ashraf K, Mujeeb M, Ahmad A, Ahmad S, Ahmad N, Amir M. Determination of gingerols in ginger by ultrahigh-performance liquid chromatography-tandem mass spectrometry. Anal Lett. 2014;47(12):2120–2128. [Google Scholar]
- 118.Tao Y, Li W, Liang W, Van Breemen RB. Identification and quantification of gingerols and related compounds in ginger dietary supplements using high-performance liquid chromatography-tandem mass spectrometry. J Agric Food Chem. 2009;57(21):10014–10021. doi: 10.1021/jf9020224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Park SY, Jung MY. UHPLC-ESI‐MS/MS for the quantification of eight major Gingerols and Shogaols in ginger products: Effects of ionization polarity and mobile phase modifier on the sensitivity. J Food Sci. 2016;81(10):C2457–2465. doi: 10.1111/1750-3841.13429. [DOI] [PubMed] [Google Scholar]
- 120.Aldoghaim FS, Flematti GR, Hammer KA. Antimicrobial activity of several cineole-rich western australian Eucalyptus essential oils. Microorganisms. 2018;6(4):122. doi: 10.3390/microorganisms6040122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kanama SK, Viljoen AM, Kamatou GP, Chen W, Sandasi M, Adhami H-R, Van Wyk B-E. Simultaneous quantification of anthrones and chromones in Aloe ferox (Cape aloes) using UHPLC–MS. Phytochem Lett. 2015;13:85–90. [Google Scholar]
- 122.Reynolds T. The compounds in Aloe leaf exudates: a review. Bot J Linn Soc. 1985;90(3):157–177. [Google Scholar]
- 123.Kumar S, Yadav M, Yadav A, Rohilla P, Yadav JP. Antiplasmodial potential and quantification of aloin and aloe-emodin in Aloe vera collected from different climatic regions of India. BMC Complement Altern Med. 2017;17(1):369. doi: 10.1186/s12906-017-1883-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fitmawati F, Resida E, Kholifah SN, Roza RM, Almurdani M, Emrizal E. Phytochemical screening and antioxidant profiling of Sumatran wild mangoes (Mangifera spp.): a potential source for medicine antidegenerative effects. F1000Res. 2020;9:220. doi: 10.12688/f1000research.22380.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Song L, Wang J, Gao Q, Ma X, Wang Y, Zhang Y, Xun H, Yao X, Tang F. Simultaneous determination of five azadirachtins in the seed and leaf extracts of Azadirachta indica by automated online solid-phase extraction coupled with LC–Q-TOF–MS. Chem Cent J. 2018;12(1):1–9. doi: 10.1186/s13065-018-0453-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Forim MR, Cass QB, Fernandes JB, Vieira PC. Simultaneous quantification of azadirachtin and 3-tigloylazadirachtol in brazilian seeds and oil of Azadirachta indica: application to quality control and marketing. Anal Methods. 2010;2(7):860–869. [Google Scholar]
- 127.Boudreau MD, Olson GR, Tryndyak VP, Bryant MS, Felton RP, Beland FA. From the cover: aloin, a component of the aloe vera plant leaf, induces pathological changes and modulates the composition of microbiota in the large intestines of f344/N male rats. Toxicol Sci. 2017;158(2):302–318. doi: 10.1093/toxsci/kfx105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bayne HJ. FDA issues final rule banning use of aloe and cascara sagrada in OTC drug products. HerbalGram. 2002;56:56. [Google Scholar]
- 129.EUR-Lex 32021R0468 EN EUR-Lex Commission Regulation (EU) 2021/468 of 18 March 2021. Available online: https://eur-lex.europa.eu/eli/reg/2021/468/oj. Accessed 5 Feb 2023.
- 130.Lucini L, Pellizzoni M, Molinari GP. Anthraquinones and β-polysaccharides content and distribution in Aloe plants grown under different light intensities. Biochem Syst Ecol. 2013;51:264–268. [Google Scholar]
- 131.Ling-Tong JIANGC-Q, Feng Q, Na S, Chang-Hai Y, Xiao-Ming W, ZHENG Q-S Distribution of mineral nutrients and active ingredients in Aloe vera irrigated with diluted seawater. Pedosphere. 2014;24(6):722–730. [Google Scholar]
- 132.Byamukama R, Barbara G, Namukobe J, Heydenreich M, Kiremire BT. Bioactive compounds in the stem bark of Albizia coriaria (Welw. Ex Oliver) Int J Biol Chem Sci. 2015;9(2):1013–1024. [Google Scholar]
- 133.Omara T, Kiprop AK, Kosgei VJ. Isolation and characterization of compounds in ethanolic extract of Albizia coriaria (welw ex. Oliver) leaves: a further evidence of its ethnomedicinal diversity. Bull Natl Res Centre. 2022;46(1):1–15. [Google Scholar]
- 134.Omara T, Kiprop AK, Kosgei VJ. Intraspecific variation of phytochemicals, antioxidant, and antibacterial activities of different solvent extracts of Albizia coriaria leaves from some agroecological zones of Uganda. Evid Based Complement Alternat Med. 2021;2021:2335454. doi: 10.1155/2021/2335454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Anywar G, Kakudidi E, Byamukama R, Mukonzo J, Schubert A, Oryem-Origa H. Indigenous traditional knowledge of medicinal plants used by herbalists in treating opportunistic infections among people living with HIV/AIDS in Uganda. J Ethnopharmacol. 2020;246:112205. doi: 10.1016/j.jep.2019.112205. [DOI] [PubMed] [Google Scholar]
- 136.Sidhu OP, Behl HM. Seasonal variation in azadirachtins in seeds of Azadirachta indica. Curr Sci. 1996:1084–6.
- 137.Gupta V, Ahlawat S, Kumar R, Ajit Datta A. Effect of season and year on azadirachtin A and oil content in neem (Azadirachta indica A. Juss) seeds and relationship of azadirachtin A and oil content with rainfall, temperature and humidity. Curr Sci. 2010;10:953–6. [Google Scholar]
- 138.Jung MY, Lee MK, Park HJ, Oh E-B, Shin JY, Park JS, Jung SY, Oh J-H, Choi D-S. Heat-induced conversion of gingerols to shogaols in ginger as affected by heat type (dry or moist heat), sample type (fresh or dried), temperature and time. Food Sci Biotechnol. 2018;27(3):687–693. doi: 10.1007/s10068-017-0301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pace R, Martinelli EM. The phytoequivalence of herbal extracts: a critical evaluation. Fitoterapia. 2022;162:105262. doi: 10.1016/j.fitote.2022.105262. [DOI] [PubMed] [Google Scholar]
- 140.Kioy D, Gray AI, Waterman PG. A comparative study of the stem-bark drimane sesquiterpenes and leaf volatile oils of Warburgia ugandensis and W. stuhlmannii. Phytochemistry. 1990;29(11):3535–3538. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.